Long-Term Outcomes of Endoscopic Submucosal Dissection for Superficial Esophageal Squamous Cell Carcinoma
Simple Summary
Abstract
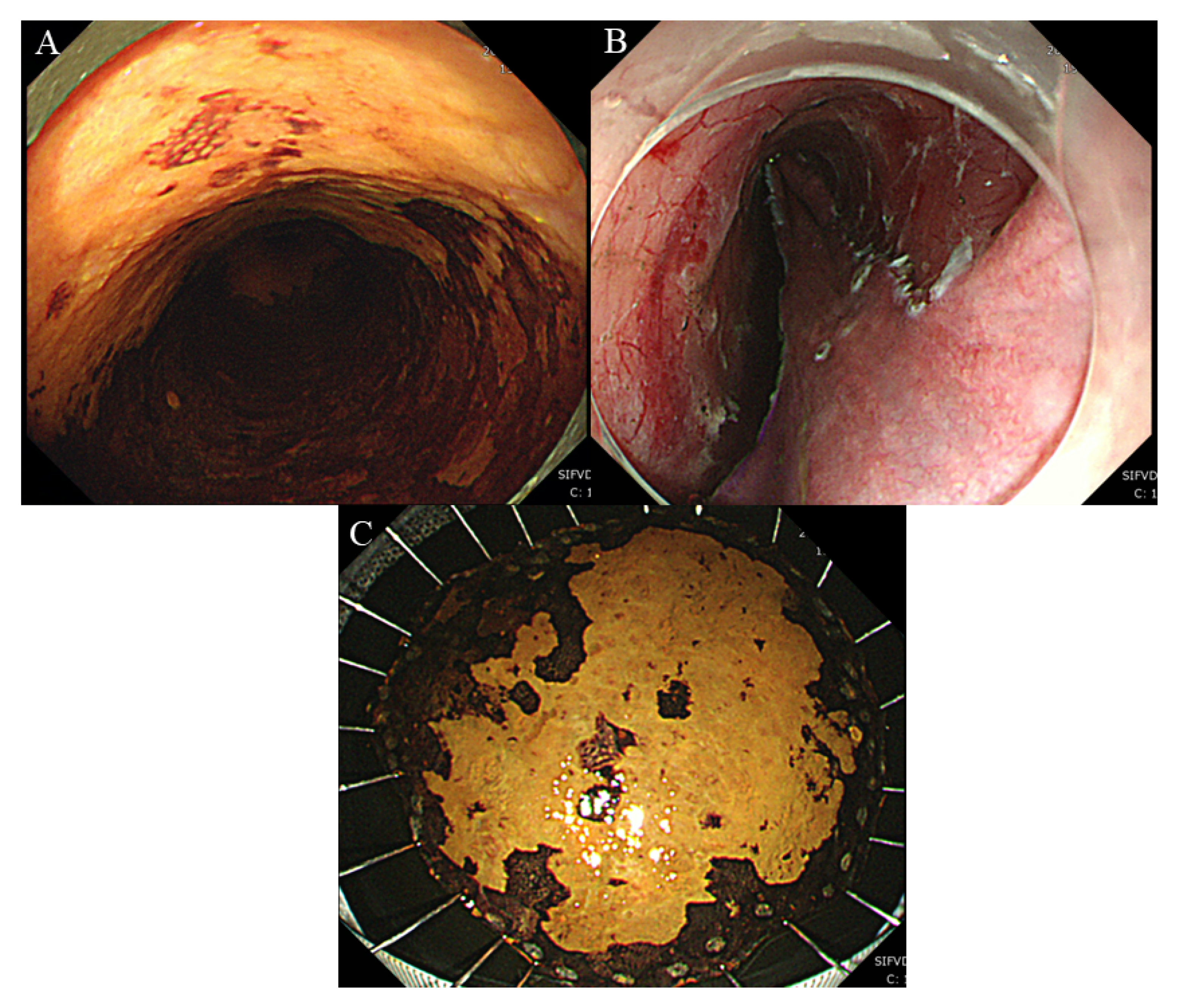
1. Introduction
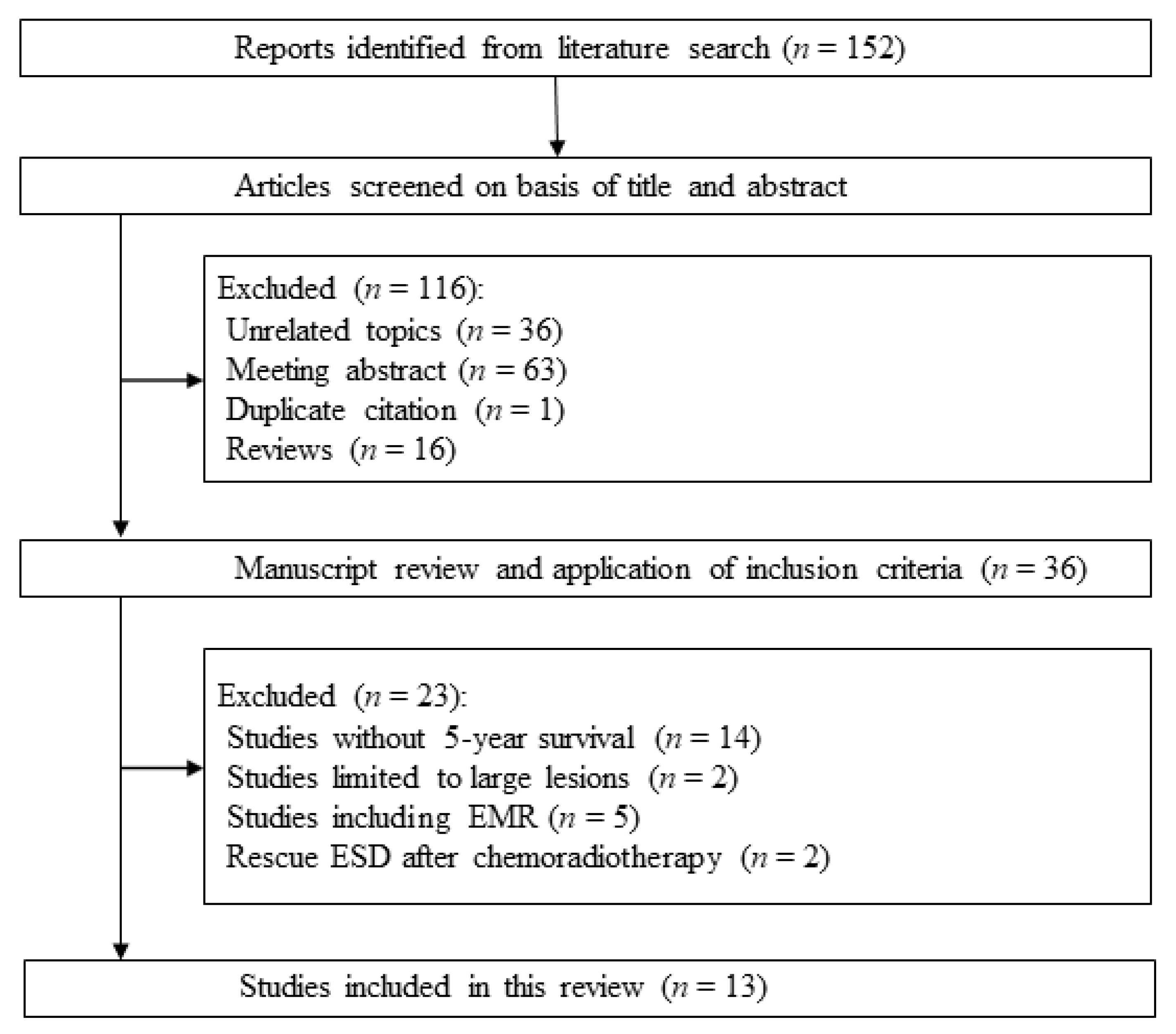
2. Literature Search and Selection
3. Long-Term Outcomes of ESD for Superficial Esophageal Squamous Cell Carcinoma
4. Long-Term Outcomes of ESD for Superficial Esophageal Squamous Cell Carcinoma without Additional Treatment
5. Comparison between Elderly and the Younger Generation in Esophageal ESD
6. Comparison between ESD and Other Resection Methods for Superficial Esophageal Squamous Cell Carcinoma
7. Chemoradiotherapy and ESD for Esophageal Squamous Cell Carcinoma with Submucosal Invasion
8. Cumulative Metachronous Cancer Rate after Esophageal ESD
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Oda, I.; Shimizu, Y.; Yoshio, T.; Katada, C.; Yokoyama, T.; Yano, T.; Suzuki, H.; Abiko, S.; Takemura, K.; Koike, T.; et al. Long-term outcome of endoscopic resection for intramucosal esophageal squamous cell cancer: A secondary analysis of the Japan Esophageal Cohort study. Endoscopy 2020. [Google Scholar] [CrossRef] [PubMed]
- Ono, S.; Fujishiro, M.; Koike, K. Endoscopic submucosal dissection for superficial esophageal neoplasms. World J. Gastrointest. Endosc. 2012, 4, 162–166. [Google Scholar] [CrossRef]
- Inoue, H.; Endo, M. Endoscopic esophageal mucosal resection using a transparent tube. Surg. Endosc. 1990, 4, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Gotoda, T.; Kondo, H.; Ono, H.; Saito, Y.; Yamaguchi, H.; Saito, D.; Yokota, T. A new endoscopic mucosal resection procedure using an insulation-tipped electrosurgical knife for rectal flat lesions: Report of two cases. Gastrointest. Endosc. 1999, 50, 560–563. [Google Scholar] [CrossRef]
- Nishizawa, T.; Yahagi, N. Long-Term Outcomes of Using Endoscopic Submucosal Dissection to Treat Early Gastric Cancer. Gut Liver 2017, 12, 119–124. [Google Scholar] [CrossRef]
- Oyama, T.; Tomori, A.; Hotta, K.; Morita, S.; Kominato, K.; Tanaka, M.; Miyata, Y. Endoscopic Submucosal Dissection of Early Esophageal Cancer. Clin. Gastroenterol. Hepatol. 2005, 3, S67–S70. [Google Scholar] [PubMed]
- Wang, J.; Ge, J.; Zhang, X.-H.; Liu, J.-Y.; Yang, C.-M.; Zhao, S.-L. Endoscopic submucosal dissection versus endoscopic mucosal resection for the treatment of early esophageal carcinoma: A meta-analysis. Asian Pac. J. Cancer Prev. 2014, 15, 1803–1806. [Google Scholar] [CrossRef]
- Nishizawa, T.; Yahagi, N. Endoscopic mucosal resection and endoscopic submucosal dissection. Curr. Opin. Gastroenterol. 2017, 33, 315–319. [Google Scholar] [CrossRef]
- Oyama, T. Counter traction makes endoscopic submucosal dissection easier. Clin. Endosc. 2012, 45, 375–378. [Google Scholar] [CrossRef]
- Nishizawa, T.; Uraoka, T.; Ochiai, Y.; Suzuki, H.; Goto, O.; Fujimoto, A.; Maehata, T.; Kanai, T.; Yahagi, N. The “Two-Sword Fencing” Technique in Endoscopic Submucosal Dissection. Clin. Endosc. 2015, 48, 85–86. [Google Scholar] [CrossRef]
- Yahagi, N.; Nishizawa, T.; Sasaki, M.; Ochiai, Y.; Uraoka, T. Water pressure method for duodenal endoscopic submucosal dissection. Endoscopy 2017, 49, E227–E228. [Google Scholar] [CrossRef] [PubMed]
- Nishizawa, T.; Suzuki, H.; Matsuzaki, J.; Kanai, T.; Yahagi, N. Propofol versus traditional sedative agents for endoscopic submucosal dissection. Dig. Endosc. 2014, 26, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Yoshio, T.; Ishiyama, A.; Tsuchida, T.; Yoshimizu, S.; Horiuchi, Y.; Omae, M.; Hirasawa, T.; Yamamoto, Y.; Sano, H.; Yokota, M.; et al. Efficacy of novel sedation using the combination of dexmedetomidine and midazolam during endoscopic submucosal dissection for esophageal squamous cell carcinoma. Esophagus 2019, 16, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Nishizawa, T.; Suzuki, H.; Sagara, S.; Kanai, T.; Yahagi, N. Dexmedetomidine versus midazolam for gastrointestinal endoscopy: A meta-analysis. Dig. Endosc. 2015, 27, 8–15. [Google Scholar] [CrossRef]
- Sakaguchi, Y.; Tsuji, Y.; Ono, S.; Saito, I.; Kataoka, Y.; Takahashi, Y.; Nakayama, C.; Shichijo, S.; Matsuda, R.; Minatsuki, C.; et al. Polyglycolic acid sheets with fibrin glue can prevent esophageal stricture after endoscopic submucosal dissection. Endoscopy 2014, 47, 336–340. [Google Scholar] [CrossRef]
- Aadam, A.A.; Abe, S. Endoscopic submucosal dissection for superficial esophageal cancer. Dis. Esophagus 2018, 31. [Google Scholar] [CrossRef] [PubMed]
- Mitsunaga, Y.; Nishizawa, T.; Fujimoto, A.; Sasaki, A.; Yahagi, N. Successful endoscopic submucosal dissection for superficial esophageal cancer on solitary esophageal varix. Gastrointest. Endosc. 2017, 86, 913–914. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, S.; Nishizawa, T.; Ochiai, Y.; Fujimoto, A.; Takabayashi, K.; Kato, M.; Goto, O.; Maehata, T.; Yahagi, N.; Uraoka, T. Salvage endoscopic submucosal dissection for incompletely resected esophageal or gastric neoplasms (case series). Endosc. Int. Open 2020, 8, E20–E24. [Google Scholar] [CrossRef]
- Kinoshita, S.; Uraoka, T.; Nishizawa, T.; Naganuma, M.; Iwao, Y.; Ochiai, Y.; Fujimoto, A.; Goto, O.; Shimoda, M.; Ogata, H.; et al. The role of colorectal endoscopic submucosal dissection in patients with ulcerative colitis. Gastrointest. Endosc. 2018, 87, 1079–1084. [Google Scholar] [CrossRef]
- Ono, S.; Fujishiro, M.; Niimi, K.; Goto, O.; Kodashima, S.; Yamamichi, N.; Omata, M. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest. Endosc. 2009, 70, 860–866. [Google Scholar]
- Tanaka, M.; Ono, H.; Takizawa, K.; Kakushima, N.; Imai, K.; Hotta, K.; Matsubayashi, H. Clinical Course or Superficial Esophageal Cancer Treated by Endoscopic Submucosal Dissection. Stomach Intest. 2013, 48, 1253–1261. [Google Scholar]
- Nagami, Y.; Ominami, M.; Shiba, M.; Minamino, H.; Fukunaga, S.; Kameda, N.; Sugimori, S.; Machida, H.; Tanigawa, T.; Yamagami, H.; et al. The five-year survival rate after endoscopic submucosal dissection for superficial esophageal squamous cell neoplasia. Dig. Liver Dis. 2017, 49, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Hashimoto, S.; Mizuno, K.-I.; Kobayashi, T.; Tominaga, K.; Sato, H.; Kohisa, J.; Ikarashi, S.; Hayashi, K.; Takeuchi, M.; et al. Management decision based on lymphovascular involvement leads to favorable outcomes after endoscopic treatment of esophageal squamous cell carcinoma. Endoscopy 2017, 50, 662–670. [Google Scholar] [CrossRef] [PubMed]
- Bollschweiler, E.; Baldus, S.E.; Schröder, W.; Prenzel, K.; Gutschow, C.; Schneider, P.M.; Hölscher, A.H. High Rate of Lymph-Node Metastasis in Submucosal Esophageal Squamous-Cell Carcinomas and Adenocarcinomas. Endoscopy 2006, 38, 149–156. [Google Scholar] [CrossRef]
- Tajima, Y.; Nakanishi, Y.; Tachimori, Y.; Kato, H.; Watanabe, H.; Yamaguchi, H.; Yoshimura, K.; Kusano, M.; Shimoda, T. Significance of involvement by squamous cell carcinoma of the ducts of esophageal submucosal glands. Analysis of 201 surgically resected superficial squamous cell carcinomas. Cancer 2000, 89, 248–254. [Google Scholar] [CrossRef]
- Hagens, E.R.C.; Henegouwen, M.I.V.B.; Gisbertz, S.S. Distribution of Lymph Node Metastases in Esophageal Carcinoma Patients Undergoing Upfront Surgery: A Systematic Review. Cancers 2020, 12, 1592. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Uno, T.; Oyama, T.; Kato, K.; Kato, H.; Kawakubo, H.; Kawamura, O.; Kusano, M.; Kuwano, H.; Takeuchi, H.; et al. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: Part 1. Esophagus 2019, 16, 1–24. [Google Scholar] [CrossRef]
- Pimentel-Nunes, P.; Dinis-Ribeiro, M.; Ponchon, T.; Repici, A.; Vieth, M.; De Ceglie, A.; Amato, A.; Berr, F.; Bhandari, P.; Bialek, A.; et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015, 47, 829–854. [Google Scholar] [CrossRef]
- Joo, D.C.; Kim, G.H.; Park, D.Y.; Jhi, J.H.; Song, G.A. Long-term outcome after endoscopic submucosal dissection in patients with superficial esophageal squamous cell carcinoma: A single-center study. Gut Liver 2014, 8, 612–618. [Google Scholar] [CrossRef]
- Qi, Z.-P.; Chen, T.; Li, B.; Ren, Z.; Yao, L.-Q.; Shi, Q.; Cai, S.-L.; Zhong, Y.-S.; Zhou, P.-H. Endoscopic submucosal dissection for early esophageal cancer in elderly patients with relative indications for endoscopic treatment. Endoscopy 2018, 50, 839–845. [Google Scholar] [CrossRef]
- Iizuka, T.; Kikuchi, D.; Hoteya, S. Outcomes of endoscopic submucosal dissection for superficial esophageal cancer in an elderly population: A retrospective single center cohort study. Endosc. Int. Open 2019, 7, E355–E360. [Google Scholar] [CrossRef] [PubMed]
- Lindenmann, J.; Fediuk, M.; Fink-Neuboeck, N.; Porubsky, C.; Pichler, M.; Brcic, L.; Anegg, U.; Balic, M.; Dandachi, N.; Maier, A.; et al. Hazard Curves for Tumor Recurrence and Tumor-Related Death Following Esophagectomy for Esophageal Cancer. Cancers 2020, 12, 2066. [Google Scholar] [CrossRef] [PubMed]
- Min, Y.W.; Lee, H.; Song, B.G.; Min, B.; Kim, H.K.; Choi, Y.S.; Lee, J.H.; Hwang, N.-Y.; Carriere, K.C.; Rhee, P.-L.; et al. Comparison of endoscopic submucosal dissection and surgery for superficial esophageal squamous cell carcinoma: A propensity score-matched analysis. Gastrointest. Endosc. 2018, 88, 624–633. [Google Scholar] [CrossRef]
- Lee, H.D.; Chung, H.; Kwak, Y.; Choi, J.; Lee, A.; Kim, J.L.; Cho, S.-J.; Kim, S.G. Endoscopic Submucosal Dissection Versus Surgery for Superficial Esophageal Squamous Cell Carcinoma: A Propensity Score-Matched Survival Analysis. Clin. Transl. Gastroenterol. 2020, 11, e00193. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.; Rahmi, G.; Perrod, G.; Pioche, M.; Canard, J.-M.; Cesbron-Métivier, E.; Boursier, J.; Samaha, E.; Vienne, A.; Lépilliez, V.; et al. Long-term follow-up after endoscopic resection for superficial esophageal squamous cell carcinoma: A multicenter Western study. Endoscopy 2018, 51, 298–306. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Uno, T.; Oyama, T.; Kato, K.; Kato, H.; Kawakubo, H.; Kawamura, O.; Kusano, M.; Kuwano, H.; Takeuchi, H.; et al. Esophageal cancer practice guidelines 2017 edited by the Japan esophageal society: Part 2. Esophagus 2019, 16, 25–43. [Google Scholar] [CrossRef]
- Suzuki, G.; Yamazaki, H.; Aibe, N.; Masui, K.; Shimizu, D.; Kimoto, T.; Nishimura, T.; Nakashima, A.; Takenaka, T.; Dohi, O.; et al. Radiotherapy for T1N0M0 Esophageal Cancer: Analyses of the Predictive Factors and the Role of Endoscopic Submucosal Dissection in the Local Control. Cancers 2018, 10, 259. [Google Scholar] [CrossRef]
- Yoshimizu, S.; Yoshio, T.; Ishiyama, A.; Tsuchida, T.; Horiuchi, Y.; Omae, M.; Hirasawa, T.; Asari, T.; Chin, K.; Fujisaki, J. Long-term outcomes of combined endoscopic resection and chemoradiotherapy for esophageal squamous cell carcinoma with submucosal invasion. Author’s reply. Dig. Liver Dis. 2018, 50, 1255–1256. [Google Scholar] [CrossRef]
- Kinoshita, S.; Nishizawa, T.; Banno, S.; Uraoka, T. Chemotherapy followed by gastric endoscopic submucosal dissection. Jpn. J. Clin. Oncol. 2018, 48, 598–599. [Google Scholar] [CrossRef]
- Tsujii, Y.; Nishida, T.; Nishiyama, O.; Yamamoto, K.; Kawai, N.; Yamaguchi, S.; Yamada, T.; Yoshio, T.; Kitamura, S.; Nakamura, T.; et al. Clinical outcomes of endoscopic submucosal dissection for superficial esophageal neoplasms: A multicenter retrospective cohort study. Endoscopy 2015, 47, 775–783. [Google Scholar] [CrossRef]
- Kuwai, T.; Yamaguchi, T.; Imagawa, H.; Miura, R.; Sumida, Y.; Takasago, T.; Miyasako, Y.; Nishimura, T.; Iio, S.; Yamaguchi, A.; et al. Endoscopic submucosal dissection for early esophageal neoplasms using the stag beetle knife. World J. Gastroenterol. 2018, 24, 1632–1640. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, A.; Katada, C.; Yokoyama, T.; Yano, T.; Kaneko, K.; Oda, I.; Shimizu, Y.; Doyama, H.; Koike, T.; Takizawa, K.; et al. Alcohol abstinence and risk assessment for second esophageal cancer in Japanese men after mucosectomy for early esophageal cancer. PLoS ONE 2017, 12, e0175182. [Google Scholar] [CrossRef] [PubMed]
- Businello, G.; Parente, P.; Mastracci, L.; Pennelli, G.; Traverso, G.; Milione, M.; Bellan, E.; Michelotto, M.; Kotsafti, A.; Grillo, F.; et al. The Pathologic and Molecular Landscape of Esophageal Squamous Cell Carcinogenesis. Cancers 2020, 12, 2160. [Google Scholar] [CrossRef] [PubMed]
- Ono, S.; Fujishiro, M.; Niimi, K.; Goto, O.; Kodashima, S.; Yamamichi, N.; Omata, M. Predictors of postoperative stricture after esophageal endoscopic submucosal dissection for superficial squamous cell neoplasms. Endoscopy 2009, 41, 661–665. [Google Scholar] [CrossRef]
- Hashimoto, S.; Mizuno, K.-I.; Takahashi, K.; Sato, H.; Yokoyama, J.; Takeuchi, M.; Sato, Y.; Kobayashi, M.; Terai, S. Evaluating the effect of injecting triamcinolone acetonide in two sessions for preventing esophageal stricture after endoscopic submucosal dissection. Endosc. Int. Open 2019, 7, E764–E770. [Google Scholar] [CrossRef]
| Author | Depth | Number of | Additional Therapy | 5-Year Overall | 5-Year Cause |
|---|---|---|---|---|---|
| Year | Patients | Number (%) | Survival | Specific Survival | |
| Ono | HGN/M1/M2 | 56 | - | 95% | 100% |
| 2009 | M3/SM1/SM2 | 28 | CRT/RT 6 (21%), Ope 9 (32%) | 56% * | 85% * |
| Tanaka | M1/M2 | 122 | - | 85% | 98% |
| 2013 | M3/SM1 | 56 | CRT/RT 12 (21%), Ope 1 (2%) | 82% | 93% |
| SM2 | 26 | CRT/RT 14 (54%), Ope 3 (12%) | 83% | 100% | |
| Nagami | HGN/M1/M2 | 60 | - | 95% | 100% |
| 2017 | M3/SM1 | 19 | CRT/CY 13 (68%), Ope 2 (11%) | 84% | 100% |
| SM2 | 4 | CRT/CY 3 (75%), Ope 1 (25%) | 75% * | 100% | |
| Takahashi | M3/SM1 | 102 | CRT 9 (9%), Ope 3 (3%) | 84% | 98% |
| 2018 |
| Author | Number of | Age (Years) | Depth | Number of | Vascular | Death Due to | 5-Year Overall |
|---|---|---|---|---|---|---|---|
| Year | Patients | Mean (Range) | Patients (%) | Involvement (%) | Esophageal Cancer | Survival | |
| Joo | 28 | 64 (46–76) | M1/M2 | 23 (82%) | 0 | 0 | 84% |
| 2014 | M3–SM2 | 5 (18%) | |||||
| Qi | 158 | 66 (60–84) | M1/M2 | 89 (56%) | 3 (3.4%) | 0 | 96.6% |
| 2018 | M3–SM1 | 69 (44%) | 6 (8.7%) | 1 (1.4%) | 95.6% |
| Author | Generation | Number of | m3–sm | Additional Therapy | 5-Year Overall | 5-Year Cause |
|---|---|---|---|---|---|---|
| Year | Patients | (%) | Number (%) | Survival | Specific Survival | |
| Iizuka | Elderly | 162 | 21% | CRT 13 (8%), Ope 1 (0.6%) *** | 83.6% * | 97.3% |
| 2019 | Young | 502 | 22.1% | CRT 72 (14.3%), Ope 32 (6.4%) | 91.2% | 97.5% |
| Author | Therapy | Number of | m3–sm | 5-Year Overall | 5-Year Disease-Free Survival | Adverse Events |
|---|---|---|---|---|---|---|
| Year | Patients | Number (%) | Survival | |||
| Min | ESD | 120 | 56 (46.7%) | 93.9% | 92.8% | 8.9% *** |
| 2018 | Surgery | 120 | 57 (47.5%) | 91.2% | 95.3% | 48.2% |
| Lee | ESD | 34 | 15 (44.1%) | 89.4% | 90.9% | 2.9% *** |
| 2020 | Surgery | 34 | 14 (41.2%) | 87.8% | 91.6% | 23.5% |
| Berger | ESD | 68 | 26 (32.8%) | - | 95.2% ** | 2.9% † |
| 2019 | EMR | 80 | 27 (33.8%) | - | 73.4% | 1.3% † |
| Author | Treatment | Number of | 5-Year Overall | 5-Year Disease | Local | Metastatic |
|---|---|---|---|---|---|---|
| Year | (Additional Rate) | Patients | Survival | Free Survival | Recurrence | Recurrence |
| Yoshimizu | CRT | 43 | 79.1% | 59.2% * | 19% * | 7% |
| 2018 | ESD/EMR + CRT | 21 | 85.1% | 85.1% | 0% | 10% |
| Author | Year | Number of | 3-Year Metachronous | 5-Year Metachronous | Overall |
|---|---|---|---|---|---|
| Patients | Cancer Rate | Cancer Rate | Survival | ||
| Tsuji | 2015 | 214 | 9.9% | 24.5% | - |
| Kuwai | 2018 | 57 | 14% | 26% | 75.0% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishizawa, T.; Suzuki, H. Long-Term Outcomes of Endoscopic Submucosal Dissection for Superficial Esophageal Squamous Cell Carcinoma. Cancers 2020, 12, 2849. https://doi.org/10.3390/cancers12102849
Nishizawa T, Suzuki H. Long-Term Outcomes of Endoscopic Submucosal Dissection for Superficial Esophageal Squamous Cell Carcinoma. Cancers. 2020; 12(10):2849. https://doi.org/10.3390/cancers12102849
Chicago/Turabian StyleNishizawa, Toshihiro, and Hidekazu Suzuki. 2020. "Long-Term Outcomes of Endoscopic Submucosal Dissection for Superficial Esophageal Squamous Cell Carcinoma" Cancers 12, no. 10: 2849. https://doi.org/10.3390/cancers12102849
APA StyleNishizawa, T., & Suzuki, H. (2020). Long-Term Outcomes of Endoscopic Submucosal Dissection for Superficial Esophageal Squamous Cell Carcinoma. Cancers, 12(10), 2849. https://doi.org/10.3390/cancers12102849






