Acute Hypoxia Profile is a Stronger Prognostic Factor than Chronic Hypoxia in Advanced Stage Head and Neck Cancer Patients
Abstract
1. Introduction
2. Results
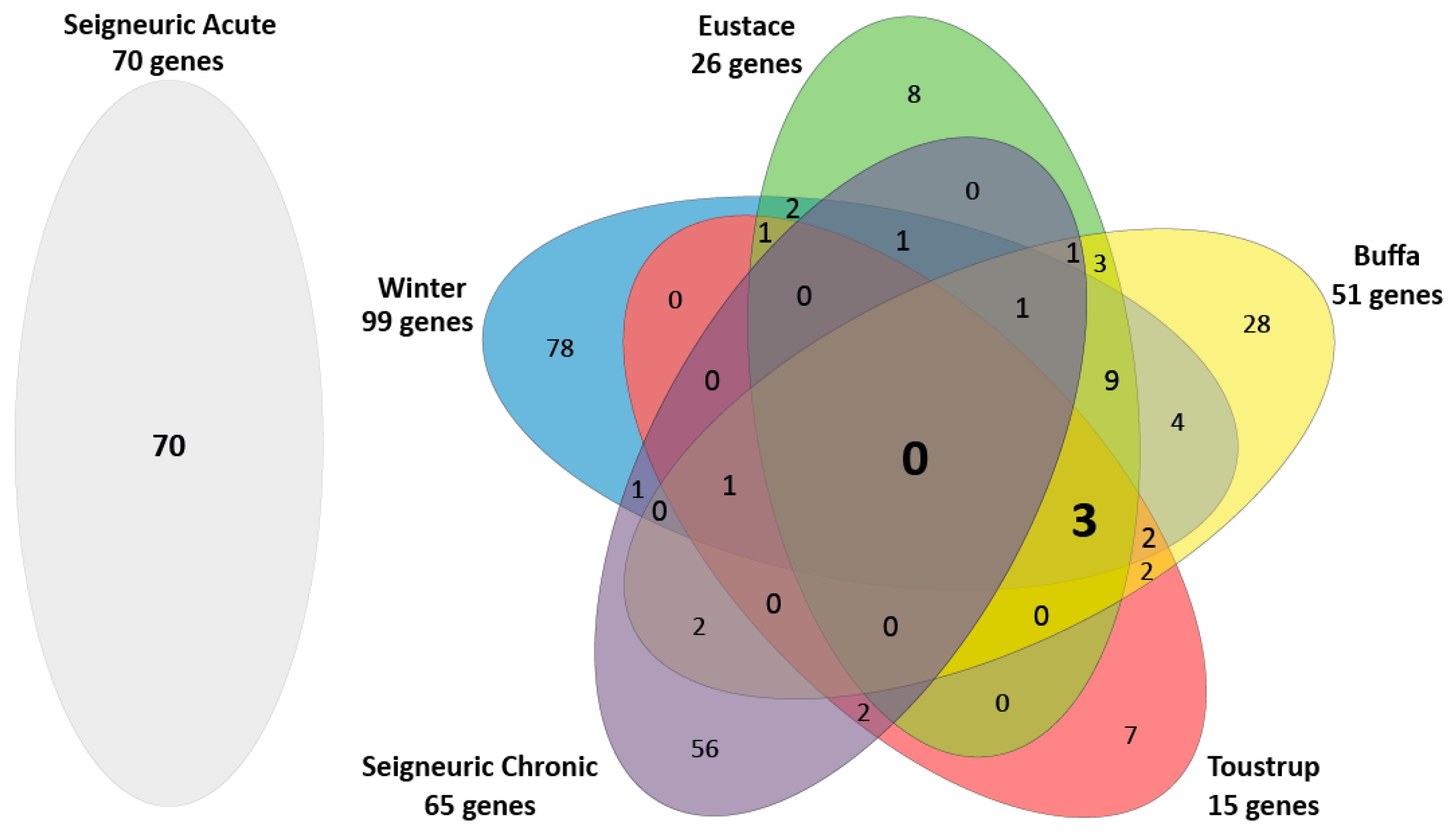
2.1. Few Overlapping Genes in the Four Clinical HNSCC Hypoxia Gene Expression Profiles
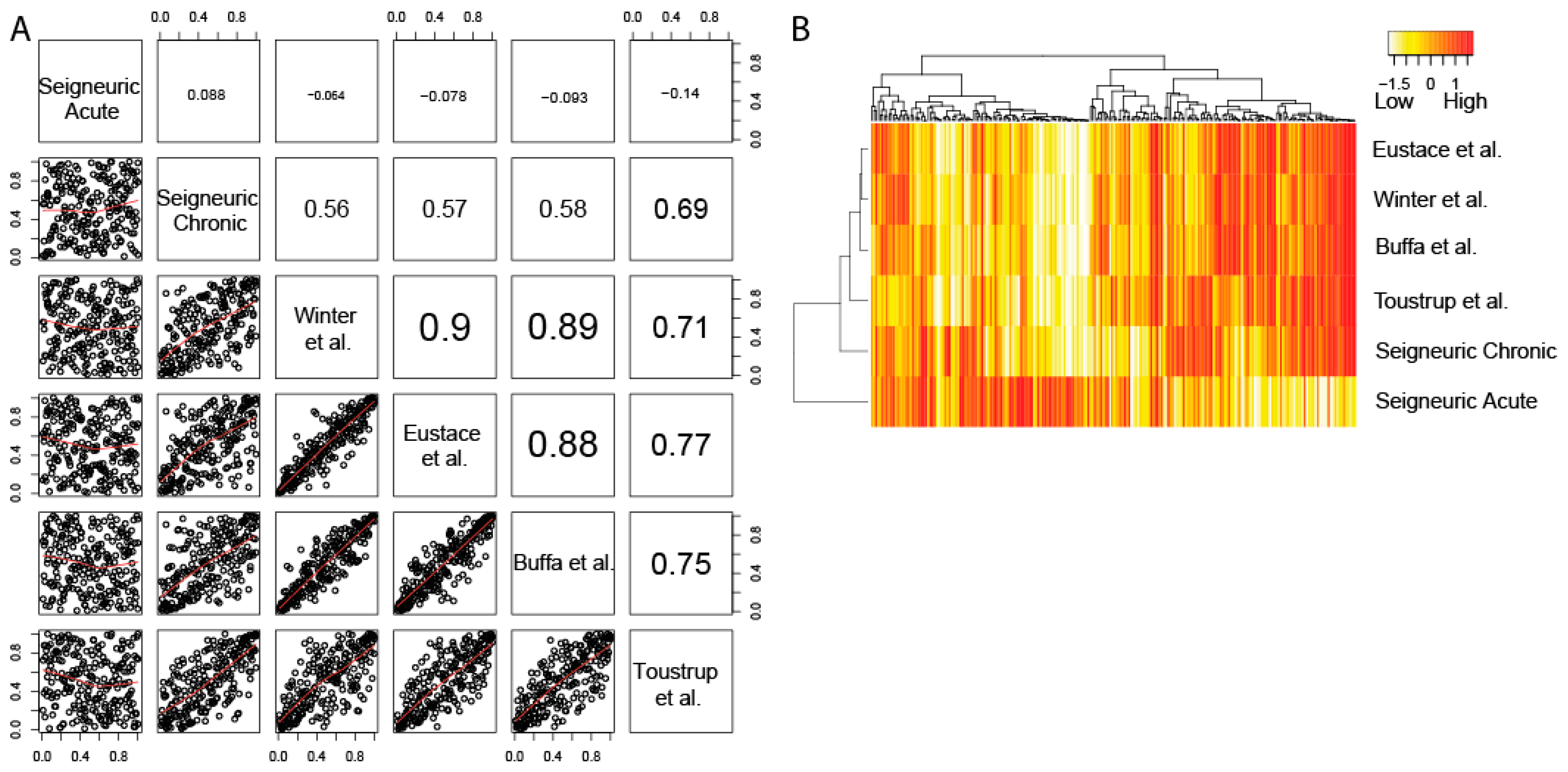
2.2. The Four Clinical HNSCC Hypoxia Gene Expression Profiles are Correlated and Resemble Chronic Hypoxia Response
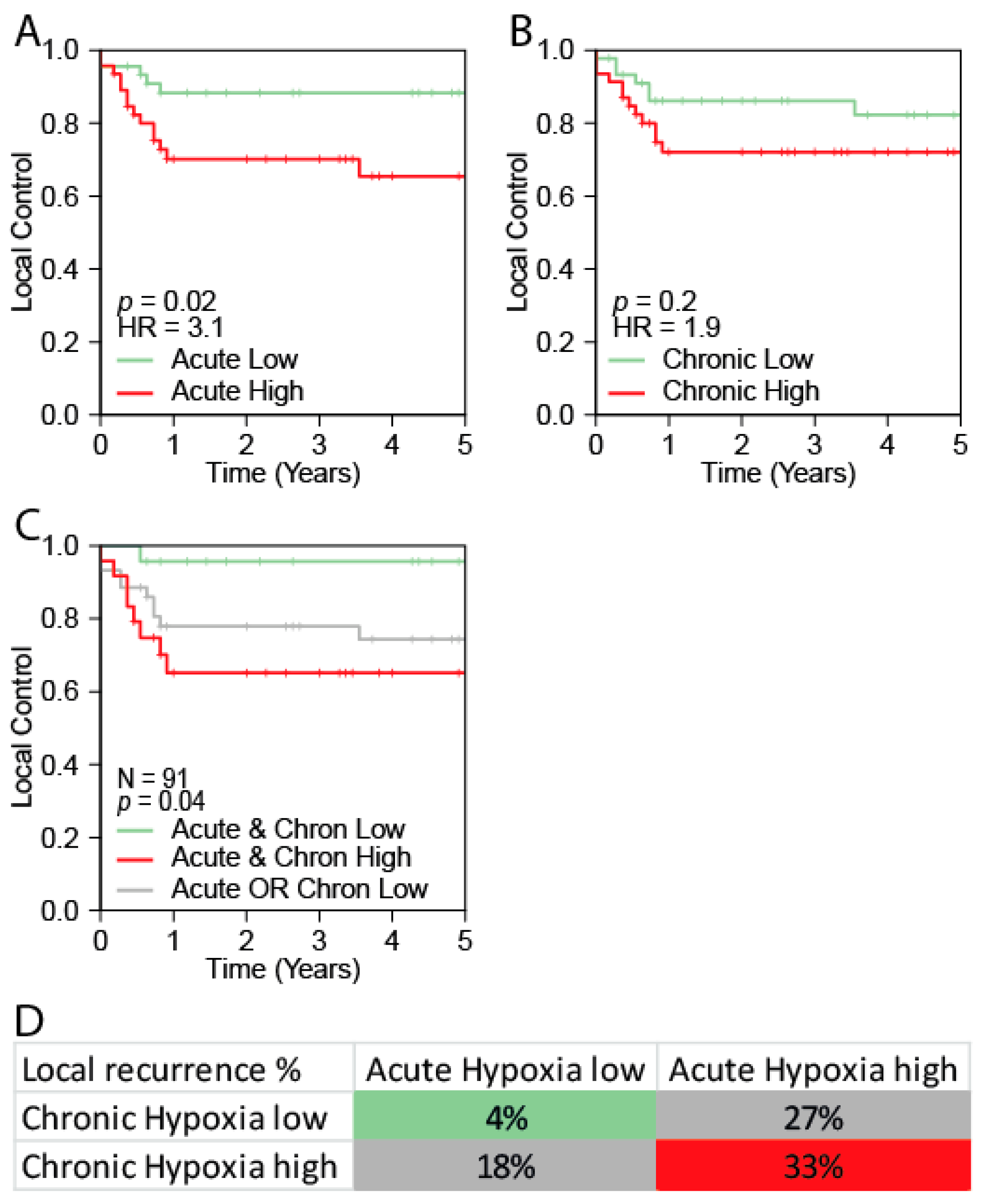
2.3. The Acute Hypoxia Profile is Associated with Local Control
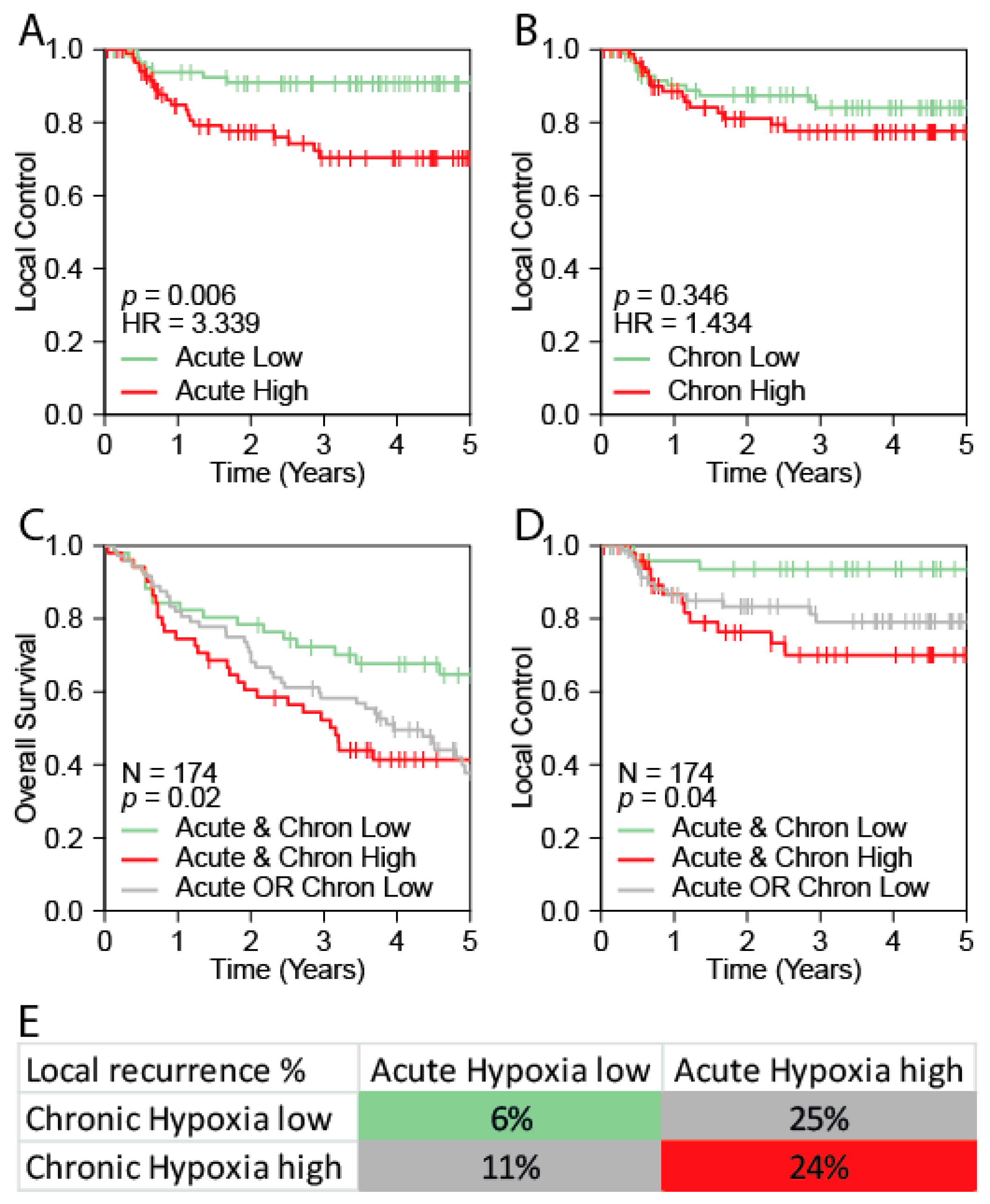
2.4. Validation of the Acute Hypoxia Profile as a Prognostic Marker for Outcome in HNSCC
2.5. Multivariable Analysis Confirms the Prognostic Value of Acute Hypoxia
3. Discussion
3.1. Acute and Chronic Hypoxia
3.2. Acute Hypoxia and Prognosis
4. Materials and Methods
4.1. Gene Expression Profiles
4.2. Datasets
4.3. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Shin, H.R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 2010. [Google Scholar] [CrossRef]
- Groome, P.A.; Schulze, K.; Boysen, M.; Hall, S.F.; Mackillop, W.J.; O’Sullivan, B.; Irish, J.C.; Warde, P.R.; Schneider, K.M.; Mackenzie, R.G.; et al. A comparison of published head and neck stage groupings in laryngeal cancer using data from two countries. J. Clin. Epidemiol. 2002. [Google Scholar] [CrossRef]
- Groome, P.A.; Schulze, K.M.; Mackillop, W.J.; Grice, B.; Goh, C.; Cummings, B.J.; Hall, S.F.; Liu, F.F.; Payne, D.; Rothwell, D.M.; et al. A comparison of published head and neck stage groupings in carcinomas of the tonsillar region. Cancer 2001, 92, 1484–1494. [Google Scholar] [CrossRef]
- Hall, S.F.; Groome, P.A.; Irish, J.; O’Sullivan, B. TNM-based stage groupings in head and neck cancer: Application in cancer of the hypopharynx. Head Neck 2009, 31, 1–8. [Google Scholar] [CrossRef]
- de Jong, M.C.; Pramana, J.; Knegjens, J.L.; Balm, A.J.M.; van den Brekel, M.W.M.; Hauptmann, M.; Begg, A.C.; Rasch, C.R. HPV and high-risk gene expression profiles predict response to chemoradiotherapy in head and neck cancer, independent of clinical factors. Radiother. Oncol. 2010, 95, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Janssen, H.L.; Haustermans, K.M.; Balm, A.J.; Begg, A.C. Hypoxia in head and neck cancer: How much, how important? Head Neck 2005, 27, 622–638. [Google Scholar] [CrossRef] [PubMed]
- Bristow, R.G.; Hill, R.P. Hypoxia and metabolism: Hypoxia, DNA repair and genetic instability. Nat. Rev. Cancer 2008, 8, 180–892. [Google Scholar] [CrossRef] [PubMed]
- Ma, N.Y.; Tinganelli, W.; Maier, A.; Durante, M.; Kraft-Weyrather, W. Influence of chronic hypoxia and radiation quality on cell survival. J. Radiat. Res. 2013, 54 (Suppl. 1), i13–i22. [Google Scholar] [CrossRef]
- Gray, L.H.; Conger, A.D.; Ebert, M.; Hornsey, S.; Scott, O.C. The concentration of oxygen dissolved in tissues at the time of irradiation as a factor in radiotherapy. Br. J. Radiol. 1953, 26, 638–648. [Google Scholar] [CrossRef] [PubMed]
- De Gonzalez, A.B.; Curtis, R.E.; Kry, S.F.; Gilbert, E.; Lamart, S.; Berg, C.D.; Stovall, M.; Ron, E. Proportion of second cancers attributable to radiotherapy treatment in adults: A cohort study in the US SEER cancer registries. Lancet Oncol. 2011, 12, 353–360. [Google Scholar] [CrossRef]
- Overgaard, J. Hypoxic modification of radiotherapy in squamous cell carcinoma of the head and neck—A systematic review and meta-analysis. Radiother. Oncol. 2011, 100, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Winter, S.C.; Shah, K.A.; Han, C.; Campo, L.; Turley, H.; Leek, R.; Corbridge, R.J.; Cox, G.J.; Harris, A.L. The Relation Between Hypoxia-Inducible Factor (HIF) -1 a and HIF-2 a Expression With Anemia and Outcome in Surgically Treated Head and Neck Cancer. Cancer. 2006. [Google Scholar] [CrossRef]
- Toustrup, K.; Sørensen, B.S.; Nordsmark, M.; Busk, M.; Wiuf, C.; Alsner, J.; Overgaard, J. Development of a hypoxia gene expression classifier with predictive impact for hypoxic modification of radiotherapy in head and neck cancer. Cancer Res. 2011, 71, 5923–5931. [Google Scholar] [CrossRef]
- Rademakers, S.E.; Hoogsteen, I.J.; Rijken, P.F.; Oosterwijk, E.; Terhaard, C.H.; Doornaert, P.A.; Langendijk, J.A.; van den Ende, P.; Takes, R.; De Bree, R.; et al. Pattern of CAIX expression is prognostic for outcome and predicts response to ARCON in patients with laryngeal cancer treated in a phase III randomized trial. Radiother. Oncol. 2013, 108, 517–522. [Google Scholar] [CrossRef]
- Thomson, D.; Yang, H.; Baines, H.; Miles, E.; Bolton, S.; West, C.; Slevin, N. NIMRAD—A phase III trial to investigate the use of nimorazole hypoxia modification with intensity-modulated radiotherapy in head and neck cancer. Clin. Oncol. 2014, 26, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Nordsmark, M.; Bentzen, S.M.; Rudat, V.; Brizel, D.; Lartigau, E.; Stadler, P.; Becker, A.; Adam, M.; Molls, M.; Dunst, J.; et al. Prognostic value of tumor oxygenation in 397 head and neck tumors after primary radiation therapy. An international multi-center study. Radiother. Oncol. 2005, 77, 18–24. [Google Scholar] [CrossRef]
- Brizel, D.M.; Sibley, G.S.; Prosnitz, L.R.; Scher, R.L.; Dewhirst, M.W. Tumor hypoxia adversely affects the prognosis of carcinoma of the head and neck. Int. J. Radiat. Oncol. Biol. Phys. 1997, 38, 285–289. [Google Scholar] [CrossRef]
- Nordsmark, M.; Overgaard, J. A confirmatory prognostic study on oxygenation status and loco-regional control in advanced head and neck squamous cell carcinoma treated by radiation therapy. Radiother. Oncol. 2000, 57, 39–43. [Google Scholar] [CrossRef]
- Nordsmark, M.; Overgaard, M.; Overgaard, J. Pretreatment oxygenation predicts radiation response in advanced squamous cell carcinoma of the head and neck. Radiother. Oncol. 1996, 41, 31–39. [Google Scholar] [CrossRef]
- Kaanders, J.H.; Wijffels, K.I.; Marres, H.A.; Ljungkvist, A.S.; Pop, L.A.; van den Hoogen, F.J.; de Wilde, P.C.; Bussink, J.; Raleigh, J.A.; van der Kogel, A.J. Pimonidazole binding and tumor vascularity predict for treatment outcome in head and neck cancer. Cancer Res. 2002, 62, 7066–7074. [Google Scholar] [PubMed]
- Schrijvers, M.L.; van der Laan, B.F.A.M.; de Bock, G.H.; Pattje, W.J.; Mastik, M.F.; Menkema, L.; Langendijk, J.A.; Kluin, P.M.; Schuuring, E.; van der Wal, J.E. Overexpression of Intrinsic Hypoxia Markers HIF1α and CA-IX Predict for Local Recurrence in Stage T1–T2 Glottic Laryngeal Carcinoma Treated With Radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 161–169. [Google Scholar] [CrossRef]
- Koukourakis, M.I.; Giatromanolaki, A.; Sivridis, E.; Simopoulos, C.; Turley, H.; Talks, K.; Gatter, K.C.; Harris, A.L. Hypoxia-inducible factor (HIF1A and HIF2A), angiogenesis, and chemoradiotherapy outcome of squamous cell head-and-neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 2002, 53, 1192–1202. [Google Scholar] [CrossRef]
- Panek, R.; Welsh, L.; Dunlop, A.; Wong, K.H.; Riddell, A.M.; Koh, D.-M.; Schmidt, M.A.; Doran, S.; Mcquaid, D.; Hopkinson, G.; et al. Repeatability and sensitivity of T2* measurements in patients with head and neck squamous cell carcinoma at 3T. J. Magn. Reson. Imaging 2016, 44, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Fleming, I.N.; Manavaki, R.; Blower, P.J.; West, C.; Williams, K.J.; Harris, A.L.; Domarkas, J.; Lord, S.; Baldry, C.; Gilbert, F.J. Imaging tumour hypoxia with positron emission tomography. Br. J. Cancer 2015, 112, 238–250. [Google Scholar] [CrossRef] [PubMed]
- Winter, S.C.; Buffa, F.M.; Silva, P.; Miller, C.; Valentine, H.R.; Turley, H.; Shah, K.A.; Cox, G.J.; Corbridge, R.J.; Homer, J.J.; et al. Relation of a hypoxia metagene derived from head and neck cancer to prognosis of multiple cancers. Cancer Res. 2007, 67, 3441–3449. [Google Scholar] [CrossRef] [PubMed]
- Buffa, F.M.; Harris, A.L.; West, C.M.; Miller, C.J. Large meta-analysis of multiple cancers reveals a common, compact and highly prognostic hypoxia metagene. Br. J. Cancer 2010, 102, 428–435. [Google Scholar] [CrossRef]
- Eustace, A.; Mani, N.; Span, P.N.; Irlam, J.J.; Taylor, J.; Betts, G.N.; Denley, H.; Miller, C.J.; Homer, J.J.; Rojas, A.M.; et al. A 26-gene hypoxia signature predicts benefit from hypoxia-modifying therapy in laryngeal cancer but not bladder cancer. Clin. Cancer Res. 2013, 19, 4879–4888. [Google Scholar] [CrossRef] [PubMed]
- Koukourakis, M.I.; Bentzen, S.M.; Giatromanolaki, A.; Wilson, G.D.; Daley, F.M.; Saunders, M.I.; Dische, S.; Sivridis, E.; Harris, A.L. Endogenous markers of two separate hypoxia response pathways (hypoxia inducible factor 2 alpha and carbonic anhydrase 9) are associated with radiotherapy failure in head and neck cancer patients recruited in the CHART randomized trial. J. Clin. Oncol. 2006, 24, 727–735. [Google Scholar] [CrossRef]
- Rademakers, S.E.; Lok, J.; van der Kogel, A.J.; Bussink, J.; Kaanders, J.H.A.M. Metabolic markers in relation to hypoxia; staining patterns and colocalization of pimonidazole, HIF-1α, CAIX, LDH-5, GLUT-1, MCT1 and MCT4. BMC Cancer 2011, 11, 167. [Google Scholar] [CrossRef]
- Tawk, B.; Schwager, C.; Deffaa, O.; Dyckhoff, G.; Warta, R.; Linge, A.; Krause, M.; Weichert, W.; Baumann, M.; Herold-Mende, C.; et al. Comparative analysis of transcriptomics based hypoxia signatures in head- and neck squamous cell carcinoma. Radiother. Oncol. 2016, 118, 350–358. [Google Scholar] [CrossRef]
- Seigneuric, R.; Starmans, M.H.W.; Fung, G.; Krishnapuram, B.; Nuyten, D.S.A.; van Erk, A.; Magagnin, M.G.; Rouschop, K.M.; Krishnan, S.; Rao, R.B.; et al. Impact of supervised gene signatures of early hypoxia on patient survival. Radiother. Oncol. 2007, 83, 374–382. [Google Scholar] [CrossRef]
- Pramana, J.; Van den Brekel, M.W.M.; van Velthuysen, M.-L.F.; Wessels, L.F.A.; Nuyten, D.S.; Hofland, I.; Atsma, D.; Pimentel, N.; Hoebers, F.J.; Rasch, C.R.; et al. Gene expression profiling to predict outcome after chemoradiation in head and neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 2007, 69, 1544–1552. [Google Scholar] [CrossRef] [PubMed]
- De Jong, M.C.; Pramana, J.; Van Der Wal, J.E.; Lacko, M.; Peutz-Kootstra, C.J.; De Jong, J.M.; Takes, R.P.; Kaanders, J.H.; van der Laan, B.F.; Wachters, J.; et al. CD44 expression predicts local recurrence after radiotherapy in larynx cancer. Clin. Cancer Res. 2010, 16, 5329–5338. [Google Scholar] [CrossRef]
- De Jong, M.C.; Ten Hoeve, J.J.; Grénman, R.; Wessels, L.F.; Kerkhoven, R.; Te Riele, H.; van den Brekel, M.W.; Verheij, M.; Begg, A.C. Pretreatment microRNA expression impacting on epithelial-to-mesenchymal transition predicts intrinsic radiosensitivity in head and neck cancer cell lines and patients. Clin. Cancer Res. 2015, 21, 5630–5638. [Google Scholar] [CrossRef] [PubMed]
- Van der Heijden, M.; Essers, P.; Verheij, M.; Van den Brekel, M.; Vens, C. OC-0487: EMT signatures as a prognostic marker for metastasis in HPV-negative HNSCC. Radiother. Oncol. 2018, 127, S250–S251. [Google Scholar] [CrossRef]
- Van der Heijden, M.; Essers, P.; Verhagen, C.; Willems, S.; Sanders, J.; de Roest, R.; Vossen, D.M.; Leemans, C.R.; Verheij, M.; Brakenhoff, R.H.; et al. Epithelial-to-mesenchymal transistion is a prognostic marker for patient outcome in advanced stage HNSCC patients treated with chemoradiotherapy. Manuscript under review.
- Linge, A.; Lock, S.; Gudziol, V.; Nowak, A.; Lohaus, F.; Von Neubeck, C.; Jütz, M.; Abdollahi, A.; Debus, J.; Tinhofer, I.; et al. Low cancer stem cell marker expression and low hypoxia identify good prognosis subgroups in HPV(-) HNSCC after postoperative radiochemotherapy: A multicenter study of the DKTK-ROG. Clin. Cancer Res. 2016, 22, 2639–2649. [Google Scholar] [CrossRef] [PubMed]
- Roepman, P.; Kemmeren, P.; Wessels, L.F.A.; Slootweg, P.J.; Holstege, F.C.P. Multiple robust signatures for detecting lymph node metastasis in head and neck cancer. Cancer Res. 2006, 66, 2361–2366. [Google Scholar] [CrossRef] [PubMed]
- Lendahl, U.; Lee, K.L.; Yang, H.; Poellinger, L. Generating specificity and diversity in the transcriptional response to hypoxia. Nat. Rev. Genet. 2009, 10, 821–832. [Google Scholar] [CrossRef] [PubMed]
- Bayer, C.; Shi, K.; Astner, S.T.; Maftei, C.A.; Vaupel, P. Acute versus chronic hypoxia: Why a simplified classification is simply not enough. Int. J. Radiat. Oncol. Biol. Phys. 2011, 80, 965–968. [Google Scholar] [CrossRef]
- Bayer, C.; Vaupel, P. Acute versus chronic hypoxia in tumors: Controversial data concerning time frames and biological consequences. Strahlenther. Onkol. 2012, 188, 616–627. [Google Scholar] [CrossRef]
- Janssen, H.L.K.; Haustermans, K.M.G.; Sprong, D.; Blommestijn, G.; Hofland, I.; Hoebers, F.J.; Blijweert, E.; Raleigh, J.A.; Semenza, G.L.; Varia, M.A.; et al. HIF-1α, pimonidazole, and iododeoxyuridine to estimate hypoxia and perfusion in human head-and-neck tumors. Int. J. Radiat. Oncol. Biol. Phys. 2002, 54, 1537–1549. [Google Scholar] [CrossRef]
- Maftei, C.A.; Bayer, C.; Shi, K.; Vaupel, P. Intra-and intertumor heterogeneities in total, chronic, and acute hypoxia in xenografted squamous cell carcinomas: Detection and quantification using (immuno-)fluorescence techniques. Strahlenther. Onkol. 2012, 188, 606–615. [Google Scholar] [CrossRef]
- Wijffels, K.I.; Kaanders, J.H.; Rijken, P.F.; Bussink, J.; van den Hoogen, F.J.; Marres, H.A.; de Wilde, P.C.; Raleigh, J.A.; van der Kogel, A.J. Vascular architecture and hypoxic profiles in human head and neck squamous cell carcinomas. Br. J. Cancer 2000, 83, 674–683. [Google Scholar] [CrossRef]
- Brown, J.M. Evidence for acutely hypoxic cells in mouse tumours, and a possible mechanism of reoxygenation. Br. J. Radiol. 1979. [Google Scholar] [CrossRef] [PubMed]
- Chan, N.; Koritzinsky, M.; Zhao, H.; Bindra, R.; Glazer, P.M.; Powell, S.; Belmaaza, A.; Wouters, B.; Bristow, R.G. Chronic hypoxia decreases synthesis of homologous recombination proteins to offset chemoresistance and radioresistance. Cancer Res. 2008, 68, 605–614. [Google Scholar] [CrossRef]
- Pires, I.M.; Bencokova, Z.; Milani, M.; Folkes, L.K.; Li, J.A.; Stratford, M.R.; Harris, A.L.; Hammond, E.M. Effects of acute versus chronic hypoxia on DNA damage responses and genomic instability. Cancer Res. 2010, 70, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Hänzelmann, S.; Castelo, R.; Guinney, J. GSVA: Gene set variation analysis for microarray and RNA-Seq data. BMC Bioinform. 2013, 14. [Google Scholar] [CrossRef]
| Use | Study | Cohorts | N | Sites | Treatment | Material | Assay |
|---|---|---|---|---|---|---|---|
| Combined for classification analyses | Pramana [32] | Stage III-IV HNSCCs | 91 | All head and neck | Chemo- radiotherapy | FF | Dual channel Operon microarray |
| test cohort | |||||||
| De Jong 1 [33] | Larynx / oropharynx | 99 | Larynx/oropharynx | Radiotherapy | FF | Illumina beads microarray | |
| De Jong 2 [34] | T2-3 larynx | 34 | Larynx | Radiotherapy | FFPE | RNAseq | |
| Combined for validation cohort | Van der Heijden - NKI-CRAD [35,36] | Stage III-IV HNSCCs | 98 | Larynx, hypopharynx, HPV-neg oropharynx | Chemo- radiotherapy | FF | RNAseq |
| Van der Heijden – DESIGN [35,36] | Stage III-IV HNSCCs | 76 | Larynx, hypopharynx, HPV-neg oropharynx | Chemo- radiotherapy | FF | RNAseq |
| Variable | OS | PFS | LC | LRC | DM | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR | p-Value | HR | p-Value | HR | p-Value | HR | p-Value | HR | p-Value | |
| Gender | ||||||||||
| Female | 0.83 | 0.04 | 0.56 | 0.04 | 0.16 | 0.013 | 0.19 | 0.004 | 0.28 | 0.04 |
| Male | REF | REF | REF | REF | REF | |||||
| Tumor site | ||||||||||
| Oropharynx | REF | REF | REF | REF | REF | |||||
| Hypopharynx | 0.64 | 0.09 | 0.69 | 0.15 | 0.96 | 0.12 | 0.97 | 0.94 | 0.52 | 0.16 |
| Larynx | 0.58 | 0.9 | 0.79 | 0.45 | 1.27 | 0.56 | 1.08 | 0.86 | 1.08 | 0.87 |
| Disease stage | ||||||||||
| II-III | 0.83 | 0.57 | 0.78 | 0.45 | 3.74 | 0.037 | 1.68 | 0.3 | 0.38 | 0.2 |
| IVA-IVB | REF | REF | REF | REF | REF | |||||
| Cumulative cisplatin < 200 | ||||||||||
| No | REF | REF | REF | REF | REF | |||||
| Yes | 2.03 | 0.003 | 1.93 | 0.004 | 6.4 | 0.0003 | 2.7 | 0.012 | 0.81 | 0.64 |
| Tumor Volume | 1.01 | 0.000044 | 1.008 | 0.0006 | 1.014 | 0.034 | 1.007 | 0.16 | 1.006 | 0.19 |
| Acute Hypoxia | 4.14 | 0.021 | 4.02 | 0.017 | 46.4 | 0.014 | 30 | 0.0022 | 5.5 | 0.13 |
| Chronic Hypoxia | 0.83 | 0.65 | 1 | 0.99 | 0.51 | 0.48 | 1.23 | 0.75 | 1.26 | 0.73 |
| Acute Hypoxia * Tumor Volume | 0.98 | 0.007 | 0.98 | 0.03 | 0.96 | 0.12 | 0.96 | 0.017 | 0.98 | 0.26 |
| Chronic Hypoxia * Tumor Volume | 1 | 0.99 | 0.99 | 0.7 | 1 | 0.98 | 0.99 | 0.52 | 0.99 | 0.57 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Heijden, M.; de Jong, M.C.; Verhagen, C.V.M.; de Roest, R.H.; Sanduleanu, S.; Hoebers, F.; Leemans, C.R.; Brakenhoff, R.H.; Vens, C.; Verheij, M.; et al. Acute Hypoxia Profile is a Stronger Prognostic Factor than Chronic Hypoxia in Advanced Stage Head and Neck Cancer Patients. Cancers 2019, 11, 583. https://doi.org/10.3390/cancers11040583
van der Heijden M, de Jong MC, Verhagen CVM, de Roest RH, Sanduleanu S, Hoebers F, Leemans CR, Brakenhoff RH, Vens C, Verheij M, et al. Acute Hypoxia Profile is a Stronger Prognostic Factor than Chronic Hypoxia in Advanced Stage Head and Neck Cancer Patients. Cancers. 2019; 11(4):583. https://doi.org/10.3390/cancers11040583
Chicago/Turabian Stylevan der Heijden, Martijn, Monique C. de Jong, Caroline V. M. Verhagen, Reinout H. de Roest, Sebastian Sanduleanu, Frank Hoebers, C. René Leemans, Ruud H. Brakenhoff, Conchita Vens, Marcel Verheij, and et al. 2019. "Acute Hypoxia Profile is a Stronger Prognostic Factor than Chronic Hypoxia in Advanced Stage Head and Neck Cancer Patients" Cancers 11, no. 4: 583. https://doi.org/10.3390/cancers11040583
APA Stylevan der Heijden, M., de Jong, M. C., Verhagen, C. V. M., de Roest, R. H., Sanduleanu, S., Hoebers, F., Leemans, C. R., Brakenhoff, R. H., Vens, C., Verheij, M., & van den Brekel, M. W. M. (2019). Acute Hypoxia Profile is a Stronger Prognostic Factor than Chronic Hypoxia in Advanced Stage Head and Neck Cancer Patients. Cancers, 11(4), 583. https://doi.org/10.3390/cancers11040583






