Screening a Broad Range of Solid and Haematological Tumour Types for CD70 Expression Using a Uniform IHC Methodology as Potential Patient Stratification Method
Abstract
:1. Introduction
2. Results
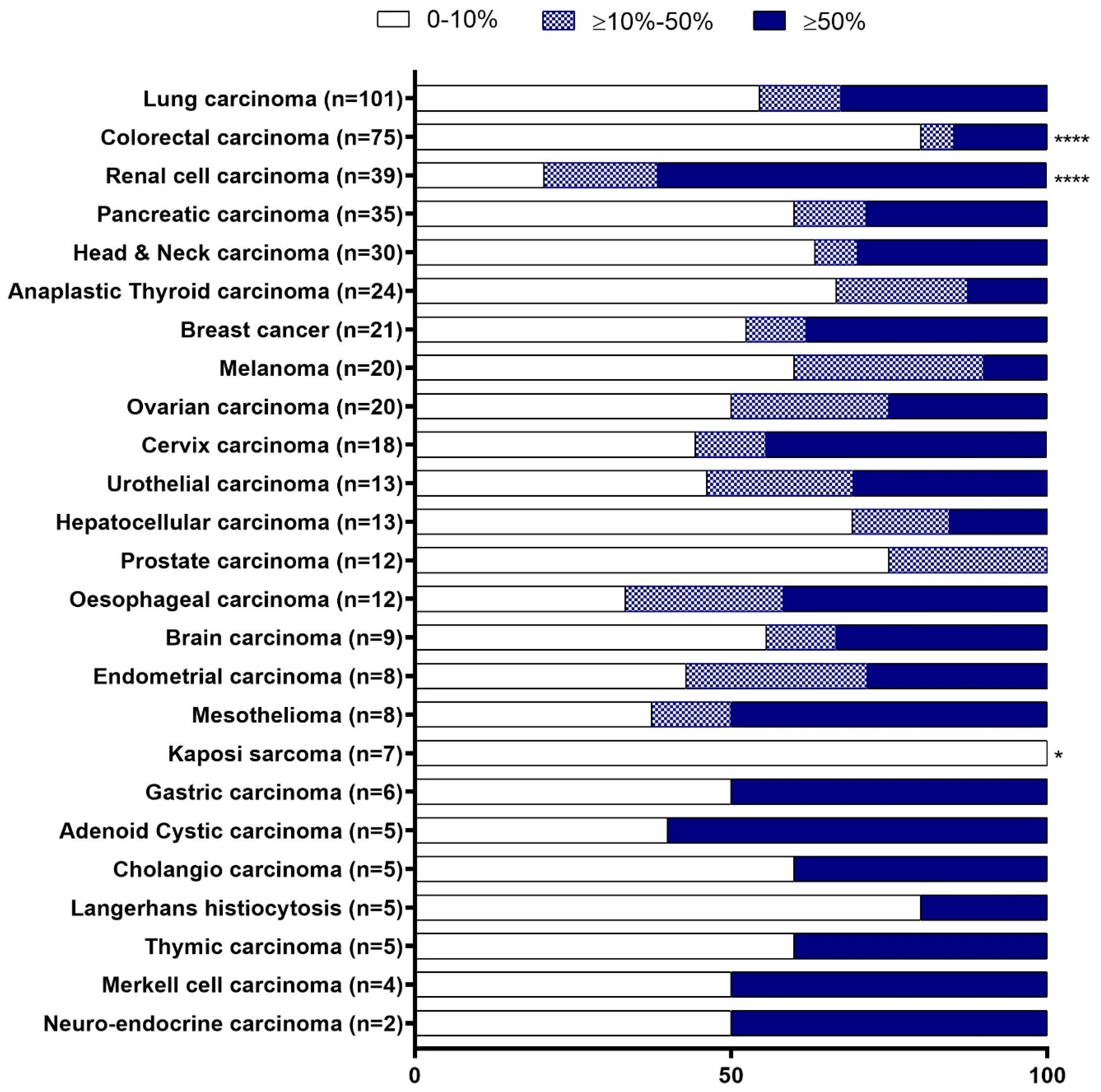
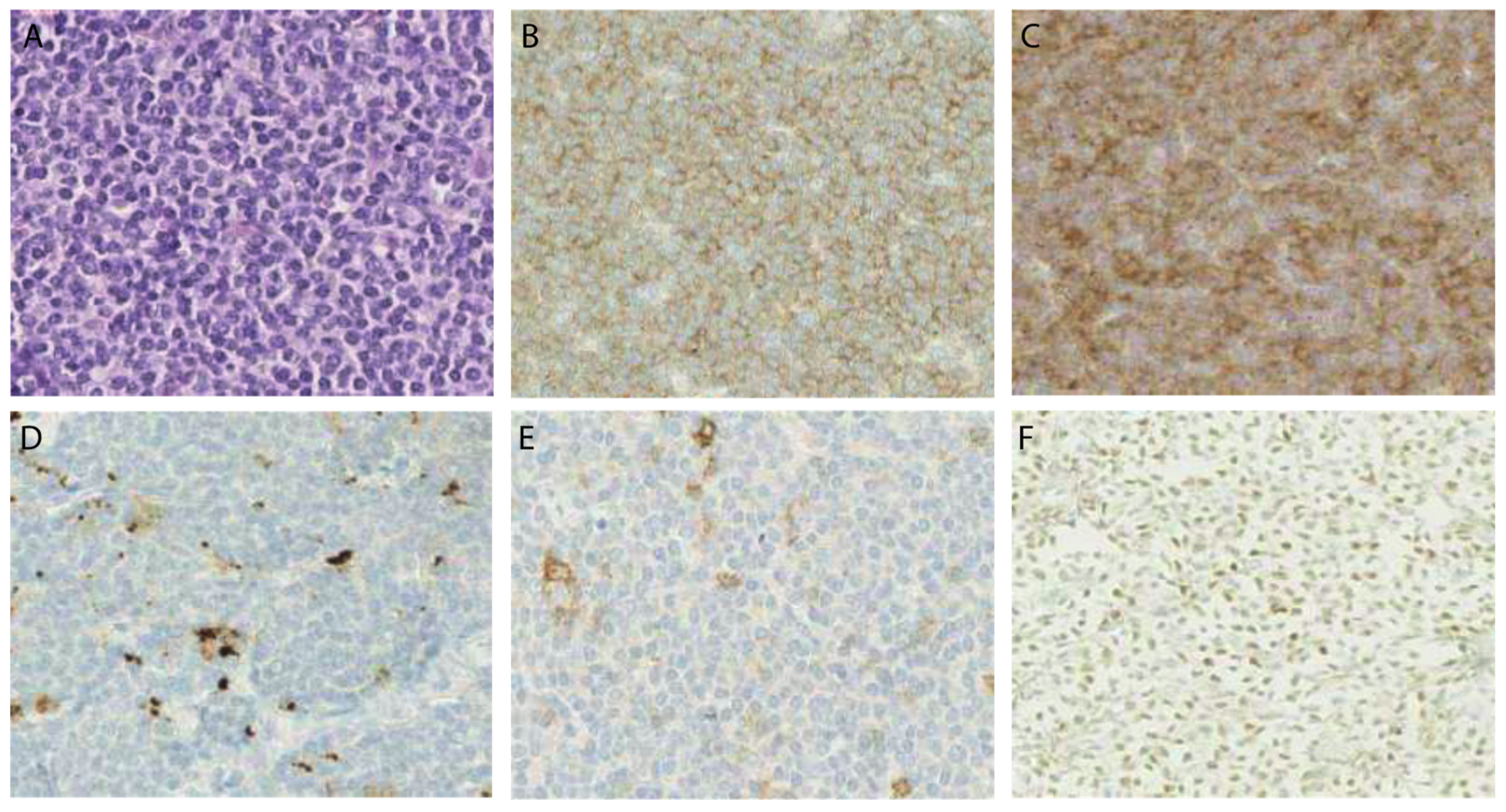
2.1. CD70 Staining Patterns in Solid Tumour Types
2.2. CD70 and CD27 Protein Expression in Haematological Malignancies
2.3. Programmed Cell Death Protein 1 (PD-1) and Its Ligand (PD-L1) Expression in MCL Patient Cohort
3. Discussion
4. Materials and Methods
4.1. Patient Selection and Tissue Specimen
4.2. CD70 IHC
4.3. CD27, PD-1 and PD-L1
4.4. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Zou, W.; Wolchok, J.D.; Chen, L. PD-L1 (B7-H1) and PD-1 pathway blockade for cancer therapy: Mechanisms, response, biomarkers and combinations. Sci. Transl. Med. 2016, 8, 328rv4. [Google Scholar] [CrossRef]
- Cottrell, T.R.; Taube, J.M. PD-L1 and Emerging Biomarkers in Immune Checkpoint Blockade Therapy. Cancer J. 2018, 24, 41–46. [Google Scholar] [CrossRef]
- Nolte, M.A.; van Olffen, R.W.; van Gisbergen, K.P.J.M.; van Lier, R.A.W. Timing and tuning of CD27-CD70 interactions: The impact of signal strength in setting the balance between adaptive responses and immunopathology. Immunol. Rev. 2009, 229, 216–231. [Google Scholar] [CrossRef]
- Laouar, A.; Haridas, V.; Vargas, D.; Zhinan, X.; Chaplin, D.; van Lier, R.A.W.; Manjunath, N. CD70+ antigen-presenting cells control the proliferation and differentiation of T cells in the intestinal mucosa. Nat. Immunol. 2005, 6, 698–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wajant, H. Therapeutic targeting of CD70 and CD27. Expert Opin. Ther. Targets 2016, 20, 959–973. [Google Scholar] [CrossRef] [PubMed]
- Tesselaar, K.; Arens, R.; van Schijndel, G.M.W.; Baars, P.A.; van der Valk, M.A.; Borst, J.; van Oers, M.H.J.; van Lier, R.A.W. Lethal T cell immunodeficiency induced by chronic costimulation via CD27-CD70 interactions. Nat. Immunol. 2003, 4, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Boursalian, T.E.; McEarchern, J.A.; Law, C.-L.; Grewal, I.S. Targeting CD70 for human therapeutic use. Adv. Exp. Med. Biol. 2009, 647, 108–119. [Google Scholar]
- De Meulenaere, A.; Vermassen, T.; Aspeslagh, S.; Zwaenepoel, K.; Deron, P.; Duprez, F.; Ferdinande, L.; Rottey, S. CD70 Expression and Its Correlation with Clinicopathological Variables in Squamous Cell Carcinoma of the Head and Neck. Pathobiology 2016, 83, 327–333. [Google Scholar] [CrossRef]
- Pahl, J.H.; Santos, S.J.; Kuijjer, M.L.; Boerman, G.H.; Sand, L.G.; Szuhai, K.; Cleton-Jansen, A.; Egeler, R.M.; Bovee, J.V.; Schilham, M.W.; et al. Expression of the immune regulation antigen CD70 in osteosarcoma. Cancer Cell Int. 2015, 15, 31. [Google Scholar] [CrossRef]
- Claus, C.; Riether, C.; Schurch, C.; Matter, M.S.; Hilmenyuk, T.; Ochsenbein, A.F. CD27 signaling increases the frequency of regulatory T cells and promotes tumor growth. Cancer Res. 2012, 72, 3664–3676. [Google Scholar] [CrossRef]
- Diegmann, J.; Junker, K.; Loncarevic, I.F.; Michel, S.; Schimmel, B.; von Eggeling, F. Immune escape for renal cell carcinoma: CD70 mediates apoptosis in lymphocytes. Neoplasia 2006, 8, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Wischhusen, J.; Jung, G.; Radovanovic, I.; Beier, C.; Steinbach, J.P.; Rimner, A.; Huang, H.; Schulz, J.B.; Ohgaki, H.; Aguzzi, A.; et al. Identification of CD70-mediated apoptosis of immune effector cells as a novel immune escape pathway of human glioblastoma. Cancer Res. 2002, 62, 2592–2599. [Google Scholar] [PubMed]
- Yang, Z.-Z.; Grote, D.M.; Xiu, B.; Ziesmer, S.C.; Price-Troska, T.L.; Hodge, L.S.; Yates, D.M.; Novak, A.J.; Ansell, S.M. TGF-beta upregulates CD70 expression and induces exhaustion of effector memory T cells in B-cell non-Hodgkin’s lymphoma. Leukemia 2014, 28, 1872–1884. [Google Scholar] [CrossRef] [PubMed]
- Riether, C.; Schurch, C.M.; Buhrer, E.D.; Hinterbrandner, M.; Huguenin, A.-L.; Hoepner, S.; Zlobec, I.; Pabst, T.; Radpour, R.; Ochsenbein, A.F. CD70/CD27 signaling promotes blast stemness and is a viable therapeutic target in acute myeloid leukemia. J. Exp. Med. 2017, 214, 359–380. [Google Scholar] [CrossRef]
- Lens, S.M.; Drillenburg, P.; den Drijver, B.F.; van Schijndel, G.; Pals, S.T.; van Lier, R.A.; van Oers, M.H. Aberrant expression and reverse signalling of CD70 on malignant B cells. Br. J. Haematol. 1999, 106, 491–503. [Google Scholar] [CrossRef]
- Riether, C.; Schurch, C.M.; Flury, C.; Hinterbrandner, M.; Druck, L.; Huguenin, A.-L.; Baerlocher, G.M.; Radpour, R.; Ochsenbein, A.F. Tyrosine kinase inhibitor-induced CD70 expression mediates drug resistance in leukemia stem cells by activating Wnt signaling. Sci. Transl. Med. 2015, 7, 298ra119. [Google Scholar] [CrossRef]
- Aftimos, P.; Rolfo, C.; Rottey, S.; Offner, F.; Bron, D.; Maerevoet, M.; Soria, J.; Moshir, M.; Dreier, T.; Rompaey, L.V.; et al. Phase I Dose-Escalation Study of the Anti-CD70 Antibody ARGX-110 in Advanced Malignancies. Clin. Cancer Res. 2017, 23, 6411–6420. [Google Scholar] [CrossRef] [Green Version]
- Ochsenbein, A.F.; Riether, C.; Bacher, U.; Müller, R.; Höpner, S.; Banz, Y.; Hinterbrandner, M.; Bargetzi, M.; Manz, M.G.; Van Rompaey, L.; et al. Argx-110 Targeting CD70, in Combination with Azacitidine, Shows Favorable Safety Profile and Promising Anti-Leukemia Activity in Newly Diagnosed AML Patients in an Ongoing Phase 1/2 Clinical Trial. Blood 2018, 132, 2680. [Google Scholar] [CrossRef]
- Diegmann, J.; Junker, K.; Gerstmayer, B.; Bosio, A.; Hindermann, W.; Rosenhahn, J.; von Eggeling, F. Identification of CD70 as a diagnostic biomarker for clear cell renal cell carcinoma by gene expression profiling, real-time RT-PCR and immunohistochemistry. Eur. J. Cancer 2005, 41, 1794–1801. [Google Scholar] [CrossRef]
- Jacobs, J.; Deschoolmeester, V.; Zwaenepoel, K.; Rolfo, C.; Silence, K.; Rottey, S.; Lardon, F.; Smits, E.; Pauwels, P. CD70: An emerging target in cancer immunotherapy. Pharmacol. Ther. 2015, 155, 1–10. [Google Scholar] [CrossRef]
- Bertrand, P.; Maingonnat, C.; Penther, D.; Guney, S.; Ruminy, P.; Picquenot, J.M.; Mareschal, S.; Alcantara, M.; Bouzelfen, A.; Dubois, S.; et al. The costimulatory molecule CD70 is regulated by distinct molecular mechanisms and is associated with overall survival in diffuse large B-cell lymphoma. Genes. Chromosomes Cancer 2013, 52, 764–774. [Google Scholar] [CrossRef] [PubMed]
- Jilaveanu, L.B.; Sznol, J.; Aziz, S.A.; Duchen, D.; Kluger, H.M.; Camp, R.L. CD70 expression patterns in renal cell carcinoma. Hum. Pathol. 2012, 43, 1394–1399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petrau, C.; Cornic, M.; Bertrand, P.; Maingonnat, C.; Marchand, V.; Picquenot, J.-M.; Jardin, F.; Clatot, F. CD70: A Potential Target in Breast Cancer? J. Cancer 2014, 5, 761–764. [Google Scholar] [CrossRef] [PubMed]
- Goto, N.; Tsurumi, H.; Takemura, M.; Kanemura, N.; Kasahara, S.; Hara, T.; Yasuda, I.; Shimizu, M.; Yamada, T.; Sawada, M.; et al. Serum soluble CD27 level is associated with outcome in patients with diffuse large B-cell lymphoma treated with rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone. Leuk. Lymphoma 2012, 53, 1494–1500. [Google Scholar] [CrossRef]
- Nilsson, A.; de Milito, A.; Mowafi, F.; Winberg, G.; Bjork, O.; Wolpert, E.Z.; Chiodi, F. Expression of CD27-CD70 on early B cell progenitors in the bone marrow: Implication for diagnosis and therapy of childhood ALL. Exp. Hematol. 2005, 33, 1500–1507. [Google Scholar] [CrossRef]
- Jacobs, J.; Zwaenepoel, K.; Rolfo, C.; Van den Bossche, J.; Deben, C.; Silence, K.; Hermans, C.; Smits, E.; Van Schil, P.; Lardon, F.; et al. Unlocking the potential of CD70 as a novel immunotherapeutic target for non-small cell lung cancer. Oncotarget 2015, 6, 13462–13475. [Google Scholar] [CrossRef] [Green Version]
- Rolfo, C.; Sortino, G.; Smits, E.; Passiglia, F.; Bronte, G.; Castiglia, M.; Russo, A.; Santos, E.S.; Janssens, A.; Pauwels, P.; et al. Immunotherapy: Is a minor god yet in the pantheon of treatments for lung cancer? Expert Rev. Anticancer Ther. 2014, 14, 1173–1187. [Google Scholar] [CrossRef]
- Riether, C.; Schurch, C.; Ochsenbein, A.F. Modulating CD27 signaling to treat cancer. Oncoimmunology 2012, 1, 1604–1606. [Google Scholar] [CrossRef] [Green Version]
- Silence, K.; Dreier, T.; Moshir, M.; Ulrichts, P.; Gabriels, S.M.E.; Saunders, M.; Wajant, H.; Brouckaert, P.; Huyghe, L.; Hauwermeiren, T.V.; et al. ARGX-110, a highly potent antibody targeting CD70, eliminates tumors via both enhanced ADCC and immune checkpoint blockade. MAbs 2014, 6, 523–532. [Google Scholar] [CrossRef]
- Rizzardi, A.E.; Johnson, A.T.; Vogel, R.I.; Pambuccian, S.E.; Henriksen, J.; Skubitz, A.P.; Metzger, G.J.; Schmechel, S.C. Quantitative comparison of immunohistochemical staining measured by digital image analysis versus pathologist visual scoring. Diagn. Pathol. 2012, 7, 42. [Google Scholar] [CrossRef]
- Law, C.-L.; Gordon, K.A.; Toki, B.E.; Yamane, A.K.; Hering, M.A.; Cerveny, C.G.; Petroziello, J.M.; Ryan, M.C.; Smith, L.; Simon, R.; et al. Lymphocyte activation antigen CD70 expressed by renal cell carcinoma is a potential therapeutic target for anti-CD70 antibody-drug conjugates. Cancer Res. 2006, 66, 2328–2337. [Google Scholar] [CrossRef] [PubMed]
- Junker, K.; Hindermann, W.; von Eggeling, F.; Diegmann, J.; Haessler, K.; Schubert, J. CD70: A new tumor specific biomarker for renal cell carcinoma. J. Urol. 2005, 173, 2150–2153. [Google Scholar] [CrossRef] [PubMed]
- Ryan, M.C.; Kostner, H.; Gordon, K.A.; Duniho, S.; Sutherland, M.K.; Yu, C.; Kim, K.M.; Nesterova, A.; Anderson, M.; McEarchern, J.A.; et al. Targeting pancreatic and ovarian carcinomas using the auristatin-based anti-CD70 antibody-drug conjugate SGN-75. Br. J. Cancer 2010, 103, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Adam, P.J.; Terrett, J.A.; Steers, G.; Stockwin, L.; Loader, J.A.; Fletcher, G.C.; Lu, L.-S.; Leach, B.I.; Mason, S.; Stamps, A.C.; et al. CD70 (TNFSF7) is expressed at high prevalence in renal cell carcinomas and is rapidly internalised on antibody binding. Br. J. Cancer 2006, 95, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, K.; Kishibe, K.; Nagato, T.; Ueda, S.; Komabayashi, Y.; Takahara, M.; Harabuchi, Y. Expression of CD70 in nasal natural killer/T cell lymphoma cell lines and patients; its role for cell proliferation through binding to soluble CD27. Br. J. Haematol. 2013, 160, 331–342. [Google Scholar] [CrossRef]
- Xerri, L.; Chetaille, B.; Serriari, N.; Attias, C.; Guillaume, Y.; Arnoulet, C.; Olive, D. Programmed death 1 is a marker of angioimmunoblastic T-cell lymphoma and B-cell small lymphocytic lymphoma/chronic lymphocytic leukemia. Hum. Pathol. 2008, 39, 1050–1058. [Google Scholar] [CrossRef]
- Andorsky, D.J.; Yamada, R.E.; Said, J.; Pinkus, G.S.; Betting, D.J.; Timmerman, J.M. Programmed death ligand 1 is expressed by non-hodgkin lymphomas and inhibits the activity of tumor-associated T cells. Clin. Cancer Res. 2011, 17, 4232–4244. [Google Scholar] [CrossRef]
- Menter, T.; Bodmer-Haecki, A.; Dirnhofer, S.; Tzankov, A. Evaluation of the diagnostic and prognostic value of PDL1 expression in Hodgkin and B-cell lymphomas. Hum. Pathol. 2016, 54, 17–24. [Google Scholar] [CrossRef]
- Lesokhin, A.M.; Ansell, S.M.; Armand, P.; Scott, E.C.; Halwani, A.; Gutierrez, M.; Millenson, M.M.; Cohen, A.D.; Schuster, S.J.; Lebovic, D.; et al. Nivolumab in Patients With Relapsed or Refractory Hematologic Malignancy: Preliminary Results of a Phase Ib Study. J. Clin. Oncol. 2016, 34, 2698–2704. [Google Scholar] [CrossRef] [Green Version]


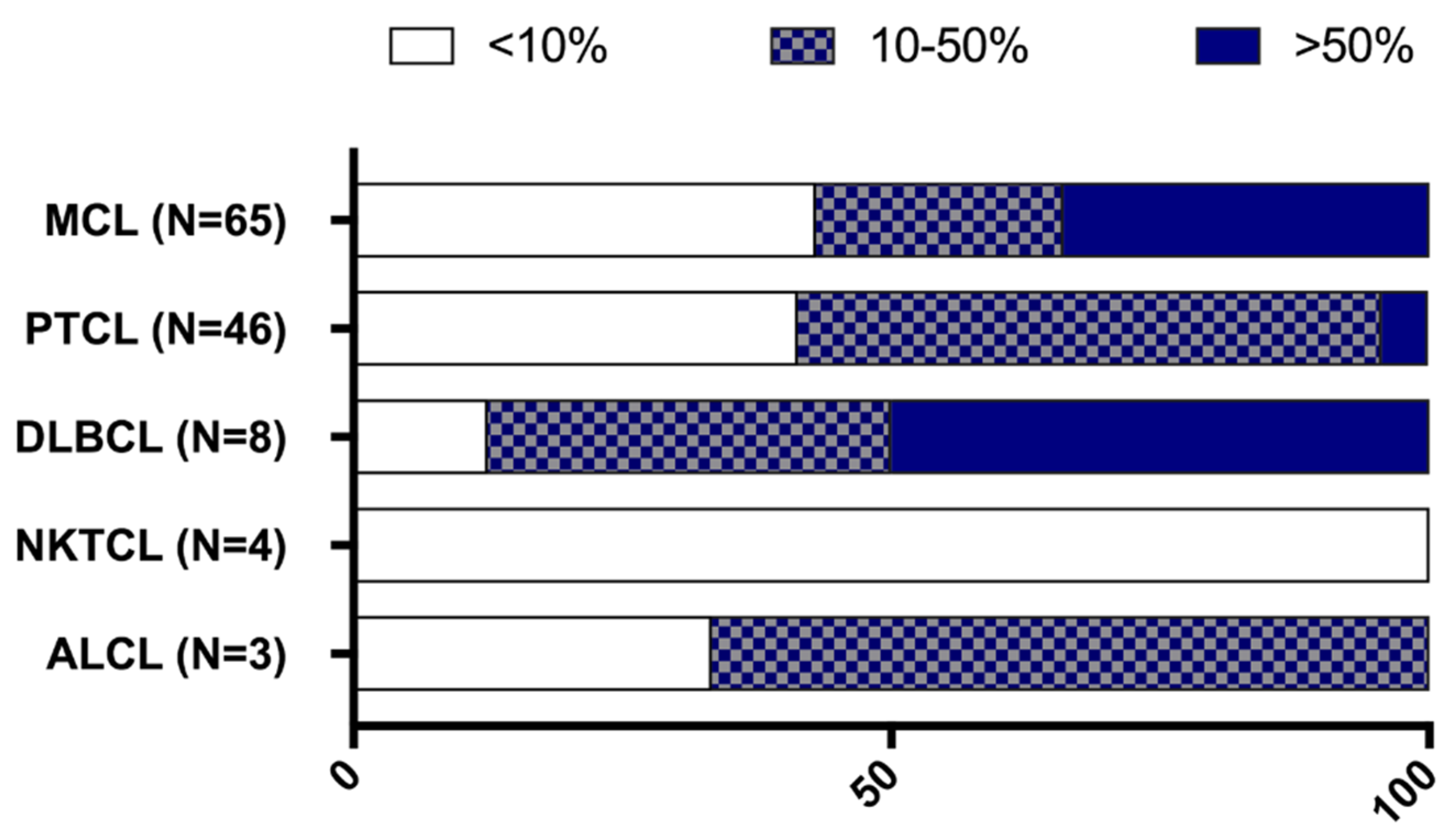
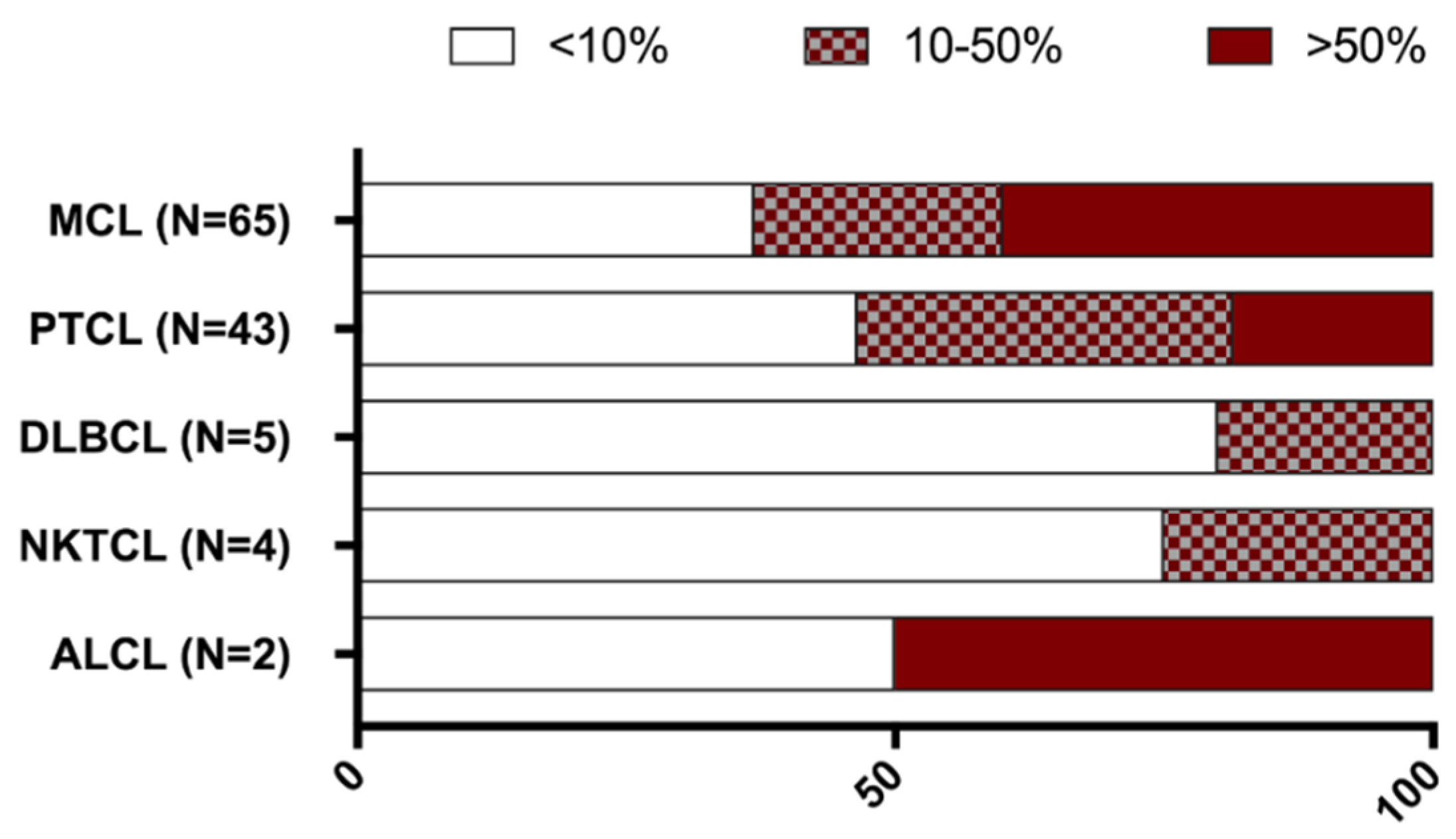

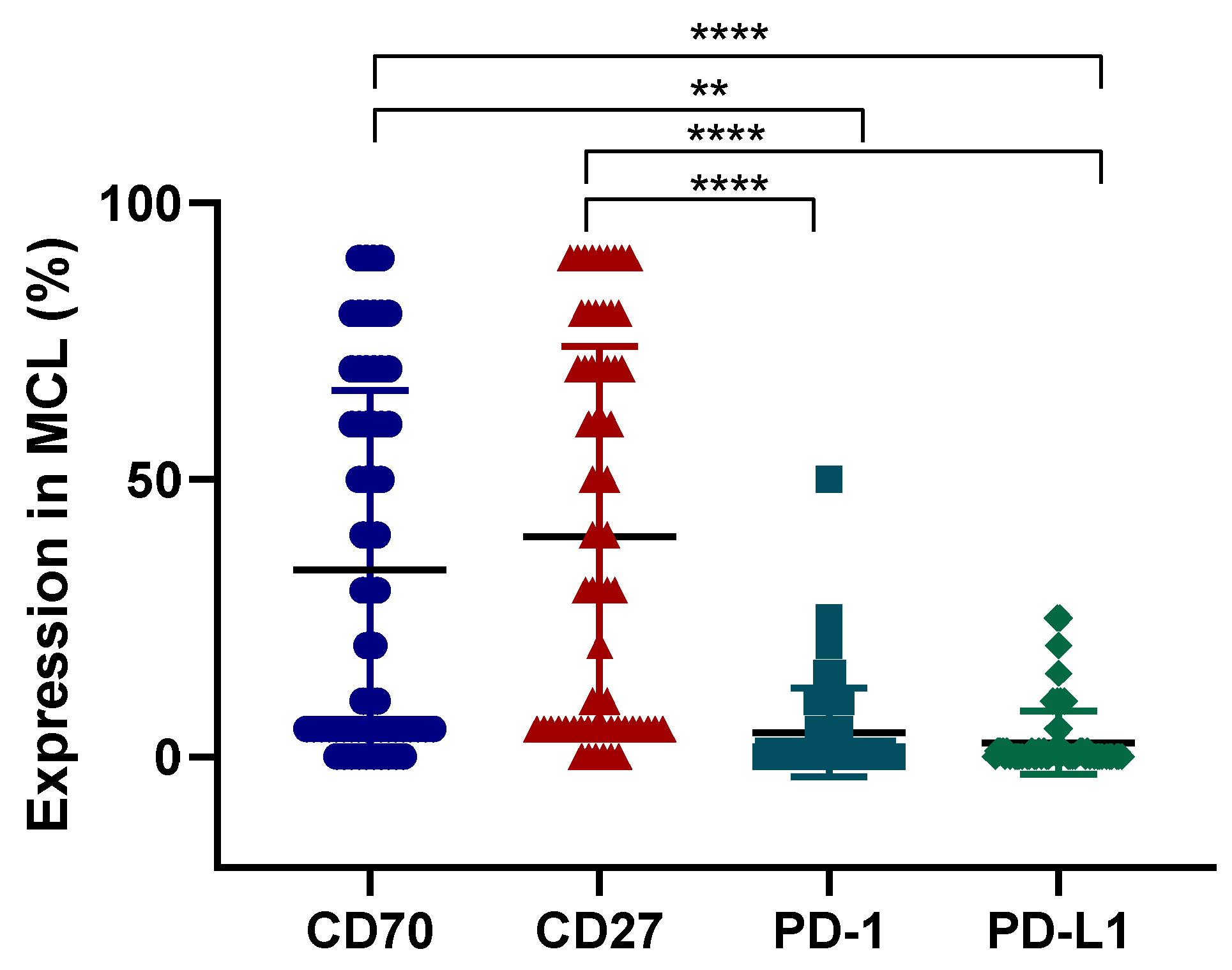
| CD70/CD27 | Diagnosis N = 37 | Relapse N = 28 | All Tumour Samples N = 65 |
|---|---|---|---|
| CD70+, n (%) | 20 (54) | 17 (61) | 37 (57) |
| Staining %, median (range) | 60% (10–90%) | 60% (10–90%) | 60% (10–90%) |
| ≥ 50% staining, n (%) | 13 (65) | 13 (76) | 26 (70) |
| CD27+, n (%) | 24 (65) | 17 (61) | 41(63) |
| Staining %, median (range) | 60% (30–90%) | 70% (10–90%) | 70% (10–90%) |
| ≥ 50% staining, n (%) | 16 (67) | 13 (76) | 29 (71) |
| CD70+, CD27+, n (%) | 15 (41) | 10 (36) | 25 (38) |
| PD-L1/PD-1 | Diagnosis N = 37 | Relapse N = 28 | All Tumour Samples N = 65 |
|---|---|---|---|
| PD-L1+, n (%) | 7 (19) | 5 (18) | 12 (18) |
| Staining %, median (range) | 10% (10–25%) | 10% (5–25%) | 10% (5–25%) |
| PD-1+, n (%) | 14 (38) | 9 (32) | 23 (35) |
| Staining %, median (range) | 10% (5–25%) | 10% (5–50%) | 10% (5–50%) |
| PD-1+, PD-L1+, n (%) | 5 (14) | 3 (11) | 8 (12) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flieswasser, T.; Camara-Clayette, V.; Danu, A.; Bosq, J.; Ribrag, V.; Zabrocki, P.; Van Rompaey, L.; de Haard, H.; Zwaenepoel, K.; Smits, E.; et al. Screening a Broad Range of Solid and Haematological Tumour Types for CD70 Expression Using a Uniform IHC Methodology as Potential Patient Stratification Method. Cancers 2019, 11, 1611. https://doi.org/10.3390/cancers11101611
Flieswasser T, Camara-Clayette V, Danu A, Bosq J, Ribrag V, Zabrocki P, Van Rompaey L, de Haard H, Zwaenepoel K, Smits E, et al. Screening a Broad Range of Solid and Haematological Tumour Types for CD70 Expression Using a Uniform IHC Methodology as Potential Patient Stratification Method. Cancers. 2019; 11(10):1611. https://doi.org/10.3390/cancers11101611
Chicago/Turabian StyleFlieswasser, Tal, Valérie Camara-Clayette, Alina Danu, Jacques Bosq, Vincent Ribrag, Piotr Zabrocki, Luc Van Rompaey, Hans de Haard, Karen Zwaenepoel, Evelien Smits, and et al. 2019. "Screening a Broad Range of Solid and Haematological Tumour Types for CD70 Expression Using a Uniform IHC Methodology as Potential Patient Stratification Method" Cancers 11, no. 10: 1611. https://doi.org/10.3390/cancers11101611
APA StyleFlieswasser, T., Camara-Clayette, V., Danu, A., Bosq, J., Ribrag, V., Zabrocki, P., Van Rompaey, L., de Haard, H., Zwaenepoel, K., Smits, E., Pauwels, P., & Jacobs, J. (2019). Screening a Broad Range of Solid and Haematological Tumour Types for CD70 Expression Using a Uniform IHC Methodology as Potential Patient Stratification Method. Cancers, 11(10), 1611. https://doi.org/10.3390/cancers11101611







