Calcium Regulates HCC Proliferation as well as EGFR Recycling/Degradation and Could Be a New Therapeutic Target in HCC
Abstract
1. Introduction
2. Results
2.1. EGFR Sequencing
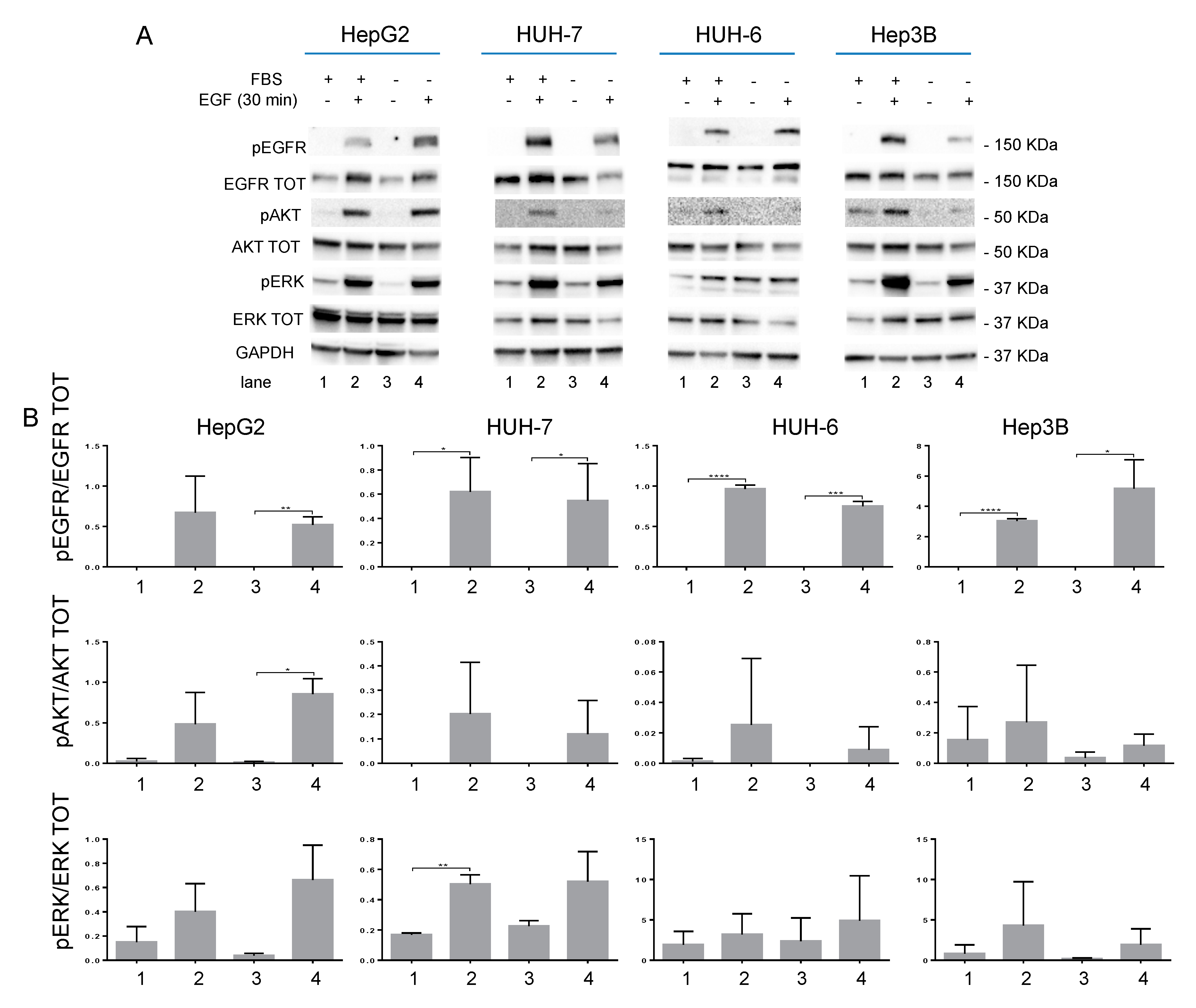
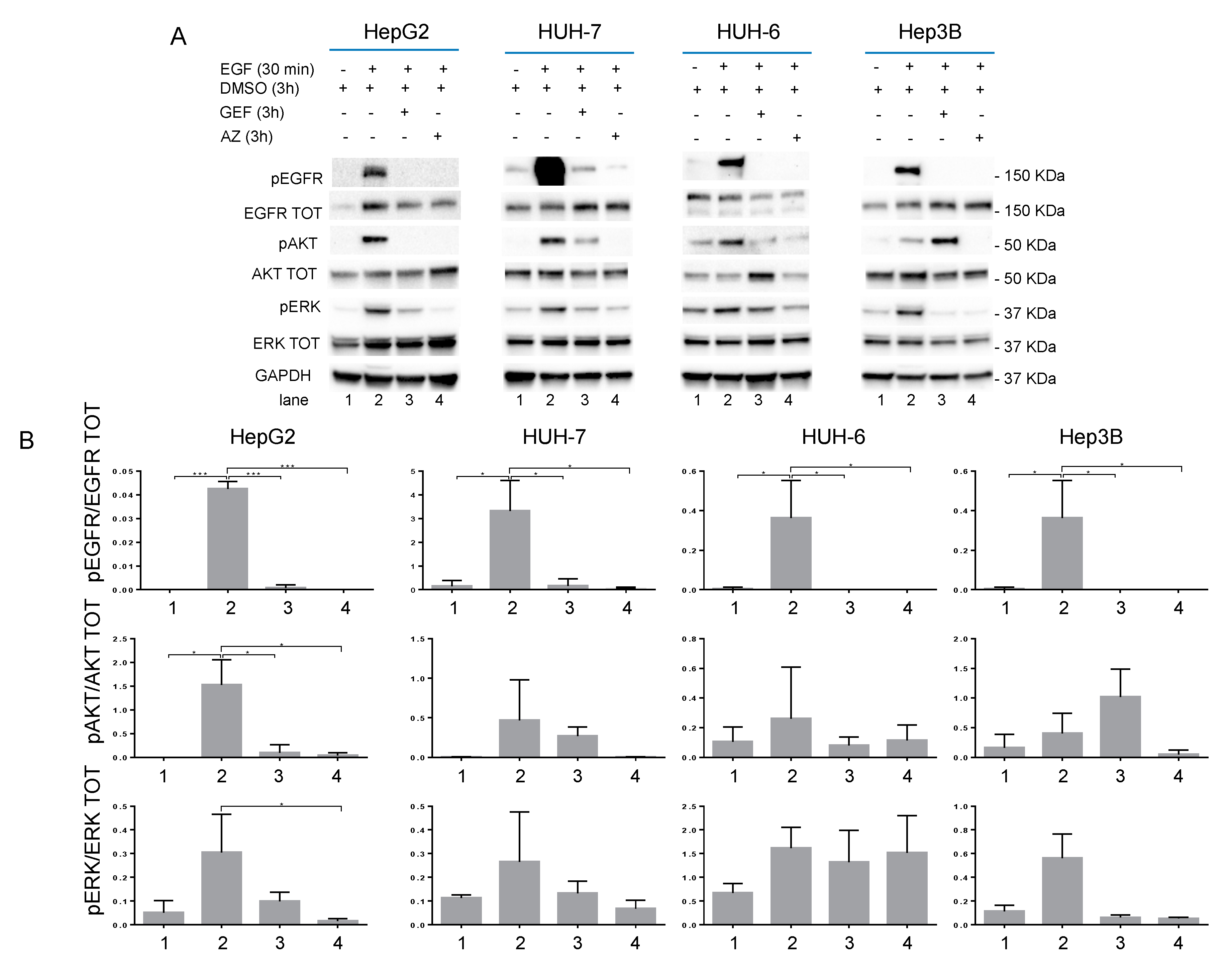
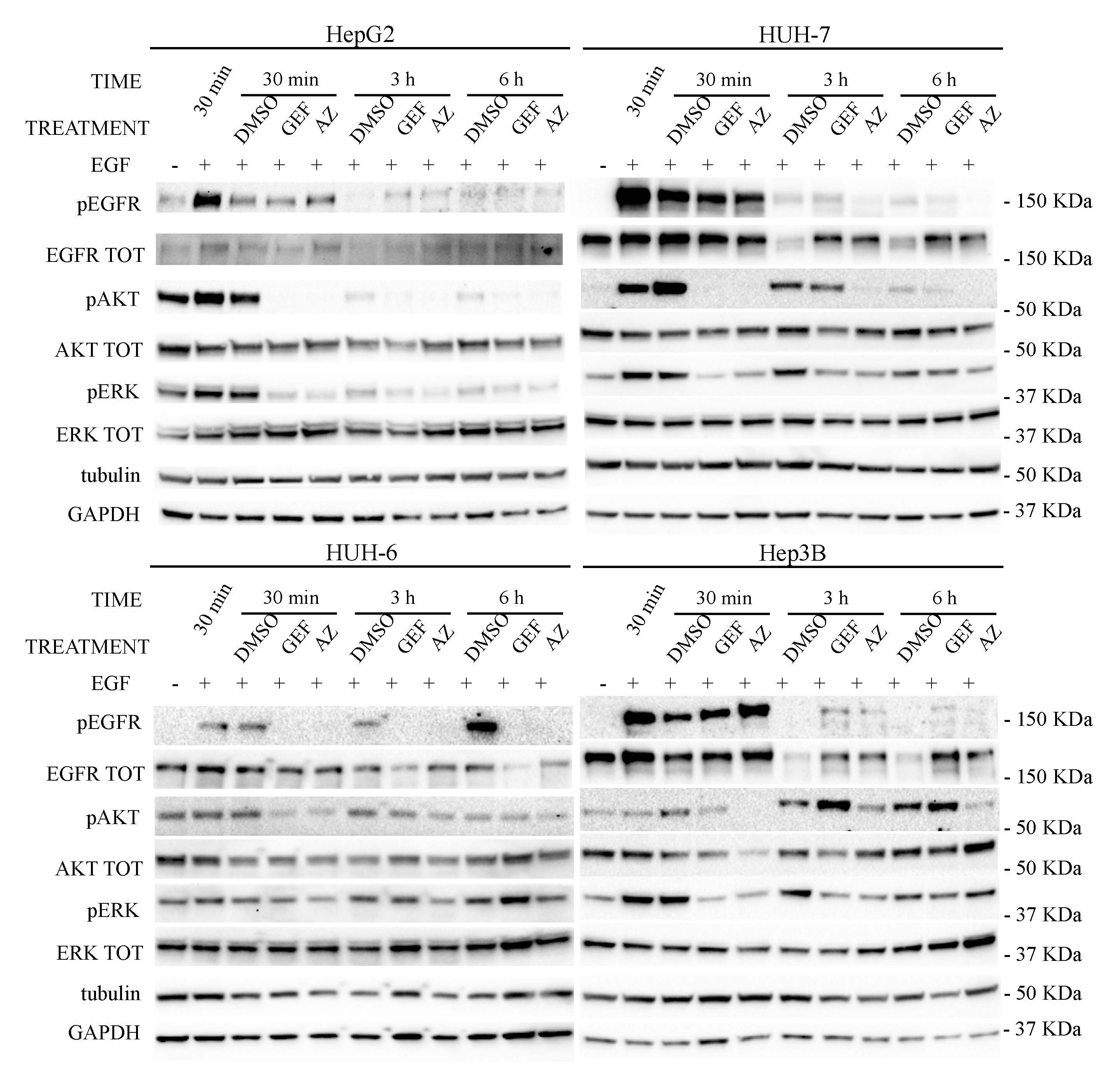
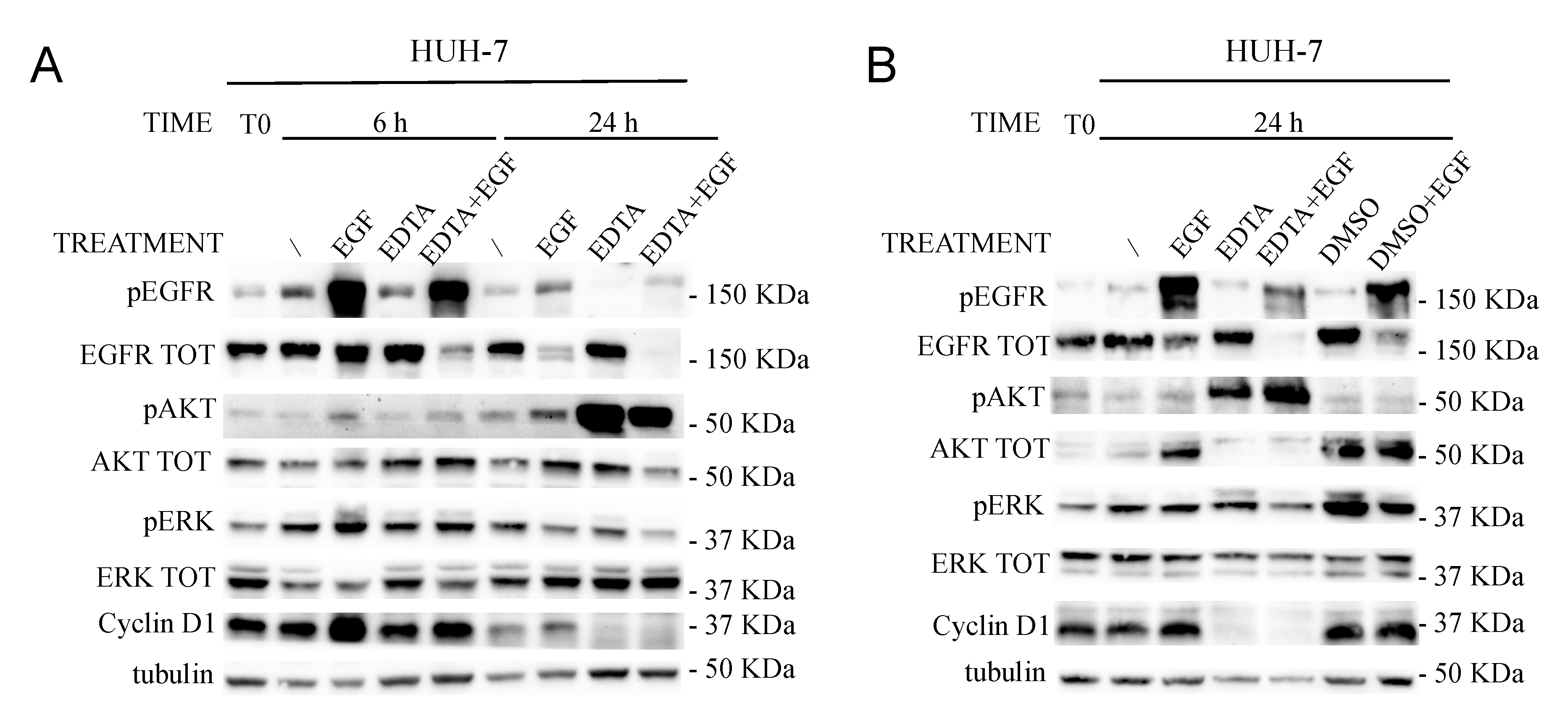
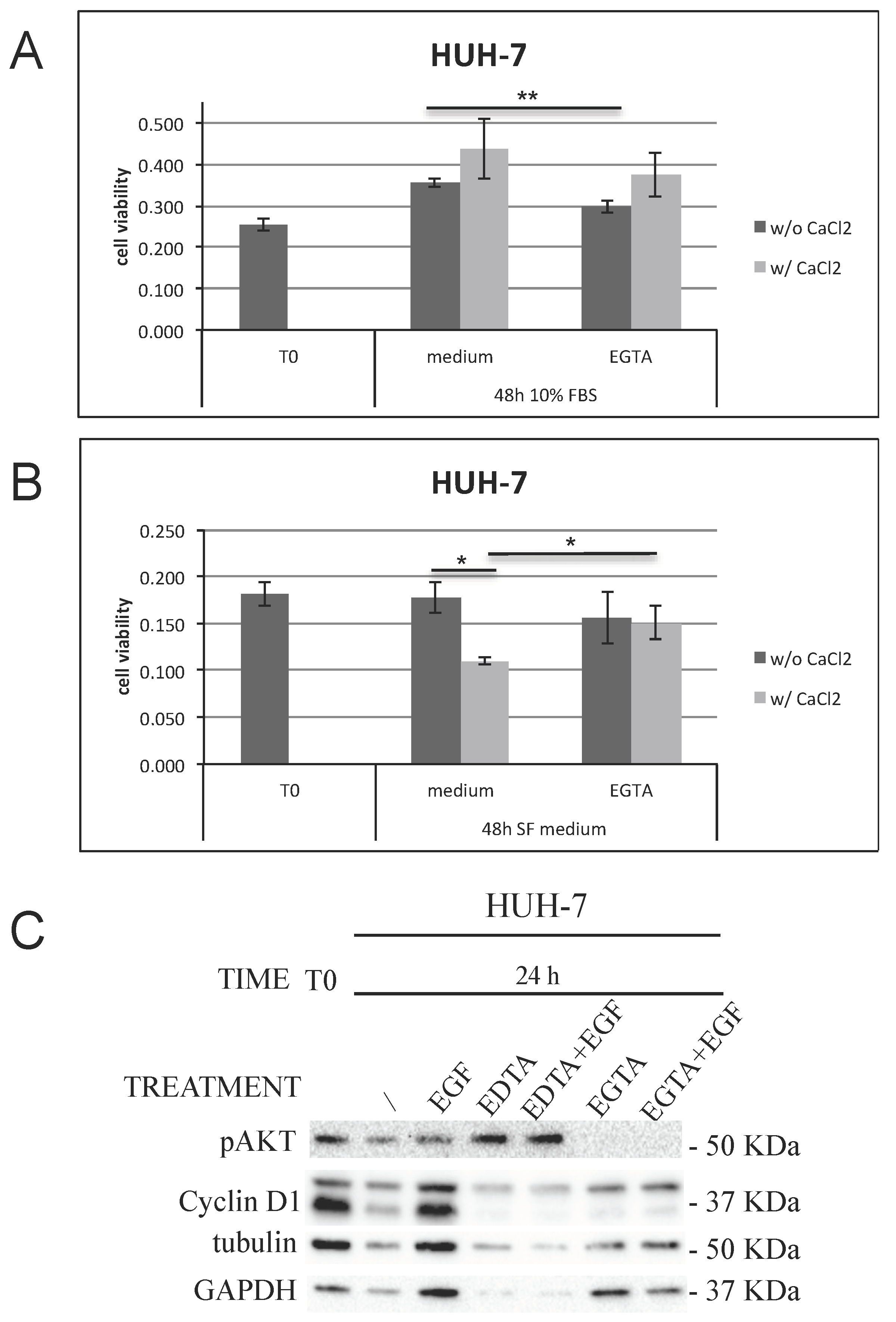
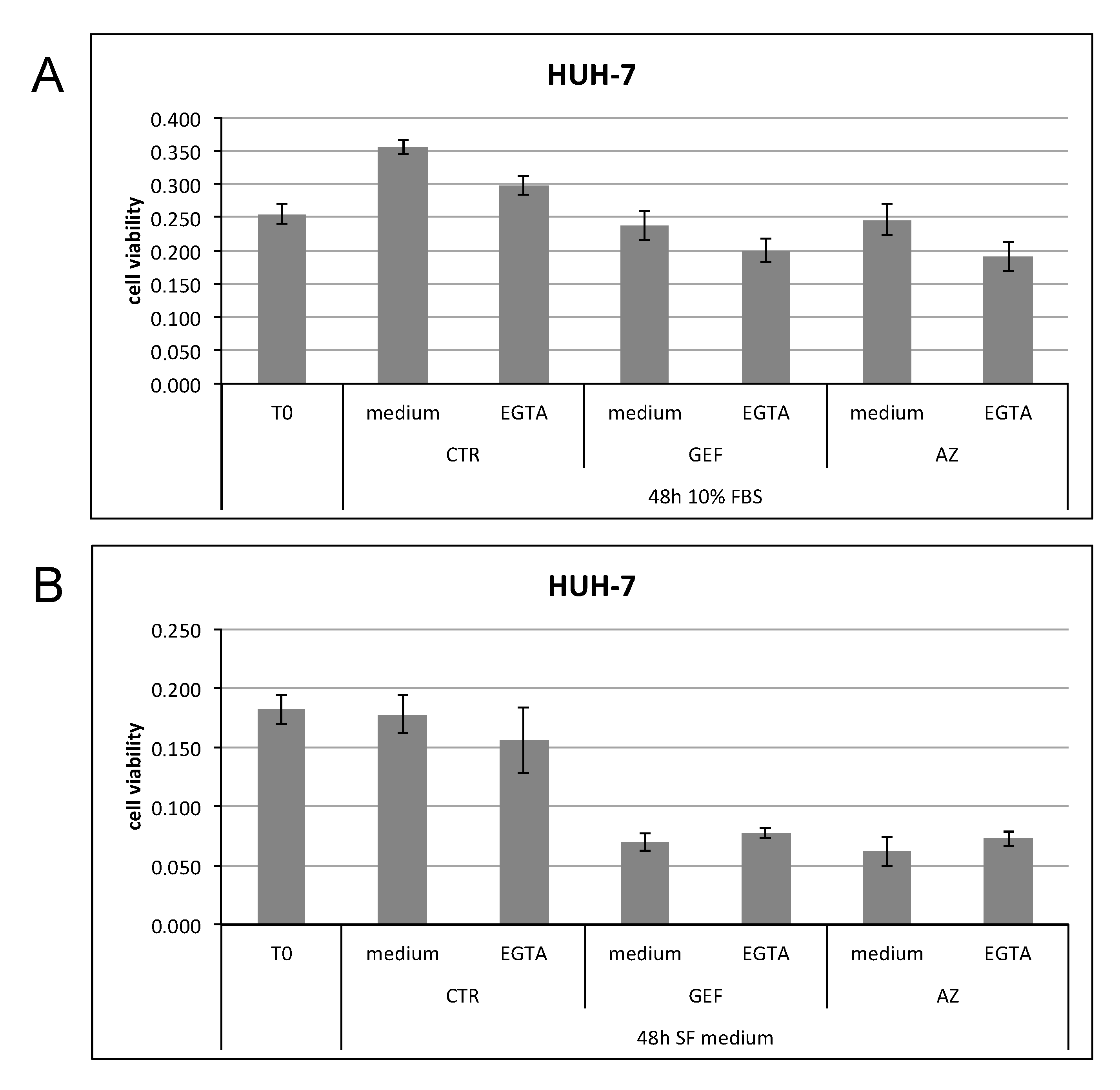
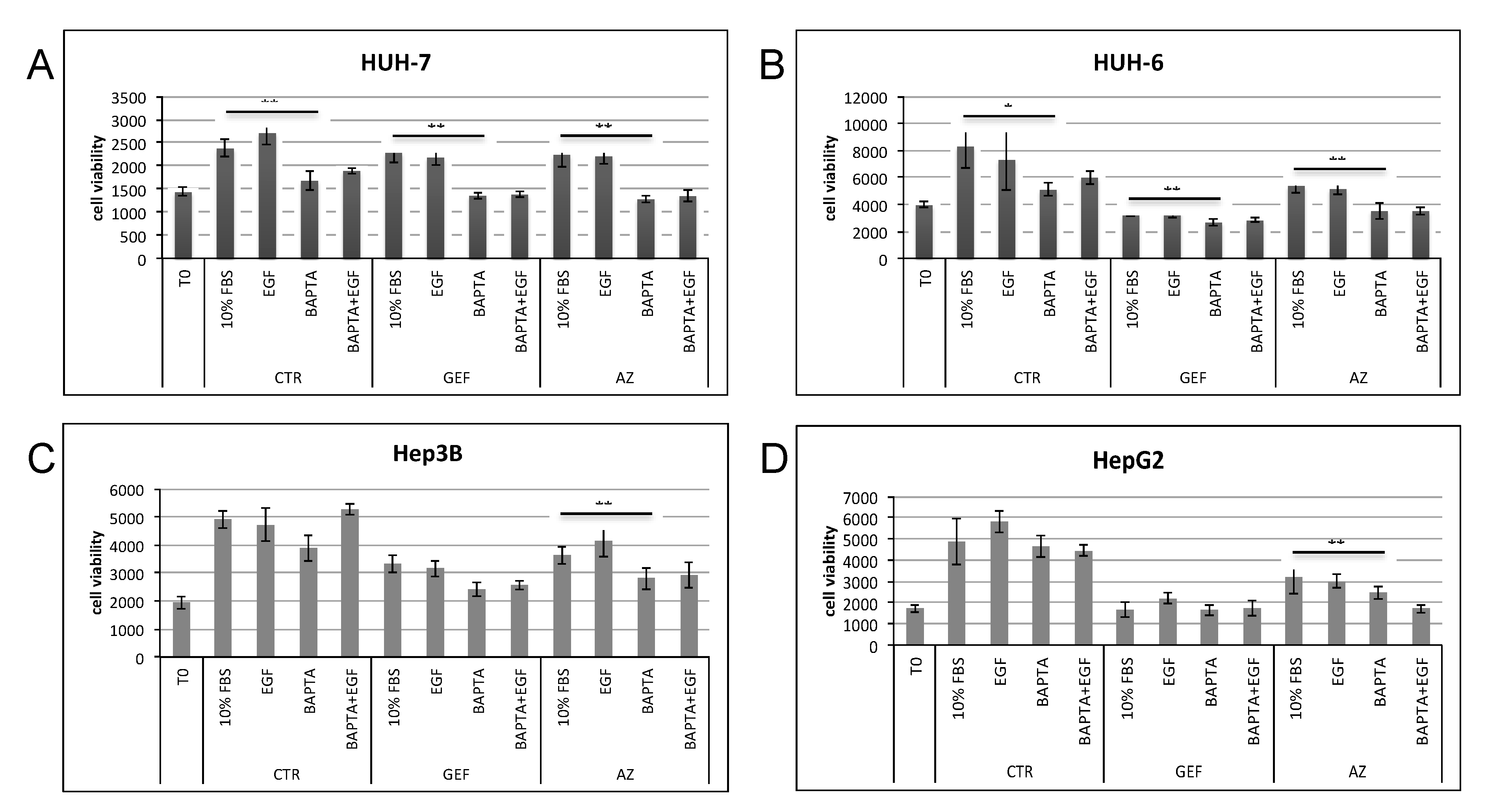
2.2. EGFR Signaling and Its Inhibition
2.3. EGFR Signaling and Calcium Chelators
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. Protein Extraction
4.3. Cell Viability Assay
4.4. Antibodies and Drug Formulations
4.5. Western Blot Analysis
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Llovet, J.M.; Beaugrand, M. Hepatocellular carcinoma: Present status and future prospects. J. Hepatol. 2003, 38, 136–149. [Google Scholar] [CrossRef]
- Parkin, D.M.; Bray, F.; Ferlay, J.; Pisani, P. Global cancer statistics. CA Cancer J. Clin. 2005, 55, 74–108. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Wolk, A. Overweight, obesity and risk of liver cancer: A meta-analysis of cohort studies. Br. J. Cancer 2007, 97, 1005–1008. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, A.; Llovet, J.M. Targeted therapies for hepatocellular carcinoma. Gastroenterology 2011, 140, 1410–1426. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, A.; Newell, P.; Chiang, D.; Friedman, S.; Llovet, J.M. Genomics and Signaling Pathways in Hepatocellular Carcinoma. Semin. Liver Dis. 2007, 27, 55–76. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, S.; Marais, R.; Zhu, A.X. The role of signaling pathways in the development and treatment of hepatocellular carcinoma. Oncogene 2010, 29, 4989–5005. [Google Scholar] [CrossRef]
- Berridge, M.J.; Lipp, P.; Bootman, M.D. The versatility and universality of calcium signalling. Nat. Rev. Mol. Cell Biol. 2000, 1, 11–21. [Google Scholar] [CrossRef]
- Michael, M.; Kulkarni, R.N.; Postic, C.; Previs, S.F.; Shulman, G.I.; Magnuson, M.A.; Kahn, C. Loss of Insulin Signaling in Hepatocytes Leads to Severe Insulin Resistance and Progressive Hepatic Dysfunction. Mol. Cell 2000, 6, 87–97. [Google Scholar] [CrossRef]
- Sjögren, K.; Liu, J.-L.; Blad, K.; Skrtic, S.; Vidal, O.; Wallenius, V.; Leroith, D.; Törnell, J.; Isaksson, O.G.P.; Jansson, J.-O.; et al. Liver-derived insulin-like growth factor I (IGF-I) is the principal source of IGF-I in blood but is not required for postnatal body growth in mice. Proc. Natl. Acad. Sci. USA 1999, 96, 7088–7092. [Google Scholar] [CrossRef]
- Bataller, R.B.D. Liver fibrosis. J. Clin. Investig. 2005, 115, 209–218. [Google Scholar] [CrossRef]
- Trusolino, L.; Bertotti, A.; Comoglio, P.M. MET signalling: Principles and functions in development, organ regeneration and cancer. Nat. Rev. Mol. Cell Biol. 2010, 11, 834–848. [Google Scholar] [CrossRef] [PubMed]
- Joffre, C.; Barrow, R.; Ménard, L.; Calleja, V.; Hart, I.R.; Kermorgant, S. A direct role for Met endocytosis in tumorigenesis. Nature 2011, 13, 827–837. [Google Scholar] [CrossRef] [PubMed]
- Thorgeirsson, S.S.; Grisham, J.W. Molecular pathogenesis of human hepatocellular carcinoma. Nat. Genet. 2002, 31, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Berasain, C.C.J.; Perrugorrìa, M.J.; Prieto, J.; Avila, M.A. Amphiregulin: A new growth factor in hepatocarcinogenesis. Cancer Letter 2007, 254, 30–41. [Google Scholar] [CrossRef]
- Paradis, V.; Bieche, I.; Dargere, D.; Laurendeau, I.; Laurent, C.; Bioulac Sage, P.; Degott, C.; Belghiti, J.; Vidaud, M.; Bedossa, P. Molecular Profiling of Hepatocellular Carcinomas (HCC) Using a Large-Scale Real-Time RT-PCR Approach. Am. J. Pathol. 2003, 163, 733–741. [Google Scholar] [CrossRef]
- Zaiss, D.M.; Van Loosdregt, J.; Gorlani, A.; Bekker, C.P.; Grone, A.; Sibilia, M.; Henegouwen, P.M.P.V.B.E.; Roovers, R.C.; Coffer, P.J.; Sijts, A.J.A.M. Amphiregulin enhances regulatory T cell-suppressive function via the epidermal growth factor receptor. Immunity 2013, 38, 275–284. [Google Scholar] [CrossRef]
- Gan, H.K.; Cvrljevic, A.N.; Johns, T.G. The epidermal growth factor receptor variant III (EGFRvIII): where wild things are altered. FEBS J. 2013, 280, 5350–5370. [Google Scholar] [CrossRef]
- Martinelli, E.; De Palma, R.; Orditura, M.; De Vita, F.; Ciardiello, F. Anti-epidermal growth factor receptor monoclonal antibodies in cancer therapy. Clin. Exp. Immunol. 2009, 158, 1–9. [Google Scholar] [CrossRef]
- Ciardiello, F.; Tortora, G. EGFR Antagonists in Cancer Treatment. N. Engl. J. Med. 2008, 358, 1160–1174. [Google Scholar] [CrossRef]
- Tanaka, H. Immunohistochemical studies on epidermal growth factor receptor in hepatocellular carcinoma. Nihon Shokakibyo Gakkai Zasshi 1991, 88, 138–144. [Google Scholar] [CrossRef][Green Version]
- Nosseir, M.; Zoheiry, M.; Ghali, A.; El-Bassiouni, N.; El-Bassiouni, A.; El-Ahwany, E.; El-Bassiouni, A.; El-Ahwany, E. Immunohistochemical expression of CD95 (Fas), c-myc and epidermal growth factor receptor in hepatitis C virus infection, cirrhotic liver disease and hepatocellular carcinoma. APMIS 2006, 114, 420–427. [Google Scholar]
- Ito, Y.; Takeda, T.; Sakon, M.; Tsujimoto, M.; Higashiyama, S.; Noda, K.; Miyoshi, E.; Monden, M.; Matsuura, N. Expression and clinical significance of erb-B receptor family in hepatocellular carcinoma. Br. J. Cancer 2001, 84, 1377–1383. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Qin, L.; Wang, X.; Zhou, G.; Liao, Y.; Weng, Y.; Jiang, X.; Lin, Z.; Liu, K.; Ye, S. Alterations of oncogenes, tumor suppressor genes and growth factors in hepatocellular carcinoma: with relation to tumor size and invasiveness. Chin. Med. J. 1998, 111, 313–318. [Google Scholar] [PubMed]
- Höpfner, M.; Sutter, A.P.; Huether, A.; Schuppan, D.; Zeitz, M.; Scherübl, H. Targeting the epidermal growth factor receptor by gefitinib for treatment of hepatocellular carcinoma. J. Hepatol. 2004, 41, 1008–1016. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Poon, R.T.; Shao, W.; Sun, X.; Chen, H.; Kok, T.W.; Fan, S.T. Blockage of epidermal growth factor receptor by quinazoline tyrosine kinase inhibitors suppresses growth of human hepatocellular carcinoma. Cancer Lett. 2007, 248, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Schiffer, E.; Housset, C.; Cacheux, W.; Wendum, D.; Rey, C.; Poupon, R.; Rosmorduc, O.; Solís-Herruzo, J.A.; Mihalik, K.; Tilton, J.C.; et al. Gefitinib, an EGFR inhibitor, prevents hepatocellular carcinoma development in the rat liver with cirrhosis. Hepatology 2005, 41, 307–314. [Google Scholar] [CrossRef]
- Ranson, M. ZD1839 (IressaTM): For More Than Just Non-Small Cell Lung Cancer. Oncology 2002, 7, 16–24. [Google Scholar] [CrossRef]
- Ranson, M.; Hammond, L.A.; Ferry, D.; Kris, M.; Tullo, A.; Murray, P.I.; Miller, V.; Averbuch, S.; Ochs, J.; Morris, C.; et al. ZD1839, a selective oral epidermal growth factor receptor-tyrosine kinase inhibitor, is well tolerated and active in patients with solid, malignant tumors: Results of a phase I trial. J. Clin. Oncol. 2002, 20, 2240–2250. [Google Scholar] [CrossRef]
- Ranson, M.; Mansoor, W.; Jayson, G. ZD1839 (IRESSA): A selective EGFR-TK inhibitor. Expert Rev. Anticancer Ther. 2002, 2, 161–168. [Google Scholar] [CrossRef]
- Giannelli, G.; Azzariti, A.; Fransvea, E.; Porcelli, L.; Antonaci, S.; Paradiso, A. Laminin-5 offsets the efficacy of gefitinib (‘Iressa’) in hepatocellular carcinoma cells. Br. J. Cancer 2004, 91, 1964–1969. [Google Scholar] [CrossRef]
- Cross, D.A.E.; Ashton, S.E.; Ghiorghiu, S.; Eberlein, C.; Nebhan, C.A.; Spitzler, P.J.; Orme, J.P.; Finlay, M.R.V.; Ward, R.A.; Mellor, M.J.; et al. AZD9291, an Irreversible EGFR TKI, Overcomes T790M-Mediated Resistance to EGFR Inhibitors in Lung Cancer. Cancer Discov. 2014, 4, 1046–1061. [Google Scholar] [CrossRef] [PubMed]
- Ercan, D.; Choi, H.G.; Yun, C.-H.; Capelletti, M.; Xie, T.; Eck, M.J.; Gray, N.S.; Jänne, P.A. EGFR mutations and resistance to Irreversible pyrimidine based EGFR inhibitors. Clin. Cancer Res. 2015, 21, 3913–3923. [Google Scholar] [CrossRef] [PubMed]
- Finlay, M.R.V.; Anderton, M.; Ashton, S.; Ballard, P.; Bethel, P.A.; Box, M.R.; Bradbury, R.H.; Brown, S.J.; Butterworth, S.; Campbell, A.; et al. Discovery of a Potent and Selective EGFR Inhibitor (AZD9291) of Both Sensitizing and T790M Resistance Mutations That Spares the Wild Type Form of the Receptor. J. Med. Chem. 2014, 57, 8249–8267. [Google Scholar] [CrossRef]
- Gomes, D.A.; Rodrigues, M.A.; Leite, M.F.; Gomez, M.V.; Varnai, P.; Balla, T.; Bennett, A.M.; Nathanson, M.H. c-Met must translocate to the nucleus to initiate calcium signals. J. Biol. Chem. 2008, 283, 4344–4351. [Google Scholar] [CrossRef]
- Rodrigues, M.A.; Gomes, D.A.; Andrade, V.A.; Leite, M.F.; Nathanson, M.H. Insulin induces calcium signals in the nucleus of rat hepatocytes. Hepatology 2008, 48, 1621–1631. [Google Scholar] [CrossRef]
- Burgstahler, A.D.; Nathanson, M.H. Coordination of calcium waves among hepatocytes: Teamwork gets the job done. Hepatology 1998, 27, 634–635. [Google Scholar] [CrossRef]
- Leite, M.F.; Hirata, K.; Pusl, T.; Burgstahler, A.D.; Okazaki, K.; Ortega, J.M.; Goes, A.M.; Prado, M.A.M.; Spray, D.C.; Nathanson, M.H. Molecular Basis for Pacemaker Cells in Epithelia. J. Biol. Chem. 2002, 277, 16313–16323. [Google Scholar] [CrossRef]
- Nathanson, M.H.; Gautam, A.; Bruck, R.; Isales, C.M.; Boyer, J.L. Effects of Ca2+ agonists on cytosolic Ca2+ in isolated hepatocytes and on bile secretion in the isolated perfused rat liver. Hepatology 1992, 15, 107–116. [Google Scholar] [CrossRef]
- Blackmore, P.F.; Strickland, W.G.; Bocckino, S.B.; Exton, J.H. Mechanism of hepatic glycogen synthase inactivation induced by Ca2+-mobilizing hormones. Studies using phospholipase C and phorbol myristate acetate. Biochem. J. 1986, 237, 235–242. [Google Scholar] [CrossRef]
- Krebs, E.G. Role of the Cyclic AMP—Dependent Protein Kinase in Signal Transduction. JAMA 1989, 262, 1815. [Google Scholar] [CrossRef]
- Exton, J.H. Mechanisms of hormonal regulation of hepatic glucose metabolism. Diabetes Metab. Rev. 1987, 3, 163–183. [Google Scholar] [CrossRef] [PubMed]
- Groigno, L.; Whitaker, M. An Anaphase Calcium Signal Controls Chromosome Disjunction in Early Sea Urchin Embryos. Cell 1998, 92, 193–204. [Google Scholar] [CrossRef]
- Steinhardt, R.A.; Alderton, J. Intracellular free calcium rise triggers nuclear envelope breakdown in the sea urchin embryo. Nature 1988, 332, 364–366. [Google Scholar] [CrossRef] [PubMed]
- Kahl, C.R.; Means, A.R. Regulation of Cell Cycle Progression by Calcium/Calmodulin-Dependent Pathways. Endocr. Rev. 2003, 24, 719–736. [Google Scholar] [CrossRef] [PubMed]
- Poenie, M.; Alderton, J.; Steinhardt, R.; Tsien, R. Calcium rises abruptly and briefly throughout the cell at the onset of anaphase. Science 1986, 233, 886–889. [Google Scholar] [CrossRef]
- Rasmussen, C.D.; Means, A.R. The Presence of Parvalbumin in a Nonmuscle Cell Line Attenuates Progression through Mitosis. Mol. Endocrinol. 1989, 3, 588–596. [Google Scholar] [CrossRef]
- Roman, R.M.; Bodily, K.O.; Wang, Y.; Raymond, J.R.; Fitz, J.G. Activation of protein kinase C alpha couples cell volume to membrane Cl- permeability in HTC hepatoma and Mz-ChA-1 cholangiocarcinoma cells. Hepatology 1998, 28, 1073–1080. [Google Scholar] [CrossRef]
- Twigg, J.P.R.; Whitaker, M. Translational Control of InsP3-induced chromatin condensation during the early cell-cyc les of sea-urchin embryos. Nature 1988, 332, 366–369. [Google Scholar] [CrossRef]
- Nicou, A.; Serrière, V.; Hilly, M.; Prigent, S.; Combettes, L.; Guillon, G.; Tordjmann, T. Remodelling of calcium signalling during liver regeneration in the rat. J. Hepatol. 2007, 46, 247–256. [Google Scholar] [CrossRef]
- Mine, T.; Kojima, I.; Ogata, E.; Nakamura, T. Comparison of effects of HGF and EGF on cellular calcium in rat hepatocytes. Biochem. Biophys. Res. Commun. 1991, 181, 1173–1180. [Google Scholar] [CrossRef]
- Tanaka, Y.; Hayashi, N.; Kaneko, A.; Ito, T.; Miyoshi, E.; Sasaki, Y.; Fusamoto, H.; Kamada, T. Epidermal growth factor induces dose-dependent calcium oscillations in single fura-2–loaded Hepatocytes. Hepatology 1992, 16, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Rizzuto, R.B.M.; Murgia, M.; Pozzan, T. Microdomains with high Ca2+ close to IP3-sensitive channels that are sensed by neighboring mitochondria. Science 1993, 262, 744–747. [Google Scholar] [CrossRef] [PubMed]
- Hajnoczky, G.; Robb-Gaspers, L.D.; Seitz, M.B.; Thomas, A.P. Decoding of cytosolic calcium oscillations in the mitochondria. Cell 1995, 82, 415–424. [Google Scholar] [CrossRef]
- Jouaville, L.S.; Ichas, F.; Holmuhamedov, E.L.; Camacho, P.; Lechleiter, J.D. Synchronization of calciumwaves by mitochondrial substrates in Xenopus laevis oocytes. Nature 1995, 377, 438–441. [Google Scholar] [CrossRef] [PubMed]
- Leite, M.F.; Thrower, E.C.; Echevarria, W.; Koulen, P.; Hirata, K.; Bennett, A.M.; Ehrlich, B.E.; Nathanson, M.H. Nuclear and cytosolic calcium are regulated independently. Proc. Natl. Acad. Sci. USA 2003, 100, 2975–2980. [Google Scholar] [CrossRef]
- Oliva-Vilarnau, N.; Hankeova, S.; Vorrink, S.U.; Mkrtchian, S.; Andersson, E.R.; Lauschke, V.M. Calcium Signaling in Liver Injury and Regeneration. Front. Med. 2018, 5, 192. [Google Scholar] [CrossRef]
- Barbieri, M. Epidermal Growth Factor and Membrane Trafficking: EGF Receptor Activation of Endocytosis Requires Rab5a. J. Cell Biol. 2000, 151, 539–550. [Google Scholar] [CrossRef]
- Burke, P.; Schooler, K.; Wiley, H.S. Regulation of Epidermal Growth Factor Receptor Signaling by Endocytosis and Intracellular Trafficking. Mol. Biol. Cell 2001, 12, 1897–1910. [Google Scholar] [CrossRef]
- Er, E.E.; Mendoza, M.C.; Mackey, A.M.; Rameh, L.E.; Blenis, J. AKT facilitates EGFR trafficking and degradation by phosphorylating and activating PIKfyve. Sci. Signal. 2013, 6, ra45. [Google Scholar] [CrossRef]
- Nishimura, Y.; Yoshioka, K.; Bereczky, B.; Itoh, K. Evidence for efficient phosphorylation of EGFR and rapid endocytosis of phosphorylated EGFR via the early/late endocytic pathway in a gefitinib-sensitive non-small cell lung cancer cell line. Mol. Cancer 2008, 7, 42. [Google Scholar] [CrossRef]
- Roepstorff, K.; Grandal, M.V.; Henriksen, L.; Knudsen, S.L.J.; Lerdrup, M.; Grøvdal, L.; Willumsen, B.M.; Van Deurs, B. Differential Effects of EGFR Ligands on Endocytic Sorting of the Receptor. Traffic 2009, 10, 1115–1127. [Google Scholar] [CrossRef] [PubMed]
- Martina, J.A.; Lelouvier, B.; Puertollano, R. The calcium channel mucolipin-3 is a novel regulator of trafficking along the endosomal pathway. Traffic 2009, 10, 1143–1156. [Google Scholar] [CrossRef] [PubMed]
- Vieira, A.V.; Lamaze, C.; Schmid, S.L. Control of EGF Receptor Signaling by Clathrin-Mediated Endocytosis. Science 1996, 274, 2086–2089. [Google Scholar] [CrossRef] [PubMed]
- Jo, U.; Park, K.H.; Whang, Y.M.; Sung, J.S.; Won, N.H.; Park, J.K.; Kim, Y.H. EGFR endocytosis is a novel therapeutic target in lung cancer with wild-type EGFR. Oncotarget 2014, 5, 1265–1278. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Hirata, A.; Kometani, T.; Miyagawa, M.; Ueda, S.-I.; Kinoshita, H.; Fujii, T.; Kuwano, M. Sensitivity to gefitinib (Iressa, ZD1839) in non-small cell lung cancer cell lines correlates with dependence on the epidermal growth factor (EGF) receptor/extracellular signal-regulated kinase 1/2 and EGF receptor/Akt pathway for proliferation. Mol. Cancer Ther. 2004, 3, 465–472. [Google Scholar]
- He, F.; Liu, W.; Zheng, S.; Zhou, L.; Ye, B.; Qi, Z. Ion transport through dimethyl sulfoxide (DMSO) induced transient water pores in cell membranes. Mol. Membr. Biol. 2012, 29, 107–113. [Google Scholar] [CrossRef]
- Modica, T.M.E.; Maiorani, O.; Sartori, G.; Pivetta, E.; Doliana, R.; Capuano, A.; Colombatti, A.; Spessotto, P. The extracellular matrix protein EMILIN1 silences the RAS-ERK pathway via alpha4beta1 integrin and decreases tumor cell growth. Oncotarget 2017, 8, 27034–27046. [Google Scholar] [CrossRef]
- Morley, P.; Whitfield, J.F. The differentiation inducer, dimethyl sulfoxide, transiently increases the intracellular calcium ion concentration in various cell types. J. Cell. Physiol. 1993, 156, 219–225. [Google Scholar] [CrossRef]
- Neely, A.; Hidalgo, P. Structure-function of proteins interacting with the alpha1 pore-forming subunit of high-voltage-activated calcium channels. Front. Physiol. 2014, 5, 209. [Google Scholar] [CrossRef]
- Notman, R.; Noro, M.; O’Malley, B.; Anwar, J. Molecular Basis for Dimethylsulfoxide (DMSO) Action on Lipid Membranes. J. Am. Chem. Soc. 2006, 128, 13982–13983. [Google Scholar] [CrossRef]
- Jiang, L.; Yan, Q.; Fang, S.; Liu, M.; Yuan, Y.-F.; Li, Y.; Zhu, Y.; Qi, J.; Yang, X.; Kwong, D.L.W.; et al. Calcium-binding protein 39 promotes hepatocellular carcinoma growth and metastasis by activating extracellular signal-regulated kinase signaling pathway. Hepatology 2017, 66, 1529–1545. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, S.; Lu, F.; Zhang, T.; Chen, H.; Wu, S.; Zhuang, H. A role of functional T-type Ca2+ channel in hepatocellular carcinoma cell proliferation. Oncol. Rep. 2009, 22, 1229–1235. [Google Scholar] [PubMed]
- Matsui, T.; Li, L.; Del Monte, F.; Fukui, Y.; Franke, T.F.; Hajjar, R.J.; Rosenzweig, A. Adenoviral Gene Transfer of Activated Phosphatidylinositol 3′-Kinase and Akt Inhibits Apoptosis of Hypoxic Cardiomyocytes In Vitro. Circulation 1999, 100, 2373–2379. [Google Scholar] [CrossRef] [PubMed]
- Franke, T.F.; Hornik, C.P.; Segev, L.; A Shostak, G.; Sugimoto, C. PI3K/Akt and apoptosis: Size matters. Oncogene 2003, 22, 8983–8998. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.; Liang, C.; Chen, E.; Chen, W.; Liang, F.; Zhi, X.; Wei, T.; Xue, F.; Li, G.; Yang, Q.; et al. Regulation of Multi-drug Resistance in hepatocellular carcinoma cells is TRPC6/Calcium Dependent. Sci. Rep. 2016, 6, 23269. [Google Scholar] [CrossRef] [PubMed]
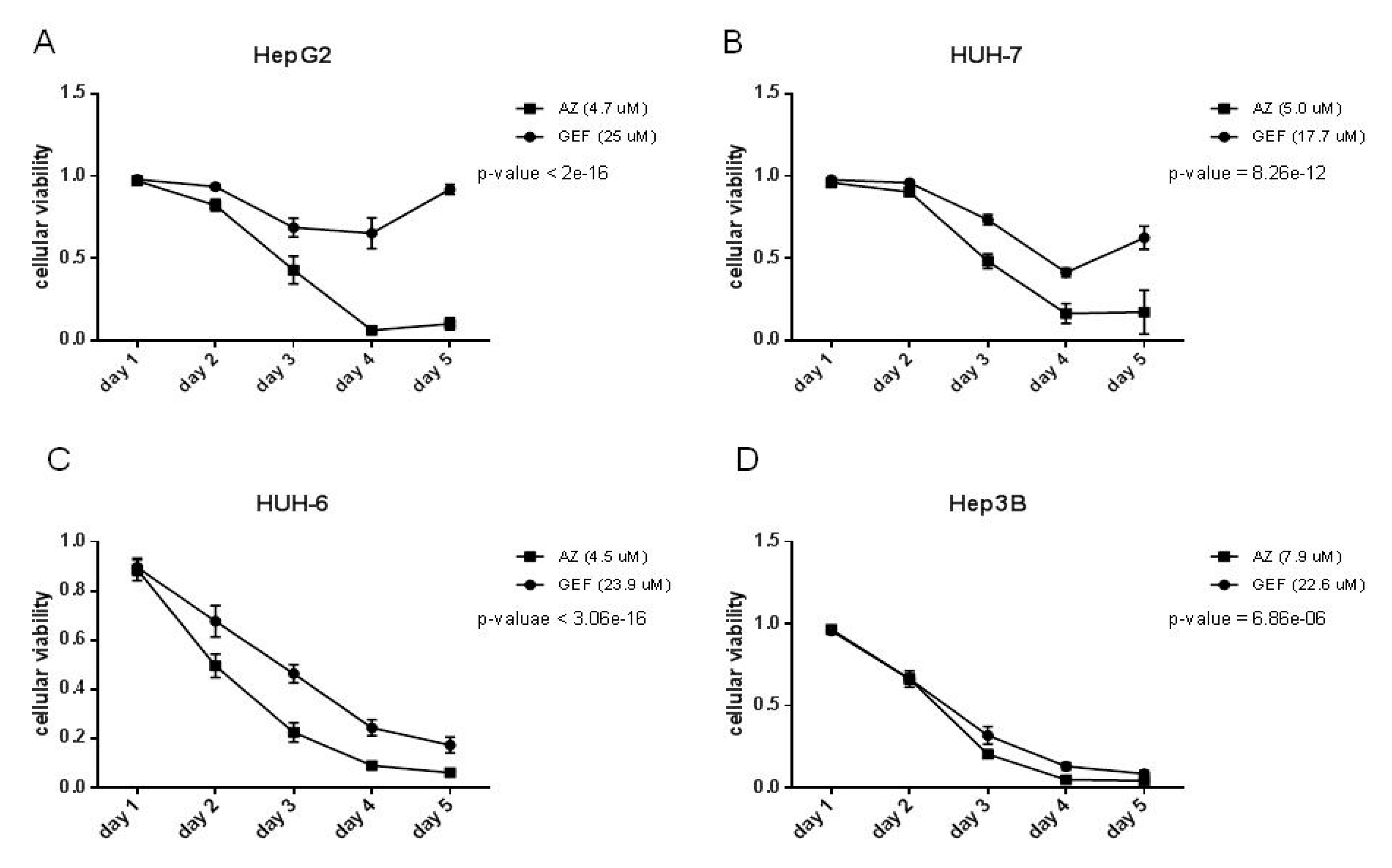



| Cell Line | GEF (µM) | AZ (µM) |
|---|---|---|
| HepG2 | >25 | 4.7 ± 0.2 |
| HUH-7 | 17.7 ± 1.6 | 5.0 ± 0.1 |
| HUH-6 | 23.9 ± 0.3 | 4.5 ± 0.1 |
| Hep3B | 22.6 ± 0.07 | 7.9 ± 0.2 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Modica, T.M.E.; Dituri, F.; Mancarella, S.; Pisano, C.; Fabregat, I.; Giannelli, G. Calcium Regulates HCC Proliferation as well as EGFR Recycling/Degradation and Could Be a New Therapeutic Target in HCC. Cancers 2019, 11, 1588. https://doi.org/10.3390/cancers11101588
Modica TME, Dituri F, Mancarella S, Pisano C, Fabregat I, Giannelli G. Calcium Regulates HCC Proliferation as well as EGFR Recycling/Degradation and Could Be a New Therapeutic Target in HCC. Cancers. 2019; 11(10):1588. https://doi.org/10.3390/cancers11101588
Chicago/Turabian StyleModica, Teresa Maria Elisa, Francesco Dituri, Serena Mancarella, Claudio Pisano, Isabel Fabregat, and Gianluigi Giannelli. 2019. "Calcium Regulates HCC Proliferation as well as EGFR Recycling/Degradation and Could Be a New Therapeutic Target in HCC" Cancers 11, no. 10: 1588. https://doi.org/10.3390/cancers11101588
APA StyleModica, T. M. E., Dituri, F., Mancarella, S., Pisano, C., Fabregat, I., & Giannelli, G. (2019). Calcium Regulates HCC Proliferation as well as EGFR Recycling/Degradation and Could Be a New Therapeutic Target in HCC. Cancers, 11(10), 1588. https://doi.org/10.3390/cancers11101588








