Increased Expression and Activation of FAK in Small-Cell Lung Cancer Compared to Non-Small-Cell Lung Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Tissues Samples
2.2. Multiplex Immunofluorescence Immunohistochemistry (mIF-IHC)
2.3. Stained Slides Imaging
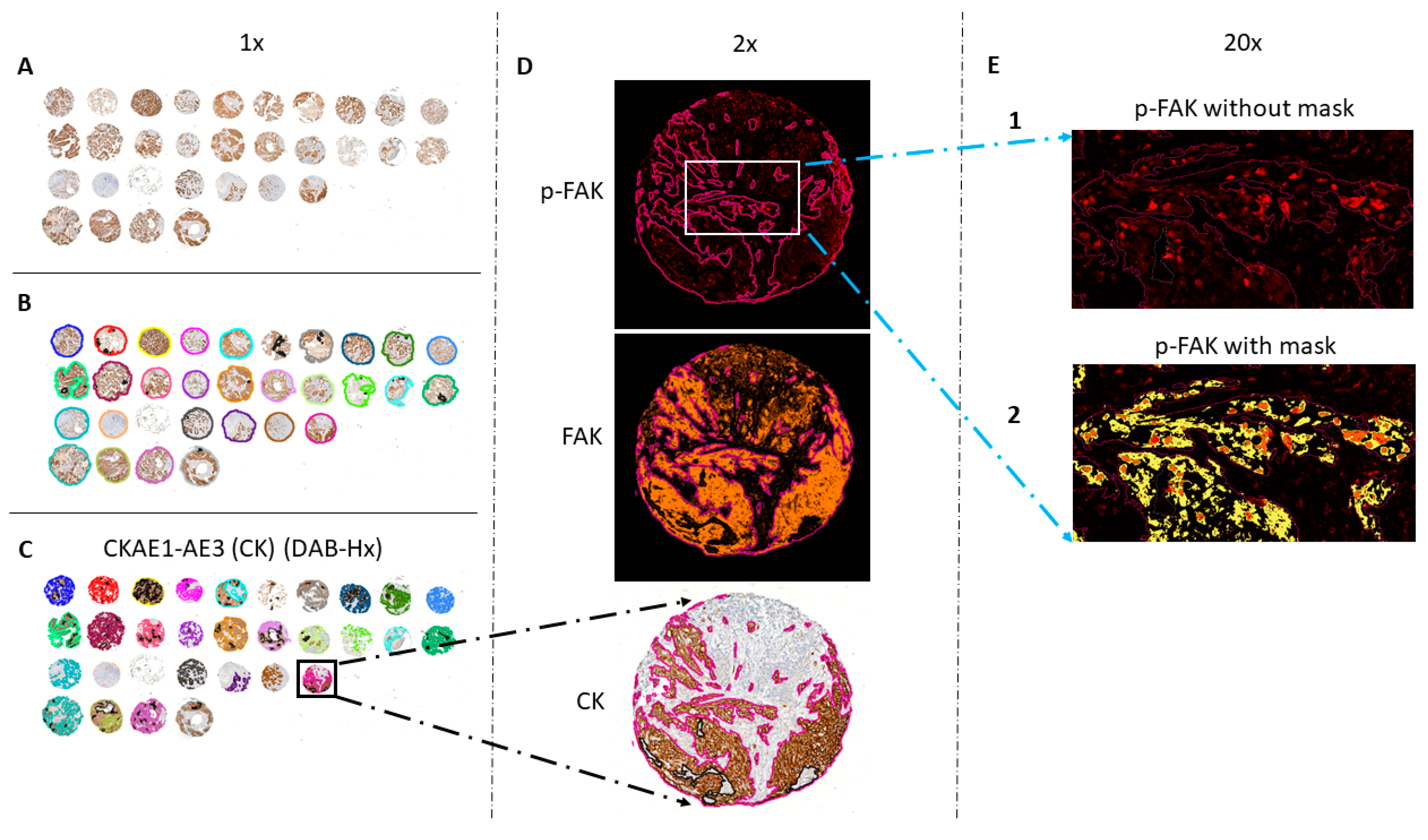
2.4. Quantitative Evaluation of Immunostaining
2.5. Western Blot
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
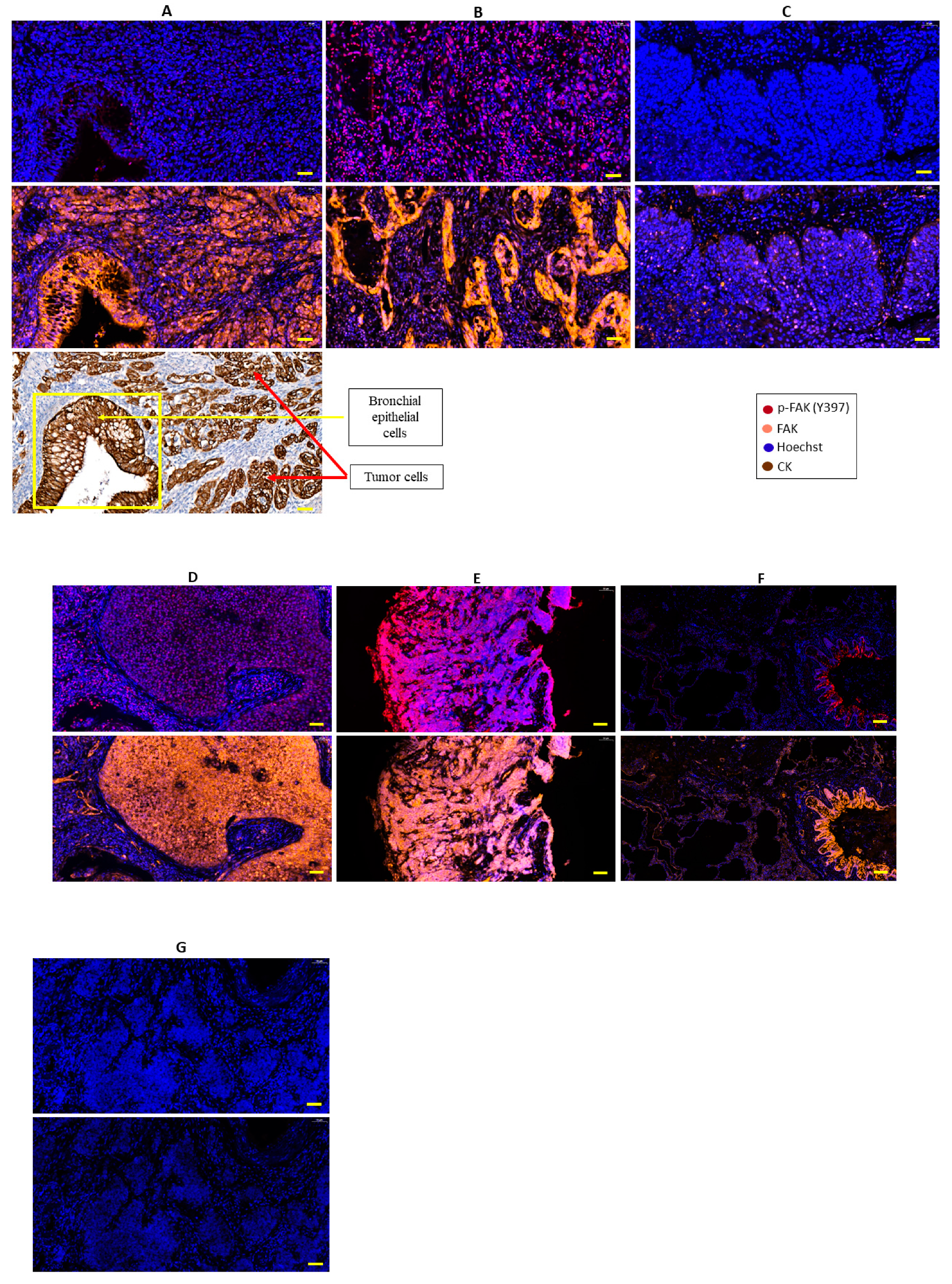
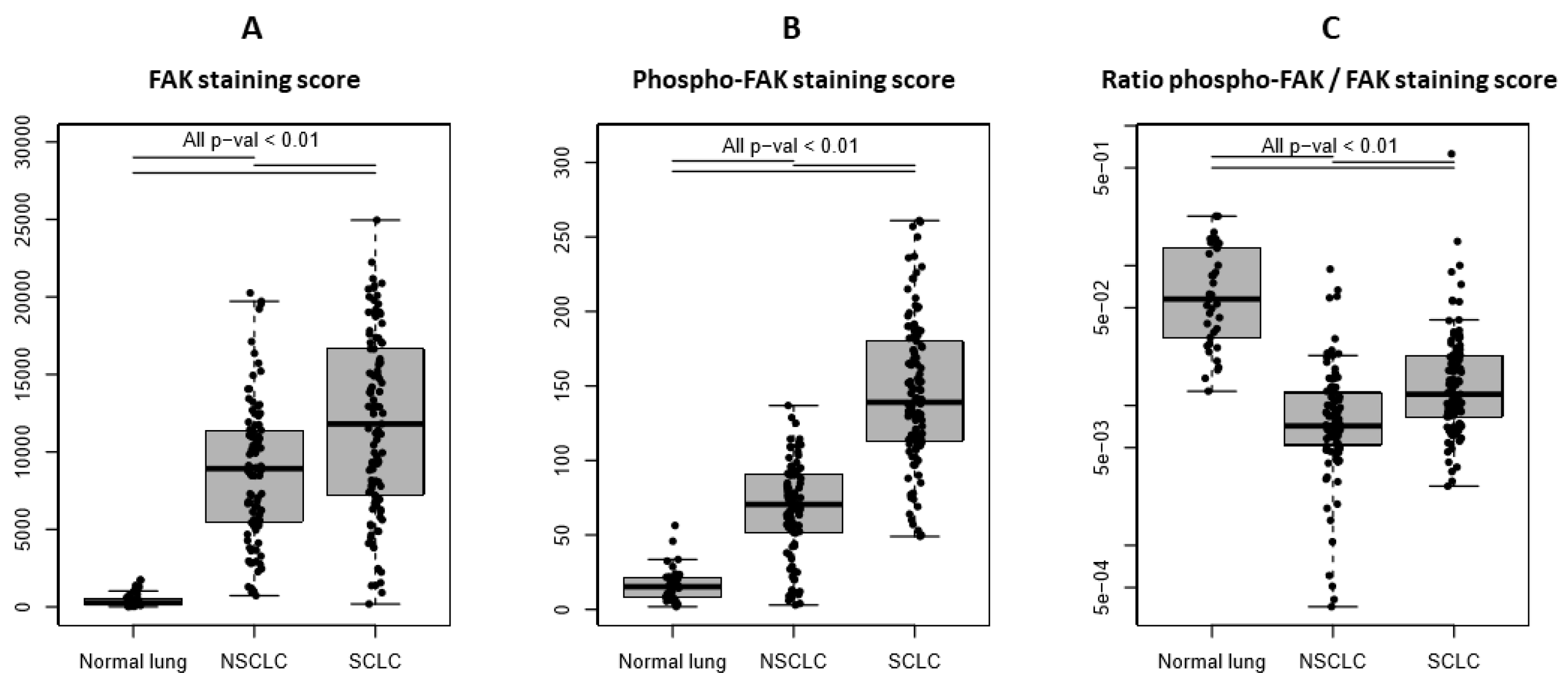
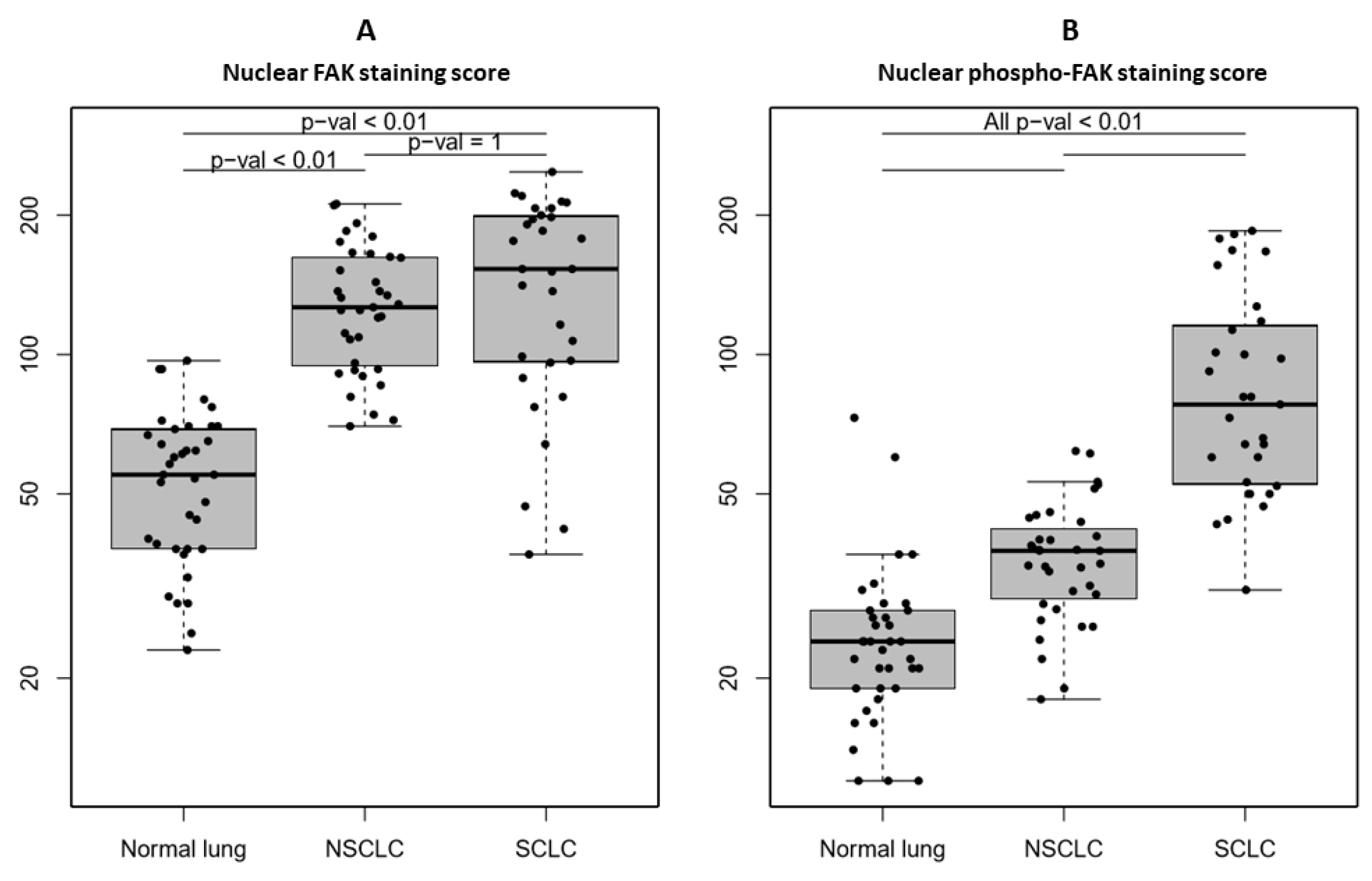
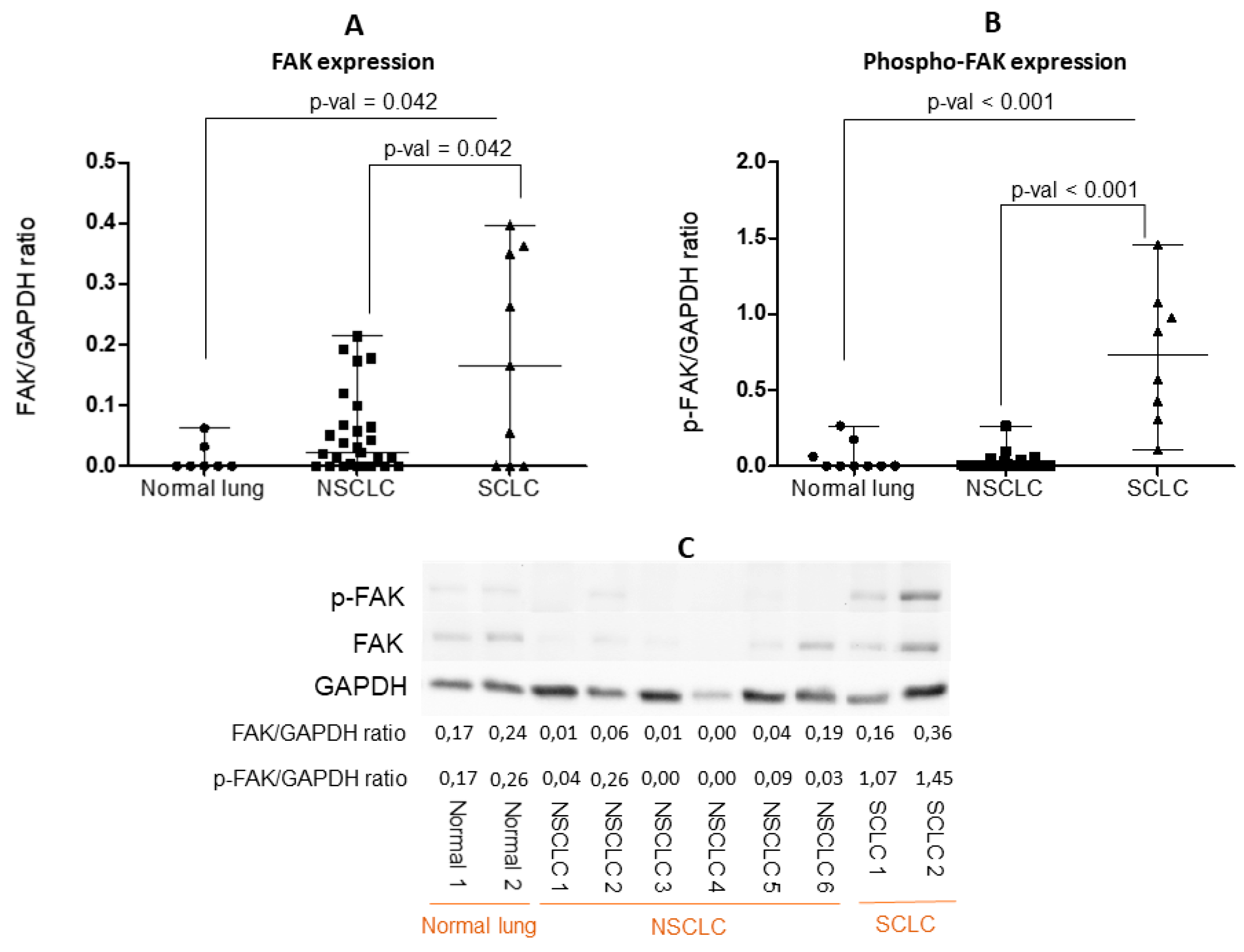
3.2. FAK Expression and Activity Are Higher in SCLC than NSCLC and Normal Lung
3.3. FAK Expression and Activity Do Not Correlate with Patient Characteristics or Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Houston, K.A.; Henley, S.J.; Li, J.; White, M.C.; Richards, T.B. Patterns in lung cancer incidence rates and trends by histologic type in the United States, 2004–2009. Lung Cancer 2014, 86, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Govindan, R.; Page, N.; Morgensztern, D.; Read, W.; Tierney, R.; Vlahiotis, A.; Spitznagel, E.L.; Piccirillo, J. Changing Epidemiology of Small-Cell Lung Cancer in the United States Over the Last 30 Years: Analysis of the Surveillance, Epidemiologic, and End Results Database. J. Clin. Oncol. 2006, 24, 4539–4544. [Google Scholar] [CrossRef] [PubMed]
- Recondo, G.; Facchinetti, F.; Olaussen, K.A.; Besse, B.; Friboulet, L. Making the first move in EGFR-driven or ALK-driven NSCLC: First-generation or next-generation TKI? Nat. Rev. Clin. Oncol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Garon, E.B.; Hellmann, M.D.; Rizvi, N.A.; Carcereny, E.; Leighl, N.B.; Ahn, M.-J.; Eder, J.P.; Balmanoukian, A.S.; Aggarwal, C.; Horn, L.; et al. Five-Year Overall Survival for Patients with Advanced Non‒Small-Cell Lung Cancer Treated with Pembrolizumab: Results from the Phase I KEYNOTE-001 Study. J. Clin. Oncol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://seer.cancer.gov/statfacts/html/lungb.html (accessed on 29 July 2019).
- Horn, L.; Mansfield, A.S.; Szczęsna, A.; Havel, L.; Krzakowski, M.; Hochmair, M.J.; Huemer, F.; Losonczy, G.; Johnson, M.L.; Nishio, M.; et al. First-Line Atezolizumab plus Chemotherapy in Extensive-Stage Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2220–2229. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Ruest, P.J.; Hanks, S.K. FAK regulates tyrosine phosphorylation of CAS, paxillin, and PYK2 in cells expressing v-Src, but is not a critical determinant of v-Src transformation. J. Cell. Biochem. 2002, 84, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.T. Focal adhesion kinase: The first ten years. J. Cell Sci. 2003, 116, 1409–1416. [Google Scholar] [CrossRef]
- Hanks, S.K.; Ryzhova, L.; Shin, N.Y.; Brabek, J. Focal adhesion kinase signaling activities and their implications in the control of cell survival and motility. Front. Biosci. A J. Virtual Libr. 2003, 8, d982–d996. [Google Scholar] [CrossRef]
- Mitra, S.K.; Hanson, D.A.; Schlaepfer, D.D. Focal adhesion kinase: In command and control of cell motility. Nat. Rev. Mol. Cell Biol. 2005, 6, 56–68. [Google Scholar] [CrossRef]
- Siesser, P.M.; Hanks, S.K. The signaling and biological implications of FAK overexpression in cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2006, 12, 3233–3237. [Google Scholar] [CrossRef]
- Gu, H.J.; Zhou, B. Focal adhesion kinase promotes progression and predicts poor clinical outcomes in patients with osteosarcoma. Oncol. Lett. 2018, 15, 6225–6232. [Google Scholar] [CrossRef] [PubMed]
- Almstedt, K.; Sicking, I.; Battista, M.J.; Huangfu, S.; Heimes, A.S.; Weyer-Elberich, V.; Hasenburg, A.; Schmidt, M. Prognostic Significance of Focal Adhesion Kinase in Node-Negative Breast Cancer. Breast Care 2017, 12, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Omura, G.; Ando, M.; Saito, Y.; Kobayashi, K.; Yoshida, M.; Ebihara, Y.; Kanaya, K.; Fujimoto, C.; Sakamoto, T.; Kondo, K.; et al. Association of the upregulated expression of focal adhesion kinase with poor prognosis and tumor dissemination in hypopharyngeal cancer. Head Neck 2016, 38, 1164–1169. [Google Scholar] [CrossRef] [PubMed]
- Gomez Del Pulgar, T.; Cebrian, A.; Fernandez-Acenero, M.J.; Borrero-Palacios, A.; Del Puerto-Nevado, L.; Martinez-Useros, J.; Marin-Arango, J.P.; Carames, C.; Vega-Bravo, R.; Rodriguez-Remirez, M.; et al. Focal adhesion kinase: Predictor of tumour response and risk factor for recurrence after neoadjuvant chemoradiation in rectal cancer. J. Cell. Mol. Med. 2016, 20, 1729–1736. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Hong, L.I.; Liao, M.; Guo, G. Expression and clinical significance of focal adhesion kinase and adrenomedullin in epithelial ovarian cancer. Oncol. Lett. 2015, 10, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Stone, R.L.; Baggerly, K.A.; Armaiz-Pena, G.N.; Kang, Y.; Sanguino, A.M.; Thanapprapasr, D.; Dalton, H.J.; Bottsford-Miller, J.; Zand, B.; Akbani, R.; et al. Focal adhesion kinase: An alternative focus for anti-angiogenesis therapy in ovarian cancer. Cancer Biol. Ther. 2014, 15, 919–929. [Google Scholar] [CrossRef][Green Version]
- Golubovskaya, V.M.; Ylagan, L.; Miller, A.; Hughes, M.; Wilson, J.; Wang, D.; Brese, E.; Bshara, W.; Edge, S.; Morrison, C.; et al. High focal adhesion kinase expression in breast carcinoma is associated with lymphovascular invasion and triple-negative phenotype. BMC Cancer 2014, 14, 769. [Google Scholar] [CrossRef]
- Ji, H.F.; Pang, D.; Fu, S.B.; Jin, Y.; Yao, L.; Qi, J.P.; Bai, J. Overexpression of focal adhesion kinase correlates with increased lymph node metastasis and poor prognosis in non-small-cell lung cancer. J. Cancer Res. Clin. Oncol. 2013, 139, 429–435. [Google Scholar] [CrossRef]
- de Vicente, J.C.; Rosado, P.; Lequerica-Fernandez, P.; Allonca, E.; Villallain, L.; Hernandez-Vallejo, G. Focal adhesion kinase overexpression: Correlation with lymph node metastasis and shorter survival in oral squamous cell carcinoma. Head Neck 2013, 35, 826–830. [Google Scholar] [CrossRef]
- Yuan, Z.; Zheng, Q.; Fan, J.; Ai, K.X.; Chen, J.; Huang, X.Y. Expression and prognostic significance of focal adhesion kinase in hepatocellular carcinoma. J. Cancer Res. Clin. Oncol. 2010, 136, 1489–1496. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, B.L.; Yoon, J.; Kim, J.; Kim, M.A.; Yang, H.K.; Kim, W.H. Focal adhesion kinase (FAK) gene amplification and its clinical implications in gastric cancer. Hum. Pathol. 2010, 41, 1664–1673. [Google Scholar] [CrossRef] [PubMed]
- Lark, A.L.; Livasy, C.A.; Dressler, L.; Moore, D.T.; Millikan, R.C.; Geradts, J.; Iacocca, M.; Cowan, D.; Little, D.; Craven, R.J.; et al. High focal adhesion kinase expression in invasive breast carcinomas is associated with an aggressive phenotype. Mod. Pathol. 2005, 18, 1289–1294. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Wang, G.-Z.; Zhou, G.-B.; Wen, Z.-S.; Zhou, Y.-C.; Huang, Y.-C.; Chen, Y. Somatic Mutations and Splicing Variants of Focal Adhesion Kinase in Non–Small Cell Lung Cancer. JNCI J. Natl. Cancer Inst. 2017, 110, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Aboubakar Nana, F.; Lecocq, M.; Ladjemi, M.Z.; Detry, B.; Dupasquier, S.; Feron, O.; Massion, P.P.; Sibille, Y.; Pilette, C.; Ocak, S. Therapeutic potential of Focal Adhesion Kinase inhibition in small cell lung cancer. Mol. Cancer Ther. 2019, 18, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Shao, H.; Golubovskaya, V.M.; Chen, H.; Cance, W.; Adjei, A.A.; Dy, G.K. Efficacy of focal adhesion kinase inhibition in non-small cell lung cancer with oncogenically activated MAPK pathways. Br. J. Cancer 2016, 115, 203. [Google Scholar] [CrossRef] [PubMed]
- Roberts, W.G.; Ung, E.; Whalen, P.; Cooper, B.; Hulford, C.; Autry, C.; Richter, D.; Emerson, E.; Lin, J.; Kath, J.; et al. Antitumor Activity and Pharmacology of a Selective Focal Adhesion Kinase Inhibitor, PF-562,271. Cancer Res. 2008, 68, 1935–1944. [Google Scholar] [CrossRef]
- Infante, J.R.; Camidge, D.R.; Mileshkin, L.R.; Chen, E.X.; Hicks, R.J.; Rischin, D.; Fingert, H.; Pierce, K.J.; Xu, H.; Roberts, W.G.; et al. Safety, pharmacokinetic, and pharmacodynamic phase I dose-escalation trial of PF-00562271, an inhibitor of focal adhesion kinase, in advanced solid tumors. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2012, 30, 1527–1533. [Google Scholar] [CrossRef]
- Jones, S.F.; Siu, L.L.; Bendell, J.C.; Cleary, J.M.; Razak, A.R.; Infante, J.R.; Pandya, S.S.; Bedard, P.L.; Pierce, K.J.; Houk, B.; et al. A phase I study of VS-6063, a second-generation focal adhesion kinase inhibitor, in patients with advanced solid tumors. Investig. New Drugs 2015, 33, 1100–1107. [Google Scholar] [CrossRef]
- Shimizu, T.; Fukuoka, K.; Takeda, M.; Iwasa, T.; Yoshida, T.; Horobin, J.; Keegan, M.; Vaickus, L.; Chavan, A.; Padval, M.; et al. A first-in-Asian phase 1 study to evaluate safety, pharmacokinetics and clinical activity of VS-6063, a focal adhesion kinase (FAK) inhibitor in Japanese patients with advanced solid tumors. Cancer Chemother. Pharmacol. 2016, 77, 997–1003. [Google Scholar] [CrossRef]
- Constanzo, J.D.; Tang, K.-J.; Rindhe, S.; Melegari, M.; Liu, H.; Tang, X.; Rodriguez-Canales, J.; Wistuba, I.; Scaglioni, P.P. PIAS1-FAK Interaction Promotes the Survival and Progression of Non-Small Cell Lung Cancer. Neoplasia 2016, 18, 282–293. [Google Scholar] [CrossRef]
- Ocak, S.; Yamashita, H.; Udyavar, A.R.; Miller, A.N.; Gonzalez, A.L.; Zou, Y.; Jiang, A.; Yi, Y.; Shyr, Y.; Estrada, L.; et al. DNA copy number aberrations in small-cell lung cancer reveal activation of the focal adhesion pathway. Oncogene 2010, 29, 6331–6342. [Google Scholar] [CrossRef] [PubMed]
- Ocak, S.; Chen, H.; Callison, C.; Gonzalez, A.L.; Massion, P.P. Expression of focal adhesion kinase in small-cell lung carcinoma. Cancer 2012, 118, 1293–1301. [Google Scholar] [CrossRef] [PubMed]
- Dy, G.K.; Ylagan, L.; Pokharel, S.; Miller, A.; Brese, E.; Bshara, W.; Morrison, C.; Cance, W.G.; Golubovskaya, V.M. The Prognostic Significance of Focal Adhesion Kinase Expression in Stage I Non–Small-Cell Lung Cancer. J. Thorac. Oncol. 2014, 9, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Kononen, J.; Bubendorf, L.; Kallionimeni, A.; Bärlund, M.; Schraml, P.; Leighton, S.; Torhorst, J.; Mihatsch, M.J.; Sauter, G.; Kallionimeni, O.-P. Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat. Med. 1998, 4, 844–847. [Google Scholar] [CrossRef] [PubMed]
- Massion, P.P.; Kuo, W.-L.; Stokoe, D.; Olshen, A.B.; Treseler, P.A.; Chin, K.; Chen, C.; Polikoff, D.; Jain, A.N.; Pinkel, D.; et al. Genomic Copy Number Analysis of Non-small Cell Lung Cancer Using Array Comparative Genomic Hybridization. Implic. Phosphatidylinositol 3-Kinase Pathw. 2002, 62, 3636–3640. [Google Scholar]
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef]
- Detterbeck, F.C.; Boffa, D.J.; Kim, A.W.; Tanoue, L.T. The Eighth Edition Lung Cancer Stage Classification. CHEST 2017, 151, 193–203. [Google Scholar] [CrossRef]
- Tang, K.-J.; Constanzo, J.D.; Venkateswaran, N.; Melegari, M.; Ilcheva, M.; Morales, J.C.; Skoulidis, F.; Heymach, J.V.; Boothman, D.A.; Scaglioni, P.P. Focal Adhesion Kinase Regulates the DNA Damage Response and Its Inhibition Radiosensitizes Mutant KRAS Lung Cancer. Clin. Cancer Res. 2016, 22, 5851–5863. [Google Scholar] [CrossRef]
- Jiang, H.; Hegde, S.; Knolhoff, B.L.; Zhu, Y.; Herndon, J.M.; Meyer, M.A.; Nywening, T.M.; Hawkins, W.G.; Shapiro, I.M.; Weaver, D.T.; et al. Targeting focal adhesion kinase renders pancreatic cancers responsive to checkpoint immunotherapy. Nat. Med. 2016, 22, 851. [Google Scholar] [CrossRef]
- Haemmerle, M.; Bottsford-Miller, J.; Pradeep, S.; Taylor, M.L.; Choi, H.J.; Hansen, J.M.; Dalton, H.J.; Stone, R.L.; Cho, M.S.; Nick, A.M.; et al. FAK regulates platelet extravasation and tumor growth after antiangiogenic therapy withdrawal. J. Clin. Investig. 2016, 126, 1885–1896. [Google Scholar] [CrossRef]
- Owens, L.V.; Xu, L.; Craven, R.J.; Dent, G.A.; Weiner, T.M.; Kornberg, L.; Liu, E.T.; Cance, W.G. Overexpression of the focal adhesion kinase (p125FAK) in invasive human tumors. Cancer Res. 1995, 55, 2752–2755. [Google Scholar] [PubMed]
- Carelli, S.; Zadra, G.; Vaira, V.; Falleni, M.; Bottiglieri, L.; Nosotti, M.; Di Giulio, A.M.; Gorio, A.; Bosari, S. Up-regulation of focal adhesion kinase in non-small cell lung cancer. Lung Cancer 2006, 53, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yang, R.; Yue, D.; Zhang, Z. Expression of FAK and PTEN in Bronchioloalveolar Carcinoma and Lung Adenocarcinoma. Lung 2009, 187, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Imaizumi, M.; Nishimura, M.; Takeuchi, S.; Murase, M.; Hamaguchi, M. Role of tyrosine specific phosphorylation of cellular proteins, especially EGF receptor and p125FAK in human lung cancer cells. Lung Cancer 1997, 17, 69–84. [Google Scholar] [CrossRef]
- Hsu, N.Y.; Chen, C.Y.; Hsu, C.P.; Lin, T.Y.; Chou, M.C.; Chiou, S.H.; Chow, K.C. Prognostic significance of expression of nm23-H1 and focal adhesion kinase in non-small cell lung cancer. Oncol. Rep. 2007, 18, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Itoh, S.; Maeda, T.; Shimada, M.; Aishima, S.; Shirabe, K.; Tanaka, S.; Maehara, Y. Role of expression of focal adhesion kinase in progression of hepatocellular carcinoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2004, 10, 2812–2817. [Google Scholar] [CrossRef]
- Thanapprapasr, K.; Nartthanarung, A.; Thanapprapasr, D.; Jinawath, A. pFAK-Y397 overexpression as both a prognostic and a predictive biomarker for patients with metastatic osteosarcoma. PLoS ONE 2017, 12, e0182989. [Google Scholar] [CrossRef]
- Schlaepfer, D.D.; Hauck, C.R.; Sieg, D.J. Signaling through focal adhesion kinase. Prog. Biophys. Mol. Biol. 1999, 71, 435–478. [Google Scholar] [CrossRef]
- Kleinschmidt, E.G.; Schlaepfer, D.D. Focal adhesion kinase signaling in unexpected places. Curr. Opin. Cell Biol. 2017, 45, 24–30. [Google Scholar] [CrossRef]
- Damstrup, L.; Rygaard, K.; Spang-Thomsen, M.; Skovgaard Poulsen, H. Expression of transforming growth factor beta (TGF beta) receptors and expression of TGF beta 1, TGF beta 2 and TGF beta 3 in human small cell lung cancer cell lines. Br. J. Cancer 1993, 67, 1015–1021. [Google Scholar] [CrossRef]
- Dowell, J.E.; Amirkhan, R.H.; Lai, W.S.; Frawley, W.H.; Minna, J.D. Survival in small cell lung cancer is independent of tumor expression of VEGF and COX-2. Anticancer Res. 2004, 24, 2367–2373. [Google Scholar] [PubMed]
- Ma, P.C.; Tretiakova, M.S.; Nallasura, V.; Jagadeeswaran, R.; Husain, A.N.; Salgia, R. Downstream signalling and specific inhibition of c-MET/HGF pathway in small cell lung cancer: Implications for tumour invasion. Br. J. Cancer 2007, 97, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Yu, H.; Badzio, A.; Boyle, T.A.; Schildhaus, H.-U.; Lu, X.; Dziadziuszko, R.; Jassem, J.; Varella-Garcia, M.; Heasley, L.E.; et al. Fibroblast Growth Factor Receptor 1 and Related Ligands in Small-Cell Lung Cancer. J. Thorac. Oncol. 2015, 10, 1083–1090. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thomas, A.; Lee, J.H.; Abdullaev, Z.; Park, K.S.; Pineda, M.; Saidkhodjaeva, L.; Miettinen, M.; Wang, Y.; Pack, S.D.; Giaccone, G. Characterization of fibroblast growth factor receptor 1 in small-cell lung cancer. J. Thorac. Oncol. 2014, 9, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Lucchi, M.; Mussi, A.; Fontanini, G.; Faviana, P.; Ribechini, A.; Angeletti, C.A. Small cell lung carcinoma (SCLC): The angiogenic phenomenon. Eur. J. Cardio-Thorac. Surg. 2002, 21, 1105–1110. [Google Scholar] [CrossRef]
- Beviglia, L.; Kramer, R.H. HGF induces FAK activation and integrin-mediated adhesion in MTLn3 breast carcinoma cells. Int. J. Cancer. J. Int. Du Cancer 1999, 83, 640–649. [Google Scholar] [CrossRef]
- Rodrı́guez-Fernández, J.L.; Rozengurt, E. Bombesin, Vasopressin, Lysophosphatidic Acid, and Sphingosylphosphorylcholine Induce Focal Adhesion Kinase Activation in Intact Swiss 3T3 Cells. J. Biol. Chem. 1998, 273, 19321–19328. [Google Scholar] [CrossRef]
- Leyton, J.; Garcia-Marin, L.J.; Tapia, J.A.; Jensen, R.T.; Moody, T.W. Bombesin and gastrin releasing peptide increase tyrosine phosphorylation of focal adhesion kinase and paxillin in non-small cell lung cancer cells. Cancer Lett. 2001, 162, 87–95. [Google Scholar] [CrossRef]
- Serrels, A.; McLeod, K.; Canel, M.; Kinnaird, A.; Graham, K.; Frame, M.C.; Brunton, V.G. The role of focal adhesion kinase catalytic activity on the proliferation and migration of squamous cell carcinoma cells. Int. J. Cancer 2012, 131, 287–297. [Google Scholar] [CrossRef]
- Beierle, E.A.; Ma, X.; Stewart, J.; Nyberg, C.; Trujillo, A.; Cance, W.G.; Golubovskaya, V.M. Inhibition of focal adhesion kinase decreases tumor growth in human neuroblastoma. Cell Cycle 2010, 9, 1005–1015. [Google Scholar] [CrossRef]
- Hochwald, S.N.; Nyberg, C.; Zheng, M.; Zheng, D.; Wood, C.; Massoll, N.A.; Magis, A.; Ostrov, D.; Cance, W.G.; Golubovskaya, V.M. A novel small molecule inhibitor of FAK decreases growth of human pancreatic cancer. Cell Cycle 2009, 8, 2435–2443. [Google Scholar] [CrossRef]
- Soria, J.C.; Gan, H.K.; Blagden, S.P.; Plummer, R.; Arkenau, H.T.; Ranson, M.; Evans, T.R.; Zalcman, G.; Bahleda, R.; Hollebecque, A.; et al. A phase I, pharmacokinetic and pharmacodynamic study of GSK2256098, a focal adhesion kinase inhibitor, in patients with advanced solid tumors. Ann. Oncol. 2016, 27, 2268–2274. [Google Scholar] [CrossRef] [PubMed]
- Lai, I.R.; Chu, P.Y.; Lin, H.S.; Liou, J.Y.; Jan, Y.J.; Lee, J.C.; Shen, T.L. Phosphorylation of focal adhesion kinase at Tyr397 in gastric carcinomas and its clinical significance. Am. J. Pathol. 2010, 177, 1629–1637. [Google Scholar] [CrossRef] [PubMed]
- Ren, K.; Lu, X.; Yao, N.; Chen, Y.; Yang, A.; Chen, H.; Zhang, J.; Wu, S.; Shi, X.; Wang, C.; et al. Focal adhesion kinase overexpression and its impact on human osteosarcoma. Oncotarget 2015, 6, 31085–31103. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, M.; Machida, K.; Imaizumi, M.; Abe, T.; Umeda, T.; Takeshima, E.; Watanabe, T.; Ohnishi, Y.; Takagi, K.; Hamaguchi, M. Tyrosine phosphorylation of 100-130 kDa proteins in lung cancer correlates with poor prognosis. Br. J. Cancer 1996, 74, 780–787. [Google Scholar] [CrossRef]
- Wang, B.; Qi, X.; Li, D.; Feng, M.; Meng, X.; Fu, S. Expression of pY397 FAK promotes the development of non-small cell lung cancer. Oncol. Lett. 2016, 11, 979–983. [Google Scholar] [CrossRef]
- Brown, N.F.; Williams, M.; Arkenau, H.T.; Fleming, R.A.; Tolson, J.; Yan, L.; Zhang, J.; Swartz, L.; Singh, R.; Auger, K.R.; et al. A study of the focal adhesion kinase inhibitor GSK2256098 in patients with recurrent glioblastoma with evaluation of tumor penetration of [11C]GSK2256098. Neuro-Oncol. 2018, 20, 1634–1642. [Google Scholar] [CrossRef]
- Serrels, A.; Lund, T.; Serrels, B.; Byron, A.; McPherson, R.C.; von Kriegsheim, A.; Gómez-Cuadrado, L.; Canel, M.; Muir, M.; Ring, J.E.; et al. Nuclear FAK Controls Chemokine Transcription, Tregs, and Evasion of Anti-tumor Immunity. Cell 2015, 163, 160–173. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.T.; Chen, X.L.; Lim, Y.; Hanson, D.A.; Vo, T.T.; Howerton, K.; Larocque, N.; Fisher, S.J.; Schlaepfer, D.D.; Ilic, D. Nuclear FAK promotes cell proliferation and survival through FERM-enhanced p53 degradation. Mol. Cells 2008, 29, 9–22. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.T. Nuclear FAK: A new mode of gene regulation from cellular adhesions. Mol. Cells 2013, 36, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Serrels, B.; McGivern, N.; Canel, M.; Byron, A.; Johnson, S.C.; McSorley, H.J.; Quinn, N.; Taggart, D.; Von Kreigsheim, A.; Anderton, S.M.; et al. IL-33 and ST2 mediate FAK-dependent antitumor immune evasion through transcriptional networks. Sci. Signal. 2017, 10. [Google Scholar] [CrossRef] [PubMed]
| A | |
|---|---|
| Variable | NSCLC Patients (n = 95) |
| Histological subtype | |
| Squamous | 34 (35.8) |
| Non-squamous | 61 (64.2) |
| Stage-n (%) | |
| I | 45 (47.4) |
| II | 23 (24.2) |
| III | 19 (20.0) |
| IV | 8 (8.4) |
| Gender-n (%) | |
| Female | 26 (27.4) |
| Male | 69 (72.6) |
| Age at diagnostic >75 y/o-n (%) | |
| No | 74 (77.9) |
| Yes | 21 (22.1) |
| Smoking history-n (%) | |
| Unknown | 1 (1.1) |
| Never | 4 (4.2) |
| Ex | 57 (60.0) |
| Current | 33 (34.7) |
| Pack per year | |
| Median | 40 |
| Range | 2–107 |
| B | |
| Variable | SCLC Patients (n = 105) |
| Stage-n (%) | |
| ED | 69 (65.7) |
| LD | 21 (20.0) |
| Unknown | 15 (14.3) |
| Gender-n (%) | |
| Female | 38 (36.2) |
| Male | 67 (63.8) |
| Age at diagnostic >75 y/o-n (%) | |
| No | 78 (74.3) |
| Yes | 27 (25.7) |
| Smoking history-n (%) | |
| Unknown | 10 (9.5) |
| Never | 1 (1.0) |
| Ex | 32 (30.5) |
| Current | 62 (59.0) |
| Pack per year | |
| Median | 43 |
| Range | 1–170 |
| C | |
| Variable | Healthy Donors (n = 37) |
| Gender-n (%) | |
| Female | 3 (8.1) |
| Male | 34 (91.9) |
| Age >75 y/o-n (%) | |
| No | 36 (97.3) |
| Yes | 1 (2.7) |
| Agee (year) | |
| Median | 59.5 |
| Range | 19−79 |
| Smoking history-n (%) | |
| Unknown | 19 (51.4) |
| Never | 8 (21.6) |
| Yes | 10 (27.0) |
| A | ||||
|---|---|---|---|---|
| Variable | Recurrence-Free Survival | Overall Survival | ||
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| FAK staining score | 1.00 (1.00–1.00) | 0.92 | 1.00 (1.00–1.00) | 0.99 |
| Phospho-FAK staining score | 0.99 (0.98–1.00) | 0.1 | 0.99 (0.98–1.00) | 0.21 |
| Ratio phospho-FAK/FAK staining scores | 0.86 (0.60–1.23) | 0.33 | 0.89 (0.64–1.21) | 0.4 |
| B | ||||
| Variable | Recurrence-Free Survival | Overall Survival | ||
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| FAK staining score | 1.00 (1.00–1.00) | 0.76 | 1.00 (1.00–1.00) | 0.66 |
| Phospho-FAK staining score | 1.00 (1.00–1.01) | 0.5 | 1.00 (0.99–1.00) | 0.8 |
| 100 × ratio phospho-FAK/FAK staining scores | 0.96 (0.90–1.02) | 0.13 | 1.00 (0.97–1.03) | 0.75 |
| A | ||||
|---|---|---|---|---|
| Variable | Recurrence-Free Survival | Overall Survival | ||
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Stage (ref: I) | ||||
| II | 1.06 (0.35–3.20) | 0.92 | 0.63 (0.19–2.04) | 0.44 |
| III | 1.92 (0.72–5.16) | 0.19 | 2.76 (1.11–6.83) | 0.03 |
| IV | 5.64 (1.79–17.7) | <0.01 | 3.21 (1.06–9.66) | 0.04 |
| Age at diagnostic (ref: <75 y/o) | ||||
| >75 y/o | 1.19 (0.49–3.07) | 0.72 | 0.75 (0.28–2.03) | 0.57 |
| Smoking history (ref: ex and never) | ||||
| Current | 0.82 (0.35–1.89) | 0.64 | 0.88 (0.39–1.96) | 0.75 |
| Histology (ref: ADC) | ||||
| SCC | 0.66 (0.26–1.69) | 0.39 | 1.59 (0.70–3.62) | 0.27 |
| Phospho-FAK staining score | 0.99 (0.98–1.00) | 0.15 | 0.99 (0.98–1.01) | 0.30 |
| B | ||||
| Variable | Recurrence-Free Survival | Overall Survival | ||
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| Stage (ref: LD) | ||||
| ED | 3.75 (2.08–6.78) | <0.01 | 3.47 (1.91–6.32) | <0.01 |
| Age at diagnostic (ref: <75 y/0) | ||||
| >75 y/o | 1.56 (0.93–2.63) | 0.09 | 1.42 (0.88–2.29) | 0.15 |
| Smoking history (ref: ex and never) | ||||
| Current | 1.23 (0.78–1.93) | 0.37 | 1.11 (0.73–1.70) | 0.62 |
| 100 × ratio phospho-FAK/FAK staining scores | 0.95 (0.89–1.02) | 0.14 | 1.00 (0.97–1.03) | 0.87 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aboubakar Nana, F.; Hoton, D.; Ambroise, J.; Lecocq, M.; Vanderputten, M.; Sibille, Y.; Vanaudenaerde, B.; Pilette, C.; Bouzin, C.; Ocak, S. Increased Expression and Activation of FAK in Small-Cell Lung Cancer Compared to Non-Small-Cell Lung Cancer. Cancers 2019, 11, 1526. https://doi.org/10.3390/cancers11101526
Aboubakar Nana F, Hoton D, Ambroise J, Lecocq M, Vanderputten M, Sibille Y, Vanaudenaerde B, Pilette C, Bouzin C, Ocak S. Increased Expression and Activation of FAK in Small-Cell Lung Cancer Compared to Non-Small-Cell Lung Cancer. Cancers. 2019; 11(10):1526. https://doi.org/10.3390/cancers11101526
Chicago/Turabian StyleAboubakar Nana, Frank, Delphine Hoton, Jérôme Ambroise, Marylène Lecocq, Marie Vanderputten, Yves Sibille, Bart Vanaudenaerde, Charles Pilette, Caroline Bouzin, and Sebahat Ocak. 2019. "Increased Expression and Activation of FAK in Small-Cell Lung Cancer Compared to Non-Small-Cell Lung Cancer" Cancers 11, no. 10: 1526. https://doi.org/10.3390/cancers11101526
APA StyleAboubakar Nana, F., Hoton, D., Ambroise, J., Lecocq, M., Vanderputten, M., Sibille, Y., Vanaudenaerde, B., Pilette, C., Bouzin, C., & Ocak, S. (2019). Increased Expression and Activation of FAK in Small-Cell Lung Cancer Compared to Non-Small-Cell Lung Cancer. Cancers, 11(10), 1526. https://doi.org/10.3390/cancers11101526







