Salivary Gland Function, Antioxidant Defence and Oxidative Damage in the Saliva of Patients with Breast Cancer: Does the BRCA1 Mutation Disturb the Salivary Redox Profile?
Abstract
1. Introduction
2. Material and Methods
2.1. Patients
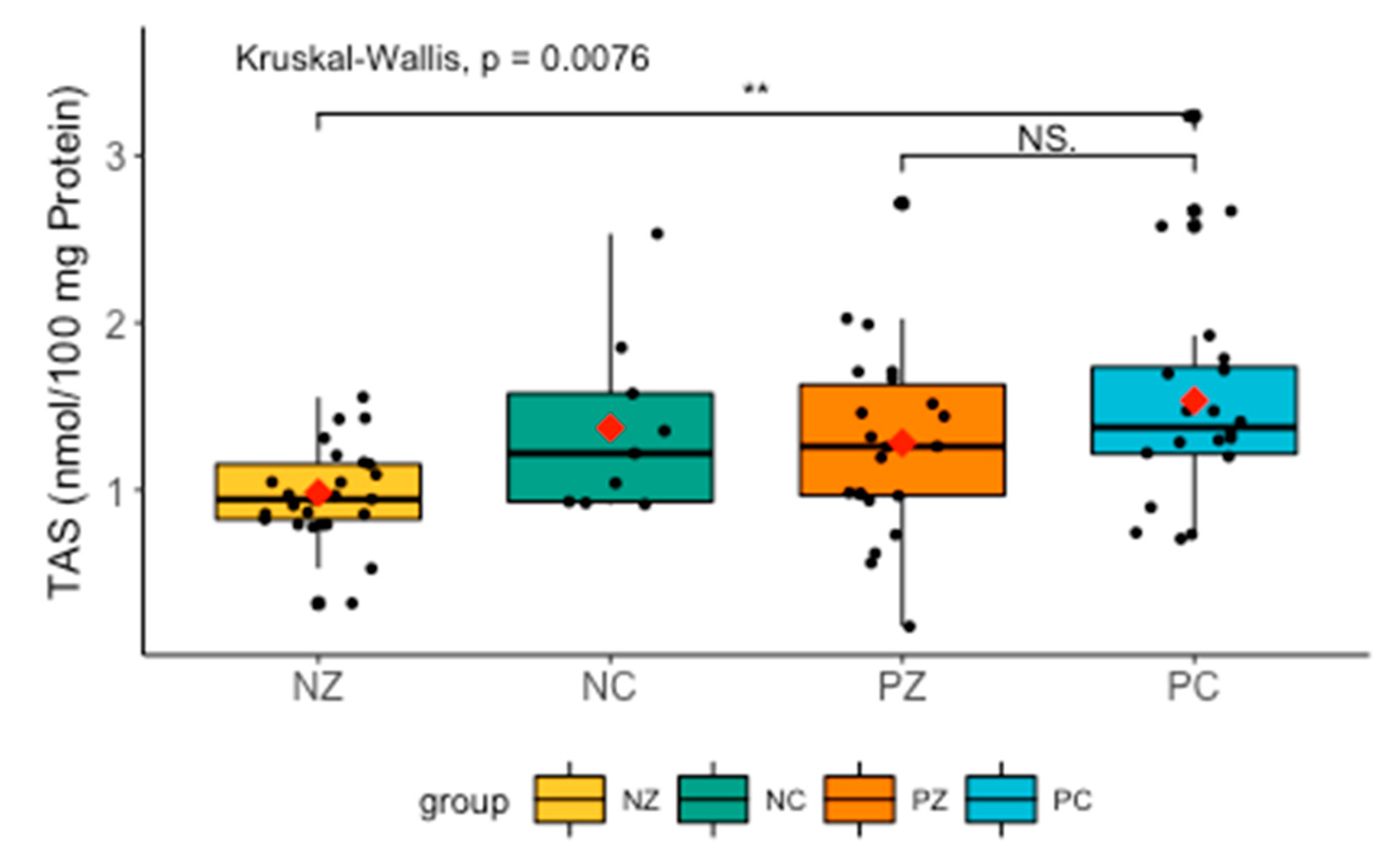
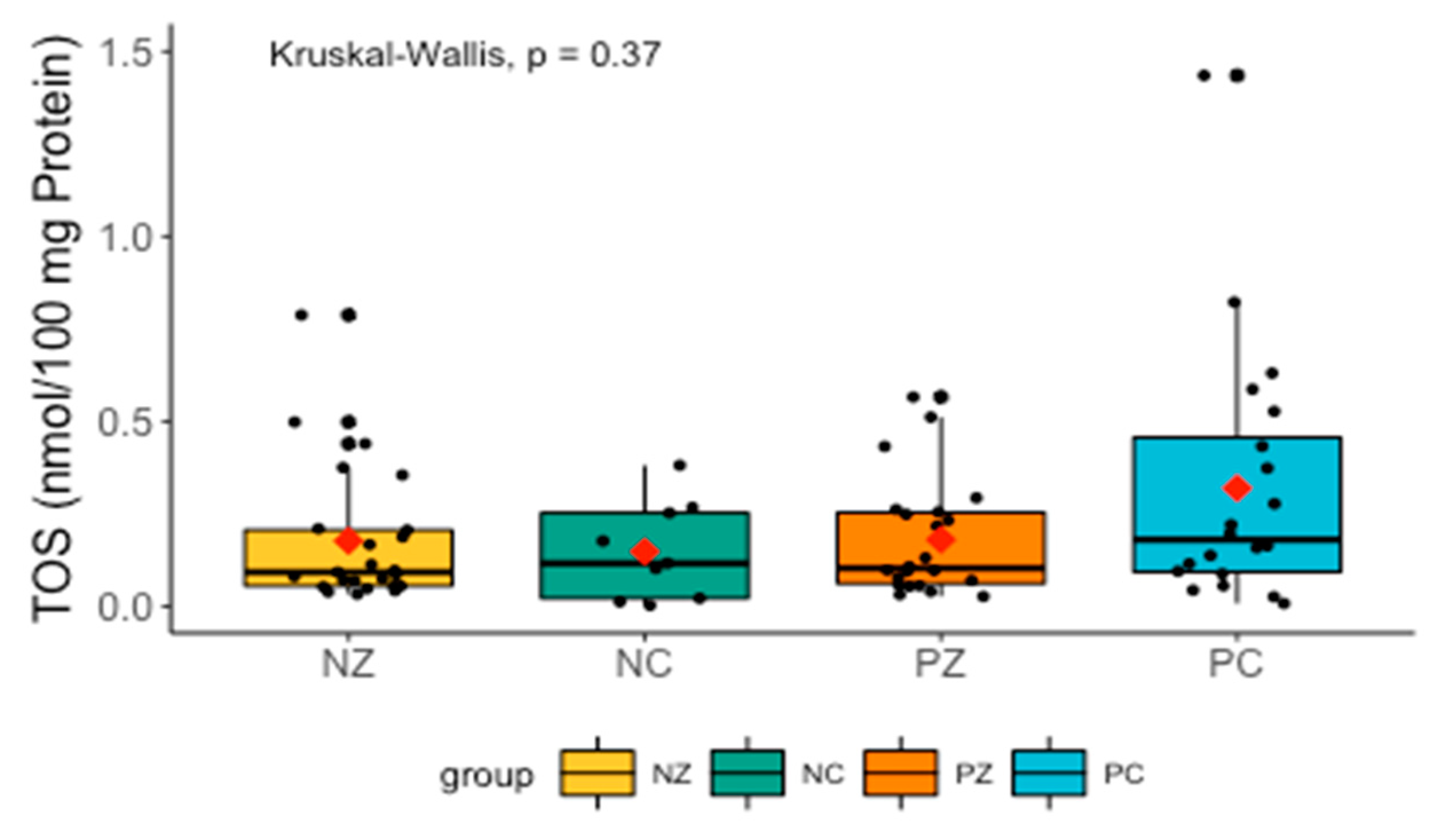
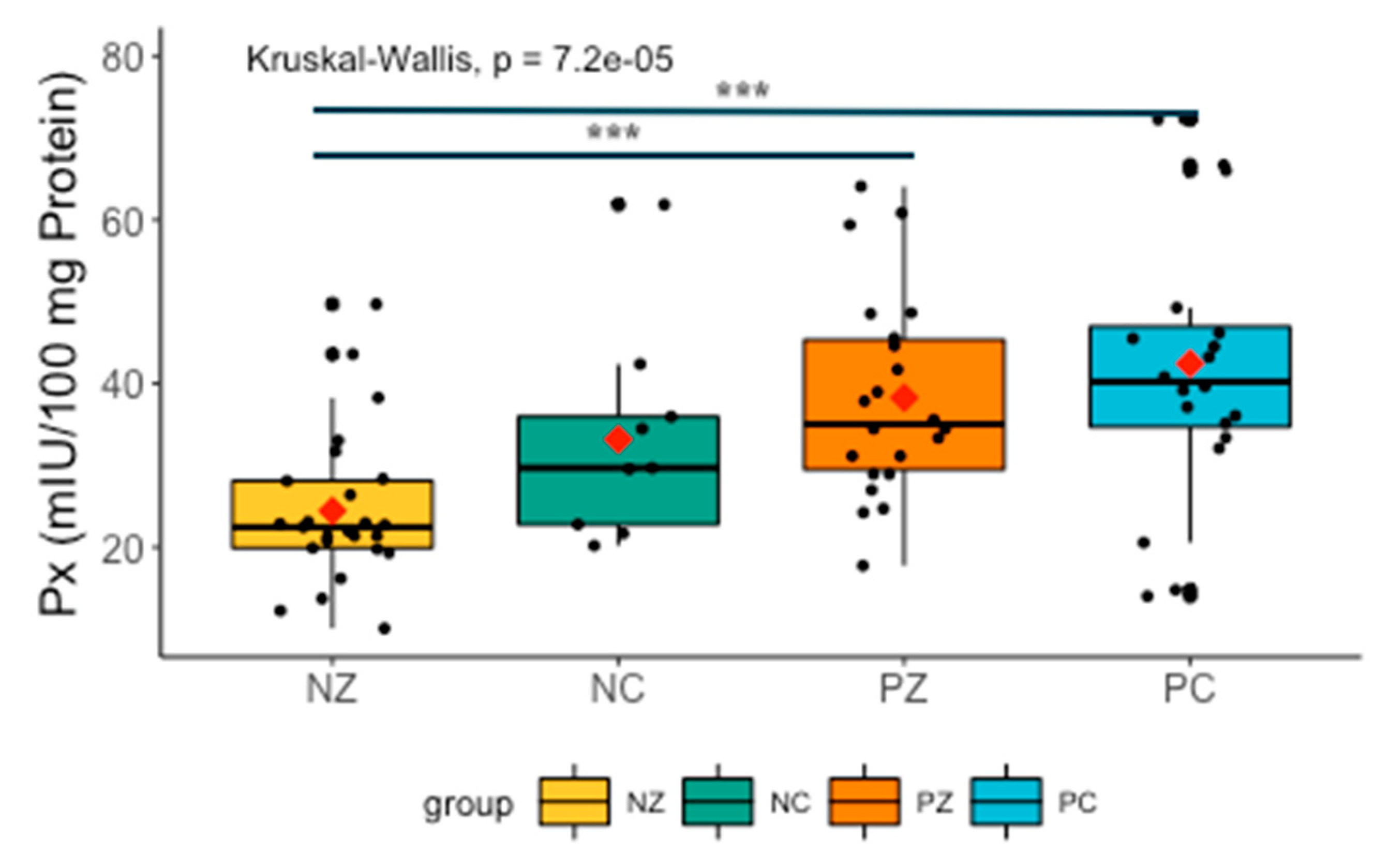
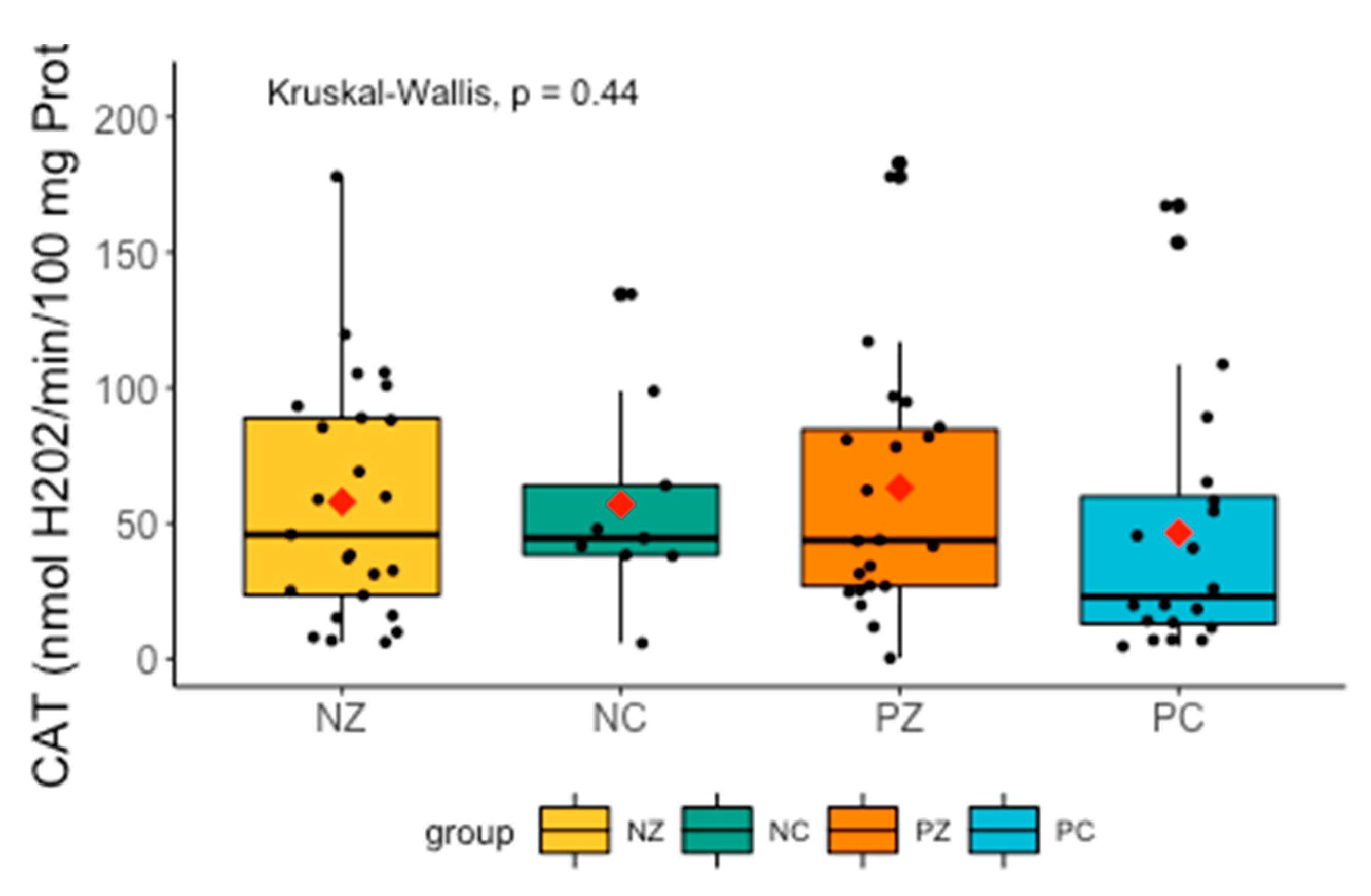
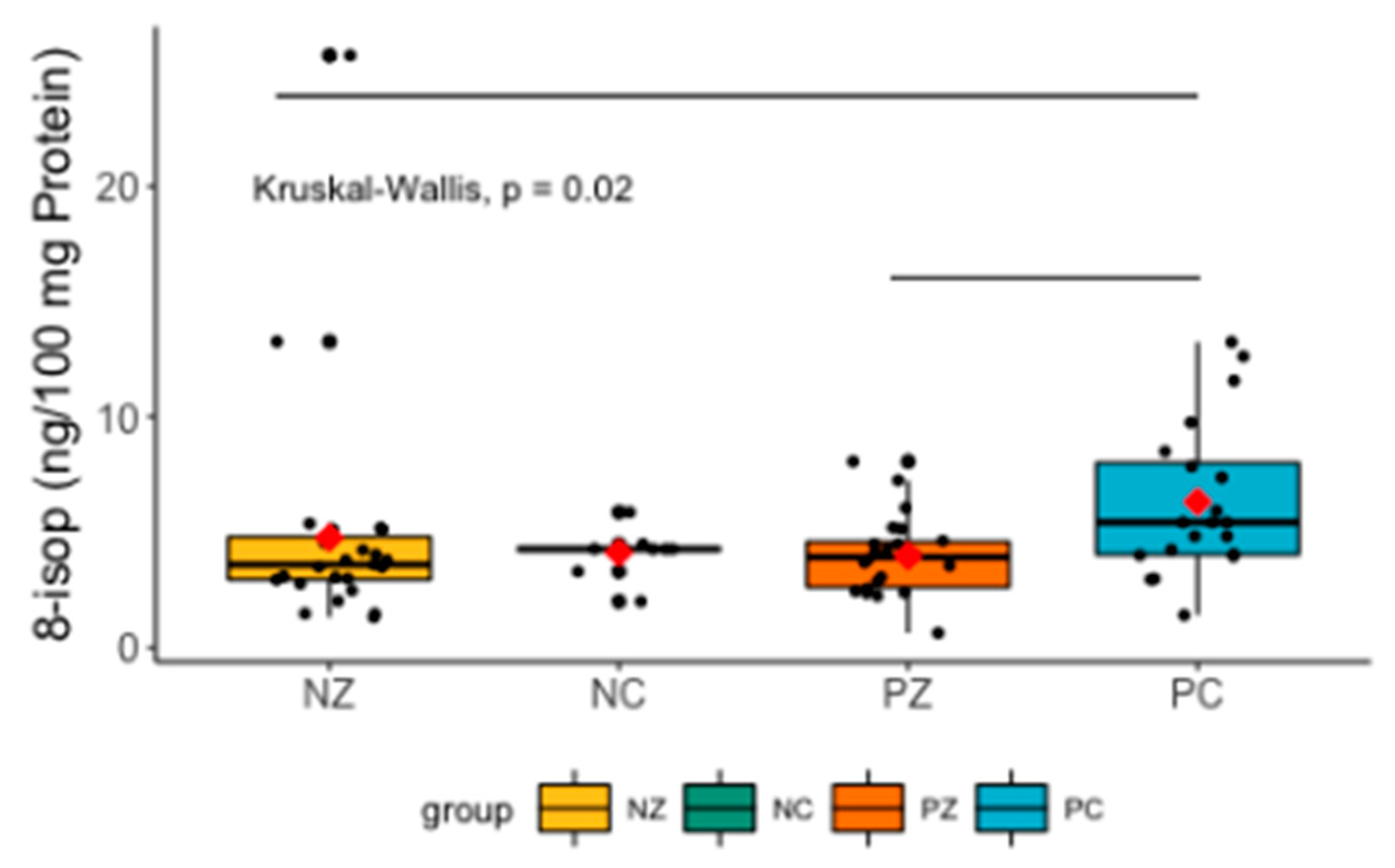
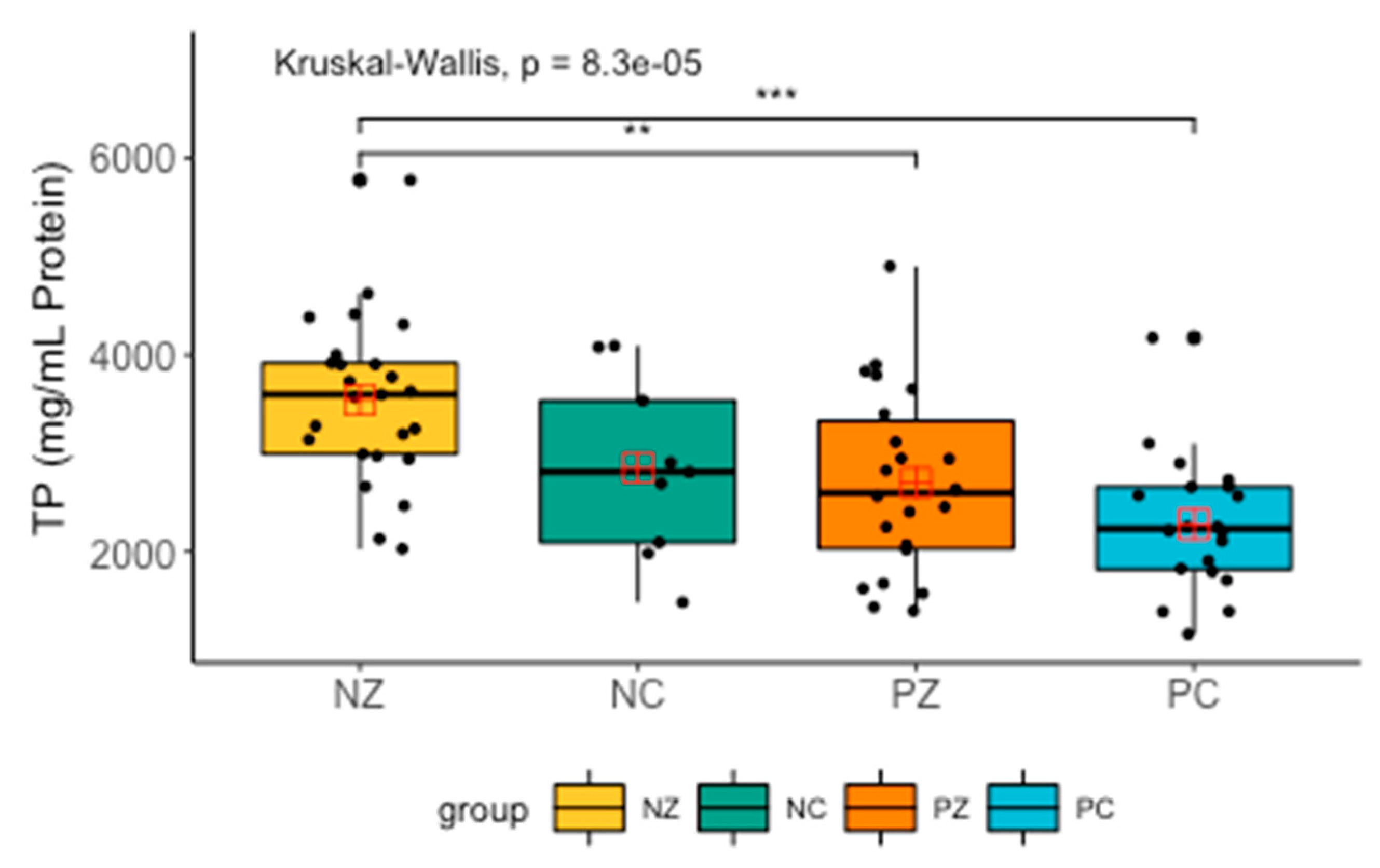
- NZ (negative healthy)—generally healthy patients without the BRCA1 mutation (25 women),
- NC (negative with cancer)—patients with breast cancer but without the BRCA1 mutation (nine women),
- PZ (positive healthy)—generally healthy patients with the BRCA1 mutation (22 women),
- PC (positive with cancer)—patients with both breast cancer and the BRCA1 mutation (20 women).
2.2. Saliva Collection
2.3. Dental Examination
2.4. Biochemical Tests
2.4.1. Redox Status
2.4.2. Salivary Antioxidants
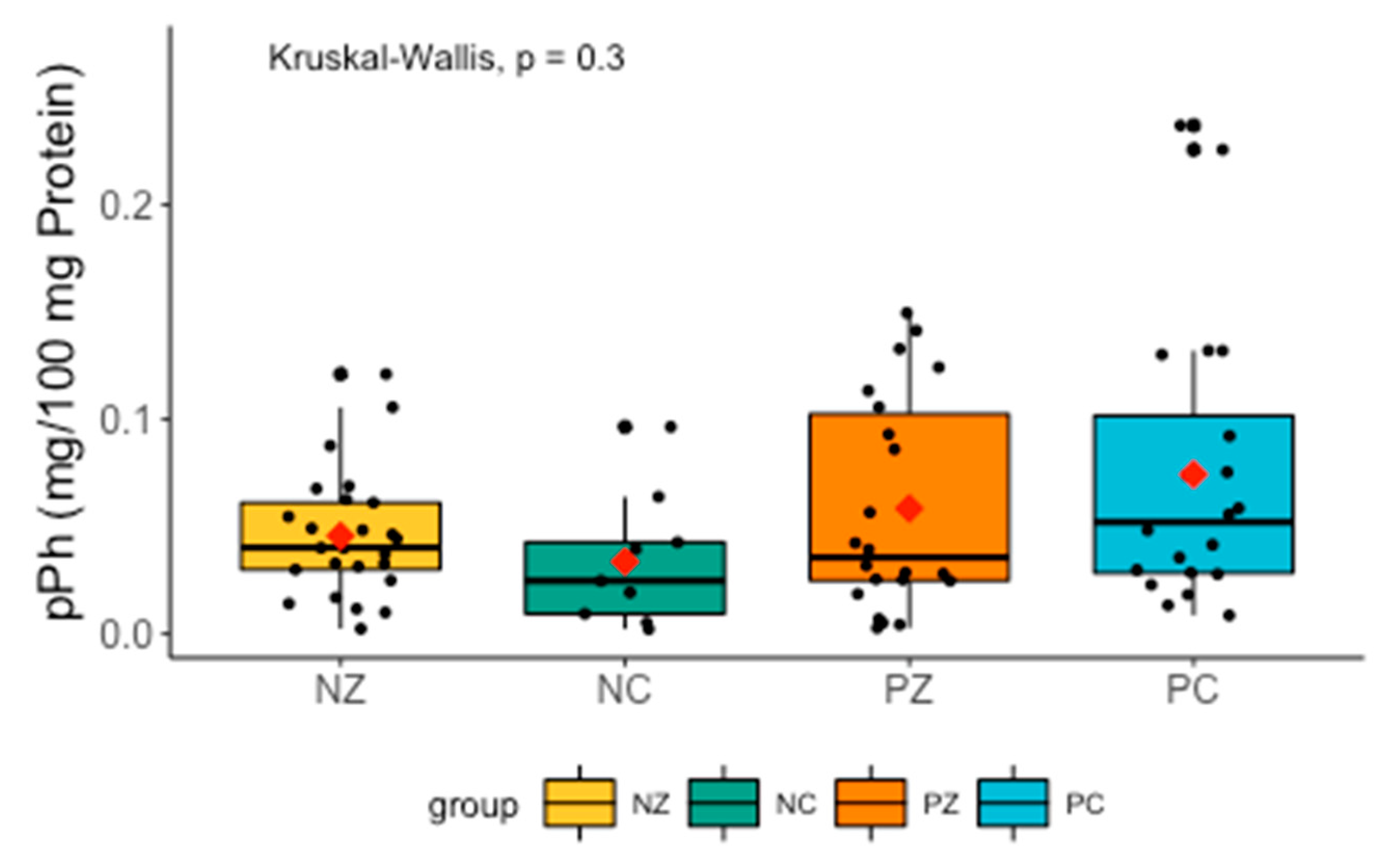
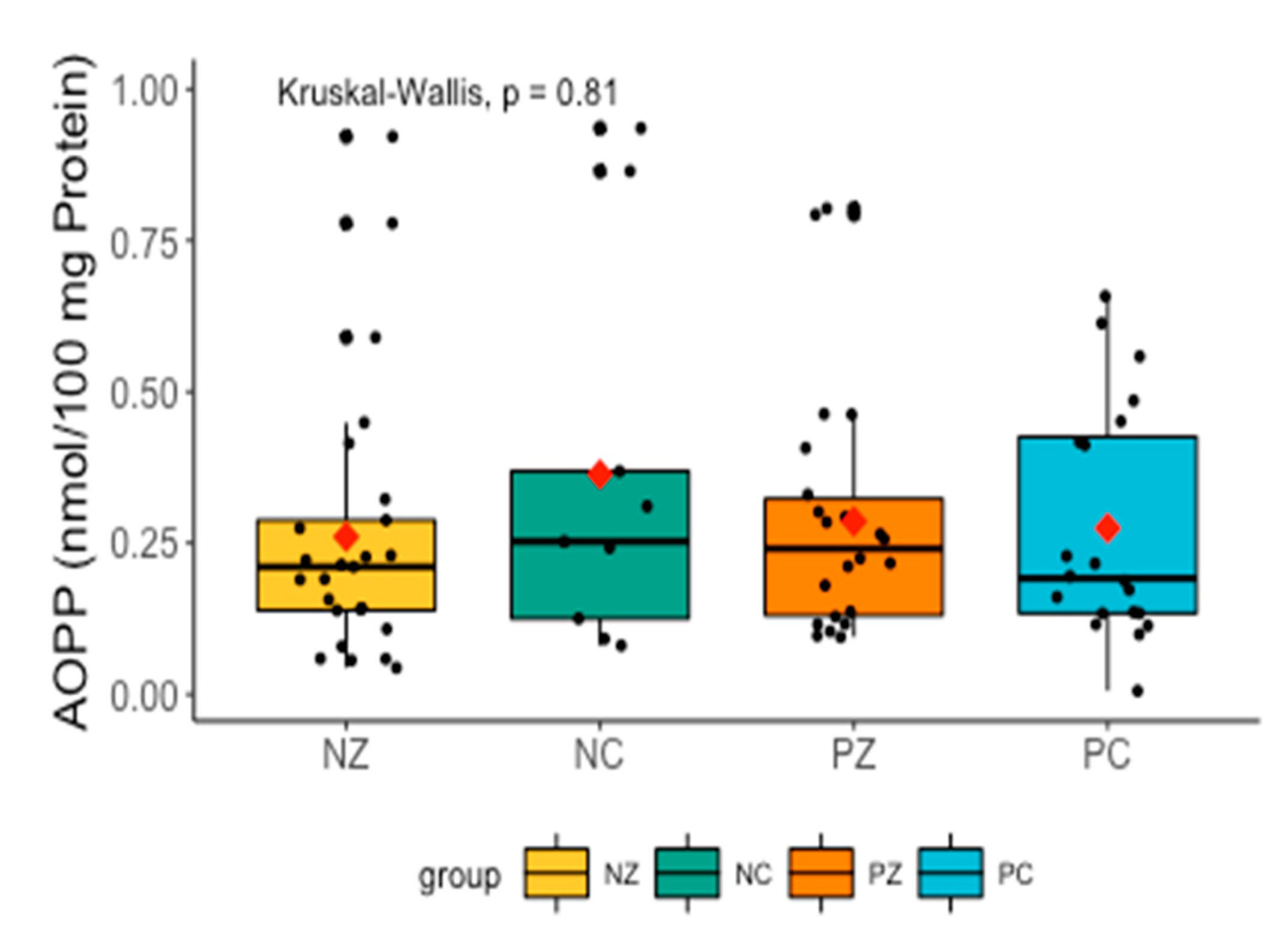
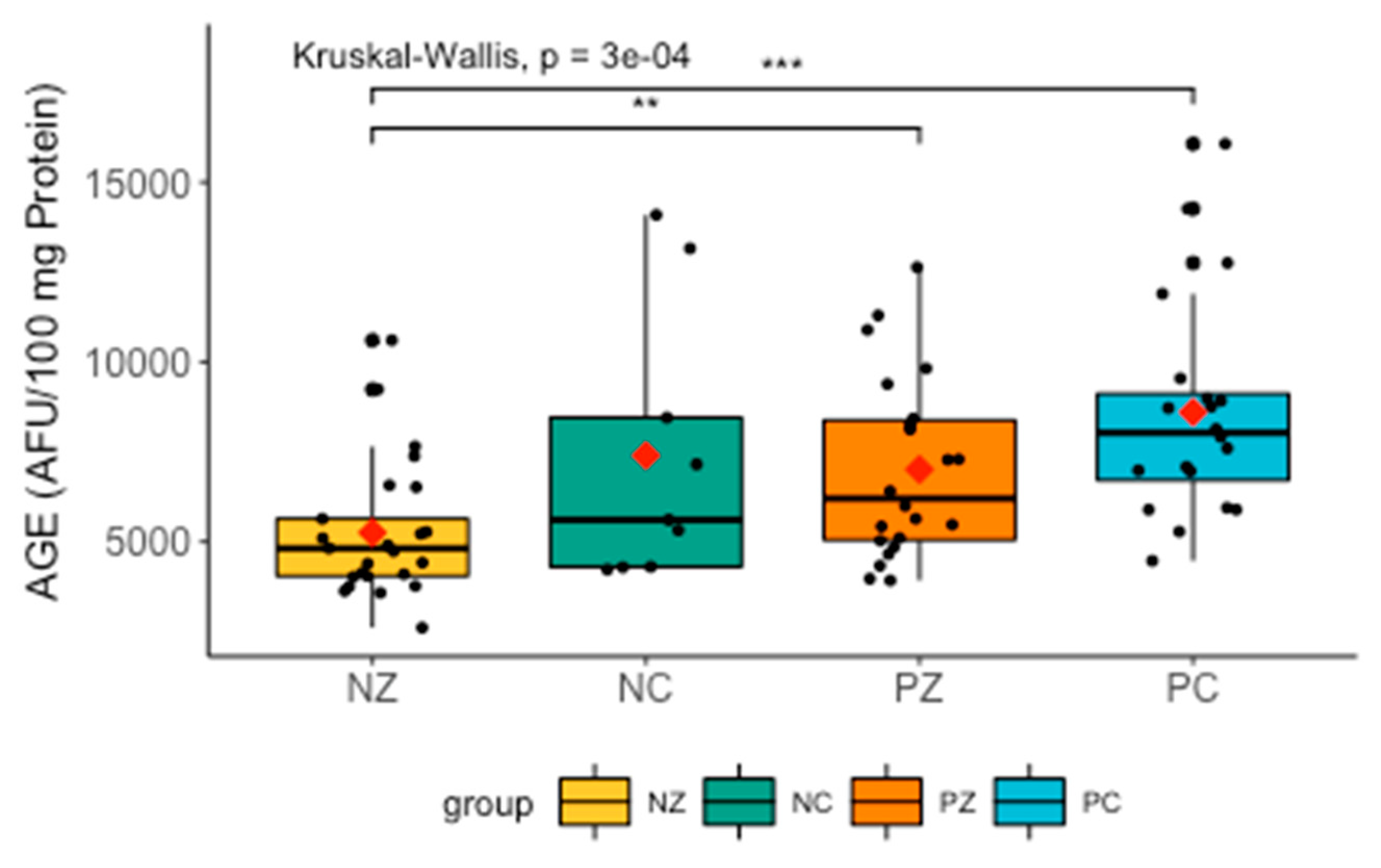
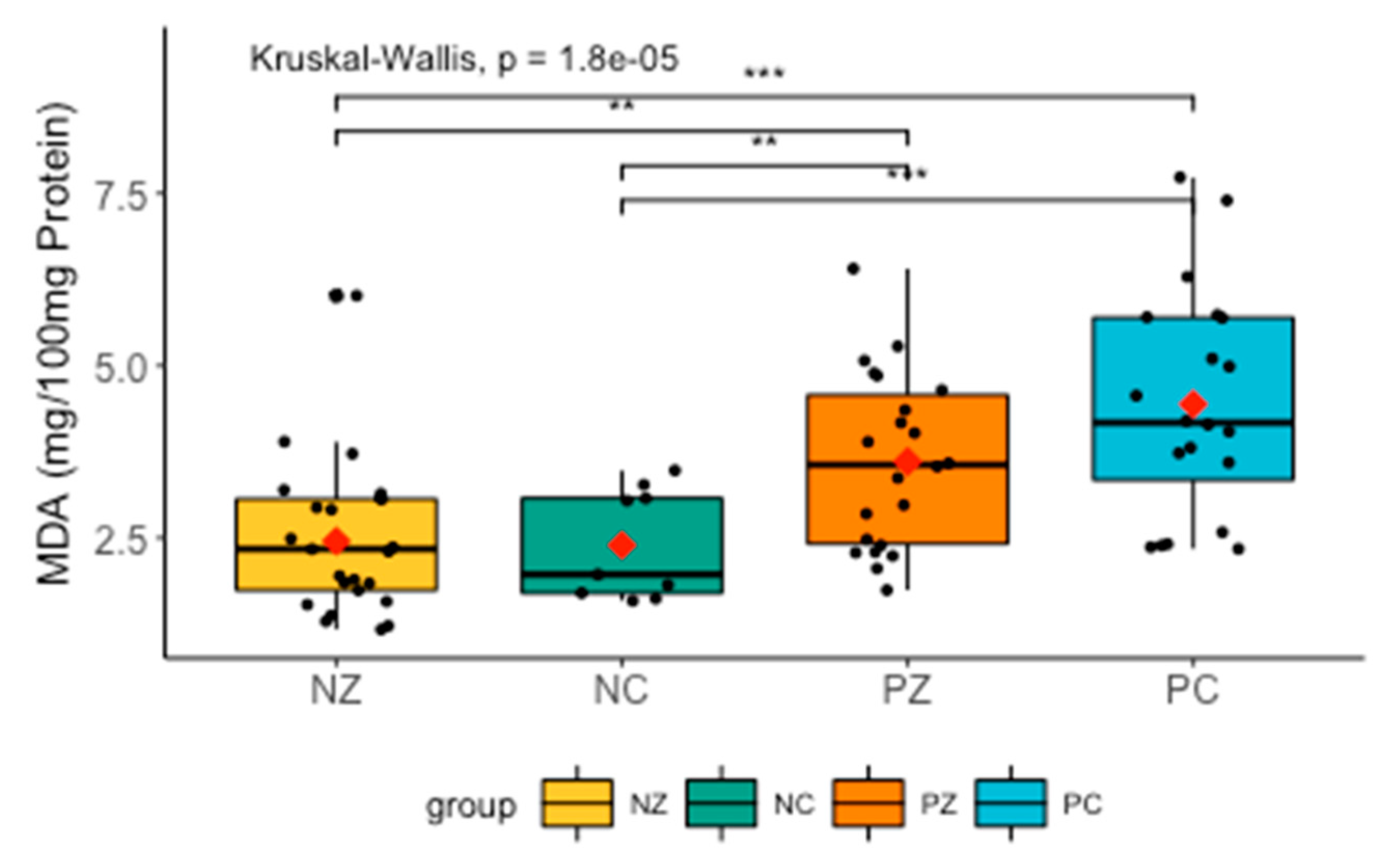
2.4.3. Oxidative Damage Products
2.4.4. Total Protein (TP)
2.5. Statistical Analysis
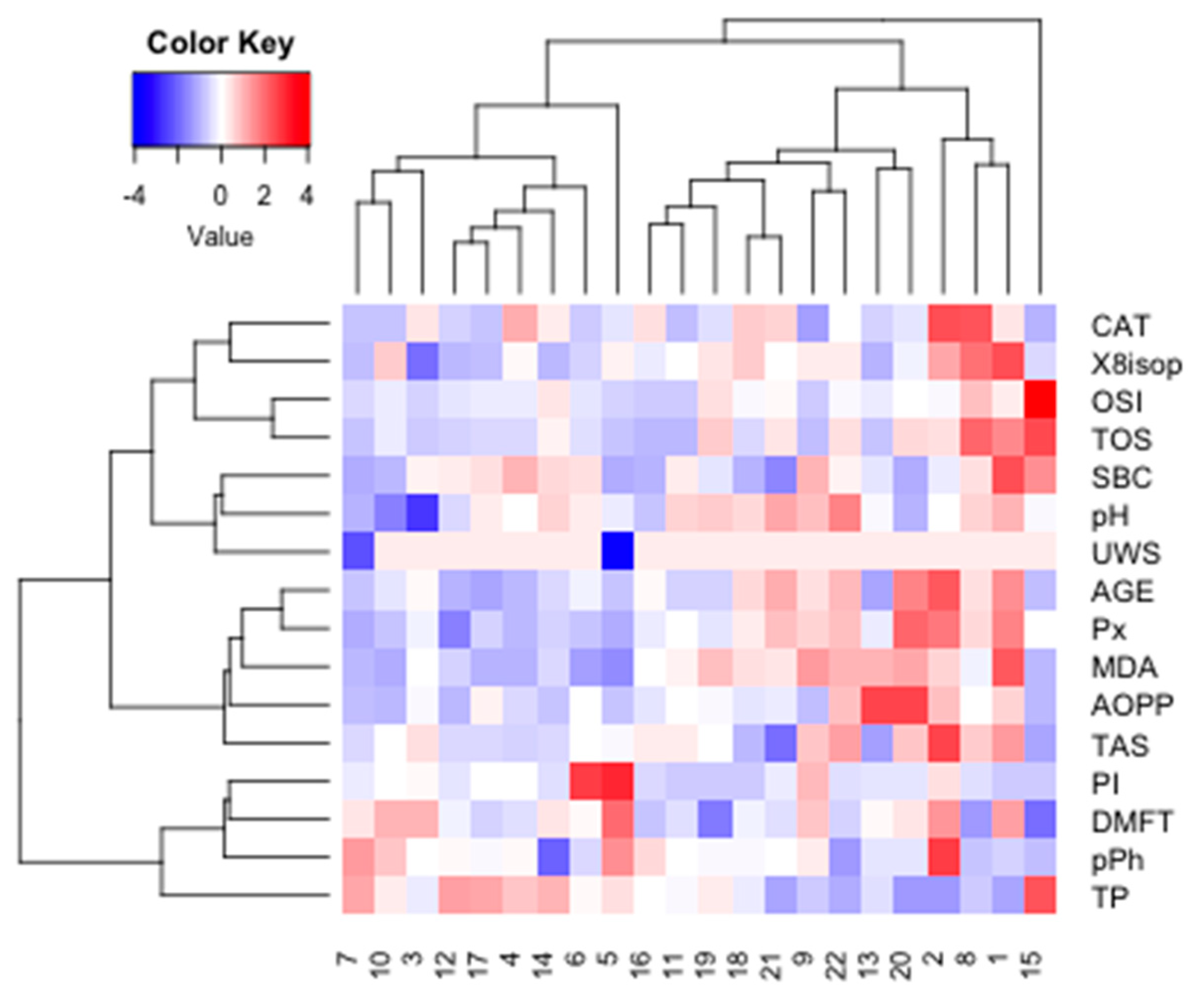
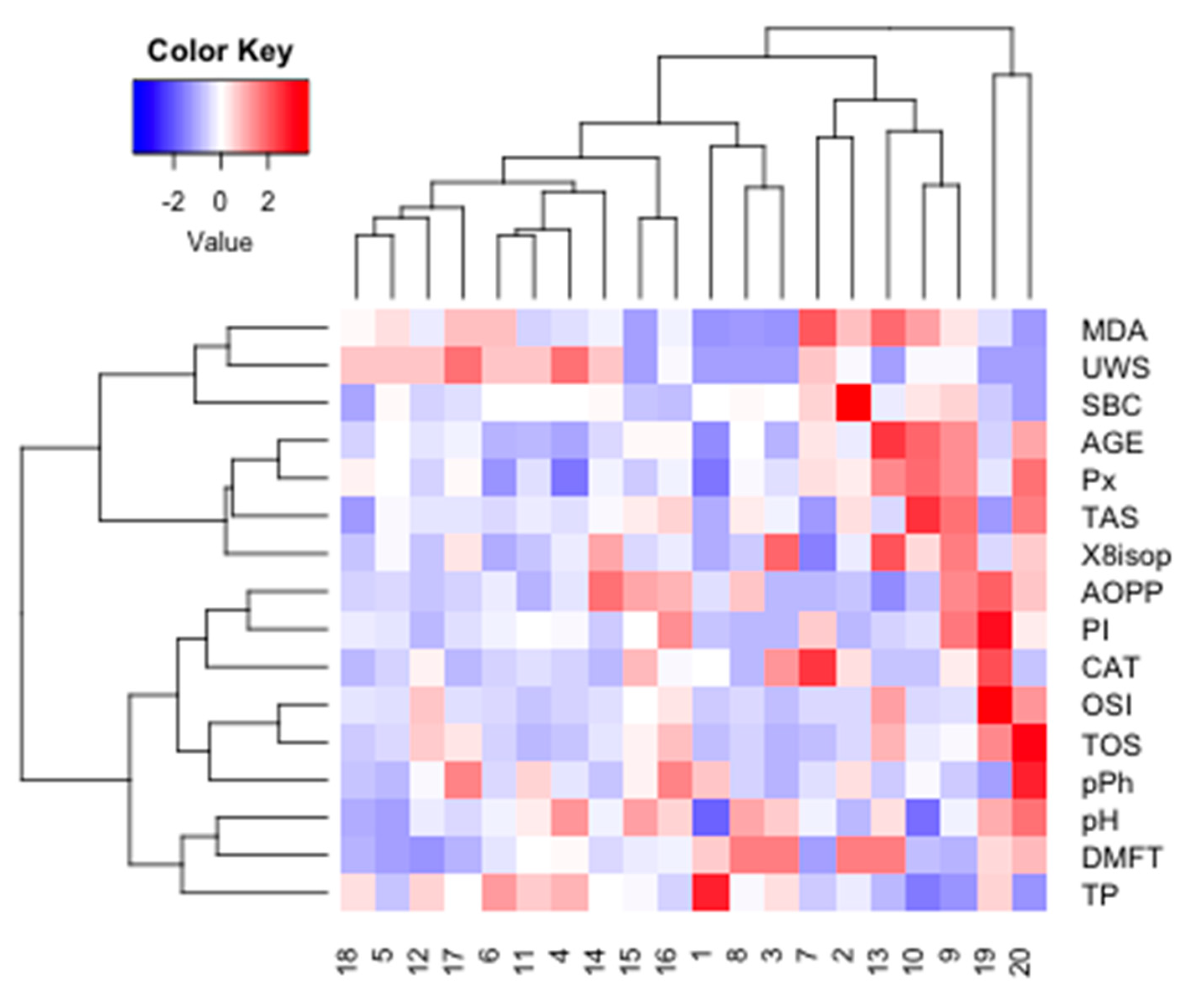
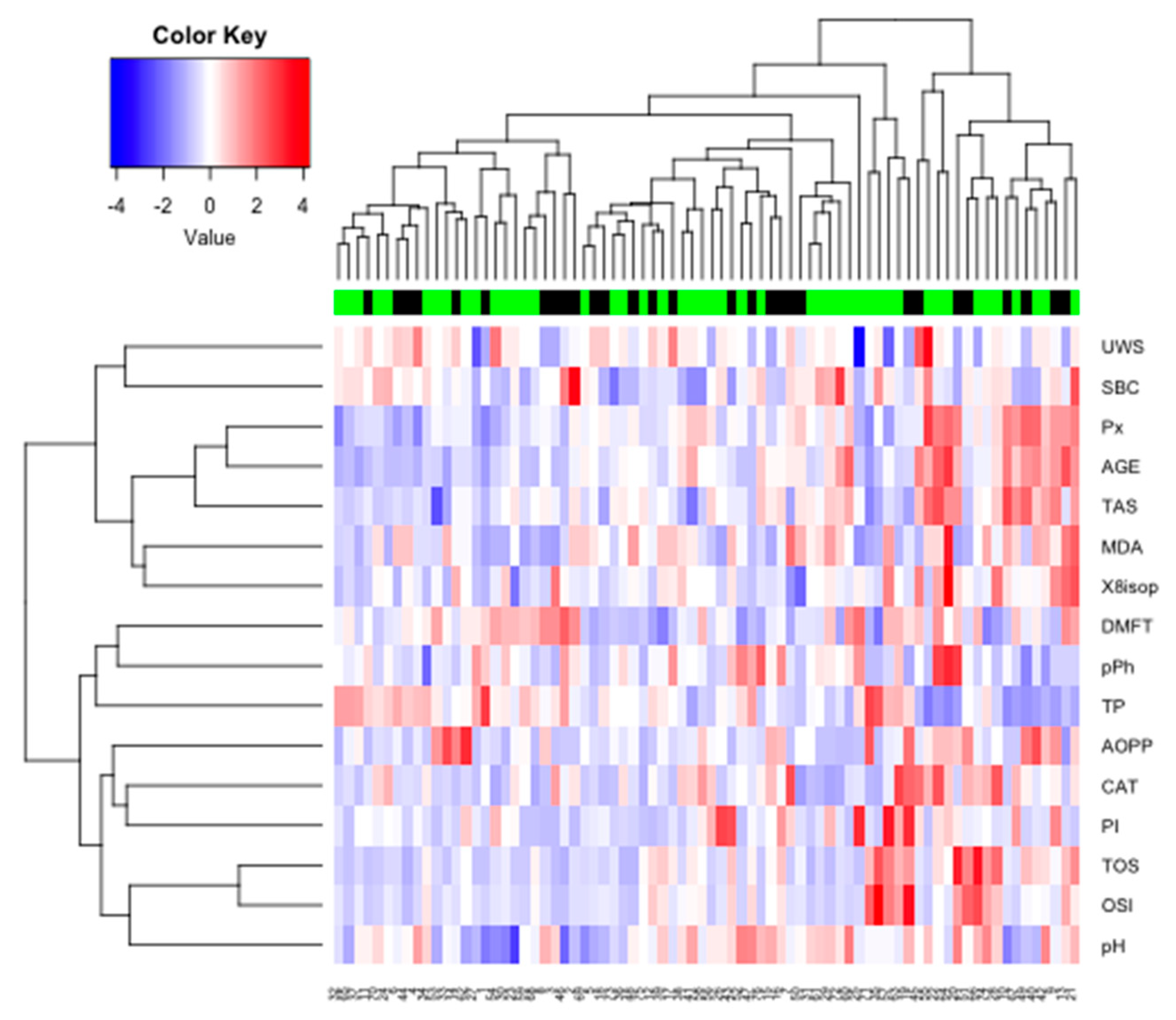
3. Results
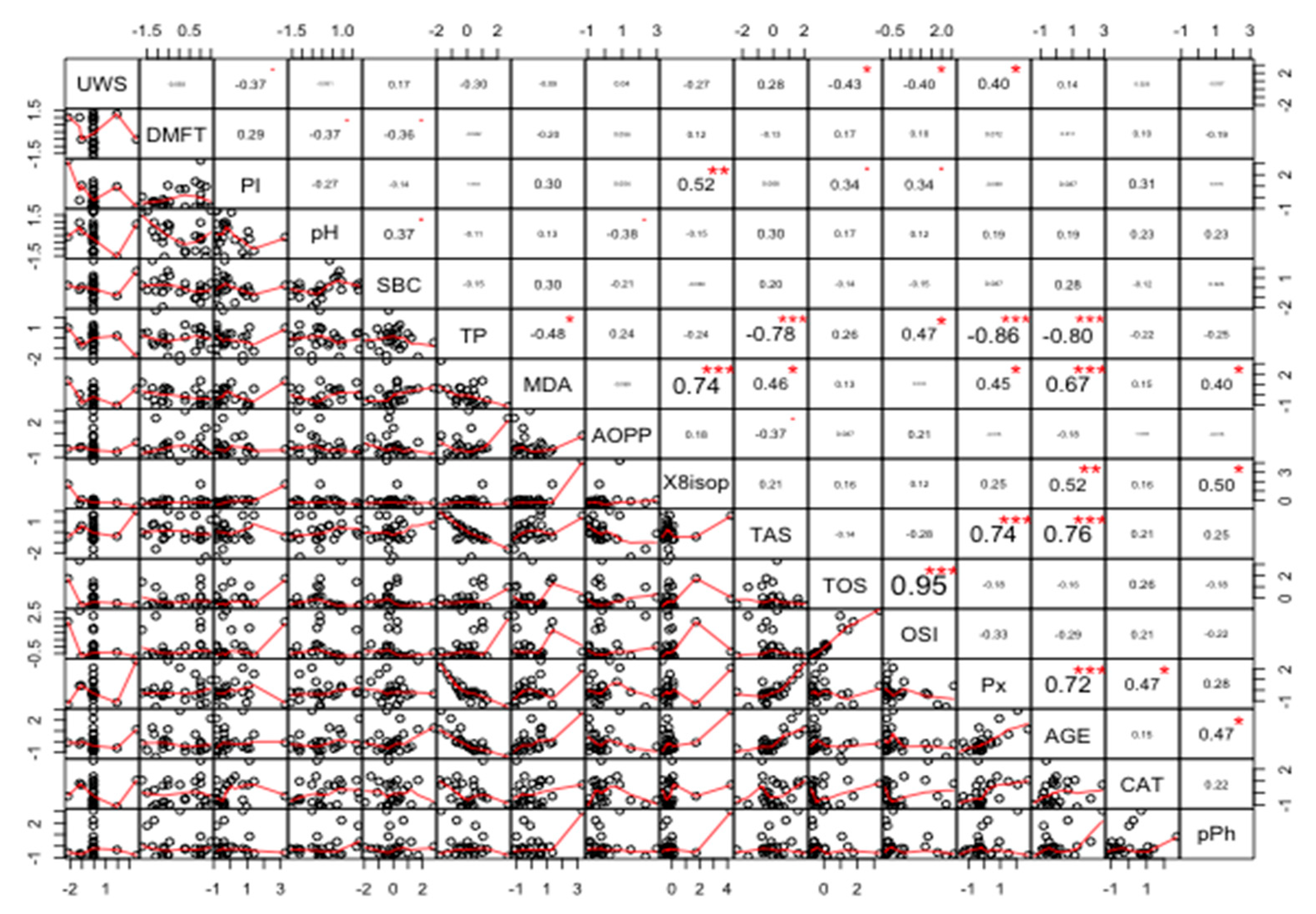
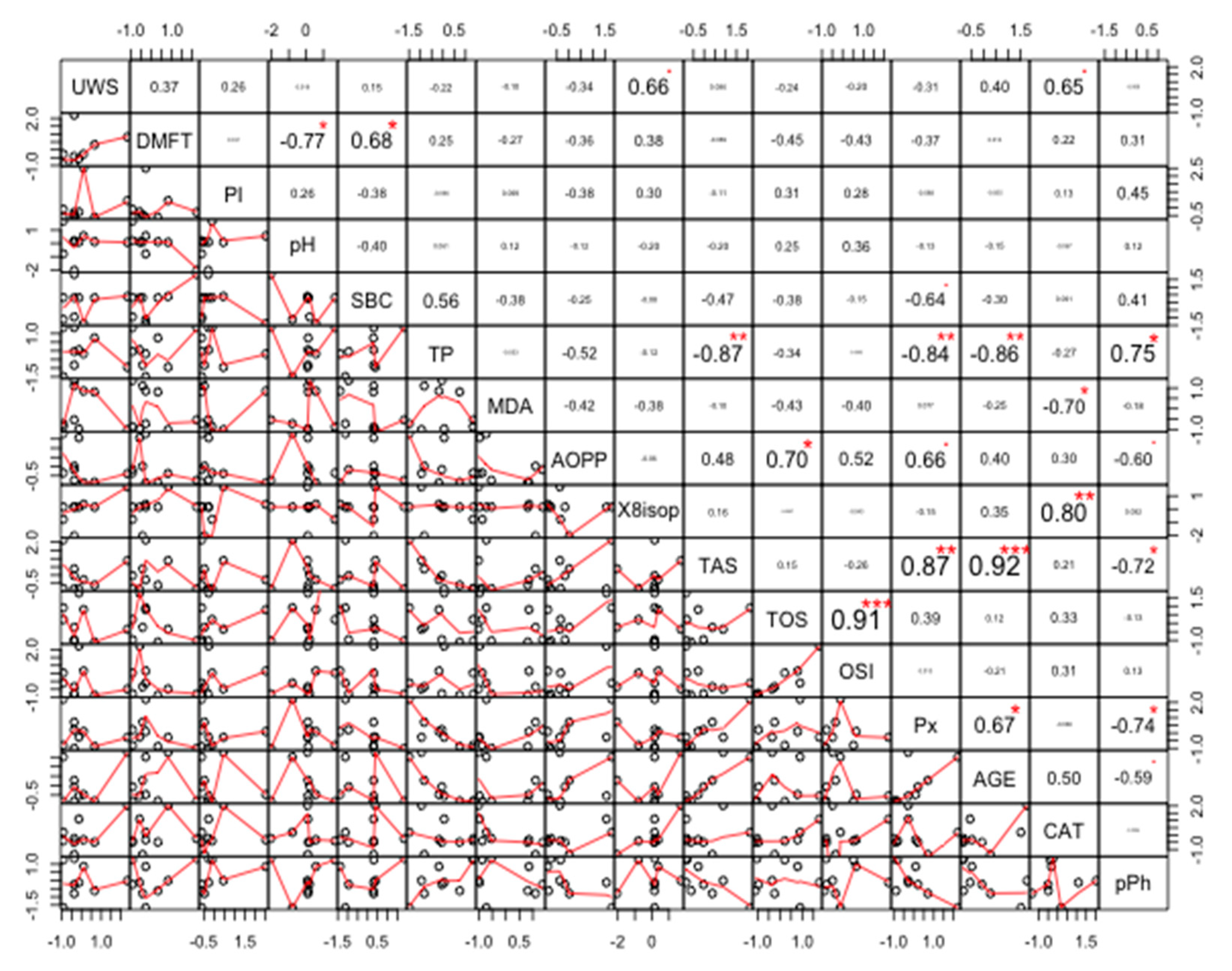
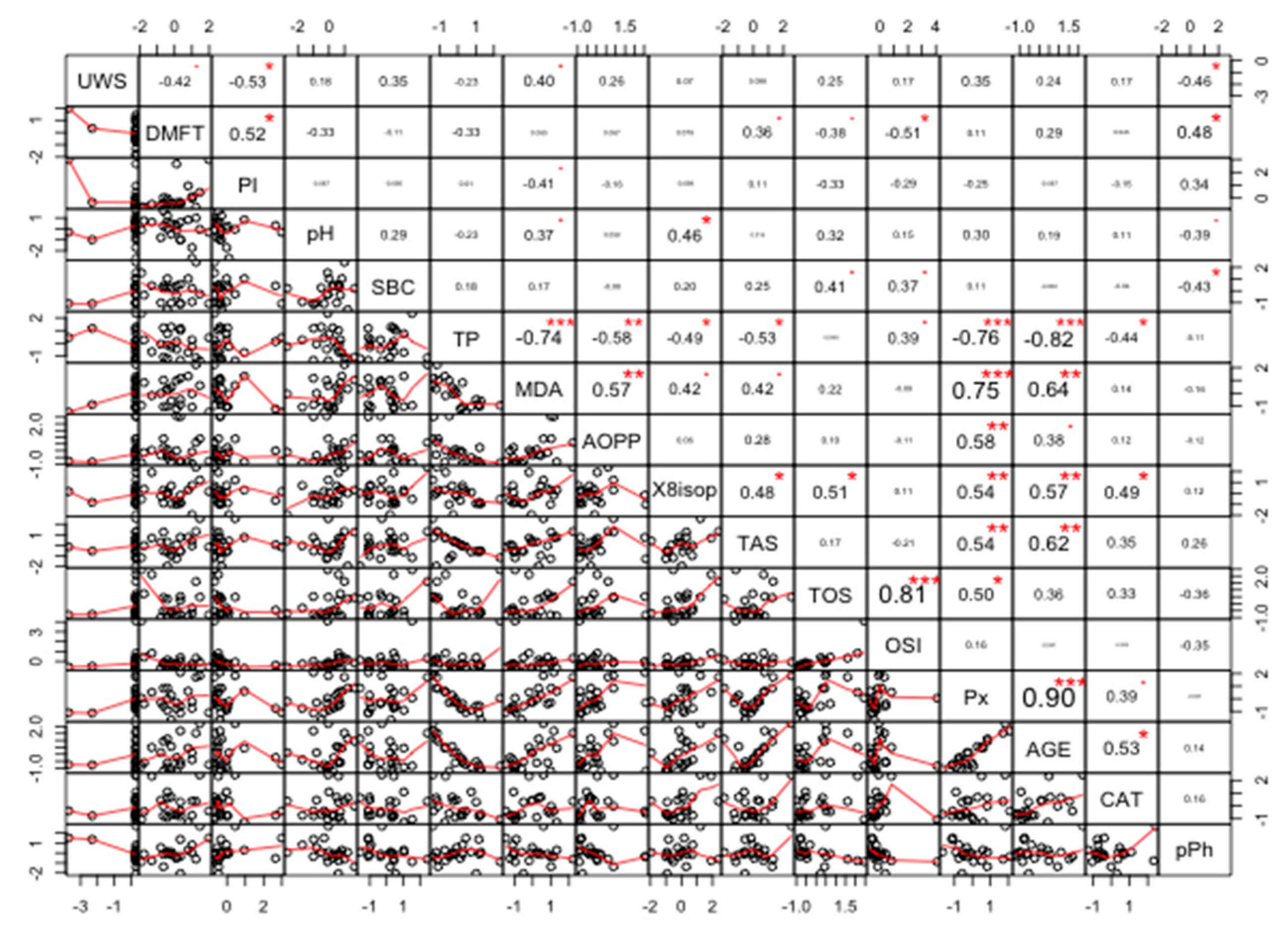
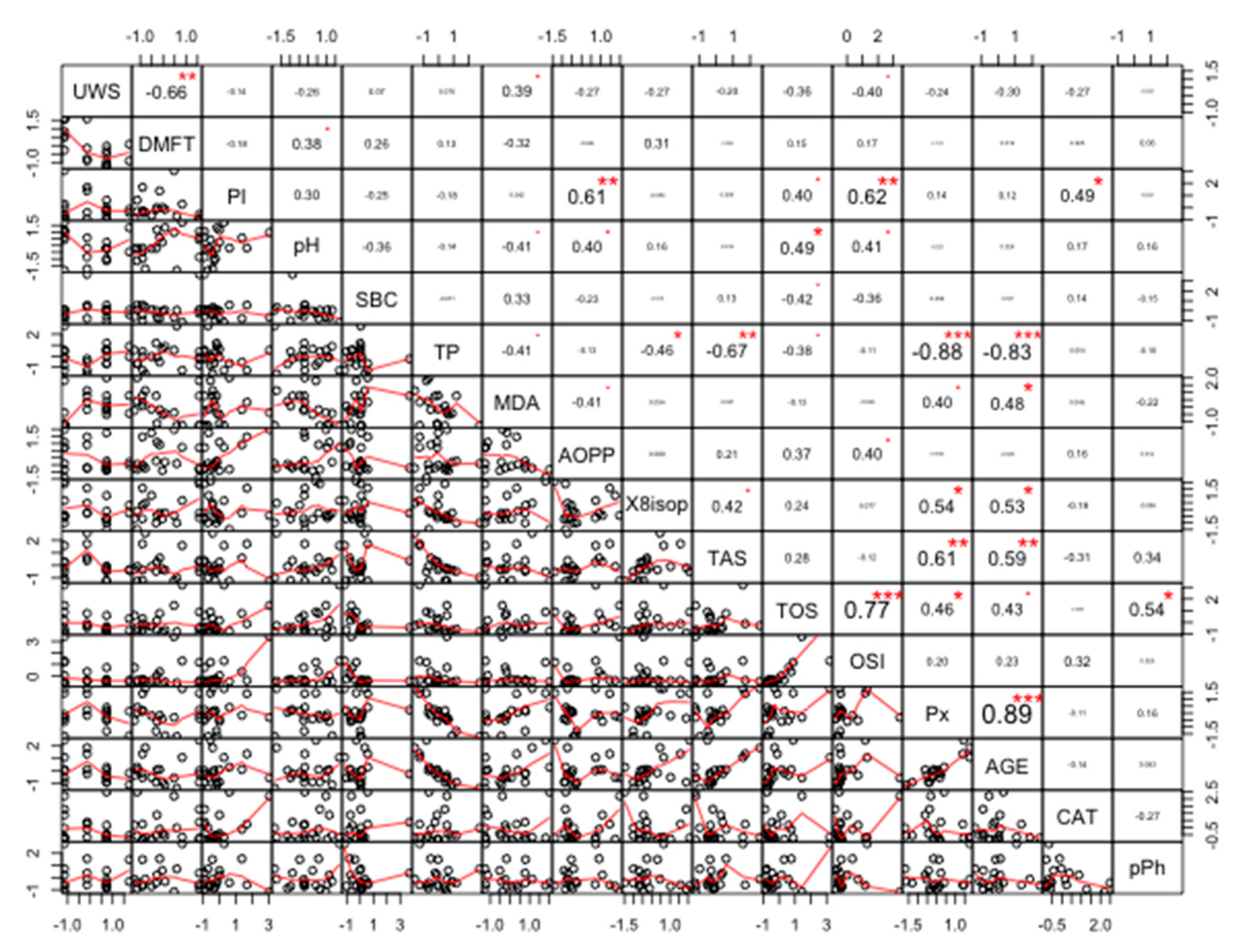
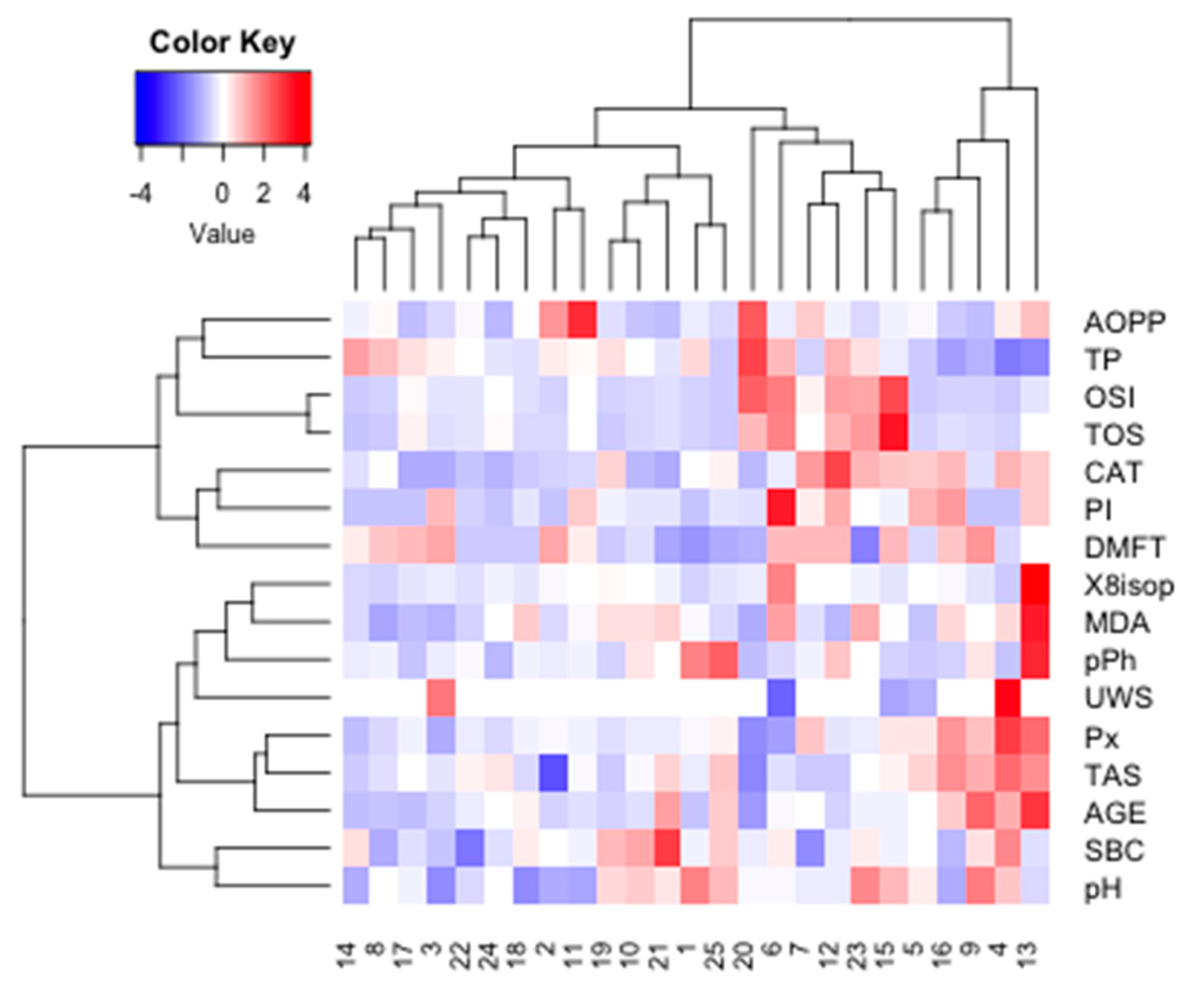
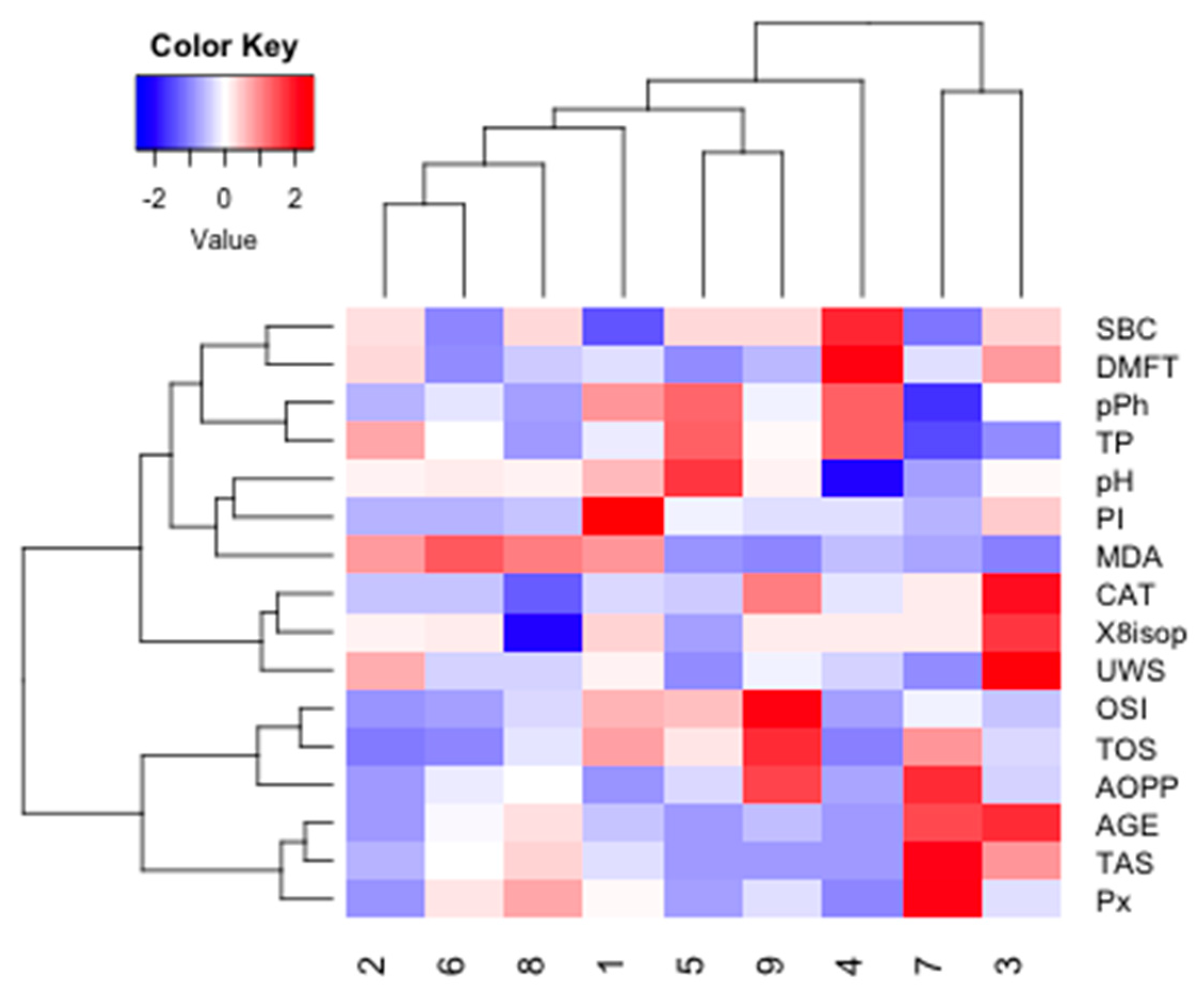
Correlations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Winters, S.; Martin, C.; Murphy, D.; Shokar, N.K. Breast cancer epidemiology, prevention, and screening. In Progress in Molecular Biology and Translational Science; Academic Press: Cambridge, MA, USA, 2017. [Google Scholar]
- Huszno, J.; Kołosza, Z.; Grzybowska, E. BRCA1 mutation in breast cancer patients: Analysis of prognostic factors and survival. Oncol. Lett. 2019, 17, 1986–1995. [Google Scholar] [CrossRef] [PubMed]
- Marks, J.R. Refining the role of BRCA1 in combating oxidative stress. Breast Cancer Res. 2013, 15, 320. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.W.; Kang, H.J.; Bae, I. BRCA1 and oxidative stress. Cancers 2014, 6, 771–795. [Google Scholar] [CrossRef] [PubMed]
- Valko, M.; Leibfritz, D.; Moncol, J.; Cronin, M.T.D.; Mazur, M.; Telser, J. Free radicals and antioxidants in normal physiological functions and human disease. Int. J. Biochem. Cell Biol. 2007, 39, 44–84. [Google Scholar] [CrossRef]
- Rajneesh, C.P.; Manimaran, A.; Sasikala, K.R.; Adaikappan, P. Lipid peroxidation and antioxidant status in patients with breast cancer. Singap. Med. J. 2008, 49, 640–643. [Google Scholar]
- Ray, G.; Batra, S.; Shukla, N.K.; Deo, S.; Raina, V.; Ashok, S.; Husain, S.A. Lipid peroxidation, free radical production and antioxidant status in breast cancer. Breast Cancer Res. Treat. 2000, 59, 163–170. [Google Scholar] [CrossRef]
- Gönenç, A.; Erten, D.; Aslan, S.; Akinci, M.; Şimşek, B.; Torun, M. Lipid peroxidation and antioxidant status in blood and tissue of malignant breast tumor and benign breast disease. Cell Biol. Int. 2006, 30, 376–380. [Google Scholar] [CrossRef]
- Söder, B.; Yakob, M.; Meurman, J.H.; Andersson, L.C.; Klinge, B.; Söder, P.Ö. Periodontal disease may associate with breast cancer. Breast Cancer Res. Treat. 2011, 127, 497–502. [Google Scholar] [CrossRef]
- Emekli-Alurfan, E.; Demir, G.; Kasikci, E.; Tunali-Akbay, T.; Pisiriciler, R.; Caliskan, E.; Yarat, A. Altered biochemical parameters in the saliva of patients with breast cancer. Tohoku J. Exp. Med. 2008, 214, 89–96. [Google Scholar] [CrossRef]
- Gornitsky, M.; Velly, A.M.; Mohit, S.; Almajed, M.; Su, H.; Panasci, L.; Schipper, H.M. Altered levels of salivary 8-oxo-7-hydrodeoxyguanosine in breast cancer. JDR Clin. Transl. Res. 2016, 1, 171–177. [Google Scholar] [CrossRef]
- Hecht, F.; Pessoa, C.F.; Gentile, L.B.; Rosenthal, D.; Carvalho, D.P.; Fortunato, R.S. The role of oxidative stress on breast cancer development and therapy. Tumor Biol. 2016, 37, 4281–4291. [Google Scholar] [CrossRef] [PubMed]
- Gurer-Orhan, H.; Ince, E.; Konyar, D.; Saso, L.; Suzen, S. The role of oxidative stress modulators in breast cancer. Curr. Med. Chem. 2017, 25, 4084–4101. [Google Scholar] [CrossRef] [PubMed]
- Zalewska, A.; Ziembicka, D.; Żendzian-Piotrowska, M.; Maciejczyk, M. The impact of high-fat diet on mitochondrial function, free radical production, and nitrosative stress in the salivary glands of wistar rats. Oxid. Med. Cell. Longev. 2019, 2019, 2606120. [Google Scholar] [CrossRef] [PubMed]
- Kołodziej, U.; Maciejczyk, M.; Miasko, A.; Matczuk, J.; Knas, M.; Zukowski, P.; Zendzian-Piotrowska, M.; Borys, J.; Zalewska, A. Oxidative modification in the salivary glands of high fat-diet induced insulin resistant rats. Front. Physiol. 2017, 8, 20. [Google Scholar] [CrossRef]
- Porto-Mascarenhas, E.C.; Assad, D.X.; Chardin, H.; Gozal, D.; De Luca Canto, G.; Acevedo, A.C.; Guerra, E.N.S. Salivary biomarkers in the diagnosis of breast cancer: A review. Crit. Rev. Oncol. Hematol. 2017, 110, 62–73. [Google Scholar] [CrossRef]
- Fejfer, K.; Buczko, P.; Niczyporuk, M.; Ładny, J.R.; Hady, H.R.; Knaś, M.; Waszkiel, D.; Klimiuk, A.; Zalewska, A.; Maciejczyk, M. Oxidative modification of biomolecules in the nonstimulated and stimulated saliva of patients with morbid obesity treated with bariatric surgery. Biomed. Res. Int. 2017, 2017, 4923769. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Szulimowska, J.; Skutnik, A.; Taranta-Janusz, K.; Wasilewska, A.; Wiśniewska, N.; Zalewska, A. Salivary biomarkers of oxidative stress in children with chronic kidney disease. J. Clin. Med. 2018, 7, 209. [Google Scholar] [CrossRef]
- Klimiuk, A.; Maciejczyk, M.; Choromańska, M.; Fejfer, K.; Waszkiewicz, N.; Zalewska, A. Salivary redox biomarkers in different stages of dementia severity. J. Clin. Med. 2019, 8, 840. [Google Scholar] [CrossRef]
- Choromańska, M.; Klimiuk, A.; Kostecka-Sochoń, P.; Wilczyńska, K.; Kwiatkowski, M.; Okuniewska, N.; Waszkiewicz, N.; Zalewska, A.; Maciejczyk, M. Antioxidant defence, oxidative stress and oxidative damage in saliva, plasma and erythrocytes of dementia patients. Can salivary AGE be a marker of dementia? Int. J. Mol. Sci. 2017, 18, 2205. [Google Scholar] [CrossRef]
- World Health Organization. Oral Health Surveys: Basic Methods; WHO: Geneva, Switzerland, 2013; ISBN 9789241548649. [Google Scholar]
- Maciejczyk, M.; Skutnik-Radziszewska, A.; Zieniewska, I.; Matczuk, J.; Domel, E.; Waszkiel, D.; Żendzian-Piotrowska, M.; Szarmach, I.; Zalewska, A. Antioxidant defense, oxidative modification, and salivary gland function in an early phase of cerulein pancreatitis. Oxid. Med. Cell. Longev. 2019, 2019, 1–14. [Google Scholar] [CrossRef]
- Mansson-Rahemtulla, B.; Baldone, D.C.; Pruitt, K.M.; Rahemtulla, F. Specific assays for peroxidases in human saliva. Arch. Oral Biol. 1986, 31, 661–668. [Google Scholar] [CrossRef]
- Aebi, H. Catalase in vitro. In Methods in Enzymology; Academic Press: Cambridge, MA, USA, 1984; Volume 105, pp. 121–126. ISBN 9780121820053. [Google Scholar]
- Singleton, V.L.; Orthofer, R.; Lamuela-Raventós, R.M. Analysis of Total Phenols and Other Oxidation Substrates and Antioxidants by Means of Folin-Ciocalteu Reagent. Methods in Enzymology; Academic Press: Cambridge, MA, USA, 1999; Volume 299, pp. 152–178. [Google Scholar] [CrossRef]
- Kalousová, M.; Skrha, J.; Zima, T. Advanced glycation end-products and advanced oxidation protein products in patients with diabetes mellitus. Physiol. Res. 2002, 51, 597–604. [Google Scholar] [PubMed]
- Buege, J.A.; Aust, S.D. Microsomal lipid peroxidation. Methods Enzymol. 1978, 52, 302–310. [Google Scholar] [PubMed]
- Żukowski, P.; Maciejczyk, M.; Waszkiel, D. Sources of free radicals and oxidative stress in the oral cavity. Arch. Oral Biol. 2018, 92, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Tothova, L.; Kamodyova, N.; Cervenka, T.; Celec, P. Salivary markers of oxidative stress in oral diseases. Front. Cell. Infect. Microbiol. 2015, 5, 73. [Google Scholar] [CrossRef] [PubMed]
- Pande, D.; Negi, R.; Karki, K.; Khanna, S.; Khanna, R.S.; Khanna, H.D. Oxidative damage markers as possible discriminatory biomarkers in breast carcinoma. Transl. Res. 2012, 160, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Rice-Evans, C.; Miller, N.J. [241 Total Antioxidant Status in Plasma and Body Fluids. Methods in Enzymology; Academic Press: Cambridge, MA, USA, 1994; Volume 234, pp. 279–293. [Google Scholar] [CrossRef]
- Borys, J.; Maciejczyk, M.; Antonowicz, B.; Krętowski, A.; Waszkiel, D.; Bortnik, P.; Czarniecka-Bargłowska, K.; Kocisz, M.; Szulimowska, J.; Czajkowski, M.; et al. Exposure to Ti4Al4V titanium alloy leads to redox abnormalities, oxidative stress, and oxidative damage in patients treated for mandible fractures. Oxid. Med. Cell. Longev. 2018. [Google Scholar] [CrossRef]
- Knaś, M.; Maciejczyk, M.; Waszkiel, D.; Zalewska, A. Oxidative stress and salivary antioxidants. Dent. Med. Probl. 2013, 50, 461–466. [Google Scholar]
- Nagler, R.M.; Klein, I.; Zarzhevsky, N.; Drigues, N.; Reznick, A.Z. Characterization of the differentiated antioxidant profile of human saliva. Free Radic. Biol. Med. 2002, 32, 268–277. [Google Scholar] [CrossRef]
- Fini, M.A.; Elias, A.; Johnson, R.J.; Wright, R.M. Contribution of uric acid to cancer risk, recurrence, and mortality. Clin. Transl. Med. 2012, 1, 16. [Google Scholar] [CrossRef]
- Yue, C.F.; Feng, P.N.; Yao, Z.R.; Yu, X.G.; Lin, W.B.; Qian, Y.M.; Guo, Y.M.; Li, L.S.; Liu, M. High serum uric acid concentration predicts poor survival in patients with breast cancer. Clin. Chim. Acta 2017, 473, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell. Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef] [PubMed]
- Maciejczyk, M.; Żebrowska, E.; Chabowski, A. Insulin resistance and oxidative stress in the brain: What’s new? Int. J. Mol. Sci. 2019, 20, 874. [Google Scholar] [CrossRef] [PubMed]
- Wautier, M.-P.; Chappey, O.; Corda, S.; Stern, D.M.; Schmidt, A.M.; Wautier, J.-L. Activation of NADPH oxidase by AGE links oxidant stress to altered gene expression via RAGE. Am. J. Physiol. Metab. 2001, 280, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Irani, S.; Bidari-Zerehpoush, F. BRCA1/2 mutations in salivary pleomorphic adenoma and carcinoma-ex-pleomorphic adenoma. J. Int. Soc. Prev. Community Dent. 2017, 7, S155–S162. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Mikoluc, B.; Pietrucha, B.; Heropolitanska—Pliszka, E.; Pac, M.; Motkowski, R.; Car, H. Oxidative stress, mitochondrial abnormalities and antioxidant defense in Ataxia-telangiectasia, Bloom syndrome and Nijmegen breakage syndrome. Redox Biol. 2017, 11, 375–383. [Google Scholar] [CrossRef]
- Lavin, M.F.; Scott, S.; Gueven, N.; Kozlov, S.; Peng, C.; Chen, P. Functional consequences of sequence alterations in the ATM gene. DNA Repair 2004, 3, 1197–1205. [Google Scholar] [CrossRef]
- Angèle, S.; Hall, J. The ATM gene and breast cancer: Is it really a risk factor? Mutat. Res. Rev. Mutat. Res. 2000, 462, 167–178. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Kossakowska, A.; Szulimowska, J.; Klimiuk, A.; Car, H.; Ładny, J.R.; Chabowski, A.; Zalewska, A. Lysosomal exoglycosidase profile and secretory function in the salivary glands of rats with streptozotocin-induced diabetes. J. Diabetes Res. 2017, 2017. [Google Scholar] [CrossRef]
- Javaid, M.A.; Ahmed, A.S.; Durand, R.; Tran, S.D. Saliva as a diagnostic tool for oral and systemic diseases. J. Oral Biol. Craniofacial Res. 2016, 6, 66–75. [Google Scholar] [CrossRef]

| NZ (n = 25) | NC (n = 9) | PZ (n = 22) | PC (n = 20) | Kruskal–Wallis (P) | |
|---|---|---|---|---|---|
| Mean age | 39.73 | 43.33 | 43.40 | 48.70 | 0.07 |
| Median age | 41.00 | 42.00 | 41.00 | 48.00 | 0.07 |
| Reproductive status | |||||
| Reproductive | 64.00% | 55.58% | 68.18% | 45.00% | NA |
| Premenopausal | 8.00% | 11.11% | 4.55% | 10.00% | NA |
| Menopausal | 28.00% | 11.11% | 27.27% | 25.00% | NA |
| Postmenopausal | 0.00% | 22.2% | 0.00% | 20.00% | NA |
| Mean age at menarche | 13.92 | 14.44 | 14.05 | 13.80 | 0.84 |
| Fertility rate | |||||
| 0 children | 12.00% | 11.11% | 18.18% | 25.00% | NA |
| 1–2 children | 56.00% | 77.78% | 54.55% | 45.00% | NA |
| >2 children | 32.00% | 11.11% | 27.27% | 30.00% | NA |
| Mean number of children | 1.84 | 2.22 | 1.95 | 1.85 | 0.98 |
| Cancer location | |||||
| Left breast | no cancer | 33.33% | no cancer | 45.00% | NA |
| Right breast | no cancer | 55.56% | no cancer | 45.00% | NA |
| Both breasts | no cancer | 11.11% | no cancer | 10.00% | NA |
| Cancer type | |||||
| Ductal | 0.0% | 100.00% | 0.0% | 100.00% | NA |
| Lobular | 0.0% | 0% | 0.0% | 0.0% | NA |
| NZ (n = 25) | NC (n = 9) | PZ (n = 22) | PC (n = 20) | |
|---|---|---|---|---|
| pH | 7.20 (7.62–6.61) | 7.21 (7.72–6.80) | 7.30 (7.83–6.84) | 7.10 (7.80–5.98) |
| DMFT | 5.0 (10.0–3.7) | 4.7 (6.5–2.5) | 5.5 (10.00–2.8) | 4.2 (6.9–1.7) |
| Pl.I | 0.25 (3.33–0.00) | 0.30 (2.60–0.00) | 0.43 (2.60–0.00) | 0.49 (5.55–0.00) |
| SBC | 6.57 (9.37–3.52) | 7.30 (15.00–1.87) | 6.44 (20.00–2.14) | 6.75 (14.28–2.00) |
| UWS flow rate | 0.27 (0.61–0.20) | 0.33 (0.55–0.20) | 0.27 (0.40–0.20) | 0.33 (0.33–0.13) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawczuk, B.; Maciejczyk, M.; Sawczuk-Siemieniuk, M.; Posmyk, R.; Zalewska, A.; Car, H. Salivary Gland Function, Antioxidant Defence and Oxidative Damage in the Saliva of Patients with Breast Cancer: Does the BRCA1 Mutation Disturb the Salivary Redox Profile? Cancers 2019, 11, 1501. https://doi.org/10.3390/cancers11101501
Sawczuk B, Maciejczyk M, Sawczuk-Siemieniuk M, Posmyk R, Zalewska A, Car H. Salivary Gland Function, Antioxidant Defence and Oxidative Damage in the Saliva of Patients with Breast Cancer: Does the BRCA1 Mutation Disturb the Salivary Redox Profile? Cancers. 2019; 11(10):1501. https://doi.org/10.3390/cancers11101501
Chicago/Turabian StyleSawczuk, Beata, Mateusz Maciejczyk, Magdalena Sawczuk-Siemieniuk, Renata Posmyk, Anna Zalewska, and Halina Car. 2019. "Salivary Gland Function, Antioxidant Defence and Oxidative Damage in the Saliva of Patients with Breast Cancer: Does the BRCA1 Mutation Disturb the Salivary Redox Profile?" Cancers 11, no. 10: 1501. https://doi.org/10.3390/cancers11101501
APA StyleSawczuk, B., Maciejczyk, M., Sawczuk-Siemieniuk, M., Posmyk, R., Zalewska, A., & Car, H. (2019). Salivary Gland Function, Antioxidant Defence and Oxidative Damage in the Saliva of Patients with Breast Cancer: Does the BRCA1 Mutation Disturb the Salivary Redox Profile? Cancers, 11(10), 1501. https://doi.org/10.3390/cancers11101501








