Radiation Pneumonitis: Old Problem, New Tricks
Abstract
1. Introduction
2. Pathogenesis and Clinical Manifestations
3. Grading
4. Factors Associated with Radiation Pneumonitis
4.1. Patient Related Factors
4.2. Treatment Related Factors
4.2.1. Chemotherapy
4.2.2. Immunotherapy
4.2.3. Surgery
4.2.4. Radiation Therapy
Dosimetric Correlates
Treatment Technique: 3D vs. IMRT
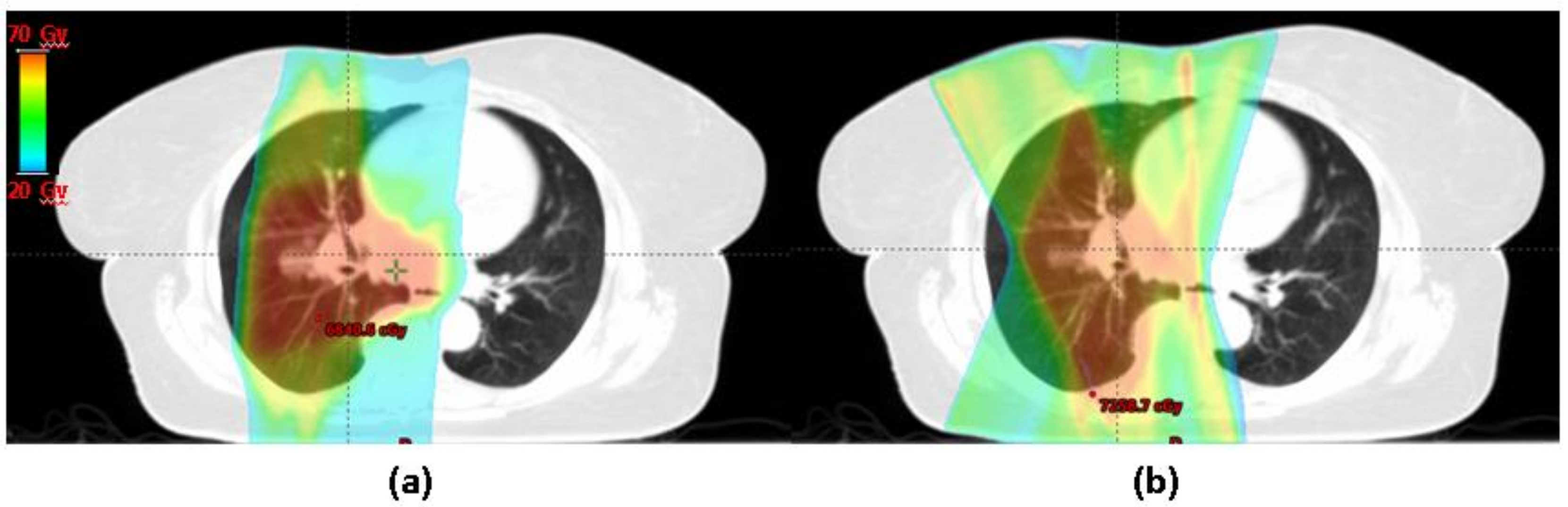
Treatment Modality: Protons vs. Photons
5. New Frontiers
5.1. Using 4D CT for Functional Avoidance Planning
5.2. Imaging Based Biomarkers: Pre-Treatment FDG
5.3. NTCP Modeling for Risk Assessment
6. Management of RP: Targets and Therapies
6.1. Therapies Targeting Free Radical Production
6.2. Targeting Recruitment of Inflammatory Cells
6.3. Targeting Cytokine and Growth Factor Expression
6.4. Other Miscellaneous Targets
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Trott, K.R.; Herrmann, T.; Kasper, M. Target cells in radiation pneumopathy. Int. J. Radiat. Oncol. Biol. Phys. 2004, 58, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Wade, M.; Li, Y.-C.; Wahl, G.M. MDM2, MDMX and p53 in oncogenesis and cancer therapy. Nat. Rev. Cancer 2013, 13, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.J.; Wright, T.W.; Rubin, P.; Finkelstein, J.N. Alterations in the expression of chemokine mRNA levels in fibrosis-resistant and -sensitive mice after thoracic irradiation. Exp. Lung Res. 1998, 24, 321–337. [Google Scholar] [CrossRef] [PubMed]
- Hallahan, D.E.; Virudachalam, S. Ionizing radiation mediates expression of cell adhesion molecules in distinct histological patterns within the lung. Cancer Res. 1997, 57, 2096–2099. [Google Scholar] [PubMed]
- Moore, A.H.; Olschowka, J.A.; Williams, J.P.; Paige, S.L.; O’Banion, M.K. Radiation-induced edema is dependent on cyclooxygenase 2 activity in mouse brain. Radiat. Res. 2004, 161, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Graves, P.R.; Siddiqui, F.; Anscher, M.S.; Movsas, B. Radiation pulmonary toxicity: From mechanisms to management. Semin. Radiat. Oncol. 2010, 20, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, G.; Lock, M.; D’Souza, D.; Yu, E.; Van Dyk, J. Prediction of radiation pneumonitis by dose-volume histogram parameters in lung cancer—A systematic review. Radiother. Oncol. 2004, 71, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Palma, D.A.; Senan, S.; Tsujino, K.; Barriger, R.B.; Rengan, R.; Moreno, M.; Jeffrey, D.; Kim, T.H.; Ramella, S.; Marks, L.B.; et al. Predicting Radiation Pneumonitis after Chemoradiotherapy for Lung Cancer: An International Individual Patient Data Meta- analysis. Int. J. Radiat. Oncol. 2013, 85, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Borst, G.R.; De Jaeger, K.; Belderbos, J.S.A.; Burgers, S.A.; Lebesque, J. V Pulmonary function changes after radiotherapy in non-small-cell lung cancer patients with long-term disease-free survival. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Mehta, V. Radiation pneumonitis and pulmonary fibrosis in non-small-cell lung cancer: Pulmonary function, prediction, and prevention. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 5–24. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.L.; Zhou, S.M.; Barrier, R.C., Jr.; Shafman, T.; Folz, R.J.; Clough, R.W.; Marks, L.B. Long-term changes in pulmonary function tests after definitive radiotherapy for lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2003, 56, 611–615. [Google Scholar] [CrossRef]
- De Jaeger, K.; Seppenwoolde, Y.; Boersma, L.J.; Muller, S.H.; Baas, P.; Belderbos, J.S.A.; Lebesque, J.V. Pulmonary function following high-dose radiotherapy of non-small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 1331–1340. [Google Scholar] [CrossRef]
- National Institute of Cancer. Common Terminology Criteria for Adverse Events (CTCAE). Available online: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_40 (accessed on 5 April 2018).
- Cox, J.D.; Stetz, J.; Pajak, T.F. Toxicity criteria of the radiation therapy oncology group (RTOG) and the european organization for research and treatment of cancer (EORTC). Int. J. Radiat. Oncol. Biol. Phys. 1995, 31, 1341–1346. [Google Scholar] [CrossRef]
- Green, S.; Weiss, G.R. Southwest Oncology Group standard response criteria, endpoint definitions and toxicity criteria. Investig. New Drugs 1992, 10, 239–253. [Google Scholar] [CrossRef]
- Oken, M.; Creech, R.; Tormey, D.; Horton, J.; Davis, T.; McFadden, E.; Carbone, P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–656. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Handbook for Reporting Results of Cancer Treatment; WHO: Geneva, Switzerland, 1979. [Google Scholar]
- Vogelius, I.R.; Bentzen, I.S. A literature-based meta-analysis of clinical risk factors for development of radiation induced pneumonitis. Anta Oncol. 2013, 51, 975–983. [Google Scholar] [CrossRef]
- Bjermer, L.; Cai, Y.; Nilsson, K.; Hellstrom, S.; Henriksson, R. Tobacco smoke exposure suppresses radiation-induced inflammation in the lung: A study of bronchoalveolar lavage and ultrastructural morphology in the rat. Eur. Respir. J. 1993, 6, 1173–1180. [Google Scholar] [PubMed]
- Laviolette, M.; Coulombe, R.; Picard, S.; Braquet, P.; Borgeat, P. Decreased leukotriene B4 synthesis in smokers’ alveolar macrophages in vitro. J. Clin. Investig. 1986, 77, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Schiller, J.H.; Gazdar, A.F. Lung cancer in never smokers—A different disease. Nat. Rev. Cancer 2007, 7, 778–790. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Kunieda, E.; Ohashi, T.; Aoki, Y.; Oku, Y.; Enomoto, T.; Nomura, K.; Sugiura, M. Severe COPD is correlated with mild radiation pneumonitis following stereotactic body radiotherapy. Chest 2012, 141, 858–866. [Google Scholar] [CrossRef] [PubMed]
- Bahig, H.; Filion, E.; Vu, T.; Chalaoui, J.; Lambert, L.; Roberge, D.; Gagnon, M.; Fortin, B.; Béliveau-Nadeau, D.; Mathieu, D.; et al. Severe radiation pneumonitis after lung stereotactic ablative radiation therapy in patients with interstitial lung disease. Pract. Radiat. Oncol. 2016, 6, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Ozawa, Y.; Abe, T.; Omae, M.; Matsui, T.; Kato, M.; Hasegawa, H.; Enomoto, Y.; Ishihara, T.; Inui, N.; Yamada, K.; et al. Impact of preexisting interstitial lung disease on acute, extensive radiation pneumonitis: Retrospective analysis of patients with lung cancer. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Ohguri, T.; Ide, S.; Aoki, T.; Imada, H.; Yahara, K.; Narisada, H.; Korogi, Y. Stereotactic body radiotherapy for lung tumors in patients with subclinical interstitial lung disease: The potential risk of extensive radiation pneumonitis. Lung Cancer 2013, 82, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, S.; Ohguri, T.; Matsuki, Y.; Yahara, K.; Oki, H.; Imada, H.; Narisada, H.; Korogi, Y. Radiotherapy for thoracic tumors: Association between subclinical interstitial lung disease and fatal radiation pneumonitis. Int. J. Clin. Oncol. 2015, 20, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Curran, W.J.; Paulus, R.; Langer, C.J.; Komaki, R.; Lee, J.S.; Hauser, S.; Movsas, B.; Wasserman, T.; Rosenthal, S.A.; Gore, E.; et al. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: Randomized phase III trial RTOG 9410. J. Natl. Cancer Inst. 2011, 103, 1452–1460. [Google Scholar] [CrossRef] [PubMed]
- Onishi, H.; Kuriyama, K.; Yamaguchi, M.; Komiyama, T.; Tanaka, S.; Araki, T.; Nishikawa, K.; Ishihara, H. Concurrent two-dimensional radiotherapy and weekly docetaxel in the treatment of stage III non-small cell lung cancer: A good local response but no good survival due to radiation pneumonitis. Lung Cancer 2003, 40, 79–84. [Google Scholar] [CrossRef]
- Parashar, B.; Edwards, A.; Mehta, R.; Pasmantier, M.; Wernicke, A.G.; Sabbas, A.; Kerestez, R.S.; Nori, D.; Chao, K.S.C. Chemotherapy significantly increases the risk of radiation pneumonitis in radiation therapy of advanced lung cancer. Am. J. Clin. Oncol. 2011, 34, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Fehrenbacher, L.; Spira, A.; Ballinger, M.; Kowanetz, M.; Vansteenkiste, J.; Mazieres, J.; Park, K.; Smith, D.; Artal-Cortes, A.; Lewanski, C.; et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): A multicentre, open-label, phase 2 randomised controlled trial. Lancet 2016, 387, 1837–1846. [Google Scholar] [CrossRef]
- Borghaei, H.; Paz-Ares, L.; Horn, L.; Spigel, D.R.; Steins, M.; Ready, N.E.; Chow, L.Q.; Vokes, E.E.; Felip, E.; Holgado, E.; et al. Nivolumab versus docetaxel in advanced non-squamous non-small cell lung cancer. N. Engl. J. Med. 2015, 373, 1627–1639. [Google Scholar] [CrossRef] [PubMed]
- Brahmer, J.; Reckamp, K.L.; Baas, P.; Crinò, L.; Eberhardt, W.E.E.; Poddubskaya, E.; Antonia, S.; Pluzanski, A.; Vokes, E.E.; Holgado, E.; et al. Nivolumab versus docetaxel in advanced squamous-cell non–small-cell lung cancer. N. Engl. J. Med. 2015, 373, 123–135. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Yokoi, T.; Chiappori, A.; Lee, K.H.; de Wit, M.; et al. Durvalumab after Chemoradiotherapy in Stage III Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Delaunay, M.; Cadranel, J.; Lusque, A.; Meyer, N.; Gounaut, V.; Moro-Sibilot, D.; Michot, J.M.; Raimbourg, J.; Girard, N.; Guisier, F.; et al. Immune-checkpoint inhibitors associated with interstitial lung disease in cancer patients. Eur. Respir. J. 2017, 50. [Google Scholar] [CrossRef] [PubMed]
- Nishino, M.; Giobbie-Hurder, A.; Hatabu, H.; Ramaiya, N.H.; Hodi, F.S. Incidence of programmed cell death 1 inhibitor-related pneumonitis in patients with advanced cancer a systematic review and meta-analysis. JAMA Oncol. 2016, 2, 1607–1616. [Google Scholar] [CrossRef] [PubMed]
- Crequit, P.; Wislez, M.; Fleury Feith, J.; Rozensztajn, N.; Jabot, L.; Friard, S.; Lavole, A.; Gounant, V.; Fillon, J.; Antoine, M.; et al. Crizotinib associated with ground-glass opacity predominant pattern interstitial lung disease: A retrospective observational cohort study with a systematic literature review. J. Thorac. Oncol. 2015, 10, 1148–1155. [Google Scholar] [CrossRef] [PubMed]
- Hochstrasser, A.; Benz, G.; Joerger, M.; Templeton, A.; Brutsche, M.; Frh, M. Interstitial pneumonitis after treatment with pemetrexed: A rare event? Chemotherapy 2012, 58, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Roychowdhury, D.F.; Cassidy, C.A.; Peterson, P.; Arning, M. A report on serious pulmonary toxicity associated with gemcitabine-based therapy. Investig. New Drugs 2002, 20, 311–315. [Google Scholar] [CrossRef]
- Grande, C.; Villanueva, M.J.; Huidobro, G.; Casal, J. Docetaxel-induced interstitial pneumonitis following non-small-cell lung cancer treatment. Clin. Transl. Oncol. 2007, 9, 578–581. [Google Scholar] [CrossRef] [PubMed]
- Konishi, J.; Yamazaki, K.; Kinoshita, I.; Isobe, H.; Ogura, S.; Sekine, S.; Ishida, T.; Takashima, R.; Nakadate, M.; Nishikawa, S.; et al. Analysis of the response and toxicity to gefitinib of non-small cell lung cancer. Anticancer Res. 2005, 25, 435–441. [Google Scholar] [PubMed]
- Liu, V.; White, D.A.; Zakowski, M.F.; Travis, W.; Kris, M.G.; Ginsberg, M.S.; Miller, V.A.; Azzoli, C.G. Pulmonary toxicity associated with erlotinib. Chest 2007, 132, 1042–1044. [Google Scholar] [CrossRef] [PubMed]
- Twyman-Saint Victor, C.; Rech, A.J.; Maity, A.; Rengan, R.; Pauken, K.E.; Stelekati, E.; Benci, J.L.; Xu, B.; Dada, H.; Odorizzi, P.M.; et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 2015, 520, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Shaverdian, N.; Lisberg, A.E.; Bornazyan, K.; Veruttipong, D.; Goldman, J.W.; Formenti, S.C.; Garon, E.B.; Lee, P. Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: A secondary analysis of the KEYNOTE-001 phase I trial. Lancet Oncol. 2017, 18, 895–903. [Google Scholar] [CrossRef]
- Kocak, Z.; Yu, X.; Zhou, S.M.; D’Amico, A.; Hollis, D.; Kahn, D.; Tisch, A.; Shafman, T.D.; Marks, L.B. The impact of pre-radiotherapy surgery on radiation-induced lung injury. Clin. Oncol. 2005, 17, 210–216. [Google Scholar] [CrossRef]
- Albain, K.S.; Swann, R.S.; Rusch, V.W.; Turrisi, A.T.; Shepherd, F.A.; Smith, C.; Chen, Y.; Livingston, R.B.; Feins, R.H.; Gandara, D.R.; et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: A phase III randomised controlled trial. Lancet 2009, 374, 379–386. [Google Scholar] [CrossRef]
- Van Luijk, P.; Faber, H.; Meertens, H.; Schippers, J.M.; Langendijk, J.A.; Brandenburg, S.; Kampinga, H.H.; Coppes, R.P. The impact of heart irradiation on dose-volume effects in the rat lung. Int. J. Radiat. Oncol. Biol. Phys. 2007, 69, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Ghobadi, G.; Van Der Veen, S.; Bartelds, B.; De Boer, R.A.; Dickinson, M.G.; De Jong, J.R.; Faber, H.; Niemantsverdriet, M.; Brandenburg, S.; Berger, R.M.F.; et al. Physiological interaction of heart and lung in thoracic irradiation. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84. [Google Scholar] [CrossRef] [PubMed]
- Huang, E.X.; Hope, A.J.; Lindsay, P.E.; Trovo, M.; El Naqa, I.; Deasy, J.O.; Bradley, J.D. Heart irradiation as a risk factor for radiation pneumonitis. Acta Oncol. 2011, 50, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Wijsman, R.; Dankers, F.J.W.M.; Troost, E.G.C.; Hoffmann, A.L.; van der Heijden, E.H.F.M.; de Geus-Oei, L.F.; Bussink, J. Inclusion of incidental radiation dose to the cardiac atria and ventricles does not improve the prediction of radiation pneumonitis in advanced-stage non-small cell lung cancer patients treated with intensity modulated radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Yom, S.S.; Liao, Z.; Liu, H.H.; Tucker, S.L.; Hu, C.S.; Wei, X.; Wang, X.; Wang, S.; Mohan, R.; Cox, J.D.; et al. Initial evaluation of treatment-related pneumonitis in advanced-stage non-dmall-cell lung cancer patients treated with concurrent chemotherapy and intensity-modulated radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2007, 68, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.W.C.; Kwong, D.L.W.; Sham, J.S.T. Target dose conformity in 3-dimensional conformal radiotherapy and intensity modulated radiotherapy. Radiother. Oncol. 2004, 71, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.; Ackerson, B.; Gu, L.; Kelsey, C.R. Dosimetric advantages of intensity modulated radiation therapy in locally advanced lung cancer. Adv. Radiat. Oncol. 2017, 2, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Chun, S.G.; Hu, C.; Choy, H.; Komaki, R.U.; Timmerman, R.D.; Schild, S.E.; Bogart, J.A.; Dobelbower, M.C.; Bosch, W.; Galvin, J.M.; et al. Impact of intensity-modulated radiation therapy technique for locally advanced non-small-cell lung cancer: A secondary analysis of the NRG oncology RTOG 0617 randomized clinical trial. J. Clin. Oncol. 2017, 35, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Berman, A.T.; Teo, B.-K.K.; Dolney, D.; Swisher-McClure, S.; Shahnazi, K.; Both, S.; Rengan, R. An in-silico comparison of proton beam and IMRT for postoperative radiotherapy in completely resected stage IIIA non-small cell lung cancer. Radiat. Oncol. 2013, 8, 144. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, Y.; Pan, X.; Xiaoqiang, L.; Mohan, R.; Komaki, R.; Cox, J.D.; Chang, J.Y. Intensity-modulated proton therapy reduces the dose to normal tissue compared with intensity-modulated radiation therapy or passive scattering proton therapy and enables individualized radical radiotherapy for extensive stage IIIB non-small-cell lung canc. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 357–366. [Google Scholar] [CrossRef] [PubMed]
- Higgins, K.A.; O’Connell, K.; Liu, Y.; Gillespie, T.W.; McDonald, M.W.; Pillai, R.N.; Patel, K.R.; Patel, P.R.; Robinson, C.G.; Simone, C.B.; et al. National cancer database analysis of proton versus photon radiation therapy in non-small cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Liao, Z.; Lee, J.J.; Komaki, R.; Gomez, D.R.; O’Reilly, M.S.; Fossella, F.V.; Blumenschein, G.R.; Heymach, J.V.; Vaporciyan, A.A.; Swisher, S.G.; et al. Bayesian adaptive randomization trial of passive scattering proton therapy and intensity-modulated photon radiotherapy for locally advanced non-small-cell lung cancer. J. Clin. Oncol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Vinogradskiy, Y.; Gan, G.; Castillo, R.; Castillo, E.; Martel, M.; Guerrero, T.; Miften, M. Quantitative assessment of lung function in stage I and stage III lung radiation therapy patients using 4DCT-based ventilation imaging. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, S754. [Google Scholar] [CrossRef]
- Vinogradskiy, Y.; Schubert, L.; Diot, Q.; Waxweiller, T.; Koo, P.; Castillo, R.; Castillo, E.; Guerrero, T.; Rusthoven, C.; Gaspar, L.; et al. Regional lung function profiles of stage i and III lung cancer patients: An evaluation for functional avoidance radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2016, 95, 1273–1280. [Google Scholar] [CrossRef] [PubMed]
- Marks, L.B.; Spencer, D.P.; Bentel, G.C.; Ray, S.K.; Sherouse, G.W.; Sontag, M.R.; Edward Coleman, R.; Jaszczak, R.J.; Turkington, T.G.; Tapson, V.; et al. The utility of SPECT lung perfusion scans in minimizing and assessing the physiologic consequences of thoracic irradiation. Int. J. Radiat. Oncol. Biol. Phys. 1993, 26, 659–668. [Google Scholar] [CrossRef]
- Christian, J.A.; Partridge, M.; Nioutsikou, E.; Cook, G.; McNair, H.A.; Cronin, B.; Courbon, F.; Bedford, J.L.; Brada, M. The incorporation of SPECT functional lung imaging into inverse radiotherapy planning for non-small cell lung cancer. Radiother. Oncol. 2005, 77, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Castillo, R.; Castillo, E.; Martinez, J.; Guerrero, T. TU-B-204B-04: Ventilation from Four Dimensional Computed Tomography: Density versus Jacobian Methods. Med. Phys. 2010, 37, 377. [Google Scholar] [CrossRef]
- Bates, E.L.; Bragg, C.M.; Wild, J.M.; Hatton, M.Q.F.; Ireland, R.H. Functional image-based radiotherapy planning for non-small cell lung cancer: A simulation study. Radiother. Oncol. 2009, 93, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Brennan, D.; Schubert, L.; Diot, Q.; Castillo, R.; Castillo, E.; Guerrero, T.; Martel, M.K.; Linderman, D.; Gaspar, L.E.; Miften, M.; et al. Clinical validation of 4-dimensional computed tomography ventilation with pulmonary function test data. Int. J. Radiat. Oncol. Biol. Phys. 2015, 92, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Faught, A.M.; Miyasaka, Y.; Kadoya, N.; Castillo, R.; Castillo, E.; Vinogradskiy, Y.; Yamamoto, T. Evaluating the toxicity reduction with computed tomographic ventilation functional avoidance radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Kabus, S.; Bal, M.; Keall, P.; Benedict, S.; Daly, M. The first patient treatment of computed tomography ventilation functional image-guided radiotherapy for lung cancer. Radiother. Oncol. 2016, 118, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Waxweiler, T.; Schubert, L.; Diot, Q.; Faught, A.; Stuhr, K.; Castillo, R.; Castillo, E.; Guerrero, T.; Rusthoven, C.; Gaspar, L.; et al. A complete 4DCT-ventilation functional avoidance virtual trial: Developing strategies for prospective clinical trials. J. Appl. Clin. Med. Phys. 2017, 18, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Petit, S.F.; Van Elmpt, W.J.C.; Oberije, C.J.G.; Vegt, E.; Dingemans, A.M.C.; Lambin, P.; Dekker, A.L.A.J.; De Ruysscher, D. [18F]fluorodeoxyglucose uptake patterns in lung before radiotherapy identify areas more susceptible to radiation-induced lung toxicity in non-small-cell lung cancer patients. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Castillo, R.; Pham, N.; Ansari, S.; Meshkov, D.; Castillo, S.; Li, M.; Olanrewaju, A.; Hobbs, B.; Castillo, E.; Guerrero, T. Pre-radiotherapy FDG PET predicts radiation pneumonitis in lung cancer. Radiat. Oncol. 2014, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, A.A.; Binkley, M.S.; Rigdon, J.; Carter, J.N.; Aggarwal, S.; Dudley, S.A.; Qian, Y.; Kumar, K.A.; Hara, W.Y.; Gensheimer, M.; et al. Pre-treatment non-target lung FDG-PET uptake predicts symptomatic radiation pneumonitis following Stereotactic Ablative Radiotherapy (SABR) pre-treatment non-target lung FDG-PET uptake predicts radiation pneumonitis after SABR. Radiother. Oncol. 2016, 119, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Anthony, G.J.; Cunliffe, A.; Castillo, R.; Pham, N.; Guerrero, T.; Armato, S.G.; Al-Hallaq, H.A. Incorporation of pre-therapy 18F-FDG uptake data with CT texture features into a radiomics model for radiation pneumonitis diagnosis. Med. Phys. 2017, 44, 3686–3694. [Google Scholar] [CrossRef] [PubMed]
- Marks, L.; Bentzen, S.; Deasy, J.; Kong, F. Radiation dose volume effects in the lung. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Appelt, A.L.; Vogelius, I.R.; Farr, K.P.; Khalil, A.A.; Bentzen, S.M. Towards individualized dose constraints: Adjusting the QUANTEC radiation pneumonitis model for clinical risk factors. Acta Oncol. 2014, 53, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Tucker, S.L.; Liu, H.H.; Liao, Z.; Wei, X.; Wang, S.; Jin, H.; Komaki, R.; Martel, M.K.; Mohan, R. Analysis of radiation pneumonitis risk using a generalized lyman model. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 568–574. [Google Scholar] [CrossRef] [PubMed]
- Tucker, S.L.; Li, M.; Xu, T.; Gomez, D.; Yuan, X.; Yu, J.; Liu, Z.; Yin, M.; Guan, X.; Wang, L.E.; et al. Incorporating single-nucleotide polymorphisms into the lyman model to improve prediction of radiation pneumonitis. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Langendijk, J.A.; Lambin, P.; de Ruysscher, D.; Widder, J.; Bos, M.; Verheij, M. Selection of patients for radiotherapy with protons aiming at reduction of side effects: The model-based approach. Radiother. Oncol. 2013, 107, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Antonadou, D.; Petridis, A.; Synodinou, M.; Throuvalas, N.; Bolanos, N.; Veslemes, M.; Sagriotis, A. Amifostine reduces radiochemotherapy-induced toxicities in patients with locally advanced non-small cell lung cancer. Semin. Oncol. 2003, 30, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Movsas, B.; Scott, C.; Langer, C.; Werner-Wasik, M.; Nicolaou, N.; Komaki, R.; Machtay, M.; Smith, C.; Axelrod, R.; Sarna, L.; et al. Randomized trial of amifostine in locally advanced non-small-cell lung cancer patients receiving chemotherapy and hyperfractionated radiation: Radiation therapy oncology group trial 98-01. J. Clin. Oncol. 2005, 23, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Greenberger, J.S.; Epperly, M.W. Antioxidant gene therapeutic approaches to normal tissue radioprotection and tumor radiosensitization. In Vivo 2007, 21, 141–146. [Google Scholar] [PubMed]
- Epperly, M.W.; Epstein, C.J.; Travis, E.L.; Greenberger, J.S. Decreased pulmonary radiation resistance of manganese superoxide dismutase (MnSOD)-deficient mice is corrected by human manganese superoxide dismutase-Plasmid/Liposome (SOD2-PL) intratracheal gene therapy. Radiat. Res. 2000, 154, 365–374. [Google Scholar] [CrossRef]
- Gauter-Fleckenstein, B.; Fleckenstein, K.; Owzar, K.; Jiang, C.; Batinic-Haberle, I.; Vujaskovic, Z. Comparison of two Mn porphyrin-based mimics of superoxide dismutase in pulmonary radioprotection. Free Radic. Biol. Med. 2008, 44, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Delanian, S.; Baillet, F.; Huart, J.; Lefaix, J.L.; Maulard, C.; Housset, M. Successful treatment of radiation-induced fibrosis using liposomal Cu/Zn superoxide dismutase: Clinical trial. Radiother. Oncol. 1994, 32, 12–20. [Google Scholar] [CrossRef]
- Christofidou-Solomidou, M.; Tyagi, S.; Tan, K.S.; Hagan, S.; Pietrofesa, R.; Dukes, F.; Arguiri, E.; Heitjan, D.F.; Solomides, C.C.; Cengel, K.A. Dietary flaxseed administered post thoracic radiation treatment improves survival and mitigates radiation-induced pneumonopathy in mice. BMC Cancer 2011, 11, 269. [Google Scholar] [CrossRef] [PubMed]
- Calveley, V.L.; Jelveh, S.; Langan, A.; Mahmood, J.; Yeung, I.W.T.; Van Dyk, J.; Hill, R.P. Genistein Can Mitigate the Effect of Radiation on Rat Lung Tissue. Radiat. Res. 2010, 173, 602–611. [Google Scholar] [CrossRef] [PubMed]
- Day, R.M.; Barshishat-Kupper, M.; Mog, S.R.; McCart, E.A.; Prasanna, P.G.S.; Davis, T.A.; Landauer, M.R. Genistein protects against biomarkers of delayed lung sequelae in mice surviving high-dose total body irradiation. J. Radiat. Res. 2008, 49, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Gore, E. Celecoxib and radiation therapy in non-small-cell lung cancer. Oncology 2004, 18, 10–14. [Google Scholar] [PubMed]
- Mason, R.P.; Walter, M.F.; Day, C.A.; Jacob, R.F. Active metabolite of atorvastatin inhibits membrane cholesterol domain formation by an antioxidant mechanism. J. Biol. Chem. 2006, 281, 9337–9345. [Google Scholar] [CrossRef] [PubMed]
- Mathew, B.; Huang, Y.; Jacobson, J.R.; Berdyshev, E.; Gerhold, L.M.; Wang, T.; Moreno-Vinasco, L.; Lang, G.; Zhao, Y.; Chen, C.T.; et al. Simvastatin attenuates radiation-induced murine lung injury and dysregulated lung gene expression. Am. J. Respir. Cell Mol. Biol. 2011, 44, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Wedlake, L.J.; Silia, F.; Benton, B.; Lalji, A.; Thomas, K.; Dearnaley, D.P.; Blake, P.; Tait, D.; Khoo, V.S.; Andreyev, H.J.N. Evaluating the efficacy of statins and ACE-inhibitors in reducing gastrointestinal toxicity in patients receiving radiotherapy for pelvic malignancies. Eur. J. Cancer 2012, 48, 2117–2124. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.N.; Johnston, C.; Barrett, T.; Oberdörster, G. Particulate-cell interactions and pulmonary cytokine expression. Environ. Health Perspect. 1997, 105, 1179–1182. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.H.; Jung, S.M.; Tsao, T.C.; Wu, C.J.; Lee, C.Y.; Chen, F.H.; Hsu, C.H.; McBride, W.H.; Chiang, C.S. Bronchoalveolar lavage and interstitial cells have different roles in radiation-induced lung injury. Int. J. Radiat. Biol. 2003, 79, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Hyrien, O.; Williams, J.; Okunieff, P.; Smudzin, T.; Rubin, P. Interleukin (IL)-1A and IL-6: Applications to the predictive diagnostic testing of radiation pneumonitis. Int. J. Radiat. Oncol. Biol. Phys. 2005, 62, 60–266. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Liao, Z.; Liu, Z.; Wang, L.-E.; Tucker, S.L.; Mao, L.; Wang, X.S.; Martel, M.; Komaki, R.; Cox, J.D.; et al. Single Nucleotide Polymorphism at rs1982073:T869C of the TGFβ1 gene is associated with the risk of radiation pneumonitis in patients with non-small-cell lung cancer treated with definitive radiotherapy. J. Clin. Oncol. 2009, 27, 3370–3378. [Google Scholar] [CrossRef] [PubMed]
- Anscher, M.S.; Thrasher, B.; Zgonjanin, L.; Rabbani, Z.N.; Corbley, M.J.; Fu, K.; Sun, L.; Lee, W.-C.; Ling, L.E.; Vujaskovic, Z. Small molecular inhibitor of transforming growth factor-beta protects against development of radiation-induced lung injury. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Matěj, R.; Housa, D.; Poučková, P.; Zadinová, M.; Olejár, T. Radiation-induced production of PAR-1 and TGF-beta 1 mRNA in lung of C57Bl6 and C3H murine strains and influence of pharmacoprophylaxis by ACE inhibitors. Pathol. Res. Pract. 2007, 203, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.N.; Zhang, R.; Fish, B.L.; Semenenko, V.A.; Li, X.A.; Moulder, J.E.; Jacobs, E.R.; Medhora, M. Renin-angiotensin system suppression mitigates experimental radiation pneumonitis. Int. J. Radiat. Oncol. Biol. Phys. 2009, 75, 1528–1536. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.P.; Bedi, M.; Irving, A.A.; Jacobs, E.; Tomic, R.; Klein, J.; Lawton, C.A.; Moulder, J.E. Mitigation of late renal and pulmonary injury after hematopoietic stem cell transplantation. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Chopra, M.; Scott, N.; McMurray, J.; McLay, J.; Bridges, A.; Smith, W.E.; Belch, J.J. Captopril: A free radical scavenger. Br. J. Clin. Pharmacol. 1989, 27, 396–399. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liao, Z.; Zhuang, Y.; Xu, T.; Nguyen, Q.N.; Levy, L.B.; O’Reilly, M.; Gold, K.A.; Gomez, D.R. Do Angiotensin-converting enzyme inhibitors reduce the risk of symptomatic radiation pneumonitis in patients with non-small cell lung cancer after definitive radiation therapy? Analysis of a single-institution database. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
| Criteria | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 |
|---|---|---|---|---|---|
| CTCAE v4.0 | Asymptomatic | Symptomatic; Required medical intervention; Limits ADLs | Severe symptoms; Oxygen indicated; Impairs ADLs | Life threatening respiratory dysfunction | Death |
| RTOG | Mild symptoms | Persistent symptoms requiring symptomatic treatment | Severe symptoms, possibly requiring intermittent O2 or steroids | Severe symptoms requiring continuous O2 or assisted ventilation | - |
| EORTC (LENT-SOMA) | Asymptomatic or mild symptoms; slight imaging changes | Moderate symptoms; patchy imaging changes | Severe symptoms; increased density imaging changes | Severe symptoms requiring continuous O2 or assisted ventilation | Death |
| SWOG | Imaging changes; mild symptoms without steroids | Symptoms requiring steroids or tap for effusion | Symptoms requiring oxygen | Symptoms requiring assisted ventilation | Death |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jain, V.; Berman, A.T. Radiation Pneumonitis: Old Problem, New Tricks. Cancers 2018, 10, 222. https://doi.org/10.3390/cancers10070222
Jain V, Berman AT. Radiation Pneumonitis: Old Problem, New Tricks. Cancers. 2018; 10(7):222. https://doi.org/10.3390/cancers10070222
Chicago/Turabian StyleJain, Varsha, and Abigail T. Berman. 2018. "Radiation Pneumonitis: Old Problem, New Tricks" Cancers 10, no. 7: 222. https://doi.org/10.3390/cancers10070222
APA StyleJain, V., & Berman, A. T. (2018). Radiation Pneumonitis: Old Problem, New Tricks. Cancers, 10(7), 222. https://doi.org/10.3390/cancers10070222





