Applications of Laser Welding in Dentistry: A State-of-the-Art Review
Abstract
1. Introduction
2. State-of-the-Art of Laser Technology
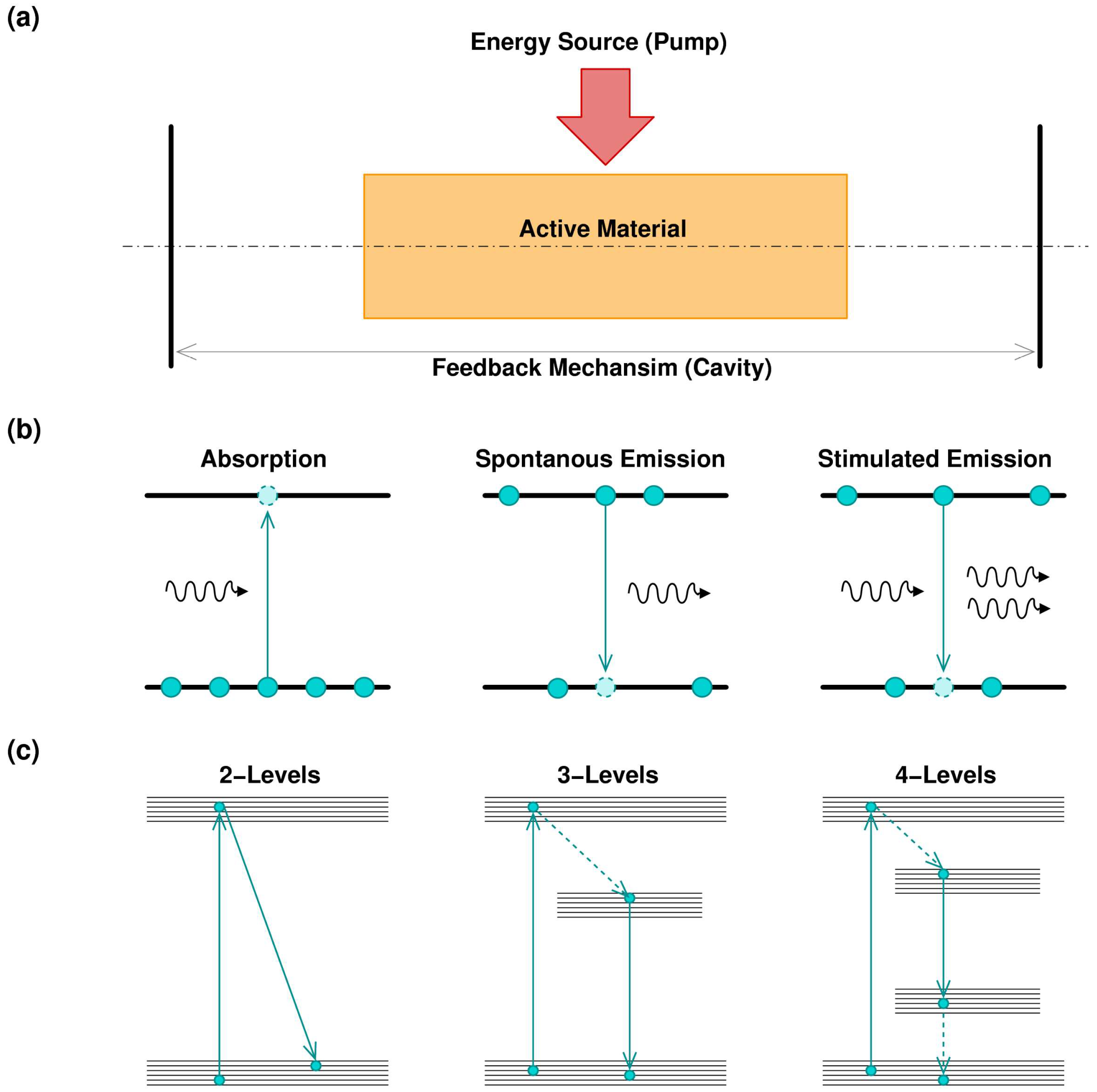
2.1. Principle of Laser
- Semiconductor lasers (diode laser): typically obtained using a p-n junction, pumping with an electrical current. Semiconductor laser are versatile and can be found in several wavelengths covering the visible spectrum, the near-infrared (IR) and the mid-IR. The emission power can vary from a few milliwatts to several watts (for industrial application). Pulsed operation can be easily achieved. In general, semiconductor lasers emit beams with poor quality; for this reason, it is common to use this kind of laser as a pump for other kinds of lasers that permits a better output quality.
- Gas lasers: these lasers are characterized by gaseous gain media. Pumping is obtained by electrical discharges. The emitted beam quality is very high. The main characteristic of gas lasers is to efficiently emit where the other types of lasers have a poor emission. As an example, CO2 laser can emit kilowatts of power at 10.6 µm, making this laser suitable for macro-machining operation, welding and cutting [24]. Another interesting example of gas laser is represented by excimer lasers, which can emit hundreds of watts of average power in pulsed operation, in the region of ultraviolet (UV) [25].
- Solid-state lasers: are lasers where the gain media are crystals or glasses, properly doped with rare earth or transition metal ions. Common media include: Nd:YAG, Nd:glass, Yb:YAG, Yb:glass, Ti:shapphire, Cr:YAG, Er:YAG, and Er:glass. Pumping is achieved by a discharge lamp. The diode pump is also possible to use. With typical emissions in the near-IR region, this kind of laser offers a large span of emission power, with a remarkable beam quality. Pulsed operation, with very short pulses, in case of Ti: sapphire laser, can be obtained.
- Fiber lasers: they are similar, regarding the principle of operation, to solid-state lasers. The doped area is located in the core of the fiber. Thanks to the fiber geometry, this kind of laser offers a better thermal dispersion and a unique possibility to operate in transversal single mode operation [26]. This permits achieving several kilowatts of emission maintaining higher beam quality [27]. Typically, Yb-doped and Yb/Eb-doped fiber lasers are used for industrial applications that require high precision machining. In medical applications, Tm-doped fiber lasers permit a better interaction with the soft tissues [28,29].
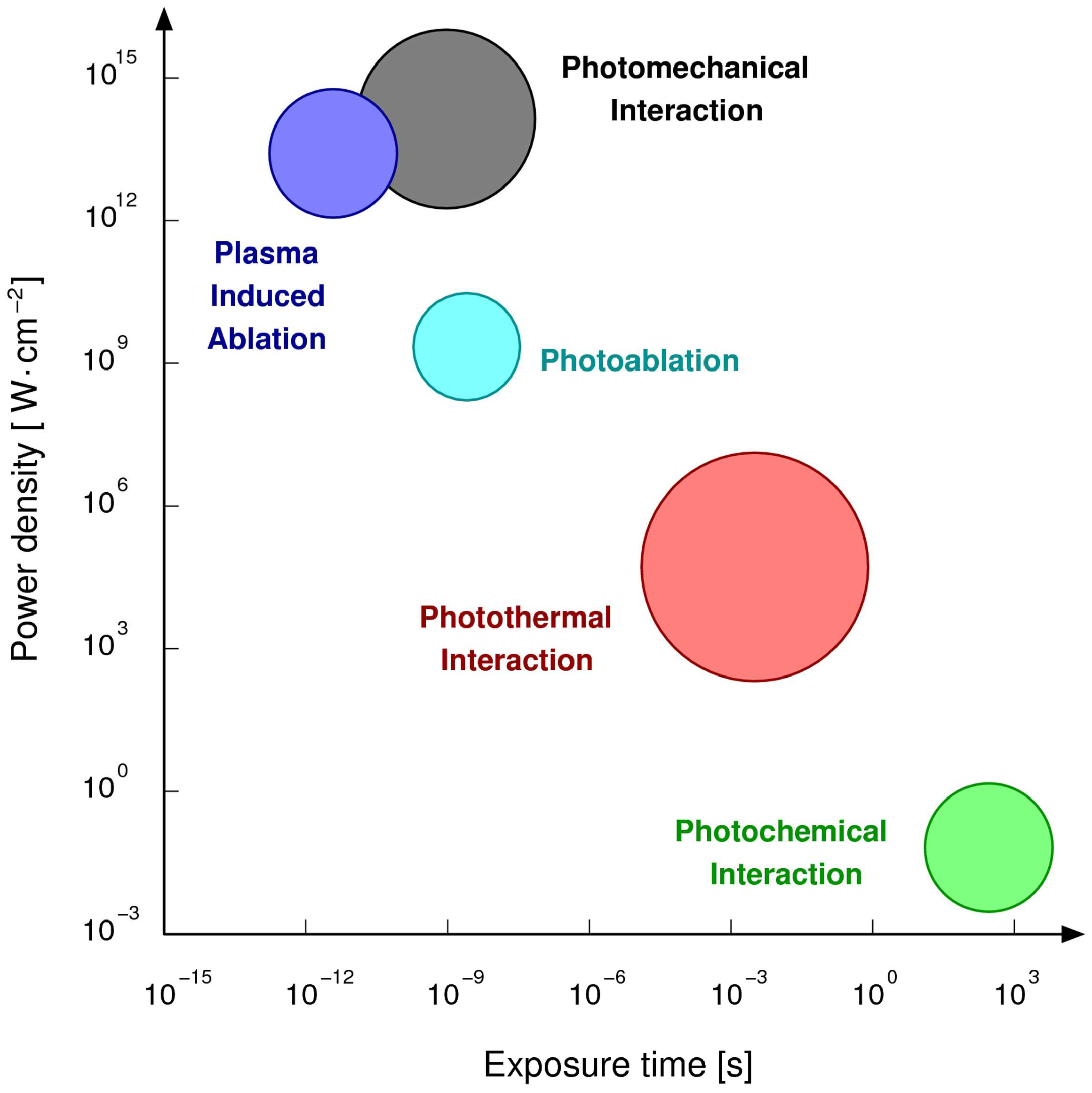
2.2. Laser Matter Interaction
2.3. Laser Welding Principle
2.4. Other Potential Application of Lasers in Dentistry
3. Types of Dental Alloys and Their Properties
3.1. Alloys for Crown and Bridge Work
3.2. Alloys for Orthodontics
3.3. Alloys for Implants
4. Laser Welding of Dental Alloys
5. Laser Welding Phenomena
6. Future Trends
7. Conclusions
Author Contributions
Conflicts of Interest
References
- Craig, R.G.; Welker, D.; Rothaut, J.; Krumbholz, K.G.; Stefan, K.P.; Dermann, K.; Rehberg, H.J.; Franz, G.; Lehmann, K.M.; Borchert, M. Dental Materials; Wiley Online Library: Hoboken, NJ, USA, 2000. [Google Scholar]
- Mosch, J.; Hoffmann, A.; Hopp, M. Lightening in a bottle-state of the art joining techniques in dental technologypart 1. Contin. Educ. 2004, 4, 110–119. [Google Scholar]
- Bertrand, C.; Poulon-Quintin, A. Proposals for optimization of laser welding in prosthetic dentistry. J. Prosthodont. 2010, 19, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.D.; Broughton, S.; Drangsholt, M. Oral lichen planus and dental materials: A case-control study. Contact Dermatitis 2003, 48, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Perfetti, G.; Maggiore, C.; Isidori, F. A case of leukoplakia from bimetallism in a single tooth. Attual. Dent. 1988, 4, 36. [Google Scholar] [PubMed]
- Johansson, B.I.; Stenman, E.; Bergman, M. Clinical registration of charge transfer between dental metallic materials in patients with disorders and/or discomfort allegedly caused by corrosion. Eur. J. Oral Sci. 1986, 94, 357–363. [Google Scholar] [CrossRef]
- Apotheker, H.; Nishimura, I.; Seerattan, C. Laser-welded vs soldered nonprecious alloy dental bridges: A comparative study. Lasers Surg. Med. 1984, 4, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Da Silveira-Júnior, C.B.D.; de Castro, M.G.; Davi, L.C.R.; das Neves, F.V.D.; Novais, V.R.; Simamoto-Júnior, P.C.Z. Welding techniques in dentistry. In Welding Processes; InTech: London, UK, 2012. [Google Scholar]
- Gordon, T.E.; Smith, D.L. Laser welding of prostheses—An initial report. J. Prosthet. Dent. 1970, 24, 472–476. [Google Scholar] [CrossRef]
- Solmi, R.; Martini, D.; Zanarini, M.; Penco, S.I.; Rimondini, L.; Carinci, P.; Borea, G.; Ruggeri, A. Interactions of fibroblasts with soldered and laser-welded joints. Biomaterials 2004, 25, 735–740. [Google Scholar] [CrossRef]
- Maiman, T.H. Stimulated optical radiation in ruby. In Essentials of Lasers; Elsevier: New York, NY, USA, 1960. [Google Scholar]
- Majumdar, J.D.; Manna, I. Laser processing of materials. Sadhana 2003, 28, 495–562. [Google Scholar] [CrossRef]
- Verma, S.K.; Maheshwari, S.; Singh, R.K.; Chaudhari, P.K. Laser in dentistry: An innovative tool in modern dental practice. Natl. J. Maxillofac. Surg. 2012, 3, 124. [Google Scholar] [CrossRef] [PubMed]
- Svelto, O. Principles of Lasers; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Molardi, C.; Yu, X.; Liang, H.; Zhang, Y.; Cucinotta, A.; Selleri, S. Modal analysis in 2D media with variable disorder. Opt. Express 2015, 23, 3681–3689. [Google Scholar] [CrossRef] [PubMed]
- Molardi, C.; Yu, X.; Liang, H.; Zhang, Y.; Qiu, C.-W.; Cucinotta, A.; Selleri, S. Analysis of mid-infrared lasing in active random media. Opt. Express 2015, 23, 12286–12292. [Google Scholar] [CrossRef] [PubMed]
- Moloney, J.V.; Hader, J.; Koch, S.W. Quantum design of semiconductor active materials: Laser and amplifier applications. Laser Photonics Rev. 2007, 1, 24–43. [Google Scholar] [CrossRef]
- Bennett, W.R. Background of an inversion: The first gas laser. IEEE J. Sel. Top. Quantum Electron. 2000, 6, 869–875. [Google Scholar] [CrossRef]
- Huber, G.; Kränkel, C.; Petermann, K. Solid-state lasers: Status and future. JOSA B 2010, 27, B93–B105. [Google Scholar] [CrossRef]
- Siegman, A.E. Lasers; University Science Books: Mill Valley, CA, USA, 1986; Volume 37, p. 208. [Google Scholar]
- Zayhowski, J.J. Q-switched operation of microchip lasers. Opt. Lett. 1991, 16, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Hargrove, L.; Fork, R.L.; Pollack, M. Locking of He–Ne laser modes induced by synchronous intracavity modulation. Appl. Phys. Lett. 1964, 5, 4–5. [Google Scholar] [CrossRef]
- Liu, X.; Du, D.; Mourou, G. Laser ablation and micromachining with ultrashort laser pulses. IEEE J. Quantum Electron. 1997, 33, 1706–1716. [Google Scholar] [CrossRef]
- Robinson, A.; Johnson, D. A carbon dioxide laser bibliography, 1964–1969. IEEE J. Quantum Electron. 1970, 6, 590–599. [Google Scholar] [CrossRef]
- Ewing, J. Excimer laser technology development. IEEE J. Sel. Top. Quantum Electron. 2000, 6, 1061–1071. [Google Scholar] [CrossRef]
- Molardi, C.; Poli, F.; Rosa, L.; Selleri, S.; Cucinotta, A. Mode discrimination criterion for effective differential amplification in Yb-doped fiber design for high power operation. Opt. Express 2017, 25, 29013–29025. [Google Scholar] [CrossRef]
- Jauregui, C.; Limpert, J.; Tünnermann, A. High-power fibre lasers. Nat. Photonics 2013, 7, 861. [Google Scholar] [CrossRef]
- Coscelli, E.; Molardi, C.; Cucinotta, A.; Selleri, S. Symmetry-free tm-doped photonic crystal fiber with enhanced mode area. IEEE J. Sel. Top. Quantum Electron. 2014, 20, 544–550. [Google Scholar] [CrossRef]
- Molardi, C.; Sun, B.; Yu, X.; Cucinotta, A.; Selleri, S. Polarization-maintaining large mode area fiber design for 2-μm operation. IEEE Photonics Technol. Lett. 2016, 28, 2483–2486. [Google Scholar] [CrossRef]
- Rehn, L.; Picraux, S.; Wiedersich, H. Surface Alloying by Ion, Electron and Laser Beams; American Society for Metals: Metals Park, OH, USA, 1986. [Google Scholar]
- Pronko, P.; Dutta, S.; Squier, J.; Rudd, J.; Du, D.; Mourou, G. Machining of sub-micron holes using a femtosecond laser at 800 nm. Opt. Commun. 1995, 114, 106–110. [Google Scholar] [CrossRef]
- Bransch, H.; Weckman, D.; Kerr, H. Effects of Pulse Shaping on Nchyag Spot Welds in Austenitic Stainless Steel; U.S. Department of Energy: Washington, DC, USA, 1994.
- Chiang, S.; Albright, C. The limit of joint penetration in high energy density beam welding. Weld. J. N. Y. 1993, 72, 117-s. [Google Scholar]
- Limmaneevichitr, C.; Kou, S. Visualization of marangoni convection in simulated weld pools. Weld. J. N. Y. 2000, 79, 126-s. [Google Scholar]
- Peças, P.; Henrique, M.; Miranda, R.; Quintino, L. Laser welding of low-thickness zinc-coated and uncoated carbon steel sheets. Opt. Quantum Electron. 1995, 27, 1193–1201. [Google Scholar]
- Li, L. The advances and characteristics of high-power diode laser materials processing. Opt. Lasers Eng. 2000, 34, 231–253. [Google Scholar] [CrossRef]
- Quintino, L.; Costa, A.; Miranda, R.; Yapp, D.; Kumar, V.; Kong, C.J. Welding with high power fiber lasers—A preliminary study. Mater. Des. 2007, 28, 1231–1237. [Google Scholar] [CrossRef]
- Niemz, M.H. Laser-Tissue Interactions: Fundamentals and Applications; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Mester, E.; Szende, B.; Tota, J. Effect of laser on hair growth of mice. Kiserl Orvostud 1967, 19, 628–631. [Google Scholar]
- Merigo, E.; Fornaini, C.; Manfredi, M.; Meleti, M.; Alberici, F.; Corcione, L.; Buzio, C.; Rocca, J.-P.; Ferri, T.; Vescovi, P. Orofacial granulomatosis treated with low-level laser therapy: A case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, e25–e29. [Google Scholar] [CrossRef] [PubMed]
- Mohammadpour, H.; Fekrazad, R. Antitumor effect of combined Dkk-3 and 5-ALA mediated photodynamic therapy in breast cancer cell’s colony. Photodiagn. Photodyn. Ther. 2016, 14, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.; Murphy, D.; White, J.; Gold, S. Conservative soft tissue management with the low-powered pulsed Nd: YAG dental laser. Prac. Periodontics Aesthet. Dent. PPAD 1992, 4, 6–12. [Google Scholar]
- Fornaini, C. Er: YAG and adhesion in conservative dentistry: Clinical overview. Laser Ther. 2013, 22, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.; Augros, C.; Rocca, J.; Lagori, G.; Fornaini, C. Ktp and Er: YAG laser dental bleaching comparison: A spectrophotometric, thermal and morphologic analysis. Lasers Med. Sci. 2015, 30, 2157–2164. [Google Scholar] [CrossRef] [PubMed]
- Le, Q.-T.; Bertrand, C.; Vilar, R. Femtosecond laser ablation of enamel. J. Biomed. Opt. 2016, 21, 065005. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Riceputi, D.; Lupi-Pegurier, L.; Rocca, J.P. Patient responses to Er: YAG laser when used for conservative dentistry. Lasers Med. Sci. 2012, 27, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Le, Q.; Vilar, R.; Bertrand, C. Influence of external cooling on the femtosecond laser ablation of dentin. Lasers Med. Sci. 2017, 32, 1943–1951. [Google Scholar] [CrossRef] [PubMed]
- Merigo, E.; Fornaini, C.; Clini, F.; Fontana, M.; Cella, L.; Oppici, A. Er: Yag laser dentistry in special needs patients. Laser Ther. 2015, 24, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Rocca, J.P. CO2 laser treatment of drug-induced gingival overgrowth. Laser Ther. 2012, 21, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, R.L.; Powers, J.M. Craig’s Restorative Dent. Mater.-e-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Knosp, H.; Nawaz, M.; Stümke, M. Dental gold alloys. Gold Bull. 1981, 14, 57–64. [Google Scholar] [CrossRef]
- Wataha, J.C. Principles of biocompatibility for dental practitioners. J. Prosthet. Dent. 2001, 86, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Wataha, J.C. Alloys for prosthodontic restorations. J. Prosthet. Dent. 2002, 87, 351–363. [Google Scholar] [CrossRef] [PubMed]
- Clayton, C.R. Materials Science and Engineering: An Introduction: By WD Callister Jr.; Published by Wiley, Chichester, West Sussex, 1985; 602 pp.; Price, £ 40.40; Elsevier: Amsterdam, The Netherlands, 1987. [Google Scholar]
- Anusavice, K.; Cascone, P. Dental casting and soldering alloys. Phillips Sci. Dent. Mater. 2003, 11, 563–620. [Google Scholar]
- Eftekhari, A. Fractal study of Ni–Cr–Mo alloy for dental applications: Effect of beryllium. Appl. Surf. Sci. 2003, 220, 343–348. [Google Scholar] [CrossRef]
- Pan, J.; Geis-Gerstorfer, J.; Thierry, D.; Leygraf, C. Electrochemical studies of the influence of beryllium on the corrosion resistance of Ni-25Cr-10Mo cast alloys for dental applications. J. Electrochem. Soc. 1995, 142, 1454–1458. [Google Scholar] [CrossRef]
- Geurtsen, W. Biocompatibility of dental casting alloys. Crit. Rev. Oral Biol. Med. 2002, 13, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Baumann, B.; Pai, W.-H.; Bennani, V.; Waddell, J. Dental alloys used for crown and bridge restorations by dental technicians in New Zealand. N. Z. Dent. J. 2010, 106, 43–49. [Google Scholar] [PubMed]
- Lucas, L.C.; Lemons, J.E. Biodegradation of restorative metallic systems. Adv. Dent. Res. 1992, 6, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Brantley, W.A.; Eliades, T. Orthodontic Materials: Scientific and Clinical Aspects; Thieme: Stuttgart, Germany, 2011. [Google Scholar]
- Ferrance, J. Metal Alloys for Orthodontics, Prosthodontics and Pediatric Dentistry. Materials in Dentistry: Principles and Applications; Lippincott Company: Philadelphia, PA, USA, 1995; pp. 281–282. [Google Scholar]
- Smith, D.C. Dental implants: Materials and design considerations. Int. J. Prosthodont. 1993, 6, 106–117. [Google Scholar] [PubMed]
- Parr, G.R.; Gardner, L.K.; Toth, R.W. Titanium: The mystery metal of implant dentistry. Dental materials aspects. J. Prosthet. Dent. 1985, 54, 410–414. [Google Scholar] [CrossRef]
- Adell, R.; Eriksson, B.; Lekholm, U.; Brånemark, P.-I.; Jemt, T. A long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int. J. Oral Maxillofac. Implants 1990, 5, 347–359. [Google Scholar] [PubMed]
- Jemt, T.; Chai, J.; Harnett, J.; Heath, M.R.; Hutton, J.E.; Johns, R.B.; McKenna, S.; McNamara, D.C.; van Steenberghe, D.; Taylor, R. A 5-year prospective multicenter follow-up report on overdentures supported by osseointegrated implants. Int. J. Oral Maxillofac. Implants 1996, 11, 291–298. [Google Scholar] [PubMed]
- Niinomi, M. Mechanical properties of biomedical titanium alloys. Mater. Sci. Eng. A 1998, 243, 231–236. [Google Scholar] [CrossRef]
- Sykaras, N.; Iacopino, A.M.; Marker, V.A.; Triplett, R.G.; Woody, R.D. Implant materials, designs, and surface topographies: Their effect on osseointegration. A literature review. Int. J. Oral Maxillofac. Implants 2000, 15, 675–690. [Google Scholar] [PubMed]
- McCracken, M. Dental implant materials: Commercially pure titanium and titanium alloys. J. Prosthodont. 1999, 8, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Kohal, R.J.; Att, W.; Bächle, M.; Butz, F. Ceramic abutments and ceramic oral implants. An update. Periodontology 2000 2008, 47, 224–243. [Google Scholar] [CrossRef] [PubMed]
- Osman, R.B.; Swain, M.V. A critical review of dental implant materials with an emphasis on titanium versus zirconia. Materials 2015, 8, 932–958. [Google Scholar] [CrossRef] [PubMed]
- Tambasco, J.; Anthony, T.; Sandven, O. Laser welding in the dental laboratory: An alternative to soldering. J. Dent. Technol. 1996, 13, 23–31. [Google Scholar] [PubMed]
- Goldman, L.; Goldman, B.; Lieu, N.V. Current laser dentistry. Lasers Surg. Med. 1987, 6, 559–562. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, C.; Le Petitcorps, Y.; Albingre, L.; Dupuis, V. Prosthodontics: The laser welding technique applied to the non precious dental alloys procedure and results. Br. Dent. J. 2001, 190, 255–257. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bertrand, C.; Le Petitcorps, Y.; Albingre, L.; Dupuis, V. Optimization of operator and physical parameters for laser welding of dental materials. Br. Dent. J. 2004, 196, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, C.; Laplanche, O.; Rocca, J.; Le Petitcorps, Y.; Nammour, S. Effect of the combination of different welding parameters on melting characteristics of grade 1 titanium with a pulsed Nd–YAG laser. Lasers Med. Sci. 2007, 22, 237–244. [Google Scholar] [CrossRef] [PubMed]
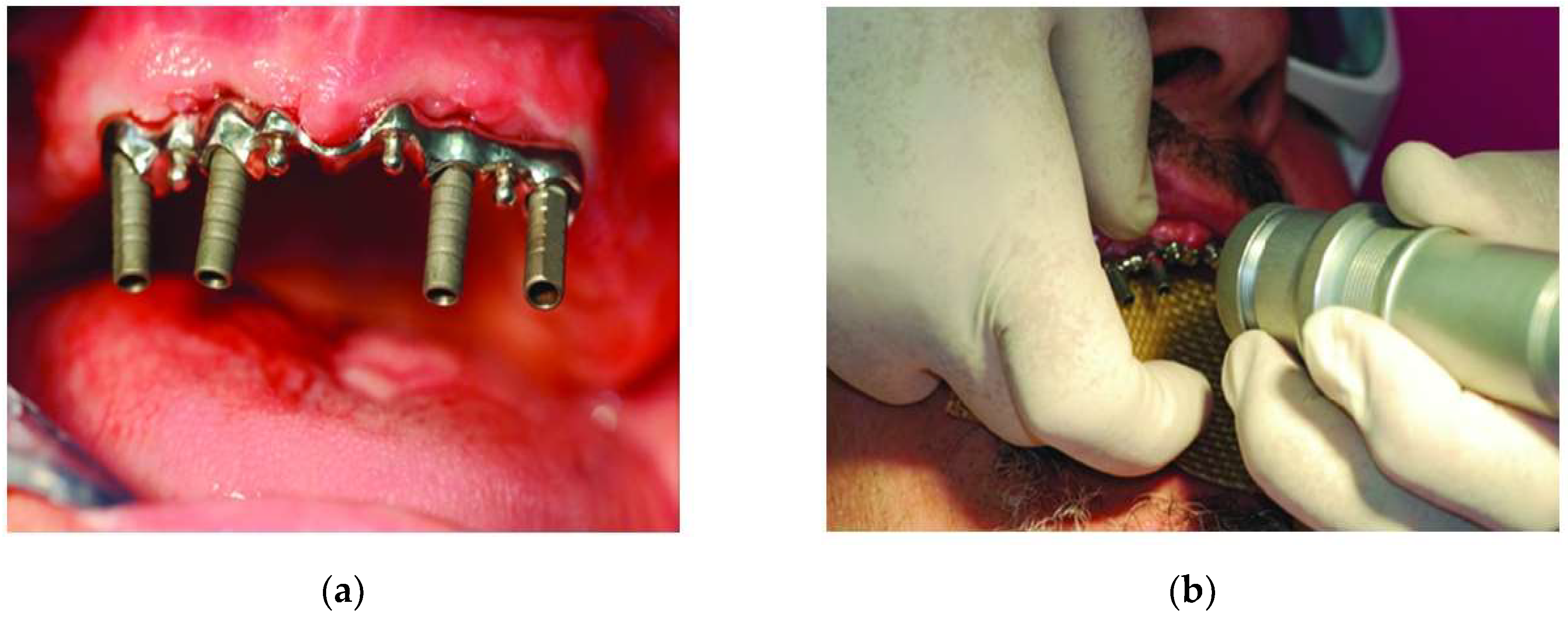
- Fornaini, C.; Merigo, E.; Cernavin, I.; Lòpez de Castro, G.; Vescovi, P. Intraoral laser welding (ilw) in implant prosthetic dentistry: Case report. Case Rep. Dent. 2012, 2012. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brudvik, J.S.; Lee, S.; Croshaw, S.N.; Reimers, D.L. Laser welding of removable partial denture frameworks. Int. J. Prosthodont. 2008, 21, 285–291. [Google Scholar] [PubMed]
- Fornaini, C.; Passaretti, F.; Villa, E.; Rocca, J.-P.; Merigo, E.; Vescovi, P.; Meleti, M.; Manfredi, M.; Nammour, S. Intraoral laser welding: Ultrastructural and mechanical analysis to compare laboratory laser and dental laser. Lasers Med. Sci. 2011, 26, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Meleti, M.; Vescovi, P.; Merigo, E.; Rocca, J.-P. Laser welding and syncristallization techniques comparison: “Ex vivo” study. Laser Ther. 2013, 22, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Fanali, S.; Villa, T.; Fanali, D.; Carinci, F. Optimization of implant-abutment connection in electro-welded implantology: Study and mechanical characterization. Eur. J. Inflamm. 2011, 9, 63–70. [Google Scholar]
- Fornaini, C.; Merigo, E.; Vescovi, P.; Meleti, M.; Nammour, S. Laser welding and syncristallization techniques comparison: In vitro study. Int. J. Dent. 2012, 2012. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Baba, N.; Watanabe, I.; Liu, J.; Atsuta, M. Mechanical strength of laser-welded cobalt–chromium alloy. J. Biomed. Mater. Res. Part B Appl. Biomater. 2004, 69, 121–124. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Nardi, D.; Piattelli, A. Immediate loading of the edentulous maxilla with a final restoration supported by an intraoral welded titanium bar: A case series of 20 consecutive cases. J. Periodontol. 2008, 79, 2207–2213. [Google Scholar] [CrossRef] [PubMed]
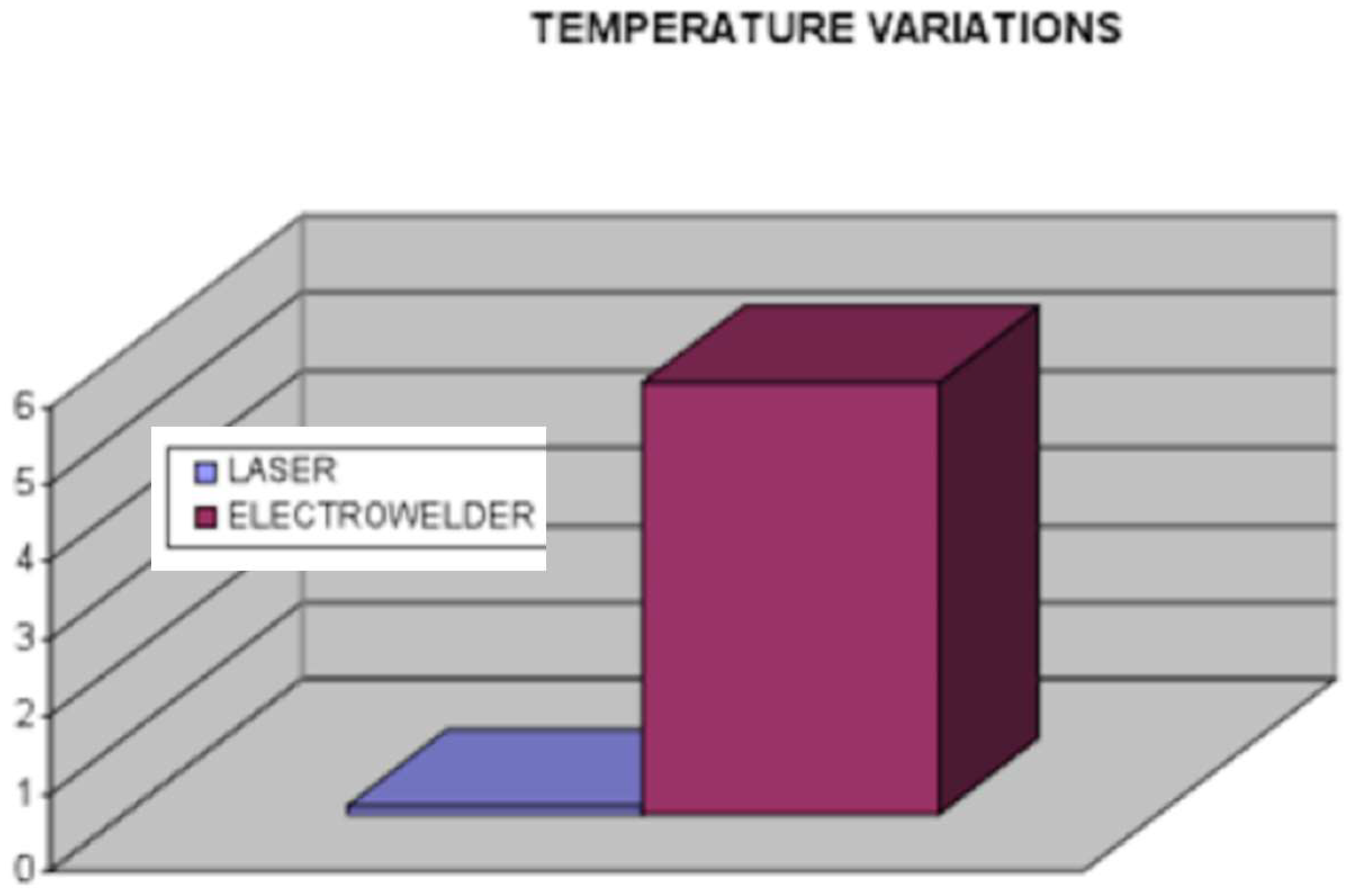
- Fornaini, C.; Meleti, M.; Bonanini, M.; Lagori, G.; Vescovi, P.; Merigo, E.; Nammour, S. Laser welded versus resistance spot welded bone implants: Analysis of the thermal increase and strength. Sci. World J. 2014, 2014. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fornaini, C.; Bertrand, C.; Bonanini, M.; Rocca, J.-P.; Nammour, S. Welding in the dental office by fiber-delivered laser: A new technique. Photomed. Laser Surg. 2009, 27, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Rocca, J.; Bertrand, M.; Merigo, E.; Nammour, S.; Vescovi, P. Nd: YAG and diode laser in the surgical management of soft tissues related to orthodontic treatment. Photomed. Laser Surg. 2007, 25, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Merigo, E.; Vescovi, P.; Lagori, G.; Rocca, J. Use of laser in orthodontics: Applications and perspectives. Laser Ther. 2013, 22, 115. [Google Scholar] [PubMed]
- Watanabe, I.; Topham, D.S. Laser welding of cast titanium and dental alloys using argon shielding. J. Prosthodont. 2006, 15, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, K.; Ohkawa, S.; Uo, M.; Akasaka, T.; Watari, F. Laser welding of titanium and dental precious alloys. Mater. Trans. 2004, 45, 1140–1146. [Google Scholar] [CrossRef]
- Nishio, K. A study on laser welding of dental alloy for dentures. Nihon Hotetsu Shika Gakkai Zasshi 2004, 48, 104–113. [Google Scholar] [CrossRef]
- Sjögren, G.; Andersson, M.; Bergman, M. Laser welding of titanium in dentistry. Acta Odontol. Scand. 1988, 46, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Chai, T.; Chou, C.K. Mechanical properties of laser-welded cast titanium joints under different conditions. J. Prosthet. Dent. 1998, 79, 477–483. [Google Scholar] [CrossRef]
- Watanabe, I.; Liu, J.; Atsuta, M. Effects of heat treatments on mechanical strength of laser-welded equi-atomic AuCu-6at% Ga alloy. J. Dent. Res. 2001, 80, 1813–1817. [Google Scholar] [CrossRef] [PubMed]
- Berg, E.; Wagner, W.C.; Davik, G.; Dootz, E.R. Mechanical properties of laser-welded cast and wrought titanium. J. Prosthet. Dent. 1995, 74, 250–257. [Google Scholar] [CrossRef]
- Walter, M.; Reppel, P.D.; Böning, K.; Freesmeyer, W. Six-year follow-up of titanium and high-gold porcelain-fused-to-metal fixed partial dentures. J. Oral Rehabil. 1999, 26, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Baba, N.; Watanabe, I. Penetration depth into dental casting alloys by Nd: YAG laser. J. Biomed. Mater. Res. Part B Appl. Biomater. 2005, 72, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.R.; Chang, C.T. Thermal modeling of laser welding for titanium dental restorations. J. Prosthet. Dent. 1998, 79, 335–341. [Google Scholar] [CrossRef]
- Watanabe, I.; Baba, N.; Chang, J.; Chiu, Y. Nd: YAG laser penetration into cast titanium and gold alloy with different surface preparations. J. Oral Rehabil. 2006, 33, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Waddell, J.N.; Payne, A.G.; Swain, M.V. Physical and metallurgical considerations of failures of soldered bars in bar attachment systems for implant overdentures: A review of the literature. J. Prosthet. Dent. 2006, 96, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.; Acciari, H.; Vercik, L.; Guastaldi, A.C. Laser weld: Microstructure and corrosion study of Ag–Pd–Au–Cu alloy of the dental application. Mater. Lett. 2003, 57, 1888–1893. [Google Scholar] [CrossRef]
- Jemt, T.; Henry, P.; Lindén, B.; Naert, I.; Weber, H.; Bergström, C. A comparison of laser-welded titanium and conventional cast frameworks supported by implants in the partially edentulous jaw: A 3-year prospective multicenter study. Int. J. Prosthodont. 2000, 13, 282–288. [Google Scholar] [PubMed]
- Liu, J.; Watanabe, I.; Yoshida, K.; Atsuta, M. Joint strength of laser-welded titanium. Dent. Mater. 2002, 18, 143–148. [Google Scholar] [CrossRef]
- White, J.M.; Goodis, H.E.; Rose, C.L. Use of the pulsed Nd: YAG laser for intraoral soft tissue surgery. Lasers Surg. Med. 1991, 11, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Welsch, G. Joining titanium materials with tungsten inert gas welding, laser welding, and infrared brazing. J. Prosthet. Dent. 1995, 74, 521–530. [Google Scholar] [CrossRef]
- Grevey, D.; Sallamand, P.; Cicala, E.; Ignat, S. Gas protection optimization during Nd: YAG laser welding. Opt. Laser Technol. 2005, 37, 647–651. [Google Scholar] [CrossRef]
- Matsui, Y. Cracking in laser welds of dental Ni-Cr alloys. Effect of alloy composition. Nihon Hotetsu Shika Gakkai Zasshi 1990, 34, 531–544. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, F.; Ueyama, T. Solidification crack susceptibility of laser weld metal in 0.2 C-Ni-Cr-Mo steels: Effects of bead configuration and S and P contents. Weld. Int. 1993, 7, 686–692. [Google Scholar] [CrossRef]
- Lin, M.-C.; Lin, S.-C.; Wang, Y.-T.; Hu, S.-W.; Lee, T.-H.; Chen, L.-K.; Huang, H.-H. Fracture resistance of Nd: YAG laser-welded cast titanium joints with various clinical thicknesses and welding pulse energies. Dent. Mater. J. 2007, 26, 367–372. [Google Scholar] [CrossRef] [PubMed][Green Version]
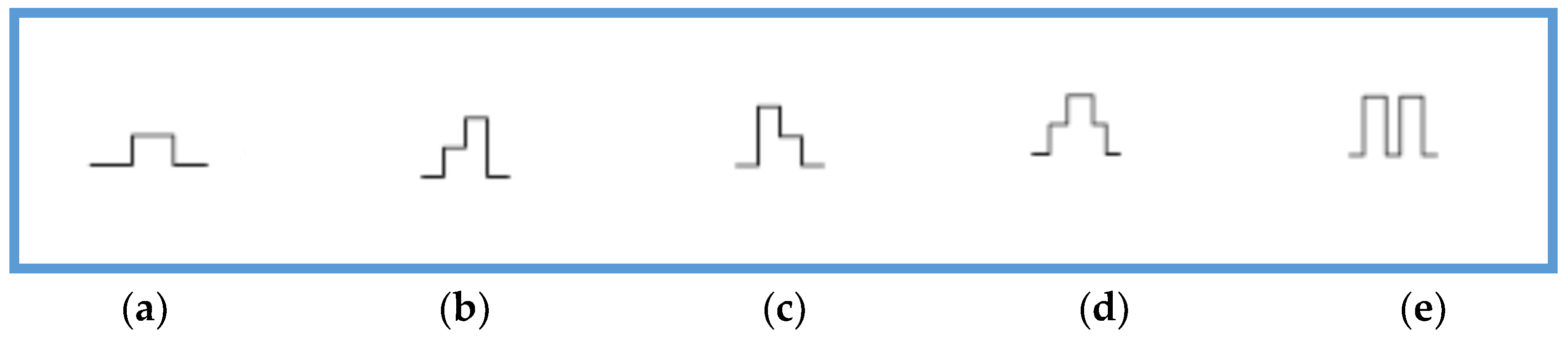
- Bertrand, C.; Poulon-Quintin, A. Temporal pulse shaping: A key parameter for the laser welding of dental alloys. Lasers Med. Sci. 2015, 30, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Boere, G. Influence of fluoride on titanium in an acidic environment measured by polarization resistance technique. J. Appl. Biomater. 1995, 6, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-H.; Lin, M.-C.; Lin, C.-C.; Lin, S.-C.; Hsu, C.-C.; Chen, F.-L.; Lee, S.-Y.; Hung, C.-C. Retraction: Effects of welding pulse energy and fluoride ion on the cracking susceptibility and fatigue behavior of Nd: YAG laser-welded cast titanium joints. Dent. Mater. J. 2006, 25, 632–640. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huang, H.-H.; Lin, S.-C.; Lee, T.-H.; Chen, C.-C. Effect of welding voltage on the mechanical behavior of a laser-welded cast titanium joint for dental prosthesis. J. Mater. Sci. 2005, 40, 789–792. [Google Scholar] [CrossRef]
- Huang, H.-H. Effects of fluoride concentration and elastic tensile strain on the corrosion resistance of commercially pure titanium. Biomaterials 2002, 23, 59–63. [Google Scholar] [CrossRef]
- Nakagawa, M.; Matsuya, S.; Udoh, K. Corrosion behavior of pure titanium and titanium alloys in fluoride-containing solutions. Dent. Mater. J. 2001, 20, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Matono, Y.; NAKAGAWA, M.; MATSUYA, S.; ISHIKAWA, K.; TERADA, Y. Corrosion behavior of pure titanium and titanium alloys in various concentrations of acidulated phosphate fluoride (APF) solutions. Dent. Mater. J. 2006, 25, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, M.; Matsuya, S.; Udoh, K. Effects of fluoride and dissolved oxygen concentrations on the corrosion behavior of pure titanium and titanium alloys. Dent. Mater. J. 2002, 21, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, I.; Watanabe, E. Surface changes induced by fluoride prophylactic agents on titanium-based orthodontic wires. Am. J. Orthodont. Dent. Orthop. 2003, 123, 653–656. [Google Scholar] [CrossRef]
- Pröbster, L.; Lin, W.; Hüttemann, H. Effect of fluoride prophylactic agents on titanium surfaces. Int. J. Oral Maxillofac. Implants 1992, 7, 116–125. [Google Scholar]
- Zavanelli, R.; Guilherme, A.; Pessanha-Henriques, G.; Antônio de Arruda Nóbilo, M.; Mesquita, M. Corrosion-fatigue of laser-repaired commercially pure titanium and Ti-6Al-4V alloy under different test environments. J. Oral Rehabil. 2004, 31, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Cheung, G. A preliminary investigation into the longevity and causes of failure of single unit extracoronal restorations. J. Dent. 1991, 19, 160–163. [Google Scholar] [CrossRef]
- Giordano, R.; McLaren, E.A. Ceramics overview: Classification by microstructure and processing methods. Compend. Contin. Educ. Dent. 2010, 31, 682–684. [Google Scholar] [PubMed]
- Saraçoğlu, A.; Cura, C.; Cötert, H. Effect of various surface treatment methods on the bond strength of the heat-pressed ceramic samples. J. Oral Rehabil. 2004, 31, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Poli, F.; Merigo, E.; Brulat-Bouchard, N.; El Gamal, A.; Rocca, J.-P.; Selleri, S.; Cucinotta, A. Disilicate dental ceramic surface preparation by 1070 nm fiber laser: Thermal and ultrastructural analysis. Bioengineering 2018, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Sozzil, M.; Merigo, E.; Parsottil, P.; Selleril, S.; Cucinotta, A. Supercontinuum source in the investigation of laser-tissue interactions: Ex vivo study. J. Biomed. 2017, 2, 12–19. [Google Scholar] [CrossRef]
| Method | Torch Soldering | Post (Ceramic Furnace) or Infrared Soldering | Spot Welding | Plasma Welding | Laser Welding | Tungsten Inert Gas (TIG) |
|---|---|---|---|---|---|---|
| Equipment expenditure | Small | Moderate | Small | Moderate | High | Moderate |
| Application depth, versatility | high | High | Small | medium | High | High |
| Educational prerequisite | Moderate | Moderate | Small | medium | Medium | Medium |
| Biocompatibility | Small | Small | Good | Moderate | Good | Good |
| Heat Affected zone | large | large | Small | medium | Very small | Very small |
| Type of Alloy | Noble Metal Content |
|---|---|
| High noble | Minimum of 40% gold and at least 60% of noble metal elements Example: gold-platinum-palladium, gold-palladium-silver and gold-palladium |
| Noble | ≥25% by weight noble metals. Example: palladium-silver, palladium-copper-gallium, and palladium-gallium |
| Base metal | ≤ 25% noble metal Example: Nickel-chromium and cobalt-chromium |
| Ti and its alloys | Ti content more than 85% |
| Alloy Group | Vicker Hardness | Modulus of Elastic (GPa) | 0.2% Proof Stress (MPa) | Tensile Strength (MPa) | Specific Gravity (g/cm3) |
|---|---|---|---|---|---|
| High Gold | 200 | 90 | 480 | 580 | 18.1 |
| Gold-palladium (no silver) | 240 | 124 | 550 | 800 | 14.8 |
| Gold-palladium-silver | 200 | 110 | 600 | 680 | 14.9 |
| Palladium-Copper | 275 | 96 | 800 | 851 | 10.6 |
| Palladium-Silver | 260 | 138 | 650 | 810 | 11.4 |
| Nickel-Chromium | 240 | 160 | 360 | 580 | 8.6 |
| Nickel-Chromium-Beryllium | 240 | 192 | 552 | 1138 | 7.8 |
| Cobalt-Chromium | 310 | 210 | 480 | 720 | 8.5 |
| Implant Material | Common Name or Abbreviation |
|---|---|
| I. Metals | |
| Titanium | CpTi |
| Titanium alloys | Ti-6A1-4V extra low interstitial (ELI) |
| Ti-6A1-4V | |
| Ti-6Al-7Nb | |
| Ti-5Al-2.5Fe | |
| Ti-15 Zr-4Nb-2Ta-0.2Pd | |
| Ti-29Nb-13Ta-4.6Zr | |
| Roxolid (83–87%Ti-13–17%Zr) | |
| Stainless Steel | SS, 316 LSS |
| Cobalt Chromium Alloy | Vitallium, Co-Cr-Mo |
| Gold Alloys | Au Alloys |
| Tantalum | Ta |
| II. Ceramics | |
| Alumina | Al2O3, polycrystalline alumina or single-crystal sapphire |
| Hydroxyapatite | HA, Ca10(PO4)10, (OH)2 |
| Beta-Tricalcium phosphate | β-TCP, Ca3(PO4)2 |
| Carbon | C |
| vitreous | |
| low-temperature isotropic (LTI) | |
| ultra-low-temperature isotropic (ULTI) | |
| Carbon-Silicon | C-Si |
| Bioglass | SiO2/CaO/Na2O/P2O5 |
| Zirconia | ZrO2 |
| Zirconia-toughened alumina | ZTA |
| III. Polymers | |
| Polymethylmethacrylate | PMMA |
| Polytetrafluoroethylene | PTFE |
| Polyethylene | PE |
| Polysulfone | PSF |
| Polyurethane | PU |
| Polyether ether ketone | PEEK |
| Materials | Laser Type |
|---|---|
| Ti and its Alloy | CW–CO2, Pulsed Nd:YAG laser, Fiber laser, Yb:YAG ytterbium laser |
| Ceramics | CW–CO2, KrF excimer laser, pulsed YAG laser |
| Steel and its alloy | Pulsed Nd:YAG, CW-laser, Photolytic iodine laser, CW–CO2 and diode laser |
| Al alloy | Pulsed Nd:YAG laser, CW–CO2, Fiber laser |
| Gold | Semiconductor laser, Nd:YAG laser |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perveen, A.; Molardi, C.; Fornaini, C. Applications of Laser Welding in Dentistry: A State-of-the-Art Review. Micromachines 2018, 9, 209. https://doi.org/10.3390/mi9050209
Perveen A, Molardi C, Fornaini C. Applications of Laser Welding in Dentistry: A State-of-the-Art Review. Micromachines. 2018; 9(5):209. https://doi.org/10.3390/mi9050209
Chicago/Turabian StylePerveen, Asma, Carlo Molardi, and Carlo Fornaini. 2018. "Applications of Laser Welding in Dentistry: A State-of-the-Art Review" Micromachines 9, no. 5: 209. https://doi.org/10.3390/mi9050209
APA StylePerveen, A., Molardi, C., & Fornaini, C. (2018). Applications of Laser Welding in Dentistry: A State-of-the-Art Review. Micromachines, 9(5), 209. https://doi.org/10.3390/mi9050209





