1. Introduction
In drug development, typical experiments for drug discovery often use animal experiments and cell-based assay tests. Animal experiments have various issues, such as ethical considerations and species differences. Cell-based assays have issues with cultured cells that do not retain the organ’s function in vitro. In recent years, in medicine and life sciences, microphysiological systems (MPSs), including organ-on-a-chip (OoC), are attracting attention as promising technologies that can reproduce in vivo-like tissue structures and fluid flow on microfabricated platforms. MPSs are increasingly being utilized to evaluate drug pharmacokinetics, toxicity, absorption, metabolism, and interorgan interactions under controlled in vitro conditions [
1,
2,
3,
4]. Multiorgan microphysiological systems (MO-MPSs) enable the co-culture of multiple organ-derived cells, allowing the study of complex organ–organ interactions in real time and contributing to more accurate drug evaluation systems [
5,
6,
7,
8].
A key element for reproducing physiological conditions in MPSs is the application of dynamic fluid flow to simulate blood circulation. Conventionally, syringe and peristaltic pumps have been used to generate perfusion flow; however, these external pump systems require complex tubing connections, present contamination risks and air bubbles, and consume large volumes of culture medium, increasing experimental costs and reducing throughput [
9,
10]. Various integrated pumping methods, including pneumatic pumps, membrane pumps, and gravity-based systems, have been developed to address these issues. However, many still involve complicated operations or closed-channel configurations that reduce usability for long-term culture and co-culture setups.
To overcome these limitations, a stirrer-based kinetic pump system was previously developed, which generates fluid circulation by rotating miniature magnetic stir bars embedded inside the culture device [
11]. This technology led to the development of the Kinetic Pump Integrated Microfluidic Plate (KIM-Plate), which combines the stirrer-based kinetic pump with an open-top culture chamber multiorgan microphysiological design [
12]. The KIM-Plate comprises six independent MO-MPS units conforming to ANSI/SBS microplate standards, allowing direct use with commercially available cell culture inserts and disks. Open-top culture chambers of the KIM-plate simplify handling and enable the co-culture of multiple organ models. However, the KIM-Plate was made of black polymer, which made it difficult to check the stirrer rotation. Sumitomo Bakelite developed the BioStellar™ Plate as a redesigned next-generation system based on the KIM-Plate concept to improve usability. The design principles of the BioStellar™ Plate’s open-top culture chamber architecture and kinetic pump integration provide a versatile framework that can be adapted for use with other commercial MPS platforms. This approach offers simplified handling, reduced contamination risk, and increased experimental throughput across various MPS platforms. The BioStellar™ Plate retains the exact kinetic pump mechanism and open-top culture chamber design but employs transparent polystyrene for full compatibility with standard microscopy. While the BioStellar™ Plate provides continuous perfusion, it cannot apply controlled fluidic shear stress (FSS), which is an important factor influencing cellular morphology, differentiation, and barrier function under physiological conditions, because of the open-top culture chambers.
To address this limitation, we developed FSS loading attachments capable of guiding fluid flow and introducing controlled FSS onto epithelial cells cultured within the BioStellar™ Plate in this study. We designed and fabricated fluidic shear stress attachments (FSSAs) for the BioStellar™ Plate, conducted flow simulations, and verified their hydrodynamic behavior through experiments. We successfully introduced controlled FSS during dynamic perfusion by applying these attachments to epithelial cell cultures. The controlled FSS environment created by these attachments enables the investigation of cellular responses across multiple cell types, including endothelial and epithelial cells, as well as potentially other mechanosensitive cell populations that are crucial for modeling various organ systems and disease states. As a result, cells exposed to FSS showed improved growth and organization compared to static cultures, demonstrating the effectiveness of this approach in enhancing the BioStellar™ Plate for future microphysiological applications. The modular design approach of these microfluidic accessories will adapt to other commercial MPS platforms, potentially expanding the utility of controlled shear stress applications across the broader MPS research community.
2. Materials and Methods
2.1. BioStellar™ Plate
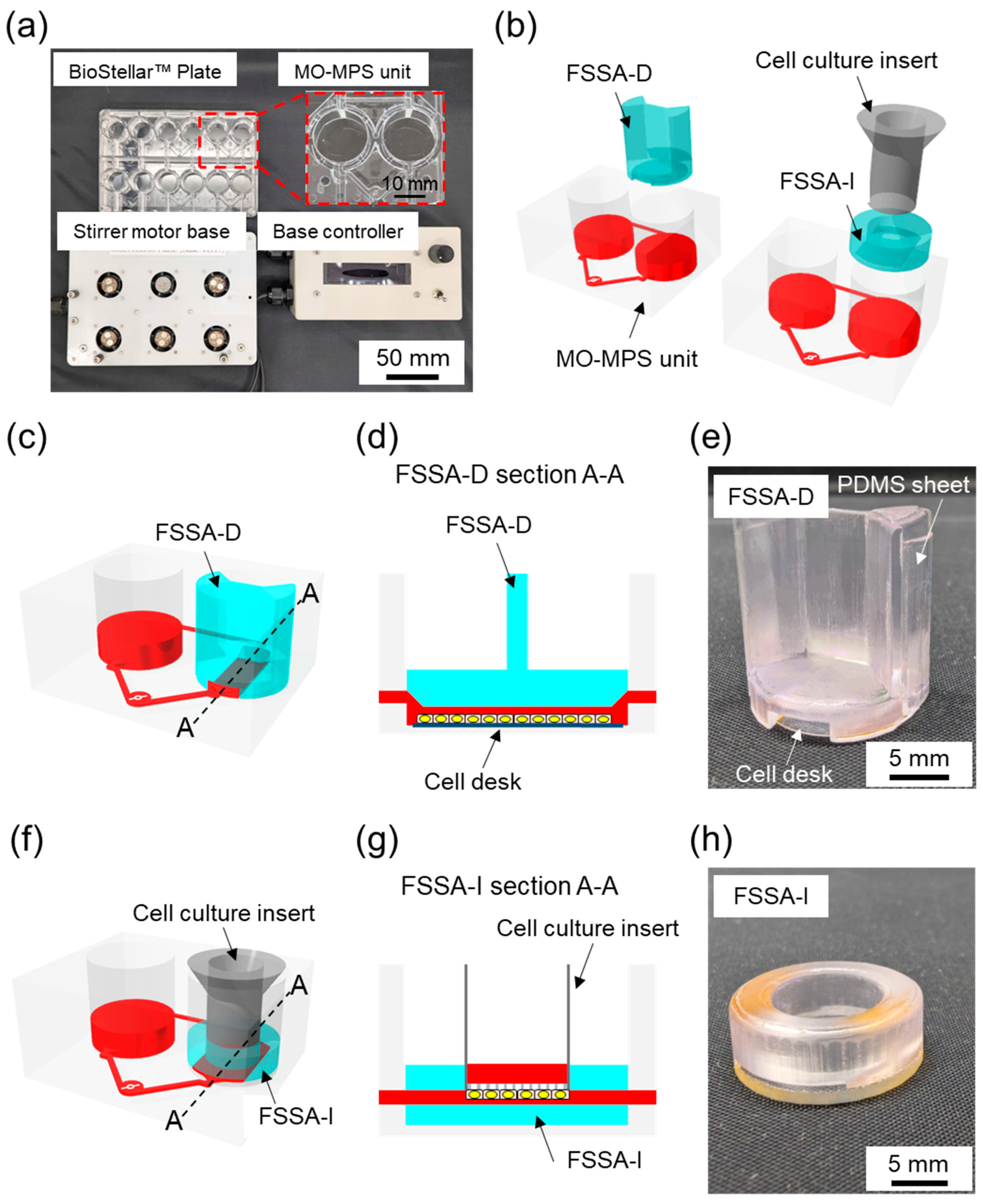
The BioStellar™ Plate (Sumitomo Bakelite, Tokyo, Japan) consists of six independent MO-MPS units that conform to ANSI/SBS microplate standards (128 mm × 85 mm × 40 mm). Each unit features dual microchannel-connected open-top culture chambers with the same diameter and configuration as standard 24-well plates, making it fully compatible with conventional cell culture protocols. Commercially available cell culture inserts and disks can be used directly within the plate without any modifications (
Figure 1a). The entire plate body was fabricated from optically clear polystyrene (PS) using injection molding. This enhances imaging compatibility and allows for seamless observation during culture. The microfluidic architecture connects each chamber pair by microchannels (1.0 mm wide × 0.3 mm high). These channels were positioned 1.2 mm above the bottom of the chamber. This construction limited direct fluid shear stress on cells.
Culture medium circulation was achieved through an embedded stirrer-based kinetic pump driven by a 3 mm × 0.2 mm stainless-steel stirrer bar. The clockwise rotation of a magnetic rotor beneath the plate generates forward flow through the main channel. In contrast, backflow through the secondary channel completes the loop, creating a continuous circulation system. The BioStellar™ Plate was designed to be used with a custom-built magnetic stirrer motor base that holds six magnetic rotor units, each driven by DC axial fans (108-AFB0412HHA-TA5F, Delta Electronics, Taipei, Taiwan). The base and its controller, produced by Microfluidic System Works, allow simultaneous control of rotor speeds, ensuring consistent and adjustable flow across all six MO-MPS units (
Figure 1a). The system could reach rotation speeds of up to 6500 rpm in its current configuration, allowing for a broad operational range that generates various flow rates suitable for both low-shear and high-shear experimental conditions.
2.2. Fluidic Shear Stress Attachments
To specifically introduce regulated FSS to cell cultures within the BioStellar™ Plate, we developed two customized fluidic shear stress attachments (FSSAs), each designed to accommodate different cell culture formats while maintaining compatibility with the BioStellar™ Plate (
Figure 1b).
The first attachment, the Fluidic Shear Stress Attachment—Cell Desk (FSSA-D), supports flat-surface cultures on the cell desk (
Figure 1c,d and
Figure S1a). Its primary function is to establish a controlled flow channel directly above the cultured cells. The centrally aligned straight microchannel measures 5.5 mm in width and 0.4 mm in height after cell desk installation. To maintain consistent flow, the channel incorporates 35° slopes at both the inlet and outlet, which guide fluid into the central region. The FSSA-D body is 15.9 mm in diameter and 17.0 mm in height, with a concave slot at the bottom (13.7 mm diameter; 0.3 mm depth) to secure the cell desk (MS-92132, Sumitomo Bakelite, Tokyo, Japan). Two grooves, each 0.5 mm deep and 7.6 mm wide, run along the sidewalls to accommodate PDMS sheets and form a watertight seal with the BioStellar™ Plate. This channel design enables unidirectional laminar flow across the apical cell surface, closely replicating physiological fluidic shear stimulation observed in blood vessels and other flow-exposed tissues (
Figure 1e).
The second attachment, the Fluidic Shear Stress Attachment—Insert (FSSA-I), is engineered for cell culture inserts compatible with 24-well plate formats (
Figure 1f,g and
Figure S1b). This design applies fluidic shear stress to the basal surface of cell monolayers grown on microporous membranes. The FSSA-I consists of a circular body (16.0 mm diameter; 5.5 mm height) with a central insertion port (4.0 mm height; 9.4 mm diameter) that securely holds the insert. The flow-guiding region beneath the insert is a rectangular channel (9.3 mm width; 0.5 mm height), which ensures even perfusion of medium along the basal membrane surface. The bottom structure, made from 1 mm thick acrylic, provides rigidity and optical clarity for microscopy. By directing flow beneath the membrane, the FSSA-I enables localized fluidic shear stress on the basal side of epithelial layers, replicating dynamic microenvironments found in intestinal, renal, or vascular systems (
Figure 1h). Both attachments utilize the BioStellar™ Plate’s circulation system to generate physiologically relevant mechanical stimulation on cultured cells, eliminating the need for external pumps or complex tubing.
2.3. Fabrication of the FSSAs
FSSAs were fabricated using a high-resolution 3D printer Formlabs Form 3B+ (PKG-F3B-COMPLETE-EW-1, Formlabs, MA, USA) with BioMed Clear resin (RS-F2-BMCL-01, Formlabs, MA, USA), a biocompatible photopolymer suitable for cell culture applications. The FSSAs’ geometries were designed using AutoCAD 2019 (Autodesk, CA, USA) and exported as STL files, which were subsequently processed in PreForm software (Formlabs, MA, USA). The models were printed using default settings with a layer thickness of 50 µm to achieve high-dimensional precision and smooth surface quality suitable for microfluidic use. Following printing, the attachments were washed in isopropyl alcohol (IPA) using the Form Wash (FH-WA-02, Formlabs, MA, USA) for 15 min to remove uncured resin from channel structures and surfaces. The printed parts were then post-cured using Form Cure (FH-CU-01, Formlabs, MA, USA) at 60 °C for 30 min, ensuring complete crosslinking and the mechanical stability of the material. The cured attachments underwent a detailed multi-step solvent-washing protocol designed to remove toxins from the printed material and prepare it for further biological use. Initially, each FSSA was submerged in acetone and cleaned with an ultrasonic washer for 60 min. After the acetone wash, the attachments were rinsed in IPA for 30 min using an ultrasonic washer to ensure that any traces of acetone were thoroughly removed. The attachments underwent three consecutive washes, each lasting 30 min, with ion-exchanged water, again using an ultrasonic washer. Finally, the attachments were sterilized by autoclaving at 120 °C for 20 min. This high-temperature process eliminated any potential microbial contamination. After autoclaving, the FSSAs were allowed to cool overnight to minimize the risk of cracking caused by thermal stress, ensuring they were safe and ready for further applications.
The bottom of FSSA-D was installed using the cell desk and double-sided tape, forming a connected perfusion chamber. To reinforce the lateral fit and maintain structural alignment within the BioStellar™ Plate, a 0.5 mm thick PDMS sheet was applied along the sidewall’s grooves of the attachment (
Figure 1e). Conversely, the FSSA-I was assembled onto a custom-fabricated acrylic base to accommodate a cell culture insert (Transwell
®, 3450, Corning, New York, NY, USA) (
Figure 1h). The components were joined using double-sided tape to ensure stable integration.
Following assembly, the FSSAs underwent gas sterilization to ensure sterility across all contact and interface surfaces. Before beginning biological experiments, the FSSAs were stored for at least one week to remove any potential cytotoxicity from residual sterilant gases.
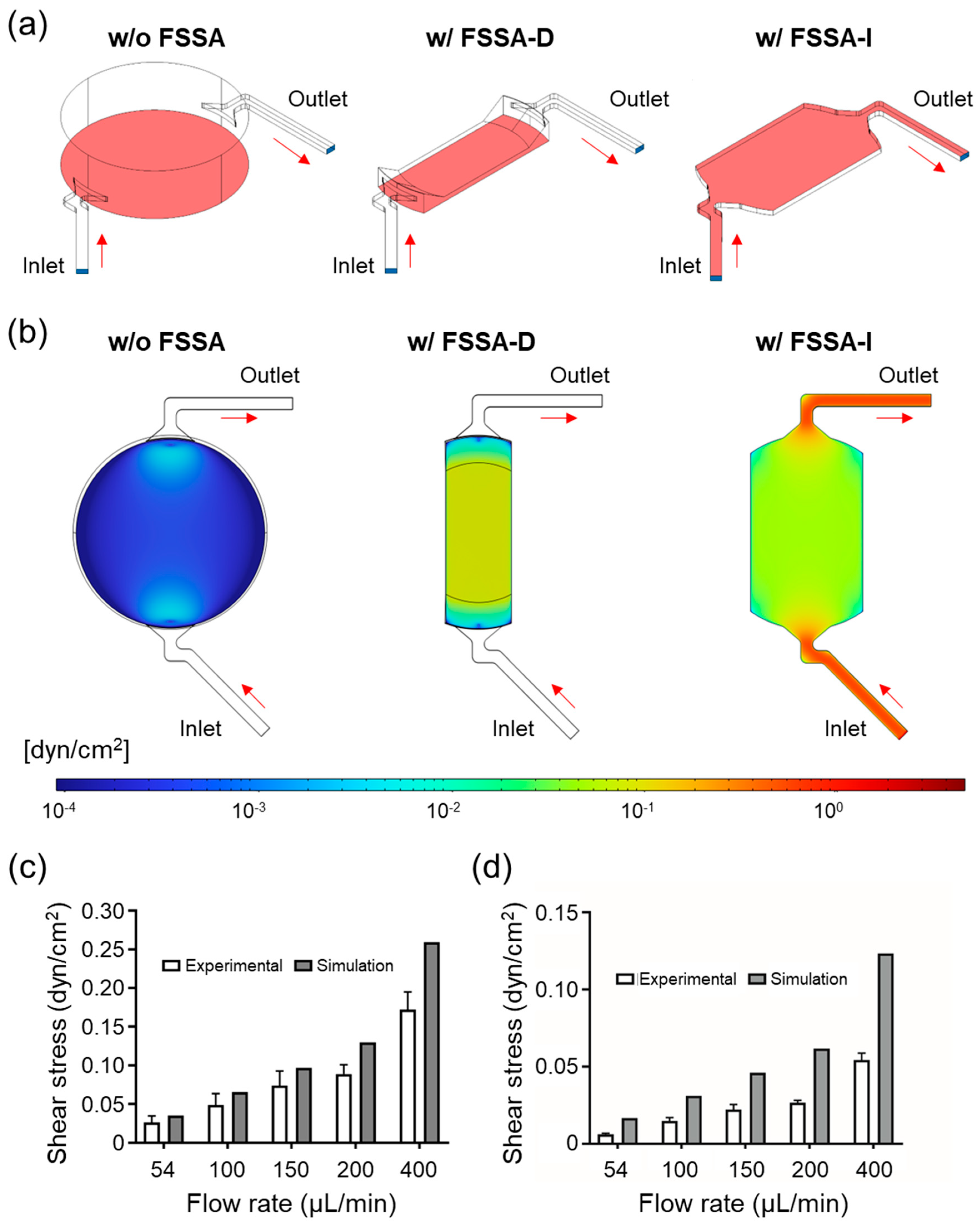
2.4. Numerical Simulation in Flow
To evaluate the flow characteristics within the BioStellar™ Plate, 3D models of the cell culture chamber, FSSA-D, and FSSA-I were constructed using COMSOL Multiphysics 6.1 (COMSOL, Stockholm, Sweden) to assess the flow characteristics. The simulation chamber dimensions were chosen to replicate the actual geometry of the BioStellar™ Plate, rather than the standard 24-well plate dimensions. Standard 24-well plates typically feature wells with a diameter of approximately 15.6-16.5 mm and a total depth of 17.0 mm. The BioStellar™ Plate features open-top culture chambers optimized for the integrated kinetic pump system and operates under different parameters. The simulation domain consisted of a cylindrical chamber with a diameter of 16.4 mm and a height of 4.7 mm, with two fluidic channels positioned at opposite ends. The chamber diameter of 16.4 mm matches the inner diameter of the BioStellar™ Plate culture chambers, which have a height of 4.7 mm, corresponding to the water level when filled with 1 mL of culture medium, the standard working volume for this system. Each channel was 1.0 mm wide and 0.5 mm high, serving as both the inlet and outlet, and representing the actual fluidic connections in the BioStellar™ Plate system. The working fluid was modeled using water properties at 37 °C, with minor adjustments to reflect physiological conditions. Simulations were performed at five different inlet flow velocities to analyze variations in velocity distribution across both FSSA designs.
2.5. Flow Observation
To experimentally validate flow simulations and characterize flow behavior, we performed particle tracking velocimetry using fluorescent microbeads (10 μm in diameter, 1.1 × 10
8 particles/mL, 18142, Polyscience, IL, USA) as flow tracers. Instead of using the full BioStellar™ Plate, we employed a custom-fabricated PDMS-based open-top culture chamber model that resembled the BioStellar™ Plate architecture. The chamber model retained the essential features of the BioStellar™ Plate, including inlet and outlet water channels and a single cell culture chamber, but also included a glass bottom to facilitate high-resolution imaging (
Figure S2).
The FSSAs were mounted onto the chamber model to replicate the in situ flow environment. Flow was driven by two syringe pumps programmed to mimic the pulsatile perfusion behavior generated by the BioStellar™ Plate. We recorded bead movement in the central region of each attachment using an Olympus IX71 (Olympus Corporation, Tokyo, Japan) inverted fluorescence microscope paired with a video camera (FDR-AX700, Sony, Tokyo, Japan) operating in super slow-motion mode (240 fps).
The captured videos were analyzed using FlowExpert64 Ver 1.3.0 software (Katokoken, Kanagawa, Japan), a particle image velocimetry (PIV) platform, to quantitatively extract flow velocity fields and estimate local FSS in the attachment channels. The
Supplementary Information includes a representative video of the microbead flow behavior (
Figure S3; Videos S1 and S2).
2.6. Estimation of FSS
FSS (
τ) (Pa) was calculated from the velocity data using the following equation [
13,
14]:
where
μ is the viscosity of water at 37 °C (0.6913 mPa·s),
u is the average flow velocity (m/s), and
h is the channel height (m).
It is worth noting that the flow velocity obtained through microscopy reflects the peak velocity at the center (z-axis) of the microchannel rather than the average velocity across the entire cross-section, an important distinction when calculating FSS. Additionally, while FSS was calculated using standard SI units (Pascal, Pa) via the equation, the values reported throughout the results section are expressed in dyne per square centimeter (dyn/cm
2) for consistency with the biological literature. For reference, 1 Pa is equivalent to 10 dyn/cm
2. In cylindrical channels, the average velocity is generally assumed to be half the maximum. However, this relationship does not carry over to rectangular channels like the FSSAs. To address this, we used ANSYS Fluent 2022 R1 (Ansys, PA, USA) to simulate the precise channel geometries of both FSSA-D and FSSA-I and to determine the ratio between maximum and average velocities. From these simulations, correction factors of 1.55 for FSSA-D and 1.56 for FSSA-I were obtained and applied to convert the measured peak velocities into more accurate average velocities (
Figure S4).
2.7. Cell Culture
Human epithelial colorectal adenocarcinoma cells (Caco-2, ATCC, Virginia, USA) were cultured in 100 mm culture dishes (3020-100, Iwaki, Shizuoka, Japan) using Dulbecco’s Modified Eagle Medium (DMEM, 11885092, Thermo Fisher Scientific, Massachusetts, USA). The medium contained 1 g/L glucose and 25 mM HEPES, supplemented with 10% fetal bovine serum (FBS, 10270-106, Thermo Fisher Scientific, Massachusetts, USA), 1% antibiotic-antimycotic (AA, 161-23181, Fujifilm Wako Pure Chemical Corporation, Osaka, Japan), and 1% non-essential amino acids (NEAA, 11140-050, Thermo Fisher Scientific, MA, USA). Cultures were maintained at 37 °C in a humidified incubator with 5% CO2. The culture medium was replaced every two days throughout the expansion and experimental culture periods to maintain nutrient balance and cell viability.
In the FSSA-D configuration, the FSS group was cultured using dynamic perfusion within the FSSA placed on the cell desk. The control group was cultured on cell desks in standard well plates without the FSSA under conventional static conditions. This configuration allowed for a direct comparison between conventional static culture and the effect of applied FSS generated by the FSSA-D. In the FSSA-I configuration, cells were cultured on the basal side of a microporous membrane of a cell culture insert (Transwell®, 3450, Corning, New York, USA) in both the control group and the FSS group. This configuration allowed access to the basal membrane surface for FSS exposure.
Two types of extracellular matrix (ECM) coatings were prepared. For FSSA-D, a Collagen Type I-P solution was prepared by mixing 1 mL of Collagen Type I-P (634-00663, Nitta Gelatin, Osaka, Japan) with 9 mL of ultrapure water, followed by the addition of 10 µL of hydrochloric acid to adjust the pH to approximately 3. The FSSA-D was submerged in this solution and incubated at 37 °C for 1 h to allow for uniform coating of the microchannel surfaces. For the FSSA-I, Matrigel (354230, Corning, New York, NY, USA) was used at a 1:25 dilution in a cold medium and applied solely to the membrane surface of the cell culture insert. The inserts were incubated at 37 °C for 1 h to ensure a consistent ECM coating.
In case of cell seeding for FSSA-D, Caco-2 cells were seeded directly into the coated channels at 2 × 105 cells/cm2. Approximately 80 µL of the cell suspension was introduced into each channel, followed by a 5 h pre-culture period in a 12-well plate containing the surrounding culture medium. After sufficient cell attachment, the FSSA-D were transferred into the BioStellar™ Plate to initiate perfusion culture.
In case of cell seeding for FSSA-I, inverted seeding facilitated basal membrane culture. The cell culture inserts were placed upside down in a 12-well plate, and 2 × 105 cells/cm2 of Caco-2 cells were seeded onto the basal membrane surface using a custom-fabricated PDMS cup-like holder to retain the seeding medium. Each insert received 100 µL of medium and was incubated inverted for 3 h for cell attachment. Afterwards, the inserts were returned to their upright position and pre-cultured in a standard 24-well plate for 1 day, then transferred into the BioStellar™ Plate system for perfusion culture.
2.8. TEER Measurement
For the FSSA-I experiments, epithelial barrier formation was assessed using a transepithelial electrical resistance (TEER) measurement system (Millicell ERS-2, MERS00002, Merck Millipore, MA, USA). Chopstick electrodes were positioned with one probe in the apical compartment and the other in the basal compartment. TEER values were calculated by subtracting the background resistance of a blank insert from the resistance measured in the cell-seeded insert. TEER measurements were performed before each medium change to monitor barrier development under consistent conditions. TEER measurements were not conducted for the FSSA-D configuration. The flat-bottom culture chamber does not include a microporous membrane or separate apical and basal compartments, which are necessary for precise electrode placement and reliable resistance measurement.
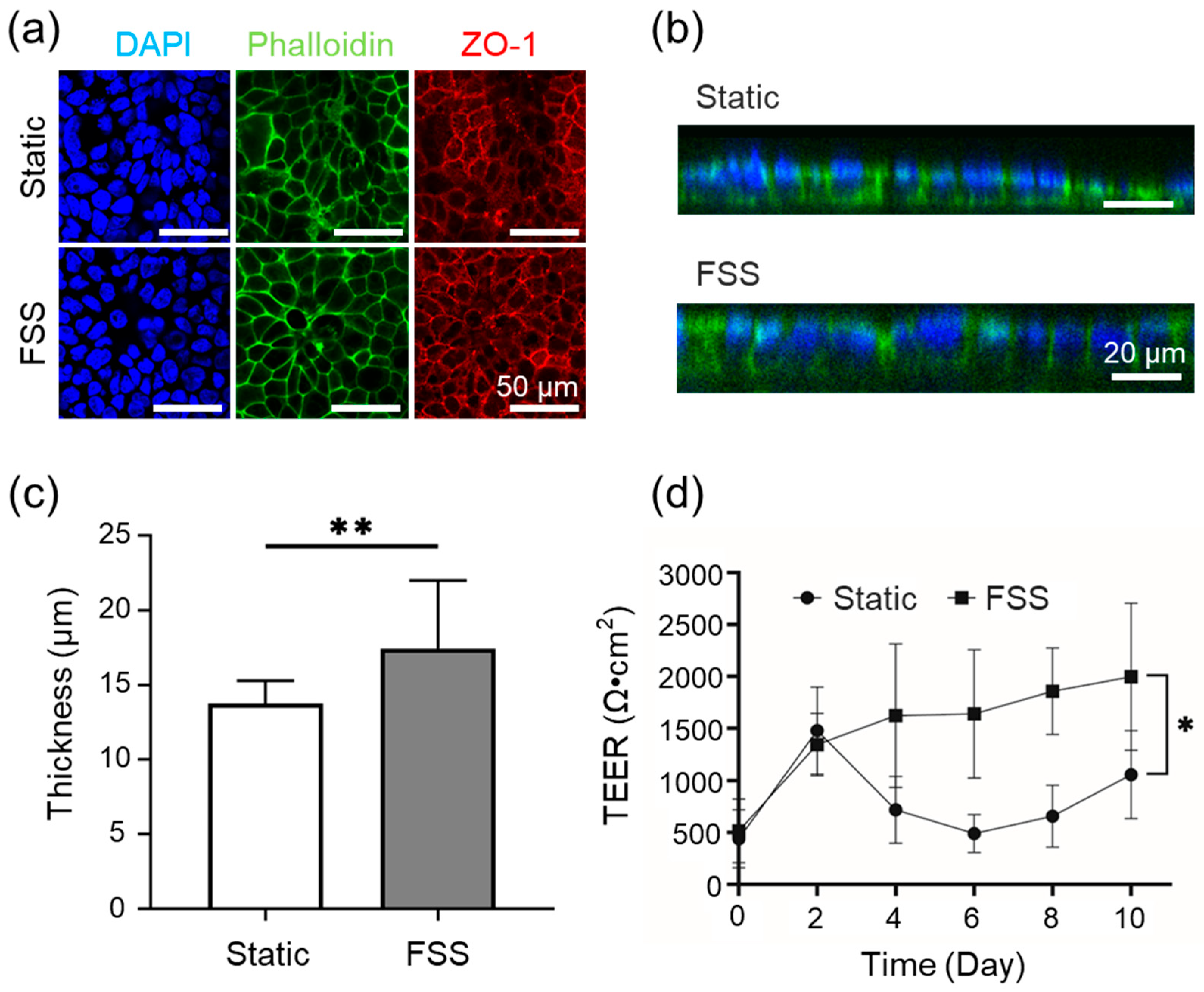
2.9. Fluorescence Staining and Imaging
To visualize cell morphology and tight junction formation, cultured cells were prepared for fluorescence staining. Cells were rinsed with PBS (+) (D8662-500mL, Sigma-Aldrich, MA, USA) and fixed using 4% paraformaldehyde (163-20145, Wako Pure Chemical Corporation, Osaka, Japan) for 15 min. After rinsing with PBS (-) (D1408-500mL, Sigma-Aldrich, MA, USA) the cells were permeabilized with 1% Triton X-100 (02081155, KISHIDA CHEMICAL, Osaka, Japan) for 10 min, followed by additional washes with PBS (-). Samples were blocked using 1% BSA/PBS for 1 h at room temperature.
Tight junctions were stained using a primary ZO-1 antibody (21773-1-AP, Proteintech, IL, USA) diluted 1:500 in 1% BSA/PBS and incubated overnight at 4 °C in the dark. On the next day, cells were washed and stained with a combined solution of DAPI (340-07971, DOJINDO, Kumamoto, Japan) (1:1000), Alexa Fluor 488 Phalloidin (PHDG1, Cytoskelton.inc., Colorado, USA) (14 µM), and Alexa 568 secondary antibody (A10042, Thermo Fisher Scientific, Massachusetts, USA) (1:1000), all diluted in 1% BSA/PBS. The staining solution was applied to the inserts and incubated for 1 h at room temperature. After the final washes with PBS (-), the samples were stored in PBS (-) and imaged using a confocal laser microscope at the Tokai University Imaging Center for Advanced Research.
2.10. Statistical Analysis
All data are presented as the mean ± standard deviation (SD) derived from a minimum of three independent experiments. Statistical analysis was conducted using Student’s t-test, with statistical significance determined at a threshold of * p < 0.05, ** p < 0.01, and *** p < 0.005.
4. Discussion
In this study, we developed and evaluated two FSSAs, FSSA-D and FSSA-I, for integration with the BioStellar™ Plate microphysiological system platform. These attachments enable the precise application of low-level FSS to epithelial cell cultures. Our combination of computational simulations and experimental flow validation demonstrated that both attachments effectively transformed the previously irregular recirculating flow within the BioStellar™ Plate chamber into stable, uniform laminar flow environments [
18]. The controlled hydrodynamic conditions produced by these devices facilitated reproducible FSS loading.
Our modular FSSA design can be adapted to a range of commercial MPS. By converting the open-top culture chamber’s recirculating flow to a controlled laminar flow, this approach is applicable to MPS platforms such as CN Bio’s PhysioMimix (CN Bio, Cambridge, England) and other open-top culture chamber-format MPSs [
19]. Our work introduces a design concept that can be adapted for use with other commercial MPSs that share similar open-top culture chamber formats. Although we developed our attachments for the BioStellar™ Plate’s standard microplate size, the core design principles and modular approach offer a flexible framework that can be adjusted for other MPS platforms. While we validated the design with intestinal epithelial cells, the controlled FSS environment created by these attachments could also benefit other mechanosensitive cell types. For example, endothelial cells, essential for vascular modeling and dependent on physiological fluidic shear stress for proper function, could benefit [
13,
16]. Offering controlled mechanical stimulation without changing standard culture formats, these accessories can advance multi-organ and disease modeling research across the MPS field.
Biological assessments utilizing Caco-2 cells indicated that static and FSS conditions using both FSSA-D and FSSA-I supported the formation of a confluent monolayer. Cells exposed to controlled FSS exhibited enhanced transepithelial electrical resistance (TEER), increased epithelial layer thickness, and improved barrier function compared to static controls. The FSS of 0.02 dyn/cm
2 in the cell culture experiment is a physiologically relevant mechanical stimulus closely mimicking the in vivo environment for intestinal epithelial cells [
20,
21,
22,
23]. This value has been reported as optimal in prior studies: for example, Shin et al. demonstrated that flow-dependent physical cues control human intestinal morphogenesis in microengineered gut-on-chip systems, while other research has shown that physiological shear stress enhances differentiation, mucus formation, barrier integrity, and 3D tissue architecture at this stress level [
20,
21,
22,
23,
24,
25]. Most notably, quantitative functional assessment of epithelial barrier properties, as measured by TEER, was possible in the FSSA-I configuration [
26]. Here, the application of FSS resulted in a progressive increase and stabilization of TEER values, indicative of tighter junctions and improved barrier integrity [
27,
28]. These results corroborate the extensive literature indicating that mechanical cues from physiologically relevant FSS accelerate epithelial maturation, enhance cytoskeletal and junctional organization, and support the development of more predictive and robust in vitro intestinal models [
20,
21,
22,
23,
29]. These findings confirm that low-level FSS improves architecture and barrier function, demonstrating the effectiveness of the BioStellar™ Plate system with FSSAs and its reliability in modeling physiological epithelial responses [
25,
30,
31].
In conclusion, incorporating these FSSAs significantly enhances the functional capabilities of the BioStellar™ Plate platform by introducing controllable mechanical stimulation while ensuring compatibility with standard culture formats. These design principles lay the groundwork for using controlled fluidic shear stress with different cell types and commercial MPS platforms. This could help more researchers use mechanical stimulation that better reflects in vivo conditions. Future studies that include a wider range of cell types, such as endothelial and hepatic cells, will help demonstrate the broad applicability of this approach for disease modeling and drug development [
8]. Our FSSAs provide a straightforward and accessible approach for mimicking physiologically relevant flow conditions in vitro. Our attachments help investigate FSS-mediated effects on epithelial cell function and intestinal barrier models within MPSs.