3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine
Abstract
1. Introduction
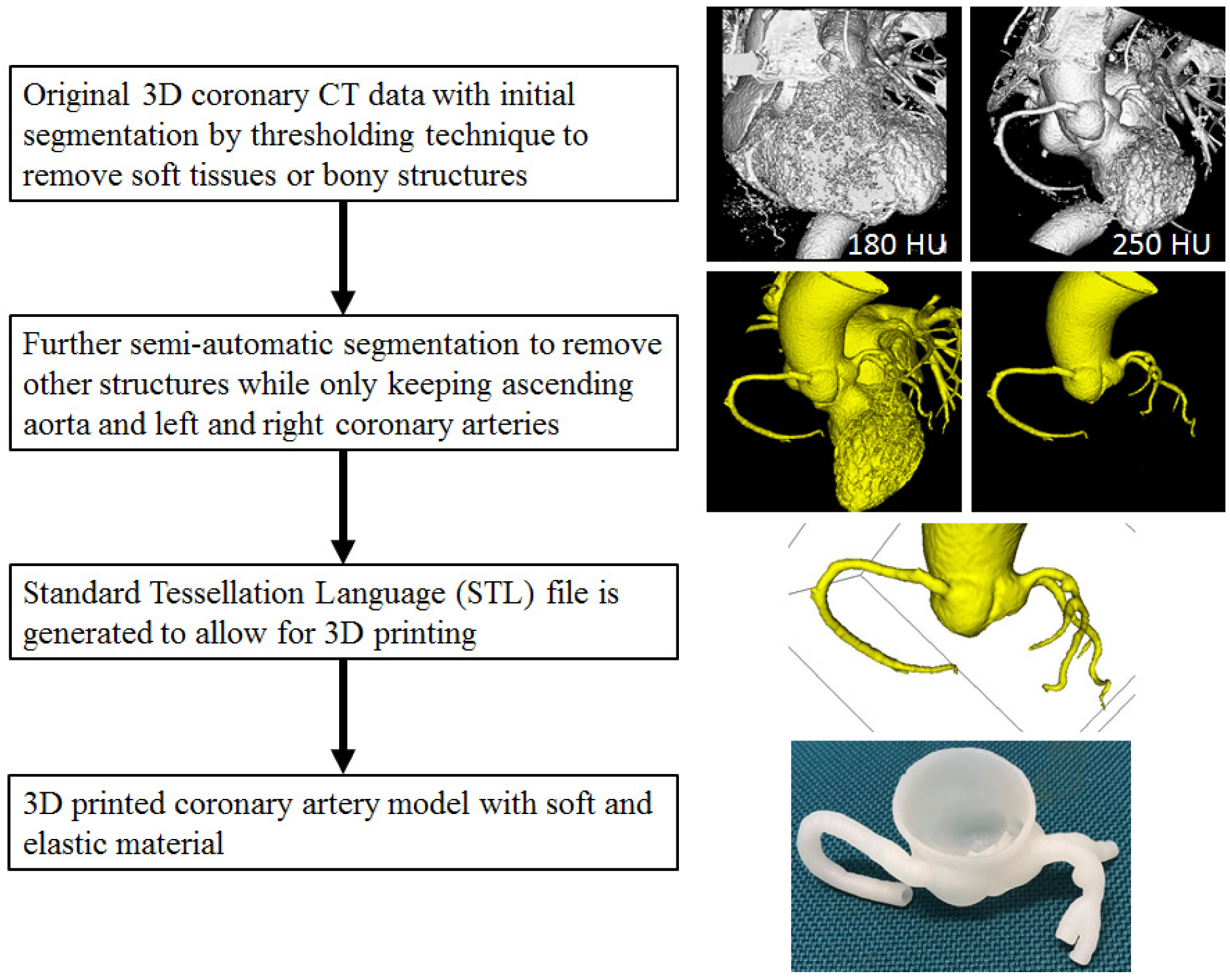
2. Processes from Image Post-Processing to 3D Printed Models
3. 3D Printers and Printing Materials
4. Education Value of 3D Printed Models in Cardiovascular Disease
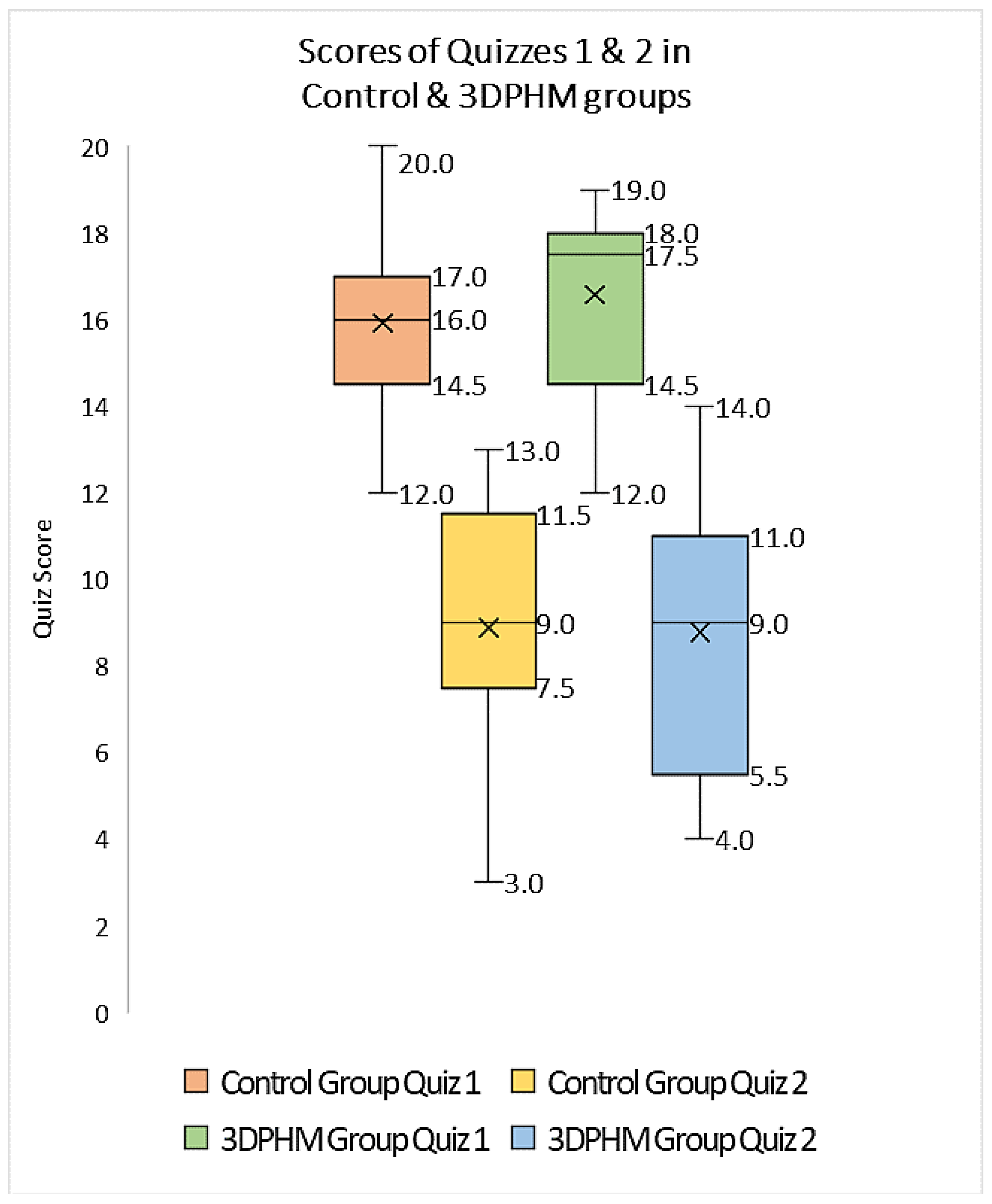
4.1. Medical Student Education
4.2. Clinician Education
5. Clinical Applications of 3D Printed Models in Cardiovascular Disease
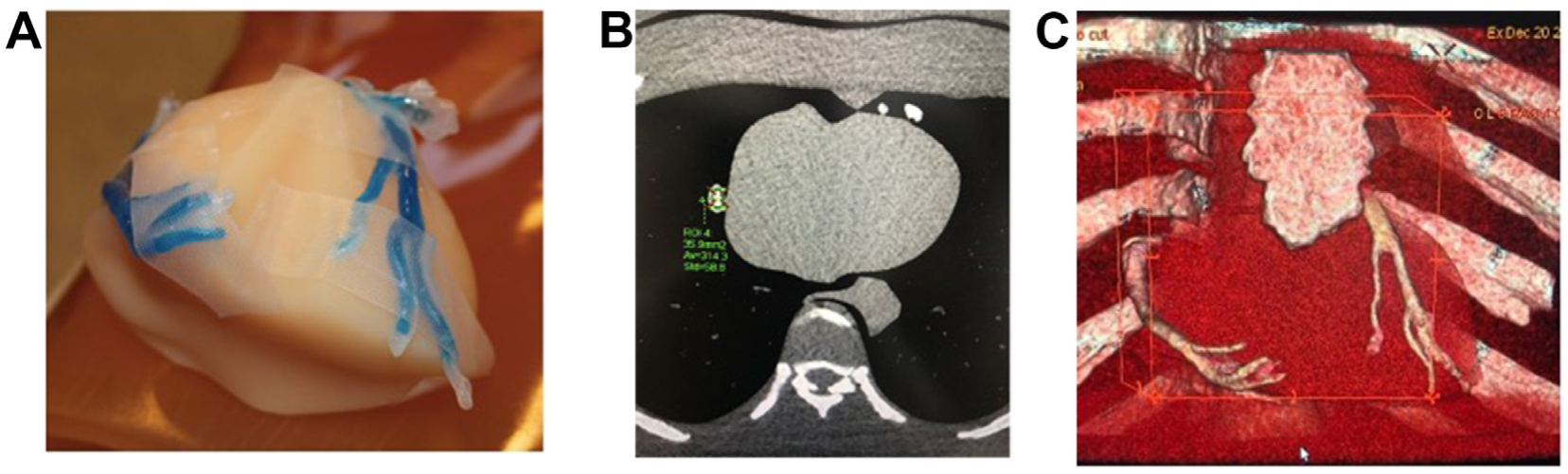
5.1. Pre-Surgical Planning of Complex Cardiac or Cardiovascular Procedures
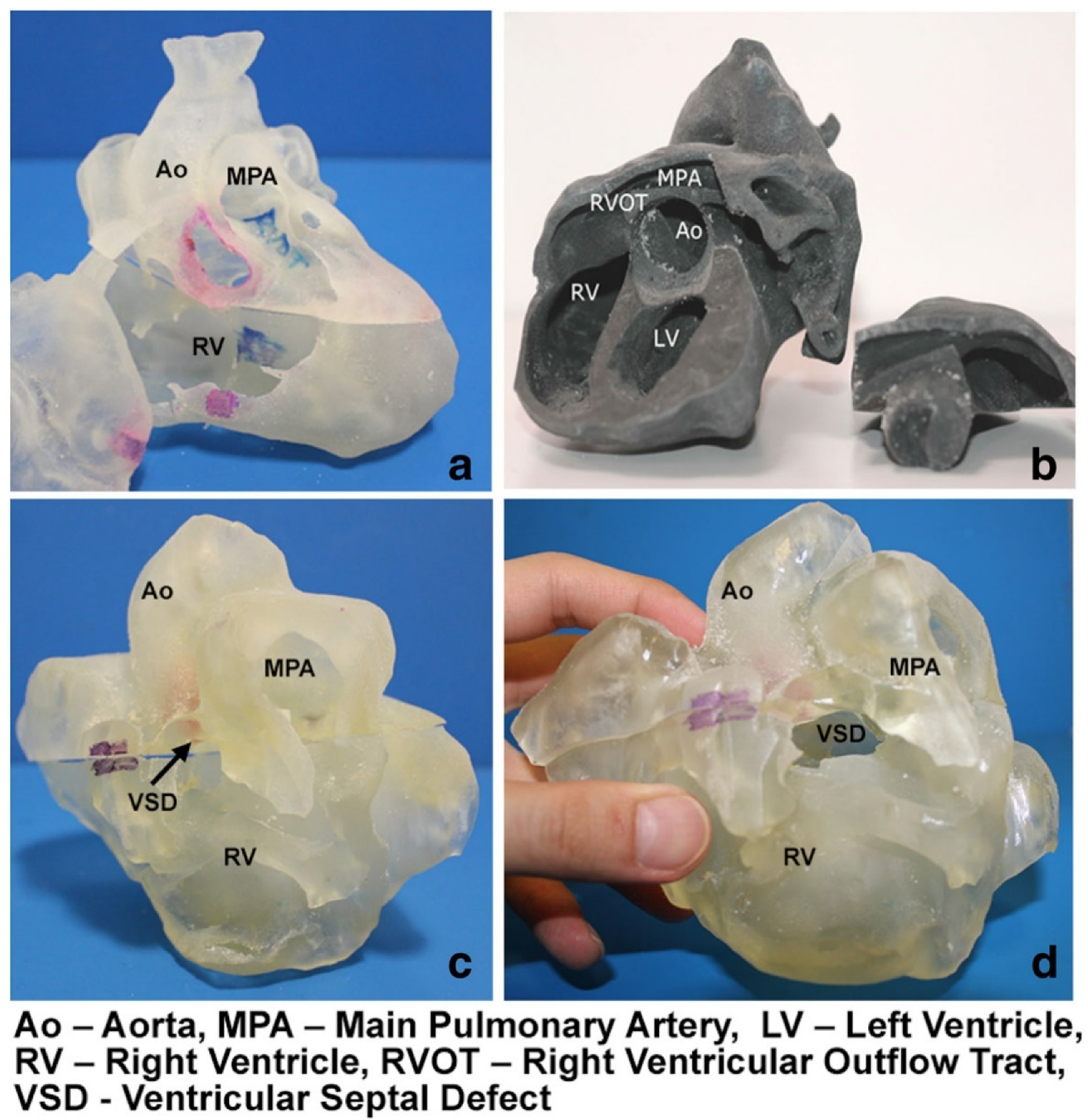
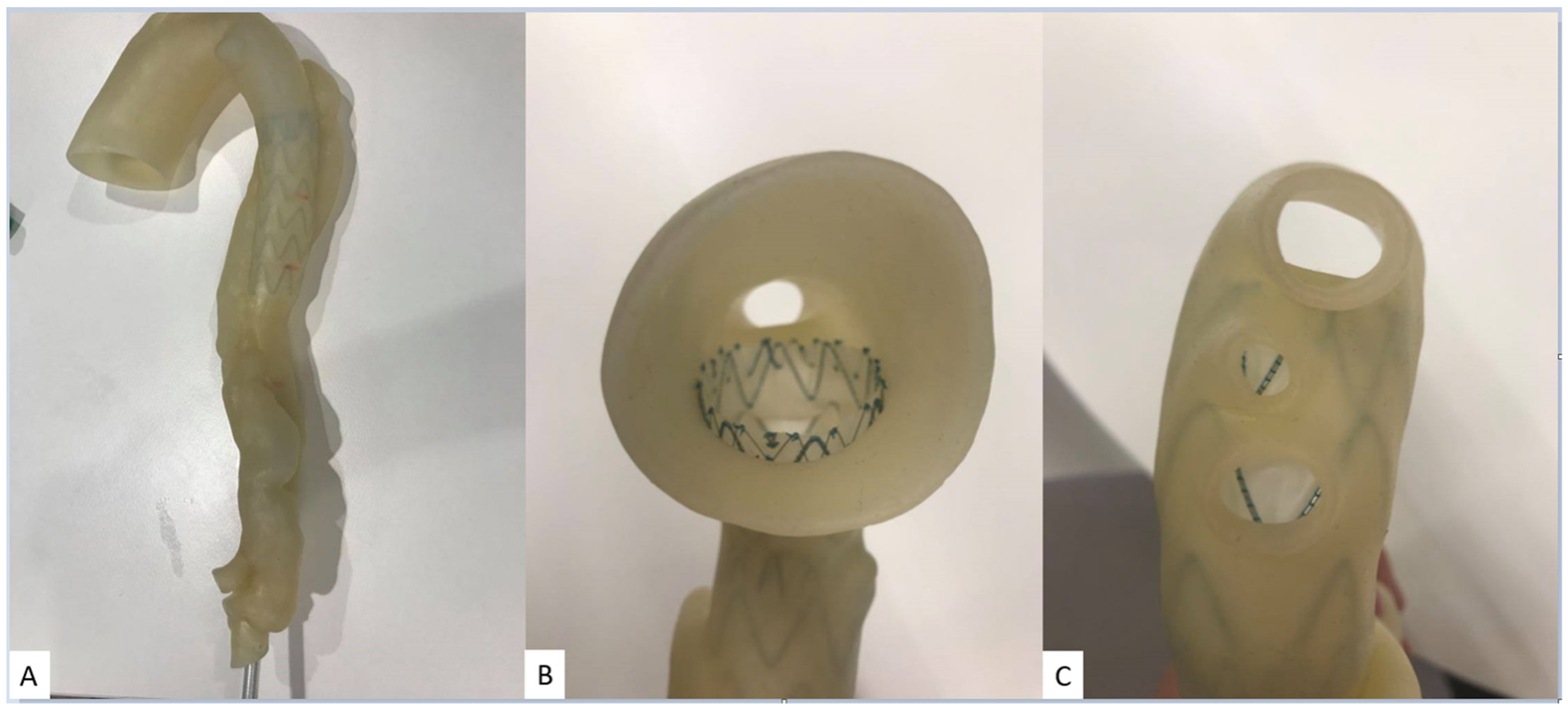
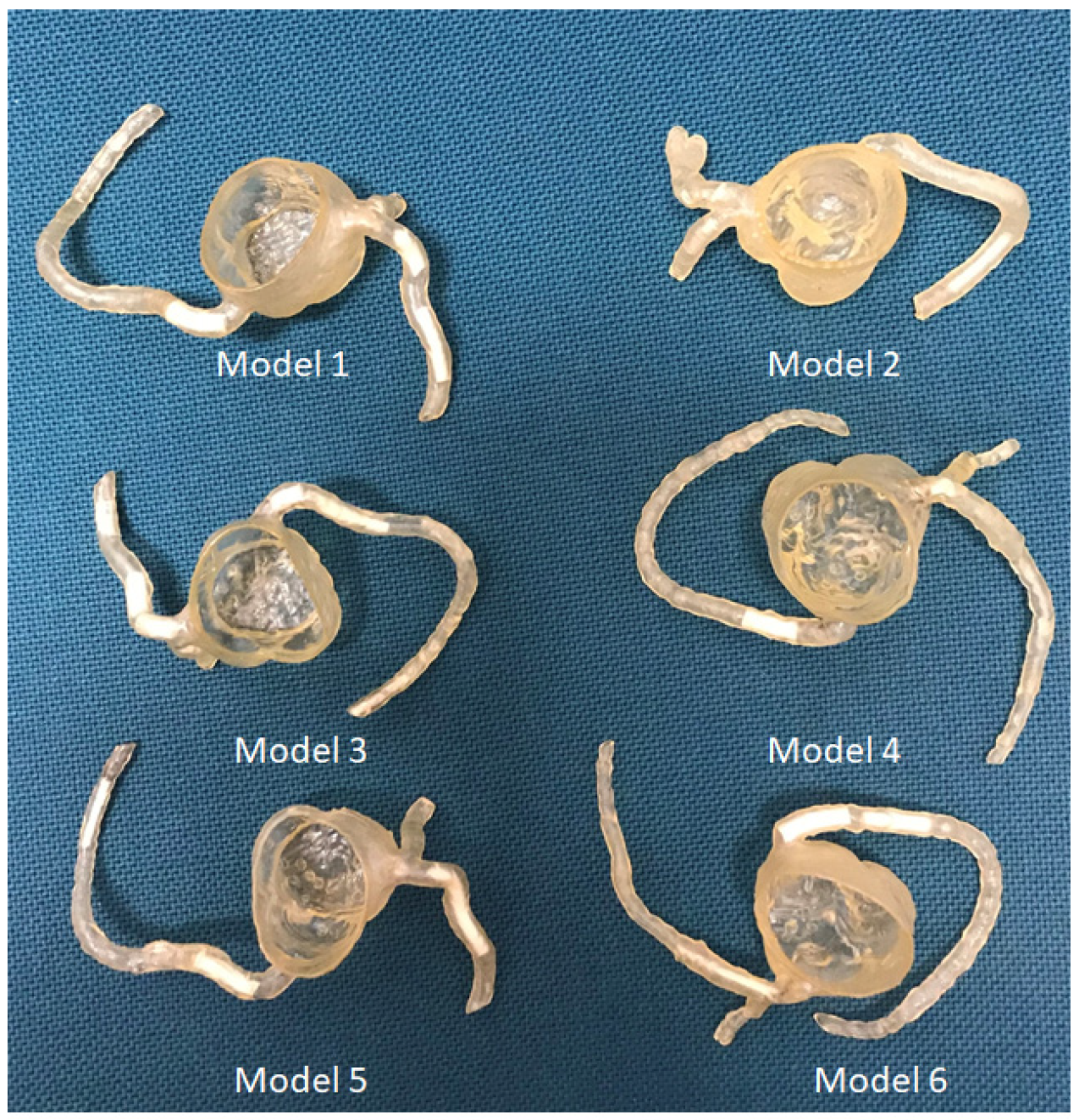
5.2. Simulation of Surgical or Interventional Procedures
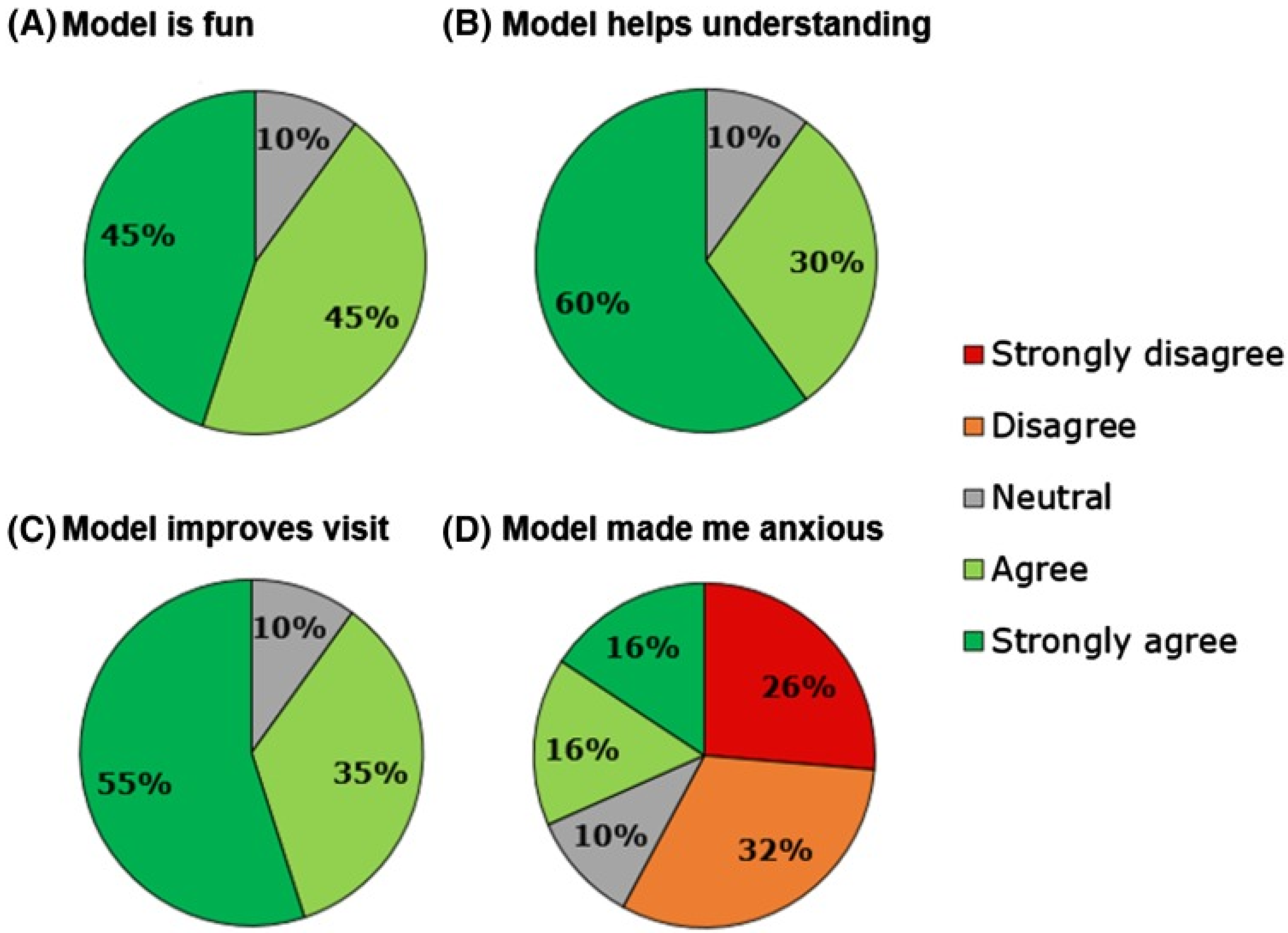
5.3. Enhancement of Doctor-to-Patient Communication
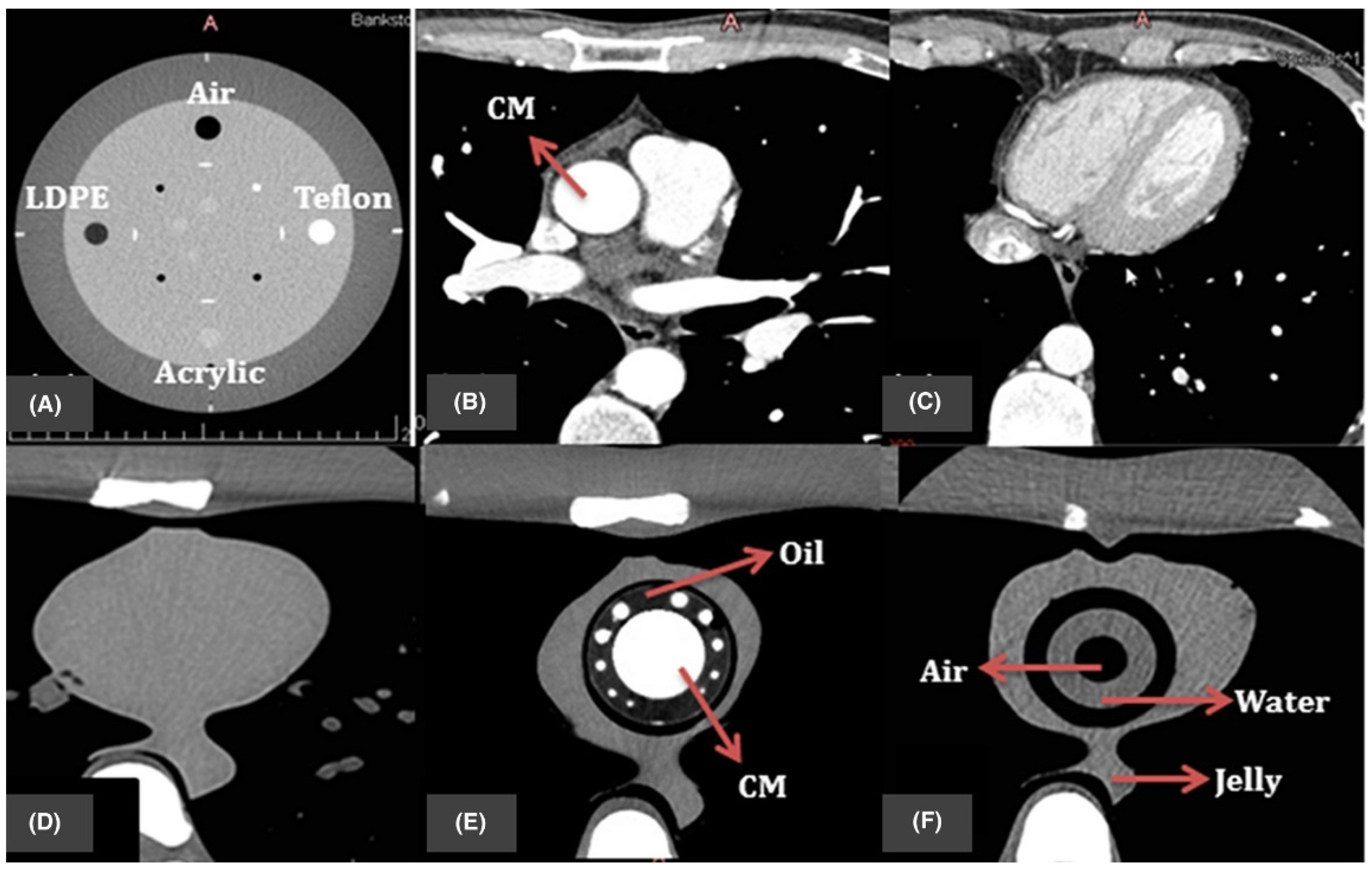
5.4. Development of Optimal CT Scanning Protocols
6. Limitations, Barriers and Future Directions
7. Summary and Concluding Remarks
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Giannopoulos, A.A.; Steigner, M.L.; George, E.; Barile, M.; Hunsaker, A.R.; Rybicki, F.J.; Mitsouras, D. Cardiothoracic applications of 3-dimensional printing. J. Thorac. Imaging 2016, 31, 253–272. [Google Scholar] [CrossRef]
- Witowski, J.; Wake, N.; Grochowska, A.; Sun, Z.; Budzynski, A.; Major, P.; Popiela, T.J.; Pedziwiatr, M. Investigating accuracy of 3d printed liver models with computed tomography. Quant. Imaging Med. Surg. 2019, 9, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Perica, E.; Sun, Z. Patient-specific three-dimensional printing for pre-surgical planning in hepatocellular carcinoma treatment. Quant. Imaging Med. Surg. 2017, 7, 668–677. [Google Scholar] [CrossRef]
- Costello, J.; Olivieri, L.; Krieger, A.; Thabit, O.; Marshall, M.B.; Yoo, S.J.; Kim, P.C.; Jonas, R.A.; Nath, D.S. Utilizing three-dimensional printing technology to assess the feasibility of high-fidelity synthetic ventricular septal defect models for simulation in medical education. World. J. Pediatr. Congenit. Heart. Surg. 2014, 5, 421–426. [Google Scholar] [CrossRef]
- Costello, J.P.; Olivieri, L.J.; Su, L.; Krieger, A.; Alfares, F.; Thabit, O.; Marshall, M.B.; Yoo, S.J.; Kim, P.C.; Jonas, R.A.; et al. Incorporating three-dimensional printing into a simulation-based congenital heart disease and critical care training curriculum for resident physicians. Congenit. Heart. Dis. 2015, 10, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Javan, R.; Zeman, M. A prototype educational model for hepatobiliary interventions: Unveiling the role of graphic designers in medical 3D printing. J. Digit. Imaging 2018, 31, 133–143. [Google Scholar] [CrossRef]
- Sun, Z.; Lau, I.; Wong, Y.H.; Yeong, C.H. Personalized three-dimensional printed models in congenital heart disease. J. Clin. Med. 2019, 8, 522. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Lee, S. A systematic review of 3D printing in cardiovascular and cerebrovascular diseases. Anatol. J. Cardiol. 2017, 17, 423–435. [Google Scholar]
- Lupulescu, C.; Sun, Z. A systematic review of the clinical value and applications of three-dimensional printing in renal surgery. J. Clin. Med. 2019, 8, 990. [Google Scholar] [CrossRef]
- Sun, Z.; Liu, D. A systematic review of clinical value of three-dimensional printing in renal disease. Quant. Imaging Med. Surg. 2018, 8, 311–325. [Google Scholar] [CrossRef]
- Lau, I.; Sun, Z. Three-dimensional printing in congenital heart disease: A systematic review. J. Med. Radiat. Sci. 2018, 65, 226–236. [Google Scholar] [CrossRef]
- Bhatla, P.; Tretter, J.T.; Chikkabyrappa, S.; Chakravarti, S.; Mosca, R.S. Surgical planning for a complex double-outlet right ventricle using 3D printing. Echocardiography 2017, 34, 802–804. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Milano, E.G.; Capelli, C.; Wray, J.; Shearn, A.I.; Caputo, M.; Bucciarelli-Ducci, C.; Taylor, A.M.; Schievano, S. Three-dimensional printing in congenital heart disease: Considerations on training and clinical implementation from a teaching session. Int. J. Artif. Organs 2019, 42, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Ho, D.; Squelch, A.; Sun, Z. Modelling of aortic aneurysm and aortic dissection through 3D printing. J. Med. Radiat. Sc. 2017, 64, 10–17. [Google Scholar] [CrossRef]
- Perica, E.R.; Sun, Z. A systematic review of three-dimensional printing in liver disease. J. Digit. Imaging 2018, 31, 692–701. [Google Scholar] [CrossRef]
- Lau, I.; Sun, Z. Dimensional accuracy and clinical value of 3D printed models in congenital heart disease: A systematic review and meta-analysis. J. Clin. Med. 2019, 8, 1483. [Google Scholar] [CrossRef]
- Anwar, S.; Rockefeller, T.; Raptis, D.; Woodard, P.; Eghtesady, P. 3D printing provides a precise approach in the treatment of tetralogy of Fallot, pulmonary atresia with major aortopulmonary collateral arteries. Curr. Treat. Options. Cardiovasc. Med. 2018, 20, 5. [Google Scholar] [CrossRef]
- Godnell, J.; Pietila, T.; Samuel, B.P.; Kurup, H.K.N.; Haw, M.P.; Vettukattil, J.J. Integration of computed tomography and three-dimensional echocardiography for hybrid three-dimensional printing in congenital heart disease. J. Digit. Imaging 2016, 29, 665–669. [Google Scholar] [CrossRef]
- Ripley, B.; Kelil, T.; Cheezum, M.K.; Goncalves, A.; Di Carli, M.F.; Rybicki, F.J.; Steigner, M.; Mitsouras, D.; Blankstein, R. 3D printing based on cardiac CT assists anatomic visualization prior to transcatheter aortic valve replacement. J. Cardiovasc. Comput. Tomor. 2016, 10, 28–36. [Google Scholar] [CrossRef]
- Loke, Y.H.; Harahsheh, A.S.; Krieger, A.; Olivier, L.J. Usage of 3D models of tetralogy of Fallot for medical education: Impact on learning congenital heart disease. BMC. Med. Educ. 2017, 7, 54. [Google Scholar] [CrossRef]
- Sun, Z. Clinical applications of patient-specific 3D printed models in cardiovascular disease: Current status and future directions. Biomolecules 2020, 10, 1577. [Google Scholar] [CrossRef]
- Gomez-Ciriza, G.; Gomez-Cia, T.; Rivas-Gonzalez, J.A.; Velasco Forte, M.N.; Valverde, I. Affordable three-dimensional printed heart models. Front. Cardiovasc. Med. 2021, 8, 642011. [Google Scholar] [CrossRef]
- Moore, R.A.; Riggs, K.W.; Kourtidou, S.; Schneider, K.; Szugye, N.; Troja, W.; D’Souza, G.; Rattan, M.; Bryant, R., 3rd; Taylor, M.D.; et al. Three-dimensional printing and virtual surgery for congenital heart procedural planning. Birth. Defects. Res. 2018, 110, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Kiraly, L.; Shah, N.C.; Abdullah, O.; Al-Ketan, O.; Rowshan, R. Three-dimensional virtual and printed prototypes in complex congenital and pediatric cardiac surgery-A multidisciplinary team-learning experience. Biomolecules 2021, 11, 1703. [Google Scholar] [CrossRef]
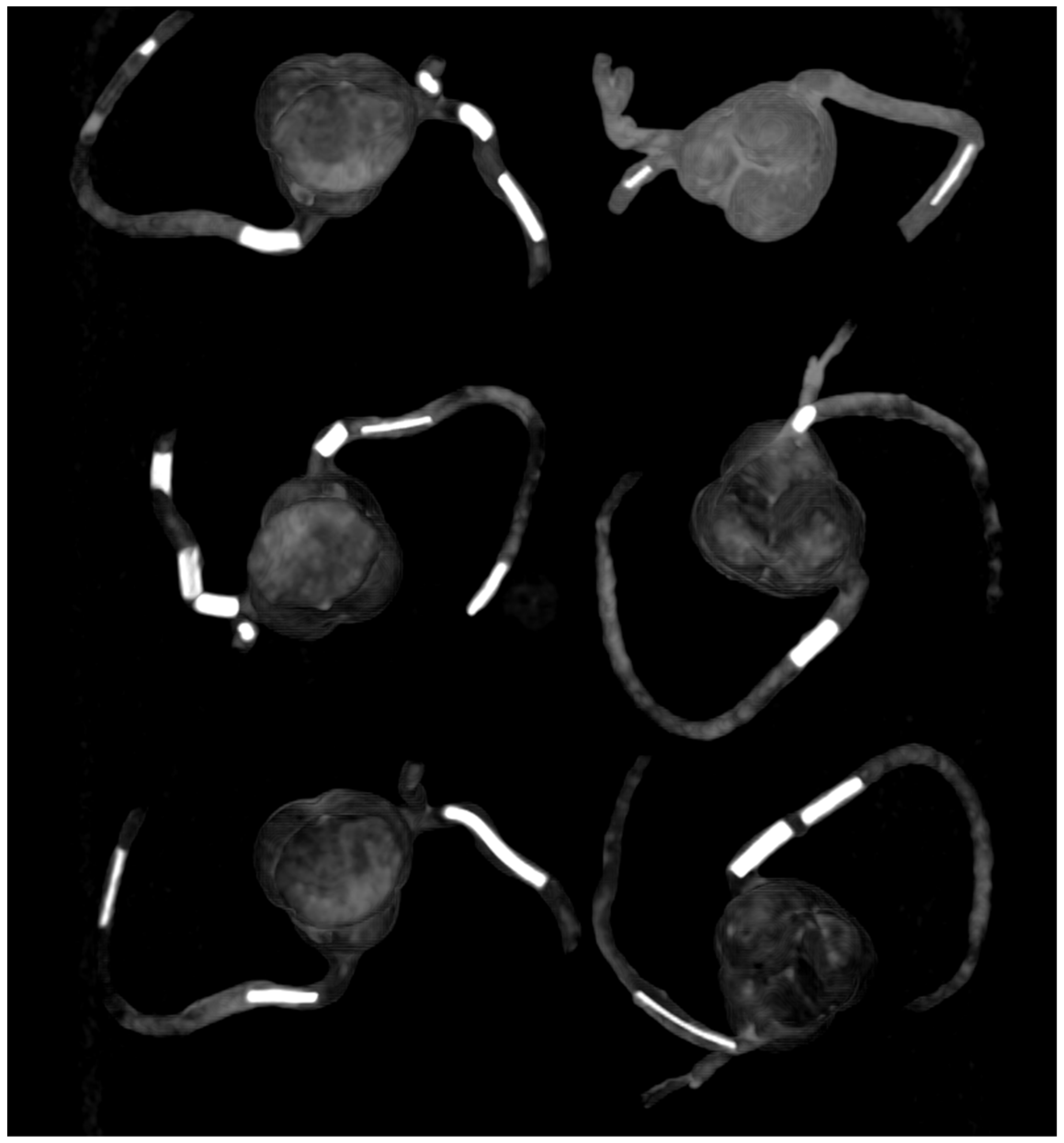
- Wu, C.A.; Squelch, A.; Jansen, S.; Sun, Z. Optimization of computed tomography angiography protocols for follow-up type B aortic dissection patients by using 3D printed model. Appl. Sci. 2021, 11, 6844. [Google Scholar] [CrossRef]
- Garas, M.; Vacccarezza, M.; Newland, G.; McVay-Doonbusch, K.; Hasani, J. 3D-printed speciamens as a valuable tool in anatomy education: A pilot study. Ann. Anat. 2018, 219, 57–64. [Google Scholar] [CrossRef] [PubMed]
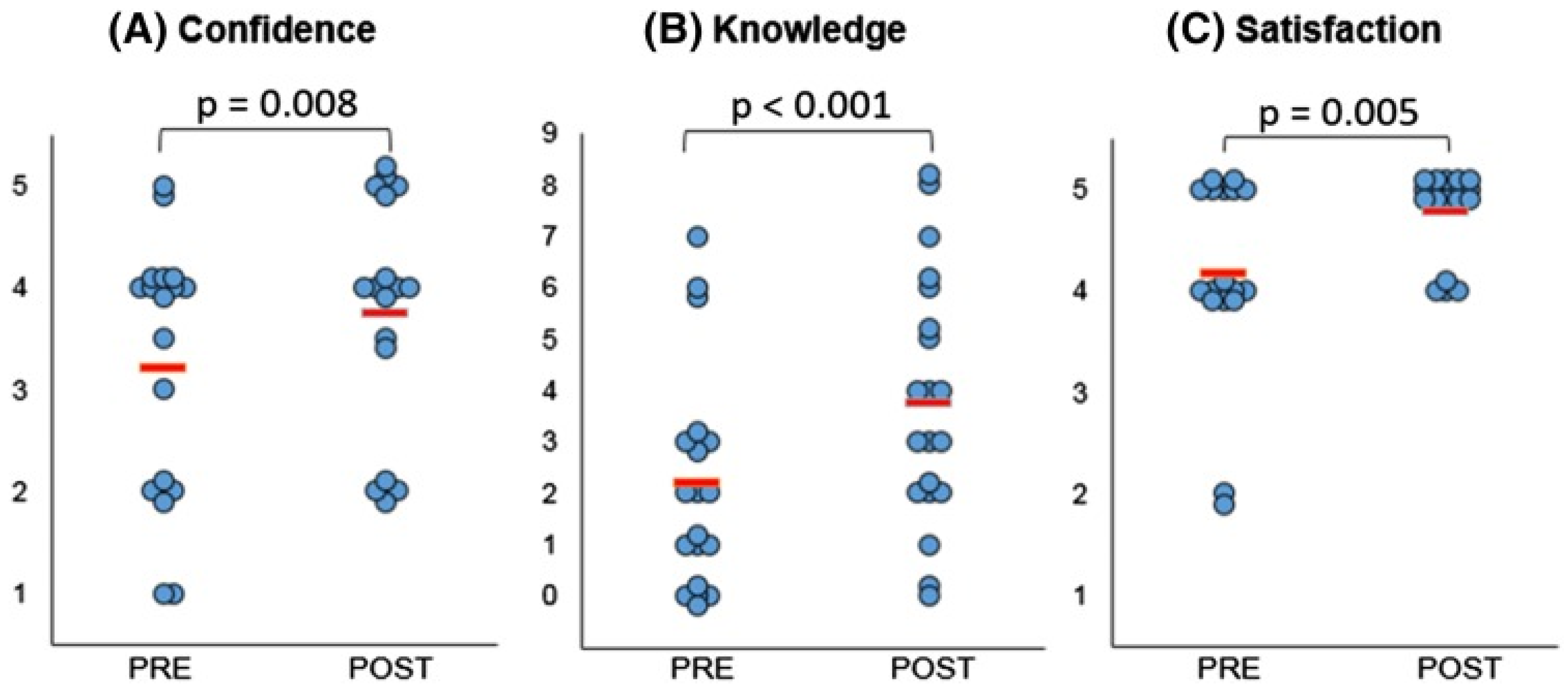
- Lau, I.; Sun, Z. The role of 3D printed heart models in immediate and long-term knowledge retention in medical education. Rev. Cardiovasc. Med. 2022, 23, 22. [Google Scholar] [CrossRef]
- Karsenty, C.; Guitarte, A.; Dulac, Y.; Briot, J.; Hascoet, S.; Vincent, R.; Delepaul, B.; Vignaud, P.; Djeddai, C.; Hadeed, K.; et al. The usefulness of 3D printed heart models for medical student education in congenital heart disease. BMC. Med. Edc. 2021, 21, 480. [Google Scholar] [CrossRef]
- Lim, K.H.; Loo, Z.Y.; Goldie, S.; Adams, J.; McMenamin, P. Use of 3D printed models in medical education: A randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anat. Sci. Educ. 2016, 9, 213–221. [Google Scholar] [CrossRef]
- Smerling, J.; Marboe, C.C.; Lefkowitch, J.H.; Pavilicova, M.; Bacha, E.; Einstein, A.J.; Naka, Y.; Glickstein, J.; Farooqi, K.M. Utility of 3D printed cardiac models for medical student education in congenital heart disease: Across a spectrum of disease severity. Pediatr. Cardiol. 2019, 40, 1258–1265. [Google Scholar] [CrossRef] [PubMed]
- Su, W.; Xiao, Y.; He, S.; Huang, P.; Deng, X. Three-dimensional printing models in congenital heart disease education for medical students: A controlled comparative study. BMC. Med. Educ. 2018, 18, 178. [Google Scholar] [CrossRef]
- Lau, I.; Gupta, A.; Sun, Z. Clinical value of virtual reality versus 3D printing in congenital heart disease. Biomolecules 2021, 11, 884. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.W.; Secker, M.D. Use of 3D models of vascular rings and slings to improve resident education. Congenit. Heart. Dis. 2017, 12, 578–582. [Google Scholar] [CrossRef] [PubMed]
- Krishnasamy, S.; Mokhtar, R.A.R.; Singh, R.; Sivallingam, S.; Abdul Aziz, Y.F.; Mathaneswaran, V. 3D rapid prototyping heart model validation for teaching and learning-A pilot project in a teaching institution. Braz. J. Cardiothorac. Surg. 2021, 36, 707–716. [Google Scholar]
- Valverde, I.; Gomez, G.; Byrne, N.; Anwar, S.; Silva Cerpa, M.A.; Talavera, M.M.; Pushparajah, K.; Velasco Forte, M.N. Criss-cross heart three-dimensional printed models in medical education: A multicentre study on their value as a supporting tool to conventional imaging. Anat. Sci. Educ. 2022, 15, 719–730. [Google Scholar] [CrossRef] [PubMed]
- White, S.C.; Sedler, J.; Jones, T.W.; Seckeler, M. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects. Congenit. Heart. Dis. 2018, 13, 1045–1049. [Google Scholar] [CrossRef]
- Tan, H.; Huang, E.; Deng, X.; Ouyang, S. Application of 3D printing technology combined with PBL teaching model in teaching clinical nursing in congenital heart surgery: A case-control study. Medicine 2021, 100, 20. [Google Scholar] [CrossRef]
- Biglino, G.; Capelli, C.; Koniordou, D.; Robertshaw, D.; Leaver, L.K.; Schievano, S.; Taylor, A.M.; Wray, J. Use of 3D models of congenital heart disease as an education tool for cardiac nurses. Congenit. Heart. Dis. 2017, 12, 113–118. [Google Scholar] [CrossRef]
- Liang, J.; Zhao, X.; Pan, G.; Zhang, G.; Zhao, D.; Xu, J.; Li, D.; Lu, B. Comparison of blood pool and myocardial 3D printing in the diagosis of types of congenital hear disease. Sci. Rep. 2022, 12, 7136. [Google Scholar] [CrossRef]
- Sutherland, J.; Belek, J.; Sheikh, A.; Chepelev, L.; Althobaity, W.; Chow, B.J.W.; Mitsouris, D.; Christensen, A.; Rybicki, F.J.; La Russa, D.J. Applying modern virtual and augmented reality technologies to medical images and models. J. Digit. Imaging 2019, 32, 38–53. [Google Scholar] [CrossRef]
- Dhar, P.; Rocks, T.; Samarasinghe, R.M.; Stephenson, G.; Smith, C. Augmented reality in medical education: Students’ experience and learning outcomes. Med. Educ. Online 2021, 26, 1953953. [Google Scholar] [CrossRef]
- Patel, N.; Costa, A.; Sanders, S.P.; Ezon, D. Stereoscopic virtual reality does not improve knowledge retention of congenital heart disease. Int. J. Cardiovasc. Imaging 2021, 37, 2283–2290. [Google Scholar] [CrossRef]
- Maresky, H.S.; Oikonomou, A.; Ali, I.; Ditkofsky, N.; Pakkal, M.; Ballyk, B. Virtual reality and cardiac anatomy: Exploring immersive three-dimensional cardiac imaging, a pilot study in undergraduate medical anatomy education. Clin. Anat. 2019, 32, 238–243. [Google Scholar] [CrossRef]
- Barteit, S.; Lanfermann, L.; Barnighausen, T.; Neuhann, F.; Beiersmann, C. Augmentted reality, mixed and virtual reality-based head-mounted devices for medical education: Systematic review. JMIR. Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef]
- Illmann, C.; Ghadiry-Tavi, R.; Hosking, M.; Harris, K.C. Utility of 3D printed cardiac models in congenital heart disease: A scoping review. Heart 2020, 106, 1631–1637. [Google Scholar] [CrossRef]
- Bernhard, B.; Illi, J.; Gloecker, M.; Pilgrim, T.; Praz, F.; Windecker, S.; Haeberlin, A.; Grani, C. Imaging-based, patient-specific three-dimensional printing to plan, train, and guide cardiovascular interventions: A systematic review and meta-analysis. Heart Lung Circ. 2022, 31, 1203–1218. [Google Scholar] [CrossRef]
- Valverde, I.; Gomez-Ciriza, G.; Hussain, T.; Suarez-Mejias, C.; Velasco-Forte, M.N.; Byrne, N.; Ordonex, A.; Gonzalez-Calle, A.; Anderson, D.; Hazekamp, M.G.; et al. Three dimensional printed models for surgical planning of complex congenital heart defects: An international multicenter study. Eur. J. Cardiothorac. Surg. 2017, 52, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Liufu, R.; Wen, S.; Qiu, H.; Liu, X.; Chen, X.; Yuan, H.; Huang, M.; Zhuang, J. Three-dimensional printing, virtual reality and mixed reality for pulmonary atresia: Early surgical outcomes evaluation. Heart Lung Circ. 2021, 30, 296–302. [Google Scholar]
- Guo, H.; Wang, Y.; Dai, J.; Ren, C.; Li, J.; Lai, Y. Application of 3D printing in the surgical planning of hypertrophic obstructive cardiomyopathy and physician-patient communication: A preliminary study. J. Thorac. Dis. 2018, 10, 867–873. [Google Scholar] [CrossRef]
- Ryan, J.; Plasencia, J.; Richardson, R.; Velez, D.; Nigro, J.J.; Pophal, S.; Frakes, D. 3D printing for congenital heart disease: A single site’s initial three-year experience. 3D Print. Med. 2018, 4, 10. [Google Scholar] [CrossRef]
- Zhao, L.; Zhou, S.; Fan, T.; Li, B.; Liang, W.; Dong, H. Three-dimensional printing enhances preparation for repair of double outlet right ventricular surgery. J. Card. Surg. 2018, 33, 24–27. [Google Scholar] [CrossRef]
- Ghosh, R.M.; Jolley, M.A.; Mascio, C.E.; Chen, J.M.; Fuller, S.; Rome, J.J.; Silvestro, E.; Whitehead, K.K. Clinical 3D modeling to guide pediatric cardiothoracic surgery and intervention using 3D printed anatomic models, computer aided design and virtual reality. 3D Pring. Med. 2022, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Russo, J.J.; Yuen, T.; Tan, J.; Willson, A.B.; Gurvitch, R. Assessment of coronary artery obstruction risk during transcatheter aortic valve replacement utilising 3D-printing. Heart Lung Circ. 2022, 31, 1134–1143. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Yang, F.; Cheung, S.H.; Chan, A.K.Y.; Wang, D.D.; Lam, Y.Y.; Chow, M.C.K.; Leong, M.C.W.; Kam, K.K.; So, K.C.Y.; et al. Device sizing guided by echocardiography-based three-dimensional printing is associated with superior outcome after percutaneous left atrial appendage occlusion. J. Am. Soc. Echocardiogr. 2019, 32, 708–719. [Google Scholar] [CrossRef] [PubMed]
- Hell, M.H.; Achenbach, S.; Yoo, I.S.; Franke, J.; Blackutzik, F.; Roether, J.; Graf, V.; Raaz-Schrauder, D.; Marvann, M.; Schlundt, C. 3D printing for sizing left atrial appendage closure device: Head-to head comparison with computed tomography and transoesophageal echocardiography. EuroIntervention 2017, 13, 1234–1241. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Yao, Q.; Shen, B.; Shu, M.; Zhong, L.; Wang, X.; Song, Z. Application of 3D printing technology to left atrial appendage occlusion. Int. J. Cardiol. 2017, 231, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Conti, M.; Marconi, S.; Muscogiuri, G.; Guglielmo, M.; Baggiano, A.; Italiano, G.; Mancini, M.E.; Auricchio, F.; Andreini, D.; Rabbat, M.G.; et al. Left atrial appendage closure guided by 3D computed tomography printing technology: A case control study. J. Cardiovasc. Comput. Tomogr. 2019, 13, 336–339. [Google Scholar] [CrossRef]
- Goitein, O.; Fink, N.; Guettar, V.; Beinart, R.; Brodov, Y.; Konen, E.; Goitein, D.; Segni, E.D.; Grupper, A.; Glikson, M. Printed MDCT 3D models for prediction of left atrial appendage (LAA) occlude device size: A feasibility study. EuroIntervention 2017, 13, e1076–e1079. [Google Scholar] [CrossRef]
- Torres, I.O.; De Luccia, N. A simulator for training in endovascular aneurysm repair: The use of three dimensional printers. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 247–253. [Google Scholar] [CrossRef]
- Karkkainen, J.M.; Sandri, G.; Tenorio, E.R.; Alexander, A.; Bjellum, K.; Matsumoto, J.; Morris, J.; Mendes, B.C.; DeMartino, R.R.; Oderich, G.S. Simulation of endovascular aortic repair using 3D printed abdominal aortic aneurysm model and fluid pump. Cardiovasc. Intervent. Radiol. 2019, 42, 1627–1634. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, R.; Zech, C.J.; Takes, M.; Brantner, P.; Thieringer, F.; Dentschmann, M.; Hergan, K.; Scharinger, B.; Hecht, S.; Rezar, R.; et al. Vascular 3D printing with a novel biological tissue mimicking resin for patient-specific procedure simulations in interventional radiology: A feasibility study. J. Digit. Imaging 2022, 35, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Sheu, A.Y.; Laidlaw, G.L.; Fell, J.C.; Triana, B.P.; Goetti, C.S.; Shah, R.P. Custom 3-dimentional printed ultrasound-compatible vascular access models: Training medical students for vascular access. J. Vasc. Interv. Radiol. 2019, 30, 922–927. [Google Scholar] [CrossRef] [PubMed]
- Goudie, C.; Kinnin, J.; Bartellas, M.; Gullipalli, R.; Dubrowski, A. The use of 3D printed vasculature for simulation-based medical education within interventional radiology. Cureus 2019, 11, e4381. [Google Scholar] [CrossRef] [PubMed]
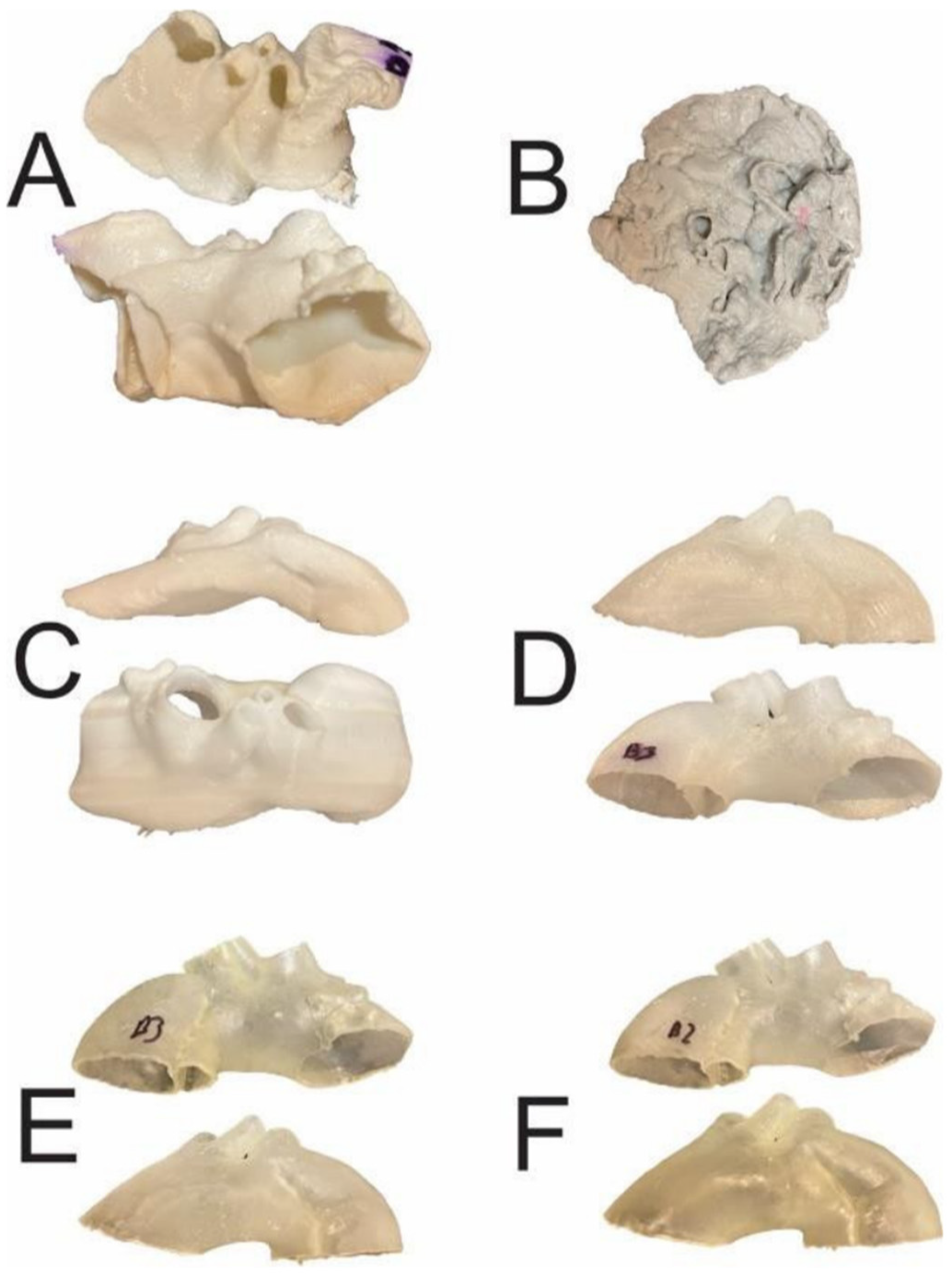
- Yoo, S.J.; Spray, T.; Austin, E.H.; Yun, T.J.; van Arsdell, G.S. Hands-on surgical training of congenital heart surgery suing 3-dimensional print models. J. Thorac. Cardiovasc. Surg. 2017, 153, 15301–15540. [Google Scholar] [CrossRef] [PubMed]
- Brunner, B.S.; Thierij, A.; Jakob, A.; Tengler, A.; Grab, M.; Thierfelder, N.; Leuner, C.J.; Haas, N.A.; Hopfner, C. 3D-printed heart models for hands-on training in pediatric cardiology-the future of modern learning and teaching? GMS. J. Med. Educ. 2022, 39, Doc23. [Google Scholar]
- Rynio, P.; Galant, K.; Wojcik, L.; Gryorcewicz, B.; Kazimierczak, A.; Falkowski, P.; Dolegowska, B.; Kawa, M. Effects of sterilization methods on different 3D printable materials for templates of physician-modified aortic stent grafts used in vascular surgery-A preliminary study. Int. J. Mol. Sci. 2022, 23, 3539. [Google Scholar] [CrossRef]
- Huang, J.; Li, G.; Wang, W.; Wu, K.; Le, T. 3D printing guiding stent graft fenestration: A novel technique for fenestration in endovascular aneurysm repair. Vascular 2017, 25, 442–446. [Google Scholar] [CrossRef]
- Tam, M.D.; Laycock, S.D.; Brown, J.R.; Jakeways, M. 3D printing of an aortic aneurysm to facilitate decision making and device selection for endovascular aneurysm repair in complex neck anatomy. J. Endovasc. Ther. 2013, 20, 863–867. [Google Scholar] [CrossRef]
- Bortman, J.; Mahmood, F.; Schermerhorn, M.; Lo, R.; Swerdlow, N.; Mahmood, F.; Matyal, R. Use of 3-dimensional printing to create patient-specific abdominal aortic aneurysm models for preoperative planning. J. Cardiothorac. Vasc. Anesth. 2019, 33, 1442–1446. [Google Scholar] [CrossRef]
- Wu, C.; Squelch, A.; Sun, Z. Investigation of three-dimensional printing materials for printing aorta model replicating type B aortic dissection. Curr. Med. Imaging 2021, 17, 843–849. [Google Scholar] [CrossRef]
- Traynor, G.; Shearn, A.I.U.; Milano, E.G.; Ordonez, M.V.; Nieves, M.; Forte, V.; Caputo, M.; Schievano, S.; Mustard, H.; Wray, J.; et al. The use of 3D-printed models in patient communication: A scoping review. J. 3D Print. Med. 2022, 6, 13–23. [Google Scholar] [CrossRef]
- Biglino, G.; Koniordou, D.; Gasparini, M.; Capelli, C.; Leaver, L.K.; Khambadkone, S.; Schievano, S.; Taylor, A.M.; Wray, J. Piloting the use of patient-specific cardiac models as a novel tool to facilitate communication during clinical consultations. Pediatr. Cardiol. 2017, 38, 813–818. [Google Scholar] [CrossRef]
- Biglino, G.; Capelli, C.; Wray, J.; Schievano, S.; Leaver, L.K.; Khambadkone, S.; Giardini, A.; Derrick, G.; Jones, A.; Taylor, A.M. 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: Feasibility and acceptability. BMJ. Open 2015, 5, e007165. [Google Scholar] [CrossRef]
- Biglino, G.; Moharem-Elgamal, S.; Lee, M.; Tulloh, R.; Caputo, M. The perception of a three-dimensional-printed heart model from the perspective of different stakeholders: A complex case of truncus arteriosus. Front. Pediatr. 2017, 5, 209. [Google Scholar] [CrossRef]
- Biglino, G.; Capelli, C.; Leaver, L.K.; Schievano, S.; Taylor, A.M.; Wray, J. Involving patient, family and medical staff in the evaluation of 3D printing models of congenital heart disease. Common. Med. 2015, 12, 157–169. [Google Scholar] [CrossRef]
- Lau, I.W.W.; Liu, D.; Xu, L.; Fan, Z.; Sun, Z. Clinical value of patient-specific three-dimensional printing of congenital heart disease: Quantitative and qualitative assessments. PLoS ONE 2018, 13, e0194333. [Google Scholar] [CrossRef]
- Illmann, C.F.; Hosking, M.; Harris, K.C. Utility and access to 3-dimensional printing in the context of congenital heart disease: An International physician survey study. CJC. Open 2020, 2, 207–213. [Google Scholar] [CrossRef]
- Sun, Z. Cardiac CT imaging in coronary artery disease: Current status and future directions. Quant. Imaging Med. Surg. 2012, 2, 98–105. [Google Scholar]
- Rubin, G.D.; Leipsic, J.; Schoepf, J.U.; Fleischmann, D.; Napel, S. CT angiography after 20 years: A transformation in cardiovascular disease characterization continues to advance. Radiology 2014, 271, 633–652. [Google Scholar] [CrossRef]
- Sun, Z.; Al Moudi, M.; Cao, Y. CT angiography in the diagnosis of cardiovascular disease: A transformation in cardiovascular CT practice. Quant. Imaging Med. Surg. 2014, 4, 376–396. [Google Scholar]
- Abdullah, K.A.; McEntee, M.F.; Reed, W.; Kench, P.L. Development of an organ-specific insert phantom generated using a 3D printer for investigations of cardiac computed tomographic protocols. J. Med. Radiat. Sci. 2018, 65, 175–183. [Google Scholar] [CrossRef]
- Morup, S.D.; Stowe, J.; Precht, H.; Gervig, M.H.; Foley, S. Design of a 3D printed coronary artery model for CT optimization. Radiography 2022, 28, 426–432. [Google Scholar] [CrossRef] [PubMed]
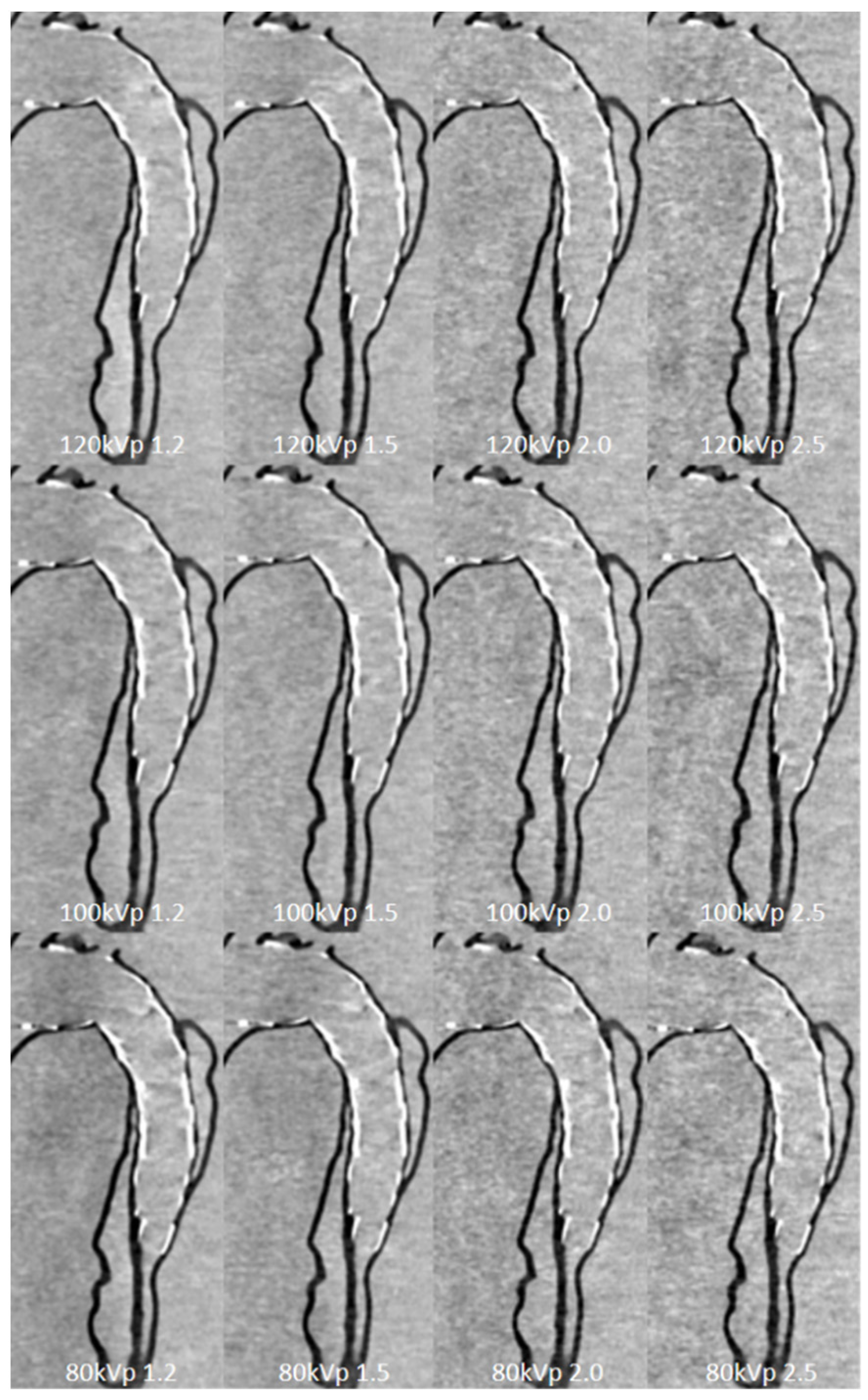
- Sun, Z.; Ng, C.K.C.; Wong, Y.H.; Yeong, C.H. 3D-printed coronary plaques to simulate high calcification in the coronary arteries for investigation of blooming artifacts. Biomolecules 2021, 11, 1307. [Google Scholar] [CrossRef]
- Sun, Z.; Ng, C.K.; Squelch, A. Synchrotron radiation computed tomography assessment of calcified plaques and coronary stenosis with different slice thicknesses and beam energies on 3D printed coronary models. Quant. Imaging Med. Surg. 2019, 9, 6–22. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z. 3D printed coronary models offer new opportunities for developing optimal coronary CT angiography protocols in imaging coronary stents. Quant. Imaging Med. Surg. 2019, 9, 1350–1355. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Jansen, S. Personalized 3D printed coronary models in coronary stenting. Quant. Imaging Med. Surg. 2019, 9, 1356–1367. [Google Scholar] [CrossRef] [PubMed]
- Sommer, K.N.; Lyer, V.; Kumamaru, K.K.; Rava, R.A.; Ionita, C.N. Method to simulate distal flow resistance in coronary arteries in 3D printed patient specific coronary models. 3D Print. Med. 2020, 6, 19. [Google Scholar] [CrossRef]
- Wu, C.; Squelch, A.; Sun, Z. Assessment of optimization of computed tomography angiography protocols for follow-up type B aortic dissection patients by using a 3D-printed model. J. 3D. Print. Med. 2022, 6, 117–127. [Google Scholar] [CrossRef]
- Aldosari, S.; Jansen, S.; Sun, Z. Optimization of computed tomography pulmonary angiography protocols using 3D printed model with simulation of pulmonary embolism. Quant. Imaging Med. Surg. 2019, 9, 53–62. [Google Scholar] [CrossRef]
- Aldosari, S.; Jansen, S.; Sun, Z. Patient-specific 3D printed pulmonary artery model with simulation of peripheral pulmonary embolism for developing optimal computed tomography pulmonary angiography protocols. Quant. Imaging Med. Surg. 2019, 9, 75–85. [Google Scholar] [CrossRef]
- Lin, A.; Kolossvary, M.; Motwani, M.; Isgum, I.; Maurovich-Horvat, P.; Sloka, P.; Dey, D. Artificial intelligence in cardiovascular CT: Current status and future implications. J. Cardiovasc. Comput. Tomogr. 2021, 15, 462–469. [Google Scholar] [CrossRef]
- Barragan-Montero, A.; Javaid, U.; Valdes, G.; Nguyen, D.; Desbordes, P.; Macq, B.; Willems, S.; Vandewinckele, L.; Holmstrom, M.; Lofman, F.; et al. Artificial intelligence and machine learning for medical imaging: A technology review. Phys. Med. 2021, 83, 242–256. [Google Scholar] [CrossRef] [PubMed]
- Van de Oever, L.B.; Vonder, M.; van Assen, M.; van Ooijen, P.M.A.; de Bock, G.H.; Xie, X.Q.; Vliegenthart, R. Application of artificial intelligence in cardiac CT: From basics to clinical practice. Eur. J. Radiol. 2020, 128, 108969. [Google Scholar] [CrossRef]
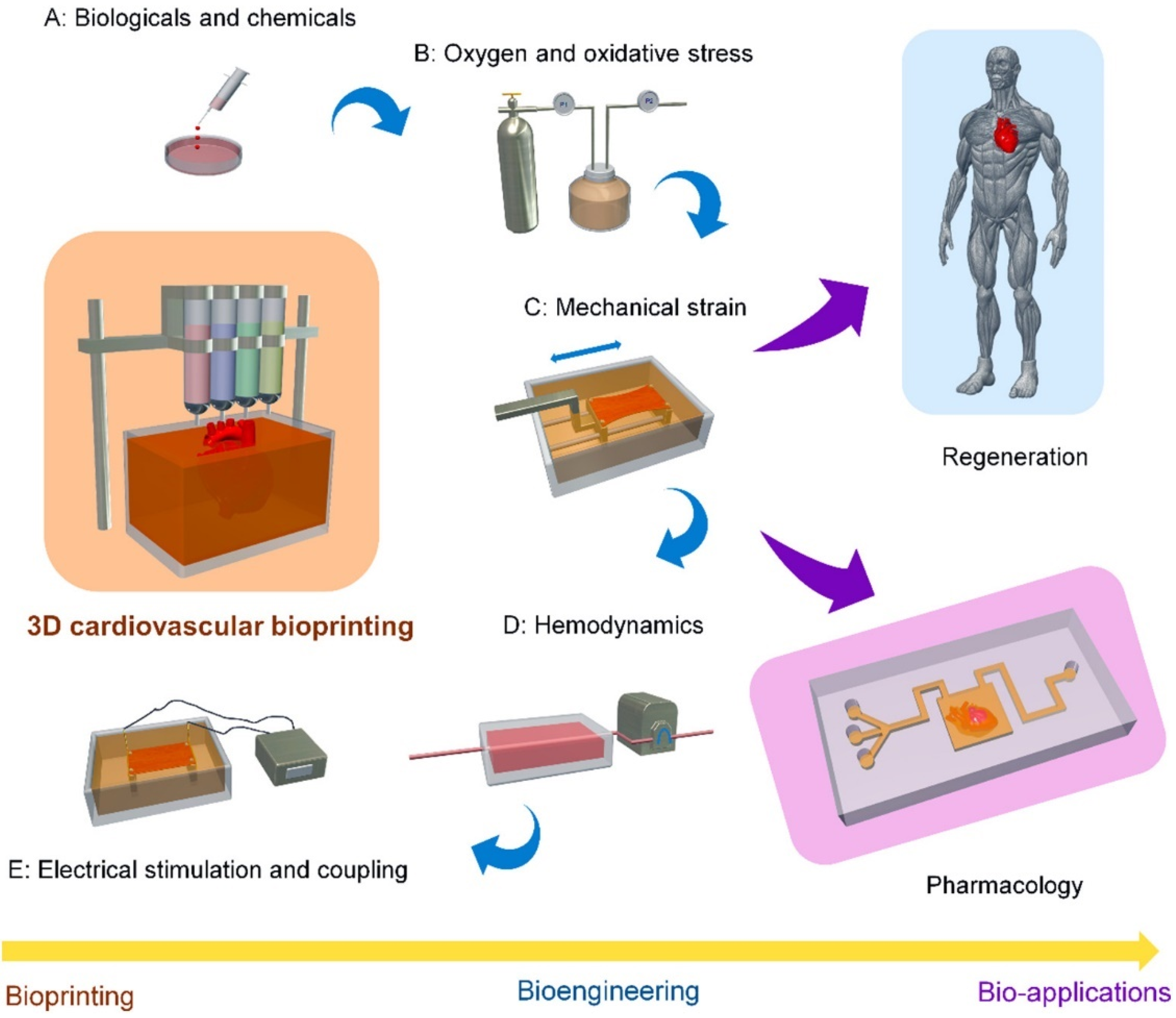
- Cui, H.; Miao, S.; Esworthy, T.; Zhou, X.; Lee, S.J.; Liu, C.; Yu, Z.; Fisher, J.P.; Mohiuddin, M.; Zhang, L.G. 3D bioprinting for cardiovascular regeneration and pharmacology. Adv. Drug. Deliv. Rev. 2018, 132, 252–269. [Google Scholar] [CrossRef] [PubMed]
- Alonzo, M.; Anilkumar, S.; Roman, B.; Tasnim, N.; Joddar, B. 3D bioprinting of cardiac tissue and cardiac stem cell therapy. Transl. Res. 2019, 211, 64–83. [Google Scholar] [CrossRef]
- Zhang, J.; Wehrle, E.; Rubert, M.; Muller, R. 3D bioprinting of human tissues: Biofabrication, bioinks and bioreactors. Int. J. Mol. Sci. 2021, 22, 3971. [Google Scholar] [CrossRef]
- Wang, Z.; Lee, S.J.; Cheng, H.J.; Yoo, J.J.; Atala, A. 3D bioprinted functional and contractile cardiac tissue constructs. Acta. Biomater. 2018, 70, 48–56. [Google Scholar] [CrossRef]
- Xia, Z.; Jin, S.; Ye, K. Tissue and organ 3D bioprinting. SLAS. Technol. 2018, 23, 301–314. [Google Scholar] [CrossRef]
- Kato, B.; Wisser, G.; Agrawal, D.K.; Wood, T.; Thankam, F.G. 3D bioprinting of cardiac tissue: Current challenges and perspectives. J. Mater. Sci. Mater. Med. 2021, 32, 54. [Google Scholar] [CrossRef]
- Chessa, M.; Van De Bruaene, A.; Farooqi, K.; Valverde, I.; Jung, C.; Votta, E.; Sturla, F.; Paul Diller, G.; Brida, M.; Sun, Z.; et al. Three-dimensional printing, holograms, computational modelling, and artificial intelligence for adult congenital heart disease care: An exciting future. Eur. Heart J. 2022, 43, 2672–2684. [Google Scholar]
| Author | Study Design | Sample Size and Participants | Original Data Source | Application in CVD | Image Processing Software | 3D Printer/ Printing Parameters | 3D Printing Material | Key Findings | |
|---|---|---|---|---|---|---|---|---|---|
| Garas et al. [26] | Cross-sectional study | Twenty-three students from first-year health science courses (n = 11) and third-year human biology preclinical courses (n = 12). All participants were exposed to plastinated, 3D-printed models and cadaverous specimens. | MRI and CT | 3D printed models of heart, shoulder and thigh | NR | NR | Resin | 3D printed models have the potential to assist students in anatomy learning when compared to traditional teaching methods: 3D printed models were scored to be easiest to identify anatomical features than others (p<0.001). 3D printed models received the highest percentage of the preferred method of learning anatomy compared to cadavers and plastinated models (45% vs. 36% and 18%, p < 0.001). | |
| Lau & Sun [27] | Cohort study | Fifty-three second-year (n = 48) and third-year (n = 5) medical students, with 28 in the 3D printing group and 25 in the control group. The control group received an education workshop, digital 3D models and 2D images, while the 3D printing group received all the above plus 3D printed models. | CT | Four types of CHD: ASD, VSD, ToF and DORV | Mimics Innovation Suite 22.0 (Materialise, Leuven, Belgium) | Formlabs (Somerville, MA, USA) & Fabbxible Technology (Pulau Pinang, Malaysia). A 1 mm-thick shell was added to the digital model. | Flexible V4 Resin & TPU80A | 3D printed models do not significantly improve both immediate knowledge acquisition and knowledge retention among the medical students, although 3D printed model group had slightly higher scores than the control group (7.79 ± 2.63 vs. 7.04 ± 2.64). 3D printed models were ranked to increase their knowledge in CHD, but no significant difference compared to 2D/3D views (p > 0.05). | |
| Karsenty et al. [28] | Randomized controlled trial | Three hundred forty-seven fifth-year medical students. Students were randomized into printing groups or control groups. All students received the same 20 min lecture with projected digital 2D images. The 3D printing groups also received 3D printed models during the lecture. | CT | CHD includes ASD, VSD, CoA and ToF | Mimics and 3-Matic (Materialise, Leuven, Belgium). The mean time from segmentation to printing: ASD and CoA: 15 min VSD: 30 min ToF: 60 min | Stream 20 pro printer (Volumic, France) | Biodegradable polylactic acid (PLA) filament | Objective knowledge improvement after the lecture was higher in the 3D printing group compared to the control group (16.3 ± 2.6 vs. 14.8 ± 2.8 out of 20, p < 0.0001). Similar results were observed for each CHD for post-lecture scores (p = 0.0001 ASD group; p = 0.002 VSD group; p = 0.0005 CoA group; p = 0.003 ToF group). Students’ opinion of their understanding of CHDs was higher in the 3D printing group compared to the control group (respectively 4.2 ± 0.5 vs. 3.8 ± 0.4 out of 5, p < 0.0001). | |
| Lim et al. [29] | A double-blinded randomized controlled trial | Fifty-two first-year medical students were randomly assigned to three groups who underwent self-directed learning sessions using either cadaveric materials (n = 18), 3D prints (n = 17), or a combination of cadaveric materials/3D prints (combined materials) (n = 18). | CT |
3D prints of heart and great vessels: 2 × 3D printed prosected heart with great vessels 2 × 3D printed heart without great vessels 3 × 3D printed coronary artery models | NR | NR | NR | 3D printed models did not disadvantage students relative to cadaveric materials. Post-test scores were significantly higher for the 3D printing group compared to the cadaveric materials or combined materials groups (mean score of 60.83 vs. 44.81 and 44.62, p = 0.010). A significant improvement in test scores was detected for the 3D printing group (+18.4%, p = 0.003) but not for the other two groups (+8.06%, p = 0.083, +7.45%, p = 0.080). | |
| Smerling et al. [30] | Cross-sectional study | Forty-five medical students were rotated through four different teaching stations: Station 1: embryology video Station 2: 2D diagrams Station 3: Pathology specimens Station 4: 3D printed models. | CT | 3D printed cardiac models were created for the following lesions: pulmonic stenosis (PS), ASD, ToF, d-TGA, CoA and HLHS | Mimics (Materialise, Leuven, Belgium), Meshlab | Uprint SE printer (Stratasys, Eden Prairie, MN, USA) | NR | The use of 3D printed models significantly improved students’ knowledge for every pathology (mean improvement ± SD): PS (0.3 ± 0.6, 3.52, p < 0.001), ASD (0.6 ± 0.5, 7.69, p < 0.001), TOF (0.8 ± 0.5, 10.08, p < 0.001), d-TGA (0.9 ± 0.7, 8.70, p < 0.001), CoA (0.8 ± 0.6, 8.93, p < 0.001), HLHS (1.1 ± 0.7, 11.05, p < 0.001). Students “strongly agreed” the 3D printed models made them more confident in explaining congenital cardiac anatomy to others (4.23 ± 0.69), and they strongly recommended the use of 3D models for future educational sessions (mean = 4.40 ±0.69). | |
| Su et al. [31] | Randomized controlled trial | Sixty-three medical students were randomly allocated to two groups (32 students in the experimental and 31 in the control group). Each group attended a teaching seminar on VSD, with the experimental group receiving 3D printing as an additional component | CT | 3D printed models of 3 subtypes of VSD (perimembranous, subarterial and muscular). | NR | SL600 3D printer (ZRapid Tech, Wujiang, China) | Plastic material | The test results were statistically significantly higher in the experimental group (p = 0.02–0.03). The inter-group differences in both questionnaire and test results were significantly higher in structural conceptualization (p = 0.03) but not in knowledge acquisition (p = 0.06–0.09). Open-ended responses in the questionnaire showed the advantages of using 3D models over traditional teaching methods. | |
| Lau et al. [32] | Cross-sectional study | Twenty-nine participants: cardiac radiologist (1), interventional radiologist (1), general radiologists (3), radiology registrars (4), sonographers (3), radiographers (16) and student radiographer (1). | CT | Four 3D printed CHD models: ASD, VSD, ToF and DORV. All participants attended 15-min demonstration session of 3D printed models and VR. | Mimics 22.0 (Materialise, Leuven, Belgium) | NR. A 1 mm-thick shell was added to the digital model. | Thermoplastic polyurethane (TPU) and flexible resin. | No significant difference was found between 3D printed models ad VR in medical education and preoperative planning of CHD (p > 0.05). Further, subgroup analysis between doctors and non-doctors did not reach a significant difference in these two areas regarding the value of these two technologies (p > 0.05). | |
| Jones & Seckeler [33] | Randomized controlled trial | Thirty-six pediatric and combined pediatric and emergency medicine residents were randomized into interventional (n = 17) and control groups (n = 19). Each group received the 20-min lecture on vascular rings and slings, while the intervention group received 3D printed models. | CT & MRI | 3D printed models of pediatric aortic arch anomalies (vascular rings and pulmonary artery slings) | Philips IntelliSpace Portal (Philips Healthcare, Best, The Netherlands) Autodesk MeshMixer (Auto- desk, Inc., San Rafael, CA, USA) | Dremel 3D Idea Buidler (Dremel, Mount Prospect, IL, USA). | Polylactic acid (PLA). | 3D printed models significantly increased the interventional group’s objective tests assessing anatomy of rings and slings (p = 0.001), diagnosis of rings and slings (p< 0.001) and treatment of rings and slings (p< 0.001). While the total improvement from pre- to post-test scores did not reach statistical significance, the intervention group received the highest average score increase than the control group after the lecture (2.6 vs. 1.8, p = 0.084). | |
| Krishnasamy et al. [34] | Cross-sectional study | Thirty doctors, including four cardiothoracic surgeons, 12 cardiologists, five radiologists and nine surgical registrars. All participants were exposed to 3D printed models and asked to complete a questionnaire. | CT | 3D printed models of the normal heart | BioModroid | ZCorp Z450 and Stratasys multi-material Connex500 | Rubber (cardiac chambers), Tango Plus- synthetic rubber-like material (cardiac muscle), plastic (outer structures). | 93% rated the model accuracy as good and above; 64% of the clinicians evaluated this model as an excellent teaching tool for anatomy class. As a visual aid for surgery and planning of treatment, 90% and 74% scored the model to be above average, respectively; 70% of the clinicians scored the model as above average for training purposes. Overall, this 3D printed heart model was rated as excellent (33%), good (50%), and average (17%). | |
| Loke et al. [20] | Randomized controlled trial | Thirty-five pediatric residents with similar previous clinical exposure to Tetralogy of Fallot (ToF). Participants were randomized into control (2D drawings of ToF, n = 17) and interventional (3D printed models, n = 18) | CT, MRI and 3D echocardiography | 3D printed models of a normal infant heart, an adult ToF (repaired) and an infant ToF (unrepaired). | Mimics (Materialize, Leuven, Belgium) | NR | NR | 3D printed models gave higher composite learner satisfaction scores (p = 0.03). The 3D printed model group also had higher self-efficacy aggregate scores, but the difference was not statistically significant (p = 0.39). No significant difference in pre- and post-test scores was found in knowledge acquisition between 2D images and 3D printed models (p > 0.05). | |
| Valverde et al. [35] | Non-randomized cross-over study | One hundred and twenty-seven participants (consultants in pediatric cardiology, fellows in pediatric cardiology, and medical students) were randomly distributed into four groups (Groups 1–4) and shown as specific crisscross heart cases (Cases 1–4). Conventional imaging teaching and 3D printed models were presented to each group. | Echocardiography and CMR | Crisscross heart is one of the most complex and extremely rare forms of congenital heart disease. All 3D printed models were based on the four patient-specific CMR datasets. Average printing time: 9.0 ± 1.6 h Average cost of 3D printed model: USD$98 ± 7.5 | ITK-SNAP software, version 3.8.0 (University of Pennsylvania, Philadelphia, PA, USA) | 3D printer BQ Witbox 1 (Mundo Reader S.L., Madrid, Spain). Models were printed with a 0.2 mm layer height supporting line distance of 5 mm and an overhang angle of 60°. | Filaflex 82A, a flexible polyurethane filament | 3D printed models significantly improved crisscross heart anatomy (p < 0.001). The increase in the questionnaire marks was statistically significant across all academic groups (p < 0.05). Ninety-four percent (120) and 95.2% (121) of the participants agreed or strongly agreed, respectively, that 3D models helped them to better understand the medical images of cardiac anatomy. The average score of overall satisfaction for 3D printing was 9.1 out of 10, with students providing the highest scores than clinical fellows (9.7 vs. 8.6). | |
| White et al. [36] | Randomized controlled trial | Sixty pediatric and emergency medicine residents participated in 2 studies based on pathology (VSD and ToF). Twenty-six were in a VSD study (12 in the control group and 14 in the intervention group). Thirty-four were in the ToF study, 17 each in control and interventional groups. Each group received a 20-min lecture on VSD, with the interventional group receiving 3D printed models. | NR | Four cases, including VSD and ToF | Philips IntelliSpace Portal (Philips Healthcare, Best, The Netherlands) | Dremel 3D Idea Builder (Dremel, Mount Prospect, IL, USA) | Polylactic acid (PLA) | There does not seem to be an added benefit for understanding VSDs (the control group scored higher than the intervention group [p = 0.012), but there is for ToF (the interventional group scored higher than the control group, p = 0.037). This is likely due to the increased complexity of the lesion and difficulty visualizing spatial relationships in CHD with multiple components. | |
| Tan et al. [37] | Randomized controlled trial | One hundred and thirty-two nursing students in congenital heart surgery were randomly divided into the 3D printing group (n = 66) or traditional group (n = −66). Both groups were exposed to the same teaching environment with 3D printed model incorporated into the 3D printing group. | One hundred and thirty-two nursing students in congenital heart surgery were randomly divided into the 3D printing group (n = 66) or traditional group (n = −66). Both groups were exposed to the same teaching environment with 3D printed model incorporated into the 3D printing group. | NR | 3D printed model of a patient-specific case of ASD | NR | NR | NR | In the classroom assessment of theoretical knowledge, the 3D printing group scored significantly higher than the traditional group, with corresponding sores being 7.08 ± 1.66 and 6.56 ± 1.17, respectively (p = 0.02). The 3D printing group scored significantly higher than the traditional group in the self-evaluation of comprehensive ability and teaching satisfaction score (p < 0.05). Similarly, the 3D printing group scored significantly higher than the traditional group in the critical thinking ability assessment (p < 0.05). |
| Biglino et al. [38] | Cross-sectional study | One hundred nurses (65 pediatric cardiac nurses and 35 adult cardiac nurses) attended a training course about CHD. | NR | Nine models were created, including: a healthy heart, repaired transposition of the great vessels, ToF, pulmonary atresia with an intact ventricular septum and palliated hypoplastic left heart syndrome. | NR | NR | NR | The majority of the nurses indicated that 3D printed models helped them to understand cardiac anatomy (86%), spatial orientation (70%) and anatomical complexity after treatment (66%). The 3D printed models were rated as useful by the cardiac nurses, with an average score of 5.1 out of 7. | |
| Liang et al. [39] | Cross-sectional study | Eight CHD cases were 3D printed with clinical values assessed by two groups: one group including 40 experts (20 cardiac surgeons and 20 sonographers); another group consisting of 40 3rd year postgraduate students. | CT | Diagnostic value of 3D printed CHD models, which were printed with blood pool and myocardium models. Eight types of CHD were classified as simple (PDA, CoA and VSD) and complex (ccTGA, DORV, WA, CAF and ToF). | Mimics (Materialize, Leuven, Belgium) | SLA (Shaanxi Hengtong Intelligent Machine Co., Ltd., Xi’an, China). Time and cost for 3D printing and post-processing: 5.88 h and $41 for blood pool models, and 6.25 hr and $42 for myocardial models. | Rigid white resin | 3D printing improved the diagnostic rate in both the expert and student groups, with the average value being 95.9% and 91.6% after using 3D printed models vs. 88.75% and 60% before using 3D printed models (p = 0.000–0.001). 3D printed models were found to be more important in diagnosing complex CHD than simple CHD, and the demand was stronger in students than from experts. Myocardial models were found to be more advantageous in DORV and VSD by demonstrating the location and structure of the lesions, while blood pool models were more effective in assessing other CHD diseases. |
| Observation Indices | 3D Printing Group n = 64 | Traditional Group n = 66 | T Value | p Value |
|---|---|---|---|---|
| Total score | (299.98 ± 1.20) | (282.61 ± 0.67) | 12.586 | <0.01 |
| Truth-seeking | (42.00 ± 0.58) | (40.67 ± 0.29) | 2.046 | 0.02 |
| Open-mindedness | (43.73 ± 0.52) | (40.83 ± 0.26) | 4.913 | <0.01 |
| Analytical ability | (42.59 ± 0.42) | (39.95 ± 0.23) | 5.449 | <0.01 |
| Systemic ability | (44.56 ± 0.27) | (40.30 ± 0.23) | 11.926 | <0.01 |
| Confidence in thinking | (44.38 ± 0.24) | (41.16 ± 0.28) | 8.878 | <0.01 |
| Curiosity | (42.21 ± 0.36) | (40.73 ± 0.42) | 2.690 | <0.01 |
| Cognitive maturity | (40.52 ± 0.45) | (38.97 ± 0.35) | 2.716 | <0.01 |
| Author | Study Design | Sample Size and Participants | Original Data Source | Application in CVD | Image Processing Software | 3D Printer/ Printing Parameters | 3D Printing Material | Key Findings |
|---|---|---|---|---|---|---|---|---|
| Valverde et al. [47] | Prospective multi-center study | Forty patients with complex CHD. Patients took part in the surgical planning meetings alongside surgeons, cardiologists and radiologists. | CT and MRI | 3D printed models of complex CHD: DORV: 19 and other types of CHD: 21 | ITK snap software & Meshmixer version 11.0.544 | BQ Witbox, Spain. A 0.8 mm outer shell was added outside of the blood pool interface. | Fused deposition modeling with the use of polyurethane filament | The surgical planning of 21 cases (52% of total cases, confidence interval 38.5–70.7%) was not influenced by 3D printed models, and the surgical decision remained based on the patient’s imaging. The surgical decision in the other 19 cases was changed by 3D printed models (47.5% of total cases, confidence interval of 29.6–61.5%). A 53.6% change in the surgical plan after using 3D printed models. |
| Chen et al. [48] | Cross-sectional study | Five patients with pulmonary atresia (PA) with VSD or major aortopulmonary collateral arteries (MAPCA) had a 3D model of their heart printed prior to the unifocalization procedure. | Echocardiography and CT | Five patients with PA/VSD/MAPCA were subjected to 3D printing of the heart before the single-stage unifocalization procedure. The 3D models were also visualized in the operating room using VR glasses. | 3Matic (Materialise, Leuven, Belgium) & ITKsnap 3X. Microsoft HoloLens for mixed reality | NR | NR | The 3D models aided surgeons in visualizing spatial relationships between the major vessels and the precise location of each MAPCA up to a few mm in accuracy. This was beneficial to the surgical strategy and pre-operative planning as surgeons had a better comprehension of the procedure prior to the surgery. VR simulation enabled surgeons to have a comprehensive understanding of both spatial anatomy and surgical procedure. |
| Gomez-Ciriza et al. [22] | Cross-sectional study with seven years of experience | One hundred thirty-eight heart models were generated. In addition, 13 cardiac surgeons and 30 pediatric cardiologists were introduced to 3D-printed models of congenital heart diseases. | CT and MRI | Patients with CHD were recruited from several hospitals. One hundred and thirty-eight low-cost 3D printed models, with 83 used for surgical planning, 48 for interventional planning and 7 for the interventional simulator | ITK-SNAP and Cura. Average time for printing and cleaning: 13.5 h Average cost of each model: EUR85.7 | BQ Witbox Fused Deposition Modeling 3D printer. Z-axis resolution: 0.02 mm. Heart models were printed with 0.15 mm Z resolution. | Filaflex | With the use of 3D printed models, the surgical planning was modified in 47.5% of the patients compared to the original surgical plan, which used only clinical information and medical imaging. 3D printed models were scored useful for communicating with parents and patients. Further, they were allowed to plan specific interventions and develop new strategies for treating CHD. |
| Guo et al. [49] | Cross-sectional study | Seven HOCM patients who received surgical management had 3D models of their hearts printed. | CT | Surgical management of hypertrophic obstructive cardiomyopathy (HOCM) | Mimics 19.0 (Materialise, Leuven, Belgium) | Objet350 Connex3 (Stratasys Ltd., Eden Prairie, MN, USA) | VeroMagenata Veroclear VeroCyan Tango material | The pre- and postoperative echocardiographic evaluation revealed that left ventricular outflow tract (LVOT) obstruction was adequately relieved (82.71 ± 31.63 to 14.91 ± 6.89 mmHg, p < 0.001) and septal thickness was reduced from 21.57 ± 4.65 to 17.42 ± 5.88 mm (p < 0.001). Patients were highly satisfied with the use of 3D printed models in explaining the disease. |
| Kiraly et al. [24] | A cross-sectional study amongst the multidisciplinary and intraoperative team | Fifteen patients with complex congenital cardiac conditions for cardiac surgery. | CT | 3D prototypes of the heart-great vessels for 15 case scenarios undergoing surgical management. | Mimics (Materialise, Leuven Belgium) and 3D Slicer | Stratasys J750 resin-based 3D printer (Stratasys, Eden Prairie, MN, USA). Hollow models with 2–3 mm wall thickness. | VeroMagenta, TangoPlus and HeartPrint Flex | 3D printed models refined diagnosis in 9 out of 15 cases, while in 13 cases (86.66%), redo-operations were planned after reviewing 3D printed models. 3D printed models revealed new anatomic findings in 60% of cases, of which 3D printed models offered an alternative surgical plan in 3 cases. 3D printed models enabled surgical simulation and pre-procedural planning for the shape and size patches. |
| Ryan et al. [50] | Cross-sectional study with a single center of 3 years of experience | One hundred sixty-four models were printed for various purposes with operating room length and mortality/morbidity compared between the standard of care (SoC) and the use of 3D printed models. | CT & MRI | 79 3D printed models of CHD (different types) were used for surgical planning and comparison between the methods. | Mimics (Materialise, Leuven, Belgium) | zPrinter 650 (3D Systems, Rock Hill, SC, USA). | Gypsum-based resin | 3D printed models reduced operating length of time (mean 202.7 vs. 229.3 min, p = 0.674), reduced 30-day mortality, and readmission rate for patients (60% vs. 71.6%) when compared to SoC, although these comparisons did not reach statistical significance. |
| Zhao et al. [51] | Cross-sectional study | Twenty-five patients with complex DORV were divided into two groups: the control group (17) and the 3D printing group (8). | CT | Clinical value of 3D printed models in planning preoperative strategies for surgical repair of patients with complex DORV. | Mimics (Materialise, Leuven, Belgium) | ZPrinter 650 | Polylactic acid | The 3D printing group had significantly reduced the mechanical ventilation time (56.43 vs. 96.76 h, p = 0.040) and intensive care unit time (99.04 vs. 166.94 h, p = 0.008) than the control group. The operative, cardiopulmonary bypass and aortic-clamping times were shorter in the 3D printing group than in the control group, with no significant difference (p > 0.05 for all). |
| Ghosh et al. [52] | Retrospective study over a period of 3 years | One hundred and twelve patient-specific 3D printed models of CHD, with 16 used for teaching purposes and 96 for pre-operative planning. | MRI and CT | How 3D printing service is incorporated into routine pre-procedural care of pediatric patients with acquired or congenital CHD. | Mimics 20.0 (Materialise, Leuven, Belgium) | Objet500 Connex 3 & J750, Stratasys(Eden Prairie, MN, USA) | Rigid photopolymers with a minimum thickness of 1.0 mm and flexible rubber photopolymers with a minimum thickness of 0.75 mm. | The most common applications of 3D printed models were to evaluate intracardiac anatomy for complex biventricular repair (31%) and preoperative evaluation of extracardiac pathology (20%), followed by repair of multiple ventricular septal defects (12%). In about one-third (34%) of cases, 3D printed models were requested prior to patients undergoing CT or MRI imaging. 3D printed models can be incorporated into the pre-procedural care of patients with CHD. |
| Russo et al. [53] | Cross-sectional multi-center study | Thirteen patients with aortic stenosis at a high risk of coronary artery obstruction (CAO). | CT | 3D printed models to simulate transcatheter aortic valve replacement (TAVR) procedures for improving CAO risk assessment and prediction of complications and procedural safety. | Mimics 20.0 (Materialise, Leuven, Belgium) | NR | Heart-Print Flex technology- a combination of flexible and rigid polymers. | TAVR was successfully stimulated in all 13 printed models with a high risk of CAO. The 3D model simulations correlated well with clinical outcomes by accurately replicating specific anatomy and procedural outcomes. 3D printed models serve as a useful simulation platform in high-risk TAVR patients to predict complications. |
| Author | Study Design | Sample Size and Participants | Original Data Source | Application in CVD | Image Processing Software | 3D Printer/ Printing Parameters | 3D Printing Material | Key Findings |
|---|---|---|---|---|---|---|---|---|
| Fan et al. [54] | A mix of retrospective and prospective study | Retrospective group of 72 patients with LAA occlusion guided by 3D TEE imaging. Prospective group of 32 patients with LAA occlusion guided by 3D printed models. | 3D transesophageal echocardiography (TEE) | 3D printed models in LAA device selection and assessment of procedural safety and efficacy. | Mimics 19.0 (Materialise, Leuven, Belgium) | Objet350 Connex 3 (Stratasys). Hollow wall thickness: 1 mm. Printing resolution: 32 μm. | Agilus A30 Clear (Stratasys) | The implantation success was 100% and 93.1% in retrospective and prospective groups. The prospective group with the use of 3D printed models achieved shorter procedural time, few devices used for the procedure (p < 0.05 for all) with no procedure complications. There were no major adverse cardiac events or mortality in the prospective group at a mean follow-up of 9.4 months, while there were three major adverse events and nine deaths in the retrospective group at a mean follow-up of 3 years. |
| Hell et al. [55] | Cross-sectional study | Twenty-two patients underwent LAA occlusion | TEE and CT | Prediction of device size and compression for LAA occlusion | 3D Slicer 5–6 h, 20 EUR | Ultimaker 2 (Ultimaker, B.V., Geldermalsen, The Netherlands) | Silicon rubber | There was 95% agreement between 3D printed model-based sizing and the finally implanted device sizes, while the agreement between CT- and TEE-based device sizes was only 77% and 45%, respectively. The 3D printed models correlated well with the prediction of device compression (p = 0.003). |
| Li et al. [56] | Randomized controlled trial | Twenty-one patients in the 3D printing group with 3D printed model guiding occlusion device selection. Twenty-one patients in the control group with an occlusion device selected by TEE, CT and angiography. | TEE and CT | LAA occlusion device selection. | Mimics 17.0 (Materialise, Leuven, Belgium) | NR | NR | The occlusion procedure was successful in both groups. The procedure time, contrast volume, and costs were 96.4 ± 12.5 vs. 101.2 ± 13.6 min, 22.6 ± 3.0 vs. 26.9 ± 6.2 mL, and 12,671.1 vs. 12,088.6 USD for 3D printing and control groups, respectively. The radiation dose was significantly lower in the 3D printing group than that in the control group (561.4 ± 25.3 vs. 651.6 ± 32.1 mGy, p < 0.05). |
| Conti et al. [57] | Case-control study | Twenty patients: 6 with LAA leak and 14 control patients without LAA leak. | CT | 3D printed models in LAA size to prevent LAA leak. | ITK-SNAP0 | Form 2 Desktop printer (Formlabs, Inc., Somerville, MA, USA) | NR | Compared to 3D printed models, the device sizes based on traditional imaging analysis were unestimated in 11 patients (55%), agreed with the implanted sizes in 7 (35%) and overestimated in 2 (10%) cases. Of 8 cases with an implant device of 22 mm, 75% of the 3D printed models matched the implanted size. |
| Goitein et al. [58] | Cross-sectional study | Twenty-nine patients underwent LAA occlusion. | TEE and CT | 3D printed models to size LAA occluder. Two types of occluder were used: AMPLATZER: n = 12 WATACHMAN: n = 17 | Comprehensive Cardiac Analysis (v 4.5, Philips Healthcare) | Objet (Rehovot, Israel) | TangioPlus FLX930 (Stratasys, Germany) | A high correlation was found between 3D printed models and the inserted device size for the AMPLATZER occluder (p = 0.001) but was a poor correlation between 3D printed models and the WATCHMAN device (p = 0.203). |
| Torres and Luccia [59] | Cross-sectional study (prospective controlled single-center trial) | Control group: 5 residents operated on 30 patients; Training group: 5 residents operated on 25 patients. | CT | Twenty-five aneurysms were 3D printed for training and simulation of EVAR procedure when compared to the traditional training approach. | TeraRecon iNtuition Unlimited (Aquarius v 4.3, TeraRecon, CA, USA) | Connex350 (Stratasys), Formlabs Form 1 and MakerFiveot | Five materials used for 3D printing: Rubber FLX930 Plastic RGD810 TangoPlus +Vero Clear Shore 60 Resin and PLA in silicone | Use of the3D models printed with flexible resin and silicone produced the best results. Patient-specific training based on 3D printed models reduced fluoroscopy time by 30% (33 vs. 48 min), total procedure time by 29% (207 vs. 292 min), the volume of the contrast medium by 25% (65 vs. 87 mL) and time for cannulation by 52% (3 vs. 6 min) when compared to the control group (p < 0.05 for all), respectively. |
| Karkkainen et al. [60] | Cross-section study (prospective pilot study) | 22 participants: 20 trainees: Group A: 13 experience in <20 EVAR Group B: 7 experience in >20 EVAR procedures. | CT | Use of a 3D printed AAA model in 20 trainees and two experienced operators to perform EVAR simulations | Mimics (Materialise, Leuven, Belgium | Objet500 Connex3 (Stratasys). Models were printed with three layers: 3 mm, 3 mm and 1 mm for rigid inner and flexible outer layers and luminal side, respectively. | VeroClear and Agilus | The mean procedure time was 37 ± 12 min for all 22 simulations. Experienced trainees completed the simulation procedures with significantly lower time and fluoroscopy time than inexperienced trainees (p < 0.05). |
| Kaufamann et al. [61] | Cross-sectional study | 27 interventional radiology (IR) procedures with 54 3D printed models. | CT | Fifty-four vascular models were printed with clear and transparent flexible resin for comparison of IR procedures. | Image J | Form 3 (Formlabs). Printing resolution: 0.1 mm. | Standard clear (transparent but rigid) and flexible resin (transparent and flexible). | Of the 216 measurements in the aorta and aortic branch diameters, there were no significant differences in all measurements between the original CT and clear and flexible resin models (p > 0.05). Printing accuracy was excellent for both materials (<0.5 mm). Printing success was 85.2% and 81.5% for standard clear and flexible resin, respectively. |
| Sheu et al. [62] | Randomized controlled trial | Forty-nine medical students were enrolled, with 26 assigned to 3D printed vascular model and 23 to the control group (commercial simulator). | CT | 3D printed model training medical students in performing femoral artery (FA) access. | TeraRecon Aquarium Intuition (TeraRecon Inc., Foster City, CA, USA) | Formlabs Form 2 SLA. The model was hollowed to 0.75 mm wall thickness. | Resin | Prior to simulation, 76.9% of trainees in 3D printing and 82.6% of trainees in the control group did not feel confident performing FA access. After the simulation, both groups agreed that the model increased their confidence in performing FA by 2 Likert points (p < 0.01). The confidence increase in the 3D printing group was non-inferior to that in the control group (p < 0.001). |
| Goodie et al. [63] | Cross-sectional study | Thirty medical students were invited to evaluate the efficacy of 3D printed vascular models. | CT and MRI | Five aorta and vascular models were created to simulate interventional radiology (IR) procedures. | Osirix Lite Library | Ultimaker 2 and Lulzbot Taz TM | PLA and NinjaTek Cheetah TM | 3D printed models served as a supplementary tool to traditional teaching for simulation and rehearsal of IR procedures. |
| Yoo et al. [64] | Cross-sectional study | Eighty-one surgeons or surgical trainees were presented with the 3D printed models and subsequently performed simulated surgical procedures under guided supervision. | CT and MRI | Hands-on surgical training using 3D printed models of CHD (DORV and HLHS) in simulation of congenital heart surgeries. | Mimics (Materialise, Leuven, Belgium) Average cost per model: $60 | Objet Connex 260 printer. A shell thickness of 1.2–1.8 mm was added to the outer surface of the segmented model. | TangoPlus FullCure resin and VeroWhite | Fifty attendees participated in the survey after training sessions. 3D printed models were considered as acceptable quality (88%) or manageable (12%) aid in surgical practice. Further improvements were suggested, including using material more akin to human cardiac valves. |
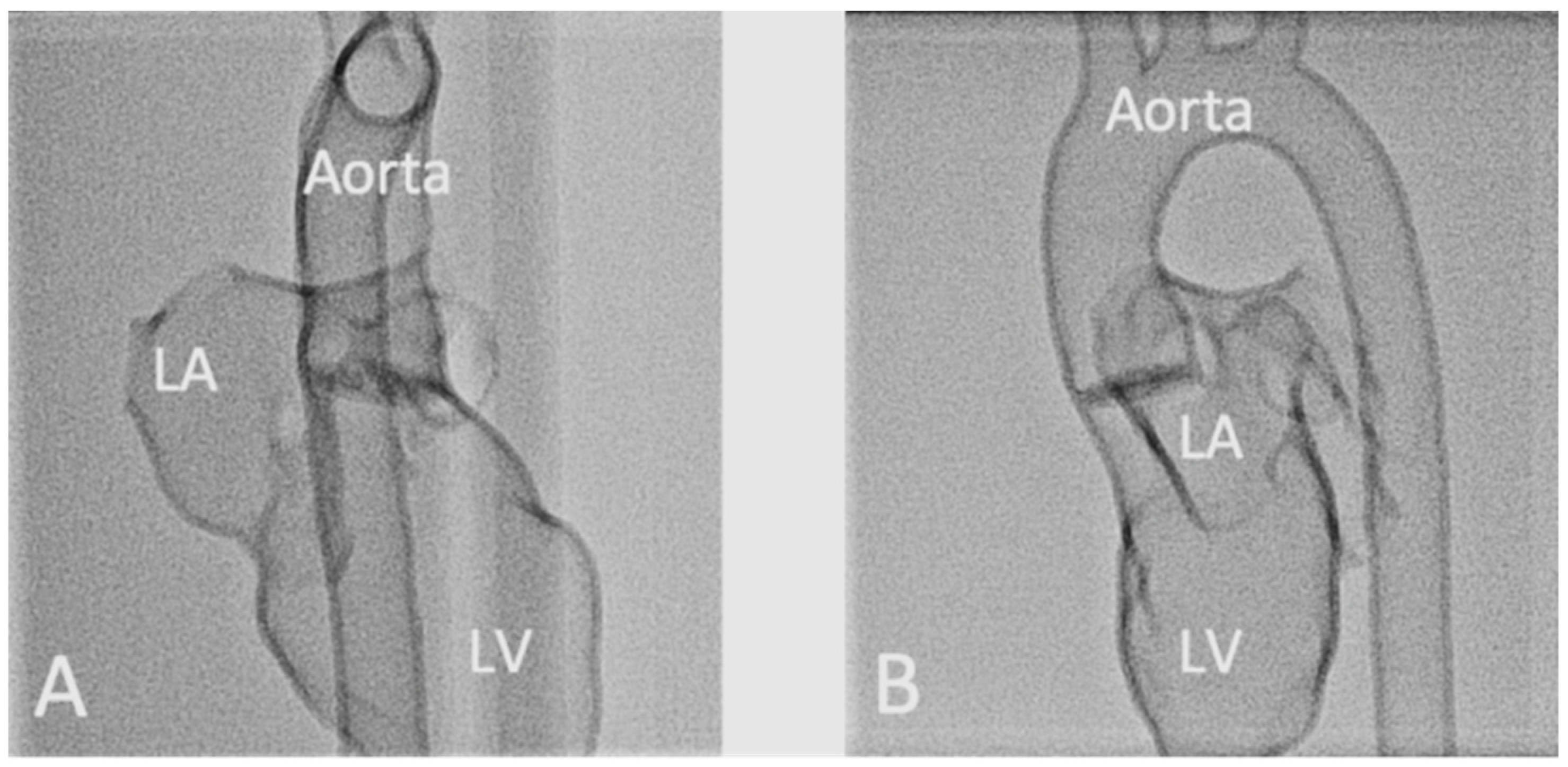
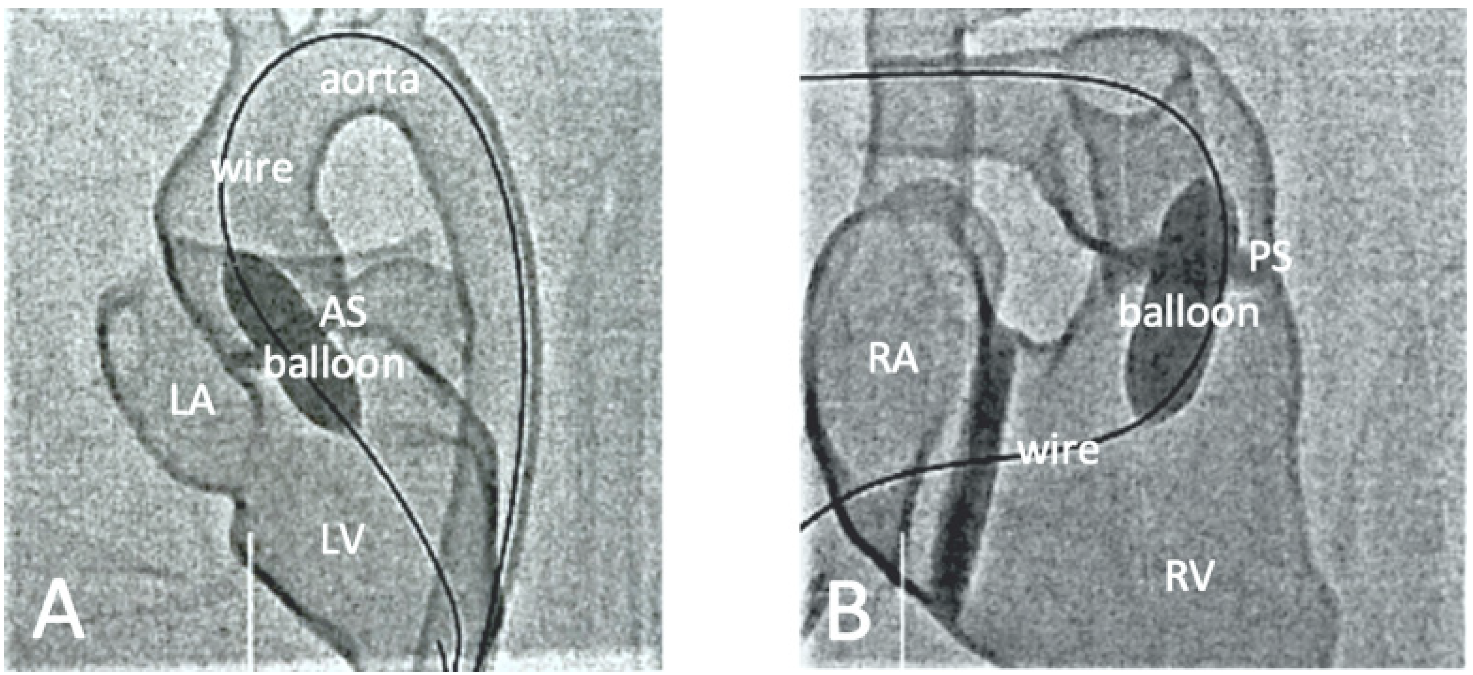
| Brunner et al. [65] | Cross-sectional study | Nineteen medical students and doctors participated in the hands-on training program. | CT | Hands-on training on simulation of interventional cardiology procedures on common CHD models. | Mimics (Materialise, Leuven, Belgium) | Agilista 3200W Polyjet 3D printer | Silicone rubber | Practicing on 3D printed models led to a significant reduction in the mean fluoroscopy time. All participants gave 3D printed models very positive ratings as a training tool for the simulation of interventional cardiac procedures. |
| Rynino et al. [66] | Cross-sectional study | Eleven models of aortic dissection cases were printed using different materials and distributed into four groups: autoclave 121 °C sterilization, plasma sterilization, gas sterilization, 105 °C autoclave sterilization. | CT | Effect of sterilization methods on the geometric changes of the 3D printed aortic template. | 3D Slicer | Raise3D Pro 2 printer (Raise3D, Irvine, CA, USA) & Form 2 (Formlabs, Somerville, MA, USA). 1.5 mm was added to the segmented aortic wall. | Polylactic acid (PLA), nylon, polypropylene (PP), polyethylene terephthalate glycol (PETG), and a rigid and flexible photopolymer resin. | 3D printed models made from PLA, PETG and PP were deformed during sterilization at high temperatures (autoclave 121 °C). However, 3D-printed models made with nylon or flexible and rigid resin did not undergo filament deformities during high-temperature sterilization. All mean geometry differences were less than 0.5 mm. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, Z.; Wee, C. 3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine. Micromachines 2022, 13, 1575. https://doi.org/10.3390/mi13101575
Sun Z, Wee C. 3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine. Micromachines. 2022; 13(10):1575. https://doi.org/10.3390/mi13101575
Chicago/Turabian StyleSun, Zhonghua, and Cleo Wee. 2022. "3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine" Micromachines 13, no. 10: 1575. https://doi.org/10.3390/mi13101575
APA StyleSun, Z., & Wee, C. (2022). 3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine. Micromachines, 13(10), 1575. https://doi.org/10.3390/mi13101575







