Current Review of Optical Neural Interfaces for Clinical Applications
Abstract
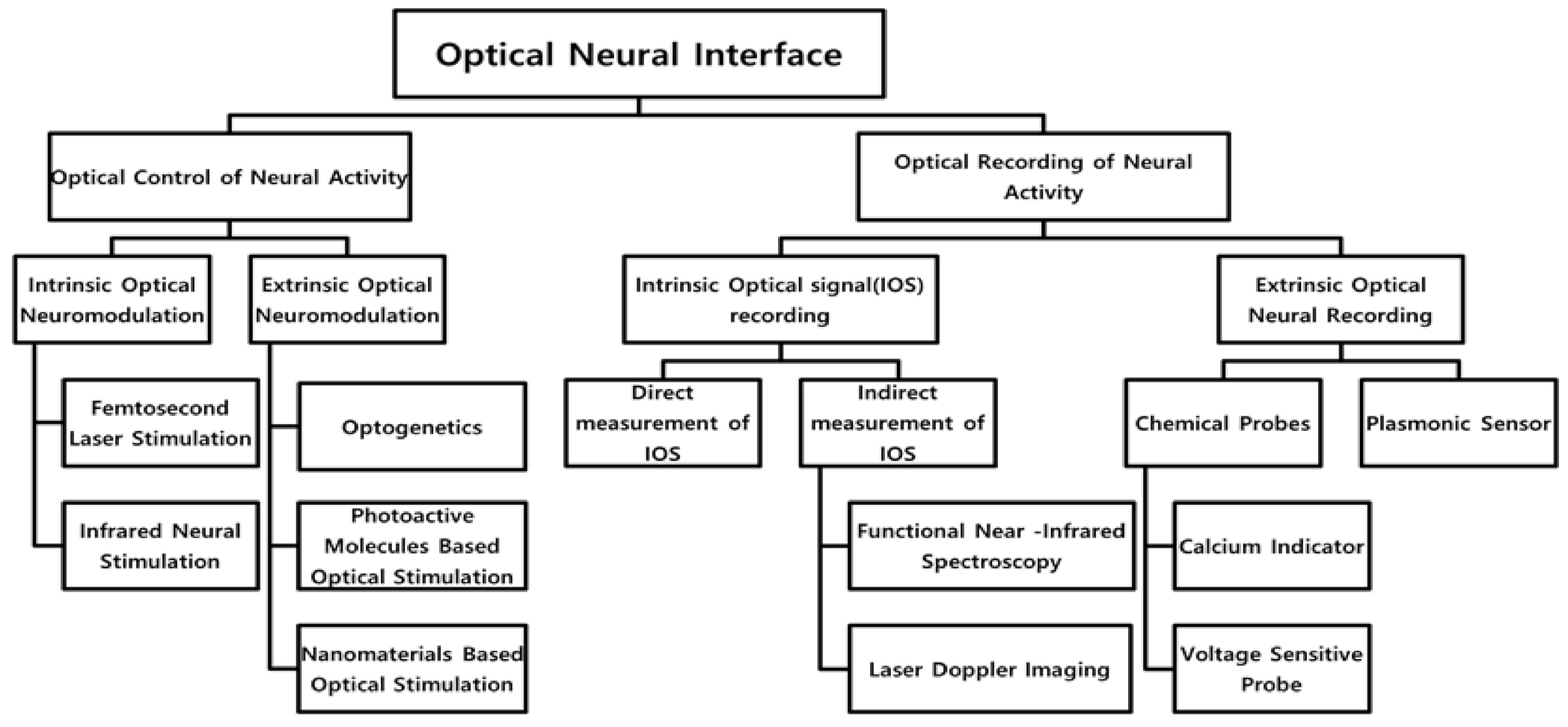
1. Introduction
2. Optical Control of Neural Activity
2.1. Intrinsic Optical Neuromodulation
2.1.1. Femtosecond Laser Stimulation
2.1.2. Infrared Neural Stimulation
2.2. Extrinsic Optical Neuromodulation
2.2.1. Optogenetics
2.2.2. Photoactive Molecules Based Optical Stimulation
2.2.3. Nanomaterials Based Optical Stimulation
3. Optical Recording of Neural Activity
3.1. Intrinsic Optical Signal (IOS) Recording
3.1.1. Direct Measurement of IOS
3.1.2. Indirect Measurement of IOS
Functional Near-Infrared Spectroscopy
Laser Doppler Imaging
Laser Speckle Contrast Imaging
3.2. Extrinsic Optical Neural Recording
3.2.1. Chemical Probes
Calcium Indicator
Voltage-Sensitive Probe
3.2.2. Plasmonic Sensor
4. Clinical Perspective of Optical Neural Interface
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Famm, K.; Litt, B.; Tracey, K.J.; Boyden, E.S.; Slaoui, M. A jump-start for electroceuticals. Nature 2013, 496, 159–161. [Google Scholar] [CrossRef]
- Brown, K.D.; Balkany, T.J. Benefits of bilateral cochlear implantation: A review. Curr. Opin. Otolaryngol. Head Neck Surg. 2007, 15, 315–318. [Google Scholar] [CrossRef]
- Fernandez, E. Development of visual Neuroprostheses: Trends and challenges. Bioelectron. Med. 2018, 4, 12. [Google Scholar] [CrossRef]
- Hatsopoulos, N.G.; Donoghue, J.P. The Science of Neural Interface Systems. Annu. Rev. Neurosci. 2009, 32, 249–266. [Google Scholar] [CrossRef] [PubMed]
- Donoghue, J.P. Bridging the Brain to the World: A Perspective on Neural Interface Systems. Neuron 2008, 60, 511–521. [Google Scholar] [CrossRef]
- Lai, W.K.; Müller-Deile, J.; Dillier, N.; Almqvist, B.; Stecker, M.; Frohne, C.; von Wallenberg, E. Measurement of the Electrically Evoked Compound Action Potential via a Neural Response Telemetry System. Ann. Otol. Rhinol. Laryngol. 2002, 111, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.J.M. EEG in the diagnosis, classification, and management of patients with epilepsy. J. Neurol. Neurosurg. Psychiatry 2005, 76, ii2–ii7. [Google Scholar] [CrossRef]
- Thompson, A.C.; Stoddart, R.P.; Jansen, E.D. Optical Stimulation of Neurons. Curr. Mol. Imaging 2015, 3, 162–177. [Google Scholar] [CrossRef] [PubMed]
- Eom, K.; Kim, J.; Choi, J.M.; Kang, T.; Chang, J.W.; Byun, K.M.; Jun, S.B.; Kim, S.J. Enhanced Infrared Neural Stimulation using Localized Surface Plasmon Resonance of Gold Nanorods. Small 2014, 10, 3853–3857. [Google Scholar] [CrossRef] [PubMed]
- Ae Kim, S.; Min Byun, K.; Lee, J.; Hoon Kim, J.; Albert Kim, D.-G.; Baac, H.; Shuler, M.L.; June Kim, S. Optical measurement of neural activity using surface plasmon resonance. Opt. Lett. 2008, 33, 914–916. [Google Scholar] [CrossRef] [PubMed]
- Warden, M.R.; Cardin, J.A.; Deisseroth, K. Optical Neural Interfaces. Annu. Rev. Biomed. Eng. 2014, 16, 103–129. [Google Scholar] [CrossRef]
- Blackmore, J.; Shrivastava, S.; Sallet, J.; Butler, C.R.; Cleveland, R.O. Ultrasound Neuromodulation: A Review of Results, Mechanisms and Safety. Ultrasound Med. Biol. 2019, 45, 1509–1536. [Google Scholar] [CrossRef] [PubMed]
- Hallett, M. Transcranial Magnetic Stimulation: A Primer. Neuron 2007, 55, 187–199. [Google Scholar] [CrossRef]
- Stapleton-Kotloski, J.; Kotloski, R.; Popli, G.; Godwin, D. Magnetoencephalography: Clinical and Research Practices. Brain Sci. 2018, 8, 157. [Google Scholar] [CrossRef]
- Hecht, E. Optics; Pearson Education: London, UK, 2017. [Google Scholar]
- Fork, R.L. Laser Stimulation of Nerve Cells in Aplysia. Science 1971, 171, 907. [Google Scholar] [CrossRef] [PubMed]
- Gratton, G.; Fabiani, M. Shedding light on brain function: The event-related optical signal. Trends Cogn. Sci. 2001, 5, 357–363. [Google Scholar] [CrossRef]
- Ferrari, M.; Quaresima, V. A brief review on the history of human functional near-infrared spectroscopy (fNIRS) development and fields of application. NeuroImage 2012, 63, 921–935. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.A.; Jun, S.B. In-vivo Optical Measurement of Neural Activity in the Brain. Exp. Neurobiol. 2013, 22, 158–166. [Google Scholar] [CrossRef]
- Balaban, P.; Esenaliev, R.; Karu, T.; Kutomkina, E.; Letokhov, V.; Oraevsky, A.; Ovcharenko, N. He-Ne laser irradiation of single identified neurons. Lasers Surg. Med. 1992, 12, 329–337. [Google Scholar] [CrossRef]
- Allègre, G.; Avrillier, S.; Albe-Fessard, D. Stimulation in the rat of a nerve fiber bundle by a short UV pulse from an excimer laser. Neurosci. Lett. 1994, 180, 261–264. [Google Scholar] [CrossRef]
- Hirase, H.; Nikolenko, V.; Goldberg, J.H.; Yuste, R. Multiphoton stimulation of neurons. J. Neurobiol. 2002, 51, 237–247. [Google Scholar] [CrossRef]
- Smith, N.I.; Fujita, K.; Kaneko, T.; Katoh, K.; Nakamura, O.; Kawata, S.; Takamatsu, T. Generation of calcium waves in living cells by pulsed-laser-induced photodisruption. Appl. Phys. Lett. 2001, 79, 1208–1210. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, Y.; Liu, X.; Lv, X.; Zhou, W.; Luo, Q.; Zeng, S. Photostimulation of astrocytes with femtosecond laser pulses. Opt. Express 2009, 17, 1291–1298. [Google Scholar] [CrossRef]
- Liu, X.; Lv, X.; Zeng, S.; Zhou, W.; Luo, Q. Noncontact and nondestructive identification of neural circuits with a femtosecond laser. Appl. Phys. Lett. 2009, 94, 061113. [Google Scholar] [CrossRef]
- Zhao, Y.; Liu, X.; Zhou, W.; Zeng, S. Astrocyte-to-neuron signaling in response to photostimulation with a femtosecond laser. Appl. Phys. Lett. 2010, 97, 063703. [Google Scholar] [CrossRef]
- Hosokawa, C.; Sakamoto, Y.; Kudoh, S.N.; Hosokawa, Y.; Taguchi, T. Femtosecond laser-induced stimulation of a single neuron in a neuronal network. Appl. Phys. A 2013, 110, 607–612. [Google Scholar] [CrossRef]
- Jang, J.M.; Lee, J.; Kim, H.; Jeon, N.L.; Jung, W. One-photon and two-photon stimulation of neurons in a microfluidic culture system. Lab. A Chip 2016, 16, 1684–1690. [Google Scholar] [CrossRef] [PubMed]
- Vogel, A.; Nahen, K.; Theisen, D.; Birngruber, R.; Thomas, R.J.; Rockwell, B.A. Influence of optical aberrations on laser-induced plasma formation in water and their consequences for intraocular photodisruption. Appl. Opt. 1999, 38, 3636–3643. [Google Scholar] [CrossRef] [PubMed]
- Vogel, A.; Noack, J.; Hüttman, G.; Paltauf, G. Mechanisms of femtosecond laser nanosurgery of cells and tissues. Appl. Phys. B 2005, 81, 1015–1047. [Google Scholar] [CrossRef]
- Yoon, J.; Ryu, S.-W.; Lee, S.; Choi, C. Cytosolic Irradiation of Femtosecond Laser Induces Mitochondria-dependent Apoptosis-like Cell Death via Intrinsic Reactive Oxygen Cascades. Sci. Rep. 2015, 5, 8231. [Google Scholar] [CrossRef]
- Wells, J.; Kao, C.; Mariappan, K.; Albea, J.; Jansen, E.D.; Konrad, P.; Mahadevan-Jansen, A. Optical stimulation of neural tissue in vivo. Opt. Lett. 2005, 30, 504–506. [Google Scholar] [CrossRef]
- Jonathon, D.W.; Chris Kao, M.D.; Jansen, E.D.; Peter, E.K.M.D.; Anita, M.-J. Application of infrared light for in vivo neural stimulation. J. Biomed. Opt. 2005, 10, 1–12. [Google Scholar] [CrossRef]
- Wells, J.; Konrad, P.; Kao, C.; Jansen, E.D.; Mahadevan-Jansen, A. Pulsed laser versus electrical energy for peripheral nerve stimulation. J. Neurosci. Methods 2007, 163, 326–337. [Google Scholar] [CrossRef] [PubMed]
- McCaughey, R.G.; Chlebicki, C.; Wong, B.J. Novel wavelengths for laser nerve stimulation. Lasers Surg. Med. 2010, 42, 69–75. [Google Scholar] [CrossRef]
- Thompson, A.C.; Wade, S.A.; Cadusch, P.J.; Brown, W.G.; Stoddart, P.R. Modeling of the temporal effects of heating during infrared neural stimulation. J. Biomed. Opt. 2013, 18, 035004. [Google Scholar] [CrossRef] [PubMed]
- Peterson, E.J.; Tyler, D.J. Motor neuron activation in peripheral nerves using infrared neural stimulation. J. Neural Eng. 2014, 11, 016001. [Google Scholar] [CrossRef]
- Izzo, A.D.; Richter, C.-P.; Jansen, E.D.; Walsh, J.T. Laser stimulation of the auditory nerve. Lasers Surg. Med. 2006, 38, 745–753. [Google Scholar] [CrossRef] [PubMed]
- Izzo, A.D.; Walsh, J.T.; Jansen, E.D.; Bendett, M.; Webb, J.; Ralph, H.; Richter, C. Optical Parameter Variability in Laser Nerve Stimulation: A Study of Pulse Duration, Repetition Rate, and Wavelength. IEEE Trans. Biomed. Eng. 2007, 54, 1108–1114. [Google Scholar] [CrossRef]
- Izzo, A.D.; Walsh, J.T., Jr.; Ralph, H.; Webb, J.; Bendett, M.; Wells, J.; Richter, C.-P. Laser stimulation of auditory neurons: Effect of shorter pulse duration and penetration depth. Biophys. J. 2008, 94, 3159–3166. [Google Scholar] [CrossRef]
- Richter, C.P.; Bayon, R.; Izzo, A.D.; Otting, M.; Suh, E.; Goyal, S.; Hotaling, J.; Walsh, J.T., Jr. Optical stimulation of auditory neurons: Effects of acute and chronic deafening. Hear. Res. 2008, 242, 42–51. [Google Scholar] [CrossRef]
- Izzo, A.D.; Suh, E.; Pathria, J.; Walsh, J.T.; Whitlon, D.S.; Richter, C.P. Selectivity of neural stimulation in the auditory system: A comparison of optic and electric stimuli. J. Biomed. Opt. 2007, 12, 021008. [Google Scholar] [CrossRef] [PubMed]
- Richter, C.-P.; Matic, A.I.; Wells, J.D.; Jansen, E.D.; Walsh, J.T., Jr. Neural stimulation with optical radiation. Laser Photon. Rev. 2011, 5, 68–80. [Google Scholar] [CrossRef] [PubMed]
- Schultz, M.; Baumhoff, P.; Maier, H.; Teudt, I.U.; Krüger, A.; Lenarz, T.; Kral, A. Nanosecond laser pulse stimulation of the inner ear—a wavelength study. Biomed. Opt. Express 2012, 3, 3332–3345. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Matic, A.I.; Robinson, A.M.; Young, H.K.; Badofsky, B.; Rajguru, S.M.; Stock, S.; Richter, C.-P. Behavioral and electrophysiological responses evoked by chronic infrared neural stimulation of the cochlea. PLoS ONE 2013, 8, e58189. [Google Scholar] [CrossRef]
- Verma, R.U.; Guex, A.A.; Hancock, K.E.; Durakovic, N.; McKay, C.M.; Slama, M.C.C.; Brown, M.C.; Lee, D.J. Auditory responses to electric and infrared neural stimulation of the rat cochlear nucleus. Hear. Res. 2014, 310, 69–75. [Google Scholar] [CrossRef]
- Teudt, I.U.; Nevel, A.E.; Izzo, A.D.; Walsh, J.T., Jr.; Richter, C.P. Optical stimulation of the facial nerve: A new monitoring technique? Laryngoscope 2007, 117, 1641–1647. [Google Scholar] [CrossRef]
- Jenkins, M.W.; Duke, A.R.; Gu, S.; Chiel, H.J.; Fujioka, H.; Watanabe, M.; Jansen, E.D.; Rollins, A.M. Optical pacing of the embryonic heart. Nat. Photonics 2010, 4, 623–626. [Google Scholar] [CrossRef]
- Cayce, J.M.; Kao, C.C.; Malphrus, J.D.; Konrad, P.E.; Mahadevan-Jansen, A.; Jansen, E.D. Infrared Neural Stimulation of Thalamocortical Brain Slices. IEEE J. Sel. Top. Quantum Electron. 2010, 16, 565–572. [Google Scholar] [CrossRef]
- Brown, W.G.A.; Needham, K.; Begeng, J.M.; Thompson, A.C.; Nayagam, B.A.; Kameneva, T.; Stoddart, P.R. Thermal damage threshold of neurons during infrared stimulation. Biomed. Opt. Express 2020, 11, 2224–2234. [Google Scholar] [CrossRef]
- Zhang, F.; Aravanis, A.M.; Adamantidis, A.; de Lecea, L.; Deisseroth, K. Circuit-breakers: Optical technologies for probing neural signals and systems. Nat. Rev. Neurosci. 2007, 8, 577–581. [Google Scholar] [CrossRef]
- Dugué, G.P.; Akemann, W.; Knöpfel, T. A comprehensive concept of optogenetics. Prog. Brain Res. 2012, 196, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Khorana, H.G.; Knox, B.E.; Nasi, E.; Swanson, R.; Thompson, D.A. Expression of a bovine rhodopsin gene in Xenopus oocytes: Demonstration of light-dependent ionic currents. Proc. Natl. Acad. Sci. USA 1988, 85, 7917–7921. [Google Scholar] [CrossRef]
- Zemelman, B.V.; Lee, G.A.; Ng, M.; Miesenböck, G. Selective photostimulation of genetically chARGed neurons. Neuron 2002, 33, 15–22. [Google Scholar] [CrossRef]
- Airan, R.D.; Thompson, K.R.; Fenno, L.E.; Bernstein, H.; Deisseroth, K. Temporally precise in vivo control of intracellular signalling. Nature 2009, 458, 1025–1029. [Google Scholar] [CrossRef]
- Oh, E.; Maejima, T.; Liu, C.; Deneris, E.; Herlitze, S. Substitution of 5-HT1A receptor signaling by a light-activated G protein-coupled receptor. J. Biol. Chem. 2010, 285, 30825–30836. [Google Scholar] [CrossRef] [PubMed]
- Nagel, G.; Ollig, D.; Fuhrmann, M.; Kateriya, S.; Musti, A.M.; Bamberg, E.; Hegemann, P. Channelrhodopsin-1: A light-gated proton channel in green algae. Science 2002, 296, 2395–2398. [Google Scholar] [CrossRef]
- Nagel, G.; Szellas, T.; Huhn, W.; Kateriya, S.; Adeishvili, N.; Berthold, P.; Ollig, D.; Hegemann, P.; Bamberg, E. Channelrhodopsin-2, a directly light-gated cation-selective membrane channel. Proc. Natl. Acad. Sci. USA 2003, 100, 13940. [Google Scholar] [CrossRef]
- Nagel, G.; Szellas, T.; Kateriya, S.; Adeishvili, N.; Hegemann, P.; Bamberg, E. Channelrhodopsins: Directly light-gated cation channels. Biochem. Soc. Trans. 2005, 33, 863–866. [Google Scholar] [CrossRef]
- Boyden, E.S.; Zhang, F.; Bamberg, E.; Nagel, G.; Deisseroth, K. Millisecond-timescale, genetically targeted optical control of neural activity. Nat. Neurosci. 2005, 8, 1263–1268. [Google Scholar] [CrossRef]
- Zhang, F.; Prigge, M.; Beyrière, F.; Tsunoda, S.P.; Mattis, J.; Yizhar, O.; Hegemann, P.; Deisseroth, K. Red-shifted optogenetic excitation: A tool for fast neural control derived from Volvox carteri. Nat. Neurosci. 2008, 11, 631–633. [Google Scholar] [CrossRef]
- Govorunova, E.G.; Spudich, E.N.; Lane, C.E.; Sineshchekov, O.A.; Spudich, J.L. New channelrhodopsin with a red-shifted spectrum and rapid kinetics from Mesostigma viride. mBio 2011, 2, e00115-11. [Google Scholar] [CrossRef]
- Béjà, O.; Aravind, L.; Koonin, E.V.; Suzuki, M.T.; Hadd, A.; Nguyen, L.P.; Jovanovich, S.B.; Gates, C.M.; Feldman, R.A.; Spudich, J.L.; et al. Bacterial rhodopsin: Evidence for a new type of phototrophy in the sea. Science 2000, 289, 1902–1906. [Google Scholar] [CrossRef] [PubMed]
- Waschuk, S.A.; Bezerra, A.G., Jr.; Shi, L.; Brown, L.S. Leptosphaeria rhodopsin: Bacteriorhodopsin-like proton pump from a eukaryote. Proc. Natl. Acad. Sci. USA 2005, 102, 6879–6883. [Google Scholar] [CrossRef] [PubMed]
- Müller, V.; Oren, A. Metabolism of chloride in halophilic prokaryotes. Extremophiles 2003, 7, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Wang, L.P.; Brauner, M.; Liewald, J.F.; Kay, K.; Watzke, N.; Wood, P.G.; Bamberg, E.; Nagel, G.; Gottschalk, A.; et al. Multimodal fast optical interrogation of neural circuitry. Nature 2007, 446, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Yizhar, O.; Fenno, L.E.; Davidson, T.J.; Mogri, M.; Deisseroth, K. Optogenetics in Neural Systems. Neuron 2011, 71, 9–34. [Google Scholar] [CrossRef]
- Sahel, J.-A.; Boulanger-Scemama, E.; Pagot, C.; Arleo, A.; Galluppi, F.; Martel, J.N.; Esposti, S.D.; Delaux, A.; de Saint Aubert, J.-B.; de Montleau, C.; et al. Partial recovery of visual function in a blind patient after optogenetic therapy. Nat. Med. 2021, 27, 1223–1229. [Google Scholar] [CrossRef]
- Kramer, R.H.; Fortin, D.L.; Trauner, D. New photochemical tools for controlling neuronal activity. Curr. Opin. Neurobiol. 2009, 19, 544–552. [Google Scholar] [CrossRef]
- Fortin, D.L.; Banghart, M.R.; Dunn, T.W.; Borges, K.; Wagenaar, D.A.; Gaudry, Q.; Karakossian, M.H.; Otis, T.S.; Kristan, W.B.; Trauner, D.; et al. Photochemical control of endogenous ion channels and cellular excitability. Nat. Methods 2008, 5, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Nerbonne, J.M. Caged compounds: Tools for illuminating neuronal responses and connections. Curr. Opin. Neurobiol. 1996, 6, 379–386. [Google Scholar] [CrossRef]
- Kandler, K.; Katz, L.C.; Kauer, J. Focal photolysis of caged glutamate produces long-term depression of hippocampal glutamate receptors. Nat. Neurosci. 1998, 1, 119–123. [Google Scholar] [CrossRef]
- Dalva, M.B.; Katz, L.C. Rearrangements of synaptic connections in visual cortex revealed by laser photostimulation. Science 1994, 265, 255–258. [Google Scholar] [CrossRef]
- Katz, L.C.; Dalva, M.B. Scanning laser photostimulation: A new approach for analyzing brain circuits. J. Neurosci. Methods 1994, 54, 205–218. [Google Scholar] [CrossRef]
- Schiller, J.; Schiller, Y.; Clapham, D.E. NMDA receptors amplify calcium influx into dendritic spines during associative pre- and postsynaptic activation. Nat. Neurosci. 1998, 1, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Schiller, J.; Major, G.; Koester, H.J.; Schiller, Y. NMDA spikes in basal dendrites of cortical pyramidal neurons. Nature 2000, 404, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Lima, S.Q.; Miesenböck, G. Remote Control of Behavior through Genetically Targeted Photostimulation of Neurons. Cell 2005, 121, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Bartels, E.; Wassermann, N.H.; Erlanger, B.F. Photochromic activators of the acetylcholine receptor. Proc. Natl. Acad. Sci. USA 1971, 68, 1820–1823. [Google Scholar] [CrossRef] [PubMed]
- Volgraf, M.; Gorostiza, P.; Numano, R.; Kramer, R.H.; Isacoff, E.Y.; Trauner, D. Allosteric control of an ionotropic glutamate receptor with an optical switch. Nat. Chem. Biol. 2006, 2, 47–52. [Google Scholar] [CrossRef]
- Banghart, M.; Borges, K.; Isacoff, E.; Trauner, D.; Kramer, R.H. Light-activated ion channels for remote control of neuronal firing. Nat. Neurosci. 2004, 7, 1381–1386. [Google Scholar] [CrossRef]
- Chambers, J.J.; Banghart, M.R.; Trauner, D.; Kramer, R.H. Light-induced depolarization of neurons using a modified Shaker K(+) channel and a molecular photoswitch. J. Neurophysiol. 2006, 96, 2792–2796. [Google Scholar] [CrossRef]
- Fortin, D.L.; Dunn, T.W.; Fedorchak, A.; Allen, D.; Montpetit, R.; Banghart, M.R.; Trauner, D.; Adelman, J.P.; Kramer, R.H. Optogenetic photochemical control of designer K+ channels in mammalian neurons. J. Neurophysiol. 2011, 106, 488–496. [Google Scholar] [CrossRef] [PubMed]
- Janovjak, H.; Szobota, S.; Wyart, C.; Trauner, D.; Isacoff, E.Y. A light-gated, potassium-selective glutamate receptor for the optical inhibition of neuronal firing. Nat. Neurosci. 2010, 13, 1027–1032. [Google Scholar] [CrossRef]
- Narayanan, D.L.; Saladi, R.N.; Fox, J.L. Review: Ultraviolet radiation and skin cancer. Int. J. Dermatol. 2010, 49, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Jaque, D.; Martínez Maestro, L.; Del Rosal, B.; Haro-Gonzalez, P.; Benayas, A.; Plaza, J.L.; Martín Rodríguez, E.; García Solé, J. Nanoparticles for photothermal therapies. Nanoscale 2014, 6, 9494–9530. [Google Scholar] [CrossRef] [PubMed]
- Baffou, G.; Quidant, R. Thermo-plasmonics: Using metallic nanostructures as nano-sources of heat. Laser Photon. Rev. 2013, 7, 171–187. [Google Scholar] [CrossRef]
- Eom, K.; Byun, K.M.; Jun, S.B.; Kim, S.J.; Lee, J. Theoretical Study on Gold-Nanorod-Enhanced Near-Infrared Neural Stimulation. Biophys. J. 2018, 115, 1481–1497. [Google Scholar] [CrossRef]
- Paviolo, C.; Haycock, J.W.; Cadusch, P.J.; McArthur, S.L.; Stoddart, P.R. Laser exposure of gold nanorods can induce intracellular calcium transients. J. Biophotonics 2014, 7, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Paviolo, C.; Haycock, J.W.; Yong, J.; Yu, A.; Stoddart, P.R.; McArthur, S.L. Laser exposure of gold nanorods can increase neuronal cell outgrowth. Biotechnol. Bioeng. 2013, 110, 2277–2291. [Google Scholar] [CrossRef]
- Yong, J.; Needham, K.; Brown, W.G.; Nayagam, B.A.; McArthur, S.L.; Yu, A.; Stoddart, P.R. Gold-nanorod-assisted near-infrared stimulation of primary auditory neurons. Adv. Healthc. Mater. 2014, 3, 1862–1868. [Google Scholar] [CrossRef]
- Carvalho-de-Souza, J.L.; Treger, J.S.; Dang, B.; Kent, S.B.H.; Pepperberg, D.R.; Bezanilla, F. Photosensitivity of Neurons Enabled by Cell-Targeted Gold Nanoparticles. Neuron 2015, 86, 207–217. [Google Scholar] [CrossRef]
- Eom, K.; Im, C.; Hwang, S.; Eom, S.; Kim, T.-S.; Jeong, H.S.; Kim, K.H.; Byun, K.M.; Jun, S.B.; Kim, S.J. Synergistic combination of near-infrared irradiation and targeted gold nanoheaters for enhanced photothermal neural stimulation. Biomed. Opt. Express 2016, 7, 1614–1625. [Google Scholar] [CrossRef]
- Nakatsuji, H.; Numata, T.; Morone, N.; Kaneko, S.; Mori, Y.; Imahori, H.; Murakami, T. Thermosensitive Ion Channel Activation in Single Neuronal Cells by Using Surface-Engineered Plasmonic Nanoparticles. Angew. Chem. Int. Ed. 2015, 54, 11725–11729. [Google Scholar] [CrossRef]
- Carvalho-de-Souza, J.L.; Nag, O.K.; Oh, E.; Huston, A.L.; Vurgaftman, I.; Pepperberg, D.R.; Bezanilla, F.; Delehanty, J.B. Cholesterol Functionalization of Gold Nanoparticles Enhances Photoactivation of Neural Activity. ACS Chem. Neurosci. 2019, 10, 1478–1487. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.; Hong, S.; Choi, Y.; Park, J.-H.; Nam, Y. Photothermal Inhibition of Neural Activity with Near-Infrared-Sensitive Nanotransducers. ACS Nano 2014, 8, 8040–8049. [Google Scholar] [CrossRef]
- Eom, K.; Hwang, S.; Yun, S.; Byun, K.M.; Jun, S.B.; Kim, S.J. Photothermal activation of astrocyte cells using localized surface plasmon resonance of gold nanorods. J. Biophotonics 2017, 10, 486–493. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.; Kim, R.; Park, J.-H.; Nam, Y. Electro-optical Neural Platform Integrated with Nanoplasmonic Inhibition Interface. ACS Nano 2016, 10, 4274–4281. [Google Scholar] [CrossRef]
- Jung, H.; Kang, H.; Nam, Y. Digital micromirror based near-infrared illumination system for plasmonic photothermal neuromodulation. Biomed. Opt. Express 2017, 8, 2866–2878. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.; Park, J.-H.; Nam, Y. Single-Cell Photothermal Neuromodulation for Functional Mapping of Neural Networks. ACS Nano 2019, 13, 544–551. [Google Scholar] [CrossRef]
- Shim, S.; Eom, K.; Jeong, J.; Kim, S.J. Retinal Prosthetic Approaches to Enhance Visual Perception for Blind Patients. Micromachines 2020, 11, 535. [Google Scholar] [CrossRef]
- Stingl, K.; Bartz-Schmidt, K.U.; Besch, D.; Braun, A.; Bruckmann, A.; Gekeler, F.; Greppmaier, U.; Hipp, S.; Hörtdörfer, G.; Kernstock, C.; et al. Artificial vision with wirelessly powered subretinal electronic implant alpha-IMS. Proc. R. Soc. B Biol. Sci. 2013, 280, 20130077. [Google Scholar] [CrossRef]
- Mathieson, K.; Loudin, J.; Goetz, G.; Huie, P.; Wang, L.; Kamins, T.I.; Galambos, L.; Smith, R.; Harris, J.S.; Sher, A.; et al. Photovoltaic retinal prosthesis with high pixel density. Nat. Photonics 2012, 6, 391–397. [Google Scholar] [CrossRef]
- Mandel, Y.; Goetz, G.; Lavinsky, D.; Huie, P.; Mathieson, K.; Wang, L.; Kamins, T.; Galambos, L.; Manivanh, R.; Harris, J.; et al. Cortical responses elicited by photovoltaic subretinal prostheses exhibit similarities to visually evoked potentials. Nat. Commun. 2013, 4, 1980. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Qin, N.; Chong, Y.; Diao, Y.; Yiliguma; Wang, Z.; Xue, T.; Jiang, M.; Zhang, J.; Zheng, G. Nanowire arrays restore vision in blind mice. Nat. Commun. 2018, 9, 786. [Google Scholar] [CrossRef]
- Savchenko, A.; Cherkas, V.; Liu, C.; Braun, G.B.; Kleschevnikov, A.; Miller, Y.I.; Molokanova, E. Graphene biointerfaces for optical stimulation of cells. Sci. Adv. 2018, 4, eaat0351. [Google Scholar] [CrossRef] [PubMed]
- Kornreich, B.G. The patch clamp technique: Principles and technical considerations. J. Vet. Cardiol 2007, 9, 25–37. [Google Scholar] [CrossRef]
- Obien, M.E.J.; Deligkaris, K.; Bullmann, T.; Bakkum, D.J.; Frey, U. Revealing neuronal function through microelectrode array recordings. Front. Neurosci. 2015, 8. [Google Scholar] [CrossRef] [PubMed]
- Christopher deCharms, R. Applications of real-time fMRI. Nat. Rev. Neurosci. 2008, 9, 720–729. [Google Scholar] [CrossRef] [PubMed]
- Shukla, A.K.; Kumar, U. Positron emission tomography: An overview. J. Med. Phys. 2006, 31, 13–21. [Google Scholar] [CrossRef]
- Hill, D.K.; Keynes, R.D. Opacity changes in stimulated nerve. J. Physiol. 1949, 108, 278–281. [Google Scholar] [CrossRef]
- Stepnoski, R.A.; LaPorta, A.; Raccuia-Behling, F.; Blonder, G.E.; Slusher, R.E.; Kleinfeld, D. Noninvasive detection of changes in membrane potential in cultured neurons by light scattering. Proc. Natl. Acad. Sci. USA 1991, 88, 9382–9386. [Google Scholar] [CrossRef] [PubMed]
- Rector, D.M.; Poe, G.R.; Kristensen, M.P.; Harper, R.M. Light scattering changes follow evoked potentials from hippocampal Schaeffer collateral stimulation. J. Neurophysiol. 1997, 78, 1707–1713. [Google Scholar] [CrossRef] [PubMed]
- Gratton, G.; Fabiani, M.; Corballis, P.M.; Hood, D.C.; Goodman-Wood, M.R.; Hirsch, J.; Kim, K.; Friedman, D.; Gratton, E. Fast and Localized Event-Related Optical Signals (EROS) in the Human Occipital Cortex: Comparisons with the Visual Evoked Potential and fMRI. NeuroImage 1997, 6, 168–180. [Google Scholar] [CrossRef]
- Gratton, G.; Corballis, P.M.; Cho, E.; Fabiani, M.; Hood, D.C. Shades of gray matter: Noninvasive optical images of human brain responses during visual stimulation. Psychophysiology 1995, 32, 505–509. [Google Scholar] [CrossRef]
- Gratton, E.; Limkeman, M. A continuously variable frequency cross-correlation phase fluorometer with picosecond resolution. Biophys. J. 1983, 44, 315–324. [Google Scholar] [CrossRef]
- Tong, S.; Thakor, N.V. Quantitative EEG Analysis Methods and Clinical Applications; Artech House: London, UK; Norwood, MA, USA, 2009. [Google Scholar]
- Steinbrink, J.; Kempf, F.C.; Villringer, A.; Obrig, H. The fast optical signal--robust or elusive when non-invasively measured in the human adult? Neuroimage 2005, 26, 996–1008. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, H.; Vanduffel, W.; Deng, H.P.; Ekstrom, L.; Boas, D.A.; Franceschini, M.A. Fast optical signal not detected in awake behaving monkeys. NeuroImage 2009, 45, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Liao, L.D.; Tsytsarev, V.; Delgado-Martínez, I.; Li, M.L.; Erzurumlu, R.; Vipin, A.; Orellana, J.; Lin, Y.R.; Lai, H.Y.; Chen, Y.Y.; et al. Neurovascular coupling: In vivo optical techniques for functional brain imaging. Biomed. Eng. Online 2013, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Scholkmann, F.; Kleiser, S.; Metz, A.J.; Zimmermann, R.; Mata Pavia, J.; Wolf, U.; Wolf, M. A review on continuous wave functional near-infrared spectroscopy and imaging instrumentation and methodology. Neuroimage 2014, 85 Pt 1, 6–27. [Google Scholar] [CrossRef]
- Jöbsis, F.F. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 1977, 198, 1264–1267. [Google Scholar] [CrossRef]
- Brazy, J.E.; Lewis, D.V.; Mitnick, M.H.; Jöbsis vander Vliet, F.F. Noninvasive monitoring of cerebral oxygenation in preterm infants: Preliminary observations. Pediatrics 1985, 75, 217–225. [Google Scholar]
- Hoshi, Y.; Tamura, M. Detection of dynamic changes in cerebral oxygenation coupled to neuronal function during mental work in man. Neurosci. Lett. 1993, 150, 5–8. [Google Scholar] [CrossRef]
- Kato, T.; Kamei, A.; Takashima, S.; Ozaki, T. Human visual cortical function during photic stimulation monitoring by means of near-infrared spectroscopy. J. Cereb. Blood Flow Metab. 1993, 13, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Villringer, A.; Planck, J.; Hock, C.; Schleinkofer, L.; Dirnagl, U. Near infrared spectroscopy (NIRS): A new tool to study hemodynamic changes during activation of brain function in human adults. Neurosci. Lett. 1993, 154, 101–104. [Google Scholar] [CrossRef]
- Herold, F.; Wiegel, P.; Scholkmann, F.; Müller, N.G. Applications of Functional Near-Infrared Spectroscopy (fNIRS) Neuroimaging in Exercise–Cognition Science: A Systematic, Methodology-Focused Review. J. Clin. Med. 2018, 7, 466. [Google Scholar] [CrossRef] [PubMed]
- Scholkmann, F.; Wolf, M. Measuring brain activity using functional near infrared spectroscopy: A short review. Spectrosc. Eur. 2012, 24, 6. [Google Scholar]
- Quaresima, V.; Ferrari, M. Functional Near-Infrared Spectroscopy (fNIRS) for Assessing Cerebral Cortex Function During Human Behavior in Natural/Social Situations: A Concise Review. Organ. Res. Methods 2016, 22, 46–68. [Google Scholar] [CrossRef]
- Watanabe, E.; Maki, A.; Kawaguchi, F.; Takashiro, K.; Yamashita, Y.; Koizumi, H.; Mayanagi, Y. Non-invasive assessment of language dominance with near-infrared spectroscopic mapping. Neurosci. Lett. 1998, 256, 49–52. [Google Scholar] [CrossRef]
- Naseer, N.; Hong, K.-S. fNIRS-based brain-computer interfaces: A review. Front. Hum. Neurosci. 2015, 9. [Google Scholar] [CrossRef]
- Hoshi, Y.; Kobayashi, N.; Tamura, M. Interpretation of near-infrared spectroscopy signals: A study with a newly developed perfused rat brain model. J. Appl. Physiol. 2001, 90, 1657–1662. [Google Scholar] [CrossRef]
- Sato, Y.; Fukuda, M.; Oishi, M.; Shirasawa, A.; Fujii, Y. Ictal near-infrared spectroscopy and electrocorticography study of supplementary motor area seizures. J. Biomed. Opt. 2013, 18, 76022. [Google Scholar] [CrossRef][Green Version]
- Zhang, T.; Zhou, J.; Jiang, R.; Yang, H.; Carney, P.R.; Jiang, H. Pre-seizure state identified by diffuse optical tomography. Sci. Rep. 2014, 4, 3798. [Google Scholar] [CrossRef] [PubMed]
- Eggebrecht, A.T.; Ferradal, S.L.; Robichaux-Viehoever, A.; Hassanpour, M.S.; Dehghani, H.; Snyder, A.Z.; Hershey, T.; Culver, J.P. Mapping distributed brain function and networks with diffuse optical tomography. Nat. Photonics 2014, 8, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Yücel, M.A.; Aasted, C.M.; Petkov, M.P.; Borsook, D.; Boas, D.A.; Becerra, L. Specificity of hemodynamic brain responses to painful stimuli: A functional near-infrared spectroscopy study. Sci. Rep. 2015, 5, 9469. [Google Scholar] [CrossRef]
- Kadamati, P.; Sugar, J.J.; Quirk, B.J.; Mehrvar, S.; Chelimsky, G.G.; Whelan, H.T.; Chelimsky, T.C.; Ranji, M. Near-infrared spectroscopy muscle oximetry of patients with postural orthostatic tachycardia syndrome. J. Innov. Opt. Health Sci. 2018, 11. [Google Scholar] [CrossRef] [PubMed]
- Rajan, V.; Varghese, B.; van Leeuwen, T.G.; Steenbergen, W. Review of methodological developments in laser Doppler flowmetry. Lasers Med. Sci. 2009, 24, 269–283. [Google Scholar] [CrossRef]
- RIVA, C.; ROSS, B.; BENEDEK, G.B. Laser Doppler Measurements of Blood Flow in Capillary Tubes and Retinal Arteries. Investig. Ophthalmol. Vis. Sci. 1972, 11, 936–944. [Google Scholar]
- Lindauer, U.; Villringer, A.; Dirnagl, U. Characterization of CBF response to somatosensory stimulation: Model and influence of anesthetics. Am. J. Physiol. 1993, 264, H1223–H1228. [Google Scholar] [CrossRef] [PubMed]
- Ngai, A.C.; Meno, J.R.; Winn, H.R. Simultaneous measurements of pial arteriolar diameter and laser-Doppler flow during somatosensory stimulation. J. Cereb. Blood Flow Metab. 1995, 15, 124–127. [Google Scholar] [CrossRef]
- Detre, J.A.; Ances, B.M.; Takahashi, K.; Greenberg, J.H. Signal averaged laser Doppler measurements of activation–flow coupling in the rat forepaw somatosensory cortex. Brain Res. 1998, 796, 91–98. [Google Scholar] [CrossRef]
- Ances, B.M.; Greenberg, J.H.; Detre, J.A. Laser Doppler Imaging of Activation-Flow Coupling in the Rat Somatosensory Cortex. NeuroImage 1999, 10, 716–723. [Google Scholar] [CrossRef]
- Serov, A.; Steenbergen, W.; de Mul, F. Laser Doppler perfusion imaging with a complimentary metal oxide semiconductor image sensor. Opt. Lett. 2002, 27, 300–302. [Google Scholar] [CrossRef]
- Serov, A.; Steinacher, B.; Lasser, T. Full-field laser Doppler perfusion imaging and monitoring with an intelligent CMOS camera. Opt. Express 2005, 13, 3681–3689. [Google Scholar] [CrossRef] [PubMed]
- Kannurpatti, S.S.; Biswal, B.B. Negative Functional Response to Sensory Stimulation and its Origins. J. Cereb. Blood Flow Metab. 2004, 24, 703–712. [Google Scholar] [CrossRef]
- Raabe, A.; Van De Ville, D.; Leutenegger, M.; Szelényi, A.; Hattingen, E.; Gerlach, R.; Seifert, V.; Hauger, C.; Lopez, A.; Leitgeb, R.; et al. Laser Doppler imaging for intraoperative human brain mapping. NeuroImage 2009, 44, 1284–1289. [Google Scholar] [CrossRef][Green Version]
- Kingwell, B.A.; Formosa, M.; Muhlmann, M.; Bradley, S.J.; McConell, G.K. Type 2 diabetic individuals have impaired leg blood flow responses to exercise: Role of endothelium-dependent vasodilation. Diabetes Care 2003, 26, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Murray, A.K.; Herrick, A.L.; King, T.A. Laser Doppler imaging: A developing technique for application in the rheumatic diseases. Rheumatology 2004, 43, 1210–1218. [Google Scholar] [CrossRef] [PubMed]
- Riva, C.E.; Falsini, B. Functional laser Doppler flowmetry of the optic nerve: Physiological aspects and clinical applications. Prog. Brain Res. 2008, 173, 149–163. [Google Scholar] [CrossRef]
- Boas, D.A.; Dunn, A.K. Laser speckle contrast imaging in biomedical optics. J. Biomed. Opt. 2010, 15, 011109. [Google Scholar] [CrossRef]
- Dunn, A.K. Laser speckle contrast imaging of cerebral blood flow. Ann. Biomed. Eng. 2012, 40, 367–377. [Google Scholar] [CrossRef]
- Senarathna, J.; Rege, A.; Li, N.; Thakor, N.V. Laser Speckle Contrast Imaging: Theory, instrumentation and applications. IEEE Rev. Biomed. Eng. 2013, 6, 99–110. [Google Scholar] [CrossRef]
- Briers, D.; Duncan, D.D.; Hirst, E.R.; Kirkpatrick, S.J.; Larsson, M.; Steenbergen, W.; Stromberg, T.; Thompson, O.B. Laser speckle contrast imaging: Theoretical and practical limitations. J. Biomed. Opt. 2013, 18, 066018. [Google Scholar] [CrossRef]
- Fercher, A.F.; Briers, J.D. Flow visualization by means of single-exposure speckle photography. Opt. Commun. 1981, 37, 326–330. [Google Scholar] [CrossRef]
- Bolay, H.; Reuter, U.; Dunn, A.K.; Huang, Z.; Boas, D.A.; Moskowitz, M.A. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nat. Med. 2002, 8, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Dunn, A.K.; Bolay, H.; Moskowitz, M.A.; Boas, D.A. Dynamic imaging of cerebral blood flow using laser speckle. J. Cereb. Blood Flow Metab. 2001, 21, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.J.; Frank, R.; Forrester, K.R.; Tulip, J.; Lindsay, R.; Bray, R.C. A comparison of two laser-based methods for determination of burn scar perfusion: Laser Doppler versus laser speckle imaging. Burns 2005, 31, 744–752. [Google Scholar] [CrossRef]
- Stewart, C.J.; Gallant-Behm, C.L.; Forrester, K.; Tulip, J.; Hart, D.A.; Bray, R.C. Kinetics of blood flow during healing of excisional full-thickness skin wounds in pigs as monitored by laser speckle perfusion imaging. Ski. Res. Technol. 2006, 12, 247–253. [Google Scholar] [CrossRef]
- Srienc, A.I.; Kurth-Nelson, Z.L.; Newman, E.A. Imaging retinal blood flow with laser speckle flowmetry. Front. Neuroenergetics 2010, 2, 128. [Google Scholar] [CrossRef] [PubMed]
- Dunn, A.K.; Devor, A.; Dale, A.M.; Boas, D.A. Spatial extent of oxygen metabolism and hemodynamic changes during functional activation of the rat somatosensory cortex. Neuroimage 2005, 27, 279–290. [Google Scholar] [CrossRef]
- Heeman, W.; Steenbergen, W.; van Dam, G.M.; Boerma, E.C. Clinical applications of laser speckle contrast imaging: A review. J. Biomed. Opt. 2019, 24, 080901. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, Y.; Araie, M.; Kawamoto, E.; Eguchi, S.; Fujii, H. Noncontact, two-dimensional measurement of retinal microcirculation using laser speckle phenomenon. Invest. Ophthalmol. Vis. Sci. 1994, 35, 3825–3834. [Google Scholar] [PubMed]
- Klijn, E.; Hulscher, H.C.; Balvers, R.K.; Holland, W.P.; Bakker, J.; Vincent, A.J.; Dirven, C.M.; Ince, C. Laser speckle imaging identification of increases in cortical microcirculatory blood flow induced by motor activity during awake craniotomy. J. Neurosurg. 2013, 118, 280–286. [Google Scholar] [CrossRef]
- Grienberger, C.; Konnerth, A. Imaging Calcium in Neurons. Neuron 2012, 73, 862–885. [Google Scholar] [CrossRef] [PubMed]
- Berridge, M.J.; Lipp, P.; Bootman, M.D. The versatility and universality of calcium signalling. Nat. Rev. Mol. Cell Biol. 2000, 1, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, R.; Nimchinsky, E.A.; Scheuss, V.; Pologruto, T.A.; Oertner, T.G.; Sabatini, B.L.; Svoboda, K. Imaging calcium concentration dynamics in small neuronal compartments. Sci STKE 2004, 2004, pl5. [Google Scholar] [CrossRef]
- Shimomura, O.; Johnson, F.H.; Saiga, Y. Extraction, Purification and Properties of Aequorin, a Bioluminescent Protein from the Luminous Hydromedusan, Aequorea. J. Cell. Comp. Physiol. 1962, 59, 223–239. [Google Scholar] [CrossRef]
- Ashley, C.C.; Ridgway, E.B. Simultaneous Recording of Membrane Potential, Calcium Transient and Tension in Single Muscle Fibres. Nature 1968, 219, 1168–1169. [Google Scholar] [CrossRef]
- Hallett, M.; Carbone, E. Studies of calcium influx into squid giant axons with aequorin. J. Cell. Physiol. 1972, 80, 219–226. [Google Scholar] [CrossRef]
- Stinnakre, J.; Tauc, L. Calcium Influx in Active Aplysia Neurones detected by Injected Aequorin. Nat. New Biol. 1973, 242, 113–115. [Google Scholar] [CrossRef]
- Tsien, R.Y. New calcium indicators and buffers with high selectivity against magnesium and protons: Design, synthesis, and properties of prototype structures. Biochemistry 1980, 19, 2396–2404. [Google Scholar] [CrossRef] [PubMed]
- Tsien, R.Y.; Pozzan, T.; Rink, T.J. Calcium homeostasis in intact lymphocytes: Cytoplasmic free calcium monitored with a new, intracellularly trapped fluorescent indicator. J. Cell Biol. 1982, 94, 325–334. [Google Scholar] [CrossRef]
- Zhong, C.; Schleifenbaum, J. Genetically Encoded Calcium Indicators: A New Tool in Renal Hypertension Research. Front. Med. 2019, 6. [Google Scholar] [CrossRef]
- Rizzuto, R.; Brini, M.; Pozzan, T. Targeting recombinant aequorin to specific intracellular organelles. Methods Cell Biol. 1994, 40, 339–358. [Google Scholar] [CrossRef]
- Ohkura, M.; Matsuzaki, M.; Kasai, H.; Imoto, K.; Nakai, J. Genetically encoded bright Ca2+ probe applicable for dynamic Ca2+ imaging of dendritic spines. Anal. Chem. 2005, 77, 5861–5869. [Google Scholar] [CrossRef]
- Russell, J.T. Imaging calcium signals in vivo: A powerful tool in physiology and pharmacology. Br. J. Pharm. 2011, 163, 1605–1625. [Google Scholar] [CrossRef]
- Wirth, D.; Gama-Norton, L.; Riemer, P.; Sandhu, U.; Schucht, R.; Hauser, H. Road to precision: Recombinase-based targeting technologies for genome engineering. Curr. Opin. Biotechnol. 2007, 18, 411–419. [Google Scholar] [CrossRef]
- Peterka, D.S.; Takahashi, H.; Yuste, R. Imaging voltage in neurons. Neuron 2011, 69, 9–21. [Google Scholar] [CrossRef]
- Tasaki, I.; Carnay, L.; Sandlin, R.; Watanabe, A. Fluorescence changes during conduction in nerves stained with Acridine Orange. Science 1969, 163, 683–685. [Google Scholar] [CrossRef]
- Cohen, L.B.; Salzberg, B.M.; Davila, H.V.; Ross, W.N.; Landowne, D.; Waggoner, A.S.; Wang, C.H. Changes in axon fluorescence during activity: Molecular probes of membrane potential. J. Membr. Biol. 1974, 19, 1–36. [Google Scholar] [CrossRef] [PubMed]
- Grinvald, A.; Ross, W.N.; Farber, I. Simultaneous optical measurements of electrical activity from multiple sites on processes of cultured neurons. Proc. Natl. Acad. Sci. USA 1981, 78, 3245–3249. [Google Scholar] [CrossRef] [PubMed]
- Grinvald, A.; Manker, A.; Segal, M. Visualization of the spread of electrical activity in rat hippocampal slices by voltage-sensitive optical probes. J. Physiol. 1982, 333, 269–291. [Google Scholar] [CrossRef] [PubMed]
- Grinvald, A.; Hildesheim, R. VSDI: A new era in functional imaging of cortical dynamics. Nat. Rev. Neurosci. 2004, 5, 874–885. [Google Scholar] [CrossRef]
- Orbach, H.; Cohen, L.; Grinvald, A. Optical mapping of electrical activity in rat somatosensory and visual cortex. J. Neurosci. 1985, 5, 1886–1895. [Google Scholar] [CrossRef] [PubMed]
- Grinvald, A.; Lieke, E.E.; Frostig, R.D.; Hildesheim, R. Cortical point-spread function and long-range lateral interactions revealed by real-time optical imaging of macaque monkey primary visual cortex. J. Neurosci. 1994, 14, 2545–2568. [Google Scholar] [CrossRef] [PubMed]
- Loew, L.M.; Cohen, L.B.; Salzberg, B.M.; Obaid, A.L.; Bezanilla, F. Charge-shift probes of membrane potential. Characterization of aminostyrylpyridinium dyes on the squid giant axon. Biophys. J. 1985, 47, 71–77. [Google Scholar] [CrossRef]
- Knöpfel, T. Genetically encoded optical indicators for the analysis of neuronal circuits. Nat. Rev. Neurosci. 2012, 13, 687–700. [Google Scholar] [CrossRef]
- Akemann, W.; Mutoh, H.; Perron, A.; Rossier, J.; Knöpfel, T. Imaging brain electric signals with genetically targeted voltage-sensitive fluorescent proteins. Nat. Methods 2010, 7, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Bando, Y.; Grimm, C.; Cornejo, V.H.; Yuste, R. Genetic voltage indicators. BMC Biol. 2019, 17, 71. [Google Scholar] [CrossRef]
- Homola, J.; Yee, S.S.; Gauglitz, G. Surface plasmon resonance sensors: Review. Sens. Actuators B Chem. 1999, 54, 3–15. [Google Scholar] [CrossRef]
- Homola, J. Surface Plasmon Resonance Sensors for Detection of Chemical and Biological Species. Chem. Rev. 2008, 108, 462–493. [Google Scholar] [CrossRef]
- Mayer, K.M.; Hafner, J.H. Localized Surface Plasmon Resonance Sensors. Chem. Rev. 2011, 111, 3828–3857. [Google Scholar] [CrossRef]
- Zhang, J.; Atay, T.; Nurmikko, A.V. Optical Detection of Brain Cell Activity Using Plasmonic Gold Nanoparticles. Nano Lett. 2009, 9, 519–524. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.A.; Kim, S.J.; Moon, H.; Jun, S.B. In vivo optical neural recording using fiber-based surface plasmon resonance. Opt. Lett. 2012, 37, 614–616. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.V.; Wu, H.-i. Biomedical Optics: Principles and Imaging; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Gratton, G.; Sarno, A.; Maclin, E.; Corballis, P.M.; Fabiani, M. Toward Noninvasive 3-D Imaging of the Time Course of Cortical Activity: Investigation of the Depth of the Event-Related Optical Signal. NeuroImage 2000, 11, 491–504. [Google Scholar] [CrossRef]
- Yang, W.; Carrillo-Reid, L.; Bando, Y.; Peterka, D.S.; Yuste, R. Simultaneous two-photon imaging and two-photon optogenetics of cortical circuits in three dimensions. Elife 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Jacques, S.L. Optical properties of biological tissues: A review. Phys. Med. Biol. 2013, 58, R37–R61. [Google Scholar] [CrossRef]
- Cramer, S.W.; Carter, R.E.; Aronson, J.D.; Kodandaramaiah, S.B.; Ebner, T.J.; Chen, C.C. Through the looking glass: A review of cranial window technology for optical access to the brain. J. Neurosci. Methods 2021, 354, 109100. [Google Scholar] [CrossRef]
- Li, Y.; Baran, U.; Wang, R.K. Application of Thinned-Skull Cranial Window to Mouse Cerebral Blood Flow Imaging Using Optical Microangiography. PLoS ONE 2014, 9, e113658. [Google Scholar] [CrossRef]
- Wells, J.D.; Thomsen, S.; Whitaker, P.; Jansen, E.D.; Kao, C.C.; Konrad, P.E.; Mahadevan-Jansen, A. Optically mediated nerve stimulation: Identification of injury thresholds. Lasers Surg. Med. 2007, 39, 513–526. [Google Scholar] [CrossRef]
- Tirlapur, U.K.; König, K.; Peuckert, C.; Krieg, R.; Halbhuber, K.-J. Femtosecond Near-Infrared Laser Pulses Elicit Generation of Reactive Oxygen Species in Mammalian Cells Leading to Apoptosis-like Death. Exp. Cell Res. 2001, 263, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Cameron, M.; Kékesi, O.; Morley, J.W.; Tapson, J.; Breen, P.P.; van Schaik, A.; Buskila, Y. Calcium Imaging of AM Dyes Following Prolonged Incubation in Acute Neuronal Tissue. PLoS ONE 2016, 11, e0155468. [Google Scholar] [CrossRef] [PubMed]
- Bar-Noam, A.S.; Farah, N.; Shoham, S. Correction-free remotely scanned two-photon in vivo mouse retinal imaging. Light Sci. Appl. 2016, 5, e16007. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-E.; Tien, C.-H. Fundus photography with subpixel registration of correlated laser speckle images. Jpn. J. Appl. Phys. 2018, 57, 09SB01. [Google Scholar] [CrossRef]
| Method | Wavelength [nm] | Optical Intensity | Safety | Human-Application |
|---|---|---|---|---|
| Femtosecond laser Stimulation | 750–850 | ~70 mW | possible safety issue due to ROS | |
| Infrared Neural Stimulation | 1844–2120 | PNS: ~700 mJ/cm2 CNS: ~550 mJ/cm2 | possible safety issue due to thermal tissue damage | |
| Optogenetics | 400–700 | ~8–12 mW/mm2 | safe | Vision Recovery [68] |
| Photoactive Molecules Based Optical Stimulation | 355–500 | ~3.5 mW/mm2 | possible safety issue due to potential toxicity of cage | |
| Nanomaterials Based Optical Stimulation | Photothermal : 500–780 Photovoltaic : 900 | Photothermal : ~159 mJ/cm2 photovoltaic: (material dependent) -photodiode: 0.5 µW/mm2 -graphene: 2.1 mW/mm2 | safe |
| Method | Spatial Resolution | Temporal Latency | Non-Invasiveness | Robustness | Human Application |
|---|---|---|---|---|---|
| EROS | ~5 mm | ~100 ms (fast) | source and detector placed outside of skin (NIR range) | poor | Functional cortical imaging [114,196] |
| fNIRS | ~1 cm | ~1 s (slow) | source and detector placed outside of skin (NIR range) | robust | Various human application including psychology, linguistics, medical application (epilepsy, pain assessment, parkinson’s disease) |
| LDF | ~100 µm | ~1 s (slow) | requires cranial window when imaging neurovascular component (NIR range) | robust | functional imaging of brain cortex and optic nerve [146,149] |
| LSCI | ~10 µm | ~1 s (slow) | requires cranial window when imaging neurovascular component (NIR range) | robust | functional brain mapping [163] |
| Calcium Probe | ~1 µm | ~1 s (slow) | requires cranial window (Visible range) | robust | - |
| Voltage-sensitive Probe | ~1 µm | ~1 ms (fast, captures action potential) | requires cranial window (Visible range) | robust | - |
| Plasmonic Sensor | point measurement | ~1 ms (fast, captures action potential) | Invasive requiring insertion of plasmonic material placed near the neuron (NIR range) | robust | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, Y.; Park, S.-Y.; Eom, K. Current Review of Optical Neural Interfaces for Clinical Applications. Micromachines 2021, 12, 925. https://doi.org/10.3390/mi12080925
Park Y, Park S-Y, Eom K. Current Review of Optical Neural Interfaces for Clinical Applications. Micromachines. 2021; 12(8):925. https://doi.org/10.3390/mi12080925
Chicago/Turabian StylePark, Younghoon, Sung-Yun Park, and Kyungsik Eom. 2021. "Current Review of Optical Neural Interfaces for Clinical Applications" Micromachines 12, no. 8: 925. https://doi.org/10.3390/mi12080925
APA StylePark, Y., Park, S.-Y., & Eom, K. (2021). Current Review of Optical Neural Interfaces for Clinical Applications. Micromachines, 12(8), 925. https://doi.org/10.3390/mi12080925







