Emerging Designs of Electronic Devices in Biomedicine
Abstract
1. Introduction
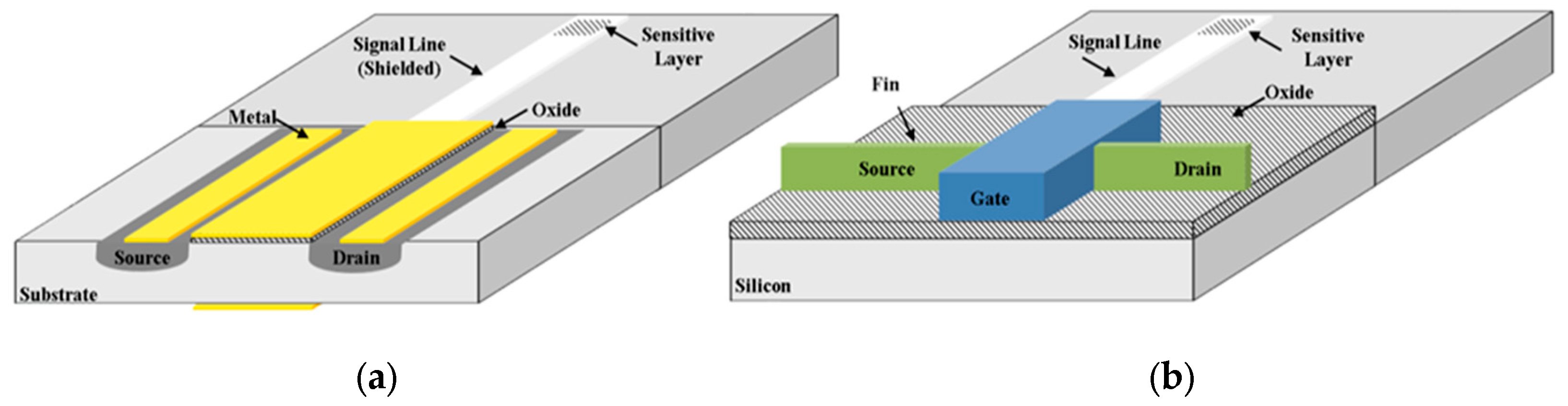
2. Fin Field-Effect Transistor (FinFET), Tunnel FET
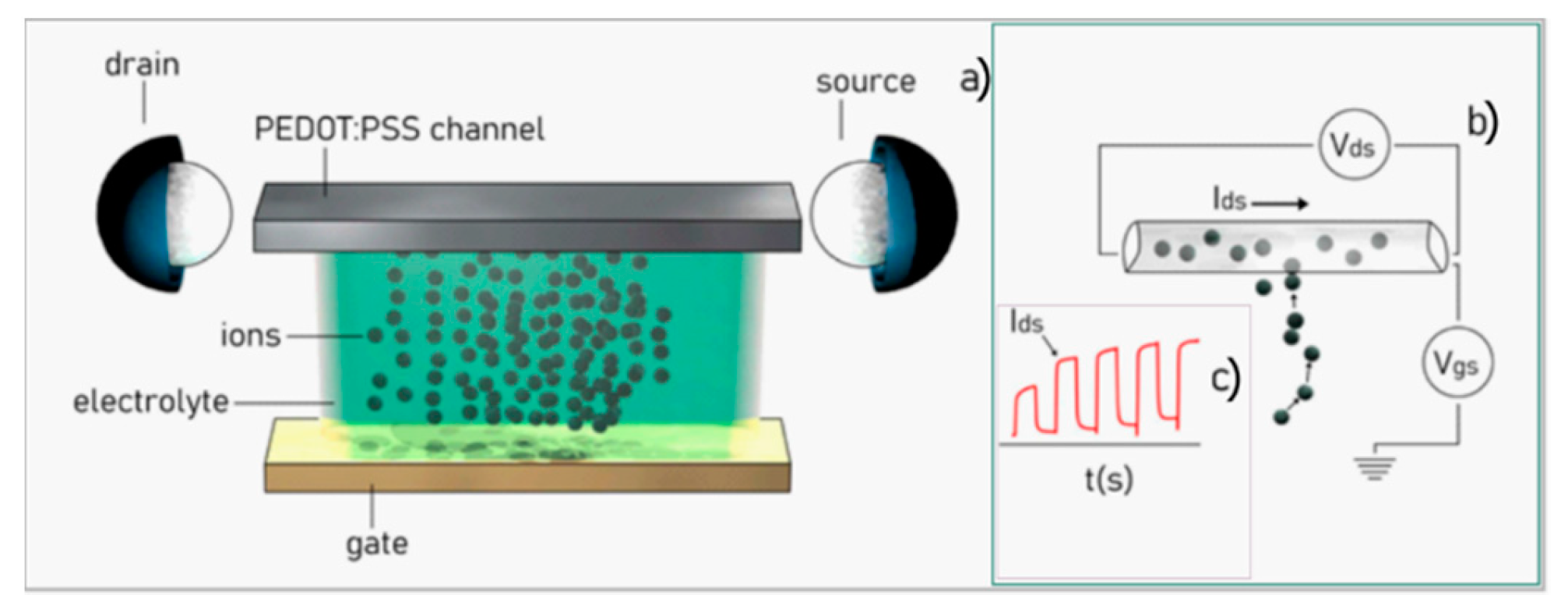
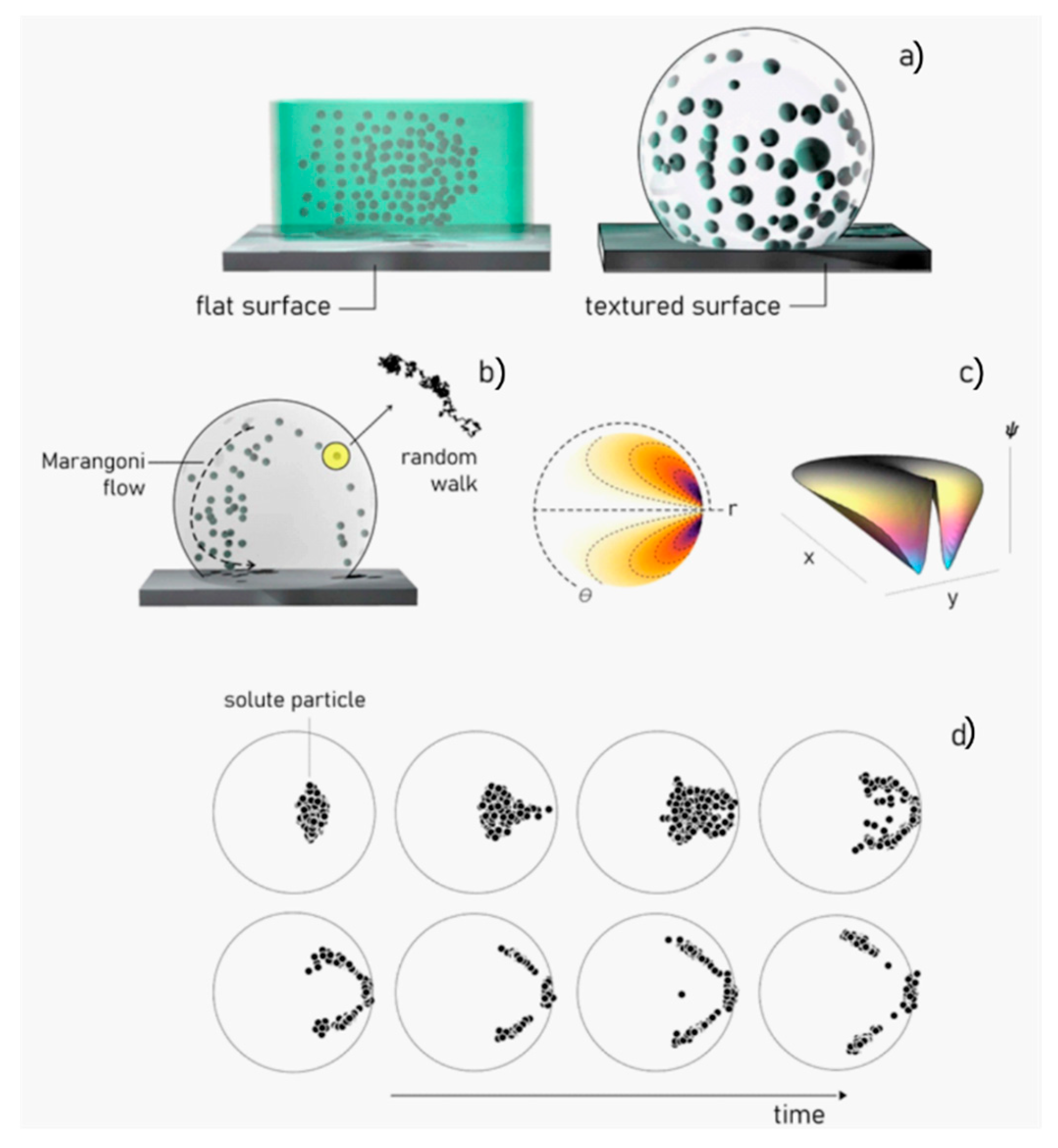
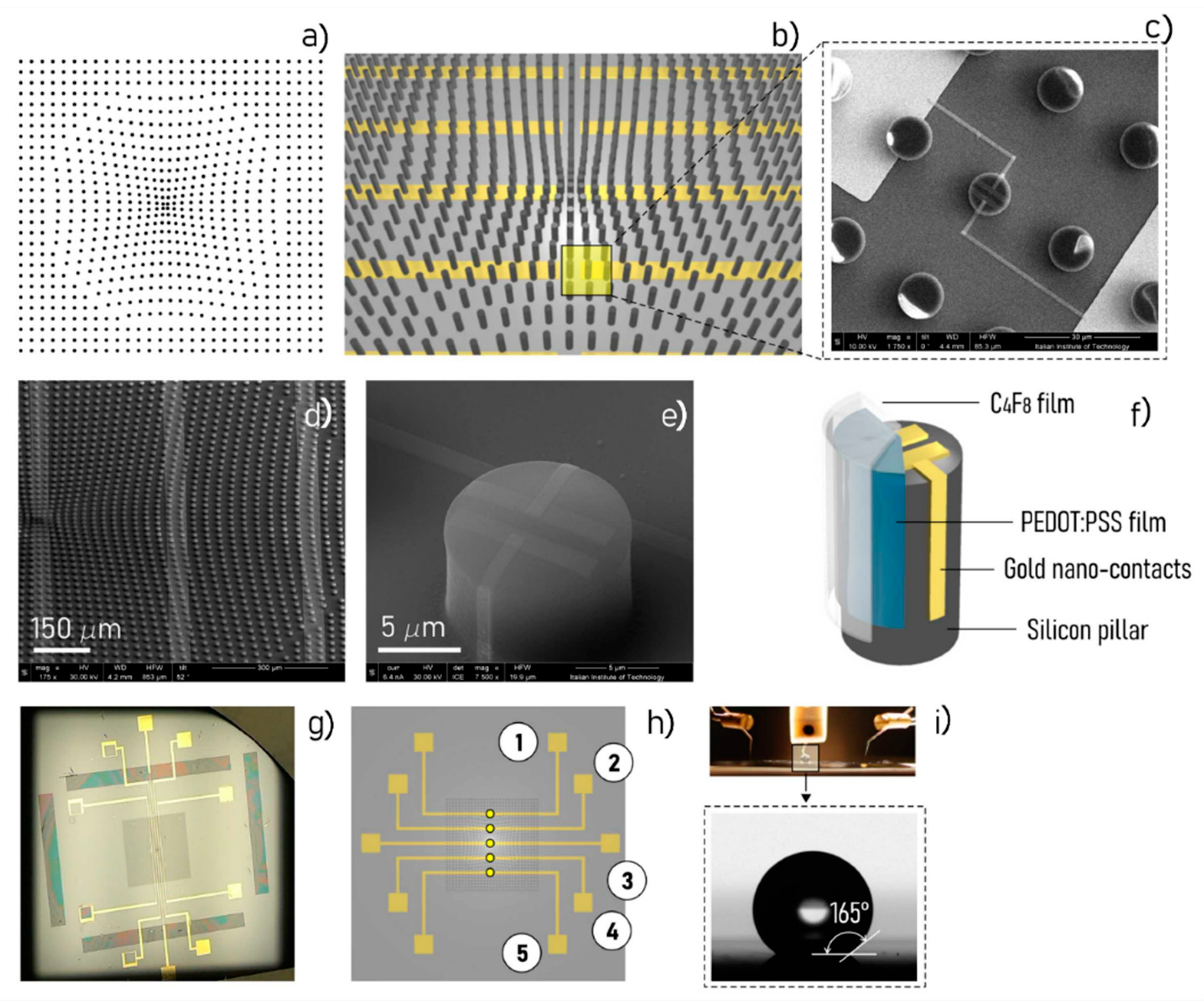
3. Organic Electrochemical Transistor Devices
4. Combined Electrochemical Biosensor and Lab-on-Chip
5. Future Trends of Combined Electrochemical Biosensor and Lab-on-Chip
6. Medical Clinical Applications
| Device | Disease | Reference |
|---|---|---|
| RNA aptamers anti HER2 | Breast cancer | [110] |
| Nanotube-wrapped anti-HER2 protein aptamers | Breast cancer | [113] |
| DNA aptamer anti ERα | Breast cancer | [114] |
| Upconversion nanoparticles DNA aptasensor for VEGF | Breast cancer | [115] |
| Electrochemical aptasensor for osteopontin | Breast cancer | [116] |
| MCF-7 aptamer-functionalized magnetic beads and quantum dots based nano-bio-probes | Breast cancer | [117] |
| G-quadruplex structured DNA aptamer against AGR-2 | Breast cancer | [118] |
| Electrochemical detection of VEGF based on Au–Pd alloy-assisted aptasensor | Lung cancer | [120] |
| Electrochemical aptasensor for VEGF | Lung cancer | [121] |
| EGFR DNA sandwich-type electrochemical biosensor | Lung cancer | [122] |
| Amperometric immunosensors for Annexin II and MUC5AC | Lung cancer | [123] |
| Amperometric sensing of HIF1α | Lung cancer | [124] |
| Amperometric sensor for NADH (nicotinamide adenine dinucleotide) using activated graphene oxide | Lung cancer | [125] |
| Volatile organic compounds (VOC) (Different methods) | GI (GastroIntestinal)-tract cancer | [126] |
| Pyruvate kinase isoenzyme type M2 (M2-PK) (Different methods) | GI-tract cancer | [127] |
| Ingestible micro-bio-electronic device (IMBED) and miniaturized luminescence readout electronics, wirelessly communicating with an external device | GI-tract cancer | [139] |
| Sarcosine (Different methods) | Colorectal, prostate, and stomach cancer; Alzheimer, dementia, sarcosinemia | [140] |
| Device | Disease | Reference |
|---|---|---|
| Isothermal nucleic acid amplification test | Influenza | [142,143] |
| Isothermal nucleic acid amplification test | Group A beta-hemolytic streptococcus | [142,144] |
| Isothermal nucleic acid amplification test | Respiratory syncytial virus | [141,145] |
| Different methods (review) | Hepatitis C | [146] |
| Different methods (review) | Trichomonas vaginalis | [147] |
| Different methods (review) | HIV | [148] |
| Different methods (review) | Urogenital Chlamydia trachomatis | [149] |
| Different methods (review) | Viral respiratory tract infections | [150] |
| Loop-mediated isothermal amplification (LAMP) | Leishmania spp | [151] |
| Gene Specific DNA Sensors | Pathogenic Infections | [152,154] |
| Different methods (review) | Antibiotic-Susceptibility Profiling | [153,154] |
| Different methods (review) | Sepsis (Lactate) | [155,156] |
| Microfluidic biochip | Sepsis (CD64) | [157,158] |
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Perozziello, G.; La Rocca, R.; Cojoc, G.; Liberale, C.; Malara, N.; Simone, G.; Candeloro, P.; Anichini, A.; Tirinato, L.; Gentile, F.; et al. Microfluidic Devices Modulate Tumor Cell Line Susceptibility to NK Cell Recognition. Small 2012, 8, 2886–2894. [Google Scholar] [CrossRef] [PubMed]
- Perozziello, G.; Simone, G.; Candeloro, P.; Gentile, F.; Malara, N.; La Rocca, R.; Coluccio, M.L.; Pullano, S.A.; Tirinato, L.; Geschke, O.; et al. A Fluidic Motherboard for Multiplexed Simultaneous. Micro and Nanosystems 2010, 2, 4. [Google Scholar] [CrossRef]
- Perozziello, G.; Catalano, R.; Francardi, M.; Rondanina, E.; Pardeo, F.; De angelis, F.; Malara, N.; Candeloro, P.; Morrone, G.; Di Fabrizio, E. A microfluidic device integrating plasmonic nanodevices for Raman spectroscopy analysis on trapped single living cells. Microel. Eng. 2013, 11, 314–319. [Google Scholar] [CrossRef]
- Simone, G.; Malara, N.; Trunzo, V.; Renne, M.; Perozziello, G.; Di Fabrizio, E.; Manz, A. Galectin-3 coats the membrane of breast cells and makes a signature of tumours. Mol. Biosyst. 2014, 10, 258–265. [Google Scholar] [CrossRef]
- Coluccio, M.L.; Gentile, F.; Das, G.; Nicastri, A.; Perri, A.M.; Candeloro, P.; Perozziello, G.; Proietti Zaccaria, R.; Gongora, J.S.; Alrasheed, S.; et al. Detection of single amino acid mutation in human breast cancer by disordered plasmonic self-similar chain. Sci. Adv. 2015, 1. [Google Scholar] [CrossRef]
- Perozziello, G.; Candeloro, P.; Gentile, F.; Nicastri, A.; Perri, A.M.; Coluccio, M.L.; Adamo, A.; Pardeo, F.; Catalano, R.; Parrotta, E. Microfluidics & nanotechnology: Towards fully integrated analytical devices for the detection of cancer biomarkers. R. Soc. Chem. RSC Adv. 2014, 4, 55590–55598. [Google Scholar]
- Malara, N.; Coluccio, M.L.; Limongi, T.; Asande, M.; Trunzo, V.; Cojoc, G.; Raso, C.; Candeloro, P.; Perozziello, G.; Raimondo, R.; et al. Folic Acid Functionalized Surface Highlights 5-Methylcytosine-Genomic Content within Circulating Tumor Cells. Small 2014, 10, 4324–4331. [Google Scholar] [CrossRef]
- Pullano, S.A.; Greco, M.; Corigliano, D.M.; Foti, D.P.; Brunetti, A.; Fiorillo, A.S. Cell-line characterization by infrared-induced pyroelectric effect. Biosens. Bioelectron. 2019, 140. [Google Scholar] [CrossRef]
- Bergveld, P. Development of an Ion–Sensitive Solid–State Device for Neurophysiological Measurements. IEEE Trans. Biomed. Eng. 1970, 17, 70–71. [Google Scholar] [CrossRef]
- Luz, R.A.S.; Rodrigo, M.; Crespilho, I.; Crespilho, F.N. Nanomaterials for Biosensors and Implantable Biodevices. In Nanobioelectrochemistry: From Implantable Biosensors to Green Power Generation; Springer: Berlin/Heidelberg, Germany, 2013; pp. 27–28. ISBN 978-3-642-29249-1. [Google Scholar]
- Van der Spiegel, J.; Lauks, I.; Chan, P.; Babic, D. The extended gate chemically sensitive field effect transistor as multi–species microprobe. Sens. Actuators 1983, 4, 291–298. [Google Scholar] [CrossRef]
- Rajan, N.K.; Brower, K.; Duan, X.; Reed, M.A. Limit of detection of field effect transistor biosensors: Effects of surface modification and size dependence. Appl. Phys. Lett. 2014, 104. [Google Scholar] [CrossRef]
- William, M.R.; Gehan, A.J.A. Silicon surface tunnel transistor. Appl. Phys. Lett. 1995, 67, 494–496. [Google Scholar]
- Hisamoto, D.; Kaga, T.; Kawamoto, Y.; Takeda, E. A fully depleted lean-channel transistor (DELTA)-a novel vertical ultra thin SOI MOSFET. In Proceedings of the International Technical Digest on Electron Devices Meeting, Washington, DC, USA, 3–6 December 1989; pp. 34.5.1–34.5.4. [Google Scholar]
- Jurczak, M.; Collaert, N.; Veloso, A.; Hoffmann, T.; Biesemans, S. Review of FINFET technology. In Proceedings of the 2009 IEEE International SOI Conference, Foster City, CA, USA, 5–8 October 2009. [Google Scholar]
- Choi, W.Y.; Lee, W. Hetero-Gate-Dielectric Tunneling Field-Effect Transistors. IEEE Trans. Electron Devices 2010, 57, 2317–2319. [Google Scholar] [CrossRef]
- Kergoat, L.; Piro, B.; Berggren, M.; Horowitz, G.; Pham, M.C. Advances in organic transistor-based biosensors: From organic electrochemical transistors to electrolyte-gated organic field-effect transistors. Anal. Bioanal. Chem. 2012, 402, 1813–1826. [Google Scholar] [CrossRef]
- Yin, L.T.; Chou, J.C.; Chung, W.Y.; Sun, T.P.; Hsiung, S.K. Study of indium tin oxide thin film for separative extended gate ISFET. Mater. Chem. Phys. 2001, 70, 12–16. [Google Scholar] [CrossRef]
- Chi, L.-L.; Chou, J.-C.; Chung, W.-Y.; Sun, T.-P.; Hsiung, S.-K. Study on extended gate field effect transistor with tin oxide sensing membrane. Mater. Chem. Phys. 2000, 63, 19–23. [Google Scholar] [CrossRef]
- Subramanian, V.; Parvais, B.; Borremans, J.; Mercha, A.; Linten, D.; Wambacq, P.; Loo, J.; Dehan, D.; Gustin, C.; Collaert, N.; et al. Planar Bulk MOSFETs Versus FinFETs: An Analog/RF Perspective. IEEE Trans. Electron Devices 2006, 53, 3071–3079. [Google Scholar] [CrossRef]
- Pullano, S.A.; Critello, C.D.; Mahbub, I.; Tasneem, N.T.; Shamsir, S.; Islam, S.K.; Greco, M.; Fiorillo, A.S. EGFET-Based Sensors for Bioanalytical Applications: A Review. Sensors 2018, 18, 4042. [Google Scholar] [CrossRef]
- Pullano, S.A.; Tasneem, N.T.; Mahbub, I.; Shamsir, S.; Greco, M.; Islam, S.K.; Fiorillo, A.S. Deep Submicron EGFET Based on Transistor Association Technique for Chemical Sensing. Sensors 2019, 19, 1063. [Google Scholar] [CrossRef]
- Ahn, J.-H.; Choi, S.-J.; Han, J.-W.; Park, T.J.; Lee, S.Y.; Choi, Y.-K. Double-Gate Nanowire Field Effect Transistor for a Biosensor. Nano Lett. 2010, 10, 2934–2938. [Google Scholar] [CrossRef]
- Sarkar, D.; Banerjee, K. Proposal for tunnel-field-effect-transistor as ultra-sensitive and label-free biosensors. Appl. Phys. Lett. 2012, 100, 143108. [Google Scholar] [CrossRef]
- Rigante, S.; Scarbolo, P.; Wipf, M.; Stoop, R.L.; Bedner, K.; Buitrago, E.; Bazigos, A.; Bouvet, D.; Calame, M.; Schönenberger, M.; et al. Sensing with Advanced Computing Technology: Fin Field-Effect Transistors with High-k Gate Stack on Bulk Silicon. ACS Nano 2015, 9, 4872–4881. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Tu, H.; Yin, H.; Wei, F.; Zhao, H.; Xue, C.; Wei, Q.; Zhang, Z.; Zhang, X.; Zhang, S.; et al. Si Nanowire Biosensors Using a FinFET Fabrication Process for Real Time Monitoring Cellular Ion Actitivies. In Proceedings of the 2018 IEEE International Electron Devices Meeting (IEDM), San Francisco, CA, USA, 1–5 December 2018. [Google Scholar]
- Rollo, S.; Rani, D.; Leturcq, R.; Olthuis, W.; Pascual Garcia, C. A high aspect ratio Fin-Ion Sensitive Field Effect Transistor: Compromises towards better electrochemical bio-sensing. Nano Lett. 2019, 19, 2879–2887. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.-H.; Kim, J.-Y.; Choi, K.; Moon, D.-I.; Kim, C.-H.; Seol, M.-L.; Park, T.J.; Lee, S.Y.; Choi, Y.-K. Nanowire FET Biosensors on a Bulk Silicon Substrate. IEEE Trans. Electron Devices 2012, 59, 2243–2249. [Google Scholar] [CrossRef]
- Chhabra, A.; Kumar, A.; Chaujar, R. Sub-20 nm GaAs Junctionless FinFET for biosensing applications. Vacuum 2019, 160, 467–471. [Google Scholar] [CrossRef]
- Ijjada, S.R.; Mannepalli, C.; Hameed Pasha, M. FinFET Modelling Using TCAD. Lect. Notes Electr. Eng. 2018, 434, 2018. [Google Scholar]
- Mao, S. Graphene Field-Effect Transistor Sensors. In Graphene Bioelectronics; Elsevier: Amsterdam, The Netherlands, 2018; pp. 113–132. [Google Scholar] [CrossRef]
- Wu, X.; Mu, F.; Wang, Y.; Zhao, H. Graphene and Graphene-Based Nanomaterials for DNA Detection: A Review. Molecules 2018, 23, 2050. [Google Scholar] [CrossRef]
- Zhan, B.; Li, C.; Yang, J.; Jenkins, G.; Huang, W.; Dong, X. Graphene Field-Effect Transistor and Its Application for Electronic Sensing. Small 2014, 10, 4042–4065. [Google Scholar] [CrossRef]
- Star, A.; Tu, E.; Niemann, J.; Gabriel, J.-C.P.; Joiner, C.S.; Valcke, C. Label-free detection of DNA hybridization using carbon nanotube network field-effect transistors. Proc. Natl. Acad. Sci. USA 2006, 103, 921–926. [Google Scholar] [CrossRef]
- Fiorillo, A.S.; Tiriolo, R.; Pullano, S.A. Absorption of Urea into zeolite layer integrated with microelectronic circuits. IEEE Trans. Nanotechnol. 2015, 14, 2015. [Google Scholar] [CrossRef]
- Fiorillo, A.S.; Vinko, J.D.; Accattato, F.; Bianco, M.G.; Critello, C.D.; Pullano, S.A. Zeolite-Based Interfaces for CB Sensors. In Nanostructured Materials for the Detection of CBRN. NATO Science for Peace and Security Series A: Chemistry and Biology; Bonča, J., Kruchinin, S., Eds.; Springer: Dordrecht, The Netherlands, 2018. [Google Scholar]
- Fiorillo, A.S.; Pullano, S.A.; Tiriolo, R.; Vinko, J.D. Iono-Electronic Interface Based on Innovative Low Temperature Zeolite Coated NMOS (Circuits) for Bio-Nanosensor Manufacture, on Nanomaterials for Security. In NATO Science for Peace and Security Series A: Chemistry and Biology; Springer: Dordrecht, The Netherlands, 2016. [Google Scholar]
- Fiorillo, A.S. Deposition of zeolite thin layer onto silicon wafers for biomedical use. IEEE Trans. Nanotechnol. 2012, 11, 654–656. [Google Scholar] [CrossRef]
- Heerema, S.J.; Schneider, G.F.; Rozemuller, M.; Vicarelli, L.; Zandbergen, H.W.; Dekker, C. 1/f noise in graphene nanopores. Nanotechnology 2015, 26. [Google Scholar] [CrossRef]
- Cristobal, P.A.; Vilela, P.; Sagheer, A.E.; Cabarcos, E.L.; Brown, T.; Muskens, O.L.; Retama, J.R.; Kanaras, A.G. Highly Sensitive DNA Sensor Based on Upconversion Nanoparticles and Graphene Oxide. ACS Appl. Mater. Interfaces 2015, 7, 12422–12429. [Google Scholar] [CrossRef]
- Lin, L.; Liu, Y.; Tang, L.; Li, J. Electrochemical DNA sensor by the assembly of graphene and DNA-conjugated gold nanoparticles with silver enhancement strategy. Analyst 2011, 136, 4732–4737. [Google Scholar] [CrossRef]
- Patel, H.N.; Carroll, I.; Lopez, R., Jr.; Sankararaman, S.; Etienne, C.; Kodigala, S.R.; Paul, M.R.; Postma, H.W.C. DNA-graphene interactions during translocation through nanogaps. PLoS ONE 2017, 12. [Google Scholar] [CrossRef]
- Merchant, C.A.; Healy, K.; Wanunu, M.; Ray, V.; Peterman, N.; Bartel, J.; Fischbein, M.D.; Venta, K.; Luo, Z.; Johnson, A.T.C.; et al. DNA Translocation through Graphene Nanopores. Nano Lett. 2010, 10, 2915–2921. [Google Scholar] [CrossRef]
- Kim, D.H.; Oh, H.G.; Park, W.H.; Jeon, D.C.; Lim, K.M.; Kim, H.J.; Jang, B.K.; Song, K.S. Detection of Alpha-Fetoprotein in Hepatocellular Carcinoma Patient Plasma with Graphene Field-Effect Transistor. Sensors 2018, 18, 4032. [Google Scholar] [CrossRef]
- Khodagholy, D.; Doublet, T.; Quilichini, P.; Gurfinkel, M.; Leleux, P.; Ghestem, A.; Ismailova, E.; Hervé, T.; Sanaur, S.; Bernard, C.; et al. In vivo recordings of brain activity using organic transistors. Nat. Commun. 2013, 4, 1–7. [Google Scholar] [CrossRef]
- Dimitrakopoulos, C.D.; Malenfant, P.R.L. Organic Thin Film Transistors for Large Area Electronics. Adv. Mater. 2002, 14, 99–117. [Google Scholar] [CrossRef]
- Tarabella, G.; Santato, C.; Yoon Yang, S.; Iannotta, S.; Malliaras, G.G.; Cicoira, F. Effect of the gate electrode on the response of organic electrochemical transistors. Appl. Phys. Lett. 2010, 97. [Google Scholar] [CrossRef]
- Yang, S.Y.; Cicoira, F.; Byrne, R.; Benito-Lopez, F.; Diamond, D.; Owens, R.M.; Malliaras, G.G. Electrochemical transistors with ionic liquids for enzymatic sensing. Chem. Commun. 2010, 46, 7972–7974. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.; Luo, X.T.; Hsing, I.M.; Yan, F. Organic Electrochemical Transistors Integrated in Flexible Microfluidic Systems and Used for Label-Free DNA Sensing. Adv. Mater. 2011, 23, 4035–4040. [Google Scholar] [CrossRef] [PubMed]
- Persson, K.M.; Karlsson, R.; Svennersten, K.; Löffler, S.; Jager, E.W.H.; Richter-Dahlfors, A.; Konradsson, P.; Berggren, M. Electronic control of cell detachment using a self-doped conducting polymer. Adv. Mater. 2011, 23, 4403–4408. [Google Scholar] [CrossRef] [PubMed]
- Tarabella, G.; D’Angelo, P.; Cifarelli, A.; Dimonte, A.; Romeo, A.; Berzina, T.; Erokhina, V.; Iannotta, S. A hybrid living/organic electrochemical transistor based on the Physarum polycephalum cell endowed with both sensing and memristive properties. Chem. Sci. 2015, 6, 2859–2868. [Google Scholar] [CrossRef] [PubMed]
- Gkoupidenis, P.; Koutsouras, D.A.; Malliaras, G.G. Neuromorphic device architectures with global connectivity through electrolyte gating. Nat. Commun. 2017, 8, 1–8. [Google Scholar] [CrossRef]
- Gkoupidenis, P.; Schaefer, N.; Garlan, B.; Malliaras, G.G. Neuromorphic Functions in PEDOT: PSS Organic Electrochemical Transistors. Adv. Mater. 2015, 27, 7176–7180. [Google Scholar] [CrossRef]
- Van De Burgt, Y.; Melianas, A.; Keene, S.T.; Malliaras, G.; Salleo, A. Organic electronics for neuromorphic computing. Nat. Electron. 2018, 1, 386–397. [Google Scholar] [CrossRef]
- Stavrinidou, E.; Gabrielsson, R.; Gomez, E.; Crispin, X.; Nilsson, O.; Simon, D.T.; Berggren, M. Electronic plants. Sci. Adv. 2015, 1. [Google Scholar] [CrossRef]
- Yeung, S.Y.; Gu, X.; Tasng, C.M.; Tsao, S.W.; Hsing, I.-M. Engineering organic electrochemical transistor (OECT) to be sensitive cell-based biosensor through tuning of channel area. Sens. Actuators A Phys. 2019, 287, 185–193. [Google Scholar] [CrossRef]
- Zhu, Z.T.; Mabeck, J.T.; Zhu, C.; Cady, N.C.; Batt, C.A.; Malliaras, G.G. A simple poly (3,4-ethylene dioxythiophene)/poly(styrene sulfonic acid) transistor for glucose sensing at neutral pH. Chem. Commun. 2004, 1556–1557. [Google Scholar] [CrossRef]
- Lin, P.; Yan, F.; Chan, H.L.W. Ion-Sensitive Properties of Organic Electrochemical Transistors. ACS Appl. Mater. Interfaces 2010, 2, 1637–1641. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-M.; Kim, C.-H.; Kim, Y.; Kim, N.; Lee, W.-J.; Lee, E.-H.; Kim, D.; Park, S.; Lee, K.; Rivnay, J.; et al. Influence of PEDOT:PSS crystallinity and composition on electrochemical transistor performance and long-term stability. Nat. Commun. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Spyropoulos, G.D.; Gelinas, J.N.; Khodagholy, D. Internal ion-gated organic electrochemical transistor: A building block for integrated bioelectronics. Sci. Adv. 2019, 5. [Google Scholar] [CrossRef] [PubMed]
- Hempel, F.; Law, J.; Susloparova, A.; Pachauri, V.; Ingebrandt, S. PEDOT: PSS Organic Electrochemical Transistors for Cell Sensing Applications. Front. Neurosci. 2016, 10. [Google Scholar] [CrossRef]
- Bai, L.; García Elósegui, C.; Li, W.; Yu, P.; Fei, J.; Mao, L. Biological Applications of Organic Electrochemical Transistors: Electrochemical Biosensors and Electrophysiology Recording. Front. Chem. 2019, 7, 313. [Google Scholar] [CrossRef]
- Macaya, D.J.; Nikolou, M.; Takamatsu, S.; Mabeck, J.T.; Owens, R.M.; Malliaras, G.G. Simple glucose sensors with micromolar sensitivity based on organic electrochemical transistors. Sens. Actuator B Chem. 2007, 123, 374–378. [Google Scholar] [CrossRef]
- Hamedi, M.; Forchheimer, R.; Inganas, O. Towards woven logic from organic electronic fibres. Nat. Mater. 2007, 6, 357–362. [Google Scholar] [CrossRef]
- Bernards, D.A.; Macaya, D.J.; Nikolou, M.; DeFranco, J.A.; Takamatsu, S.; Malliaras, G.G. Enzymatic sensing with organic electrochemical transistors. J. Mater. Chem. 2008, 18, 116. [Google Scholar] [CrossRef]
- Lin, P.; Yan, F.; Yu, J.; Chan, H.L.W.; Yang, M. The application of organic electrochemical transistors in cell-based biosensors. Adv. Mater. 2010, 22, 3655–3660. [Google Scholar] [CrossRef]
- Kim, D.J.; Lee, N.E.; Park, J.S.; Park, I.J.; Kim, J.G.; Cho, H.J. Organic electrochemical transistor based immunosensor for prostate specific antigen (PSA) detection using gold nanoparticles for signal amplification. Biosens. Bioelectron. 2010, 25, 2477–2482. [Google Scholar] [CrossRef]
- Coppedè, N.; Villani, M.; Gentile, F. Diffusion Driven Selectivity in Organic Electrochemical Transistors. Sci. Rep. 2014, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gentile, F.; Ferrara, L.; Villani, M.; Bettelli, M.; Iannotta, S.; Zappettini, A.; Cesarelli, M.; Di Fabrizio, E.; Coppedè, N. Geometrical Patterning of Super-Hydrophobic Biosensing Transistors Enables Space and Time Resolved Analysis of Biological Mixtures. Sci. Rep. 2016, 6, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Tam, D.; von Arnim, V.; McKinley, G.H.; Hosoi, A.E. Marangoni convection in droplets on superhydrophobic surfaces. J. Fluid Mech. 2009, 624, 101–123. [Google Scholar] [CrossRef]
- Astier, Y.; Data, L.; Carney, R.P.; Stellacci, F.; Gentile, F.; Di Fabrizio, E. Artificial Surface-Modified Si3N4 Nanopores for Single Surface-Modified Gold Nanoparticle Scanning. Small 2010, 7, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-M.; Zydney, A.L. Effect of electrostatic, hydrodynamic, and Brownian forces on particle trajectories and sieving in normal flow filtration. J. Colloid Interface Sci. 2004, 269, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Gentile, F.; Coluccio, M.L.; Zaccaria, R.P.; Francardi, M.; Cojoc, G.; Perozziello, G.; Raimondo, R.; Candeloroa, P.; Fabrizio, E.D. Selective on site separation and detection of molecules in diluted solutions with superhydrophobic clusters of plasmonic nanoparticles. Nanoscale 2014, 6, 8208–8225. [Google Scholar] [CrossRef] [PubMed]
- Lafuma, A.; Quéré, D. Superhydrophobic states. Nat. Mater. 2003, 2, 457–460. [Google Scholar] [CrossRef]
- Ueda, E.; Levkin, P.A. Emerging Applications of Superhydrophilic-Superhydrophobic Micropatterns. Adv. Mater. 2013, 25, 1234–1247. [Google Scholar] [CrossRef]
- Hoshian, S.; Jokinen, V.; Somerkivi, V.; Lokanathan, A.R.; Franssila, S. Robust Superhydrophobic Silicon without a Low Surface-Energy Hydrophobic Coating. ACS Appl. Mater. Interfaces 2015, 7, 941–949. [Google Scholar] [CrossRef]
- He, Y.; Jiang, C.; Yin, H.; Yuan, W. Tailoring the wettability of patterned silicon surfaces with dual-scale pillars: From hydrophilicity to superhydrophobicity. Appl. Surf. Sci. 2011, 257, 7689–7692. [Google Scholar] [CrossRef]
- Xiu, Y.; Zhu, L.; Dennis, W.; Hess, C.; Wong, P. Hierarchical Silicon Etched Structures for Controlled Hydrophobicity/Superhydrophobicity. Nano Lett. 2007, 7, 3388–3393. [Google Scholar] [CrossRef] [PubMed]
- Falde, E.J.; Yohe, S.T.; Colson, Y.L.; Grinstaff, M.W. Superhydrophobic materials for biomedical applications. Biomaterials 2016, 104, 87–103. [Google Scholar] [CrossRef] [PubMed]
- Gentile, F.; Battista, E.; Accardo, A.; Coluccio, M.; Asande, M.; Perozziello, G.; Das, G.; Liberale, C.; De Angelis, F.; Candeloro, P.; et al. Fractal Structure Can Explain the Increased Hydrophobicity of NanoPorous Silicon Films. Microelectron. Eng. 2011, 88, 2537–2540. [Google Scholar] [CrossRef]
- Bartolo, D.; Bouamrirene, F.; Verneuil, É.; Buguin, A.; Silberzan, P.; Moulinet, S. Bouncing or sticky droplets: Impalement transitions on superhydrophobic micropatterned surfaces. Europhys. Lett. 2006, 74, 2. [Google Scholar] [CrossRef]
- Gentile, F.; Coppedè, N.; Tarabella, G.; Villani, M.; Calestani, D.; Candeloro, P.; Iannotta, S.; Di Fabrizio, E. Microtexturing of the Conductive PEDOT:PSS Polymer for Superhydrophobic Organic Electrochemical Transistors. BioMed. Res. Int. 2014, 1–10. [Google Scholar] [CrossRef]
- Malara, N.; Gentile, F.; Coppedè, N.; Coluccio, M.L.; Candeloro, P.; Perozziello, G.; Ferrara, L.; Giannetto, M.; Careri, M.; Castellini, A.; et al. Superhydrophobic lab-on-chip measures secretome protonation state and provides a personalized risk assessment of sporadic tumour. NPJ Precis. Oncol. 2018, 2. [Google Scholar] [CrossRef]
- Farzin, L.; Shamsipur, M. Recent advances in design of electrochemical affinity biosensors for low level detection of cancer protein biomarkers using nanomaterial-assisted signal enhancement strategies. J. Pharmac. Biomed. Anal. 2018, 147, 185–210. [Google Scholar] [CrossRef]
- Lim, S.A.; Ahmed, A.U. Electrochemical immunosensors and their recent nanomaterial-based signal amplification strategies: A review. RSC Adv. 2016, 6, 24995–25014. [Google Scholar] [CrossRef]
- Xia, Y.Y.; Si, J.; Li, Z.Y. Fabrication techniques for microfluidic paper-based analytical devices and their applications for biological testing: A review. Biosens. Bioelectron. 2016, 77, 774–789. [Google Scholar] [CrossRef]
- Balu, B.; Berry, A.D.; Hess, D.W.; Breedveld, V. Patterning of superhydrophobic paper to control the mobility of micro-liter drops for two-dimensional lab-on-paper applications. Lab Chip 2009, 9, 3066–3075. [Google Scholar] [CrossRef]
- Kauffman, P.; Fu, E.; Lutz, B.; Yager, P. Visualization and measurement of flow in two-dimensional paper networks. Lab Chip 2010, 10, 2614–2617. [Google Scholar] [CrossRef] [PubMed]
- Kalisha, B.; Tsutsui, H. Patterned adhesive enables construction of nonplanar three-dimensional paper microfluidic circuits. Lab Chip 2014, 14, 4354–4361. [Google Scholar] [CrossRef] [PubMed]
- Mosadegh, B.; Dabiri, B.E.; Lockett, M.R.; Derda, R.; Campbell, P.; Parker, K.K.; Whitesides, G.M. Three-dimensional paper-based model for cardiac ischemia. Adv. Healthc. Mater. 2014, 3, 1036–1043. [Google Scholar] [CrossRef]
- Li, X.; Tian, J.; Garnier, G.; Shen, W. Fabrication of paper-based microfluidic sensors by printing. Surf. B 2010, 76, 564–570. [Google Scholar] [CrossRef]
- He, Y.; Wu, Y.; Xiao, X.; Fu, J.Z.; Xue, G.H. A low-cost and rapid microfluidic paper-based analytical device fabrication method: Flash foam stamp lithography. RSC Adv. 2014, 4, 63860–63865. [Google Scholar] [CrossRef]
- Olkkonen, J.; Lehtinen, K.; Erho, T. Flexographically Printed Fluidic Structures in Paper. Anal. Chem. 2010, 82, 10246–10250. [Google Scholar] [CrossRef]
- Yan, C.F.; Yu, S.Y.; Jiang, Y.; He, Q.H.; Chen, H.W. Fabrication of Paper-based Microfluidic Devices by Plasma Treatment and Its Application in Glucose Determination. Acta Chim. Sin. 2014, 72, 1099–1104. [Google Scholar] [CrossRef]
- Sones, C.L.; Katis, I.N.; He, P.J.W.; Mills, B.; Namiq, M.F.; Shardlow, P.; Ibsen, M.; Eason, R.W. Laser-induced photo-polymerisation for creation of paper-based fluidic devices. Lab Chip 2014, 14, 4567–4574. [Google Scholar] [CrossRef]
- Cai, L.; Xu, C.; Lin, S.; Luo, J.; Wu, M.; Yang, F. A simple paper-based sensor fabricated by selective wet etching of silanized filter paper using a paper mask. Biomicrofluidics 2014, 8, 5. [Google Scholar] [CrossRef]
- Renault, C.; Scida, K.; Knust, K.N.; Fosdick, S.E.; Crooks, R.M. Paper-Based Bipolar Electrochemistry. J. Electrochem. Sci. Tech. 2013, 4, 146–152. [Google Scholar] [CrossRef]
- Dungchai, W.; Chailapakul, O.; Henry Analyst, C.S. A low-cost, simple, and rapid fabrication method for paper-based microfluidics using wax screen-printing. Analyst 2011, 136, 77–82. [Google Scholar] [CrossRef]
- Liang, L.L.; Su, M.; Li, L.; Lan, F.F.; Yang, G.X.; Ge, S.G.; Yu, J.H.; Song, X.R. Aptamer-based fluorescent and visual biosensor for multiplexed monitoring of cancer cells in microfluidic paper-based analytical devices. Sens. Actuator B Chem. 2016, 229, 347–354. [Google Scholar] [CrossRef]
- Rattanarat, P.; Dungchai, W.; Cate, D.; Volckens, J.; Chailapakul, O.; Henry, C.S. Multilayer paper-based device for colorimetric and electrochemical quantification of metals. Anal. Chem. 2014, 86, 3555–3562. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Ruiz, N.; Curto, V.F.; Erenas, M.M.; Benito-Lopez, F.; Diamond, D.; Palma, A.J.; Capitan-Vallvey, L.F. Smartphone-based simultaneous pH and nitrite colorimetric determination for paper microfluidic devices. Anal. Chem. 2014, 86, 9554–9562. [Google Scholar] [CrossRef] [PubMed]
- Bonapace, G.; Marasco, O.; Scozzafava, G.; Michael, A.; Pittelli, M.; Greto, T.; Moricca, M.T.; Vismara, S.A.; Valentini, A.; Vismara, M.F.M.; et al. GP15 Phenylalanine measurements in human blood using NIR spectroscopy and DBS, a preliminary study. Arch. Dis. Child. 2019, 104, A35–A36. [Google Scholar]
- Moral-Munoz, J.A.; Zhang, W.; Cobo, M.J.; Herrera-Viedma, E.; Kaber, D.B. Smartphone-based systems for physical rehabilitation applications: A systematic review. Assist. Technol. 2019, 1–14. [Google Scholar] [CrossRef]
- Nussbaum, Y.; Kelly, C.; Quinby, E.; Mac, A.; Parmanto, B.; Dicianno, B.E. Systematic Review of Mobile Health Applications in Rehabilitation. Arch. Phys. Med. Rehabil. 2019, 100, 115–127. [Google Scholar] [CrossRef]
- Ruzycka, M.; Cimpan, M.R.; Rios-Mondragon, I.; Grudzinski, I.P. Microfluidics for studying metastatic patterns of lung cancer. J. Nanobiotechnol. 2019, 17, 71. [Google Scholar] [CrossRef]
- Mohammadniaei, M.; Nguyen, H.V.; Tieu, M.V.; Lee, M.H. 2D Materials in Development of Electrochemical Point-of-Care Cancer Screening Devices. Micromachines (Basel) 2019, 10, 662. [Google Scholar] [CrossRef]
- Mohammadniaei, M.; Park, C.; Min, J.; Sohn, H.; Lee, T. Fabrication of Electrochemical-Based Bioelectronic Device and Biosensor Composed of Biomaterial-Nanomaterial Hybrid. In Biomimetic Medical Materials: From Nanotechnology to 3D Bioprinting; Noh, I., Ed.; Springer: Singapore, 2018; pp. 263–296. [Google Scholar]
- Sajid, M.; Kawde, A.-N.; Daud, M. Designs, formats and applications of lateral flow assay: A literature review. J. Saudi Chem. Soc. 2015, 19, 689–705. [Google Scholar] [CrossRef]
- Sher, M.; Zhuang, R.; Demirci, U.; Asghar, W. Paper-based analytical devices for clinical diagnosis: Recent advances in the fabrication techniques and sensing mechanisms. Expert. Rev. Mol. Diagn. 2017, 17, 351–366. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.H.; Elsherbiny, M.E.; Emara, M. Updates on Aptamer Research. Int. J. Mol. Sci. 2019, 20, 2511. [Google Scholar] [CrossRef] [PubMed]
- Bukari, B.A.; Citartan, M.; Ch’ng, E.S.; Bilibana, M.P.; Rozhdestvensky, T.; Tang, T.H. Aptahistochemistry in diagnostic pathology: Technical scrutiny and feasibility. Histochem. Cell Biol. 2017, 147, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Huh, H.Y.; Kim, S.; Lee, D. Isolation of rna aptamers targeting HER-2-overexpressing breast cancer cells using cell-SELEX. Bull. Korean Chem. Soc. 2009, 30, 1827–1831. [Google Scholar] [CrossRef]
- Niazi, J.; Verma, S.; Niazi, S.; Qureshi, A. In vitro HER2 protein-induced affinity dissociation of carbon nanotube-wrapped anti-HER2 aptamers for HER2 protein detection. Analyst 2013, 140, 243–249. [Google Scholar] [CrossRef]
- Ahirwar, R.; Vellarikkal, S.K.; Sett, A.; Sivasubbu, S.; Scaria, V.; Bora, U.; Borthakur, B.B.; Kataki, A.C.; Sharma, J.D.; Nahar, P. Aptamer-assisted detection of the altered expression of estrogen receptor alpha in human breast cancer. PLoS ONE 2016, 11. [Google Scholar] [CrossRef]
- Lan, J.; Li, L.; Liu, Y.; Yan, L.; Li, C.; Chen, J.; Chen, X. Upconversion luminescence assay for the detection of the vascular endothelial growth factor, a biomarker for breast cancer. Microchim. Acta. 2016, 183, 3201–3208. [Google Scholar] [CrossRef]
- Meirinho, S.G.; Dias, L.G.; Peres, A.M.; Rodrigues, L.R. Development of an electrochemical aptasensor for the detection of human osteopontin. Procedia Eng. 2014, 87, 316–319. [Google Scholar] [CrossRef]
- Hua, X.; Zhou, Z.; Yuan, L.; Liu, S. Selective collection and detection of MCF-7 breast cancer cells using aptamer-functionalized magnetic beads and quantum dots based nano-bio-probes. Anal. Chim. Acta. 2013, 788, 135–140. [Google Scholar] [CrossRef]
- Wu, J.; Wang, C.; Li, X.; Song, Y.; Wang, W.; Li, C.; Hu, J.; Zhu, Z.; Li, J.; Zhang, W.; et al. Identification, characterization and application of a G-quadruplex structured DNA aptamer against cancer biomarker protein anterior gradient homolog 2. PLoS ONE 2012, 7, e46393. [Google Scholar] [CrossRef]
- Roointan, A.; Ahmad Mir, T.; Ibrahim Wani, S.; Mati-Ur-Rehman Hussain, K.K.; Ahmed, B.; Abrahim, S.; Savardashtaki, A.; Gandomani, G.; Gandomani, M.; Chinnappan, R.; et al. Early detection of lung cancer biomarkers through biosensor technology: A review. J. Pharm. Biomed. Anal. 2019, 164, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Qin, B.; Sun, Y.; Li, J. Electrochemical Detection of VEGF165 Lung Cancer Marker Based on Au-Pd Alloy Assisted Aptasenor. Int. J. Electrochem. Sci. 2017, 12, 1818–1828. [Google Scholar] [CrossRef]
- Tabrizi, M.A.; Shamsipur, M.; Farzin, L. A high sensitive electrochemical aptasensor for the determination of VEGF 165 in serum of lung cancer patient. Biosens. Bioelectron. 2015, 74, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.-W.; Weng, X.-H.; Wang, C.-L.; Lin, W.-W.; Liu, A.-L.; Chen, W.; Lin, X.-H. Detection EGFR exon 19 status of lung cancer patients by DNA electrochemical biosensor. Biosens. Bioelectron. 2016, 80, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-M.; Noh, H.-B.; Park, D.S.; Ryu, S.-H.; Koo, J.S.; Shim, Y.-B. Immunosensors for detection of Annexin II and MUC5AC for early diagnosis of lung cancer. Biosens. Bioelectron 2009, 25, 456–462. [Google Scholar] [CrossRef]
- Hussain, K.K.; Gurudatt, N.; Mir, T.A.; Shim, Y.-B. Amperometric sensing of HIF1α expressed in cancer cells and the effect of hypoxic mimicking agents. Biosens. Bioelectron 2016, 83, 312–318. [Google Scholar] [CrossRef]
- Akhtar, M.H.; Mir, T.A.; Gurudatt, N.; Chung, S.; Shim, Y.-B. Sensitive NADH detection in a tumorigenic cell line using a nano-biosensor based on the organic complex formation. Biosens. Bioelectron 2016, 85, 488–495. [Google Scholar] [CrossRef]
- Kościelniak-Merak, B.; Radosavljević, B.; Zając, A.; Tomasik, P.J. Faecal Occult Blood Point-of-Care Tests. J. Gastrointest. Cancer 2018, 49, 402–405. [Google Scholar] [CrossRef]
- Huddy, J.R.; Ni, M.Z.; Markar, S.R.; Hanna, G.B. Point-of-care testing in the diagnosis of gastrointestinal cancers: Current technology and future directions. World J. Gastroenterol. 2015, 21, 4111–4120. [Google Scholar] [CrossRef]
- Tinmouth, J.; Lansdorp-Vogelaar, I.; Allison, J.E. Faecal immunochemical tests versus guaiac faecal occult blood tests: What clinicians and colorectal cancer screening programme organisers need to know. Gut 2015, 64, 1327–1337. [Google Scholar] [CrossRef]
- Faivre, J.; Dancourt, V.; Lejeune, C. Screening for colorectal cancer with immunochemical faecal occult blood tests. Dig. Liver Dis. 2012, 44, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Li, Q.; Ge, W.; Cai, S.; Zhang, S.; Zheng, S. Predictive power of quantitative and qualitative fecal immunochemical tests for hemoglobin in population screening for colorectal neoplasm. Eur. J. Cancer Prev. 2014, 23, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Leontiadis, G.I. Fecal immunochemical tests in patients at increased risk for colorectal cancer-is it prime time yet? JAMA Intern. Med. 2017, 177, 1119–1120. [Google Scholar] [CrossRef] [PubMed]
- Imperiale, T.; Ransohoff, D.F.; Itzkowitz, S.H.; Turnbull, B.A.; Ross, M.E.; Colorectal Cancer Study Group. Fecal DNA versus fecal occult blood for colorectal cancer screening in an average-risk population. N. Engl. J. Med. 2004, 351, 2704–2714. [Google Scholar] [CrossRef] [PubMed]
- Imperiale, T.F.; Ransohoff, D.F.; Itzkowitz, S.H.; Levin, T.R.; Lavin, P.; Lidgard, G.P.; Ahlquist, D.A.; Berger, B.M. Multitarget stool DNA testing for colorectal-cancer screening. N. Engl. J. Med. 2014, 370, 1287–1297. [Google Scholar] [CrossRef] [PubMed]
- Ahlquist, D.A.; Zou, H.; Domanico, M.; Mahoney, D.W.; Yab, T.C.; Taylor, W.R.; Butz, M.L.; Thibodeau, S.N.; Rabeneck, L.; Paszat, L.F.; et al. Next-generation stool DNA test accurately detects colorectal cancer and large adenomas. Gastroenterology 2012, 142, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Mignogna, C.; Staropoli, N.; Botta, C.; De Marco, C.; Rizzuto, A.; Morelli, M.; Di Cello, A.; Franco, R.; Camastra, C.; Presta, I.; et al. Aurora Kinase A expression predicts platinum-resistance and adverse outcome in high-grade serous ovarian carcinoma patients. J. Ovarian Res. 2016, 9, 31. [Google Scholar] [CrossRef]
- Frossard, J.L.; Peyer, R. Fecal DNA for colorectal cancer screening. N. Engl. J. Med. 2005, 352, 1384–1385. [Google Scholar]
- Church, T.R.; Wandell, M.; Lofton-Day, C.; Mongin, S.J.; Burger, M.; Payne, S.R.; Castaños-Vélez, E.; Blumenstein, B.A.; Rösch, T.; Osborn, N.; et al. Prospective evaluation of methylated SEPT9 in plasma for detection of asymptomatic colorectal cancer. Gut 2014, 63, 317–325. [Google Scholar] [CrossRef]
- Ren, A.; Dong, Y.; Tsoi, H.; Yu, J. Detection of miRNA as non-invasive biomarkers of colorectal cancer. Int. J. Mol. Sci. 2015, 16, 2810–2823. [Google Scholar] [CrossRef]
- Mark, M.; Phillip, N.; Alison, H.; Sean, C.; Sarah, F.; Logan, J.; Joy, C.; Shane, M.; Richard, S.; Citorik Robert, J.; et al. An ingestible bacterial-electronic system to monitor gastrointestinal health. Science 2018, 360, 915–918. [Google Scholar] [CrossRef]
- Pundir, C.S.; Deswal, R.; Yadav, P. Quantitative analysis of sarcosine with special emphasis on biosensors: A review. Biomarkers 2019, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Kozel, T.R.; Burnham-Marusich, A.R. Point-of-Care Testing for Infectious Diseases: Past, Present, and Future. J. Clin. Microbiol. 2017, 55, 2313–2320. [Google Scholar] [CrossRef]
- Zanoli, L.M.; Spoto, G. Isothermal Amplification Methods for the Detection of Nucleic1 Acids in Microfluidic Devices. Biosensors 2013, 3, 18–43. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.; Bonner, A.; Cohen, D.M.; Birkhahn, R.; Yogev, R.; Triner, W.; Cohen, J.; Palavecino, E.; Selvarangan, R. Multicenter clinical evaluation of the novel Alere i Influenza A&B isothermal nucleic acid amplification test. J. Clin. Virol. 2014, 61, 81–86. [Google Scholar] [PubMed]
- Cohen, D.M.; Russo, M.E.; Jaggi, P.; Kline, J.; Gluckman, W.; Parekh, A. Multicenter clinical evaluation of the novel Alere i Strep A isothermal nucleic acid amplification test. J. Clin. Microbiol. 2015, 53, 2258–2261. [Google Scholar] [CrossRef]
- Hassan, F.; Hays, L.M.; Bonner, A.; Bradford, B.J.; Franklin, R., Jr.; Hendry, P.; Kaminetsky, J.; Vaughn, M.; Cieslak, K.; Moffatt, M.E.; et al. Multicenter Clinical Evaluation of the Alere i Respiratory Syncytial Virus Isothermal Nucleic Acid Amplification Assay. J. Clin. Microbiol. 2018, 56. [Google Scholar] [CrossRef]
- Grebely, J.; Applegate, T.L.; Cunningham, P.; Feld, J.J. Hepatitis C point-of-care diagnostics: In search of a single visit diagnosis. Expert Rev. Mol. Diagn. 2017, 17, 1109–1115. [Google Scholar] [CrossRef]
- Gaydos, C.A.; Klausner, J.D.; Pai, N.P.; Kelly, H.; Coltart, C.; Peeling, R.W. Rapid and point-of-care tests for the diagnosis of Trichomonas vaginalis in women and men. Sex. Transm. Infect. 2017, 93, S31–S35. [Google Scholar] [CrossRef]
- Hurt, C.B.; Nelson, J.A.E.; Hightow-Weidman, L.B.; Miller, W.C. Selecting an HIV Test: A Narrative Review for Clinicians and Researchers. Sex. Transm. Dis. 2017, 44, 739–746. [Google Scholar] [CrossRef]
- Kelly, H.; Coltart, C.E.M.; Pant Pai, N.; Klausner, J.D.; Unemo, M.; Toskin, I.; Peeling, R.W. Systematic reviews of point-of-care tests for the diagnosis of urogenital Chlamydia trachomatis infections. Sex. Transm. Infect. 2017, 93, S22–S30. [Google Scholar] [CrossRef] [PubMed]
- Basile, K.; Kok, J.; Dwyer, D.E. Point-of-care diagnostics for respiratory viral infections. Expert Rev. Mol. Diagn. 2018, 18, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Nzelu, C.O.; Kato, H.; Peters, N.C. Loop-mediated isothermal amplification (LAMP): An advanced molecular point-of-care technique for the detection of Leishmania infection. PLoS Negl. Trop. Dis. 2019, 13, e0007698. [Google Scholar] [CrossRef] [PubMed]
- Datta, M.; Desai, D.; Kumar, A. Gene Specific DNA Sensors for Diagnosis of Pathogenic Infections. Indian J. Microbiol. 2017, 57, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Syal, K.; Mo, M.; Yu, H.; Iriya, R.; Jing, W.; Guodong, S.; Wang, S.; Grys, T.E.; Haydel, S.E.; Tao, N. Current and emerging techniques for antibiotic susceptibility tests. Theranostics 2017, 10, 1795–1805. [Google Scholar] [CrossRef] [PubMed]
- Maugeri, G.; Lychko, I.; Sobral, R.; Roque, A.C.A. Identification and Antibiotic-Susceptibility Profiling of Infectious Bacterial Agents: A Review of Current and Future Trends. Biotechnol. J. 2019, 14, 1700750. [Google Scholar] [CrossRef]
- Morris, E.; McCartney, D.; Lasserson, D.; Van den Bruel, A.; Fisher, R.; Hayward, G. Point-of-care lactate testing for sepsis at presentation to health care: A systematic review of patient outcomes. Br. J. Gen. Pract. 2017, 67, e859–e870. [Google Scholar] [CrossRef]
- Baig, M.A.; Shahzad, H.; Hussain, E.; Mian, A. Validating a point of care lactate meter in adult patients with sepsis presenting to the emergency department of a tertiary care hospital of a low- to middle-income country. World J. Emerg. Med. 2017, 8, 184–189. [Google Scholar] [CrossRef][Green Version]
- Hassan, U.; Ghonge, T.; Reddy, B., Jr.; Patel, M.; Rappleye, M.; Taneja, I.; Tanna, A.; Healey, R.; Manusry, N.; Price, Z.; et al. A point-of-care microfluidic biochip for quantification of CD64 expression from whole blood for sepsis stratification. Nat. Commun. 2017, 8, 1–12. [Google Scholar] [CrossRef]
- Westra, B.L.; Landman, S.; Yadav, P.; Steinbach, M. Secondary Analysis of an Electronic Surveillance System Combined with Multi-focal Interventions for Early Detection of Sepsis. Appl. Clin. Inform. 2017, 8, 47–66. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coluccio, M.L.; Pullano, S.A.; Vismara, M.F.M.; Coppedè, N.; Perozziello, G.; Candeloro, P.; Gentile, F.; Malara, N. Emerging Designs of Electronic Devices in Biomedicine. Micromachines 2020, 11, 123. https://doi.org/10.3390/mi11020123
Coluccio ML, Pullano SA, Vismara MFM, Coppedè N, Perozziello G, Candeloro P, Gentile F, Malara N. Emerging Designs of Electronic Devices in Biomedicine. Micromachines. 2020; 11(2):123. https://doi.org/10.3390/mi11020123
Chicago/Turabian StyleColuccio, Maria Laura, Salvatore A. Pullano, Marco Flavio Michele Vismara, Nicola Coppedè, Gerardo Perozziello, Patrizio Candeloro, Francesco Gentile, and Natalia Malara. 2020. "Emerging Designs of Electronic Devices in Biomedicine" Micromachines 11, no. 2: 123. https://doi.org/10.3390/mi11020123
APA StyleColuccio, M. L., Pullano, S. A., Vismara, M. F. M., Coppedè, N., Perozziello, G., Candeloro, P., Gentile, F., & Malara, N. (2020). Emerging Designs of Electronic Devices in Biomedicine. Micromachines, 11(2), 123. https://doi.org/10.3390/mi11020123










