Recombinant Clostridium difficile Toxin Fragments as Carrier Protein for PSII Surface Polysaccharide Preserve Their Neutralizing Activity
Abstract
:1. Introduction
2. Results and Discussion
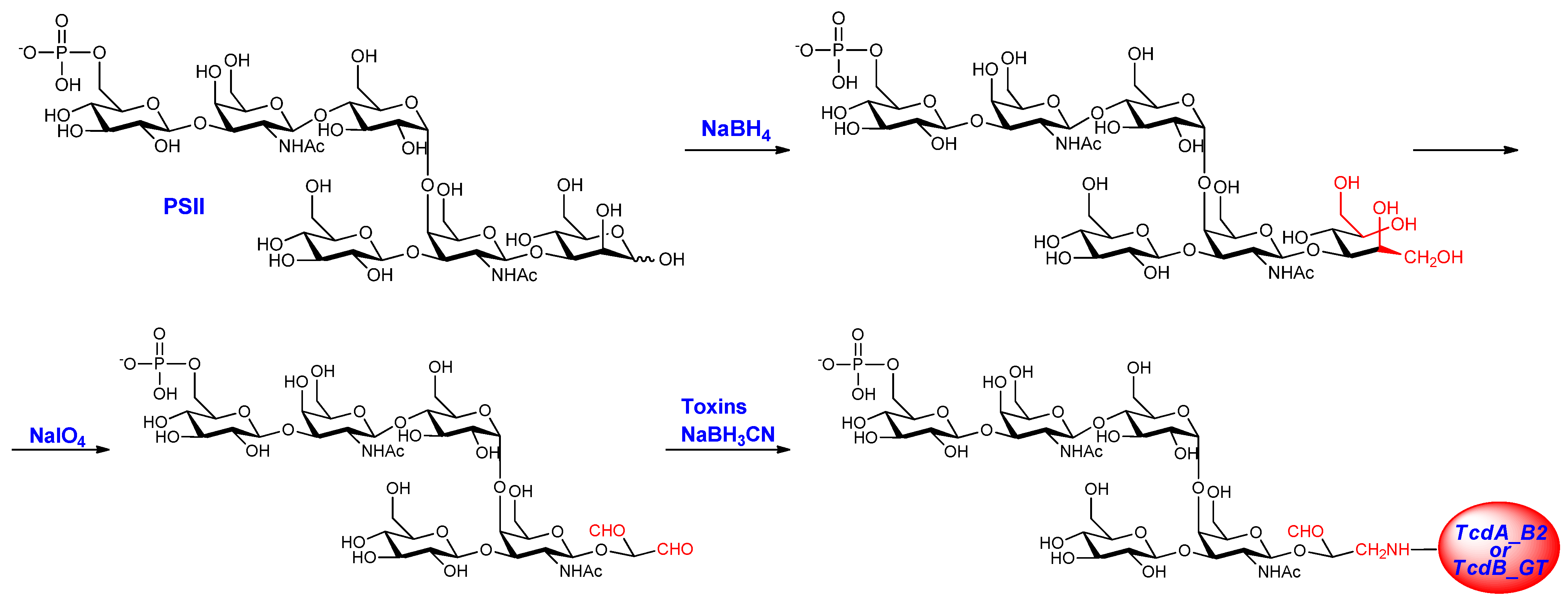
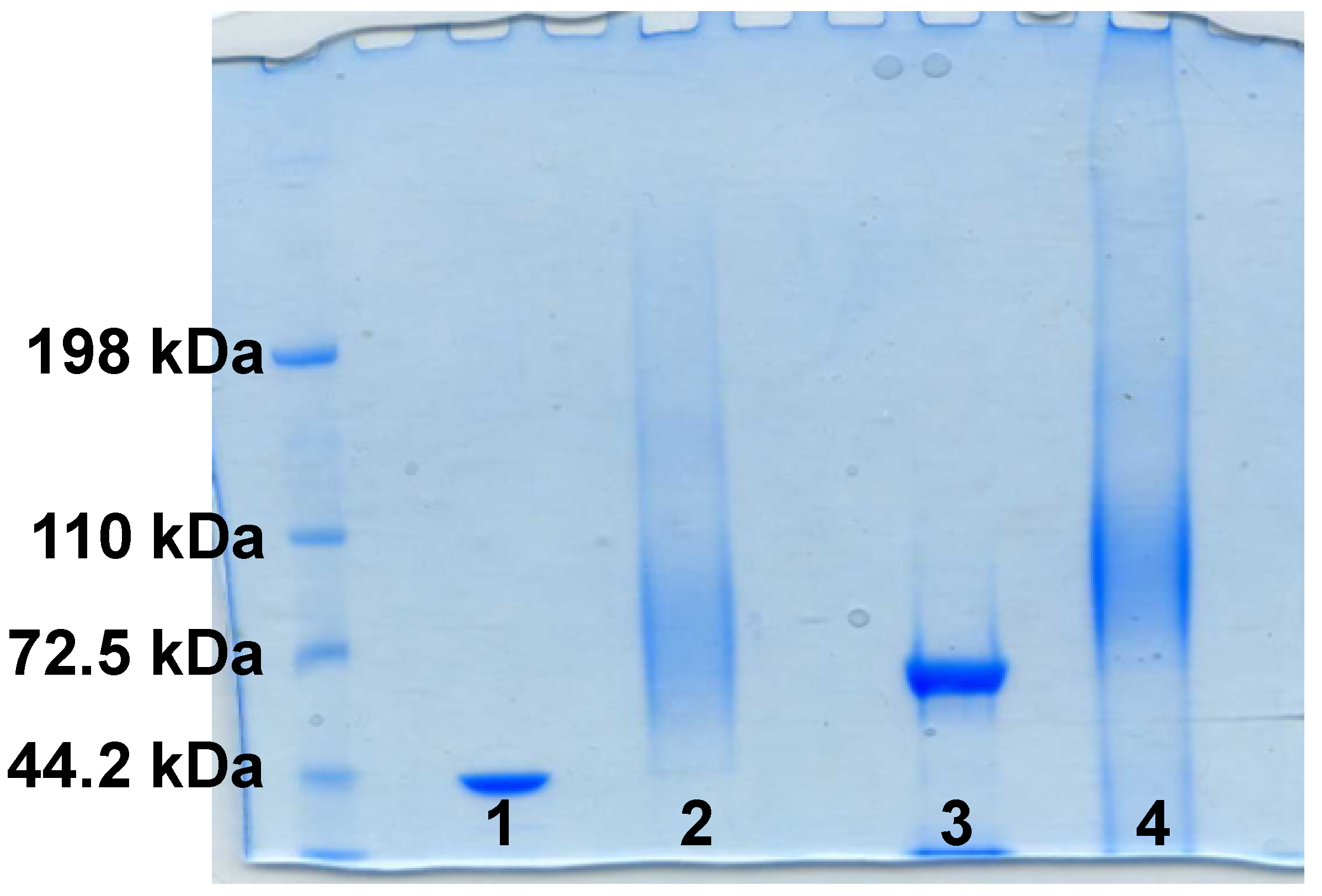
2.1. PSII-Toxins Conjugates
| Conjugates | PSII avDP | Free saccharide (%) | Saccharide/protein (w/w) |
|---|---|---|---|
| PSII-TcdA_B2 | 15 | 7.7 | 0.28 |
| PSII-TcdB_GT | 15 | 22.7 | 0.33 |
| PSII-CRM197 * | 21 | 11.2 | 0.24 |
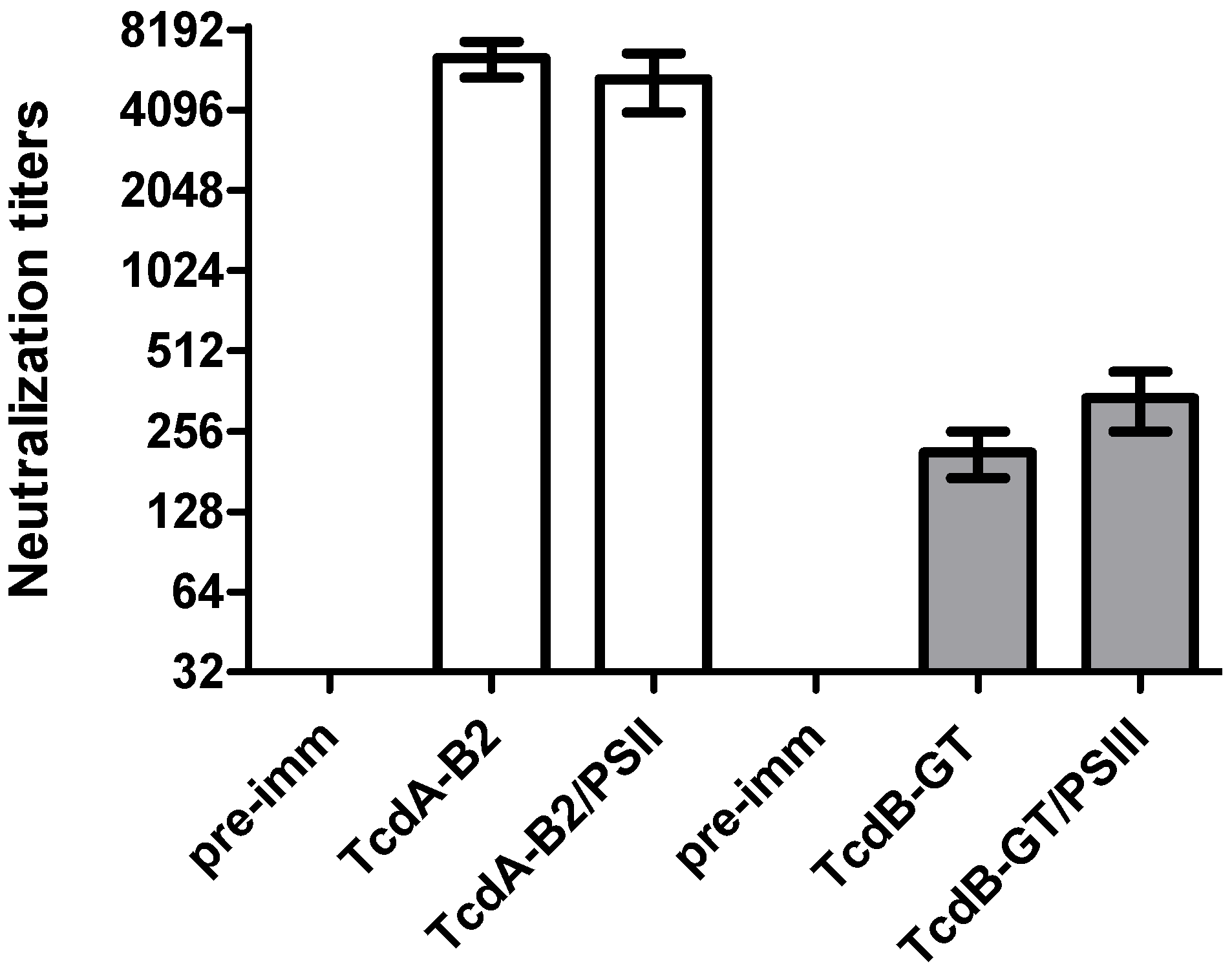
2.2. Immunological Evaluation of PSII-Toxins Conjugates
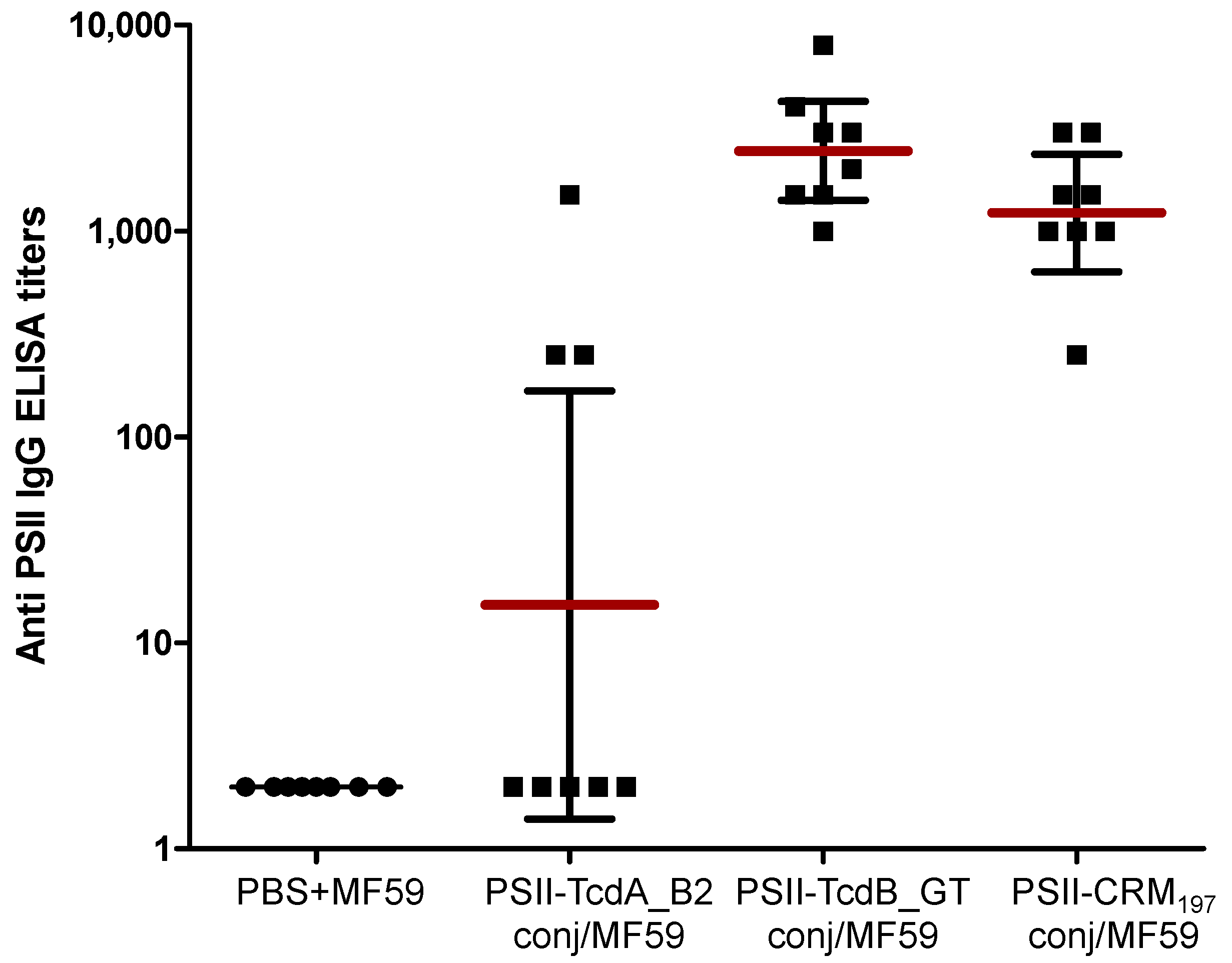
| Antigen | IgG titer (geometric mean titer) | 95% confidence interval |
|---|---|---|
| PBS | 2 | - |
| TcdA_B2 fragment protein | 1,024,000 | 374,868–4,023,000 |
| PSII-TcdA_B2 conjugate | 51,499 | 28,721–109,279 |
| TcdB_GT fragment protein | 206,317 | 47,610–400,390 |
| PSII-TcdB_GT conjugate | 106,936 | 69,489–174,511 |
| PSII-CRM197 | 2 | - |
3. Experimental Section
3.1. Preparation and Purification of PSII Glycoconjugates
3.2. Characterization of PSII Glycoconjugates
3.3. Cloning, Expression and Purification of Recombinant Fragments
3.4. Immunization Protocol
3.5. ELISA Assay
3.6. In Vitro Neutralization Assay
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kelly, C.P.; LaMont, J.T. Clostridium difficile—More difficult than ever. N. Engl. J. Med. 2008, 359, 1932–1940. [Google Scholar] [CrossRef]
- Rebeaud, F.; Bachmann, M.F. Immunization strategies for Clostridium difficile infections. Expert Rev. Vaccines 2012, 11, 469–479. [Google Scholar] [CrossRef]
- Chitnis, A.S.; Holzbauer, S.M.; Belflower, R.M.; Winston, L.G.; Bamberg, W.M.; Lyons, C.; Farley, M.M.; Dumyati, G.K.; Wilson, L.E.; Beldavs, Z.G.; et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern. Med. 2013, 173, 1359–1367. [Google Scholar] [CrossRef]
- Kyne, L.; Hamel, M.B.; Polavaram, R.; Kelly, C.P. Health care costs and mortality associated with nosocomial diarrhea due to Clostridium difficile. Clin. Infect. Dis. 2002, 34, 346–353. [Google Scholar] [CrossRef]
- Petrella, L.A.; Sambol, S.P.; Cheknis, A.; Nagaro, K.; Kean, Y.; Sears, P.S.; Babakhani, F.; Johnson, S.; Gerding, D.N. Decreased cure and increased recurrence rates for Clostridium difficile infection caused by the epidemic C. difficile BI strain. Clin. Infect. Dis. 2012, 55, 351–357. [Google Scholar] [CrossRef]
- Kyne, L.; Warny, M.; Qamar, A.; Kelly, C.P. Association between antibody response to toxin A and protection against recurrent Clostridium difficile diarrhoea. Lancet 2001, 357, 189–193. [Google Scholar] [CrossRef]
- Leav, B.A.; Blair, B.; Leney, M.; Knauber, M.; Reilly, C.; Lowy, I.; Gerding, D.N.; Kelly, C.P.; Katchar, K.; Baxter, R.; et al. Serum anti-toxin B antibody correlates with protection from recurrent Clostridium difficile infection (CDI). Vaccine 2010, 28, 965–969. [Google Scholar] [CrossRef]
- Steele, J.; Mukherjee, J.; Parry, N.; Tzipori, S. Antibody against TcdB, but not TcdA, prevents development of gastrointestinal and systemic Clostridium difficile disease. J. Infect. Dis. 2013, 207, 323–330. [Google Scholar] [CrossRef]
- Jank, T.; Giesemann, T.; Aktories, K. Rho-glucosylating Clostridium difficile toxins A and B: New insights into structure and function. Glycobiology 2007, 17, 15R–22R. [Google Scholar] [CrossRef]
- Lowy, I.; Molrine, D.C.; Leav, B.A.; Blair, B.M.; Baxter, R.; Gerding, D.N.; Nichol, G.; Thomas, W.D., Jr.; Leney, M.; Sloan, S.; et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N. Engl. J. Med. 2010, 362, 197–205. [Google Scholar] [CrossRef]
- Marozsan, A.J.; Ma, D.; Nagashima, K.A.; Kennedy, B.J.; Kang, Y.K.; Arrigale, R.R.; Donovan, G.P.; Magargal, W.W.; Maddon, P.J.; Olson, W.C. Protection against Clostridium difficile infection with broadly neutralizing antitoxin monoclonal antibodies. J. Infect. Dis. 2012, 206, 706–713. [Google Scholar] [CrossRef]
- Kotloff, K.L.; Wasserman, S.S.; Losonsky, G.A.; Thomas, W., Jr.; Nichols, R.; Edelman, R.; Bridwell, M.; Monath, T.P. Safety and immunogenicity of increasing doses of a Clostridium difficile toxoid vaccine administered to healthy adults. Infect. Immun. 2001, 69, 988–995. [Google Scholar] [CrossRef]
- Aboudola, S.; Kotloff, K.L.; Kyne, L.; Warny, M.; Kelly, E.C.; Sougioultzis, S.; Giannasca, P.J.; Monath, T.P.; Kelly, C.P. Clostridium difficile vaccine and serum immunoglobulin G antibody response to toxin A. Infect. Immun. 2003, 71, 1608–1610. [Google Scholar]
- Sougioultzis, S.; Kyne, L.; Drudy, D.; Keates, S.; Maroo, S.; Pothoulakis, C.; Giannasca, P.J.; Lee, C.K.; Warny, M.; Monath, T.P.; et al. Clostridium difficile toxoid vaccine in recurrent C. difficile-associated diarrhea. Gastroenterology 2005, 128, 764–770. [Google Scholar] [CrossRef]
- Donald, R.G.; Flint, M.; Kalyan, N.; Johnson, E.; Witko, S.E.; Kotash, C.; Zhao, P.; Megati, S.; Yurgelonis, I.; Lee, P.K.; et al. A novel approach to generate a recombinant toxoid vaccine against Clostridium difficile. Microbiology 2013, 159, 1254–1266. [Google Scholar] [CrossRef]
- Ryan, E.T.; Butterton, J.R.; Smith, R.N.; Carroll, P.A.; Crean, T.I.; Calderwood, S.B. Protective immunity against Clostridium difficile toxin A induced by oral immunization with a live, attenuated Vibrio cholerae vector strain. Infect. Immun. 1997, 65, 2941–2949. [Google Scholar]
- Ward, S.J.; Douce, G.; Figueiredo, D.; Dougan, G.; Wren, B.W. Immunogenicity of a Salmonella typhimurium aroA aroD vaccine expressing a nontoxic domain of Clostridium difficile toxin A. Infect. Immun. 1999, 67, 2145–2152. [Google Scholar]
- Tian, J.H.; Fuhrmann, S.R.; Kluepfel-Stahl, S.; Carman, R.J.; Ellingsworth, L.; Flyer, D.C. A novel fusion protein containing the receptor binding domains of C. difficile toxin A and toxin B elicits protective immunity against lethal toxin and spore challenge in preclinical efficacy models. Vaccine 2012, 30, 4249–4258. [Google Scholar] [CrossRef]
- Leuzzi, R.; Spencer, J.; Buckley, A.; Brettoni, C.; Martinelli, M.; Tulli, L.; Marchi, S.; Luzzi, E.; Irvine, J.; Candlish, D.; et al. Protective efficacy induced by recombinant Clostridium difficile toxin fragments. Infect. Immun. 2013, 81, 2851–2860. [Google Scholar] [CrossRef]
- Spencer, J.; Leuzzi, R.; Buckley, A.; Irvine, J.; Candlish, D.; Scarselli, M.; Douce, G.R. Vaccination against Clostridium difficile using toxin fragments: Observations and analysis in animal models. Gut Microbes 2014, 5. [Google Scholar] [CrossRef]
- Monteiro, M.A.; Ma, Z.; Bertolo, L.; Jiao, Y.; Arroyo, L.; Hodgins, D.; Mallozzi, M.; Vedantam, G.; Sagermann, M.; Sundsmo, J.; et al. Carbohydrate-based Clostridium difficile vaccines. Expert Rev. Vaccines 2013, 12, 421–431. [Google Scholar] [CrossRef]
- Ganeshapillai, J.; Vinogradov, E.; Rousseau, J.; Weese, J.S.; Monteiro, M.A. Clostridium difficile cell-surface polysaccharides composed of pentaglycosyl and hexaglycosyl phosphate repeating units. Carbohydr. Res. 2008, 343, 703–710. [Google Scholar] [CrossRef]
- Adamo, R.; Romano, M.R.; Berti, F.; Leuzzi, R.; Tontini, M.; Danieli, E.; Cappelletti, E.; Cakici, O.S.; Swennen, E.; Pinto, V.; et al. Phosphorylation of the synthetic hexasaccharide repeating unit is essential for the induction of antibodies to Clostridium difficile PSII cell wall polysaccharide. ACS Chem. Biol. 2012, 7, 1420–1428. [Google Scholar] [CrossRef]
- Reid, C.W.; Vinogradov, E.; Li, J.; Jarrell, H.C.; Logan, S.M.; Brisson, J.R. Structural characterization of surface glycans from Clostridium difficile. Carbohydr. Res. 2012, 354, 65–73. [Google Scholar] [CrossRef]
- Ðapa, T.; Leuzzi, R.; Ng, Y.K.; Baban, S.T.; Adamo, R.; Kuehne, S.A.; Scarselli, M.; Minton, N.P.; Serruto, D.; Unnikrishnan, M. Multiple factors modulate biofilm formation by the anaerobic pathogen Clostridium difficile. J. Bacteriol. 2013, 195, 545–555. [Google Scholar] [CrossRef]
- Berti, F.; Adamo, R. Recent mechanistic insights on glycoconjugate vaccines and future perspectives. ACS Chem. Biol. 2013, 8, 1653–1663. [Google Scholar] [CrossRef]
- Bertolo, L.; Boncheff, A.G.; Ma, Z.; Chen, Y.H.; Wakeford, T.; Friendship, R.M.; Rosseau, J.; Weese, J.S.; Chu, M.; Mallozzi, M.; et al. Clostridium difficile carbohydrates: Glucan in spores, PSII common antigen in cells, immunogenicity of PSII in swine and synthesis of a dual C. difficile-ETEC conjugate vaccine. Carbohydr. Res. 2012, 354, 79–86. [Google Scholar] [CrossRef]
- Bröker, M.; Costantino, P.; DeTora, L.; McIntosh, E.D.; Rappuoli, R. Biochemical and biological characteristics of cross-reacting material 197 CRM197, a non-toxic mutant of diphtheria toxin: Use as a conjugation protein in vaccines and other potential clinical applications. Biologicals 2011, 39, 195–204. [Google Scholar] [CrossRef]
- Costantino, P.; Rappuoli, R.; Berti, F. The design of semi-synthetic and synthetic glycoconjugate vaccines. Expert Opin. Drug Discov. 2011, 6, 1045–1067. [Google Scholar] [CrossRef]
- Oberli, M.A.; Hecht, M.L.; Bindschädler, P.; Adibekian, A.; Adam, T.; Seeberger, P.H. A possible oligosaccharide-conjugate vaccine candidate for Clostridium difficile is antigenic and immunogenic. Chem. Biol. 2011, 18, 580–588. [Google Scholar] [CrossRef]
- Danieli, E.; Lay, L.; Proietti, D.; Berti, F.; Costantino, P.; Adamo, R. First synthesis of C. difficile PS-II cell wall polysaccharide repeating unit. Org. Lett. 2011, 13, 378–381. [Google Scholar] [CrossRef]
- Galli, G.; Medini, D.; Borgogni, E.; Zedda, L.; Bardelli, M.; Malzone, C.; Nuti, S.; Tavarini, S.; Sammicheli, C.; Hilbert, A.K.; et al. Adjuvanted H5N1 vaccine induces early CD4+ T cell response that predicts long-term persistence of protective antibody levels. Proc. Natl. Acad. Sci. USA 2009, 106, 3877–3882. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Romano, M.R.; Leuzzi, R.; Cappelletti, E.; Tontini, M.; Nilo, A.; Proietti, D.; Berti, F.; Costantino, P.; Adamo, R.; Scarselli, M. Recombinant Clostridium difficile Toxin Fragments as Carrier Protein for PSII Surface Polysaccharide Preserve Their Neutralizing Activity. Toxins 2014, 6, 1385-1396. https://doi.org/10.3390/toxins6041385
Romano MR, Leuzzi R, Cappelletti E, Tontini M, Nilo A, Proietti D, Berti F, Costantino P, Adamo R, Scarselli M. Recombinant Clostridium difficile Toxin Fragments as Carrier Protein for PSII Surface Polysaccharide Preserve Their Neutralizing Activity. Toxins. 2014; 6(4):1385-1396. https://doi.org/10.3390/toxins6041385
Chicago/Turabian StyleRomano, Maria R., Rosanna Leuzzi, Emilia Cappelletti, Marta Tontini, Alberto Nilo, Daniela Proietti, Francesco Berti, Paolo Costantino, Roberto Adamo, and Maria Scarselli. 2014. "Recombinant Clostridium difficile Toxin Fragments as Carrier Protein for PSII Surface Polysaccharide Preserve Their Neutralizing Activity" Toxins 6, no. 4: 1385-1396. https://doi.org/10.3390/toxins6041385
APA StyleRomano, M. R., Leuzzi, R., Cappelletti, E., Tontini, M., Nilo, A., Proietti, D., Berti, F., Costantino, P., Adamo, R., & Scarselli, M. (2014). Recombinant Clostridium difficile Toxin Fragments as Carrier Protein for PSII Surface Polysaccharide Preserve Their Neutralizing Activity. Toxins, 6(4), 1385-1396. https://doi.org/10.3390/toxins6041385




