Profiling the Murine Acute Phase and Inflammatory Responses to African Snake Venom: An Approach to Inform Acute Snakebite Pathology
Abstract
1. Introduction
2. Results
2.1. Haematological Analyses of Envenomed Mice
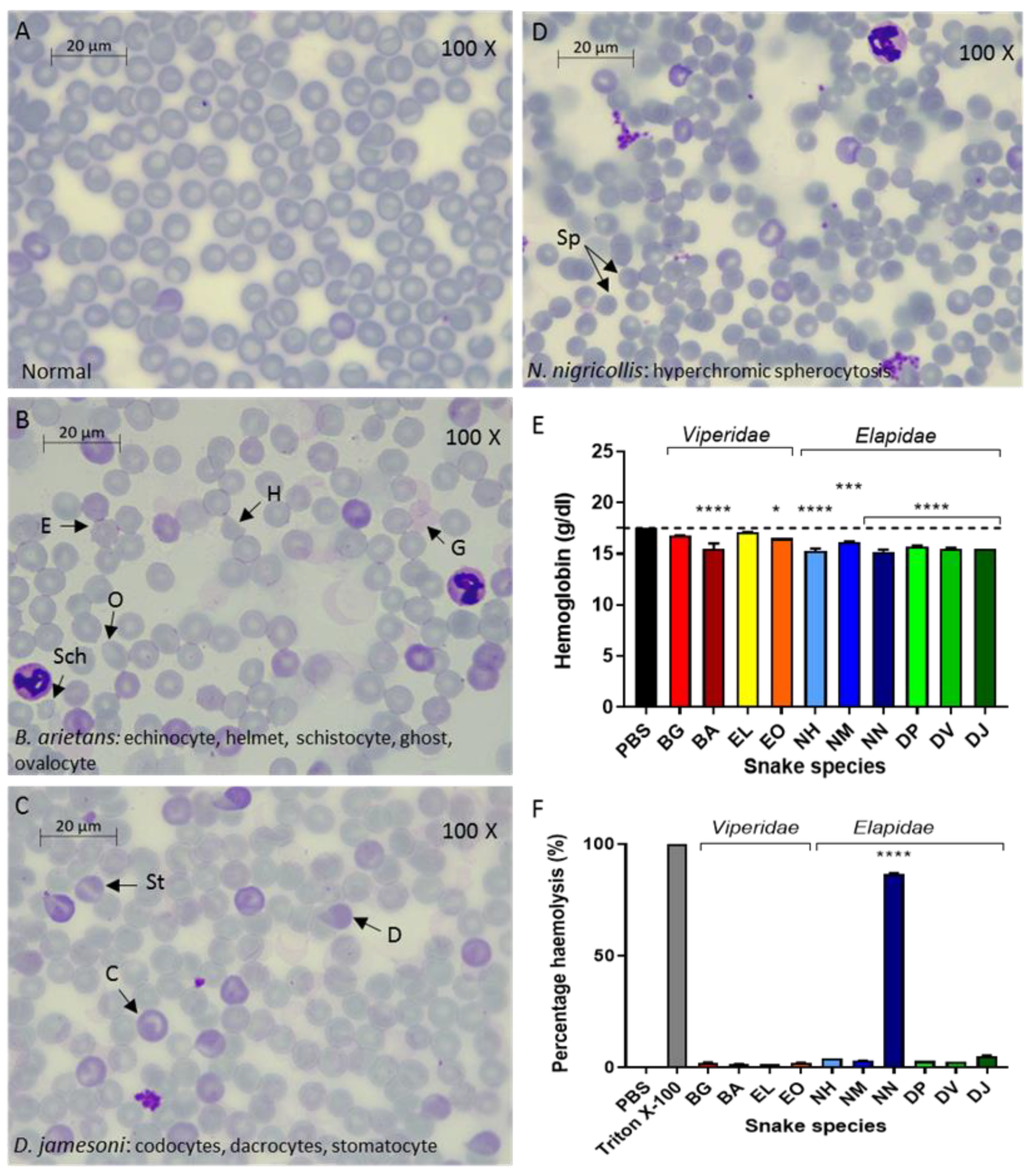
2.1.1. RBC Abnormalities Suggest Venom-Induced Haemolysis in Mice
2.1.2. Effects of Venom on Ex Vivo Human Blood
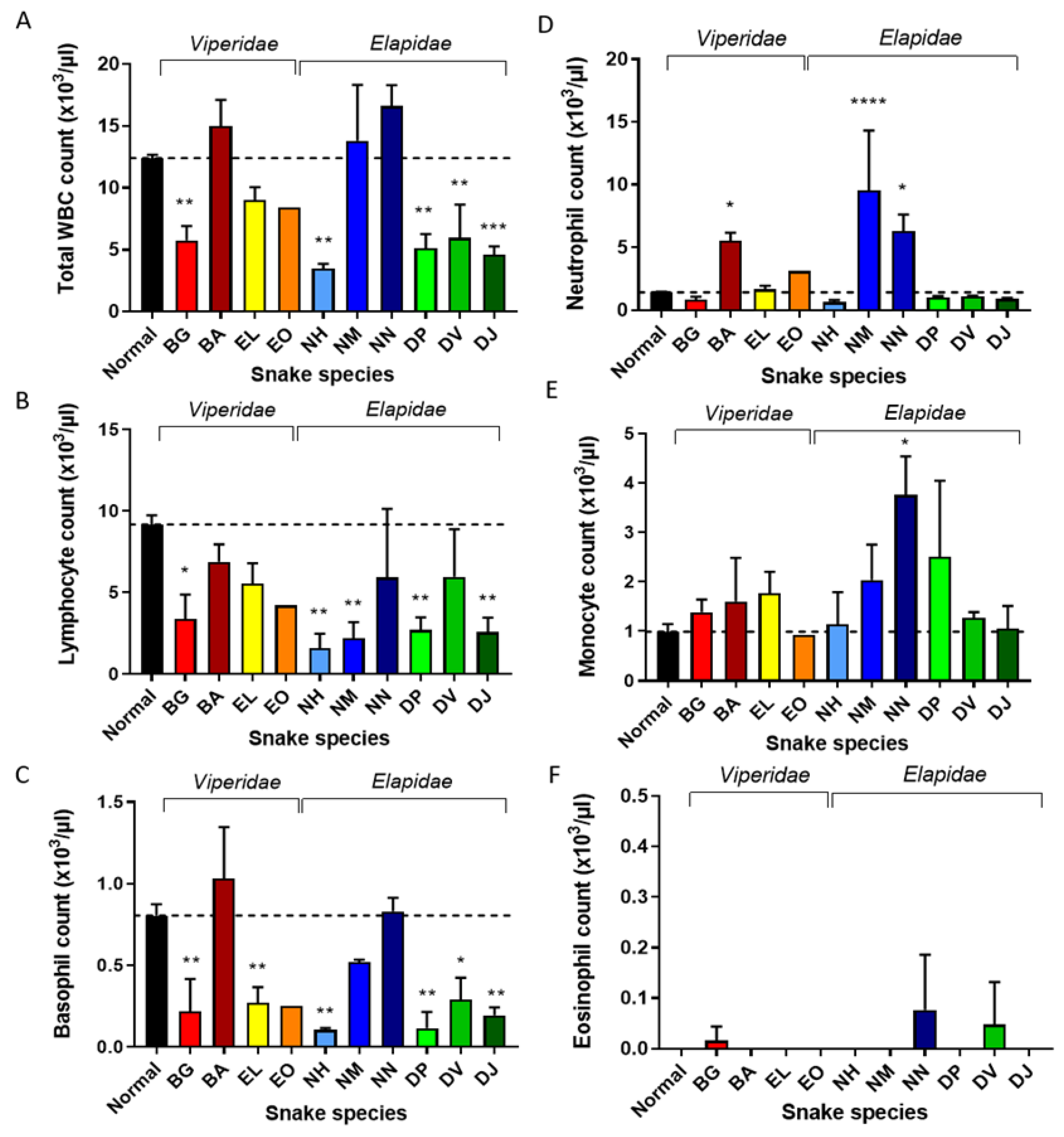
2.1.3. N. Nigricollis, N. Melanoleuca, and B. Arietans Venoms Cause Neutrophilia in Mice
2.1.4. Changes in Mouse Platelet Levels Following Injection with Viper and Elapid Venoms
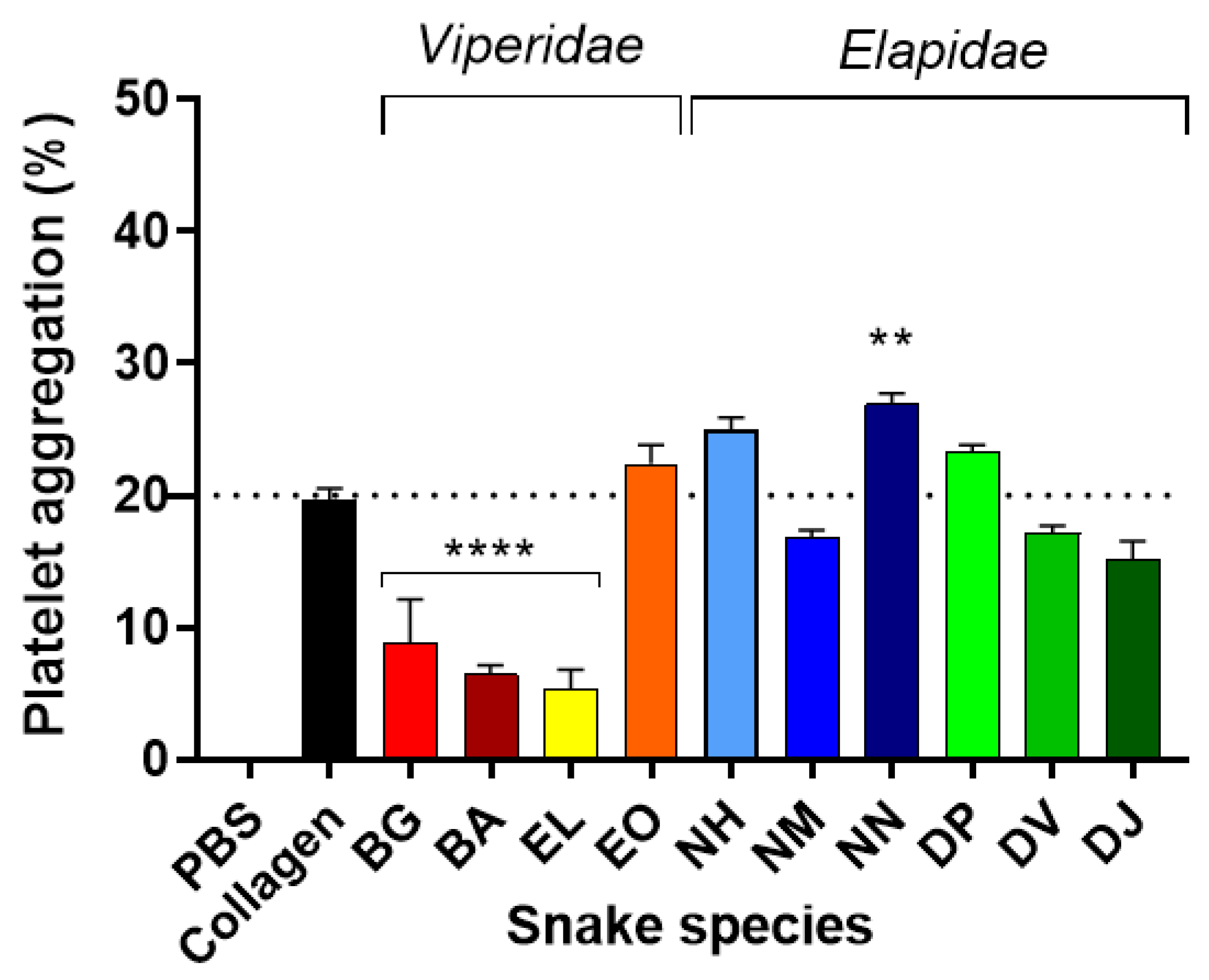
2.1.5. Platelet Aggregation in Ex Vivo Human Blood Exposed to Viper and Elapid Venoms
2.2. Acute Phase and Acute Inflammatory Responses in Envenomed Mice
2.2.1. P-Selectin Involvement in Acute Inflammatory Responses
2.2.2. Envenoming-Related Immunoglobulin Responses
2.2.3. The Acute Phase Response in Mice Subjected to Viper and Elapid Venoms
2.2.4. Naja Nigricollis Venom Causes Rapid Release of Systemic Inflammatory Mediators
2.3. Serum Biochemistry in Venom-Injected Mice
3. Discussion
3.1. Inflammatory Cytokine Responses to Venom Injection
3.2. Leukocyte Changes to Venom Injection
3.3. Haptoglobin and Serum Amyloid A Responses in Mice Injected with Venom
3.4. Venom-Induced Changes in Markers of Renal, Hepatic, Muscle and Blood Cell Damage
4. Conclusions
5. Materials and Methods
5.1. Snake Venoms
5.2. Animals and Research Design
- a thin blood film (n = 50) for microscopic analysis
- sera—blood was allowed to clot at room temperature, centrifuged for 10 min (9600× g at 4 °C) and sera stored at −20 °C (n = 50) to quantitate markers of:
- o
- acute inflammatory responses
- o
- acute phase responses
- o
- liver, heart and kidney damage.
5.3. Blood Film Preparation and Haematological Analysis
5.4. Quantification of Murine C-Reactive Protein and Cytokines by Multiplex Bead Array
5.5. Quantification of Serum Amyloid A, P-Selectin and Murine IgM by ELISA
5.6. Quantification of Murine Haptoglobin by Colorimetric Assay
5.7. Standard Biochemical Analysis of Mouse Serum Samples
5.8. Collection of Human Blood for Ex Vivo Assays
5.8.1. Quantifying Venom Haemolytic Activity on Human Erythrocytes
5.8.2. Quantifying Venom-Induced Aggregation of Human Platelets
5.8.3. Colorimetric Quantification of Venom-Induced Release of Human Haemoglobin
5.9. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gutiérrez, J.M.; Williams, D.; Fan, H.W.; Warrell, D.A. Snakebite envenoming from a global perspective: Towards an integrated approach. Toxicon 2010, 56, 1223–1235. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, J.M.; Calvete, J.J.; Habib, A.G.; Harrison, R.A.; Williams, D.J.; Warrell, D.A. Snakebite envenoming. Nat. Rev. Dis. Primers 2017, 3, 17063. [Google Scholar] [CrossRef] [PubMed]
- Chippaux, J.P. Snake-bites: Appraisal of the global situation. Bull. World Health Organ. 1998, 76, 515. [Google Scholar]
- Kasturiratne, A.; Wickremasinghe, A.R.; De Silva, N.; Gunawardena, N.K.; Pathmeswaran, A.; Premaratna, R.; Savioli, L.; Lalloo, D.G.; De Silva, H.J. The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008, 5, e218. [Google Scholar] [CrossRef]
- Casewell, N.R.; Wagstaff, S.C.; Wüster, W.; Cook, D.A.N.; Bolton, F.M.S.; King, S.I.; Pla, D.; Sanz, L.; Calvete, J.J.; Harrison, R.A. Medically important differences in snake venom composition are dictated by distinct postgenomic mechanisms. Proc. Natl. Acad. Sci. USA 2014, 111, 9205–9210. [Google Scholar] [CrossRef]
- Warrell, D.A. Treatment of bites by adders and exotic venomous snakes. Br. Med. J. 2005, 331, 1244–1247. [Google Scholar] [CrossRef]
- Arango Duque, G.; Descoteaux, A. Macrophage cytokines: Involvement in immunity and infectious diseases. Front. Immunol. 2014, 5, 491. [Google Scholar] [CrossRef]
- Teixeira, C.F.P.; Zamunér, S.R.; Zuliani, J.P.; Fernandes, C.M.; Cruz-Hofling, M.A.; Fernandes, I.; Chaves, F.; Gutiérrez, J.M. Neutrophils do not contribute to local tissue damage, but play a key role in skeletal muscle regeneration, in mice injected with Bothrops asper snake venom. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 2003, 28, 449–459. [Google Scholar] [CrossRef]
- Cray, C.; Zaias, J.; Altman, N.H. Acute phase response in animals: A review. Comp. Med. 2009, 59, 517–526. [Google Scholar] [PubMed]
- Stone, S.F.; Isbister, G.K.; Shahmy, S.; Mohamed, F.; Abeysinghe, C.; Karunathilake, H.; Ariaratnam, A.; Jacoby-Alner, T.E.; Cotterell, C.L.; Brown, S.G. Immune response to snake envenoming and treatment with antivenom; complement activation, cytokine production and mast cell degranulation. PLoS Negl. Trop. Dis. 2013, 7, e2326. [Google Scholar] [CrossRef] [PubMed]
- Baumann, H.; Gauldie, J. (Eds.) The acute phase response. Great Britain. Immunol. Today 1994, 5, 74–80. [Google Scholar] [CrossRef]
- Ávila-Agüero, M.L.; París, M.M.; Hu, S.; Peterson, P.K.; Ulloa-Gutierrez, R.; Lomonte, B.; Faingezicht, I. Systemic cytokine response in children bitten by snakes in Costa Rica. Pediatr. Emerg. Care 2001, 17, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Barraviera, B.; Lomonte, B.; Tarkowski, A.; Hanson, L.; Meira, D.A. Acute-phase reactions, including cytokines, in patients bitten by Bothrops and Crotalus snakes in Brazil. J. Venom. Anim. Toxins 1995, 1, 11–22. [Google Scholar] [CrossRef]
- De Sousa-E-Silva, M.C.; Tomy, S.C.; Tavares, F.L.; Navajas, L.; Larsson, M.H.; Lucas, S.R.; Kogika, M.M.; Sano-Martins, I.S. Hematological, hemostatic and clinical chemistry disturbances induced by Crotalus durissus terrificus snake venom in dogs. Hum. Exp. Toxicol. 2003, 22, 491–500. [Google Scholar] [CrossRef]
- Langhorn, R.; Persson, F.; Åblad, B.; Goddard, A.; Schoeman, J.P.; Willesen, J.L.; Tarnow, I.; Kjelgaard-Hansen, M. Myocardial injury in dogs with snake envenomation and its relation to systemic inflammation. J. Vet. Emerg. Crit. Care 2014, 24, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Lobetti, R.G.; Joubert, K. Retrospective study of snake envenomation in 155 dogs from the Onderstepoort area of South Africa. J. S. Afr. Vet. Assoc. 2004, 75, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Nagel, S.S.; Schoeman, J.P.; Thompson, P.N.; Wiinberg, B.; Goddard, A. Hemostatic analysis of dogs naturally envenomed by the African puffadder (Bitis arietans) and snouted cobra (Naja annulifera). J. Vet. Emerg. Crit. Care 2014, 24, 662–671. [Google Scholar] [CrossRef]
- Nogueira, R.M.B.; Sakate, M. Clinical and hematological alterations in dogs during experimental envenomation with Crotalus durissus terrificus venom and treated with antiophidic serum. J. Venom. Anim. Toxins Incl. Trop. Dis. 2006, 12, 285. [Google Scholar] [CrossRef][Green Version]
- Rucavado, A.; Nicolau, C.; Escalante, T.; Kim, J.; Herrera, C.; Gutiérrez, J.M.; Fox, J.W. Viperid envenomation wound exudate contributes to increased vascular permeability via a DAMPs/TLR-4 mediated pathway. Toxins 2016, 8, 349. [Google Scholar] [CrossRef]
- Moreira, V.; Teixeira, C.; Da Silva, H.B.; Lima, M.R.D.I.; Dos-Santos, M.C. The role of TLR2 in the acute inflammatory response induced by Bothrops atrox snake venom. Toxicon 2016, 118, 121–128. [Google Scholar] [CrossRef]
- Theakston, R.D.G.; Reid, H.A. Development of simple standard assay procedures for the characterization of snake venoms. Bull. World Health Organ. 1983, 61, 949. [Google Scholar] [PubMed]
- Rungsiwongse, J.; Ratanabanangkoon, K. Development of an ELISA to assess the potency of horse therapeutic antivenom against Thai cobra venom. J. Immunol. Methods 1991, 136, 37–43. [Google Scholar] [CrossRef]
- Pornmuttakun, D.; Ratanabanangkoon, K. Development of an in vitro potency assay for antivenom against Malayan pit viper (Calloselasma rhodostoma). Toxicon 2014, 77, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Bourke, L.A.; Zdenek, C.N.; Neri-Castro, E.; Bénard-Valle, M.; Alagón, A.; Gutiérrez, J.M.; Sanchez, E.; Aldridge, M.; Fry, B. Pan-American lancehead pit-vipers: Coagulotoxic venom effects and antivenom neutralisation of Bothrops asper and B. atrox geographical variants. Toxins 2021, 13, 78. [Google Scholar] [CrossRef]
- Chowdhury, A.; Zdenek, C.N.; Lewin, M.R.; Carter, R.; Jagar, T.; Ostanek, E.; Harjen, H.; Aldridge, M.; Soria, R.; Haw, G.; et al. Venom-Induced Blood Disturbances by Palearctic Viperid Snakes, and Their Relative Neutralization by Antivenoms and Enzyme-Inhibitors. Front. Immunol. 2021, 12, 2251. [Google Scholar] [CrossRef]
- Hoffman, J.F. On Red Blood Cells, Hemolysis and Resealed Ghosts. In The Use of Resealed Erythrocytes as Carriers and Bioreactors; Springer: Berlin/Heidelberg, Germany, 1992; pp. 1–15. [Google Scholar]
- Walton, R.M.; Brown, D.E.; Hamar, D.W.; Meador, V.P.; Horn, J.W.; Thrall, M.A. Mechanisms of echinocytosis induced by Crotalus atrox venom. Vet. Pathol. 1997, 34, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Chmielewski, P.P.; Strzelec, B. Elevated leukocyte count as a harbinger of systemic inflammation, disease progression, and poor prognosis: A review. Folia Morphol. 2018, 77, 171–178. [Google Scholar] [CrossRef]
- Ferrer-Acosta, Y.; González, M.; Fernández, M.; Valance, W.A. Emerging roles for platelets in inflammation and disease. J. Infect. Dis. Ther. 2014, 2, 149. [Google Scholar]
- O’Connell, K.E.; Mikkola, A.M.; Stepanek, A.M.; Vernet, A.; Hall, C.D.; Brown, D.E. Practical murine hematopathology: A comparative review and implications for research. Comp. Med. 2015, 65, 96–113. [Google Scholar]
- Lorant, D.E.; Topham, M.K.; Whatley, R.E.; McEver, R.P.; McIntyre, T.M.; Prescott, S.M.; Zimmerman, G.A. Inflammatory roles of P-selectin. J. Clin. Investig. 1993, 92, 559–570. [Google Scholar] [CrossRef]
- Ochsenbein, A.F.; Fehr, T.; Lutz, C.; Suter, M.; Brombacher, F.; Hengartner, H.; Zinkernagel, R.M. Control of early viral and bacterial distribution and disease by natural antibodies. Science 1999, 286, 2156–2159. [Google Scholar] [CrossRef] [PubMed]
- Baumgarth, N.; Tung, J.W.; Herzenberg, L.A. Inherent specificities in natural antibodies: A key to immune defense against pathogen invasion. Springer Semin. Immunopathol. 2005, 26, 347–362. [Google Scholar] [CrossRef] [PubMed]
- Quinton, L.J.; Jones, M.R.; Robson, B.E.; Mizgerd, J.P. Mechanisms of the hepatic acute-phase response during bacterial pneumonia. Infect. Immun. 2009, 77, 2417–2426. [Google Scholar] [CrossRef] [PubMed]
- Pathak, A.; Agrawal, A. Evolution of C-reactive protein. Front. Immunol. 2019, 10, 943. [Google Scholar] [CrossRef]
- Faqi, A.S. A Comprehensive Guide to Toxicology in Nonclinical Drug Development; Academic Press: Cambridge, MA, USA, 2016. [Google Scholar]
- Kalakonda, A.; John, S. Physiology, Bilirubin. StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Chippaux, J.-P.; Williams, V.; White, J. Snake venom variability: Methods of study, results and interpretation. Toxicon 1991, 29, 1279–1303. [Google Scholar] [CrossRef]
- Albulescu, L.-O.; Xie, C.; Ainsworth, S.; Alsolaiss, J.; Crittenden, E.; Dawson, C.A.; Softley, R.; Bartlett, K.E.; Harrison, R.A.; Kool, J.; et al. A therapeutic combination of two small molecule toxin inhibitors provides broad preclinical efficacy against viper snakebite. Nat. Commun. 2020, 11, 1–14. [Google Scholar] [CrossRef]
- Ainsworth, S.; Petras, D.; Engmark, M.; Süssmuth, R.; Whiteley, G.; Albulescu, L.-O.; Kazandjian, T.D.; Wagstaff, S.; Rowley, P.; Wüster, W.; et al. The medical threat of mamba envenoming in sub-Saharan Africa revealed by genus-wide analysis of venom composition, toxicity and antivenomics profiling of available antivenoms. J. Proteom. 2018, 172, 173–189. [Google Scholar] [CrossRef]
- Petras, D.; Sanz, L.; Segura, A.; Herrera, M.; Villalta, M.; Solano, D.; Harrison, R.A. Snake venomics of African spitting cobras: Toxin composition and assessment of congeneric cross-reactivity of the pan-African EchiTAb-Plus-ICP antivenom by antivenomics and neutralization approaches. J. Proteome Res. 2011, 10, 1266–1280. [Google Scholar] [CrossRef]
- Kazandjian, T.D.; Petras, D.; Robinson, S.D.; van Thiel, J.; Greene, H.W.; Arbuckle, K.; Barlow, A.; Carter, D.A.; Wouters, R.M.; Whiteley, G.; et al. Convergent evolution of pain-inducing defensive venom components in spitting cobras. Science 2021, 371, 386–390. [Google Scholar] [CrossRef]
- Petricevich, V.L. Cytokine and nitric oxide production following severe envenomation. Curr. Drug Targets-Inflamm. Allergy 2004, 3, 325–332. [Google Scholar] [CrossRef]
- Iddon, D.; Theakston, R.D.G.; Ownby, C.L. A study of the pathogenesis of local skin necrosis induced by Naja nigricollis (spitting cobra) venom using simple histological staining techniques. Toxicon 1987, 25, 665–672. [Google Scholar] [CrossRef]
- Rivel, M.; Solano, D.; Herrera, M.; Vargas, M.; Villalta, M.; Álvaro, S.; Arias, A.; León, G.; Gutiérrez, J.M. Pathogenesis of dermonecrosis induced by venom of the spitting cobra, Naja nigricollis: An experimental study in mice. Toxicon 2016, 119, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Heinrich, P.C.; Castell, J.V.; Andus, T. Interleukin-6 and the acute phase response. Biochem. J. 1990, 265, 621–636. [Google Scholar] [CrossRef]
- Liu, C.-C.; Ahearn, J.M. Acute-Phase Proteins and Inflammation: Immunological and Clinical Implications. In Measuring Immunity; Elsevier: Amsterdam, The Netherlands, 2005; pp. 131–143. [Google Scholar]
- Rosales, C. Neutrophil: A cell with many roles in inflammation or several cell types? Front. Physiol. 2018, 9, 113. [Google Scholar] [CrossRef]
- Santoro, M.L.; Sano-Martins, I.S.; Fan, H.W.; Cardoso, J.L.C.; Theakston, R.D.G.; Warrell, D.A. Haematological evaluation of patients bitten by the jararaca, Bothrops jararaca, in Brazil. Toxicon 2008, 51, 1440–1448. [Google Scholar] [CrossRef] [PubMed]
- Fest, J.; Ruiter, R.; Ikram, M.A.; Voortman, T.; van Eijck, C.H.J.; Stricker, B.H. Reference values for white blood-cell-based inflammatory markers in the Rotterdam Study: A population-based prospective cohort study. Sci. Rep. 2018, 8, 10566. [Google Scholar] [CrossRef]
- Aktar, F.; Aktar, S.; Yolbas, I.; Tekin, R. Evaluation of risk factors and follow-up criteria for severity of snakebite in children. Iran. J. Pediatr. 2016, 26. [Google Scholar] [CrossRef]
- Elbey, B.; Baykal, B.; Yazgan, Ü.C.; Zengin, Y. The prognostic value of the neutrophil/lymphocyte ratio in patients with snake bites for clinical outcomes and complications. Saudi J. Biol. Sci. 2017, 24, 362–366. [Google Scholar] [CrossRef]
- Aktar, F.; Tekin, R. Mean platelet volume, neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in determining the diagnosis or outcome in children with snakebite. Arch. Argent Pediatr. 2017, 115, 576–587. [Google Scholar]
- Williams, H.F.; Hayter, P.; Ravishankar, D.; Baines, A.; Layfield, H.J.; Croucher, L.; Wark, C.; Bicknell, A.B.; Trim, S.; Vaiyapuri, S. Impact of Naja nigricollis Venom on the Production of Methaemoglobin. Toxins 2018, 10, 539. [Google Scholar] [CrossRef]
- Eckersall, P.; Gow, J.W.; McComb, C.; Bradley, B.; Rodgers, J.; Murray, M.; Kennedy, P.G. Cytokines and the acute phase response in post-treatment reactive encephalopathy of Trypanosoma brucei brucei infected mice. Parasitol. Int. 2001, 50, 15–26. [Google Scholar] [CrossRef]
- Shapiro, S.Z.; Black, S.J. Identification of an acute-phase reactant in murine infections with Trypanosoma brucei. Infect. Immun. 1992, 60, 3921–3924. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Yang, J.W.; Kim, M.S.; Han, S.T.; Kim, B.R.; Shin, M.S.; Lee, J.I.; Han, B.-G.; Choi, S.O. Coagulopathy in patients who experience snakebite. Korean J. Intern. Med. 2008, 23, 94. [Google Scholar] [CrossRef]
- Warrell, D.A.; Ormerod, L.D.; Davidson, N.M. Bites by puff-adder (Bitis arietans) in Nigeria, and value of antivenom. Br. Med. J. 1975, 4, 697–700. [Google Scholar] [CrossRef] [PubMed]
- Udayabhaskaran, V.; Thomas, E.T.A.; Shaji, B. Capillary leak syndrome following snakebite envenomation. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2017, 21, 698. [Google Scholar] [CrossRef] [PubMed]
- Barcellini, W.; Fattizzo, B. Clinical applications of hemolytic markers in the differential diagnosis and management of hemolytic anemia. Dis. Markers 2015, 2015, 635670. [Google Scholar] [CrossRef]
- Gillissen, A.; Theakston, R.D.G.; Barth, J.; May, B.; Krieg, M.; Warrell, D.A. Neurotoxicity, haemostatic disturbances and haemolytic anaemia after a bite by a Tunisian saw-scaled or carpet viper (Echis ‘pyramidum’-complex): Failure of antivenom treatment. Toxicon 1994, 32, 937–944. [Google Scholar] [CrossRef]
- McCullough, S. Immune-mediated hemolytic anemia: Understanding the nemesis. Vet. Clin. Small Anim. Pract. 2003, 33, 1295–1315. [Google Scholar] [CrossRef]
- Ong, H.M.; Witham, A.; Kelers, K.; Boller, M. Presumed secondary immune-mediated haemolytic anaemia following elapid snake envenomation and its treatment in four dogs. Aust. Vet. J. 2015, 93, 319–326. [Google Scholar] [CrossRef]
- Tambourgi, D.V.; dos Santos, M.C.; Furtado, M.d.F.D.; de Freitas, M.C.W.; Dias da Silva, W.; Kipnis, T.L. Pro-inflammatory activities in elapid snake venoms. Br. J. Pharmacol. 1994, 112, 723–727. [Google Scholar] [CrossRef]
- Cleary, M.A. Creatine kinase, exertional rhabdomyolysis, and exercise-associated hyponatremia in ultra-endurance athletes: A critically appraised paper. Int. J. Athl. Ther. Train. 2016, 21, 13–15. [Google Scholar] [CrossRef]
- Torres, P.A.; Helmstetter, J.A.; Kaye, A.M.; Kaye, A.D. Rhabdomyolysis: Pathogenesis, diagnosis, and treatment. Ochsner J. 2015, 15, 58–69. [Google Scholar] [PubMed]
- Lim, A.Y.L.; Singh, P.N.; Isbister, G.K. Severe rhabdomyolysis from red-bellied black snake (Pseudechis porphyriacus) envenoming despite antivenom. Toxicon 2016, 117, 46–48. [Google Scholar] [CrossRef]
- Vikrant, S.; Jaryal, A.; Parashar, A. Clinicopathological spectrum of snake bite-induced acute kidney injury from India. World J. Nephrol. 2017, 6, 150. [Google Scholar] [CrossRef] [PubMed]
- James, O.; Godwin, E.U.; Otini, I.G. In vivo neutralization of Naja nigricollis venom by Uvaria chamae. Am. J. Biochem. Biotechnol. 2013, 9, 224. [Google Scholar] [CrossRef]
- Cheng, C.-L.; Mao, Y.-C.; Liu, P.-Y.; Chiang, L.-C.; Liao, S.-C.; Yang, C.-C. Deinagkistrodon acutus envenomation: A report of three cases. J. Venom. Anim. Toxins Incl. Trop. Dis. 2017, 23, 20. [Google Scholar] [CrossRef]
- Lavonas, E.J.; Tomaszewski, C.A.; Ford, M.D.; Rouse, A.M.; Kerns Ii, W.P. Severe puff adder (Bitis arietans) envenomation with coagulopathy. J. Toxicol. Clin. Toxicol. 2002, 40, 911–918. [Google Scholar] [CrossRef]
- Odeleye, A.A.; Presley, A.E.; Passwater, M.E.; Mintz, P.D. Rattlesnake venom-induced thrombocytopenia. Ann. Clin. Lab. Sci. 2004, 34, 467–470. [Google Scholar]
- Slagboom, J.; Kool, J.; Harrison, R.A.; Casewell, N.R. Haemotoxic snake venoms: Their functional activity, impact on snakebite victims and pharmaceutical promise. Br. J. Haematol. 2017, 177, 947–959. [Google Scholar] [CrossRef]
- Tscharre, M.; Vogel, B.; Tentzeris, I.; Freynhofer, M.K.; Rohla, M.; Wojta, J.; Weiss, T.W.; Ay, C.; Huber, K.; Farhan, S. Prognostic impact of soluble P-selectin on long-term adverse cardiovascular outcomes in patients undergoing percutaneous coronary intervention. Thromb. Haemost. 2019, 119, 340–347. [Google Scholar] [CrossRef]
- Bittenbinder, M.A.; Dobson, J.S.; Zdenek, C.N.; Brouw, B.O.D.; Naude, A.; Vonk, F.J.; Fry, B.G. Differential destructive (non-clotting) fibrinogenolytic activity in Afro-Asian elapid snake venoms and the links to defensive hooding behavior. Toxicol. Vitr. 2019, 60, 330–335. [Google Scholar] [CrossRef]
- Sun, D.S.; Chang, H.H.; Ho, P.H. Soluble P-selectin rescues viper venom-induced mortality through anti-inflammatory properties and PSGL-1 pathway-mediated correction of hemostasis. Sci. Rep. 2016, 6, 35868. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.-F.; Wang, W.-J.; Teng, C.-M.; Ouyang, C. Mechanism of action of the antiplatelet peptide, arietin, from Bitis arietans venom. BBA Gen. Subj. 1991, 1074, 144–150. [Google Scholar] [CrossRef]
- Shebuski, R.J.; Ramjit, D.R.; Bencen, G.H.; Polokoff, M.A. Characterization and platelet inhibitory activity of bitistatin, a potent arginine-glycine-aspartic acid-containing peptide from the venom of the viper Bitis arietans. J. Biol. Chem. 1989, 264, 21550–21556. [Google Scholar] [CrossRef]
- Strydom, M.A.; Bester, J.; Mbotwe, S.; Pretorius, E. The effect of physiological levels of South African puff adder (Bitis arietans) snake venom on blood cells: An in vitro model. Sci. Rep. 2016, 6, 35988. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines for the Production, Control and Regulation of Snake Antivenom Immunoglobulins; WHO: Geneva, Switzerland, 2010; p. 134. [Google Scholar]
- Dhurat, R.; Sukesh, M.S. Principles and methods of preparation of platelet-rich plasma: A review and author’s perspective. J. Cutan. Aesth. Surg. 2014, 7, 189. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.E. Determinants of Platelet Count in Humans; Haematologica, Ferrata Storti Foundation: Pavia, Italy, 2011. [Google Scholar]
- Zamuner, S.R.; Zuliani, J.P.; Fernandes, C.M.; Gutiérrez, J.M.; de Fátima Pereira Teixeira, C. Inflammation induced by Bothrops asper venom: Release of proinflammatory cytokines and eicosanoids, and role of adhesion molecules in leukocyte infiltration. Toxicon Off. J. Int. Soc. Toxinol. 2005, 46, 806–813. [Google Scholar]
- Rucavado, A.; Escalante, T.; Teixeira, C.F.P.; Fernandes, C.M.; Diaz, C.; Gutierrez, J.M. Increments in cytokines and matrix metalloproteinases in skeletal muscle after injection of tissue-damaging toxins from the venom of the snake Bothrops asper. Mediat. Inflamm. 2002, 11, 121–128. [Google Scholar]
- Lomonte, B.; Tarkowski, A.; Hanson, L.A. (Eds.) Host Response to Bothrops asper Snake Venom: Analysis of Edema Formation. Inflammatory Cells, and Cytokine Release in a Mouse Model; Plenum Publishing Corporation: New York, NY, USA, 1993. [Google Scholar]
- Petricevich, V.L.; Teixeira, C.F.P.; Tambourgi, D.V.; Gutiérrez, J.M.A. Increments in serum cytokine and nitric oxide levels in mice injected with Bothrops asper and Bothrops jararaca snake venoms. Toxicon 2000, 38, 1253–1266. [Google Scholar]
- Moreira, V.; Dos-Santos, M.C.; Nascimento, N.G.; da Silva, H.B.; Fernandes, C.M.; Lima, M.R.D.; Teixeira, C. Local inflammatory events induced by Bothrops atrox snake venom and the release of distinct classes of inflammatory mediators. Toxicon Off. J. Int. Soc. Toxinol. 2012, 60, 12–20. [Google Scholar]
- Barros, S.F.; Friedlanskaia, I.; Petricevich, V.L.; Kipnis, T.L. Local inflammation, lethality and cytokine release in mice injected with Bothrops atrox venom. Mediat. Inflamm. 1998, 7, 339–346. [Google Scholar]
- Menaldo, D.L.; Bernardes, C.P.; Zoccal, K.F.; Jacob-Ferreira, A.L.; Costa, T.R.; Del Lama, M.P.F.M. Immune cells and mediators involved in the inflammatory responses induced by a P-I metalloprotease and a phospholipase A2 from Bothrops atrox venom. Mol. Immunol. 2017, 85, 238–247. [Google Scholar]
- Clissa, P.B.; Laing, G.D.; Theakston, R.D.G.; Mota, I.; Taylor, M.J.; Moura-da-Silva, A.M. The effect of jararhagin, a metalloproteinase from Bothrops jararaca venom, on pro-inflammatory cytokines released by murine peritoneal adherent cells. Toxicon 2001, 39, 1567–1573. [Google Scholar]
- Wanderley, C.; Silva, C.; Wong, D.; Ximenes, R.; Morelo, D.; Cosker, F.; Aragão, K.; Fernandes, C.; Palheta-Júnior, R.; Havt, A.; et al. Bothrops jararacussu snake venom-induces a local inflammatory response in a prostanoid- and neutrophil-dependent manner. Toxicon Off. J. Int. Soc. Toxinol. 2014, 90, 134–147. [Google Scholar]


| Snake Species | Platelet Aggregation | Comments | |||
|---|---|---|---|---|---|
| No | Mild | Moderate | Marked | ||
| Normal | + | Mild platelet aggregation (2 colonies/field, small colonies) | |||
| B. gabonica | - | No platelet aggregation | |||
| B. arietans | - | No platelet aggregation | |||
| E. leucogaster | + | Mild platelet aggregation (2 colonies/field, small-medium colonies) | |||
| E. ocellatus | + | Mild/No platelet aggregation (<1 colonies/field, small colonies) | |||
| N. haje | + | One small (2–8 platelets/colony) colony per field | |||
| N. melanoleuca | +++ | Marked platelet aggregation (3–4 colonies/field, small, and medium colonies) | |||
| N. nigricollis | ++ | Moderate platelet aggregation (>2 colonies/field, small and medium colonies) | |||
| D. polylepis | ++ | Mild platelet aggregation (2–3 small colonies/field, medium and large colonies) | |||
| D. viridis | ++ | Mild platelet aggregation (3–4 colonies/field, small colonies) | |||
| D. jamesoni | +++ | Marked platelet aggregation (3–4 colonies/field, small, and medium colonies) | |||
| Normal | Low/Mild | High/Moderate | High +++/Marked | Low ++/+++/++++ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Marker of Venom Induced: | Assay(s) | Venoms from Echis and Bitis Viper Species | Venoms from Naja and Dendroaspis Elapid Species(#—Spitting Cobra) | ||||||||
| BG | BA | EL | EO | NH | NM | NN# | DP | DV | DJ | ||
| Human assays (ex vivo) | |||||||||||
| Changes to human blood parameters | Haemoglob-in | Low | Low ++++ | Normal | Low | Low ++++ | Low | Low ++++ | Low ++++ | Low ++++ | Low ++++ |
| Haemolysis | Normal | Normal | Normal | Normal | Normal | Normal | Marked | Normal | Normal | Normal | |
| Platelet aggregation | Low | Low ++++ | Low ++++ | High + | High ++ | Low | High +++ | High ++ | Low | Low | |
| Murine assays (in vivo) | |||||||||||
| Changes to blood cell counts, morpholo-gy, and platelets | Platelet aggregation | None | None | Mild | Mild | Mild | Marked | Moderate | Moderate | Mild | Marked |
| RBC morphology | Normal | ++ | Normal | Normal | Normal | Normal | + | Normal | Normal | + | |
| Total WBC | Low ++ | High | Low | Low | Low ++ | High | High | Low ++ | Low ++ | Low ++ | |
| Lymphocyt-es | Low + | Low | Low | Low | Low ++ | Low ++ | Low | Low ++ | Low | Low ++ | |
| Basophils | Low ++ | High | Low ++ | Low | Low ++ | Low | Normal | Low ++ | Low + | Low ++ | |
| Neutrophils | Normal | High + | Normal | Normal | Normal | High ++++ | High + | Normal | Normal | Normal | |
| Activation of acute phase and inflammat-ory responses | P-selectin | Low | Low +++ | Normal | Normal | High | High ++++ | High ++ | High | Normal | Normal |
| IgM | High + | Low ++ | Low ++ | Low | Low | Low | Normal | Low | Low + | Low ++ | |
| Haptoglob-in | Normal | Normal | Normal | Normal | Normal | High ++++ | High ++++ | Normal | Normal | Normal | |
| Serum Amyloid A | Low | High | Low | Low | Low | High ++++ | Normal | Low | Normal | Low | |
| Cytokines | Normal | Normal | Normal | Normal | Normal | Normal | IL6, ++ IL18TNF-α, IL13 | IFNg ++ | Normal | Normal | |
| Damage to kidney | Serum Creatinine | Low | Low | Low + | Low + | Low | High | Low | Low | Low | Low |
| Damage to liver function | Total serum protein | Normal | Low ++++ | Low | Normal | Low | Low | Normal | Normal | Normal | High |
| Serum Albumin | Normal | Low + | Normal | Normal | Normal | Low | Low | Normal | Normal | High | |
| Serum Bilirubin | High +++ | High + | High ++ | High + | Normal | Normal | High +++ | High + | High ++ | High + | |
| Serum ALT | Normal | Normal | Normal | Normal | Normal | Normal | High ++++ | Normal | Normal | Normal | |
| Damage to muscle | Serum CK | Normal | Normal | Normal | Normal | Normal | Normal | High ++++ | Normal | Normal | Normal |
| Serum LDH | Normal | Normal | Normal | Normal | Normal | High ++++ | High ++++ | Normal | Normal | Normal | |
| Serum AST | Normal | Normal | High | Normal | Normal | Normal | High ++++ | Normal | Normal | Normal | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsolaiss, J.; Evans, C.A.; Oluoch, G.O.; Casewell, N.R.; Harrison, R.A. Profiling the Murine Acute Phase and Inflammatory Responses to African Snake Venom: An Approach to Inform Acute Snakebite Pathology. Toxins 2022, 14, 229. https://doi.org/10.3390/toxins14040229
Alsolaiss J, Evans CA, Oluoch GO, Casewell NR, Harrison RA. Profiling the Murine Acute Phase and Inflammatory Responses to African Snake Venom: An Approach to Inform Acute Snakebite Pathology. Toxins. 2022; 14(4):229. https://doi.org/10.3390/toxins14040229
Chicago/Turabian StyleAlsolaiss, Jaffer, Chloe A. Evans, George O. Oluoch, Nicholas R. Casewell, and Robert A. Harrison. 2022. "Profiling the Murine Acute Phase and Inflammatory Responses to African Snake Venom: An Approach to Inform Acute Snakebite Pathology" Toxins 14, no. 4: 229. https://doi.org/10.3390/toxins14040229
APA StyleAlsolaiss, J., Evans, C. A., Oluoch, G. O., Casewell, N. R., & Harrison, R. A. (2022). Profiling the Murine Acute Phase and Inflammatory Responses to African Snake Venom: An Approach to Inform Acute Snakebite Pathology. Toxins, 14(4), 229. https://doi.org/10.3390/toxins14040229





