Chronic Kidney Disease-Associated Itch (CKD-aI) in Children—A Narrative Review
Abstract
1. Introduction
2. Pathogenesis of CKD-aI
2.1. Uraemic Toxins (UTs)
2.1.1. Free Water-Soluble Low Molecular Weight Molecules (LMWM)
2.1.2. Medium Molecules (MM)
β2-Microglobulin (β2-M)
Parathyroid Hormone (PTH)
Interleukin-6 (IL-6)
2.1.3. Protein-Bound Uraemic Toxins (PBUT)
Indoxyl Sulfate (IS)
p-Cresyl Sulfate (pCS)
PBUT and Their Role in Eliciting CKD-aI
2.2. Immune Dysfunction
2.3. Opioid Transmission
2.4. Infectious Agents
2.5. Skin Dryness (Xerosis)
2.6. Neuropathy
2.7. Dialysis Modality and Its Parameters
2.8. Other Factors
2.8.1. Vitamin A
2.8.2. Aluminium (Al)
2.8.3. Air Pollution
2.8.4. Protective Role of Loop Diuretics
3. Epidemiology and Clinical Picture of CKD-aI in Children
4. Management of CKD-aI in Children
4.1. Topical Therapy
4.2. Phototherapy
4.3. Systemic Therapy
4.3.1. H1-Antihistamines
4.3.2. Gabapentinoids
4.3.3. Ondansetron
4.4. Modalities Targeting PBUT
4.4.1. Reducing Production
4.4.2. Reducing Absorption
4.4.3. Increasing Clearance
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weisshaar, E.; Szepietowski, J.C.; Dalgard, F.J.; Garcovich, S.; Gieler, U.; Giménez-Arnau, A.M.; Lambert, J.; Leslie, T.; Mettang, T.; Misery, L.; et al. European S2k Guideline on Chronic Pruritus. Acta Derm. Venereol. 2019, 99, 469–506. [Google Scholar] [CrossRef]
- Ständer, S.; Weisshaar, E.; Mettang, T.; Szepietowski, J.C.; Carstens, E.; Ikoma, A.; Bergasa, N.V.; Gieler, U.; Misery, L.; Wallengren, J.; et al. Clinical classification of itch: A position paper of the International Forum for the Study of Itch. Acta Derm. Venereol. 2007, 87, 291–294. [Google Scholar] [CrossRef]
- Levey, A.S.; Eckardt, K.U.; Tsukamoto, Y.; Levin, A.; Coresh, J.; Rossert, J.; De Zeeuw, D.; Hostetter, T.H.; Lameire, N.; Eknoyan, G. Definition and classification of chronic kidney disease: A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005, 67, 2089–2100. [Google Scholar] [CrossRef]
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D. Global Prevalence of Chronic Kidney Disease—A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef]
- GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Mishra, O.P.; Rai, A.K.; Srivastava, P.; Pandey, K.; Abhinay, A.; Prasad, R.; Mishra, R.N.; Schaefer, F. Predictive ability of urinary biomarkers for outcome in children with acute kidney injury. Pediatr. Nephrol. 2017, 32, 521–527. [Google Scholar] [CrossRef]
- Harambat, J.; van Stralen, K.J.; Kim, J.J.; Tizard, E.J. Epidemiology of chronic kidney disease in children. Pediatr. Nephrol. 2012, 27, 363–373. [Google Scholar] [CrossRef]
- Kaspar, C.D.; Bholah, R.; Bunchman, T.E. A Review of Pediatric Chronic Kidney Disease. Blood Purif. 2016, 41, 211–217. [Google Scholar] [CrossRef]
- National Institute of Diabetes and Digestive and Kidney Diseases. Chronic Kidney Disease in Children Study: CKiD. Available online: https://www.niddk.nih.gov/about-niddk/research-areas/kidney-disease/chronic-kidney-disease-children-study-ckid (accessed on 30 April 2021).
- McDonald, S.P.; Craig, J.C.; Australian and New Zealand Paediatric Nephrology Association. Long-term survival of children with end-stage renal disease. N. Engl. J. Med. 2004, 350, 2654–2662. [Google Scholar] [CrossRef]
- Gerson, A.C.; Wentz, A.; Abraham, A.G.; Mendley, S.R.; Hooper, S.R.; Butler, R.W.; Gipson, D.S.; Lande, M.B.; Shinnar, S.; Moxey-Mims, M.M.; et al. Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics 2010, 125, e349–e357. [Google Scholar] [CrossRef]
- Marciano, R.C.; Soares, C.M.; Diniz, J.S.; Lima, E.M.; Silva, J.M.; Canhestro, M.R.; Gazzinelli, A.; Melo, C.C.; Dias, C.S.; Simões e Silva, A.C.; et al. Behavioral disorders and low quality of life in children and adolescents with chronic kidney disease. Pediatr. Nephrol. 2011, 26, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Kiliś-Pstrusińska, K.; Medyńska, A.; Chmielewska, I.B.; Grenda, R.; Kluska-Jóźwiak, A.; Leszczyńska, B.; Niedomagała, J.; Olszak-Szot, I.; Miklaszewska, M.; Szczepańska, M.; et al. Perception of health-related quality of life in children with chronic kidney disease by the patients and their caregivers: Multicentre national study results. Qual. Life Res. 2013, 22, 2889–2897. [Google Scholar] [CrossRef] [PubMed]
- Ständer, S.; Schäfer, I.; Phan, N.Q.; Blome, C.; Herberger, K.; Heigel, H.; Augustin, M. Prevalence of chronic pruritus in Germany: Results of a cross-sectional study in a sample working population of 11,730. Dermatology 2010, 221, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Matterne, U.; Apfelbacher, C.J.; Vogelgsang, L.; Loerbroks, A.; Weisshaar, E. Incidence and Determinants of Chronic Pruritus: A Population-based Cohort Study. Acta Derm. Venereol. 2013, 93, 532–537. [Google Scholar] [CrossRef]
- Amatya, B.; Wennersten, G.; Nordlind, K. Patients’ perspective of pruritus in chronic plaque psoriasis: A questionnaire-based study. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 822–826. [Google Scholar] [CrossRef]
- Kaaz, K.; Szepietowski, J.C.; Matusiak, Ł. Influence of Itch and Pain on Sleep Quality in Atopic Dermatitis and Psoriasis. Acta Derm. Venereol. 2019, 99, 175–180. [Google Scholar] [CrossRef]
- Dalgard, F.J.; Svensson, Å.; Halvorsen, J.A.; Gieler, U.; Schut, C.; Tomas-Aragones, L.; Lien, L.; Poot, F.; Jemec, G.B.E.; Misery, L.; et al. Itch and Mental Health in Dermatological Patients across Europe: A Cross-Sectional Study in 13 Countries. J. Investig. Dermatol. 2020, 140, 568–573. [Google Scholar] [CrossRef]
- Dimitrov, D.; Matusiak, Ł.; Szepietowski, J.C. Stigmatization in Arabic psoriatic patients in the United Arab Emirates—A cross sectional study. Postepy Dermatol. Alergol. 2019, 36, 425–430. [Google Scholar] [CrossRef]
- Sampogna, F.; Abeni, D.; Gieler, U.; Tomas-Aragones, L.; Lien, L.; Titeca, G.; Jemec, G.B.; Misery, L.; Szabó, C.; Linder, M.D.; et al. Impairment of Sexual Life in 3485 Dermatological Outpatients From a Multicentre Study in 13 European Countries. Acta Derm. Venereol. 2017, 97, 478–482. [Google Scholar] [CrossRef]
- Hawro, T.; Przybyłowicz, K.; Spindler, M.; Hawro, M.; Steć, M.; Altrichter, S.; Weller, K.; Magerl, M.; Reidel, U.; Alarbeed, E.; et al. The characteristics and impact of pruritus in adult dermatologic patients: A prospective, cross-sectional study. J. Am. Acad. Dermatol. 2021, 84, 691–700. [Google Scholar] [CrossRef]
- Pisoni, R.L.; Wikström, B.; Elder, S.J.; Akizawa, T.; Asano, Y.; Keen, M.L.; Saran, R.; Mendelssohn, D.C.; Young, E.W.; Port, F.K. Pruritus in haemodialysis patients: International results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol. Dial. Transplant. 2006, 21, 3495–3505. [Google Scholar] [CrossRef]
- Sukul, N.; Speyer, E.; Tu, C.; Bieber, B.A.; Li, Y.; Lopes, A.A.; Asahi, K.; Mariani, L.; Laville, M.; Rayner, H.C.; et al. Pruritus and Patient Reported Outcomes in Non-Dialysis CKD. Clin. J. Am. Soc. Nephrol. 2019, 14, 673–681. [Google Scholar] [CrossRef]
- Li, J.; Guo, Q.; Lin, J.; Yi, C.; Yang, X.; Yu, X. Prevalence and Associated Factors of Uraemic Pruritus in Continuous Ambulatory Peritoneal Dialysis Patients. Intern. Med. 2015, 54, 2827–2833. [Google Scholar] [CrossRef]
- Min, J.W.; Kim, S.H.; Kim, Y.O.; Jin, D.C.; Song, H.C.; Choi, E.J.; Kim, Y.L.; Kim, Y.S.; Kang, S.W.; Kim, N.H.; et al. Comparison of uremic pruritus between patients undergoing hemodialysis and peritoneal dialysis. Kidney Res. Clin. Pract. 2016, 35, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Panuccio, V.; Tripepi, R.; Bellantoni, M.; Saporito, L.; Quattrone, S.; Lacava, V.; Parlongo, G.; Tripepi, G.; Mallamaci, F.; Zoccali, C. Pruritus and quality of life in renal transplant patients. Clin. Transplant. 2017, 31. [Google Scholar] [CrossRef] [PubMed]
- Schricker, S.; Weisshaar, E.; Kupfer, J.; Mettang, T. Prevalence of Pruritus in a Single Cohort of Long-term Kidney Transplant Recipients. Acta Derm. Venereol. 2020, 100, adv00066. [Google Scholar] [CrossRef]
- Krajewski, P.K.; Olczyk, P.; Krajewska, M.; Krajewski, W.; Szepietowski, J.C. Clinical Characteristics of Itch in Renal Transplant Recipients. Front. Med. 2021, 7, 615334. [Google Scholar] [CrossRef]
- Murphy, E.L.; Murtagh, F.E.; Carey, I.; Sheerin, N.S. Understanding symptoms in patients with advanced chronic kidney disease managed without dialysis: use of a short patient-completed assessment tool. Nephron Clin. Pract. 2009, 111, c74–c80. [Google Scholar] [CrossRef]
- Solak, B.; Acikgoz, S.B.; Sipahi, S.; Erdem, T. Epidemiology and determinants of pruritus in pre-dialysis chronic kidney disease patients. Int. Urol. Nephrol. 2016, 48, 585–591. [Google Scholar] [CrossRef]
- David, T.J.; Wybrew, M.; Hennessen, U. Prodromal itching in childhood asthma. Lancet 1984, 2, 154–155. [Google Scholar] [CrossRef]
- Yerushalmi, B.; Sokol, R.J.; Narkewicz, M.R.; Smith, D.; Karrer, F.M. Use of rifampin for severe pruritus in children with chronic cholestasis. J. Pediatr. Gastroenterol. Nutr. 1999, 29, 442–447. [Google Scholar] [CrossRef]
- El-Karaksy, H.; Mansour, S.; El-Sayed, R.; El-Raziky, M.; El-Koofy, N.; Taha, G. Safety and efficacy of rifampicin in children with cholestatic pruritus. Indian J. Pediatr. 2007, 74, 279–281. [Google Scholar] [CrossRef]
- Ramachandran, P.; Shanmugam, N.P.; Sinani, S.A.; Shanmugam, V.; Srinivas, S.; Sathiyasekaran, M.; Tamilvanan, V.; Rela, M. Outcome of partial internal biliary diversion for intractable pruritus in children with cholestatic liver disease. Pediatr. Surg. Int. 2014, 30, 1045–1049. [Google Scholar] [CrossRef]
- Thébaut, A.; Habes, D.; Gottrand, F.; Rivet, C.; Cohen, J.; Debray, D.; Jacquemin, E.; Gonzales, E. Sertraline as an Additional Treatment for Cholestatic Pruritus in Children. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Van Vaisberg, V.; Tannuri, A.C.A.; Lima, F.R.; Tannuri, U. Ileal exclusion for pruritus treatment in children with progressive familial intrahepatic cholestasis and other cholestatic diseases. J. Pediatr. Surg. 2020, 55, 1385–1391. [Google Scholar] [CrossRef] [PubMed]
- Belzberg, M.; Larson, V.A.; Khanna, R.; Williams, K.A.; Semenov, Y.; Ständer, S.; Grossberg, A.L.; Kwatra, S.G. Association between Itch and Cancer in 3836 Pediatric Pruritus Patients at a Tertiary Care Center. Medicines 2019, 6, 99. [Google Scholar] [CrossRef]
- Stefaniak, A.A.; Zubkiewicz-Kucharska, A.; Matusiak, Ł.; Noczyńska, A.; Szepietowski, J.C. Itch in Children with Type 1 Diabetes: A Cross-Sectional Study. Dermatol. Ther. 2020, 10, 745–756. [Google Scholar] [CrossRef]
- Silverberg, N.B.; Singh, A.; Laude, T.A. Cutaneous manifestations of chronic renal failure in children of color. Pediatr. Dermatol. 2001, 18, 199–204. [Google Scholar] [CrossRef]
- Mettang, T.; Pauli-Magnus, C.; Alscher, D.M. Uraemic pruritus—New perspectives and insights from recent trials. Nephrol. Dial. Transplant. 2002, 17, 1558–1563. [Google Scholar] [CrossRef]
- Deshpande, P.V. Ondansetron for paediatric uraemic pruritus, a case report. Pediatr. Nephrol. 2004, 19, 694–696. [Google Scholar] [CrossRef]
- Senturk, N.; Ozkaya, O.; Aytekin, S.; Bek, K.; Açikgöz, Y.; Aydin, F.; Bek, Y.; Turanli, A.Y. Characteristics of pruritus in children on peritoneal dialysis. Nephron Clin. Pract. 2008, 109, c168–c172. [Google Scholar] [CrossRef]
- Attia, E.A.; Hassan, S.I.; Youssef, N.M. Cutaneous disorders in uremic patients on hemodialysis: An Egyptian case-controlled study. Int. J. Dermatol. 2010, 49, 1024–1030. [Google Scholar] [CrossRef] [PubMed]
- Wojtowicz-Prus, E.; Kiliś-Pstrusińska, K.; Reich, A.; Zachwieja, K.; Miklaszewska, M.; Szczepanska, M.; Szepietowski, J.C. Chronic Kidney Disease-associated Pruritus in Children. Acta Derm. Venereol. 2016, 96, 938–942. [Google Scholar] [CrossRef]
- The European Uremic Toxins (EUTox) Database. Available online: https://database.uremic-toxins.org/home.php (accessed on 30 April 2021).
- Meyer, T.W.; Hostetter, T.H. Uremia. N. Engl. J. Med. 2007, 357, 1316–1325. [Google Scholar] [CrossRef]
- Duranton, F.; Cohen, G.; De Smet, R.; Rodriguez, M.; Jankowski, J.; Vanholder, R.; Argiles, A.; European Uremic Toxin Work Group. Normal and pathologic concentrations of uremic toxins. J. Am. Soc. Nephrol. 2012, 23, 1258–1270. [Google Scholar] [CrossRef] [PubMed]
- Clark, W.R.; Dehghani, N.L.; Narsimhan, V.; Ronco, C. Uremic Toxins and their Relation to Dialysis Efficacy. Blood Purif. 2019, 48, 299–314. [Google Scholar] [CrossRef] [PubMed]
- Snauwaert, E.; Van Biesen, W.; Raes, A.; Glorieux, G.; Vanholder, R.; Vande Walle, J.; Eloot, S. A plea for more uremic toxin research in children with chronic kidney disease. Pediatr. Nephrol. 2018, 33, 921–924. [Google Scholar] [CrossRef] [PubMed]
- Snauwaert, E.; Van Biesen, W.; Raes, A.; Glorieux, G.; Van Bogaert, V.; Van Hoeck, K.; Coppens, M.; Roels, S.; Vande Walle, J.; Eloot, S. Concentrations of representative uraemic toxins in a healthy versus non-dialysis chronic kidney disease paediatric population. Nephrol. Dial. Transplant. 2018, 33, 978–986. [Google Scholar] [CrossRef]
- Snauwaert, E.; Van Biesen, W.; Raes, A.; Holvoet, E.; Glorieux, G.; Van Hoeck, K.; Van Dyck, M.; Godefroid, N.; Vanholder, R.; Roels, S.; et al. Accumulation of uraemic toxins is reflected only partially by estimated GFR in paediatric patients with chronic kidney disease. Pediatr. Nephrol. 2018, 33, 315–323. [Google Scholar] [CrossRef]
- Snauwaert, E.; Holvoet, E.; Van Biesen, W.; Raes, A.; Glorieux, G.; Vande Walle, J.; Roels, S.; Vanholder, R.; Askiti, V.; Azukaitis, K.; et al. Uremic Toxin Concentrations are Related to Residual Kidney Function in the Pediatric Hemodialysis Population. Toxins 2019, 11, 235. [Google Scholar] [CrossRef]
- Snauwaert, E.; Van Biesen, W.; Raes, A.; Glorieux, G.; Vande Walle, J.; Roels, S.; Vanholder, R.; Askiti, V.; Azukaitis, K.; Bayazit, A.; et al. Haemodiafiltration does not lower protein-bound uraemic toxin levels compared with haemodialysis in a paediatric population. Nephrol. Dial. Transplant. 2020, 35, 648–656. [Google Scholar] [CrossRef] [PubMed]
- Holle, J.; Querfeld, U.; Kirchner, M.; Anninos, A.; Okun, J.; Thurn-Valsassina, D.; Bayazit, A.; Niemirska, A.; Canpolat, N.; Bulut, I.K.; et al. Indoxyl sulfate associates with cardiovascular phenotype in children with chronic kidney disease. Pediatr. Nephrol. 2019, 34, 2571–2582. [Google Scholar] [CrossRef] [PubMed]
- Holle, J.; Kirchner, M.; Okun, J.; Bayazit, A.K.; Obrycki, L.; Canpolat, N.; Bulut, I.K.; Azukaitis, K.; Duzova, A.; Ranchin, B.; et al. Serum indoxyl sulfate concentrations associate with progression of chronic kidney disease in children. PLoS ONE 2020, 15, e0240446. [Google Scholar] [CrossRef]
- El Amouri, A.; Snauwaert, E.; Foulon, A.; Vande Moortel, C.; Van Dyck, M.; Van Hoeck, K.; Godefroid, N.; Glorieux, G.; Van Biesen, W.; Vande Walle, J.; et al. Dietary Fibre Intake Is Associated with Serum Levels of Uraemic Toxins in Children with Chronic Kidney Disease. Toxins 2021, 13, 225. [Google Scholar] [CrossRef]
- Vanholder, R.; De Smet, R.; Glorieux, G.; Argilés, A.; Baurmeister, U.; Brunet, P.; Clark, W.; Cohen, G.; De Deyn, P.P.; Deppisch, R.; et al. Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int. 2003, 63, 1934–1943. [Google Scholar] [CrossRef]
- Bellomo, G. Uric acid and chronic kidney disease: A time to act? World J. Nephrol. 2013, 2, 17–25. [Google Scholar] [CrossRef]
- Oh, T.R.; Choi, H.S.; Kim, C.S.; Bae, E.H.; Ma, S.K.; Sung, S.A.; Kim, Y.S.; Oh, K.H.; Ahn, C.; Kim, S.W. Hyperuricemia has increased the risk of progression of chronic kidney disease: Propensity score matching analysis from the KNOW-CKD study. Sci. Rep. 2019, 9, 6681. [Google Scholar] [CrossRef]
- Srivastava, A.; Kaze, A.D.; McMullan, C.J.; Isakova, T.; Waikar, S.S. Uric Acid and the Risks of Kidney Failure and Death in Individuals With CKD. Am. J. Kidney Dis. 2018, 71, 362–370. [Google Scholar] [CrossRef]
- Rodenbach, K.E.; Schneider, M.F.; Furth, S.L.; Moxey-Mims, M.M.; Mitsnefes, M.M.; Weaver, D.J.; Warady, B.A.; Schwartz, G.J. Hyperuricemia and Progression of CKD in Children and Adolescents: The Chronic Kidney Disease in Children (CKiD) Cohort Study. Am. J. Kidney Dis. 2015, 66, 984–992. [Google Scholar] [CrossRef]
- Wang, C.P.; Lu, Y.C.; Tsai, I.T.; Tang, W.H.; Hsu, C.C.; Hung, W.C.; Yu, T.H.; Chen, S.C.; Chung, F.M.; Lee, Y.J.; et al. Increased Levels of Total p-Cresylsulfate Are Associated with Pruritus in Patients with Chronic Kidney Disease. Dermatology 2016, 232, 363–370. [Google Scholar] [CrossRef]
- Noh, S.H.; Park, K.; Kim, E.J. The Incidence of Pruritus and Biochemical Marker Associated with Pruritus in Hemodialysis Patients. Ann. Dermatol. 2018, 30, 473–475. [Google Scholar] [CrossRef] [PubMed]
- Chmielewski, M.; Cohen, G.; Wiecek, A.; Jesús Carrero, J. The peptidic middle molecules: Is molecular weight doing the trick? Semin. Nephrol. 2014, 34, 118–134. [Google Scholar] [CrossRef]
- Zügel, U.; Schoel, B.; Kaufmann, S.H. Beta 2-microglobulin independent presentation of exogenously added foreign peptide and endogenous self-epitope by MHC class I alpha-chain to a cross-reactive CD8+ CTL clone. J. Immunol. 1994, 153, 4070–4080. [Google Scholar]
- Drüeke, T.B.; Massy, Z.A. Beta2-microglobulin. Semin. Dial. 2009, 22, 378–380. [Google Scholar] [CrossRef]
- Gejyo, F.; Odani, S.; Yamada, T.; Honma, N.; Saito, H.; Suzuki, Y.; Nakagawa, Y.; Kobayashi, H.; Maruyama, Y.; Hirasawa, Y.; et al. Beta 2-microglobulin: A new form of amyloid protein associated with chronic hemodialysis. Kidney Int. 1986, 30, 385–390. [Google Scholar] [CrossRef]
- Wu, H.C.; Lee, L.C.; Wang, W.J. Associations among Serum Beta 2 Microglobulin, Malnutrition, Inflammation, and Advanced Cardiovascular Event in Patients with Chronic Kidney Disease. J. Clin. Lab. Anal. 2017, 31, e22056. [Google Scholar] [CrossRef]
- Liabeuf, S.; Lenglet, A.; Desjardins, L.; Neirynck, N.; Glorieux, G.; Lemke, H.D.; Vanholder, R.; Diouf, M.; Choukroun, G.; Massy, Z.A.; et al. Plasma beta-2 microglobulin is associated with cardiovascular disease in uremic patients. Kidney Int. 2012, 82, 1297–1303. [Google Scholar] [CrossRef]
- Cheung, A.K.; Greene, T.; Leypoldt, J.K.; Yan, G.; Allon, M.; Delmez, J.; Levey, A.S.; Levin, N.W.; Rocco, M.V.; Schulman, G.; et al. Association between Serum β2-Microglobulin Level and Infectious Mortality in Hemodialysis Patients. Clin. J. Am. Soc. Nephrol. 2008, 3, 69–77. [Google Scholar] [CrossRef]
- Okuno, S.; Ishimura, E.; Kohno, K.; Fujino-Katoh, Y.; Maeno, Y.; Yamakawa, T.; Inaba, M.; Nishizawa, Y. Serum β 2 -microglobulin level is a significant predictor of mortality in maintenance haemodialysis patients. Nephrol. Dial. Transplant. 2009, 24, 571–577. [Google Scholar] [CrossRef]
- Foster, M.C.; Coresh, J.; Hsu, C.Y.; Xie, D.; Levey, A.S.; Nelson, R.G.; Eckfeldt, J.H.; Vasan, R.S.; Kimmel, P.L.; Schelling, J.; et al. Serum β-Trace Protein and β2-Microglobulin as Predictors of ESRD, Mortality, and Cardiovascular Disease in Adults With CKD in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am. J. Kidney. Dis. 2016, 68, 68–76. [Google Scholar] [CrossRef]
- Argyropoulos, C.P.; Chen, S.S.; Ng, Y.H.; Roumelioti, M.E.; Shaffi, K.; Singh, P.P.; Tzamaloukas, A.H. Rediscovering Beta-2 Microglobulin As a Biomarker across the Spectrum of Kidney Diseases. Front. Med. 2017, 4, 73. [Google Scholar] [CrossRef]
- Narita, I.; Alchi, B.; Omori, K.; Sato, F.; Ajiro, J.; Saga, D.; Kondo, D.; Skatsume, M.; Maruyama, S.; Kazama, J.J.; et al. Etiology and prognostic significance of severe uremic pruritus in chronic hemodialysis patients. Kidney Int. 2006, 69, 1626–1632. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.J.; Cao, G.; Tang, W.X.; Lv, X.Y.; Huang, S.M.; Qin, W.; Ping, F.; Ye, T. A randomized controlled trial of high-permeability haemodialysis against conventional haemodialysis in the treatment of uraemic pruritus. Clin. Exp. Dermatol. 2009, 34, 679–683. [Google Scholar] [CrossRef] [PubMed]
- Melo, N.C.; Elias, R.M.; Castro, M.C.; Romao, J.E., Jr.; Abensur, H. Pruritus in hemodialysis patients: The problem remains. Hemodial. Int. 2009, 13, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Assounga, A.G.; Bascoul, S.; Canaud, B.; Bouya, P.A.; Vendrell, J.P.; Sciolla, J.P.; Mourad, G.; Baldet, P.; Serre, A.; Mion, C. A study of beta 2-microglobulin skin deposits in dialyzed patients and healthy controls. Am. J. Kidney Dis. 1990, 15, 556–561. [Google Scholar] [CrossRef]
- Andoh, T.; Maki, T.; Li, S.; Uta, D. β2-Microglobulin elicits itch-related responses in mice through the direct activation of primary afferent neurons expressing transient receptor potential vanilloid 1. Eur. J. Pharmacol. 2017, 810, 134–140. [Google Scholar] [CrossRef]
- Goltzman, D. Physiology of Parathyroid Hormone. Front. Horm. Res. 2018, 50, 1–13. [Google Scholar] [CrossRef]
- Tageldin, N.; Martin, A. Thyroid, parathyroid hormones and calcium homeostasis. Physiology 2020, 21, 599–603. [Google Scholar] [CrossRef]
- Rodríguez-Ortiz, M.E.; Rodríguez, M. Recent advances in understanding and managing secondary hyperparathyroidism in chronic kidney disease. F1000Research 2020, 9, F1000. [Google Scholar] [CrossRef]
- Wesseling-Perry, K. Bone disease in pediatric chronic kidney disease. Pediatr. Nephrol. 2013, 28, 569–576. [Google Scholar] [CrossRef]
- Massry, S.G.; Popovtzer, M.M.; Coburn, J.W.; Makoff, D.L.; Maxwell, M.H.; Kleeman, C.R. Intractable pruritus as a manifestation of secondary hyperparathyroidism in uremia. Disappearance of itching after subtotal parathyroidectomy. N. Engl. J. Med. 1968, 279, 697–700. [Google Scholar] [CrossRef]
- Chou, F.F.; Ho, J.C.; Huang, S.C.; Sheen-Chen, S.M. A study on pruritus after parathyroidectomy for secondary hyperparathyroidism. J. Am. Coll. Surg. 2000, 190, 65–70. [Google Scholar] [CrossRef]
- Makhlough, A.; Emadi, N.; Sedighi, O.; Khademloo, M.; Bicmohamadi, A.R. Relationship between serum intact parathyroid hormone and pruritus in hemodialysis patients. Iran. J. Kidney Dis. 2013, 7, 42–46. [Google Scholar]
- Śnit, M.; Gawlik, R.; Łącka-Gaździk, B.; Kuźniewicz, R.; Dwornicki, M.; Owczarek, A.; Walaszczyk, M.; Grabiec, P.; Grzeszczak, W. Substance P and intensity of pruritus in hemodialysis and peritoneal dialysis patients. Med. Sci. Monit. 2013, 19, 723–732. [Google Scholar] [CrossRef][Green Version]
- Cho, Y.L.; Liu, H.N.; Huang, T.P.; Tarng, D.C. Uremic pruritus: Roles of parathyroid hormone and substance P. J. Am. Acad. Dermatol. 1997, 36, 538–543. [Google Scholar] [CrossRef]
- Akhyani, M.; Ganji, M.R.; Samadi, N.; Khamesan, B.; Daneshpazhooh, M. Pruritus in hemodialysis patients. BMC Dermatol. 2005, 5, 7. [Google Scholar] [CrossRef]
- Duque, M.I.; Thevarajah, S.; Chan, Y.H.; Tuttle, A.B.; Freedman, B.I.; Yosipovitch, G. Uremic pruritus is associated with higher kt/V and serum calcium concentration. Clin. Nephrol. 2006, 66, 184–191. [Google Scholar] [CrossRef]
- Ståhle-Bäckdahl, M.; Hägermark, O.; Lins, L.E.; Törring, O.; Hilliges, M.; Johansson, O. Experimental and immunohistochemical studies on the possible role of parathyroid hormone in uraemic pruritus. J. Intern. Med. 1989, 225, 411–415. [Google Scholar] [CrossRef]
- Momose, A.; Kudo, S.; Sato, M.; Saito, H.; Nagai, K.; Katabira, Y.; Funyu, T. Calcium ions are abnormally distributed in the skin of haemodialysis patients with uraemic pruritus. Nephrol. Dial. Transplant. 2004, 19, 2061–2066. [Google Scholar] [CrossRef]
- Scheller, J.; Rose-John, S. Interleukin-6 and its receptor: From bench to bedside. Med. Microbiol. Immunol. 2006, 195, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Rose-John, S. Interleukin-6 Family Cytokines. Cold Spring Harb. Perspect. Biol. 2018, 10, a028415. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.; Rose-John, S.; Garbers, C. Interleukin-6 and its receptors: A highly regulated and dynamic system. Cytokine 2014, 70, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.L.; Vignali, D.A. Molecular interactions within the IL-6/IL-12 cytokine/receptor superfamily. Immunol. Res. 2011, 51, 5–14. [Google Scholar] [CrossRef]
- Gupta, J.; Mitra, N.; Kanetsky, P.A.; Devaney, J.; Wing, M.R.; Reilly, M.; Shah, V.O.; Balakrishnan, V.S.; Guzman, N.J.; Girndt, M.; et al. Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC. Clin. J. Am. Soc. Nephrol. 2012, 7, 1938–1946. [Google Scholar] [CrossRef]
- Amdur, R.L.; Feldman, H.I.; Gupta, J.; Yang, W.; Kanetsky, P.; Shlipak, M.; Rahman, M.; Lash, J.P.; Townsend, R.R.; Ojo, A.; et al. Inflammation and Progression of CKD: The CRIC Study. Clin. J. Am. Soc. Nephrol. 2016, 11, 1546–1556. [Google Scholar] [CrossRef]
- Pecoits-Filho, R.; Bárány, P.; Lindholm, B.; Heimbürger, O.; Stenvinkel, P. Interleukin-6 is an independent predictor of mortality in patients starting dialysis treatment. Nephrol. Dial. Transplant. 2002, 17, 1684–1688. [Google Scholar] [CrossRef]
- Sun, J.; Axelsson, J.; Machowska, A.; Heimbürger, O.; Bárány, P.; Lindholm, B.; Lindström, K.; Stenvinkel, P.; Qureshi, A.R. Biomarkers of Cardiovascular Disease and Mortality Risk in Patients with Advanced CKD. Clin. J. Am. Soc. Nephrol. 2016, 11, 1163–1172. [Google Scholar] [CrossRef]
- Simmons, E.M.; Langone, A.; Sezer, M.T.; Vella, J.P.; Recupero, P.; Morrow, J.D.; Ikizler, T.A.; Himmelfarb, J. Effect of renal transplantation on biomarkers of inflammation and oxidative stress in end-stage renal disease patients. Transplantation 2005, 79, 914–919. [Google Scholar] [CrossRef]
- Akchurin, O.; Patino, E.; Dalal, V.; Meza, K.; Bhatia, D.; Brovender, S.; Zhu, Y.S.; Cunningham-Rundles, S.; Perelstein, E.; Kumar, J.; et al. Interleukin-6 Contributes to the Development of Anemia in Juvenile CKD. Kidney Int. Rep. 2018, 4, 470–483. [Google Scholar] [CrossRef]
- Sánchez Hernández, K.V.; Larrosa-Haro, A.; González Hita, M.; Martín Del Campo López, F.; Chávez Palencia, C.; Pérez Cortez, G.; Sandoval Pamplona, J.; Rivera León, É. Interleukine 6 and C-reactive protein predict growth impairment and acute malnutrition in children and adolescents with chronic kidney disease. Nutr. Hosp. 2019, 36, 1248–1253. [Google Scholar] [CrossRef]
- Panahi, Y.; Davoudi, S.M.; Beiraghdar, F.; Amiri, M.; Saadat, A.; Marzony, E.T.; Naghizadeh, M.M.; Sahebkar, A. Serum levels of interleukins 2, 4, 6, and 10 in veterans with chronic sulfur mustard-induced pruritus: A cross-sectional study. Skinmed 2013, 11, 205–209. [Google Scholar]
- Konda, D.; Chandrashekar, L.; Rajappa, M.; Kattimani, S.; Thappa, D.M.; Ananthanarayanan, P.H. Serotonin and interleukin-6: Association with pruritus severity, sleep quality and depression severity in Prurigo Nodularis. Asian J. Psychiatr. 2015, 17, 24–28. [Google Scholar] [CrossRef]
- Kimmel, M.; Alscher, D.M.; Dunst, R.; Braun, N.; Machleidt, C.; Kiefer, T.; Stülten, C.; van der Kuip, H.; Pauli-Magnus, C.; Raub, U.; et al. The role of micro-inflammation in the pathogenesis of uraemic pruritus in haemodialysis patients. Nephrol. Dial. Transplant. 2006, 21, 749–755. [Google Scholar] [CrossRef]
- Schricker, S.; Heider, T.; Schanz, M.; Dippon, J.; Alscher, M.D.; Weiss, H.; Mettang, T.; Kimmel, M. Strong Associations Between Inflammation, Pruritus and Mental Health in Dialysis Patients. Acta Derm. Venereol. 2019, 99, 524–529. [Google Scholar] [CrossRef]
- Taraz, M.; Khatami, M.R.; Gharekhani, A.; Abdollahi, A.; Khalili, H.; Dashti-Khavidaki, S. Relationship between a pro- and anti-inflammatory cytokine imbalance and depression in haemodialysis patients. Eur. Cytokine Netw. 2012, 23, 179–186. [Google Scholar] [CrossRef]
- Liu, Y.; Ho, R.C.; Mak, A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: A meta-analysis and meta-regression. J. Affect. Disord. 2012, 139, 230–239. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Hayashino, Y.; Yamazaki, S.; Akiba, T.; Akizawa, T.; Asano, Y.; Saito, A.; Kurokawa, K.; Miyachi, Y.; Fukuhara, S.; et al. Depressive symptoms predict the future risk of severe pruritus in haemodialysis patients: Japan Dialysis Outcomes and Practice Patterns Study. Br. J. Dermatol. 2009, 161, 384–389. [Google Scholar] [CrossRef]
- Kogon, A.J.; Matheson, M.B.; Flynn, J.T.; Gerson, A.C.; Warady, B.A.; Furth, S.L.; Hooper, S.R.; Chronic Kidney Disease in Children (CKiD) Study Group. Depressive symptoms in children with chronic kidney disease. J. Pediatr. 2016, 168, 164–170.e1. [Google Scholar] [CrossRef]
- Kogon, A.J.; Kim, J.Y.; Laney, N.; Radcliffe, J.; Hooper, S.R.; Furth, S.L.; Hartung, E.A. Depression and neurocognitive dysfunction in pediatric and young adult chronic kidney disease. Pediatr. Nephrol. 2019, 34, 1575–1582. [Google Scholar] [CrossRef] [PubMed]
- Vanholder, R.; Schepers, E.; Pletinck, A.; Neirynck, N.; Glorieux, G. An update on protein-bound uremic retention solutes. J. Ren. Nutr. 2012, 22, 90–94. [Google Scholar] [CrossRef]
- Meijers, B.K.; Evenepoel, P. The gut-kidney axis: Indoxyl sulfate, p-cresyl sulfate and CKD progression. Nephrol. Dial. Transplant. 2011, 26, 759–761. [Google Scholar] [CrossRef]
- Sirich, T.L.; Meyerm, T.W.; Gondouin, B.; Brunet, P.; Niwa, T. Protein-bound molecules: A large family with a bad character. Semin. Nephrol. 2014, 34, 106–117. [Google Scholar] [CrossRef]
- Rysz, J.; Franczyk, B.; Ławiński, J.; Olszewski, R.; Ciałkowska-Rysz, A.; Gluba-Brzózka, A. The Impact of CKD on Uremic Toxins and Gut Microbiota. Toxins 2021, 13, 252. [Google Scholar] [CrossRef]
- Gryp, T.; Huys, G.R.B.; Joossens, M.; Van Biesen, W.; Glorieux, G.; Vaneechoutte, M. Isolation and Quantification of Uremic Toxin Precursor-Generating Gut Bacteria in Chronic Kidney Disease Patients. Int. J. Mol. Sci. 2020, 21, 1986. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.J.; Chen, H.H.; Pan, C.F.; Chuang, C.K.; Wang, T.J.; Sun, F.J.; Wu, C.J. p-Cresylsulfate and indoxyl sulfate level at different stages of chronic kidney disease. J. Clin. Lab. Anal. 2011, 25, 191–197. [Google Scholar] [CrossRef]
- Leong, S.C.; Sirich, T.L. Indoxyl Sulfate-Review of Toxicity and Therapeutic Strategies. Toxins 2016, 8, 358. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.J.; Liou, T.C.; Pan, C.F.; Wu, P.C.; Sun, F.J.; Liu, H.L.; Chen, H.H.; Wu, C.J. The Role of Liver in Determining Serum Colon-Derived Uremic Solutes. PLoS ONE 2015, 10, e0134590. [Google Scholar] [CrossRef]
- Wu, W.; Bush, K.T.; Nigam, S.K. Key Role for the Organic Anion Transporters, OAT1 and OAT3, in the in vivo Handling of Uremic Toxins and Solutes. Sci. Rep. 2017, 7, 4939. [Google Scholar] [CrossRef] [PubMed]
- Niwa, T. Uremic toxicity of indoxyl sulfate. Nagoya J. Med. Sci. 2010, 72, 1–11. [Google Scholar]
- Miyazaki, T.; Ise, M.; Seo, H.; Niwa, T. Indoxyl sulfate increases the gene expressions of TGF-beta 1, TIMP-1 and pro-alpha 1(I) collagen in uremic rat kidneys. Kidney Int. Suppl. 1997, 62, S15–S22. [Google Scholar]
- Shimizu, H.; Bolati, D.; Adijiang, A.; Enomoto, A.; Nishijima, F.; Dateki, M.; Niwa, T. Senescence and dysfunction of proximal tubular cells are associated with activated p53 expression by indoxyl sulfate. Am. J. Physiol. Cell Physiol. 2010, 299, C1110–C1117. [Google Scholar] [CrossRef]
- Li, S.; Cheng, S.; Sun, Z.; Mungun, H.K.; Gong, W.; Yu, J.; Xia, W.; Zhang, Y.; Huang, S.; Zhang, A.; et al. Indoxyl Sulfate Induces Mesangial Cell Proliferation via the Induction of COX-2. Mediat. Inflamm. 2016, 2016, 5802973. [Google Scholar] [CrossRef]
- Motojima, M.; Hosokawa, A.; Yamato, H.; Muraki, T.; Yoshioka, T. Uremic toxins of organic anions up-regulate PAI-1 expression by induction of NF-kappaB and free radical in proximal tubular cells. Kidney Int. 2003, 63, 1671–1680. [Google Scholar] [CrossRef] [PubMed]
- Gelasco, A.K.; Raymond, J.R. Indoxyl sulfate induces complex redox alterations in mesangial cells. Am. J. Physiol. Ren. Physiol. 2006, 290, F1551–F1558. [Google Scholar] [CrossRef] [PubMed]
- Owada, S.; Goto, S.; Bannai, K.; Hayashi, H.; Nishijima, F.; Niwa, T. Indoxyl sulfate reduces superoxide scavenging activity in the kidneys of normal and uremic rats. Am. J. Nephrol. 2008, 28, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Tumur, Z.; Shimizu, H.; Enomoto, A.; Miyazaki, H.; Niwa, T. Indoxyl sulfate upregulates expression of ICAM-1 and MCP-1 by oxidative stress-induced NF-kappaB activation. Am. J. Nephrol. 2010, 31, 435–441. [Google Scholar] [CrossRef]
- Yu, M.; Kim, Y.J.; Kang, D.H. Indoxyl sulfate-induced endothelial dysfunction in patients with chronic kidney disease via an induction of oxidative stress. Clin. J. Am. Soc. Nephrol. 2011, 6, 30–39. [Google Scholar] [CrossRef]
- Adesso, S.; Popolo, A.; Bianco, G.; Sorrentino, R.; Pinto, A.; Autore, G.; Marzocco, S. The uremic toxin indoxyl sulphate enhances macrophage response to LPS. PLoS ONE 2013, 8, e76778. [Google Scholar] [CrossRef]
- Rapa, S.F.; Prisco, F.; Popolo, A.; Iovane, V.; Autore, G.; Di Iorio, B.R.; Dal Piaz, F.; Paciello, O.; Nishijima, F.; Marzocco, S. Pro-Inflammatory Effects of Indoxyl Sulfate in Mice: Impairment of Intestinal Homeostasis and Immune Response. Int. J. Mol. Sci. 2021, 22, 1135. [Google Scholar] [CrossRef]
- Matsuo, K.; Yamamoto, S.; Wakamatsu, T.; Takahashi, Y.; Kawamura, K.; Kaneko, Y.; Goto, S.; Kazama, J.J.; Narita, I. Increased Proinflammatory Cytokine Production and Decreased Cholesterol Efflux Due to Downregulation of ABCG1 in Macrophages Exposed to Indoxyl Sulfate. Toxins 2015, 7, 3155–3166. [Google Scholar] [CrossRef]
- Wakamatsu, T.; Yamamoto, S.; Ito, T.; Sato, Y.; Matsuo, K.; Takahashi, Y.; Kaneko, Y.; Goto, S.; Kazama, J.J.; Gejyo, F.; et al. Indoxyl Sulfate Promotes Macrophage IL-1β Production by Activating Aryl Hydrocarbon Receptor/NF-κ/MAPK Cascades, but the NLRP3 inflammasome Was Not Activated. Toxins 2018, 10, 124. [Google Scholar] [CrossRef]
- Nakano, T.; Katsuki, S.; Chen, M.; Decano, J.L.; Halu, A.; Lee, L.H.; Pestana, D.V.S.; Kum, A.S.T.; Kuromoto, R.K.; Golden, W.S.; et al. Uremic Toxin Indoxyl Sulfate Promotes Proinflammatory Macrophage Activation Via the Interplay of OATP2B1 and Dll4-Notch Signaling. Circulation 2019, 139, 78–96. [Google Scholar] [CrossRef]
- Barreto, F.C.; Barreto, D.V.; Liabeuf, S.; Meert, N.; Glorieux, G.; Temmar, M.; Choukroun, G.; Vanholder, R.; Massy, Z.A.; European Uremic Toxin Work Group (EUTox). Serum indoxyl sulfate is associated with vascular disease and mortality in chronic kidney disease patients. Clin. J. Am. Soc. Nephrol. 2009, 4, 1551–1558. [Google Scholar] [CrossRef] [PubMed]
- Wu, I.W.; Hsu, K.H.; Lee, C.C.; Sun, C.Y.; Hsu, H.J.; Tsai, C.J.; Tzen, C.Y.; Wang, Y.C.; Lin, C.Y.; Wu, M.S. p-Cresyl sulphate and indoxyl sulphate predict progression of chronic kidney disease. Nephrol. Dial. Transplant. 2011, 26, 938–947. [Google Scholar] [CrossRef] [PubMed]
- Kamiński, T.W.; Pawlak, K.; Karbowska, M.; Myśliwiec, M.; Pawlak, D. Indoxyl sulfate—The uremic toxin linking hemostatic system disturbances with the prevalence of cardiovascular disease in patients with chronic kidney disease. BMC Nephrol. 2017, 18, 35. [Google Scholar] [CrossRef]
- Fan, P.C.; Chang, J.C.; Lin, C.N.; Lee, C.C.; Chen, Y.T.; Chu, P.H.; Kou, G.; Lu, Y.A.; Yang, C.W.; Chen, Y.C. Serum indoxyl sulfate predicts adverse cardiovascular events in patients with chronic kidney disease. J. Formos. Med. Assoc. 2019, 118, 1099–1106. [Google Scholar] [CrossRef] [PubMed]
- Opdebeeck, B.; Maudsley, S.; Azmi, A.; De Maré, A.; De Leger, W.; Meijers, B.; Verhulst, A.; Evenepoel, P.; D’Haese, P.C.; Neven, E. Indoxyl Sulfate and p-Cresyl Sulfate Promote Vascular Calcification and Associate with Glucose Intolerance. J. Am. Soc. Nephrol. 2019, 30, 751–766. [Google Scholar] [CrossRef]
- Yamamoto, S.; Fuller, D.S.; Komaba, H.; Nomura, T.; Massy, Z.A.; Bieber, B.; Robinson, B.; Pisoni, R.; Fukagawa, M. Serum total indoxyl sulfate and clinical outcomes in hemodialysis patients: Results from the Japan Dialysis Outcomes and Practice Patterns Study. Clin. Kidney J. 2020, 14, 1236–1243. [Google Scholar] [CrossRef]
- Gryp, T.; Vanholder, R.; Vaneechoutte, M.; Glorieux, G. p-Cresyl Sulfate. Toxins 2017, 9, 52. [Google Scholar] [CrossRef]
- Rong, Y.; Kiang, T.K.L. Characterizations of Human UDP-Glucuronosyltransferase Enzymes in the Conjugation of p-Cresol. Toxicol. Sci. 2020, 176, 285–296. [Google Scholar] [CrossRef]
- Poesen, R.; Viaene, L.; Verbeke, K.; Claes, K.; Bammens, B.; Sprangers, B.; Naesens, M.; Vanrenterghem, Y.; Kuypers, D.; Evenepoel, P.; et al. Renal clearance and intestinal generation of p-cresyl sulfate and indoxyl sulfate in CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 1508–1514. [Google Scholar] [CrossRef]
- Mutsaers, H.A.; Caetano-Pinto, P.; Seegers, A.E.; Dankers, A.C.; van den Broek, P.H.; Wetzels, J.F.; van den Brand, J.A.; van den Heuvel, L.P.; Hoenderop, J.G.; Wilmer, M.J.; et al. Proximal tubular efflux transporters involved in renal excretion of p-cresyl sulfate and p-cresyl glucuronide: Implications for chronic kidney disease pathophysiology. Toxicol. In Vitro 2015, 29, 1868–1877. [Google Scholar] [CrossRef]
- Watanabe, H.; Miyamoto, Y.; Honda, D.; Tanaka, H.; Wu, Q.; Endo, M.; Noguchi, T.; Kadowaki, D.; Ishima, Y.; Kotani, S.; et al. p-Cresyl sulfate causes renal tubular cell damage by inducing oxidative stress by activation of NADPH oxidase. Kidney Int. 2013, 83, 582–592. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, M.L.; Bonan, N.B.; Dias, G.; Brehm, F.; Steiner, T.M.; Souza, W.M.; Stinghen, A.E.; Barreto, F.C.; Elifio-Esposito, S.; Pecoits-Filho, R.; et al. p-Cresyl sulfate affects the oxidative burst, phagocytosis process, and antigen presentation of monocyte-derived macrophages. Toxicol. Lett. 2016, 263, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Koppe, L.; Pillon, N.J.; Vella, R.E.; Croze, M.L.; Pelletier, C.C.; Chambert, S.; Massy, Z.; Glorieux, G.; Vanholder, R.; Dugenet, Y.; et al. p-Cresyl sulfate promotes insulin resistance associated with CKD. J. Am. Soc. Nephrol. 2013, 24, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Iwasaki, Y.; Yamato, H.; Mori, Y.; Komaba, H.; Watanabe, H.; Maruyama, T.; Fukagawa, M. p-Cresyl sulfate induces osteoblast dysfunction through activating JNK and p38 MAPK pathways. Bone 2013, 56, 347–354. [Google Scholar] [CrossRef]
- Rossi, M.; Campbell, K.L.; Johnson, D.W.; Stanton, T.; Vesey, D.A.; Coombes, J.S.; Weston, K.S.; Hawley, C.M.; McWhinney, B.C.; Ungerer, J.P.; et al. Protein-bound uremic toxins, inflammation and oxidative stress: A cross-sectional study in stage 3–4 chronic kidney disease. Arch. Med. Res. 2014, 45, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.H.; Wang, C.H.; Kuo, C.H.; Lin, Y.L.; Tsai, J.P.; Hsu, B.G. Serum P-Cresyl Sulfate Is a Predictor of Central Arterial Stiffness in Patients on Maintenance Hemodialysis. Toxins 2019, 12, 10. [Google Scholar] [CrossRef]
- Lin, C.J.; Pan, C.F.; Chuang, C.K.; Sun, F.J.; Wang, D.J.; Chen, H.H.; Liu, H.L.; Wu, C.J. P-cresyl sulfate is a valuable predictor of clinical outcomes in pre-ESRD patients. Biomed. Res. Int. 2014, 2014, 526932. [Google Scholar] [CrossRef] [PubMed]
- Bammens, B.; Evenepoel, P.; Keuleers, H.; Verbeke, K.; Vanrenterghem, Y. Free serum concentrations of the protein-bound retention solute p-cresol predict mortality in hemodialysis patients. Kidney Int. 2006, 69, 1081–1087. [Google Scholar] [CrossRef] [PubMed]
- Liabeuf, S.; Barreto, D.V.; Barreto, F.C.; Meert, N.; Glorieux, G.; Schepers, E.; Temmar, M.; Choukroun, G.; Vanholder, R.; Massy, Z.A.; et al. Free p-cresylsulphate is a predictor of mortality in patients at different stages of chronic kidney disease. Nephrol. Dial. Transplant. 2010, 25, 1183–1191. [Google Scholar] [CrossRef] [PubMed]
- Wu, I.W.; Hsu, K.H.; Hsu, H.J.; Lee, C.C.; Sun, C.Y.; Tsai, C.J.; Wu, M.S. Serum free p-cresyl sulfate levels predict cardiovascular and all-cause mortality in elderly hemodialysis patients—A prospective cohort study. Nephrol. Dial. Transplant. 2012, 27, 1169–1175. [Google Scholar] [CrossRef]
- Yamamoto, S.; Tanaka, T.; Omori, K.; Ei, I.; Kitamura, N.; Narita, I. Severity of pruritus in hemodialysis patients: Relationship to uremic toxins and dialysis modality. Nephrol. Dial. Transplant. 2020, 35, gfaa142–P1509. [Google Scholar] [CrossRef]
- Kim, S.J.; Zhang, X.; Cho, S.B.; Kim, C.H.; Park, H.C.; Moon, S.J. Uremic solutes of indoxyl sulfate and p-cresol enhance protease-activated receptor-2 expression in vitro and in vivo in keratinocytes. Hum. Exp. Toxicol. 2021, 40, 113–123. [Google Scholar] [CrossRef]
- Steinhoff, M.; Neisius, U.; Ikoma, A.; Fartasch, M.; Heyer, G.; Skov, P.S.; Luger, T.A.; Schmelz, M. Proteinase-activated receptor-2 mediates itch: A novel pathway for pruritus in human skin. J. Neurosci. 2003, 23, 6176–6180. [Google Scholar] [CrossRef]
- Akiyama, T.; Carstens, M.I.; Carstens, E. Excitation of mouse superficial dorsal horn neurons by histamine and/or PAR-2 agonist: Potential role in itch. J. Neurophysiol. 2009, 102, 2176–2183. [Google Scholar] [CrossRef]
- Barr, T.P.; Garzia, C.; Guha, S.; Fletcher, E.K.; Nguyen, N.; Wieschhaus, A.J.; Ferrer, L.; Covic, L.; Kuliopulos, A. PAR2 Pepducin-Based Suppression of Inflammation and Itch in Atopic Dermatitis Models. J. Investig. Dermatol. 2019, 139, 412–421. [Google Scholar] [CrossRef]
- Moon, S.J.; Kim, H.J.; Cho, S.B.; Lee, S.H.; Choi, H.Y.; Park, H.C.; Ha, S.K. Epidermal Proteinase-Activated Receptor-2 Expression is Increased in End-Stage Renal Disease Patients with Pruritus: A Pilot Study. Electrolyte Blood Press. 2014, 12, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Cohen, G. Immune Dysfuntion in Uremia 2020. Toxins 2020, 12, 439. [Google Scholar] [CrossRef]
- Tecklenborg, J.; Clayton, D.; Siebert, S.; Coley, S.M. The role of the immune system in kidney disease. Clin. Exp. Immunol. 2018, 192, 142–150. [Google Scholar] [CrossRef]
- Fallahzadeh, M.K.; Roozbeh, J.; Geramizadeh, B.; Namazi, M.R. Interleukin-2 serum levels are elevated in patients with uremic pruritus: A novel finding with practical implications. Nephrol. Dial. Transplant. 2011, 26, 3338–3344. [Google Scholar] [CrossRef]
- Abbas, A.K.; Trotta, E.; Simeonov, D.; Marson, A.; Bluestone, J.A. Revisiting IL-2: Biology and therapeutic prospects. Sci. Immunol. 2018, 3, eaat1482. [Google Scholar] [CrossRef]
- Wahlgren, C.F.; Tengvall Linder, M.; Hägermark, O.; Scheynius, A. Itch and inflammation induced by intradermally injected interleukin-2 in atopic dermatitis patients and healthy subjects. Arch. Dermatol. Res. 1995, 287, 572–580. [Google Scholar] [CrossRef]
- Darsow, U.; Scharein, E.; Bromm, B.; Ring, J. Skin testing of the pruritogenic activity of histamine and cytokines (interleukin-2 and tumour necrosis factor-alpha) at the dermal-epidermal junction. Br. J. Dermatol. 1997, 137, 415–417. [Google Scholar] [CrossRef]
- Nakamura, M.; Toyoda, M.; Morohashi, M. Pruritogenic mediators in psoriasis vulgaris: Comparative evaluation of itch-associated cutaneous factors. Br. J. Dermatol. 2003, 149, 718–730. [Google Scholar] [CrossRef]
- Lee, S.H.; Baig, M.; Rusciano, V.; Dutcher, J.P. Novel management of pruritus in patients treated with IL-2 for metastatic renal cell carcinoma and malignant melanoma. J. Immunother. 2010, 33, 1010–1013. [Google Scholar] [CrossRef]
- Bağci, I.S.; Ruzicka, T. IL-31: A new key player in dermatology and beyond. J. Allergy Clin. Immunol. 2018, 141, 858–866. [Google Scholar] [CrossRef]
- Hawro, T.; Saluja, R.; Weller, K.; Altrichter, S.; Metz, M.; Maurer, M. Interleukin-31 does not induce immediate itch in atopic dermatitis patients and healthy controls after skin challenge. Allergy 2014, 69, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Cevikbas, F.; Wang, X.; Akiyama, T.; Kempkes, C.; Savinko, T.; Antal, A.; Kukova, G.; Buhl, T.; Ikoma, A.; Buddenkotte, J.; et al. A sensory neuron-expressed IL-31 receptor mediates T helper cell-dependent itch: Involvement of TRPV1 and TRPA1. J. Allergy Clin. Immunol. 2014, 133, 448–460. [Google Scholar] [CrossRef] [PubMed]
- Furue, M.; Yamamura, K.; Kido-Nakahara, M.; Nakahara, T.; Fukui, Y. Emerging role of interleukin-31 and interleukin-31 receptor in pruritus in atopic dermatitis. Allergy 2018, 73, 29–36. [Google Scholar] [CrossRef]
- Ko, M.J.; Peng, Y.S.; Chen, H.Y.; Hsu, S.P.; Pai, M.F.; Yang, J.Y.; Wen, S.Y.; Jee, S.H.; Wu, H.Y.; Chiu, H.C. Interleukin-31 is associated with uremic pruritus in patients receiving hemodialysis. J. Am. Acad. Dermatol. 2014, 71, 1151–1159.e1. [Google Scholar] [CrossRef]
- Oweis, A.O.; Al-Qarqaz, F.; Bodoor, K.; Heis, L.; Alfaqih, M.A.; Almomani, R.; Obeidat, M.A.; Alshelleh, S.A. Elevated interleukin 31 serum levels in hemodialysis patients are associated with uremic pruritus. Cytokine 2021, 138, 155369. [Google Scholar] [CrossRef]
- Kinugasa, E.; Igawa, K.; Shimada, H.; Kondo, M.; Funakoshi, S.; Imada, N.; Itami, N.; Fukazawa, N.; Takubo, R.; Kawata, Y.; et al. Anti-pruritic effect of nemolizumab in hemodialysis patients with uremic pruritus: A phase II, randomized, double-blind, placebo-controlled clinical study. Clin. Exp. Nephrol. 2021. [Google Scholar] [CrossRef]
- Feld, M.; Garcia, R.; Buddenkotte, J.; Katayama, S.; Lewis, K.; Muirhead, G.; Hevezi, P.; Plesser, K.; Schrumpf, H.; Krjutskov, K.; et al. The pruritus-and TH2-associated cytokine IL-31 promotes growth of sensory nerves. J. Allergy Clin. Immunol. 2016, 138, 500–508.e24. [Google Scholar] [CrossRef]
- Da Silva, E.Z.; Jamur, M.C.; Oliver, C. Mast cell function: A new vision of an old cell. J. Histochem. Cytochem. 2014, 62, 698–738. [Google Scholar] [CrossRef]
- Gupta, K.; Harvima, I.T. Mast cell-neural interactions contribute to pain and itch. Immunol. Rev. 2018, 282, 168–187. [Google Scholar] [CrossRef]
- Siiskonen, H.; Harvima, I. Mast Cells and Sensory Nerves Contribute to Neurogenic Inflammation and Pruritus in Chronic Skin Inflammation. Front. Cell. Neurosci. 2019, 13, 422. [Google Scholar] [CrossRef]
- Stockenhuber, F.; Kurz, R.W.; Sertl, K.; Grimm, G.; Balcke, P. Increased plasma histamine levels in uraemic pruritus. Clin. Sci. 1990, 79, 477–482. [Google Scholar] [CrossRef]
- Gill, D.S.; Fonseca, V.A.; Barradas, M.A.; Balliod, R.; Moorhead, J.F.; Dandona, P. Plasma histamine in patients with chronic renal failure and nephrotic syndrome. J. Clin. Pathol. 1991, 44, 243–245. [Google Scholar] [CrossRef]
- De Marchi, S.; Cecchin, E.; Villalta, D.; Sepiacci, G.; Santini, G.; Bartoli, E. Relief of pruritus and decreases in plasma histamine concentrations during erythropoietin therapy in patients with uremia. N. Engl. J. Med. 1992, 326, 969–974. [Google Scholar] [CrossRef]
- Balaskas, E.V.; Bamihas, G.I.; Karamouzis, M.; Voyiatzis, G.; Tourkantonis, A. Histamine and serotonin in uremic pruritus: Effect of ondansetron in CAPD-pruritic patients. Nephron 1998, 78, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Mettang, T.; Fritz, P.; Weber, J.; Machleidt, C.; Hübel, E.; Kuhlmann, U. Uremic pruritus in patients on hemodialysis or continuous ambulatory peritoneal dialysis (CAPD). The role of plasma histamine and skin mast cells. Clin. Nephrol. 1990, 34, 136–141. [Google Scholar] [PubMed]
- Francos, G.C.; Kauh, Y.C.; Gittlen, S.D.; Schulman, E.S.; Besarab, A.; Goyal, S.; Burke, J.F., Jr. Elevated plasma histamine in chronic uremia. Effects of ketotifen on pruritus. Int. J. Dermatol. 1991, 30, 884–889. [Google Scholar] [CrossRef]
- De Filippi, C.; Regazzini, R.; Piazza, V.; Galli, F.; Pisati, P.; Sacchi, S.; Salvadeo, A. Uraemic pruritus is not related to plasma histamine concentrations. Clin. Exp. Dermatol. 1995, 20, 294–296. [Google Scholar] [CrossRef]
- Meixiong, J.; Anderson, M.; Limjunyawong, N.; Sabbagh, M.F.; Hu, E.; Mack, M.R.; Oetjen, L.K.; Wang, F.; Kim, B.S.; Dong, X. Activation of Mast-Cell-Expressed Mas-Related G-Protein-Coupled Receptors Drives Non-histaminergic Itch. Immunity 2019, 50, 1163–1171.e5. [Google Scholar] [CrossRef] [PubMed]
- Dugas-Breit, S.; Schöpf, P.; Dugas, M.; Schiffl, H.; Ruëff, F.; Przybilla, B. Baseline serum levels of mast cell tryptase are raised in hemodialysis patients and associated with severity of pruritus. J. Dtsch. Dermatol. Ges. 2005, 3, 343–347. [Google Scholar] [CrossRef]
- Voisin, T.; Chiu, I.M. Mast Cells Get on Your Nerves in Itch. Immunity 2019, 50, 1117–1119. [Google Scholar] [CrossRef]
- Matsumoto, M.; Ichimaru, K.; Horie, A. Pruritus and mast cell proliferation of the skin in end stage renal failure. Clin. Nephrol. 1985, 23, 285–288. [Google Scholar]
- Dimković, N.; Djukanović, L.; Radmilović, A.; Bojić, P.; Juloski, T. Uremic pruritus and skin mast cells. Nephron 1992, 61, 5–9. [Google Scholar] [CrossRef]
- Leong, S.O.; Tan, C.C.; Lye, W.C.; Lee, E.J.; Chan, H.L. Dermal mast cell density and pruritus in end-stage renal failure. Ann. Acad. Med. Singap. 1994, 23, 327–329. [Google Scholar]
- Szepietowski, J.; Thepen, T.; van Vloten, W.A.; Szepietowski, T.; Bihari, I.C. Pruritus and mast cell proliferation in the skin of haemodialysis patients. Inflamm. Res. 1995, 44, S84–S85. [Google Scholar] [CrossRef]
- Szepietowski, J.C.; Morita, A.; Tsuji, T. Ultraviolet B induces mast cell apoptosis: A hypothetical mechanism of ultraviolet B treatment for uraemic pruritus. Med. Hypotheses 2002, 58, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Benarroch, E.E. Endogenous opioid systems: Current concepts and clinical correlations. Neurology 2012, 79, 807–814. [Google Scholar] [CrossRef]
- Feng, Y.; He, X.; Yang, Y.; Chao, D.; Lazarus, L.H.; Xia, Y. Current research on opioid receptor function. Curr. Drug Targets 2012, 13, 230–246. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, G.; Willoch, F. Imaging of opioid receptors in the central nervous system. Brain 2008, 131, 1171–1196. [Google Scholar] [CrossRef]
- Reed, B.; Butelman, E.R.; Kreek, M.J. Endogenous opioid system in addiction and addiction-related behaviors. Curr. Opin. Behav. Sci. 2017, 13, 196–202. [Google Scholar] [CrossRef]
- Peciña, M.; Karp, J.F.; Mathew, S.; Todtenkopf, M.S.; Ehrich, E.W.; Zubieta, J.K. Endogenous opioid system dysregulation in depression: Implications for new therapeutic approaches. Mol. Psychiatry 2019, 24, 576–587. [Google Scholar] [CrossRef]
- Cai, Z.; Ratka, A. Opioid system and Alzheimer’s disease. Neuromol. Med. 2012, 14, 91–111. [Google Scholar] [CrossRef]
- Reich, A.; Szepietowski, J.C. Opioid-induced pruritus: An update. Clin. Exp. Dermatol. 2010, 35, 2–6. [Google Scholar] [CrossRef]
- Ko, M.C.; Song, M.S.; Edwards, T.; Lee, H.; Naughton, N.N. The role of central mu opioid receptors in opioid-induced itch in primates. J. Pharmacol. Exp. Ther. 2004, 310, 169–176. [Google Scholar] [CrossRef]
- Ko, M.C.; Naughton, N.N. An experimental itch model in monkeys: Characterization of intrathecal morphine-induced scratching and antinociception. Anesthesiology 2000, 92, 795–805. [Google Scholar] [CrossRef] [PubMed]
- Ko, M.C.; Husbands, S.M. Effects of atypical kappa-opioid receptor agonists on intrathecal morphine-induced itch and analgesia in primates. J. Pharmacol. Exp. Ther. 2009, 328, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Jiang, C.; Yao, H.; Chen, O.; Rahman, S.; Gu, Y.; Zhao, J.; Huh, Y.; Ji, R.R. Central opioid receptors mediate morphine-induced itch and chronic itch via disinhibition. Brain 2021, 144, 665–681. [Google Scholar] [CrossRef]
- Taneda, K.; Tominaga, M.; Negi, O.; Tengara, S.; Kamo, A.; Ogawa, H.; Takamori, K. Evaluation of epidermal nerve density and opioid receptor levels in psoriatic itch. Br. J. Dermatol. 2011, 165, 277–284. [Google Scholar] [CrossRef]
- Kupczyk, P.; Reich, A.; Hołysz, M.; Gajda, M.; Wysokińska, E.; Kobuszewska, A.; Nevozhay, D.; Nowakowska, B.; Strzadała, L.; Jagodziński, P.P.; et al. Opioid Receptors in Psoriatic Skin: Relationship with Itch. Acta Derm. Venereol. 2017, 97, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Tominaga, M.; Ogawa, H.; Takamori, K. Possible roles of epidermal opioid systems in pruritus of atopic dermatitis. J. Investig. Dermatol. 2007, 127, 2228–2235. [Google Scholar] [CrossRef]
- Wieczorek, A.; Krajewski, P.; Kozioł-Gałczyńska, M.; Szepietowski, J.C. Opioid receptors expression in the skin of haemodialysis patients suffering from uraemic pruritus. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2368–2372. [Google Scholar] [CrossRef]
- Danno, K.; Nishiura, K.; Tanaka, M. Increased met-enkephalin plasma levels in hemodialysis patients with or without pruritus. J. Dermatol. Sci. 1995, 10, 238–240. [Google Scholar] [CrossRef]
- Georgala, S.; Schulpis, K.H.; Papaconstantinou, E.D.; Stratigos, J. Raised beta-endorphin serum levels in children with atopic dermatitis and pruritus. J. Dermatol. Sci. 1994, 8, 125–128. [Google Scholar] [CrossRef]
- Glinski, W.; Brodecka, H.; Glinska-Ferenz, M.; Kowalski, D. Neuropeptides in psoriasis: Possible role of beta-endorphin in the pathomechanism of the disease. Int. J. Dermatol. 1994, 33, 356–360. [Google Scholar] [CrossRef]
- Glinski, W.; Brodecka, H.; Glinska-Ferenz, M.; Kowalski, D. Increased concentration of beta-endorphin in sera of patients with psoriasis and other inflammatory dermatoses. Br. J. Dermatol. 1994, 131, 260–264. [Google Scholar] [CrossRef]
- Lee, C.H.; Chuang, H.Y.; Shih, C.C.; Jong, S.B.; Chang, C.H.; Yu, H.S. Transepidermal water loss, serum IgE and beta-endorphin as important and independent biological markers for development of itch intensity in atopic dermatitis. Br. J. Dermatol. 2006, 154, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- Espi, M.; Koppe, L.; Fouque, D.; Thaunat, O. Chronic Kidney Disease-Associated Immune Dysfunctions: Impact of Protein-Bound Uremic Retention Solutes on Immune Cells. Toxins 2020, 12, 300. [Google Scholar] [CrossRef]
- Fabrizi, F.; Donato, F.M.; Messa, P. Association between hepatitis B virus and chronic kidney disease: A systematic review and meta-analysis. Ann. Hepatol. 2017, 16, 21–47. [Google Scholar] [CrossRef] [PubMed]
- Fabrizi, F.; Donato, F.M.; Messa, P. Association Between Hepatitis C Virus and Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Ann. Hepatol. 2018, 17, 364–391. [Google Scholar] [CrossRef] [PubMed]
- Tsui, J.I.; Vittinghoff, E.; Shlipak, M.G.; Bertenthal, D.; Inadomi, J.; Rodriguez, R.A.; O’Hare, A.M. Association of hepatitis C seropositivity with increased risk for developing end-stage renal disease. Arch. Intern. Med. 2007, 167, 1271–1276. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Lin, M.Y.; Chang, J.S.; Hung, C.C.; Chang, J.M.; Chen, H.C.; Yu, M.L.; Hwang, S.J. Hepatitis C virus infection increases risk of developing end-stage renal disease using competing risk analysis. PLoS ONE 2014, 9, e100790. [Google Scholar] [CrossRef] [PubMed]
- Molnar, M.Z.; Alhourani, H.M.; Wall, B.M.; Lu, J.L.; Streja, E.; Kalantar-Zadeh, K.; Kovesdy, C.P. Association of hepatitis C viral infection with incidence and progression of chronic kidney disease in a large cohort of US veterans. Hepatology 2015, 61, 1495–1502. [Google Scholar] [CrossRef]
- Fabrizi, F.; Cerutti, R.; Ridruejo, E. Hepatitis B virus infection as a risk factor for chronic kidney disease. Expert Rev. Clin. Pharmacol. 2019, 12, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Jadoul, M.; Bieber, B.A.; Martin, P.; Akiba, T.; Nwankwo, C.; Arduino, J.M.; Goodkin, D.A.; Pisoni, R.L. Prevalence, incidence, and risk factors for hepatitis C virus infection in hemodialysis patients. Kidney Int. 2019, 95, 939–947. [Google Scholar] [CrossRef]
- Fabrizi, F.; Marzano, A.; Messa, P.; Martin, P.; Lampertico, P. Hepatitis B virus infection in the dialysis population: Current perspectives. Int. J. Artif. Organs 2008, 31, 386–394. [Google Scholar] [CrossRef]
- Bonacini, M. Pruritus in patients with chronic human immunodeficiency virus, hepatitis B and C virus infections. Dig. Liver Dis. 2000, 32, 621–625. [Google Scholar] [CrossRef]
- Chiu, Y.L.; Chen, H.Y.; Chuang, Y.F.; Hsu, S.P.; Lai, C.F.; Pai, M.F.; Yang, S.Y.; Peng, Y.S. Association of uraemic pruritus with inflammation and hepatitis infection in haemodialysis patients. Nephrol. Dial. Transplant. 2008, 23, 3685–3689. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Tamano, M.; Katayama, Y.; Kuniyoshi, T.; Kagawa, K.; Takada, H.; Suzuki, K. Study of pruritus in chronic hepatitis C patients. World J. Gastroenterol. 2014, 20, 17877–17882. [Google Scholar] [CrossRef] [PubMed]
- Oeda, S.; Takahashi, H.; Yoshida, H.; Ogawa, Y.; Imajo, K.; Yoneda, M.; Koshiyama, Y.; Ono, M.; Hyogo, H.; Kawaguchi, T.; et al. Prevalence of pruritus in patients with chronic liver disease: A multicenter study. Hepatol. Res. 2018, 48, E252–E262. [Google Scholar] [CrossRef] [PubMed]
- Abdelsalam, M.; Tawfik, M.; Reda, E.M.; Eldeeb, A.A.; Abdelwahab, A.; Zaki, M.E.; Abdelkader Sobh, M. Insulin Resistance and Hepatitis C Virus-Associated Subclinical Inflammation Are Hidden Causes of Pruritus in Egyptian Hemodialysis Patients: A Multicenter Prospective Observational Study. Nephron 2019, 143, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Kossuth-Cabrejos, S.; Gavino-Gutiérrez, A.M.; Silva-Caso, W. Factors associated with the severity of pruritus in patients with terminal chronic kidney disease undergoing hemodialysis in Lima, Peru. Dermatol. Rep. 2020, 12, 8310. [Google Scholar] [CrossRef]
- Alhmada, Y.; Selimovic, D.; Murad, F.; Hassan, S.L.; Haikel, Y.; Megahed, M.; Hannig, M.; Hassan, M. Hepatitis C virus-associated pruritus: Etiopathogenesis and therapeutic strategies. World J. Gastroenterol. 2017, 23, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Lempert, K.D.; Baltz, P.S.; Welton, W.A.; Whittier, F.C. Pseudouremic pruritus: A scabies epidemic in a dialysis unit. Am. J. Kidney Dis. 1985, 5, 117–119. [Google Scholar] [CrossRef]
- Yates, J.E.; Bleyer, A.J.; Yosipovitch, G.; Sangueza, O.P.; Murea, M. Enigmatic pruritus in a kidney transplant patient. Clin. Kidney J. 2013, 6, 194–198. [Google Scholar] [CrossRef][Green Version]
- Augustin, M.; Kirsten, N.; Körber, A.; Wilsmann-Theis, D.; Itschert, G.; Staubach-Renz, P.; Maul, J.-T.; Zander, N. Prevalence, predictors and comorbidity of dry skin in the general population. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 147–150. [Google Scholar] [CrossRef]
- Wollenberg, A.; Christen-Zäch, S.; Taieb, A.; Paul, C.; Thyssen, J.P.; de Bruin-Weller, M.; Vestergaard, C.; Seneschal, J.; Werfel, T.; Cork, M.J.; et al. ETFAD/EADV Eczema task force 2020 position paper on diagnosis and treatment of atopic dermatitis in adults and children. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2717–2744. [Google Scholar] [CrossRef] [PubMed]
- Szepietowski, J.C.; Reich, A.; Schwartz, R.A. Uraemic xerosis. Nephrol. Dial. Transplant. 2004, 19, 2709–2712. [Google Scholar] [CrossRef] [PubMed]
- Wojtowicz-Prus, E.; Kilis-Pstrusinska, K.; Reich, A.; Zachwieja, K.; Miklaszewska, M.; Szczepanska, M.; Szepietowski, J.C. Disturbed skin barrier in children with chronic kidney disease. Pediatr. Nephrol. 2015, 30, 333–338. [Google Scholar] [CrossRef]
- Morton, C.A.; Lafferty, M.; Hau, C.; Henderson, I.; Jones, M.; Lowe, J.G. Pruritus and skin hydration during dialysis. Nephrol. Dial. Transplant. 1996, 11, 2031–2036. [Google Scholar] [CrossRef]
- Szepietowski, J.C.; Sikora, M.; Kusztal, M.; Salomon, J.; Magott, M.; Szepietowski, T. Uremic pruritus: A clinical study of maintenance hemodialysis patients. J. Dermatol. 2002, 29, 621–627. [Google Scholar] [CrossRef]
- Balaskas, E.; Szepietowski, J.C.; Bessis, D.; Ioannides, D.; Ponticelli, C.; Ghienne, C.; Taberly, A.; Dupuy, P. Randomized, double-blind study with glycerol and paraffin in uremic xerosis. Clin. J. Am. Soc. Nephrol. 2011, 6, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Ståhle-Bäckdahl, M. Stratum corneum hydration in patients undergoing maintenance hemodialysis. Acta Derm. Venereol. 1988, 68, 531–534. [Google Scholar]
- Park, T.H.; Park, C.H.; Ha, S.H.; Lee, S.H.; Song, K.S.; Lee, H.Y.; Han, D.S. Dry skin (xerosis) in patients undergoing maintenance haemodialysis: The role of decreased sweating of the eccrine sweat gland. Nephrol. Dial. Transplant. 1995, 10, 2269–2273. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Reis, J.; Tur, E.; Sprecher, E.; Yarnitsky, D.; Boner, G. Sweat secretion, stratum corneum hydration, small nerve function and pruritus in patients with advanced chronic renal failure. Br. J. Dermatol. 1995, 133, 561–654. [Google Scholar] [CrossRef]
- Kato, A.; Hamada, M.; Maruyama, T.; Maruyama, Y.; Hishida, A. Pruritus and hydration state of stratum corneum in hemodialysis patients. Am. J. Nephrol. 2000, 20, 437–442. [Google Scholar] [CrossRef]
- Chorążyczewska, W.; Reich, A.; Szepietowski, J.C. Lipid Content and Barrier Function Analysis in Uraemic Pruritus. Acta Derm. Venereol. 2016, 96, 402–403. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Duque, M.I.; Patel, T.S.; Ishiuji, Y.; Guzman-Sanchez, D.A.; Dawn, A.G.; Freedman, B.I.; Chan, Y.H.; Crumrine, D.; Elias, P.M. Skin barrier structure and function and their relationship to pruritus in end-stage renal disease. Nephrol. Dial. Transplant. 2007, 22, 3268–3272. [Google Scholar] [CrossRef] [PubMed]
- Okada, K.; Matsumoto, K. Effect of skin care with an emollient containing a high water content on mild uremic pruritus. Ther. Apher. Dial. 2004, 8, 419–422. [Google Scholar] [CrossRef] [PubMed]
- Szepietowski, J.C.; Reich, A.; Szepietowski, T. Emollients with endocannabinoids in the treatment of uremic pruritus: Discussion of the therapeutic options. Ther. Apher. Dial. 2005, 9, 277–279. [Google Scholar] [CrossRef] [PubMed]
- Paus, R.; Schmelz, M.; Bíró, T.; Steinhoff, M. Frontiers in pruritus research: Scratching the brain for more effective itch therapy. J. Clin. Investig. 2006, 116, 1174–1186. [Google Scholar] [CrossRef] [PubMed]
- Johannson, O.; Hilliges, M.; Ståhle-Bäckdahl, M. Intraepidermal neuron-specific enolase (NSE)-immunoreactive nerve fibres: Evidence for sprouting in uremic patients on maintenance hemodialysis. Neurosci. Lett. 1989, 99, 281–286. [Google Scholar] [CrossRef]
- Fantini, F.; Baraldi, A.; Sevignani, C.; Spattini, A.; Pincelli, C.; Giannetti, A. Cutaneous innervation in chronic renal failure patients. An immunohistochemical study. Acta. Derm. Venereol. 1992, 72, 102–105. [Google Scholar]
- Zakrzewska-Pniewska, B.; Jedras, M. Is pruritus in chronic uremic patients related to peripheral somatic and autonomic neuropathy? Study by R-R interval variation test (RRIV) and by sympathetic skin response (SSR). Neurophysiol. Clin. 2001, 31, 181–193. [Google Scholar] [CrossRef]
- Papoiu, A.D.; Emerson, N.M.; Patel, T.S.; Kraft, R.A.; Valdes-Rodriguez, R.; Nattkemper, L.A.; Coghill, R.C.; Yosipovitch, G. Voxel-based morphometry and arterial spin labeling fMRI reveal neuropathic and neuroplastic features of brain processing of itch in end-stage renal disease. J. Neurophysiol. 2014, 112, 1729–1738. [Google Scholar] [CrossRef]
- Yoganathan, S.; Bagga, A.; Gulati, S.; Toteja, G.S.; Hari, P.; Sinha, A.; Pandey, R.M.; Irshad, N. Prevalence and predictors of peripheral neuropathy in nondiabetic children with chronic kidney disease. Muscle Nerve 2018, 57, 792–798. [Google Scholar] [CrossRef]
- Abd El Naby, S.A.; Bahbah, W.A.; Kasemy, Z.A.; Mahmoud, A.A. Neurophysiological and Neuroradiological Changes in Children With Chronic Kidney Disease. Front. Pediatr. 2020, 8, 570708. [Google Scholar] [CrossRef]
- Matsuda-Abedini, M.; Fitzpatrick, K.; Harrell, W.R.; Gipson, D.S.; Hooper, S.R.; Belger, A.; Poskitt, K.; Miller, S.P.; Bjornson, B.H. Brain abnormalities in children and adolescents with chronic kidney disease. Pediatr. Res. 2018, 84, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Hartung, E.A.; Erus, G.; Jawad, A.F.; Laney, N.; Doshi, J.J.; Hooper, S.R.; Radcliffe, J.; Davatzikos, C.; Furth, S.L. Brain Magnetic Resonance Imaging Findings in Children and Young Adults With CKD. Am. J. Kidney Dis. 2018, 72, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Szepietowski, J.C.; Schwartz, R.A. Uremic pruritus. Int. J. Dermatol. 1998, 37, 247–253. [Google Scholar] [CrossRef]
- Mettang, T. Pruritus in renal disease. In Itch: Mechanisms and Treatment; Carstens, E., Akiyama, T., Eds.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2014; pp. 47–59. [Google Scholar]
- Aucella, F.; Vigilante, M.; Gesuete, A.; Maruccio, G.; Specchio, A.; Gesualdo, L. Uraemic itching: Do polymethylmethacrylate dialysis membranes play a role? Nephrol. Dial. Transplant. 2007, 22, v8–v12. [Google Scholar] [CrossRef]
- Jiang, X.; Ji, F.; Chen, Z.-W.; Huang, Q.-L. Comparison of high-flux hemodialysis with hemodialysis filtration in treatment of uraemic pruritus: A randomized controlled trial. Int. Urol. Nephrol. 2016, 48, 1533–1541. [Google Scholar] [CrossRef]
- Ko, M.-J.; Wu, H.Y.; Chen, H.-Y.; Chiu, Y.-L.; Hsu, S.-P.; Pai, M.-F.; Yang, J.-Y.; Lai, C.-F.; Lu, H.-M.; Huang, S.-C.; et al. Uremic pruritus, dialysis adequacy, and metabolic profiles in hemodialysis patients: A prospective 5-year cohort study. PLoS ONE 2013, 8, e71404. [Google Scholar] [CrossRef]
- Vanholder, R.; Van Biesen, W.; Lameire, N. A swan song for Kt/V urea. Semin. Dial. 2019, 32, 424–437. [Google Scholar] [CrossRef]
- Zucker, I.; Yosipovitch, G.; David, M.; Gafter, U.; Boner, G. Prevalence and characterization of uremic pruritus in patients undergoing hemodialysis: Uremic pruritus is still a major problem for patients with end-stage renal disease. J. Am. Acad. Dermatol. 2003, 49, 842–846. [Google Scholar] [CrossRef]
- Dyachenko, P.; Shustak, A.; Rozenman, D. Hemodialysis-related pruritus and associated cutaneous manifestations. Int. J. Dermatol. 2006, 45, 664–667. [Google Scholar] [CrossRef]
- Ding, L.; Johnston, J.; Pinsk, M.N. Monitoring dialysis adequacy: History and current practice. Pediatr. Nephrol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Berne, B.; Vahlquist, A.; Fischer, T.; Danielson, B.G.; Berne, C. UV treatment of uraemic pruritus reduces the vitamin A content of the skin. Eur. J. Clin. Investig. 1984, 14, 203–206. [Google Scholar] [CrossRef] [PubMed]
- De Kroes, S.; Smeenk, G. Serum vitamin A levels and pruritus in patients on hemodialysis. Dermatologica 1983, 166, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-W.; Weng, C.-H.; Chan, M.-J.; Lin-Tan, D.-T.; Yen, T.-H.; Huang, W.-H. Association Between Serum Aluminum Level and Uremic Pruritus in Hemodialysis Patients. Sci. Rep. 2018, 8, 17251. [Google Scholar] [CrossRef]
- Cannata-Andía, H.G.; Fernández-Martín, J.L. The clinical impact of aluminium overload in renal failure. Nephrol. Dial. Transplant. 2002, 17, 9–12. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Friga, V.; Linos, A.; Linos, D.A. Is aluminum toxicity responsible for uremic pruritus in chronic hemodialysis patients? Nephron 1997, 75, 48–53. [Google Scholar] [CrossRef]
- Song, S.; Lee, K.; Lee, Y.-M.; Lee, J.-H.; Lee, S.I.; Yu, S.-D.; Paek, D. Acute health effects of urban fine and ultrafine particles on children with atopic dermatitis. Environ. Res. 2011, 111, 394–399. [Google Scholar] [CrossRef]
- Kim, J.; Kim, E.-H.; Oh, I.; Jung, K.; Han, Y.; Cheong, H.-K.; Ahn, K. Symptoms of atopic dermatitis are influenced by outdoor air pollution. J. Allergy Clin. Immunol. 2013, 132, 495–498.e1. [Google Scholar] [CrossRef]
- Fadadu, R.P.; Grimes, B.; Jewell, N.P.; Vargo, J.; Young, A.T.; Abuabara, K.; Balmes, J.R.; Wei, M.L. Association of Wildfire Air Pollution and Health Care Use for Atopic Dermatitis and Itch. JAMA Dermatol. 2021, 157, 658–666. [Google Scholar] [CrossRef]
- Whang, K.A.; Huang, A.H.; Miller, L.S.; Kang, S.; Kwatra, S.G. Association of particulate matter air pollution and itch: A digital epidemiology approach. J. Am. Acad. Dermatol. 2019, 81, 1409–1410. [Google Scholar] [CrossRef]
- Huang, W.-H.; Lin, J.-H.; Weng, C.-H.; Hsu, C.-W.; Yen, T.-H. Environmental NO2 and CO Exposure: Ignored Factors Associated with Uremic Pruritus in Patients Undergoing Hemodialysis. Sci. Rep. 2016, 6, 31168. [Google Scholar] [CrossRef]
- Liu, M.-H.; Chan, M.-J.; Hsu, C.-W.; Weng, C.-H.; Yen, T.-H.; Huang, W.-H. Association of uremic pruritus in hemodialysis patients with the number of days of high mean 24-hour particulate matter with a diameter of <2.5 μm. Ther. Clin. Risk Manag. 2017, 13, 255–262. [Google Scholar] [CrossRef]
- Hayani, K.; Kunzmann, K.; Mettang, T.; Weiss, M.; Tschulena, U.; Weisshaar, E. Lower prevalence of chronic itch in haemodialysis patients on loop diuretics: Results from GEHIS (German Epidemiological Hemodialysis Itch Study). J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1333–1337. [Google Scholar] [CrossRef]
- Moncrieff, G.; Cork, M.; Lawton, S.; Kokiet, S.; Daly, C.; Clark, C. Use of emollients in dry-skin conditions: Consensus statement. Clin. Exp. Dermatol. 2013, 38, 231–238. [Google Scholar] [CrossRef]
- Castello, M.; Milani, M. Efficacy of topical hydrating and emollient lotion containing 10% urea ISDIN® plus dexpanthenol (Ureadin Rx 10) in the treatment of skin xerosis and pruritus in hemodialyzed patients: An open prospective pilot trial. G. Ital. Dermatol. Venereol. 2011, 146, 321–325. [Google Scholar] [PubMed]
- Chen, Y.-C.; Chiu, W.-T.; Wu, M.-S. Therapeutic effect of topical gamma-linolenic acid on refractory uremic pruritus. Am. J. Kidney Dis. 2006, 48, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Young, T.A.; Patel, T.S.; Camacho, F.; Clark, A.; Freedman, B.I.; Kaur, M.; Fountain, J.; Williams, L.L.; Yosipovitch, G.; Fleischer, A.B., Jr. A pramoxine-based anti-itch lotion is more effective than a control lotion for the treatment of uremic pruritus in adult hemodialysis patients. J. Dermatol. Treat. 2009, 20, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Wąsik, F.; Szepietowski, J.; Szepietowski, T.; Weyde, W. Relief of uraemic pruritus after balneological therapy with a bath oil containing polidocanol (Balneum Hernial Plus). An open clinical study. J. Dermatol. Treat. 1996, 7, 231–233. [Google Scholar] [CrossRef]
- Breneman, D.L.; Cardone, J.S.; Blumsack, R.F.; Lather, R.M.; Searle, E.A.; Pollack, V.E. Topical capsaicin for treatment of hemodialysis-related pruritus. J. Am. Acad. Dermatol. 1992, 26, 91–94. [Google Scholar] [CrossRef]
- Tarng, D.C.; Cho, Y.L.; Liu, H.N.; Huang, T.P. Hemodialysis-related pruritus: A double-blind, placebo-controlled, crossover study of capsaicin 0.025% cream. Nephron 1996, 72, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Makhlough, A.; Ala, S.; Haj-Heydari, S.; Kashi, Z.; Bari, A. Topical capsaicin therapy for uremic pruritus in patients on hemodialysis. Iran. J. Kidney Dis. 2010, 4, 137–140. [Google Scholar]
- Gooding, S.M.D.; Canter, P.H.; Coelho, H.F.; Boddy, K.; Ernst, E. Systematic review of topical capsaicin in the treatment of pruritus. Int. J. Dermatol. 2010, 49, 858–865. [Google Scholar] [CrossRef]
- Pauli-Magnus, C.; Klumpp, S.; Alscher, D.M.; Kuhlmann, U.; Mettang, T. Short-term efficacy of tacrolimus ointment in severe uremic pruritus. Perit. Dial. Int. 2000, 20, 802–803. [Google Scholar] [CrossRef]
- Kuypers, D.R.; Claes, K.; Evenepoel, P.; Maes, B.; Vanrenterghem, Y. A prospective proof of concept study of the efficacy of tacrolimus ointment on uraemic pruritus (UP) in patients on chronic dialysis therapy. Nephrol. Dial. Transplant. 2004, 19, 1895–1901. [Google Scholar] [CrossRef][Green Version]
- Duque, M.I.; Yosipovitch, G.; Fleischer, A.B., Jr.; Willard, J.; Freedman, B.I. Lack of efficacy of tacrolimus ointment 0.1% for treatment of hemodialysis-related pruritus: A randomized, double-blind, vehicle-controlled study. J. Am. Acad. Dermatol. 2005, 52, 519–521. [Google Scholar] [CrossRef]
- Ghorbani, A.R.; Feily, A.; Khalili, A.; Dormanesh, B. Lack of efficacy of topical calcineurin inhibitor pimecrolimus 1% on pruritus of severely uremic patients: A randomized double-blind study in 60 patients. Dermatitis 2011, 22, 167–168. [Google Scholar] [CrossRef]
- Elmets, C.A.; Lim, H.W.; Stoff, B.; Connor, C.; Cordoro, K.M.; Lebwohl, M.; Armstrong, A.W.; Davis, D.M.R.; Elewski, B.E.; Gelfand, J.M.; et al. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis with phototherapy. J. Am. Acad. Dermatol. 2019, 81, 775–804. [Google Scholar] [CrossRef]
- Wong, T.; Hsu, L.; Liao, W. Phototherapy in psoriasis: A review of mechanisms of action. J. Cutan. Med. Surg. 2013, 17, 6–12. [Google Scholar] [CrossRef]
- DeSilva, B.; McKenzie, R.C.; Hunter, J.A.A.; Norval, M. Local effects of TL01 phototherapy in psoriasis. Photodermatol. Photoimmunol. Photomed. 2008, 24, 268–269. [Google Scholar] [CrossRef] [PubMed]
- Osmancevic, A.; Landin-Wilhelmsen, K.; Larkö, O.; Krogstad, A.L. Vitamin D status in psoriasis patients during different treatments with phototherapy. J. Photochem. Photobiol. B 2010, 101, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Dotterud, L.K.; Wilsgaard, T.; Vorland, L.H.; Falk, E.S. The effect of UVB radiation on skin microbiota in patients with atopic dermatitis and healthy controls. Int. J. Circumpolar Health 2008, 67, 254–260. [Google Scholar] [CrossRef]
- Hong, S.P.; Kim, M.J.; Jung, M.-Y.; Jeon, H.; Goo, J.; Ahn, S.K.; Lee, S.H.; Elias, P.M.; Choi, E.H. Biopositive effects of low-dose UVB on epidermis: Coordinate upregulation of antimicrobial peptides and permeability barrier reinforcement. J. Investig. Dermatol. 2008, 128, 2880–2887. [Google Scholar] [CrossRef]
- Legat, F.J.; Wolf, P. Cutaneous sensory nerves: Mediators of phototherapeutic effects? Front. Biosci. 2009, 14, 4921–4931. [Google Scholar] [CrossRef][Green Version]
- Gilchrest, B.A.; Rowe, J.W.; Brown, R.S.; Steinman, T.I.; Arndt, K.A. Relief of uremic pruritus with ultraviolet phototherapy. N. Engl. J. Med. 1977, 297, 136–138. [Google Scholar] [CrossRef]
- Gilchrest, B.A.; Rowe, J.W.; Brown, R.S.; Steinman, T.I.; Arndt, K.A. Ultraviolet phototherapy of uremic pruritus. Long-term results and possible mechanism of action. Ann. Intern. Med. 1979, 91, 17–21. [Google Scholar] [CrossRef]
- Schultz, B.C.; Roenigk, H.H., Jr. Uremic pruritus treated with ultraviolet light. JAMA 1980, 243, 1836–1837. [Google Scholar] [CrossRef]
- Simpson, N.B.; Davison, A.M. Ultraviolet phototherapy for uraemic pruritus. Lancet 1981, 1, 781. [Google Scholar] [CrossRef]
- Blachley, J.D.; Blankenship, D.M.; Menter, A.; Parker, T.F., 3rd; Knochel, J.P. Uremic pruritus: Skin divalent ion content and response to ultraviolet phototherapy. Am. J. Kidney Dis. 1985, 5, 237–241. [Google Scholar] [CrossRef]
- Hsu, M.M.-L.; Yang, C.C. Uraemic pruritus responsive to broadband ultraviolet (UV) B therapy does not readily respond to narrowband UVB therapy. Br. J. Dermatol. 2003, 149, 888–889. [Google Scholar] [CrossRef]
- Ada, S.; Seçkin, D.; Budakoğlu, I.; Ozdemir, F.N. Treatment of uremic pruritus with narrowband ultraviolet B phototherapy: An open pilot study. J. Am. Acad. Dermatol. 2005, 53, 149–151. [Google Scholar] [CrossRef]
- Wang, T.-J.; Lan, L.-C.; Lu, C.-S.; Lin, K.-C.; Tung, H.-H.; Wu, S.-F.V.; Liang, S.-Y. Efficacy of narrowband ultraviolet phototherapy on renal pruritus. J. Clin. Nurs. 2014, 23, 1593–1602. [Google Scholar] [CrossRef] [PubMed]
- Sherjeena, P.B.; Binitha, M.P.; Rajan, U.; Sreelatha, M.; Sarita, S.; Nirmal, C.; Deepthi, N.S. A controlled trial of narrowband ultraviolet B phototherapy for the treatment of uremic pruritus. Indian J. Dermatol. Venereol. Leprol. 2017, 83, 247–249. [Google Scholar] [CrossRef]
- Sapam, R.; Waikhom, R. Role of narrow band ultra violet radiation as an add-on therapy in peritoneal dialysis patients with refractory uremic pruritus. World J. Nephrol. 2018, 7, 84–89. [Google Scholar] [CrossRef]
- Ko, M.J.; Yang, J.Y.; Wu, H.-Y.; Hu, F.-C.; Chen, S.-I.; Tsai, P.-J.; Jee, S.-H.; Chiu, H.-C. Narrowband ultraviolet B phototherapy for patients with refractory uraemic pruritus: A randomized controlled trial. Br. J. Dermatol. 2011, 165, 633–639. [Google Scholar] [CrossRef]
- Hercz, D.; Jiang, S.H.; Webster, A.C. Interventions for itch in people with advanced chronic kidney disease. Cochrane Database Syst. Rev. 2020, 12, CD011393. [Google Scholar] [CrossRef]
- Leurs, R.; Church, M.K.; Taglialatela, M. H1-antihistamines, inverse agonism: Anti-inflammatory actions and cardiac effects. Clin. Exp. Allergy 2002, 32, 489–498. [Google Scholar] [CrossRef]
- Church, D.S.; Church, M.K. Pharmacology of antihistamines. World Allergy Organ. J. 2011, 4, S22–S27. [Google Scholar] [CrossRef]
- Kim, H.J.; Park, J.B.; Lee, J.H.; Kim, I.-H. How stress triggers itch: A preliminary study of the mechanism of stress-induced pruritus using fMRI. Int. J. Dermatol. 2016, 55, 434–442. [Google Scholar] [CrossRef]
- Nakhaee, S.; Nasiri, A.; Waghei, Y.; Morshedi, J. Comparison of Avena sativa, vinegar, and hydroxyzine for uremic pruritus of hemodialysis patients: A crossover randomized clinical trial. Iran. J. Kidney Dis. 2015, 9, 316–322. [Google Scholar] [PubMed]
- Kebar, S.M.; Sharghi, A.; Ghorghani, M.; Hoseininia, S. Comparison of gabapentin and hydroxyzine in the treatment of pruritus in patients on dialysis. Clin. Exp. Dermatol. 2020, 45, 866–871. [Google Scholar] [CrossRef]
- Foroutan, N.; Etminan, A.; Nikvarz, N.; Abadi, M.S.S. Comparison of pregabalin with doxepin in the management of uremic pruritus: A randomized single blind clinical trial. Hemodial. Int. 2017, 21, 63–71. [Google Scholar] [CrossRef]
- Haber, R.; Bachour, J.; Salloum, A.; Maacaron, T.; Khoury, F.; Habr, L.; Ammoury, A.; Joubran, N. Comparison of gabapentin and doxepin in the management of uremic pruritus: A randomized crossover clinical trial. Dermatol. Ther. 2020, 33, e14522. [Google Scholar] [CrossRef]
- Amirkhanlou, S.; Rashedi, A.; Taherian, J.; Hafezi, A.A.; Parsaei, S. Comparison of Gabapentin and Ketotifen in Treatment of Uremic Pruritus in Hemodialysis Patients. Pak. J. Med. Sci. 2016, 32, 22–26. [Google Scholar] [CrossRef]
- Marquez, D.; Ramonda, C.; Lauxmann, J.E.; Romero, C.E.; Vukelic, V.L.; Martinatto, C.; Barrón, B.; Novoa, P.A.; Peixoto, A.J.; Orías, M. Uremic pruritus in hemodialysis patients: Treatment with desloratidine versus gabapentin. Braz. J. Nephrol. 2012, 34, 148–152. [Google Scholar] [CrossRef][Green Version]
- Legroux-Crespel, E.; Clèdes, J.; Misery, L. A comparative study on the effects of naltrexone and loratadine on uremic pruritus. Dermatology 2004, 208, 326–330. [Google Scholar] [CrossRef]
- Song, Y.-H.; Wang, S.-Y.; Lang, J.-H.; Xiao, Y.-F.; Cai, G.-Y.; Chen, X.-M. Therapeutic effect of intravenous sodium thiosulfate for uremic pruritus in hemodialysis patients. Ren. Fail. 2020, 42, 987–993. [Google Scholar] [CrossRef]
- Kobayashi, K.; Endoh, F.; Ohmori, I.; Akiyama, T. Action of antiepileptic drugs on neurons. Brain Dev. 2020, 42, 2–5. [Google Scholar] [CrossRef]
- Kaufman, K.R. Antiepileptic drugs in the treatment of psychiatric disorders. Epilepsy Behav. 2011, 21, 1–11. [Google Scholar] [CrossRef]
- Eisenberg, E.; River, Y.; Shifrin, A.; Krivoy, N. Antiepileptic drugs in the treatment of neuropathic pain. Drugs 2007, 67, 1265–1289. [Google Scholar] [CrossRef]
- Gunal, A.I.; Ozalp, G.; Yoldas, T.K.; Gunal, S.Y.; Kirciman, E.; Celiker, H. Gabapentin therapy for pruritus in haemodialysis patients: A randomized, placebo-controlled, double-blind trial. Nephrol. Dial. Transplant. 2004, 19, 3137–3139. [Google Scholar] [CrossRef]
- Naini, A.E.; Harandi, A.A.; Khanbabapour, D.; Shahidi, S.; Seirafiyan, S.; Mohseni, M. Gabapentin: A promising drug for the treatment of uremic pruritus. Saudi J. Kidney Dis. Transpl. 2007, 18, 378–381. [Google Scholar]
- Razeghi, E.; Eskandari, D.; Ganji, M.R.; Meysamie, A.P.; Togha, M.; Khashayar, P. Gabapentin and uremic pruritus in hemodialysis patients. Ren. Fail. 2009, 31, 85–90. [Google Scholar] [CrossRef]
- Rayner, H.; Baharani, J.; Smith, S.; Suresh, V.; Dasgupta, I. Uraemic pruritus: Relief of itching by gabapentin and pregabalin. Nephron Clin. Pract. 2012, 122, 75–79. [Google Scholar] [CrossRef]
- Solak, Y.; Biyik, Z.; Atalay, H.; Gaipov, A.; Guney, F.; Turk, S.; Covic, A.; Goldsmith, D.; Kanbay, M. Pregabalin versus gabapentin in the treatment of neuropathic pruritus in maintenance haemodialysis patients: A prospective, crossover study. Nephrology 2012, 17, 710–717. [Google Scholar] [CrossRef]
- Nofal, E.; Farag, F.; Nofal, A.; Eldesouky, F.; Alkot, R.; Abdelkhalik, Z. Gabapentin: A promising therapy for uremic pruritus in hemodialysis patients: A randomized-controlled trial and review of literature. J. Dermatol. Treat. 2016, 27, 515–519. [Google Scholar] [CrossRef]
- Gobo-Oliveira, M.; Pigari, V.G.; Ogata, M.S.; Miot, H.A.; Ponce, D.; Abbade, L.P. Gabapentin versus dexchlorpheniramine as treatment for uremic pruritus: A randomised controlled trial. Eur. J. Dermatol. 2018, 28, 488–495. [Google Scholar] [CrossRef]
- Rossi, G.M.; Corradini, M.; Blanco, V.; Mattei, S.; Fiaccadori, E.; Vaglio, A.; Manenti, L. Randomized trial of two after-dialysis gabapentin regimens for severe uremic pruritus in hemodialysis patients. Intern. Emerg. Med. 2019, 14, 1341–1346. [Google Scholar] [CrossRef]
- Ravindran, A.; Kunnath, R.P.; Sunny, A.; Vimal, B. Comparison of Safety and Efficacy of Pregabalin versus Gabapentin for the treatment of Uremic Pruritus in Patients with Chronic Kidney Disease on Maintenance Haemodialysis. Indian J. Palliat. Care. 2020, 26, 281–286. [Google Scholar] [CrossRef]
- Aperis, G.; Paliouras, C.; Zervos, A.; Arvanitis, A.; Alivanis, P. The use of pregabalin in the treatment of uraemic pruritus in haemodialysis patients. J. Ren. Care 2010, 36, 180–185. [Google Scholar] [CrossRef]
- Shavit, L.; Grenader, T.; Lifschitz, M.; Slotki, I. Use of pregabalin in the management of chronic uremic pruritus. J. Pain Symptom Manag. 2013, 45, 776–781. [Google Scholar] [CrossRef]
- Yue, J.; Jiao, S.; Xiao, Y.; Ren, W.; Zhao, W.; Meng, J. Comparison of pregabalin with ondansetron in treatment of uraemic pruritus in dialysis patients: A prospective, randomized, double-blind study. Int. Urol. Nephrol. 2015, 47, 161–167. [Google Scholar] [CrossRef]
- Khan, T.M.; Wu, D.B.-C.; Goh, B.-H.; Lee, L.-H.; Alhafez, A.A.; Sulaiman, S.A.S. An Observational Longitudinal Study Investigating the Effectiveness of 75 mg Pregabalin Post-Hemodialysis among Uremic Pruritus Patients. Sci. Rep. 2016, 6, 36555. [Google Scholar] [CrossRef]
- Mendham, J.E. Gabapentin for the treatment of itching produced by burns and wound healing in children: A pilot study. Burns 2004, 30, 851–853. [Google Scholar] [CrossRef]
- Goutos, I.; Eldardiri, M.; Khan, A.A.; Dziewulski, P.; Richardson, P.M. Comparative evaluation of antipruritic protocols in acute burns. The emerging value of gabapentin in the treatment of burns pruritus. J. Burn Care Res. 2010, 31, 57–63. [Google Scholar] [CrossRef]
- Ahuja, R.B.; Gupta, R.; Gupta, G.; Shrivastava, P. A comparative analysis of cetirizine, gabapentin and their combination in the relief of post-burn pruritus. Burns 2011, 37, 203–207. [Google Scholar] [CrossRef]
- Kaul, I.; Amin, A.; Rosenberg, M.; Rosenberg, L.; Meyer, W.J., 3rd. Use of gabapentin and pregabalin for pruritus and neuropathic pain associated with major burn injury: A retrospective chart review. Burns 2018, 44, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Christofaki, M.; Papaioannou, A. Ondansetron: A review of pharmacokinetics and clinical experience in postoperative nausea and vomiting. Expert Opin. Drug Metab. Toxicol. 2014, 10, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Juza, R.; Vlcek, P.; Mezeiova, E.; Musilek, K.; Soukup, O.; Korabecny, J. Recent advances with 5-HT 3 modulators for neuropsychiatric and gastrointestinal disorders. Med. Res. Rev. 2020, 40, 1593–1678. [Google Scholar] [CrossRef]
- Raderer, M.; Müller, C.; Scheithauer, W. Ondansetron for pruritus due to cholestasis. N. Engl. J. Med. 1994, 330, 1540. [Google Scholar] [CrossRef]
- Müller, C.; Pongratz, S.; Pidlich, J.; Penner, E.; Kaider, A.; Schemper, M.; Raderer, M.; Scheithauer, W.; Ferenci, P. Treatment of pruritus in chronic liver disease with the 5-hydroxytryptamine receptor type 3 antagonist ondansetron: A randomized, placebo-controlled, double-blind cross-over trial. Eur. J. Gastroenterol. Hepatol. 1998, 10, 865–870. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.A.; Molenaar, H.A.J.; Oosting, J. Ondansetron and pruritus in chronic liver disease: A controlled study. Hepatogastroenterology 2007, 54, 1196–1199. [Google Scholar]
- Schwörer, H.; Hartmann, H.; Ramadori, G. Relief of cholestatic pruritus by a novel class of drugs: 5-hydroxytryptamine type 3 (5-HT3) receptor antagonists: Effectiveness of ondansetron. Pain 1995, 61, 33–37. [Google Scholar] [CrossRef]
- O’Donohue, J.W.; Pereira, S.P.; Ashdown, A.C.; Haigh, C.G.; Wilkinson, J.R.; Williams, R. A controlled trial of ondansetron in the pruritus of cholestasis. Aliment. Pharmacol. Ther. 2005, 21, 1041–1045. [Google Scholar] [CrossRef] [PubMed]
- Tzeng, J.-I.; Chu, K.-S.; Ho, S.-T.; Cheng, K.-I.; Liu, K.-S.; Wang, J.-J. Prophylactic iv ondansetron reduces nausea, vomiting and pruritus following epidural morphine for postoperative pain control. Can. J. Anaesth. 2003, 50, 1023–1026. [Google Scholar] [CrossRef] [PubMed]
- Sarvela, P.J.; Halonen, P.M.; Soikkeli, A.I.; Kainu, J.P.; Korttila, K.T. Ondansetron and tropisetron do not prevent intraspinal morphine- and fentanyl-induced pruritus in elective cesarean delivery. Acta Anaesthesiol. Scand. 2006, 50, 239–244. [Google Scholar] [CrossRef]
- Han, D.W.; Hong, S.W.; Kwon, J.-Y.; Lee, J.W.; Kim, K.J. Epidural ondansetron is more effective to prevent postoperative pruritus and nausea than intravenous ondansetron in elective cesarean delivery. Acta Obstet. Gynecol. Scand. 2007, 86, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Ashmore, S.D.; Jones, C.H.; Newstead, C.G.; Daly, M.J.; Chrystyn, H. Ondansetron therapy for uremic pruritus in hemodialysis patients. Am. J. Kidney Dis. 2000, 35, 827–831. [Google Scholar] [CrossRef]
- Murphy, M.; Reaich, D.; Pai, P.; Finn, P.; Carmichael, A.J. A randomized, placebo-controlled, double-blind trial of ondansetron in renal itch. Br. J. Dermatol. 2003, 148, 314–317. [Google Scholar] [CrossRef]
- Weisshaar, E.; Dunker, N.; Röhl, F.-W.; Gollnick, H. Antipruritic effects of two different 5-HT3 receptor antagonists and an antihistamine in haemodialysis patients. Exp. Dermatol. 2004, 13, 298–304. [Google Scholar] [CrossRef]
- Patel, K.P.; Luo, F.J.; Plummer, N.S.; Hostetter, T.H.; Meyer, T.W. The production of p-cresol sulfate and indoxyl sulfate in vegetarians versus omnivores. Clin. J. Am. Soc. Nephrol. 2012, 7, 982–988. [Google Scholar] [CrossRef]
- Marzocco, S.; Dal Piaz, F.; Di Micco, L.; Torraca, S.; Sirico, M.L.; Tartaglia, D.; Autore, G.; Di Iorio, B. Very low protein diet reduces indoxyl sulfate levels in chronic kidney disease. Blood Purif. 2013, 35, 196–201. [Google Scholar] [CrossRef]
- Di Iorio, B.R.; Rocchetti, M.T.; De Angelis, M.; Cosola, C.; Marzocco, S.; Di Micco, L.; di Bari, I.; Accetturo, M.; Vacca, M.; Gobbetti, M.; et al. Nutritional Therapy Modulates Intestinal Microbiota and Reduces Serum Levels of Total and Free Indoxyl Sulfate and P-Cresyl Sulfate in Chronic Kidney Disease (Medika Study). J. Clin. Med. 2019, 8, 1424. [Google Scholar] [CrossRef]
- Sirich, T.L.; Plummer, N.S.; Gardner, C.D.; Hostetter, T.H.; Meyer, T.W. Effect of increasing dietary fiber on plasma levels of colon-derived solutes in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2014, 9, 1603–1610. [Google Scholar] [CrossRef]
- Rossi, M.; Johnson, D.W.; Xu, H.; Carrero, J.J.; Pascoe, E.; French, C.; Campbell, K.L. Dietary protein-fiber ratio associates with circulating levels of indoxyl sulfate and p-cresyl sulfate in chronic kidney disease patients. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 860–865. [Google Scholar] [CrossRef]
- Lu, L.; Huang, Y.-F.; Wang, M.-Q.; Chen, D.-X.; Wan, H.; Wei, L.-B.; Xiao, W. Dietary fiber intake is associated with chronic kidney disease (CKD) progression and cardiovascular risk, but not protein nutritional status, in adults with CKD. Asia Pac. J. Clin. Nutr. 2017, 26, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, S.; Jones, C. Protein restriction for children with chronic renal failure. Cochrane Database Syst. Rev. 2007, 4, CD006863. [Google Scholar] [CrossRef]
- Takayama, F.; Taki, K.; Niwa, T. Bifidobacterium in gastro-resistant seamless capsule reduces serum levels of indoxyl sulfate in patients on hemodialysis. Am. J. Kidney Dis. 2003, 41, S142–S145. [Google Scholar] [CrossRef]
- Lim, P.S.; Wang, H.F.; Lee, M.C.; Chiu, L.-S.; Wu, M.-Y.; Chang, W.-C.; Wu, T.K. The Efficacy of Lactobacillus-Containing Probiotic Supplementation in Hemodialysis Patients: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Ren. Nutr. 2021, 31, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Meijers, B.K.; De Preter, V.; Verbeke, K.; Vanrenterghem, Y.; Evenepoel, P. p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin. Nephrol. Dial. Transplant. 2010, 25, 219–224. [Google Scholar] [CrossRef]
- Cosola, C.; De Angelis, M.; Rocchetti, M.T.; Montemurno, E.; Maranzano, V.; Dalfino, G.; Manno, C.; Zito, A.; Gesualdo, M.; Ciccone, M.M.; et al. Beta-Glucans Supplementation Associates with Reduction in P-Cresyl Sulfate Levels and Improved Endothelial Vascular Reactivity in Healthy Individuals. PLoS ONE 2017, 12, e0169635. [Google Scholar] [CrossRef] [PubMed]
- Esgalhado, M.; Kemp, J.A.; Azevedo, R.; Paiva, B.R.; Stockler-Pinto, M.B.; Dolenga, C.J.; Borges, N.A.; Nakao, L.S.; Mafra, D. Could resistant starch supplementation improve inflammatory and oxidative stress biomarkers and uremic toxins levels in hemodialysis patients? A pilot randomized controlled trial. Food Funct. 2018, 9, 6508–6516. [Google Scholar] [CrossRef]
- De Preter, V.; Vanhoutte, T.; Huys, G.; Swings, J.; De Vuyst, L.; Rutgeerts, P.; Verbeke, K. Effects of Lactobacillus casei Shirota, Bifidobacterium breve, and oligofructose-enriched inulin on colonic nitrogen-protein metabolism in healthy humans. Am. J. Physiol. Gastrointest. Liver Physiol. 2007, 292, G358–G368. [Google Scholar] [CrossRef]
- Nakabayashi, I.; Nakamura, M.; Kawakami, K.; Ohta, T.; Kato, I.; Uchida, K.; Yoshida, M. Effects of synbiotic treatment on serum level of p-cresol in haemodialysis patients: A preliminary study. Nephrol. Dial. Transplant. 2011, 26, 1094–1098. [Google Scholar] [CrossRef]
- Guida, B.; Germano, R.; Trio, R.; Russo, D.; Memoli, B.; Grumetto, L.; Barbato, F.; Cataldi, M. Effect of short-term synbiotic treatment on plasma p-cresol levels in patients with chronic renal failure: A randomized clinical trial. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Rossi, M.; Johnson, D.W.; Morrison, M.; Pascoe, E.M.; Coombes, J.S.; Forbes, J.M.; Szeto, C.C.; McWhinney, B.C.; Ungerer, J.P.; Campbell, K.L. Synbiotics Easing Renal Failure by Improving Gut Microbiology (SYNERGY): A Randomized Trial. Clin. J. Am. Soc. Nephrol. 2016, 11, 223–231. [Google Scholar] [CrossRef]
- Lopes, R.d.-C.S.O.; Theodoro, J.M.V.; da Silva, B.P.; Queiroz, V.A.V.; de Castro Moreira, M.E.; Mantovani, H.C.; Hermsdorff, H.H.; Martino, H.S.D. Synbiotic meal decreases uremic toxins in hemodialysis individuals: A placebo-controlled trial. Food Res. Int. 2019, 116, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Borges, N.A.; Carmo, F.L.; Stockler-Pinto, M.B.; de Brito, J.S.; Dolenga, C.J.; Ferreira, D.C.; Nakao, L.S.; Rosado, A.; Fouque, D.; Mafra, D. Probiotic Supplementation in Chronic Kidney Disease: A Double-blind, Randomized, Placebo-controlled Trial. J. Ren. Nutr. 2018, 28, 28–36. [Google Scholar] [CrossRef]
- Hyun, H.S.; Paik, K.H.; Cho, H.Y. p-Cresyl sulfate and indoxyl sulfate in pediatric patients on chronic dialysis. Korean J. Pediatr. 2013, 56, 159–164. [Google Scholar] [CrossRef]
- Ikee, R.; Sasaki, N.; Yasuda, T.; Fukazawa, S. Chronic Kidney Disease, Gut Dysbiosis, and Constipation: A Burdensome Triplet. Microorganisms 2020, 8, 1862. [Google Scholar] [CrossRef]
- Ramos, C.I.; Armani, R.G.; Canziani, M.E.; Dolenga, C.J.R.; Nakao, L.S.; Campbell, K.L.; Cuppari, L. Bowel Habits and the Association With Uremic Toxins in Non-Dialysis-Dependent Chronic Kidney Disease Patients. J. Ren. Nutr. 2020, 30, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Pereira, N.B.F.; Ramos, C.I.; Santos de Andrade, L.; Rodrigues Teixeira, R.; Nakao, L.S.; Rodrigues, S.D.; de Lima, J.D.; Dalboni, M.A.; Cuppari, L. Influence of bowel habits on gut-derived toxins in peritoneal dialysis patients. J. Nephrol. 2020, 33, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Pederson, J.A.; Matter, B.J.; Czerwinski, A.W.; Llach, F. Relief of idiopathic generalized pruritus in dialysis patients treated with activated oral charcoal. Ann. Intern. Med. 1980, 93, 446–448. [Google Scholar] [CrossRef] [PubMed]
- Giovannetti, S.; Barsotti, G.; Cupisti, A.; Dani, L.; Bandini, S.; Angelini, D.; Antonelli, A.; Salvadori, M.; Urti, D.A. Oral activated charcoal in patients with uremic pruritus. Nephron 1995, 70, 193–196. [Google Scholar] [CrossRef]
- Fusaro, R.M. A contraindication for the use of charcoal in uremic patients. J. Am. Acad. Dermatol. 1981, 5, 219. [Google Scholar] [CrossRef]
- Asai, M.; Kumakura, S.; Kikuchi, M. Review of the efficacy of AST-120 (KREMEZIN ®) on renal function in chronic kidney disease patients. Ren. Fail. 2019, 41, 47–56. [Google Scholar] [CrossRef]
- Schulman, G.; Berl, T.; Beck, G.J.; Remuzzi, G.; Ritz, E.; Arita, K.; Kato, A.; Shimizu, M. Randomized placebo-controlled EPPIC trials of AST-120 in CKD. J. Am. Soc. Nephrol. 2015, 26, 1732–1746. [Google Scholar] [CrossRef]
- Cha, R.H.; Kang, S.W.; Park, C.W.; Cha, D.R.; Na, K.Y.; Kim, S.G.; Yoon, S.A.; Han, S.Y.; Chang, J.H.; Park, S.K.; et al. A Randomized, Controlled trial of oral intestinal sorbent AST-120 on Renal function deterioration in patients with advanced renal dysfunction. Clin. J. Am. Soc. Nephrol. 2016, 11, 559–567. [Google Scholar] [CrossRef]
- Niwa, T.; Emoto, Y.; Maeda, K.; Uehara, Y.; Yamada, N.; Shibata, M. Oral sorbent suppresses accumulation of albumin-bound indoxyl sulphate in serum of haemodialysis patients. Nephrol. Dial. Transplant. 1991, 6, 105–109. [Google Scholar] [CrossRef]
- Meert, N.; Eloot, S.; Waterloos, M.A.; Van Landschoot, M.; Dhondt, A.; Glorieux, G.; Ledebo, I.; Vanholder, R. Effective removal of protein-bound uraemic solutes by different convective strategies: A prospective trial. Nephrol. Dial. Transplant. 2009, 24, 562–570. [Google Scholar] [CrossRef]
- Krieter, D.H.; Hackl, A.; Rodriguez, A.; Chenine, L.; Moragues, H.L.; Lemke, H.D.; Wanner, C.; Canaud, B. Protein-bound uraemic toxin removal in haemodialysis and post-dilution haemodiafiltration. Nephrol. Dial. Transplant. 2010, 25, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Meert, N.; Eloot, S.; Schepers, E.; Lemke, H.D.; Dhondt, A.; Glorieux, G.; Van Landschoot, M.; Waterloos, M.A.; Vanholder, R. Comparison of removal capacity of two consecutive generations of high-flux dialysers during different treatment modalities. Nephrol. Dial. Transplant. 2011, 26, 2624–2630. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, M.K.; Middel, I.R.; Vernooij, R.W.M.; Bots, M.L.; Verhaar, M.C.; Masereeuw, R.; Grooteman, M.P.; Nubé, N.J.; van den Dorpel, M.A.; Blankestijn, P.J.; et al. Protein-Bound Uremic Toxins in Hemodialysis Patients Relate to Residual Kidney Function, Are Not Influenced by Convective Transport, and Do Not Relate to Outcome. Toxins 2020, 12, 234. [Google Scholar] [CrossRef] [PubMed]
- Krieter, D.H.; Kerwagen, S.; Rüth, M.; Lemke, H.-D.; Wanner, C. Differences in Dialysis Efficacy Have Limited Effects on Protein-Bound Uremic Toxins Plasma Levels over Time. Toxins 2019, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- Brettschneider, F.; Tolle, M.; von der Giet, M.; Passlick-Deetjen, J.; Steppan, S.; Peter, M.; Jankowski, V.; Krause, A.; Kuhne, S.; Zidek, W.; et al. Removal of protein-bound, hydrophobic uremic toxins by a combined fractionated plasma separation and adsorption technique. Artif. Organs 2013, 37, 409–416. [Google Scholar] [CrossRef]
- Saar-Kovrov, V.; Zidek, W.; Orth-Alampour, S.; Fliser, D.; Jankowski, V.; Biessen, E.A.L.; Jankowski, J. Reduction of protein-bound uraemic toxins in plasma of chronic renal failure patients: A systematic review. J. Intern. Med. 2021. [Google Scholar] [CrossRef]
- Rocchetti, M.T.; Cosola, C.; di Bari, I.; Magnani, S.; Galleggiante, V.; Scandiffio, L.; Dalfino, G.; Netti, G.S.; Atti, M.; Corciulo, R.; et al. Efficacy of Divinylbenzenic Resin in Removing Indoxyl Sulfate and P-Cresol Sulfate in Hemodialysis Patients: Results From an In Vitro Study and An In Vivo Pilot Trial (xuanro4-Nature 3.2). Toxins 2020, 12, 170. [Google Scholar] [CrossRef]
- Pavlenko, D.; van Geffen, E.; van Steenbergen, M.J.; Glorieux, G.; Vanholder, R.; Gerritsen, K.G.F.; Stamatialis, D. New low-flux mixed matrix membranes that offer superior removal of protein-bound toxins from human plasma. Sci. Rep. 2016, 6, 34429. [Google Scholar] [CrossRef]
- Yamamoto, S.; Ito, T.; Sato, M.; Goto, S.; Kazama, J.J.; Gejyo, F.; Narita, I. Adsorption of Protein-Bound Uremic Toxins Using Activated Carbon through Direct Hemoperfusion in vitro. Blood Purif. 2019, 48, 215–222. [Google Scholar] [CrossRef]
- Shi, Y.; Wang, Y.; Ma, S.; Liu, T.; Tian, H.; Zhu, Q.; Wang, W.; Li, Y.; Ding, F. Increasing the removal of protein-bound uremic toxins by liposome-supported hemodialysis. Artif. Organs 2019, 43, 490–503. [Google Scholar] [CrossRef]
- Madero, M.; Cano, K.B.; Campos, I.; Tao, X.; Maheshwari, V.; Brown, J.; Cornejo, B.; Handelman, G.; Thijssen, S.; Kotanko, P. Removal of Protein-Bound Uremic Toxins during Hemodialysis Using a Binding Competitor. Clin. J. Am. Soc. Nephrol. 2019, 14, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Meert, N.; Waterloos, M.A.; Van Landschoot, M.; Dhondt, A.; Ledebo, I.; Glorieux, G.; Goeman, J.; Van der Eycken, J.; Vanholder, R. Prospective evaluation of the change of predialysis protein-bound uremic solute concentration with postdilution online hemodiafiltration. Artif. Organs 2010, 34, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Marquez, I.O.; Tambra, S.; Luo, F.Y.; Li, Y.; Plummer, N.S.; Hostetter, T.H.; Meyer, T.W. Contribution of residual function to removal of protein-bound solutes in hemodialysis. Clin. J. Am. Soc. Nephrol. 2011, 6, 290–296. [Google Scholar] [CrossRef]
- Toth-Manikowski, S.M.; Sirich, T.L.; Meyer, T.W.; Hostetter, T.H.; Hwang, S.; Plummer, N.S.; Hai, X.; Coresh, J.; Powe, N.R.; Shafi, T. Contribution of ‘clinically negligible’ residual kidney function to clearance of uremic solutes. Nephrol. Dial. Transplant. 2020, 35, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Poesen, R.; Evenepoel, P.; de Loor, H.; Bammens, B.; Claes, K.; Sprangers, B.; Naesens, M.; Kuypers, D.; Augustijns, P.; Meijers, B. The influence of renal transplantation on retained microbial-human co-metabolites. Nephrol. Dial. Transplant. 2016, 31, 1721–1729. [Google Scholar] [CrossRef]
- Liabeuf, S.; Desjardins, L.; Massy, Z.A.; Brazier, F.; Westeel, P.F.; Mazouz, H.; Titeca-Beauport, D.; Diouf, M.; Glorieux, G.; Vanholder, R. Levels of Indoxyl Sulfate in Kidney Transplant Patients, and the Relationship With Hard Outcomes. Circ. J. 2016, 80, 722–730. [Google Scholar] [CrossRef]
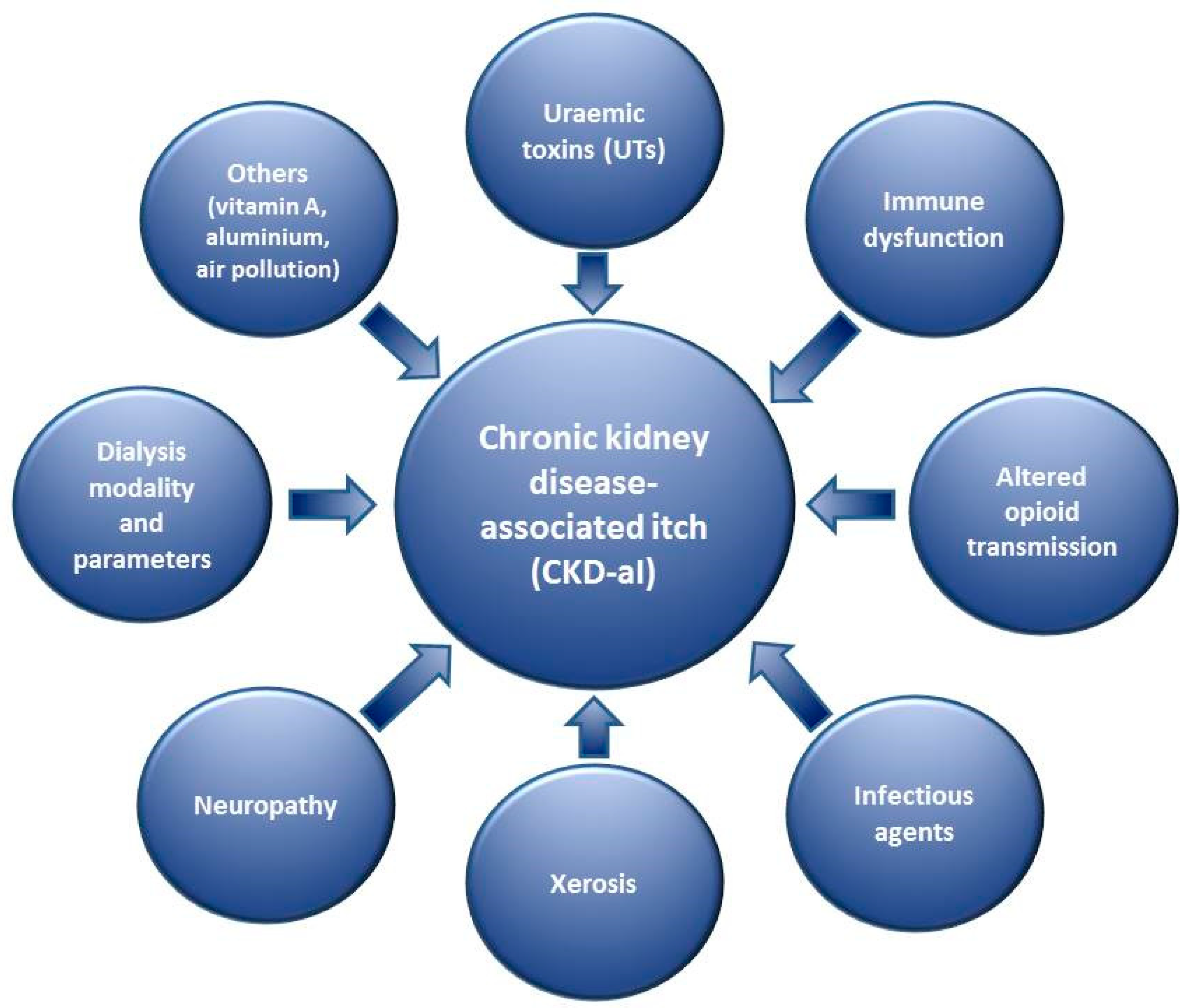
| Uraemic toxins (UTs) Immune dysfunction Altered opioid transmission Infectious agents Skin dryness (xerosis) Neuropathy Dialysis modality and its parameters Others |
| Substance Groups | Major Examples of UT |
|---|---|
| Free water-soluble low molecular weight molecules (LMWM) | Uric acid (UA) *, asymmetric dimethylarginine (ADMA), malondialdehyde, neopterin, N-methyl-2-pyridone-5-carboxamide, N-methyl-4-pyridone-3-carboxamide |
| Middle molecules (MM) | β2-Microglobulin * (β2-M), parathormone * (PTH), interleukin-6 * (IL-6), leptin, cystatin C, met-enkephalin *, β-dynorphin * |
| Protein-bound uraemic toxins (PBUT) | Indoxyl sulfate * (IS), p-cresyl sulfate * (pCS), homocysteine, carboxymethyllysine, hippuric acid |
| Therapeutic Group | Examples of Treatment |
|---|---|
| Topical therapy | Emollients |
| Phototherapy | NB-UVB |
| Systemic therapy | H1-antihistamines, gabapentin, pregabalin, ondansetron, activated charcoal |
| Targeting PBUT | Reducing production: proper protein intake, fibre intake, probiotics, prebiotics, synbiotics, laxatives |
| Decreasing intestinal absorption: activated charcoal, AST-120 | |
| Increasing removal: preserving kidney function, improving dialysis, RTx |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reszke, R.; Kiliś-Pstrusińska, K.; Szepietowski, J.C. Chronic Kidney Disease-Associated Itch (CKD-aI) in Children—A Narrative Review. Toxins 2021, 13, 450. https://doi.org/10.3390/toxins13070450
Reszke R, Kiliś-Pstrusińska K, Szepietowski JC. Chronic Kidney Disease-Associated Itch (CKD-aI) in Children—A Narrative Review. Toxins. 2021; 13(7):450. https://doi.org/10.3390/toxins13070450
Chicago/Turabian StyleReszke, Radomir, Katarzyna Kiliś-Pstrusińska, and Jacek C. Szepietowski. 2021. "Chronic Kidney Disease-Associated Itch (CKD-aI) in Children—A Narrative Review" Toxins 13, no. 7: 450. https://doi.org/10.3390/toxins13070450
APA StyleReszke, R., Kiliś-Pstrusińska, K., & Szepietowski, J. C. (2021). Chronic Kidney Disease-Associated Itch (CKD-aI) in Children—A Narrative Review. Toxins, 13(7), 450. https://doi.org/10.3390/toxins13070450







