Daboia (Vipera) palaestinae Envenomation in 123 Horses: Treatment and Efficacy of Antivenom Administration
Abstract
1. Introduction
2. Results
2.1. Patient Characteristics and Clinical Signs
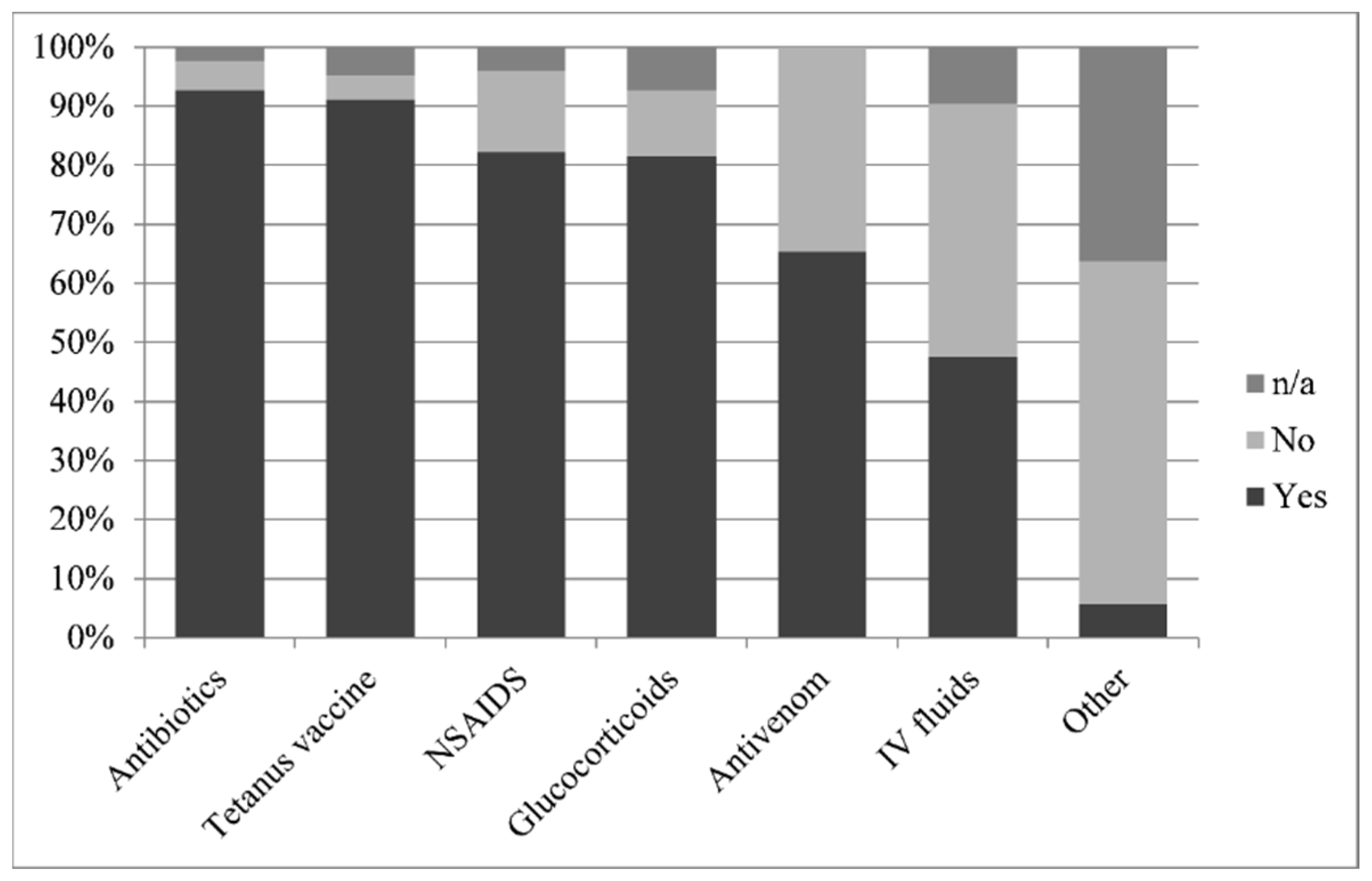
2.2. Treatment
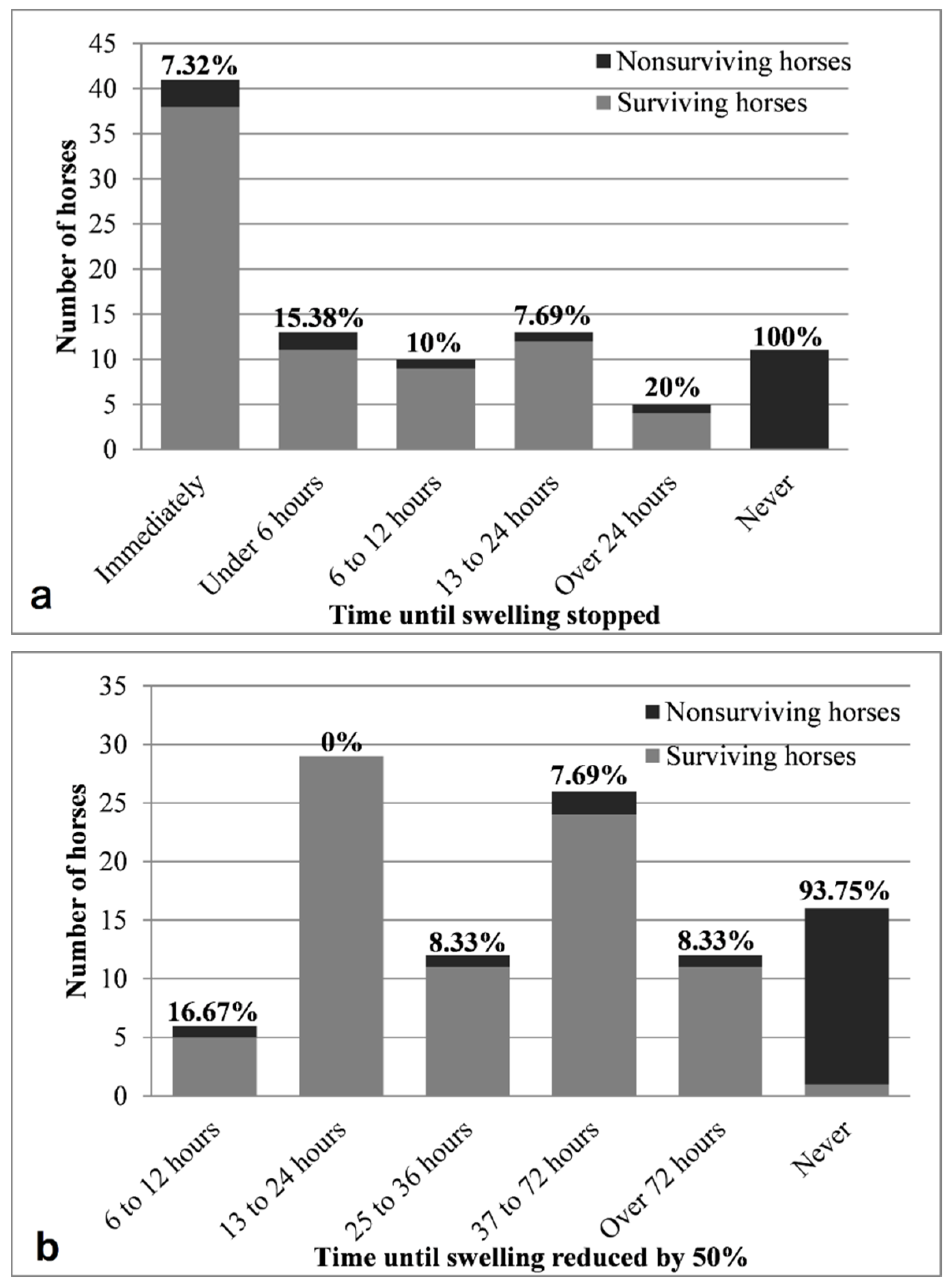
2.3. Response to Treatment
2.4. Determination of Antivenom Concentration in Two Commercially Available Antivenom Products
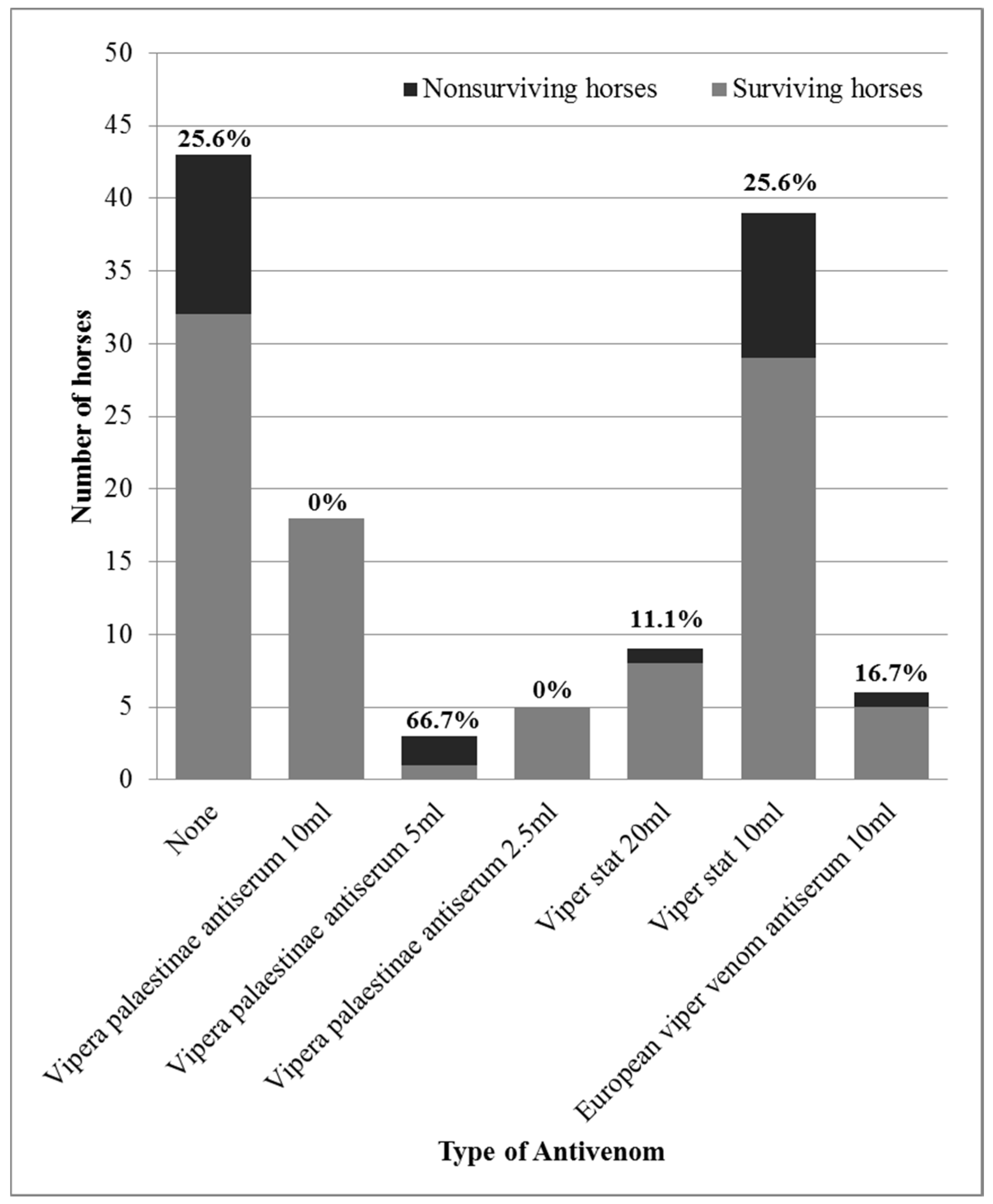
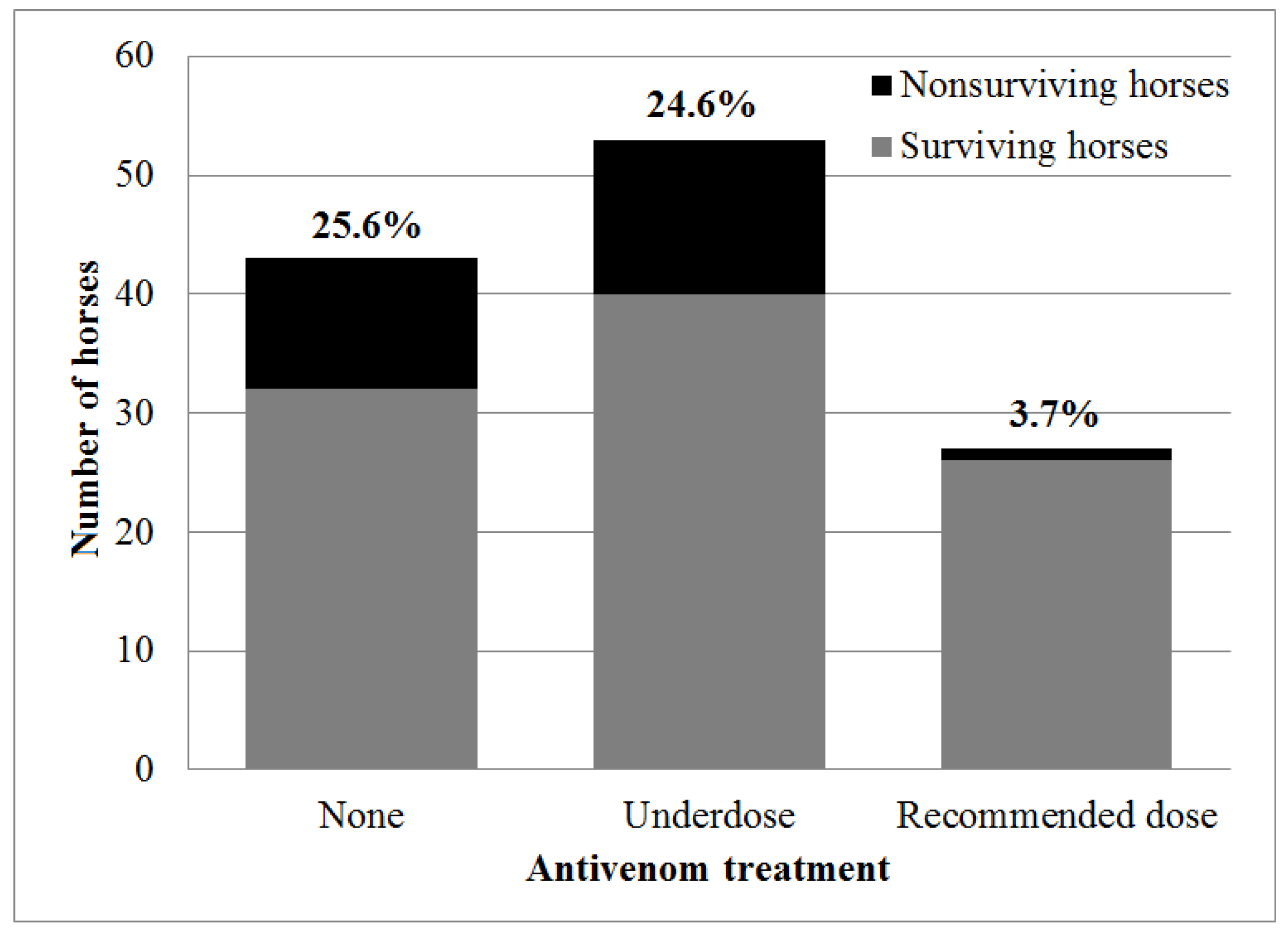
2.5. Antivenom Administration as a Prognostic Factor
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Case Selection and Data Collection
5.2. Evaluation of the Response to Treatment
5.3. Determination of Antivenom Concentration in Two Commercially Available Horse-Derived Antivenom Products
5.4. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Dose of per Mouse (µg) | Mice | Cumulative | Mortality (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Living | Dead | Living | Dead | Total | ||||
| a | Venom | ||||||||
| 8.75 | 6 | 2 | 4 | 17 | 4 | 21 | |||
| 10 | 6 | 5 | 1 | 15 | 5 | 20 | |||
| 11.25 | 6 | 4 | 2 | 10 | 7 | 17 | 41 | P1 | |
| 12.5 | 6 | 4 | 2 | 6 | 9 | 15 | 60 | P2 | |
| 13.75 | 6 | 2 | 4 | 2 | 13 | 15 | |||
| LD50 = 12.5 − [(60 − 50)/(60 − 41) × (12.5 − 11.25)] = 11.84 | |||||||||
| LD50 = 42.23 | |||||||||
| LD50/mouse = 5.3 | |||||||||
| b | Viper-Stat | ||||||||
| 0.1875 | 6 | 4 | 2 | 21 | 2 | 23 | |||
| 0.175 | 6 | 3 | 3 | 17 | 5 | 22 | |||
| 0.1625 | 6 | 6 | 6 | 14 | 11 | 25 | 44 | P1 | |
| 0.15 | 6 | 4 | 2 | 8 | 13 | 21 | 62 | P2 | |
| 0.1375 | 6 | 4 | 2 | 4 | 15 | 19 | |||
| ED50 = 0.150 + [(62 – 50)/(62 − 44) × (0.1625 − 0.15)] = 0.1583 mL | |||||||||
| 1 mL antivenom = 27 LD50 = 0.32 g venom | |||||||||
| c | Vipera palaestinae Antiserum | ||||||||
| 0.0312 | 6 | 4 | 2 | 12 | 2 | 14 | |||
| 0.025 | 4 | 2 | 2 | 8 | 4 | 12 | |||
| 0.0187 | 4 | 3 | 1 | 6 | 5 | 11 | 45.5 | P1 | |
| 0.0124 | 4 | 3 | 1 | 3 | 6 | 9 | 66.66 | P2 | |
| ED50 = 0.0124 + [(66.65 − 50)/(66.65 − 45.5) × (0.0187 − 0.0124)] = 0.0174 mL | |||||||||
| 1 mL antivenom = 247 LD50 = 2.9 g venom | |||||||||
Appendix B
| Clinical Parameter | 0 | 1 |
|---|---|---|
| Weight (Kg) | Over 200 kg | Under 200 kg |
| Swelling (scale 1–5) | 1–3 | 4–5 |
| Respiratory effort (scale 1–5) | 1–4 | 5 |
| Mental status | BAR or QAR | D or Shock |
| Envenomation site | Other | Hind leg |
| Signs of bleeding disorder | No | Yes |
| Hydration status | Under 7% | Over 7% |
References
- Chippaux, J.P. Snake-bites: Appraisal of the global situation. Bull. World Health Organ. 1998, 76, 515–524. [Google Scholar] [PubMed]
- Bentur, Y.; Raikhlin-Eisenkraft, B.; Galperin, M. Evaluation of antivenom therapy in Vipera palaestinae bites. Toxicon 2004, 44, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Bruchim, Y. Viper Snakebites. Isr. J. Vet. Med. 2010, 65, 39–41. [Google Scholar]
- Kochva, E. Venomous snakes of Israel: Ecology and snakebite. Public Health Rev. 1998, 26, 209–232. [Google Scholar] [PubMed]
- Segev, G.; Shipov, A.; Klement, E.; Harrus, S.; Kass, P.; Aroch, I. Vipera palaestinae envenomation in 327 dogs: A retrospective cohort study and analysis of risk factors for mortality. Toxicon 2004, 43, 691–699. [Google Scholar] [CrossRef]
- Aroch, I.; Harrus, S. Retrospective study of the epidemiological, clinical, haematological and biochemical findings in 109 dogs poisoned by Vipera xanthina palestinae. Vet. Rec. 1999, 144, 532–535. [Google Scholar] [CrossRef]
- Aroch, I.; Segev, G.; Klement, E.; Shipov, A.; Harrus, S. Fatal Vipera xanthina palestinae envenomation in 16 dogs. Vet. Hum. toxicol. 2004, 46, 268–272. [Google Scholar]
- Lenchner, I.; Aroch, I.; Segev, G.; Kelmer, E.; Bruchim, Y. A retrospective evaluation of Vipera palaestinae envenomation in 18 cats: (2006–2011). J. Vet. Emerg. Crit. Care 2014, 24, 437–443. [Google Scholar] [CrossRef]
- Hoffman, A.; Levi, O.; Orgad, U.; Nyska, A. Myocarditis following envenoming with Vipera palaestinae in two horses. Toxicon 1993, 31, 1623–1628. [Google Scholar] [CrossRef]
- Yeruham, I.; Avidar, Y. Lethality in a ram from the bite of a Palestine viper (Vipera xanthina palestinae). Vet. Hum. Toxicol. 2002, 44, 26–27. [Google Scholar]
- Efrati, P. Clinical manifestations and treatment of viper bite in Israel. Toxicon 1969, 7, 29–31. [Google Scholar] [CrossRef]
- Haviv, J.; Huerta, M.; Shpilberg, O.; Mimouni, D.; Ash, N.; Grotto, I. Field treatment of snakebites in the Israel Defense Forces. Public Health Rev. 1998, 26, 247–256. [Google Scholar]
- Pivko-Levy, D.; Munchnak, I.; Rimon, A.; Balla, U.; Scolnik, D.; Hoyte, C.; Voliovitch, Y.; Glatstein, M. Evaluation of antivenom therapy for Vipera palaestinae bites in children: Experience of two large, tertiary care pediatric hospitals. Clin. Toxicol. 2017, 55, 235–240. [Google Scholar] [CrossRef]
- Momic, T.; Arlinghaus, F.T.; Arien-Zakay, H.; Katzhendler, J.; Eble, J.A.; Marcinkiewicz, C.; Lazarovici, P. Pharmacological aspects of Vipera xantina palestinae venom. Toxins 2011, 3, 1420–1432. [Google Scholar] [CrossRef]
- Shemesh, I.Y.; Kristal, C.; Langerman, L.; Bourvin, A. Preliminary evaluation of Vipera palaestinae snake bite treatment in accordance to the severity of the clinical syndrome. Toxicon 1998, 36, 867–873. [Google Scholar] [CrossRef]
- Bentur, Y.; Zveibel, F.; Adler, M.; Raikhlin, B. Delayed administration of Vipera xanthina palaestinae antivenon. J. Toxicol. Clin. Toxicol. 1997, 35, 257–261. [Google Scholar] [CrossRef]
- Theakston, R.D.G.; Warrell, D.A.; Griffiths, E. Report of a WHO workshop on the standardization and control of antivenoms. Toxicon 2003, 41, 541–557. [Google Scholar] [CrossRef]
- Gutierrez, J.M.; Leon, G.; Burnouf, T. Antivenoms for the treatment of snakebite envenomings: The road ahead. Biologicals 2011, 39, 129–142. [Google Scholar] [CrossRef]
- Moroz, C. Vipera palaestinae antivenin. Public Health Rev. 1998, 26, 233–236. [Google Scholar]
- Moroz, C.; Goldblum, N.; Devries, A. Preparation of Vipera palestinae antineurotoxin using carboxymethyl-cellulose-bound neurotoxin as antigen. Nature 1963, 200, 697–698. [Google Scholar] [CrossRef]
- Moroz, C.; de Vries, A.; Goldblum, N. Preparation of an antivenin against Vipera palestinae venom with high antineurotoxic potency. Toxicon 1966, 4, 205–208. [Google Scholar] [CrossRef]
- Lurie, Y.; Bentur, Y. Vipera palaestinae bite and serum sickness during pregnancy. J. Emerg. Med. 2010, 38, e67–e70. [Google Scholar] [CrossRef] [PubMed]
- Landolt, G.A. Management of equine poisoning and envenomation. Vet. Clin. N. Am. Equine Pract. 2007, 23, 31–47. [Google Scholar] [CrossRef]
- Bamford, N.J.; Sprinkle, S.B.; Cudmore, L.A.; Cullimore, A.M.; van Eps, A.W.; Verdegaal, E.; Tennent-Brown, B.S. Elapid snake envenomation in horses: 52 cases (2006–2016). Equine Vet. J. 2017. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.J.; Gutierrez, J.M.; Calvete, J.J.; Wuster, W.; Ratanabanangkoon, K.; Paiva, O.; Brown, N.I.; Casewell, N.R.; Harrison, R.A.; Rowley, P.D.; et al. Ending the drought: New strategies for improving the flow of affordable, effective antivenoms in Asia and Africa. J. Pproteom. 2011, 74, 1735–1767. [Google Scholar] [CrossRef] [PubMed]
- Tirosh-Levy, S.; Solomovich, R.; Comte, J.; Sutton, G.A.; Steinman, A. Daboia (Vipera) palaestinae envenomation in horses: Clinical and hematological signs, risk factors for mortality and construction of a novel severity scoring system. Toxicon 2017, 137, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Efrati, P.; Reif, L. Clinical and pathological observations of sixty-five cases of viper bite in Israel. Am. J. Trop. Med. Hyg. 1953, 2, 1085–1108. [Google Scholar] [CrossRef]
- Fielding, C.L.; Pusterla, N.; Magdesian, K.G.; Higgins, J.C.; Meier, C.A. Rattlesnake envenomation in horses: 58 cases (1992–2009). J. Am. Vet. Med. Assoc. 2011, 238, 631–635. [Google Scholar] [CrossRef]
- Chippaux, J.P.; Balde, M.C.; Sessinou, E.; Yero Boiro, M.; Massougbodji, A. Evaluation of a new polyvalent antivenom against snakebite envenomation (Inoserp(R) Panafricain) in two different epidemiological settings: Northern Benin and Maritime Guinea. Med. Sante Trop. 2015, 25, 56–64. [Google Scholar] [CrossRef]
- Chippaux, J.P.; Massougbodji, A.; Stock, R.P.; Alagon, A. Clinical trial of an F(ab’)2 polyvalent equine antivenom for African snake bites in Benin. Am. J. Trop. Med. Hyg. 2007, 77, 538–546. [Google Scholar] [CrossRef]
- Minton, S.A. Neutralization of Old-World Viper Venoms by American Pit Viper Antivenin. Toxicon 1976, 14, 146–148. [Google Scholar] [CrossRef]
- Dos-Santos, M.C.; Arroyo, C.; Solano, S.; Herrera, M.; Villalta, M.; Segura, A.; Estrada, R.; Gutierrez, J.M.; Leon, G. Comparison of the effect of Crotalus simus and Crotalus durissus ruruima venoms on the equine antibody response towards Bothrops asper venom: Implications for the production of polyspecific snake antivenoms. Toxicon 2011, 57, 237–243. [Google Scholar] [CrossRef]
- Archundia, I.G.; de Roodt, A.R.; Ramos-Cerrillo, B.; Chippaux, J.P.; Olguin-Perez, L.; Alagon, A.; Stock, R.P. Neutralization of Vipera and Macrovipera venoms by two experimental polyvalent antisera: A study of paraspecificity. Toxicon 2011, 57, 1049–1056. [Google Scholar] [CrossRef]
- Paret, G.; Ben-Abraham, R.; Ezra, D.; Shrem, D.; Eshel, G.; Vardi, A.; Winkler, E.; Barzilay, Z. Vipera palaestinae snake envenomations: Experience in children. Hum. Exp. Toxicol. 1997, 16, 683–687. [Google Scholar] [CrossRef]
- Lund, H.S.; Kristiansen, V.; Eggertsdottir, A.V.; Skancke, E.; Ranheim, B. Adverse reactions to equine-derived F(ab’)2 -antivenin in 54 dogs envenomated by Vipera berus berus. J. Vet. Emerg. Crit. Care 2013, 23, 532–537. [Google Scholar] [CrossRef]
- Estrada, R.; Herrera, M.; Segura, Á.; Araya, J.; Boschini, C.; Gutiérrez, J.M.; León, G. Intravenous administration of equine-derived whole IgG antivenom does not induce early adverse reactions in non-envenomed horses and cows. Biologicals 2010, 38, 664–669. [Google Scholar] [CrossRef]
- Abraham, R.B.; Winkler, E.; Eshel, G.; Barzilay, Z.; Paret, G. Snakebite poisoning in children—A call for unified clinical guidelines. Eur. J. Emerg. Med. 2001, 8, 189–192. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A sinmple method of estimating fifty per cent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
| Antivenom Characteristic | Kamada | Viper-Stat | European |
|---|---|---|---|
| Product | Vipera palaestinae antiserum | Viper-stat® | European viper venom antiserum |
| Manufacturer | Kamada Ltd., Israel | BioVeteria, Life Sciences, LLC, Mexico | Institute of Immunology, Croatia |
| Type | Whole Ig, monovalent | F(ab)2, polyvalent | F(ab)2, polyvalent |
| Source | Horse plasma | Horse plasma | Horse plasma |
| Use | Human and veterinary | Veterinary | Human and veterinary |
| Active components in 10 mL dose | 1000 PD50 Vipera palaestinea | 250 PD50 Vipera paleestinea | 500 PD50 Vipera xantinae |
| (As declared by the manufacturer) | 250 PD50 Macrovipera lebetina obtuse | 1000 PD50 Vipera ammodytes | |
| 250 PD50 Naja palida | 1000 PD50 Vipera aspis | ||
| 250 PD50 Walterinesia aegyptia | 500 PD50 Vipera berus | ||
| 500 PD50 Bitis aretans | 500 PD50 Vipera lebetinae | ||
| 500 PD50 Cerastes cerastes | |||
| 500 PD50 Naja haja | |||
| 200 PD50 Echis leucogaster | |||
| 200 PD50 Macrovipera deserti | |||
| Recommended starting dosage | 10 mL (50 mL for humans) | 20 mL | 10 mL |
| Tube Number | Dose of Venom per Mouse (µg/0.5 mL) | Venom Concentration (µg/mL) | Volume from the Venom Stock Solution (100 µg/mL) | PBS (mL) |
|---|---|---|---|---|
| 1 | 5 | 10 | 0.4 | 3.6 |
| 2 | 6.25 | 12.5 | 0.5 | 3.5 |
| 3 | 7.5 | 15 | 0.6 | 3.4 |
| 4 | 8.75 | 17.5 | 0.7 | 3.3 |
| 5 | 10 | 20 | 0.8 | 3.2 |
| 6 | 11.25 | 22.5 | 0.9 | 3.1 |
| 7 | 12.5 | 25 | 1 | 3 |
| 8 | 13.75 | 27.5 | 1.1 | 2.9 |
| 9 | 15 | 30 | 1.2 | 2.8 |
| 10 | 16.25 | 32.5 | 1.3 | 2.7 |
| 11 | 17.5 | 35 | 1.4 | 2.6 |
| 12 | 18.75 | 37.5 | 1.5 | 2.5 |
| 13 | 20 | 40 | 1.6 | 2.4 |
| 14 | 21.25 | 42.5 | 1.7 | 2.3 |
| 15 | 22.5 | 45 | 1.8 | 2.2 |
| 16 | 23.75 | 47.5 | 1.9 | 2.1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tirosh-Levy, S.; Solomovich-Manor, R.; Comte, J.; Nissan, I.; Sutton, G.A.; Gabay, A.; Gazit, E.; Steinman, A. Daboia (Vipera) palaestinae Envenomation in 123 Horses: Treatment and Efficacy of Antivenom Administration. Toxins 2019, 11, 168. https://doi.org/10.3390/toxins11030168
Tirosh-Levy S, Solomovich-Manor R, Comte J, Nissan I, Sutton GA, Gabay A, Gazit E, Steinman A. Daboia (Vipera) palaestinae Envenomation in 123 Horses: Treatment and Efficacy of Antivenom Administration. Toxins. 2019; 11(3):168. https://doi.org/10.3390/toxins11030168
Chicago/Turabian StyleTirosh-Levy, Sharon, Reut Solomovich-Manor, Judith Comte, Israel Nissan, Gila A. Sutton, Annie Gabay, Emanuel Gazit, and Amir Steinman. 2019. "Daboia (Vipera) palaestinae Envenomation in 123 Horses: Treatment and Efficacy of Antivenom Administration" Toxins 11, no. 3: 168. https://doi.org/10.3390/toxins11030168
APA StyleTirosh-Levy, S., Solomovich-Manor, R., Comte, J., Nissan, I., Sutton, G. A., Gabay, A., Gazit, E., & Steinman, A. (2019). Daboia (Vipera) palaestinae Envenomation in 123 Horses: Treatment and Efficacy of Antivenom Administration. Toxins, 11(3), 168. https://doi.org/10.3390/toxins11030168







