Discrepancy between Knowledge and Perceptions of Dietary Omega-3 Fatty Acid Intake Compared with the Omega-3 Index
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, and Setting
2.2. Subject Recruitment
2.3. Study Instruments and Biochemical Measures
2.4. Data Analysis
3. Results
3.1. Participants
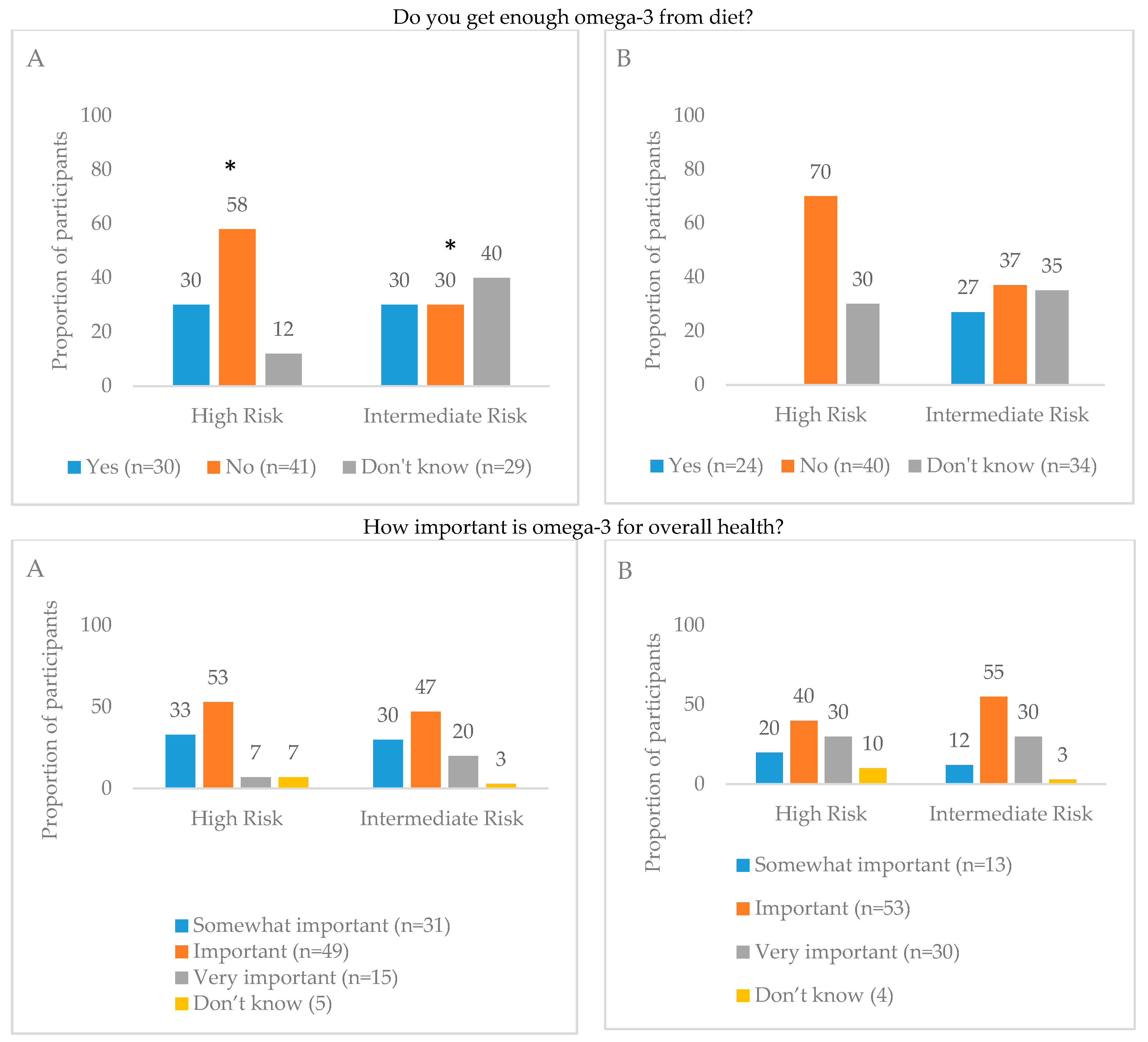
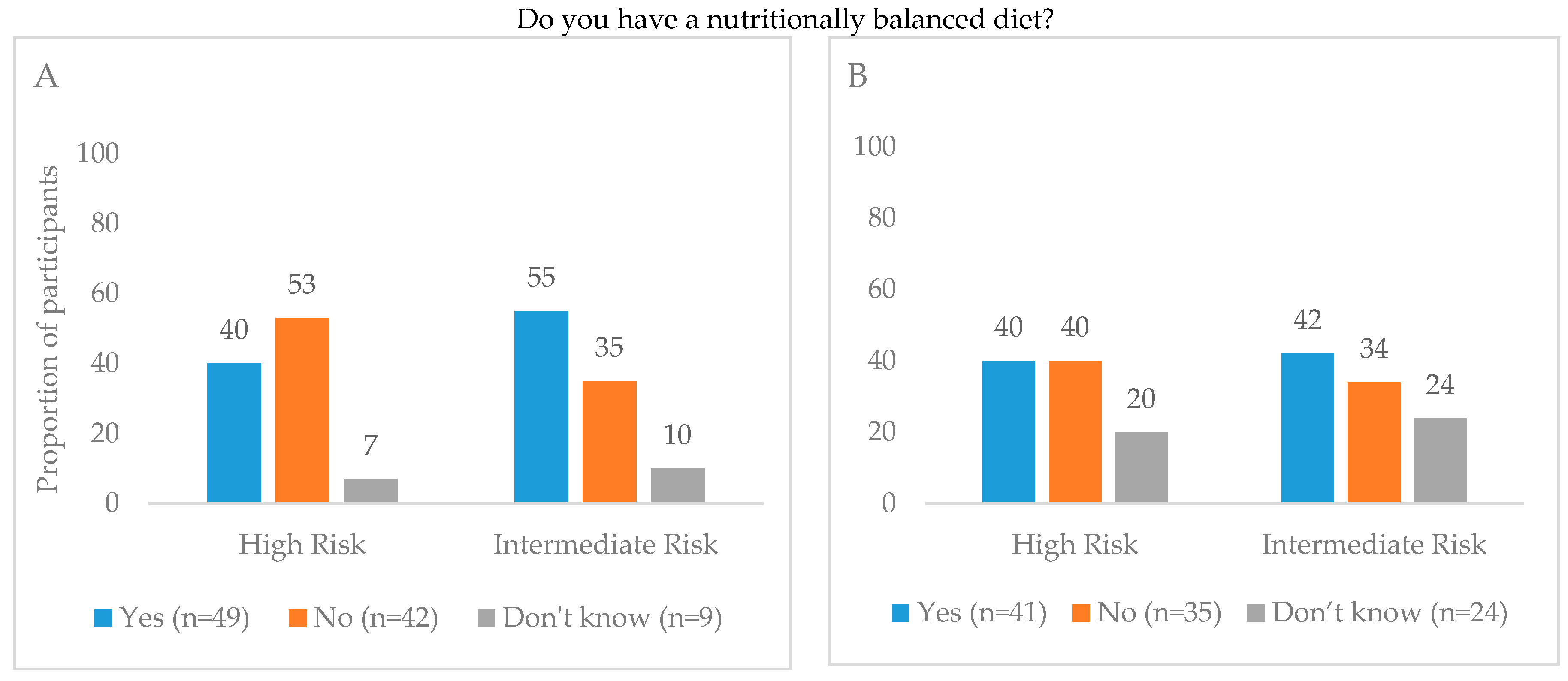
3.2. Perceptions of Diet
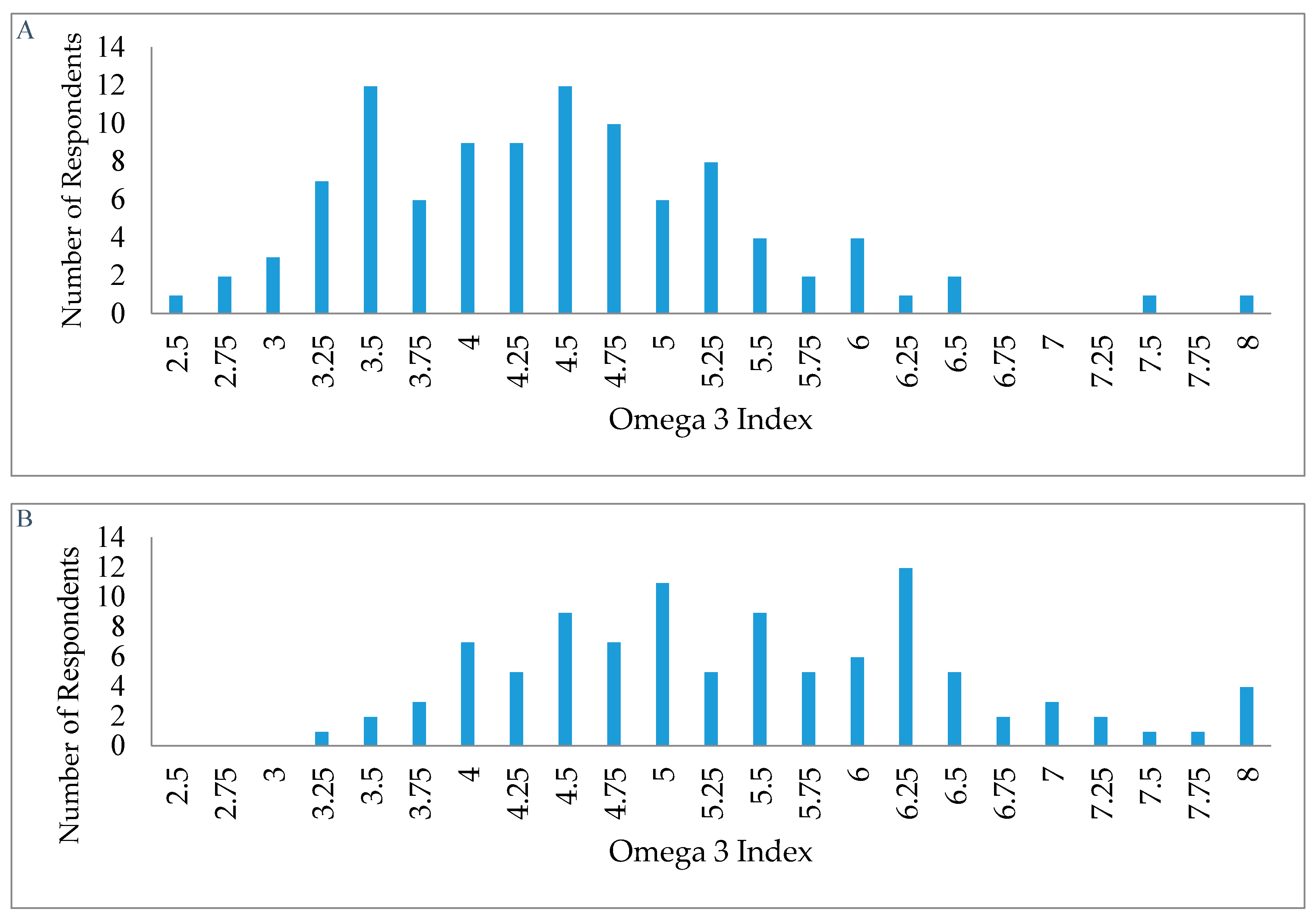
3.3. Biomarker of O3 Status
3.4. Comparison of Dietary Perceptions and Biomarker Status
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- American Dietetic Association. Position of the American dietetic association: Fortification and nutritional supplements. J. Am. Diet. Assoc. 2005, 105, 1300–1311. [Google Scholar]
- Fulgoni, V.L.; Keast, D.R.; Bailey, R.L.; Dwyer, J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J. Nutr. 2011, 141, 1847–1854. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Fulgoni, V.L.; Keast, D.R.; Lentino, C.V.; Dwyer, J.T. Do dietary supplements improve micronutrient sufficiency in children and adolescents? J. Pediatr. 2012, 161, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Gahche, J.J.; Miller, P.E.; Thomas, P.R.; Dwyer, J.T. Why us adults use dietary supplements. JAMA Intern. Med. 2013, 173, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Fulgoni, V.L.; Keast, D.R.; Dwyer, J.T. Examination of vitamin intakes among us adults by dietary supplement use. J. Acad. Nutr. Diet 2012, 112, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Fulgoni, V.L.; Keast, D.R.; Dwyer, J.T. Dietary supplement use is associated with higher intakes of minerals from food sources. Am. J. Clin. Nutr. 2011, 94, 1376–1381. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.A.; Yu, E.A.; Ciappio, E.D.; Mehta, S.; McBurney, M.I. Suboptimal plasma long chain n-3 concentrations are common among adults in the united states, NHANES 2003-2004. Nutrients 2015, 7, 10282–10289. [Google Scholar] [CrossRef] [PubMed]
- Papanikolaou, Y.; Brooks, J.; Reider, C.; Fulgoni, V.L. U.S. Adults are not meeting recommended levels for fish and omega-3 fatty acid intake: Results of an analysis using observational data from NHANES 2003-2008. Nutr. J. 2014, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Stark, K.D.; van Elswyk, M.E.; Higgins, M.R.; Weatherford, C.A.; Salem, N., Jr. Global survey of the omega-3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the blood stream of healthy adults. Prog. Lipid Res. 2016, 63, 132–152. [Google Scholar] [CrossRef] [PubMed]
- US Department of Agriculture; US Department of Health and Human Services. Dietary Guidelines for Americans, 2015-2020, 7th ed.; US Government Printing Office: Washington, DC, USA, 2015.
- German Nutrition Society. The Nutrition Report 2012; Federal Ministry of Food, Agriculture and Consumer Protection: Bonn, Germany, 2012. [Google Scholar]
- Kris-Etherton, P.M.; Hill, A.M. N-3 fatty acids: Food or supplements? J. Am. Diet Assoc. 2008, 108, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Denby, N.; Haycock, B.; Sherif, K.; Steinbaum, S.; von Schacky, C. Perceptions of a healthy diet: Insights from a 3-country survey. Nutr. Today 2015, 50, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Flock, M.R.; Skulas-Ray, A.C.; Harris, W.S.; Etherton, T.D.; Fleming, J.A.; Kris-Etherton, P.M. Determinants of erythrocyte omega-3 fatty acid content in response to fish oil supplementation: A dose-response randomized controlled trial. J. Am. Heart Assoc. 2013, 2, e000513. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.S. The omega-3 index as a risk factor for coronary heart disease. Am. J. Clin. Nutr. 2008, 87, 1997S–2002S. [Google Scholar] [PubMed]
- Harris, W.S.; von Schacky, C. The omega-3 index: A new risk factor for death from coronary heart disease? Prev. Med. 2004, 39, 212–220. [Google Scholar] [CrossRef] [PubMed]
- National Institues of Health. Omega-3 Fatty Acids—Fact Sheet for Health Professionals. Available online: https://ods.od.nih.gov/factsheets/Omega3FattyAcids-HealthProfessional/ (accessed on 1 December 2017).
- Bauch, A.; Lindtner, O.; Mensink, G.B.; Niemann, B. Dietary intake and sources of long-chain n-3 pufas in german adults. Eur. J. Clin. Nutr. 2006, 60, 810–812. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, B.; Brothersen, C.; McMahon, D.J. Fortification of foods with omega-3 polyunsaturated fatty acids. Crit. Rev. Food Sci. Nutr. 2014, 54, 98–114. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.S. N-3 fatty acid fortification: Opportunities and obstacles. Br. J. Nutr. 2007, 97, 593–595. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.S. The omega-3 index: From biomarker to risk marker to risk factor. Curr. Atheroscler. Rep. 2009, 11, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.P.; Aggarwal, K.K.; Zhang, P.Y. Omega-3 fatty acids and cardiovascular disease. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 441–445. [Google Scholar] [PubMed]
- Mori, T.A. Omega-3 fatty acids and cardiovascular disease: Epidemiology and effects on cardiometabolic risk factors. Food Funct. 2014, 5, 2004–2019. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Lemaitre, R.N.; King, I.B.; Song, X.; Spiegelman, D.; Sacks, F.M.; Rimm, E.B.; Siscovick, D.S. Circulating long-chain omega-3 fatty acids and incidence of congestive heart failure in older adults: The cardiovascular health study: A cohort study. Ann. Intern. Med. 2011, 155, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Patterson, A.C.; Chalil, A.; Aristizabal Henao, J.J.; Streit, I.T.; Stark, K.D. Omega-3 polyunsaturated fatty acid blood biomarkers increase linearly in men and women after tightly controlled intakes of 0.25, 0.5, and 1 g/d of EPA + DHA. Nutr. Res. 2015, 35, 1040–1051. [Google Scholar] [CrossRef] [PubMed]
- Superko, H.R.; Superko, S.M.; Nasir, K.; Agatston, A.; Garrett, B.C. Omega-3 fatty acid blood levels: Clinical significance and controversy. Circulation 2013, 128, 2154–2161. [Google Scholar] [CrossRef] [PubMed]
- Tatsuno, I. Omega-3 polyunsaturated fatty acids and cardiovascular disease: An emphasis on omega-3-acid ethyl esters 90 for the treatment of hypertriglyceridemia. Expert Rev. Cardiovasc. Ther. 2014, 12, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Norwegian Seafood Council. The 2014 seafood study. In Insights and Outlook: How the German Eat Fish; Norwegian Seafood Council: Tromsø, Norway, 2014. [Google Scholar]
- Johnsosn, A.A.; Swift, J. Validity of perceptions of a healthy diet. FASEB J. 2011, 25, 353.2. [Google Scholar]
- Levings, J.L.; Maalouf, J.; Tong, X.; Cogswell, M.E. Reported use and perceived understanding of sodium information on US nutrition labels. Prev. Chronic Dis. 2015, 12, E48. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.M.; Cassady, D.L. The effects of nutrition knowledge on food label use. A review of the literature. Appetite 2015, 92, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Sauvageot, N.; Malan, L.; Shivappa, N.; Hebert, J.R. Association between nutritional awareness and diet quality: Evidence from the observation of cardiovascular risk factors in Luxembourg (ORISCAV-LUX) study. Nutrients 2015, 7, 2823–2838. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Wang, Y. Do nutrition knowledge and beliefs modify the association of socio-economic factors and diet quality among us adults? Prev. Med. 2008, 46, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Dallongeville, J.; Marecaux, N.; Cottel, D.; Bingham, A.; Amouyel, P. Association between nutrition knowledge and nutritional intake in middle-aged men from northern france. Public Health Nutr. 2001, 4, 27–33. [Google Scholar] [CrossRef] [PubMed]
- McLeod, E.R.; Campbell, K.J.; Hesketh, K.D. Nutrition knowledge: A mediator between socioeconomic position and diet quality in Australian first-time mothers. J. Am. Diet. Assoc. 2011, 111, 696–704. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.S. The omega-3 index: Clinical utility for therapeutic intervention. Curr. Cardiol. Rep. 2010, 12, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Block, R.C.; Harris, W.S.; Pottala, J.V. Determinants of blood cell omega-3 fatty acid content. Open Biomark J. 2008, 1, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, A.C.; Amin, A.P.; Harris, W.S.; Chan, P.S.; Gosch, K.L.; Rich, M.W.; O’Keefe, J.H., Jr.; Spertus, J.A. Predictors of omega-3 index in patients with acute myocardial infarction. Mayo Clin. Proc. 2011, 86, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Albert, B.B.; Derraik, J.G.; Brennan, C.M.; Biggs, J.B.; Smith, G.C.; Garg, M.L.; Cameron-Smith, D.; Hofman, P.L.; Cutfield, W.S. Higher omega-3 index is associated with increased insulin sensitivity and more favourable metabolic profile in middle-aged overweight men. Sci. Rep. 2014, 4, 6697. [Google Scholar] [CrossRef] [PubMed]
- Mangano, K.M.; Kerstetter, J.E.; Kenny, A.M.; Insogna, K.L.; Walsh, S.J. An investigation of the association between omega 3 fa and bone mineral density among older adults: Results from the national health and nutrition examination survey years 2005-2008. Osteoporos Int. 2014, 25, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Carney, R.M.; Steinmeyer, B.C.; Freedland, K.E.; Rubin, E.H.; Rich, M.W.; Harris, W.S. Baseline blood levels of omega-3 and depression remission: A secondary analysis of data from a placebo-controlled trial of omega-3 supplements. J. Clin. Psychiatry 2016, 77, e138–143. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Pajak, A.; Marventano, S.; Castellano, S.; Galvano, F.; Bucolo, C.; Drago, F.; Caraci, F. Role of omega-3 fatty acids in the treatment of depressive disorders: A comprehensive meta-analysis of randomized clinical trials. PLoS ONE 2014, 9, e96905. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.C. Omega-3 fatty acids and major depression: A primer for the mental health professional. Lipids Health Dis. 2004, 3, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, I.; Hughes, M.; Rowsell, R.; Cockerell, R.; Pipingas, A.; Crewther, S.; Crewther, D. Omega-3 supplementation improves cognition and modifies brain activation in young adults. Hum. Psychopharmacol. 2014, 29, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Kulzow, N.; Witte, A.V.; Kerti, L.; Grittner, U.; Schuchardt, J.P.; Hahn, A.; Floel, A. Impact of omega-3 fatty acid supplementation on memory functions in healthy older adults. J. Alzheimers Dis. 2016, 51, 713–725. [Google Scholar] [CrossRef] [PubMed]
- Lukaschek, K.; von Schacky, C.; Kruse, J.; Ladwig, K.H. Cognitive impairment is associated with a low omega-3 index in the elderly: Results from the KORA-Age study. Dement. Geriatr. Cogn. Disord. 2016, 42, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Van der Wurff, I.S.; von Schacky, C.; Berge, K.; Zeegers, M.P.; Kirschner, P.A.; de Groot, R.H. Association between blood omega-3 index and cognition in typically developing dutch adolescents. Nutrients 2016, 8, 13. [Google Scholar] [CrossRef] [PubMed]
- Hibbeln, J.R.; Davis, J.M.; Steer, C.; Emmett, P.; Rogers, I.; Williams, C.; Golding, J. Maternal seafood consumption in pregnancy and neurodevelopmental outcomes in childhood (ALSPAC study): An observational cohort study. Lancet 2007, 369, 578–585. [Google Scholar] [CrossRef]
- Jensen, C.L. Effects of n-3 fatty acids during pregnancy and lactation. Am. J. Clin. Nutr. 2006, 83, 1452S–1457S. [Google Scholar] [PubMed]
- Oken, E.; Bellinger, D.C. Fish consumption, methylmercury and child neurodevelopment. Curr. Opin. Pediatr. 2008, 20, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Furuhjelm, C.; Warstedt, K.; Larsson, J.; Fredriksson, M.; Bottcher, M.F.; Falth-Magnusson, K.; Duchen, K. Fish oil supplementation in pregnancy and lactation may decrease the risk of infant allergy. Acta Paediatr. 2009, 98, 1461–1467. [Google Scholar] [CrossRef] [PubMed]
| United States | Germany | |||||||
|---|---|---|---|---|---|---|---|---|
| All 2 (n = 100) | Men (n = 46) | Women (n = 52) | p-Value | All (n = 100) | Men (n = 35) | Women (n = 65) | p-Value | |
| Age in years, mean (SD) a | 29 (10) | 28 (8) | 31 (12) | 0.225 | 40 (14) | 41 (14) | 40 (15) | 0.722 |
| Education% (n) b | ||||||||
| High school and above | 100 (100) | 100 (46) | 100 (52) | 0.354 | 94 (93) | 97 (33) | 92 (60) | 0.347 |
| Frequency of Exercise, % (n) b | ||||||||
| 1–2 days a week | 28 (28) | 30 (14) | 27 (14) | 0.367 | 67 (49) | 68 (19) | 67 (30) | 0.358 |
| 3–4 days a week | 51 (50) | 41 (19) | 58 (30) | 29 (21) | 32 (9) | 27 (12) | ||
| Everyday | 21 (21) | 29 (13) | 15 (8) | 4 (3) | - | 6 (3) | ||
| Tobacco Use% (n) b | ||||||||
| Never | 82 (82) | 74 (34) | 90 (47) | 0.191 | 54 (54) | 60 (21) | 51 (33) | 0.538 |
| Former | 14 (14) | 17 (8) | 10 (5) | 20 (20) | 14 (5) | 23 (15) | ||
| Current | 3 (3) | 7 (3) | 0 | 26 (26) | 26 (9) | 26 (17) | ||
| Use of alcohol, % (n) b | ||||||||
| Every day | 2 (2) | 0 | 4 (2) | 0.244 | 5 (5) | 6 (2) | 5 (3) | 0.459 |
| Some days | 85 (85) | 91 (42) | 81 (42) | 84 (84) | 88 (31) | 81 (53) | ||
| Never | 13 (13) | 9 (4) | 15 (8) | 11 (11) | 6 (2) | 14 (9) | ||
| Body Mass Index, kg/m2, Mean (SD) a | 25 (5) | 26 (4) | 24 (5) | 0.040 | 24 (4) | 25 (3) | 24 (3) | 0.036 |
| United States | |||||||
| By Sex 2 | Do you think you get enough amounts of O3 from your diet? | ||||||
| All (n = 100) | Men (n = 46) | Women (n = 52) | p-value | Yes (n = 30) | No (n = 41) | Unsure (n = 29) | p-value |
| 4.3 (4.1–4.5) | 3.8 (3.6–4.1) | 4.8 (4.5–5.0) | <0.0001 | 4.4 (4.0–4.8) | 4.1 (3.8–4.4) | 4.5 (4.3–4.8) | 0.167 |
| Germany | |||||||
| By Sex | Do you think you get enough amounts of O3 from your diet? | ||||||
| All (n = 100) | Men (n = 35) | Women (n = 65) | p-value | Yes (n = 24) | No (n = 40) | Unsure (n = 34) | p-value |
| 5.5 (5.2–5.7) | 5.3 (4.8–5.8) | 5.6 (5.3–5.9) | 0.369 | 5.7 (5.2–6.2) | 5.2 (4.8–5.6) | 5.6 (5.2–6.1) | 0.322 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thuppal, S.V.; Von Schacky, C.; Harris, W.S.; Sherif, K.D.; Denby, N.; Steinbaum, S.R.; Haycock, B.; Bailey, R.L. Discrepancy between Knowledge and Perceptions of Dietary Omega-3 Fatty Acid Intake Compared with the Omega-3 Index. Nutrients 2017, 9, 930. https://doi.org/10.3390/nu9090930
Thuppal SV, Von Schacky C, Harris WS, Sherif KD, Denby N, Steinbaum SR, Haycock B, Bailey RL. Discrepancy between Knowledge and Perceptions of Dietary Omega-3 Fatty Acid Intake Compared with the Omega-3 Index. Nutrients. 2017; 9(9):930. https://doi.org/10.3390/nu9090930
Chicago/Turabian StyleThuppal, Sowmyanarayanan V., Clemens Von Schacky, William S. Harris, Katherine D. Sherif, Nigel Denby, Suzanne R. Steinbaum, Bryan Haycock, and Regan L. Bailey. 2017. "Discrepancy between Knowledge and Perceptions of Dietary Omega-3 Fatty Acid Intake Compared with the Omega-3 Index" Nutrients 9, no. 9: 930. https://doi.org/10.3390/nu9090930
APA StyleThuppal, S. V., Von Schacky, C., Harris, W. S., Sherif, K. D., Denby, N., Steinbaum, S. R., Haycock, B., & Bailey, R. L. (2017). Discrepancy between Knowledge and Perceptions of Dietary Omega-3 Fatty Acid Intake Compared with the Omega-3 Index. Nutrients, 9(9), 930. https://doi.org/10.3390/nu9090930





