Red Blood Cell Eicosapentaenoic Acid Inversely Relates to MRI-Assessed Carotid Plaque Lipid Core Burden in Elders at High Cardiovascular Risk
Abstract
:1. Introduction
2. Material and Methods
2.1. Setting
2.2. Assessment of Risk Factors and Dietary Habits
2.3. Cell Membrane Fatty Acid Analysis
2.4. Carotid Ultrasonography
2.5. Carotid MRI
2.6. Statistical Analyses
3. Results
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Naghavi, M.; GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 385, 117–171. [Google Scholar]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [PubMed]
- Sannino, A.; Brevetti, L.; Giugliano, G.; Scudiero, F.; Toscano, E.; Mainolfi, C.; Cuocolo, A.; Perrino, C.; Stabile, E.; Trimarco, B.; et al. Non-invasive vulnerable plaque imaging: How do we know that treatment works? Eur. Heart J. Cardiovasc. Imaging. 2014, 15, 1194–1202. [Google Scholar] [CrossRef] [PubMed]
- Siscovick, D.S.; Barringer, T.A.; Fretts, A.M.; Wu, J.H.Y.; Lichtenstein, A.H.; Costello, R.B.; Kris-Etherton, P.M.; Jacobson, T.A.; Engler, M.B.; Alger, H.M.; et al. Omega-3 Polyunsaturated Fatty Acid (Fish Oil) Supplementation and the Prevention of Clinical Cardiovascular Disease: A Science Advisory from the American Heart Association. Circulation. 2017. [Google Scholar] [CrossRef] [PubMed]
- Borow, K.M.; Nelson, J.R.; Mason, R.P. Biologic plausibility, cellular effects, and molecular mechanisms of eicosapentaenoic acid (EPA) in atherosclerosis. Atherosclerosis 2015, 242, 357–366. [Google Scholar] [CrossRef] [PubMed]
- Hodson, L.; Skeaff, C.M.; Fielding, B.A. Fatty acid composition of adipose tissue and blood in humans and its use as a biomarker of dietary intake. Prog. Lipid Res. 2008, 47, 348–380. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.S.; Thomas, R.M. Biological variability of blood omega-3 biomarkers. Clin. Biochem. 2010, 43, 338–340. [Google Scholar] [CrossRef] [PubMed]
- Superko, H.R.; Superko, S.M.; Nasir, K.; Agatston, A.; Garrett, B.C. Omega-3 fatty acid blood levels: Clinical significance and controversy. Circulation 2013, 128, 2154–2161. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.Á.; Corella, D.; Salas-Salvadó, J.; Ros, E.; Covas, M.I.; Fiol, M.; Wärnberg, J.; Arós, F.; Ruíz-Gutiérrez, V.; Lapetra, R.M.L.-R.J.; et al. Cohort profile: Design and methods of the PREDIMED study. Int. J. Epidemiol. 2012, 41, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ballart, J.D.; Piñol, J.L.; Zazpe, I.; Corella, D.; Carrasco, P.; Toledo, E.; Perez-Bauer, M.; Martínez-González, M.Á.; Salas-Salvadó, J.; Martín-Moreno, J.M. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br. J. Nutr. 2010, 103, 1808–1816. [Google Scholar] [CrossRef] [PubMed]
- Moreiras, O.; Carbajal, A.; Cabrera, L.; Cuadrado, C. Tablas de Composición de Alimentos (Food Composition Tables); Ediciones Pirámide S.A.: Madrid, Spain, 2005. [Google Scholar]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65 (Suppl. 4), 1229S–1231S. [Google Scholar]
- Sala-Vila, A.; Harris, W.S.; Cofán, M.; Pérez-Heras, A.M.; Pintó, X.; Lamuela-Raventós, R.M.; Covas, M.-I.; Estruch, R.; Ros, E. Determinants of the omega-3 index in a Mediterranean population at increased risk for CHD. Br. J. Nutr. 2011, 106, 425–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Junyent, M.; Cofán, M.; Núñez, I.; Gilabert, R.; Zambón, D.; Ros, E. Influence of HDL cholesterol on preclinical carotid atherosclerosis in familial hypercholesterolemia. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Koktzoglou, I.; Chung, Y.C.; Mani, V.; Caqrroll, T.J.; Morasch, M.D.; MS, G.M.; Simonetti, O.P.; Fayad, Z.A.; Li, D. Multislice dark-blood carotid artery wall imaging: A 1.5 T and 3.0 T comparison. J. Magn. Reson. Imaging 2006, 23, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Saam, T.; Ferguson, M.S.; Yarnykh, V.L.; Takaya, N.; Xu, D.; Polissar, N.L.; Hatsukami, T.S.; Yuan, C. Quantitative evaluation of carotid plaque composition by in vivo MRI. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.S. The omega-3 index: From biomarker to risk marker to risk factor. Curr. Atheroscler. Rep. 2009, 11, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Polak, J.F.; Pencina, M.J.; Pencina, K.M.; O′Donnell, C.J.; Wolf, P.A.; D′Agostino, R.B. Carotid-wall intima-media thickness and cardiovascular events. N. Engl. J. Med. 2011, 365, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Cawood, A.L.; Ding, R.; Napper, F.L.; Young, R.H.; Williams, J.M.; Ward, M.J.A.; Gudmundsen, O.; Vige, R.; Payne, S.P.K.; Ye, S.; et al. Eicosapentaenoic acid (EPA) from highly concentrated n-3 fatty acid ethyl esters is incorporated into advanced atherosclerotic plaques and higher plaque EPA is associated with decreased plaque inflammation and increased stability. Atherosclerosis 2010, 212, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, M.; Origasa, H.; Matsuzaki, M.; Matsuzawa, Y.; Saito, Y.; Ishikawa, Y.; Oikawa, S.; Sasaki, J.; Hishida, H.; Itakura, H.; et al. Effects of eicosapentaenoic acid (EPA) on major coronary events in hypercholesterolemic patients (JELIS): A randomised open-label blinded endpoint analysis. Lancet 2007, 369, 1090–1098. [Google Scholar] [CrossRef]
- Mason, R.P.; Jacob, R.F.; Shrivastava, S.; Sherratt, S.C.R.; Chattopadhyay, A. Eicosapentaenoic acid reduces membrane fluidity, inhibits cholesterol domain formation, and normalizes bilayer width in atherosclerotic-like model membranes. Biochim. Biophys. Acta 2016, 1858, 3131–3140. [Google Scholar] [CrossRef] [PubMed]
- Guichardant, M.; Calzada, C.; Bernoud-Hubac, N.; Lagarde, M.; Véricel, E. Omega-3 polyunsaturated fatty acids and oxygenated metabolism in atherothrombosis. Biochim. Biophys. Acta. 2015, 1851, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C. The role of marine omega-3 (n-3) fatty acids in inflammatory processes, atherosclerosis and plaque stability. Mol. Nutr. Food. Res. 2012, 56, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Salic, K.; Morrison, M.C.; Verschuren, L.; Wielinga, P.Y.; Wu, L.; Kleemann, R.; Gjorstrup, P.; Kooistra, T. Resolvin E1 attenuates atherosclerosis in absence of cholesterol-lowering effects and on top of atorvastatin. Atherosclerosis 2016, 250, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Fahimi, S.; Lim, S.; Andrews, K.G.; Engell, R.E.; Powles, J.; Ezzati, M.; Mozaffarian, D. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys. BMJ 2014, 348, g2272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gil, M.; Martí, H.; Elosúa, R.; Grau, M.; Sala, J.; Masiá, R.; Pérez, G.; Roset, P.; Bielsa, O.; Vila, J.; et al. Analysis of trends in myocardial infarction case-fatality, incidence and mortality rates in Girona, Spain, 1990–1999. Rev. Esp. Cardiol. 2007, 60, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Cosin, J.; Asin, E.; Marrugat, J.; Elosua, R.; Arós, F.; de los Reyes, M.; Castro-Beiras, A.; Cabadés, A.; Diago, J.L.; López-bescos, L.; Vila, J. Prevalence of angina pectoris in Spain. Eur. J. Epidemiol. 1999, 15, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Bertomeu, A.; García-Vidal, O.; Farré, X.; Galobart, A.; Vázquez, M.; Laguna, J.C.; Ros, E. Preclinical coronary atherosclerosis in a population with low incidence of myocardial infarction: Cross-sectional autopsy study. BMJ 2003, 327, 591–592. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, S.; Fornage, M.; Gillespie, C.; et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics—2017 Update: A Report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, R.; Alonso, M.; Segura, A.; Tormo, M.J.; Artigao, L.M.; Banegas, J.R.; Brotons, C.; Elosua, R.; Fernández-Cruz, A.; Muñiz, J.; et al. Prevalence, geographic distribution, and geographic variability of major cardiovascular risk factors in Spain. Pooled analysis of data from population-based epidemiological studies: The ERICE Study. Rev. Esp. Cardiol. 2008, 61, 1030–1040. [Google Scholar] [CrossRef] [PubMed]
- Hon, G.M.; Abel, S.; Smuts, C.M.; van Jaarsveld, P.; Hassan, M.S.; van Rensburg, S.J.; Erasmus, R.T.; Matsha, T. Gas chromatography results interpretation: Absolute amounts versus relative percentages. In Gas Chromatography-Biochemicals, Narcotics and Essential Oils; Salih, B., Çelikbıçak, O., Eds.; InTech: Rijeka, Croatia, 2012; Available online: https://www.intechopen.com/books/mostdownloaded/gas-chromatography-biochemicals-narcotics-and-essential-oils (accessed on 18 September 2017).
- Stark, K.D.; Van Elswyk, M.E.; Higgins, M.R.; Weatherford, C.A.; Salem, N., Jr. Global survey of the omega-3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the blood stream of healthy adults. Prog. Lipid Res. 2016, 63, 132–152. [Google Scholar] [CrossRef] [PubMed]
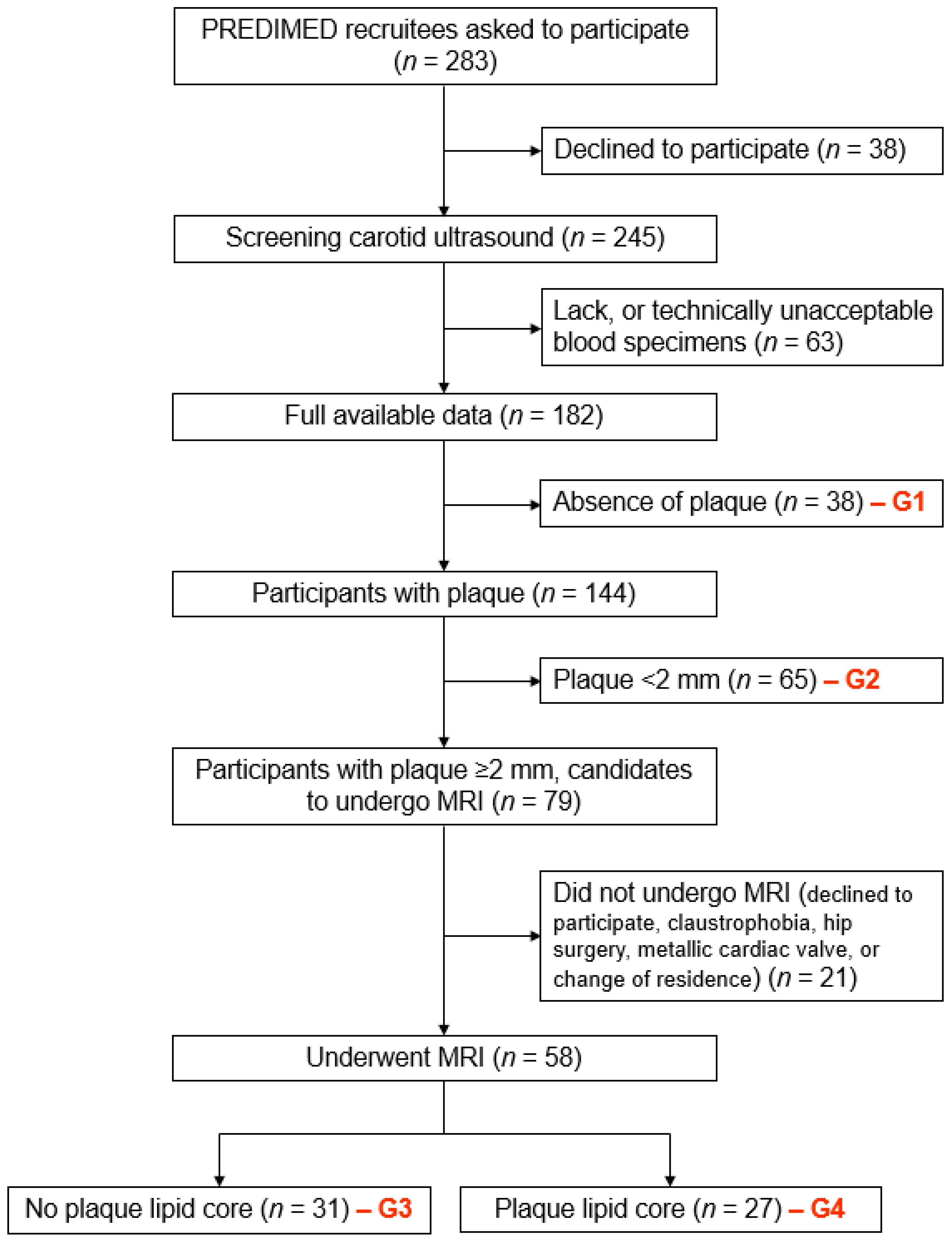
| Variable | Whole Sample (n = 161) | Absence of Plaque–Group 1 (n = 38) | Plaque <2 mm–Group 2 (n = 65) | Plaque ≥2 mm, Absence of Lipid-Rich Necrotic Core–Group 3 (n = 31) | Plaque ≥2 mm, Presence of Lipid-Rich Necrotic Core–Group 4 (n = 27) | P * |
|---|---|---|---|---|---|---|
| Male, no-% | 83 (51.6) | 16 (42.1) | 24 (36.9) | 18 (58.1) | 25 (92.6) | <0.001 |
| Age, years | 65 (61 to 70) | 62 (60 to 66) a | 65 (62 to 71) b | 65 (60 to 70) b | 65 (63 to 72) b | 0.027 |
| Family history of early-onset CHD, no-% | 73 (45.3) | 19 (50.0) | 36 (55.4) | 10 (32.3) | 8 (29.6) | 0.007 |
| Weight, kg | 77.3 (69.2 to 86.3) | 76.4 (69.2 to 84.3) | 75 (66.5 to 87.3) | 76.1 (68.8 to 89.0) | 79.6 (72.6 to 86.4) | 0.623 |
| Body mass index, kg/m2 | 29.3 (27.15 to 31.9) | 28.5 (26.9 to 32.78) | 29.4 (27.6 to 32.4) | 30.2 (27.4 to 31.7) | 28.9 (27.1 to 31.0) | 0.747 |
| Waist circumference, cm | 101 (96 to 107) | 98 (94 to 110) | 100 (96 to 105) | 101 (96 to 108) | 103 (98 to 107) | 0.724 |
| Current smoker, no-% | 30 (18.6) | 6 (15.8) | 8 (12.3) | 8 (25.8) | 8 (29.6) | 0.163 |
| Diabetes, no-% | 71 (44.1) | 13 (34.2) | 27 (41.5) | 16 (51.6) | 15 (55.6) | 0.281 |
| Hypertension, no-% | 119 (73.9) | 26 (68.4) | 48 (73.8) | 24 (77.4) | 21 (77.8) | 0.801 |
| Dyslipidemia, no-% | 112 (69.6) | 23 (60.5) | 48 (73.8) | 23 (74.2) | 18 (66.7) | 0.484 |
| Fasting glucose, mg/dL | 107 (96 to 141) | 102 (91 to 136) | 107 (96 to 139) | 115 (99 to 137) | 121 (98 to 149) | 0.221 |
| Total cholesterol, mg/dL | 211 (185 to 238) | 208 (178 to 236) | 214 (188 to 248) | 205 (181 to 234) | 212 (184 to 237) | 0.388 |
| LDL cholesterol, mg/dL | 134 (108 to 154) | 131 (103 to 155) | 142 (115 to 159) | 126 (111 to 143) | 136 (99 to 151) | 0.369 |
| HDL cholesterol, mg/dL | 50 (43 to 58) | 52 (46 to 63) a | 54 (44 to 60) a | 45 (39 to 55) b | 47 (39 to 49) b | 0.001 |
| Triglycerides, mg/dL | 115 (86 to 161) | 113 (76 to 153) | 107 (79 to 158) | 136 (106 to 179) | 120 (99 to 176) | 0.162 |
| Use of statins, no-% | 69 (49.2) | 13 (34.2) | 29 (44.6) | 13 (41.9) | 14 (51.9) | 0.543 |
| Use of antihypertensive agents, no-% | 104 (64.6) | 24 (63.2) | 40 (61.5) | 22 (71.0) | 18 (66.7) | 0.825 |
| Use of oral antidiabetic agents, no-% | 42 (26.1) | 9 (23.7) | 14 (21.5) | 11 (35.5) | 8 (29.6) | 0.492 |
| Maximum ICA-IMT, mm | -- | 0.75 (0.65 to 0.91) a | 0.93 (0.77 to 1.15) b | 1.11 (0.83 to 1.47) c | 1.14 (0.93 to 1.98) c | <0.001 |
| Plaque burden, mm | -- | -- | 1.98 (1.40 to 3.12) a | 4.89 (3.30 to 7.58) b | 7.00 (4.71 to 11.65) c | <0.001 |
| Normalized wall index | -- | -- | -- | 0.47 (0.43 to 0.50) | 0.50 (0.44 to 0.55) | 0.086 |
| Lipid-rich necrotic core, mm3 | -- | -- | -- | -- | 13.05 (9.14 to 37.27) | -- |
| Variable (g/Day) | Whole Sample (n = 161) | Absence of Plaque–Group 1 (n = 38) | Plaque <2 mm–Group 2 (n = 65) | Plaque ≥2 mm, Absence of Lipid-Rich Necrotic Core–Group 3 (n = 31) | Plaque ≥2 mm, Presence of Lipid-Rich Necrotic Core–Group 4 (n = 27) | P * |
|---|---|---|---|---|---|---|
| Total seafood † | 116 (79 to 145) | 115 (76 to 139) | 117 (86 to 152) | 120 (75 to 145) | 107 (67 to 135) | 0.419 |
| Fatty fish | 19 (9 to 56) | 19 (9 to 56) | 19 (9 to 56) | 19 (9 to 56) | 19 (9 to 56) | 0.643 |
| Lean fish | 64 (21 to 64) | 64 (10 to 64) | 64 (21 to 64) | 64 (21 to 64) | 64 (10 to 64) | 0.571 |
| Dietary EPA + DHA | 0.81 (0.54 to 1.35) | 0.86 (0.56 to 1.39) | 0.84 (0.58 to 1.37) | 0.76 (0.54 to 1.30) | 0.71 (0.50 to 1.29) | 0.612 |
| Fatty Acid (% of Total Fatty Acids) | Whole Sample (n = 161) | Absence of Plaque–Group 1 (n = 38) | Plaque <2 mm–Group 2 (n = 65) | Plaque ≥2 mm, Absence of Lipid-Rich Necrotic Core–Group 3 (n = 31) | Plaque ≥2 mm, Presence of Lipid-Rich Necrotic Core–Group 4 (n = 27) | P * |
|---|---|---|---|---|---|---|
| C18:3n-3 (alpha-linolenic acid) | 0.17 (0.12 to 0.30) | 0.20 (0.13 to 0.30) | 0.17 (0.12 to 0.28) | 0.20 (0.12 to 0.43) | 0.14 (0.12 to 0.21) | 0.409 |
| C20:5n-3 (eicosapentaenoic acid) | 1.00 (0.76 to 1.37) | 1.04 (0.75 to 1.47) | 1.00 (0.78 to 1.20) | 0.87 (0.71 to 1.39) | 1.01 (0.80 to 1.49) | 0.697 |
| C22:6n-3 (docosahexaenoic acid) | 6.15 (5.17 to 6.95) | 5.64 (5.18 to 6.80) | 6.20 (5.12 to 7.02) | 5.93 (4.88 to 7.01) | 6.27 (4.94 to 6.94) | 0.935 |
| Omega-3 index (C20:5n-3 + C22:6n-3) | 7.22 (6.11 to 8.23) | 7.11 (5.99 to 8.16) | 7.29 (6.07 to 8.14) | 7.04 (5.75 to 8.22) | 7.22 (6.89 to 8.77) | 0.631 |
| C20:4n-6 (arachidonic acid) | 16.37 (14.50 to 18.51) | 16.05 (14.55 to 17.32) | 16.89 (14.40 to 18.71) | 15.67 (13.92 to 18.60) | 15.94 (14.90 to 18.09) | 0.224 |
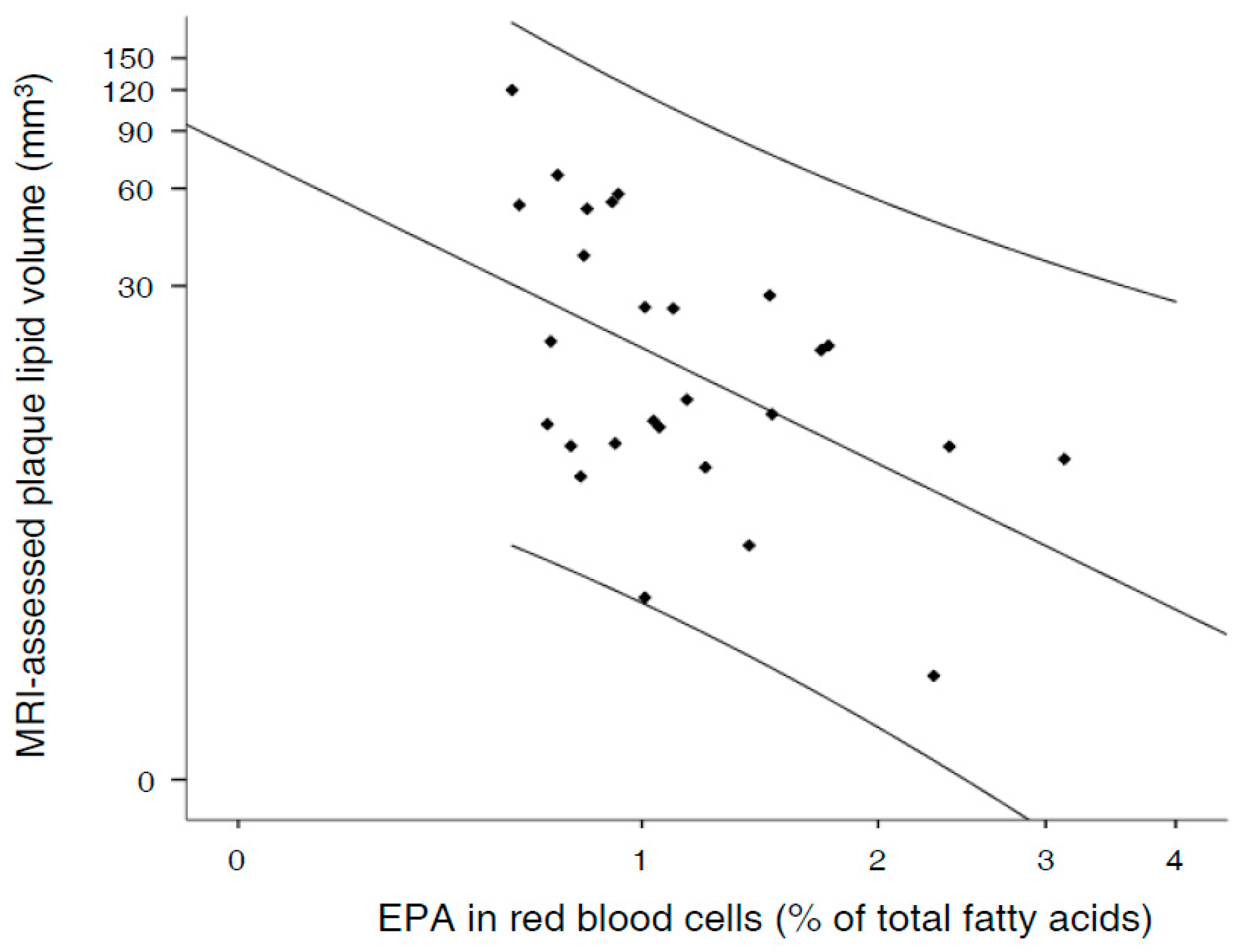
| Independent Variable | B (95% Confidence Interval) | β | p | Adjusted R2 |
|---|---|---|---|---|
| Constant | 6.284 (−119.057 to 131.625) | 0.918 | 0.318 | |
| C20:5n-3 (log transformed) | −31.300 (−57.685 to −4.915) | −0.500 | 0.022 | |
| Sex, female | −19.637 (−62.570 to 23.296) | −0.197 | 0.351 | |
| Age, year | 0.325 (−1.584 to 2.234) | 0.078 | 0.726 | |
| Diabetes at baseline, yes | 7.177 (−14.161 to 28.515) | 0.136 | 0.491 | |
| Ever smoking at baseline, yes | −1.893 (−27.989 to 24.204) | −0.030 | 0.881 | |
| Use of statins at baseline, yes | −1.007 (−22.761 to 20.747) | −0.019 | 0.924 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bargalló, N.; Gilabert, R.; Romero-Mamani, E.-S.; Cofán, M.; Calder, P.C.; Fitó, M.; Corella, D.; Salas-Salvadó, J.; Ruiz-Canela, M.; Estruch, R.; et al. Red Blood Cell Eicosapentaenoic Acid Inversely Relates to MRI-Assessed Carotid Plaque Lipid Core Burden in Elders at High Cardiovascular Risk. Nutrients 2017, 9, 1036. https://doi.org/10.3390/nu9091036
Bargalló N, Gilabert R, Romero-Mamani E-S, Cofán M, Calder PC, Fitó M, Corella D, Salas-Salvadó J, Ruiz-Canela M, Estruch R, et al. Red Blood Cell Eicosapentaenoic Acid Inversely Relates to MRI-Assessed Carotid Plaque Lipid Core Burden in Elders at High Cardiovascular Risk. Nutrients. 2017; 9(9):1036. https://doi.org/10.3390/nu9091036
Chicago/Turabian StyleBargalló, Núria, Rosa Gilabert, Edwin-Saúl Romero-Mamani, Montserrat Cofán, Philip C. Calder, Montserrat Fitó, Dolores Corella, Jordi Salas-Salvadó, Miguel Ruiz-Canela, Ramon Estruch, and et al. 2017. "Red Blood Cell Eicosapentaenoic Acid Inversely Relates to MRI-Assessed Carotid Plaque Lipid Core Burden in Elders at High Cardiovascular Risk" Nutrients 9, no. 9: 1036. https://doi.org/10.3390/nu9091036
APA StyleBargalló, N., Gilabert, R., Romero-Mamani, E.-S., Cofán, M., Calder, P. C., Fitó, M., Corella, D., Salas-Salvadó, J., Ruiz-Canela, M., Estruch, R., Ros, E., & Sala-Vila, A. (2017). Red Blood Cell Eicosapentaenoic Acid Inversely Relates to MRI-Assessed Carotid Plaque Lipid Core Burden in Elders at High Cardiovascular Risk. Nutrients, 9(9), 1036. https://doi.org/10.3390/nu9091036








