Development of the Intervention Materials for the HomeStyles Obesity Prevention Program for Parents of Preschoolers
Abstract
:1. Introduction
2. Development of Intervention Materials
2.1. Advisory Group
2.2. Theoretical Underpinnings
2.3. Philosophical Basis
2.4. Program Structure
| Description and Main Concepts |
|---|
| Healthy HomeStylesThis |
This Guide sets the stage for participating in HomeStyles. All families complete this Guide first.
|
| Family Mealtimes |
This Guide gives parents the secrets to successful family meals. Families do better when they eat together.
|
| Enjoyable Mealtimes |
This Guide helps parents have calmer, more relaxed family meals. Sharing time together at meals strengthens families.
|
| Right Sizing Portions |
This Guide helps parents serve food portions that are “just right”—and keep body weights healthy.
|
| Fuss Free Feeding |
This Guide helps parents teach kids to enjoy new, healthy foods without fussing. The whole family wins when parents use positive feeding practices.
|
| Taming TV |
This Guide helps parents swap TV-time for active playtime and reduce the effects of TV on kids. People who watch TV more than 2 h a day may have problems.
|
| Breakfast, the Right Start |
This Guide helps get the whole family off on the right foot every day.
|
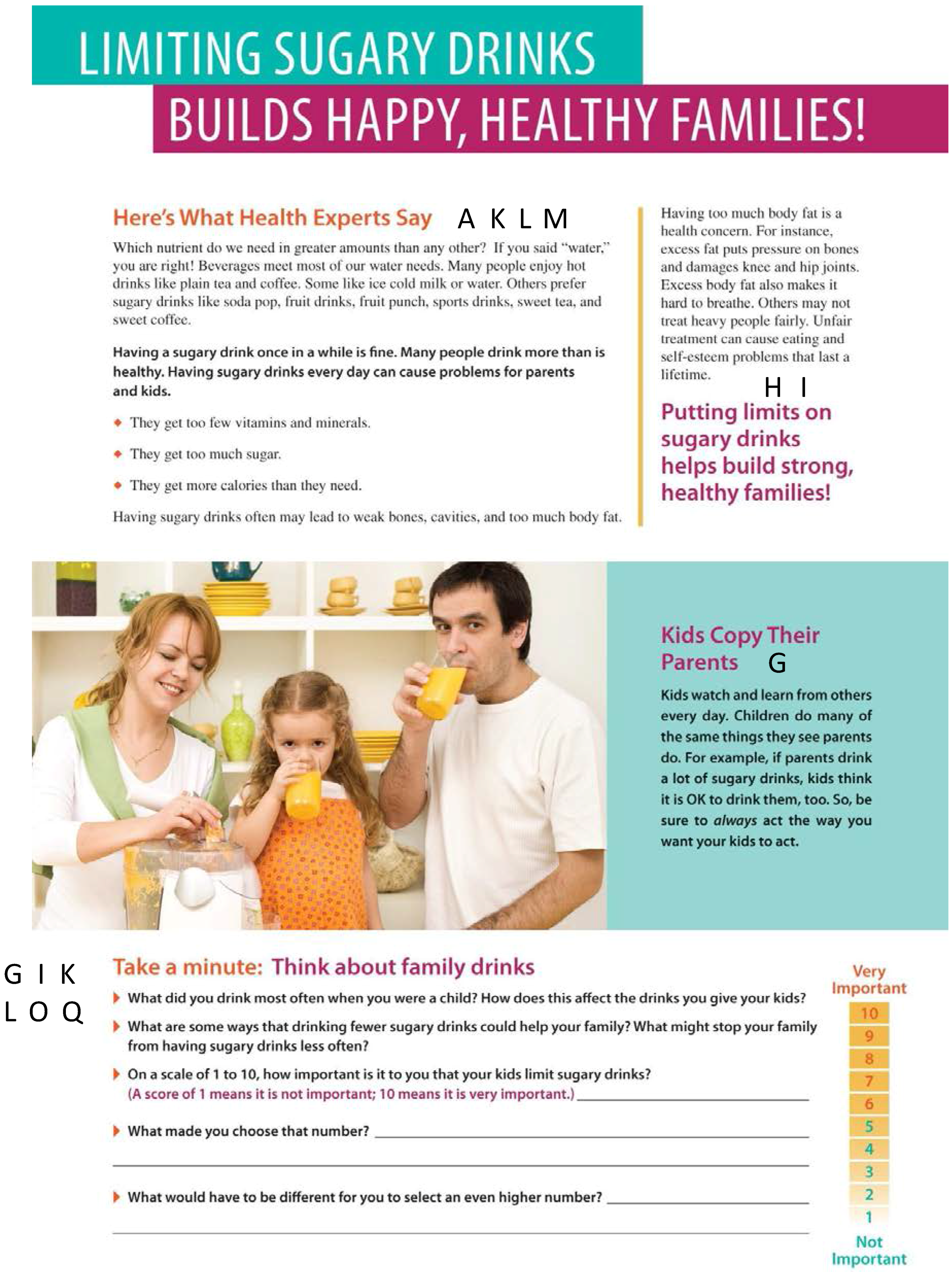
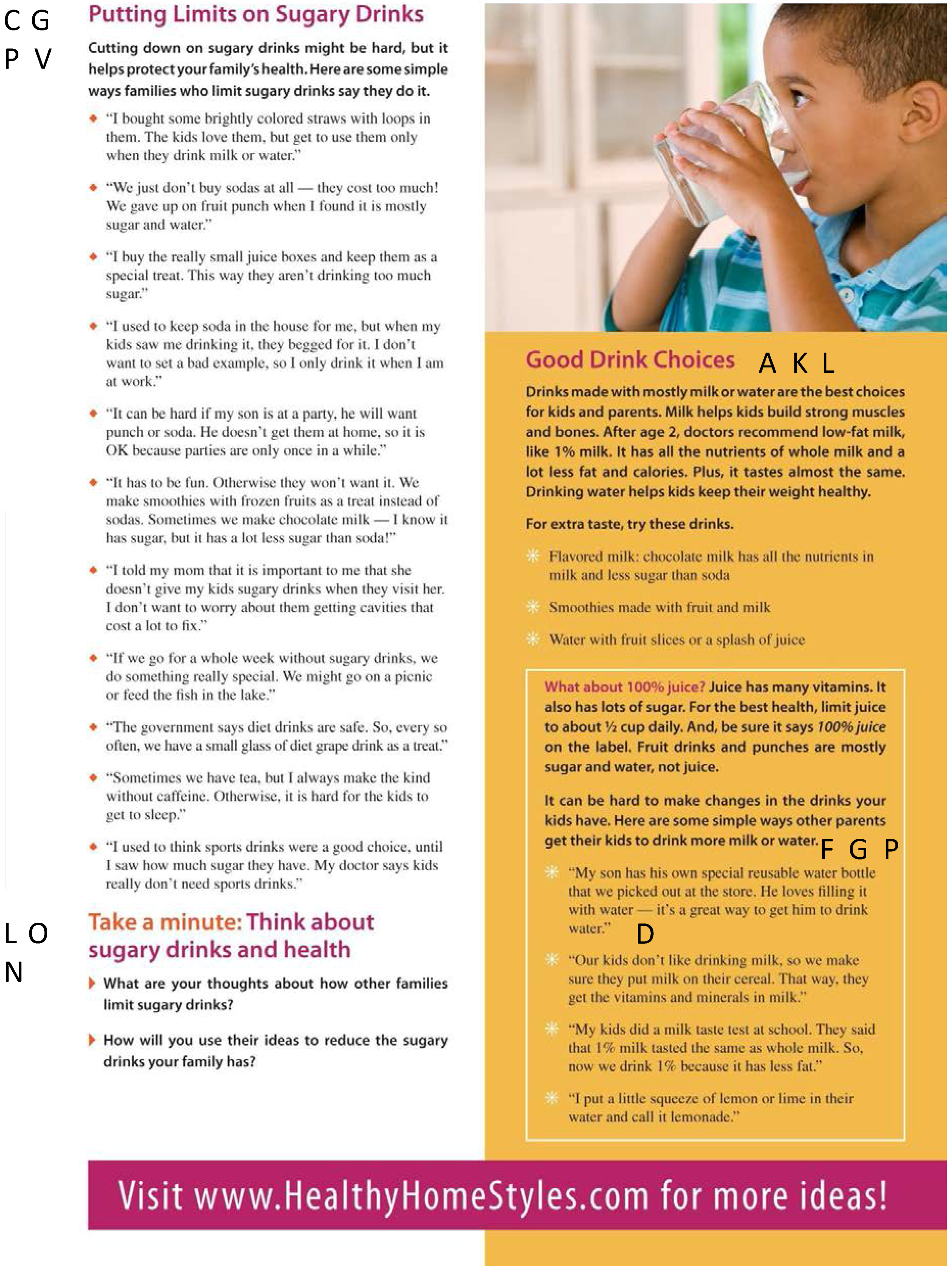
| Best Drinks for Families |
This Guide helps families go for tasty, guilt-free beverages. Having a sugary drink once in a while is fine. Many people drink more than is healthy. Having sugary drinks every day can cause problems for parents and kids.
|
| Play More, Sit Less |
This Guide helps parents trim screen-time and get more family fun time. Getting more than 2 h of screen-time each day can cause problems. Too much screen-time can harm kids.
|
| Time to Play |
This Guide helps families play more and have lots more fun together. Many kids and adults do not spend enough time in physical activity—they should get 60 min each day. Families get benefits like these when they are physically active.
|
| Good night, Sleep right |
This Guide helps families get enough sleep and wake up happy and rested. Many kids and adults do not get enough sleep. Kids who do not get enough sleep may have many problems.
|
2.5. Delivery Mode
2.6. Guide Content
2.7. Guide Development Process
| Here Is What the Experts Say |
| All Guides start with a brief summary of evidence-based research that explains why the Guide’s topic is important to health. |
| Kids Copy Their Parents |
| This section helps parents remember they are their children’s most important role model. |
| Take a Minute |
| These sections give parents a chance to think about why the behaviors discussed in the Guide are important to them personally. These sections also provide opportunities to use motivational interviewing techniques to help families make simple changes to build healthier families. |
| Here’s What Other Parents are Saying |
| This section provides tips and ideas from actual families with preschoolers. It helps parents know they are not alone, and that other families have successfully made changes to improve their kids’ health. |
| Even More |
| This section provides more tips and ideas specific to the Guide to help parents raise happier, healthier, safer kids. |
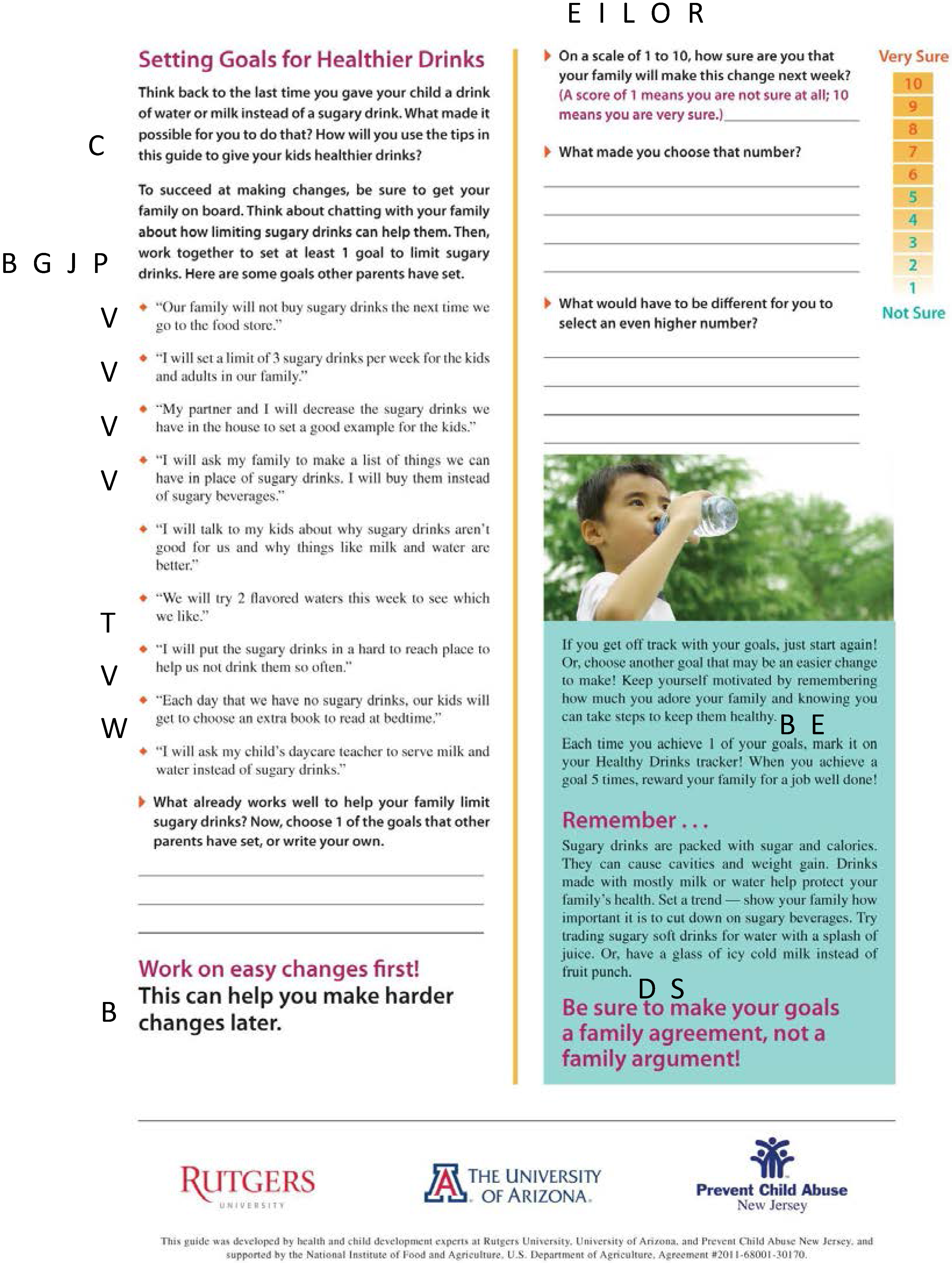
| Goal Setting |
| This section helps parents set small, attainable goals to improve their kids’ health. Parents can set their own goal or choose from the examples other families have set. |
| Remember |
| This section sums up the Guide. It also reminds families to take small, manageable steps and remember that the changes they are making are important for their family! |
3. Application of Behavior Change and Motivational Interviewing Strategies
| Letters in Black Boxes in Figure 2 | Behavior Change Strategy |
|---|---|
| A | Outcome Expectations [91] Beliefs about the likelihood and value placed on the consequences of behavioral choices. |
| B | Behavioral Capability [91] Having the necessary knowledge and skills to change a behavior. |
| C | Self-efficacy [90,91] Confidence in one’s ability to perform a behavior. |
| Supporting Self-efficacy [2] Giving a person the opportunity to express self-confidence. | |
| D | Reinforcement [91] Outcomes that give support (or take away support) for performing a behavior. Most commonly positive reinforcement to reward an individual for making a behavior change. |
| E | Self-regulation [91] Controlling oneself through self-monitoring, goal-setting, feedback, self-reward, self-instruction, and enlistment of social support |
| F | Address Barriers [91,106] Identify real or perceived factors preventing behavior change. Also called Roadblocks. |
| G | Observational Learning/Modeling [91] Learning to perform new behaviors by exposure to interpersonal or media displays of them, particularly through peer modeling |
| H | Eliciting Change [106] Examines reasons for changing a behavior. |
| I | Exploring Importance [106] Examines importance of changing a behavior. |
| J | Goal-Setting [90,91,106] Setting goals for changing a behavior (related to Self-regulation). |
| K | Rewards [106] Identifies benefits of changing a behavior that are most important to a person. |
| L | Relevance [90,106] Examines why changing behavior is important to a person. |
| M | Risk [106] Identifies the risks that a person feels are most important to avoid. |
| N | Repetition [106] Revisits questions when a person indicates resistance/ambivalence to changing a behavior. |
| O | Reflection [106] Asking open-ended questions that give a person an opportunity to think and reflect. |
| P | Normalizing [106] Helping a person to understand that personal feelings/experiences/challenges while making change are common and normal. |
| Q | Decisional Balance [106] Comparing “good” and “not so good” outcomes about changing a behavior. |
| R | Readiness to Change Scale [106] Rating change reading using a 10-point scale where 1 = definitely not ready to change and 10 = definitely ready to change. |
| S | Summaries [90] Reminds a person of main aspects of changing behavior made in the current session. |
| T | Specifying Target Behaviors [90] Identifying the specific behaviors that need to change. |
| U | Self-Monitoring [91,106] Keeping track of specific behavior that is targeted for change each time it occurs. |
| V | Stimulus Control [90] Changing and structuring the environment (usually the home) to make it easier to perform a behavior (e.g., eat healthier foods) or avoid performing a behavior (e.g., eating unhealthy foods). |
| W | Positive Reinforcement Strategies [90,106] Using praise and recognition of changes that have already occurred to encourage change. |
4. Cognitive Testing Findings
4.1. Home Visitor Content Cognitive Testing
4.2. Parent Content Cognitive Testing
| Guide Content Characteristic | Mean ± SD |
|---|---|
| Interest Level | 4.70 ± 0.68 a |
| Usefulness | 4.78 ± 0.59 a |
| Relevancy | 4.62 ± 0.72 a |
| Clarity | 4.66 ± 0.63 a |
| Reading Ease | 4.65 ± 0.65 a |
| Appeal | 4.50 ± 0.93 a |
| Likelihood to Improve Practices | 4.53 ± 0.82 a |
| Time Needed to Read | 2.09 ± 0.41 b |
| Tone | 2.91 ± 0.30 c |
| Knowledge Change after Reading Guide | 2.88 ± 0.32 d |
| Importance Placed on Engaging in Practices Described After Reading Guide | 2.90 ± 0.30 d |
4.3. Home Visitor Design Cognitive Testing
4.4. Parent Design Cognitive Testing
5. Comparison of Cognitive Testing Findings with HomeStyles Theoretical Underpinnings and Philosophy
6. Discussion
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References and Notes
- Kelder, S.; Perry, C.; Klepp, K.; Lytle, L. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am. J. Public Health 1994, 84, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Twisk, J.; Kemper, H.; Mechelen, W. Tracking of activity and fitness and the relationship with cardiovascular disease risk factors. Med. Sci. Sports Exerc. 2000, 32, 1455–1461. [Google Scholar] [CrossRef] [PubMed]
- Twisk, J.; Kemper, H.; van Mechelen, W.; Post, G. Tracking of risk factors for coronary heart disease over a 14-year period: A comparison between lifestyle and biologic risk factors with data from the amsterdam growth and health study. Am. J. Epidemiol. 1997, 145, 888–898. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.; Savage, J.; Ventura, A. Influences on the development of children’s eating beahviours: From infancy to adolescence. Can. J. Diet. Pract. Res. 2007, 68, s1–s56. [Google Scholar] [PubMed]
- Rosenkranz, R.; Dzewaltowski, D. Model of the home food environment pertaining to childhood obesity. Nutr. Rev. 2008, 66, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.; Davison, K. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr. Clin. N. Am. 2001, 48, 893–907. [Google Scholar] [CrossRef]
- Brustad, R. Attraction to physical activity in urban schoolchildren: Parental socialization and gender influences. Res. Q. Exerc. Sports 1996, 67, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Demsey, J.; Kimiecik, J.; Horn, T. Parental influence on children’s moderate to vigorous physical activity participation: An expectancy-value approach. Pediatr. Exerc. 1993, 5, 151–167. [Google Scholar]
- Gruber, K.; Haldeman, L. Using the family to combat childhood and adult obesity. Prev. Chronic Dis. 2009, 6, A106. [Google Scholar] [PubMed]
- Lau, R.; Quadrell, J.; Hartman, K. Development and change of young adults’ preventive health beliefs and behavior: Influence from parents and peers. J. Health Soc. Behav. 1990, 31, 240–259. [Google Scholar] [CrossRef] [PubMed]
- Nichlas, T.; Hayes, D. Position of the American dietetic association: Nutrition guidance for healthy children ages 2 to 11 years. J. Am. Diet. Assoc. 2006, 106, 1038–1047. [Google Scholar]
- Patterson, T.; Sallis, J.; Nader, P.; Kaplan, R.; Rupp, J. Familial similarities of changes in cognitive, behavioral and physiological variables in a cardiovascular health promotion program. J. Pediatr. Psychol. 1989, 14, 277–292. [Google Scholar] [CrossRef] [PubMed]
- Sahay, T.; Ashbury, F.; Roberts, M.; Rootman, I. Effective components for nutrition interventions: A review and application of the literature. Health Promot. Pract. 2006, 7, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Skouteris, H.; McCabe, M.; Winburn, B.; Newbreen, V.; Sacher, P.; Chadwick, P. Parental influence and obesity prefention in pre-schoolers: A systematic review of interventions. Obes. Rev. 2010, 12, 315–328. [Google Scholar] [CrossRef] [PubMed]
- Committee on Progress in Preventing Childhood Obesity. Progress in Preventing Childhood Obesity: How Do We Measure Up? National Academy Press: Washington, DC, USA, 2007. [Google Scholar]
- Fisher, J.O.; Mitchell, D.C.; Smiciklas-Wright, H.; Birch, L.L. Maternal milk consumption predicts the tradeoff between milk and soft drinks in young girls’ diets. J. Nutr. 2000, 131, 246–250. [Google Scholar]
- Fisher, J.O.; Mitchell, D.C.; Smiciklas-Wright, H.; Birch, L.L. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. J. Am. Diet. Assoc. 2002, 102, 58–64. [Google Scholar] [CrossRef]
- Gibson, E.; Wardle, J.; Watts, C. Fruit and vegetable consumption, nutritional knowledge and beliefs in mothers and children. Appetite 1998, 31, 205–228. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.O.; Birch, L.L. Restricting access to foods and children’s eating. Appetite 1999, 32, 405–419. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Carnell, S.; Cooke, L. Parental control over feeding and children’s fruit and vegetable intake: How are they related? J. Am. Diet. Assoc. 2005, 105, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Cullen, K.; Baranowski, T.; Owens, E.; Marsh, T.; Rittenberry, L.; de Moor, C. Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children’s dietary behavior. Health Educ. Behav. 2003, 30, 615–626. [Google Scholar] [CrossRef] [PubMed]
- Kratt, P.; Reynolds, K.; Shewchuk, R. The role of availability as a moderator of family fruit and vegetable consumption. Health Educ. Behav. 2000, 27, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Domel, S.; Baranowski, T.; Davis, H.; Leonard, S.; Riley, P.; Baranowski, J. Measuring fruit and vegetable preferences among 4th- and 5th-grade students. Prev. Med. 1993, 22, 886–879. [Google Scholar] [CrossRef] [PubMed]
- Resnicow, K.; Davis-Hearn, M.; Smith, M.; Baranowski, T.; Lin, L.; Baranowski, J.; Doyle, C.; Wang, D. Social-cognitive predictors of fruit and vegetable intake in children. Health Psychol. 1997, 16, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Ray, J.; Klesges, R. Influences on the eating behavior of children. Ann. N. Y. Acad. Sci. 1993, 699, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Birch, L. Effects of peer models’ food choices and eating behaviors on preschoolers’ food preferences. Child Dev. 1980, 51, 489–496. [Google Scholar] [CrossRef]
- Clarke, W.; Woolson, R.; Lauer, R. Changes in ponderosity and blood pressure in childhood: The muscatine study. Am. J. Epidemiol. 1986, 124, 195–205. [Google Scholar] [PubMed]
- Duncker, K. Experimental modification of children’s food preferences through social suggestion. J. Abnorm. Psychol. 1938, 33, 489–507. [Google Scholar] [CrossRef]
- Fitzpatrick, E.; Edmunds, L.; Dennison, B. Positive effects of family dinner are undone by television viewing. J. Am. Diet. Assoc. 2007, 107, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Fulkerson, J.; Neumark-Sztainer, D.; Story, M. Adolescent and parent views of family meals. J. Am. Diet. Assoc. 2006, 106, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Gable, S.; Chang, Y.; Krull, J. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J. Am. Diet. Assoc. 2007, 107, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Harper, L.; Sanders, K. The effect of adults’ eating on young children’s acceptance of unfamiliar foods. J. Exp. Child Psychol. 1975, 20, 206–214. [Google Scholar] [CrossRef]
- Mitchell, B.; Krammerer, C.; Reinhart, L.; Stern, M. Niddm in mexican-american families. Heterogeneity by age of onset. Diabetes Care 1994, 17, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, M.; Lifshitz, F.; Grad, G.; Fort, P.; Marks-Katz, M. Fear of obesity. A cause of short stature and delayed puberty. N. Engl. J. Med. 1983, 309, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Byrd-Bredbenner, C.; Abbot, J. Differences in food supplies of households with and without overweight individuals. Appetite 2009, 52, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Golan, M.; Crow, S. Parents are key players in the prevention and treatment of weight-related problems. Nutr. Rev. 2004, 62, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Chumlea, W.; Roche, A.; Gardner, J.; Siervogel, R. The predictive value of childhood body mass index values for overweight at age 35 years. Am. J. Clin. Nutr. 1994, 59, 810–819. [Google Scholar] [PubMed]
- Guo, S.; Wei, W.; Chumlea, W.; Roche, A. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am. J. Clin. Nutr. 2002, 76, 653–658. [Google Scholar] [PubMed]
- Kemm, J. Eating patterns in childhood and adult health. Nutr. Health 1987, 1987, 205–215. [Google Scholar] [CrossRef]
- Lagström, H.; Hakanen, M.; Niinikoski, H.; Viikari, J.; Rönnemaa, T.; Saarinen, M.; Pahkala, K.; Simell, O. Growth patterns and obesity development in overweight or normal-weight 13-year-old adolescents: The strip study. Pediatrics 2008, 122, e876–e883. [Google Scholar] [CrossRef] [PubMed]
- Mamun, A.; O’Callaghan, M.; Callaway, L.; Williams, G.; Najman, J.; Lawlor, D. Associations of gestational weight gain with offspring body mass index and blood pressure at 21 years of age evidence from a birth cohort study. Circulation 2009, 119, 1720–1727. [Google Scholar] [CrossRef] [PubMed]
- Nicklas, T.; Farris, R.; Smoak, C.; Frank, G.C.; Srinivasan, S.R.; Webber, L.S.; Berenson, G.S. Dietary factors relate to cardiovascular risk factors in early life. Arteriosclerosis 1988, 8, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Rolland-Cachera, M.; Deheeger, M.; Guilloud-Bataille, M. Tracking the development of adiposity from one month of age to adulthood. Ann. Hum. Biol. 1987, 14, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Krahnstoever, D.; Francis, L.; Birch, L. Reexamining obesigenic families: Parents’ obesity-related behaviors predict girls’ change in bmi. Obes. Res. 2005, 13, 1980–1990. [Google Scholar]
- Swinburn, B.; Edgar, G. The runaway weight gain train: Too many accelerators, not enough brakes. Br. Med. J. 2004, 329, 736–739. [Google Scholar] [CrossRef] [PubMed]
- Pearson, N.; Biddle, S.; Gorley, T. Family correlates of fruit and vegetable consumption in children and adolescents: A systematic review. Public Health Nutr. 2009, 12, 267–283. [Google Scholar] [CrossRef] [PubMed]
- Olstad, D.; McCarger, L. Prevention of overweight and obesity in children under the age of 6 years. Appl. Physiol. Nutr. Metab. 2009, 34, 551–570. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.; Witaker, R. Household routines and obesity in us preschool-aged children. Pediatrics 2010, 125, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Hill, J. A family approach to addressing obesity. In Presented at International Congress of Dietetics; Chicago, IL, USA, 2004; p. 5. [Google Scholar]
- Epstein, L.; Gordy, C.; Raynor, H.; Beddome, M.; Kilanowski, C.; Paluch, R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes. Res. 2001, 9, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Epstein, L.; Valoskii, A.; Wing, R.; McCurley, J. Ten-year follow-up of behavioral family-based treatment for obese children. J. Am. Med. Assoc. 1990, 264, 2519–2523. [Google Scholar] [CrossRef]
- Wu, S. Population and Labor Force Projections for New Jersey: 2000 to 2020. Available online: http://www.wnjpin.net/OneStopCareerCenter/LaborMarketInformation/lmi03/lfproj.pdf (accessed on 5 August 2015).
- De Oliveira, M.C.; Sichieri, R.; Moura, A.S. Weight loss associated with a daily intake of three apples or three pears among overweight women. Nutrition 2003, 19, 253–256. [Google Scholar] [CrossRef]
- Taveras, E.; Rifas-Shiman, S.; Oken, E.; Gunderson, E.; Gillman, M. Short sleep duration in infancy and risk of childhood overweight. Arch. Pediatr. Adolesc. Med. 2008, 165, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.A.; Popkin, B.M. Dietary fat does affect obesity! Am. J. Clin. Nutr. 1998, 68, 1157–1173. [Google Scholar] [PubMed]
- Lissner, L.; Heitmann, B. Dietary fat and obesity: Evidence form epidemiology. Eur. J. Clin. Nutr. 1995, 49, 79–80. [Google Scholar] [PubMed]
- Ebbeling, C.; Feldman, H.; Osganian, S.; Chomitz, V.; Ellenbogen, S.; Ludwig, D. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: A randomized, controlled pilot study. Pediatrics 2006, 117, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A. Intense sweeteners and energy density of foods: Implications for weight control. Eur. J. Clin. Nutr. 1999, 53, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Harnack, L.; Stang, J.; Story, M. Soft drink consumption among us children and adolescents: Nutritional consequences. J. Am. Diet. Assoc. 1999, 99, 436–441. [Google Scholar] [CrossRef]
- Fiore, H.; Travis, S.; Whalen, A.; Auinger, P.; Ryan, S. Potentially protective factors associated with healthful body mass index in adolescents with obese and nonobese parents: A secondary data analysis of the third national health and nutrition examination survey, 1988–1994. J. Am. Diet. Assoc. 2006, 106, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Rodearmel, S.; Wyatt, H.; Barry, M.; Dong, F.; Pan, D.; Israel, R.; Cho, S.; McBurney, M.; Hill, J. A family-based approach to preventing excessive weight gain. Obesity 2006, 14, 1392–1401. [Google Scholar] [CrossRef] [PubMed]
- Lioret, S.; Volatier, J.; Lafay, L.; Touvier, M.; Ma, B. Is food portion size a risk factor of childhood overweight? Eur. J. Clin. Nutr. 2009, 63, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Bolton, R.; Heaton, K.; Burroughs, L. The role of dietary fiber in satiety, glucose, and insulin: Studies with fruit and fruit juice. Am. J. Clin. Nutr. 1981, 34, 211–217. [Google Scholar] [PubMed]
- Galst, J. Television food commercials and pro-nutritional public service announcements as determinants of young children’s snack choices. Child Dev. 1980, 51, 935–938. [Google Scholar] [CrossRef]
- Galst, J.; White, M. The unhealthy persuader: The reinforcing value of television and children’s purchase-influence attempts at the supermarket. Child Dev. 1976, 47, 1089–1094. [Google Scholar] [CrossRef]
- Gorn, G.J.; Goldberg, M. Behavioral evidence of the effects of televised food messages on children. J. Consum. Res. 1982, 9, 200–205. [Google Scholar] [CrossRef]
- Borzekowski, D.; Robinson, T. The 30-second effect: An experiment revealing the impact of television commercials on food preferences of preschoolers. J. Am. Diet. Assoc. 2001, 101, 42–46. [Google Scholar] [CrossRef]
- Committee on Food Marketing and the Diets of Children. Food marketing to children and youth: Threat or opportunity? National Academy of Sciences: Washington, DC, USA, 2006. [Google Scholar]
- Robinson, T.; Borzekowski, D. Effects of the smart classroom curriculum to reduce child and family screen time. J. Commun. 2006, 67, 1–26. [Google Scholar] [CrossRef]
- Robinson, T. Reducing children’s television viewing to prevent obesity. J. Am. Med. Assoc. 1999, 282, 1561–1567. [Google Scholar] [CrossRef]
- American Academy of Pediatrics; Committee on Sports Medicine and Fitness. Fitness, activity, and sports participation in the preschool child. Pediatrics 1992, 90, 1001–1003. [Google Scholar]
- Carson, D.; Reiboldt, W. Parents’ agreement to purchase healthy snack foods requested by their children. J. Fam. Consum. Sci. 2010, 102, 42–48. [Google Scholar]
- Nicklas, T.; Baranowski, T.; Baranowski, J.; Cullen, K.; Rittenberry, L.; Olvera, N. Family and child-care provider influences on preschool children’s fruit, juice, and vegetable consumption. Nutr. Rev. 2001, 59, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Lumeng, J.; Gannon, K.; Appugliese, D.; Cabral, H.; Zuckerman, B. Preschool child care and risk of overweight in 6- to 12-year-old children. Int. J. Obes. 2005, 29, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Maher, E.; Li, G.; Carter, L.; Johnson, D. Preschool child care participation and obesity at the start of kindergarten. Pediatrics 2008, 122, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.; Pfeiffer, K.; Trost, S.; Ziegler, P.; Dowda, M. Physical activity among children attending preschools. Pediatrics 2004, 114, 1258–1263. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, L.; Crawford, P.; Hoelscher, D.; Sothern, M. Position of the american dietetic association: Individual, family, school, and community based interventions for pediatric overweight. J. Am. Diet. Assoc. 2006, 106, 925–945. [Google Scholar]
- Flynn, M.; McNeil, D.; Maloff, B.; Mutasingwa, D.; Wu, M.; Ford, C.; Tough, S. Reducing obesity and related chronic disease risk in children and youth: A synthesis of evidence with “best practice” recommendations. Obes. Rev. 2006, 7, 7–66. [Google Scholar] [CrossRef] [PubMed]
- Serdula, M.; Khan, L.; Dietz, W. Weight loss counseling revisited. J. Am. Med. Assoc. 2003, 289, 1747–1750. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, L.; Welk, G.; Styne, D.; Gerstein, D.; Crawford, P. Family environment and pediatric overweight: What is a parent to do? J. Am. Diet. Assoc. 2005, 105, S70–S79. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.; Froelicher, E. Management of overweight and obesity in adults: Behavioral intervention for long-term weight loss and maintenance. Eur. J. Cardiovasc. Nurs. 2006, 5, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Khan, L.K.; Sobush, K.; Keener, D.; Goodman, K.; Lowry, A.; Kakietek, J.; Zaro, S. Recommended community strategies and measurements to prevent obesity in the United States. Morb. Mortal. Wkly. Rep. 2009, 58, 1–26. [Google Scholar]
- Barnes, M. Solving the Problem of Childhood Obesity within a Generation; White House Task Force on Childhood Obesity: Washington, DC, USA, 2010. [Google Scholar]
- USDA. Dietary Guidelines for Americans. Available online: http://www.cnpp.usda.gov/dietaryguidelines.htm (accessed on 10 June 2010).
- USDHHS. Healthy People 2020: The Road Ahead. Available online: http://www.healthypeople.gov/hp2020/ (accessed on 10 June 2010).
- USDA. Maximizing the Messages: Helping Moms and Kids Make Healthier Food Choices. USDA Food and Nutrition Service: Washington, DC, USA, 2008. [Google Scholar]
- Green, L.; Krueter, M. Health Program Planning: An Educational Ecological Approach, 4th ed.; McGraw Hill: New York, NY, USA, 2004. [Google Scholar]
- Minkler, M. Using participatory action research to build healthy communities. Public Health Rep. 2000, 115, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Sloane, D.; Diamant, A.; Lewis, L. Improving the nutritional resource environment for healthy living through community-based participatory research. J. Gen. Intern. Med. 2003, 18, 568–575. [Google Scholar] [CrossRef] [PubMed]
- Faith, M.; van Horn, L.; Appel, L.; Burke, L.; Carson, J.; Franch, H.; Jakicic, J.; Kral, T.; Odoms-Young, A.; Wansink, B.; et al. Evaluating parents and adult caregivers as “agents of change” for treating obese children—Evidence for parent behavior change strategies and research gaps: A scientific statement from the American heart association. Circulation 2012, 125, 1186–1207. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Learning Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1977. [Google Scholar]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef] [PubMed]
- Byrd-Bredbenner, C.; Maurer Abbot, J. Food choice influencers of mothers of young children: Implications for nutrition educators. Top. Clin. Nutr. 2008, 25, 198–215. [Google Scholar] [CrossRef]
- Sallis, J.; Owen, N.; Fisher, E. Ecological Models of Health Behavior, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Bowman, R.; University of Colorado, Denver, CO, USA. Unpublished work. 2007.
- Richter, K.; Harris, K.; Paine-Andrews, A.; Fawcett, S.; Schmid, T.; Lankenau, B.; Johnston, J. Measuring the health environment for physical activity and nutrition among youth: A review of the literature and applications for community initiatives. Prev. Med. 2000, 31, S98–S111. [Google Scholar] [CrossRef]
- Wechsler, H.; Deveraux, R.; Davis, M.; Collins, J. Promoting physical activity and healthy eating through changes in the school environment. Prev. Med. 2000, 31, S112–S120. [Google Scholar] [CrossRef]
- McAlister, A.; Perry, C.; Parcel, G. How Individuals, Environments, and Health Behavior Interact, Social Cognitive Theory, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Contento, I.; Randell, J.; Basch, C. Review and analysis of evaluation measures used in nutrition education intervention research. J. Nutr. Educ. Behav. 2002, 34, 2–25. [Google Scholar] [CrossRef]
- Stevens, J.; Story, M.; Ring, K.; Murray, D.M.; Cornell, C.; Juhaeri; Gittelsohn, J. The impact of the pathways intervention on psychosocial variables related to diet and physical activity in American Indian schoolchildren. Prev. Med. 2003, 37, S70–S79. [Google Scholar] [CrossRef] [PubMed]
- Stewart, K.; Seemans, C.; McFarland, L.; Weinhofer, J. Social learning versus traditional teaching in an elementary school cardiovascular health promotion program. Am. J. Health Promot. 1997, 11, 194–197. [Google Scholar] [CrossRef] [PubMed]
- Thompson, V.; Bachman, C.; Baranowski, T.; Cullen, K. Self-efficacy and norm measures for lunch fruit and vegetable consumption are reliable and valid among fifth grade students. J. Nutr. Educ. Behav. 2007, 39, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Hinton, A. A social cognitive theory model to predict frequency of fruit and vegetable consumption among third-grade children. Diss. Abstr. Int. 1997, 58, 4172. [Google Scholar]
- Spahn, J.; Reeves, R.; Keim, K.; Laquatra, I.; Kellogg, M.; Jortberg, B.; Clark, N. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J. Am. Diet. Assoc. 2010, 110, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Rollnick, R.; Butler, C.; Kinnersley, P.; Gregory, J.; Mash, B. Motivational interviewing. Br. Med. J. 2010, 340, c1900. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.; Rollnick, S. Motivational Interviewing: Preparing People to Change; Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Miller, R.; Rose, G. Towards a theory of motivational interviewing. Am. Psychol. 2009, 64, 527–537. [Google Scholar] [CrossRef] [PubMed]
- Rollnick, S.; Miller, W.; Butler, C. Motivational Interviewing in Health Care: Helping Patients Change Behavior; Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Lundahl, D.; Tollefson, D.; Gambles, C.; Brownell, C. A meta-analysis of motivational interviewing: Twenty five years of empirical studies. Res. Soc. Work Pract. 2010, 20, 137–160. [Google Scholar] [CrossRef]
- Burke, B.; Arkowitz, H.; Menchola, M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. J. Consult. Clin. Psychol. 2003, 71, 843–861. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.; Carr, C.; Devellis, B.; Switzer, B.; Biddle, A.; Amamoo, M.; Walsh, J.; Zhou, B.; Sandler, R. A randomized trial of tailoring and motivational interviewing to promote fruit and vegetable consumption for cancer prevention and control. Ann. Behav. Med. 2009, 38, 71–85. [Google Scholar] [CrossRef] [PubMed]
- Blanson Henkemans, O.; van der Boog, P.; Lindenberg, J.; van der Mast, C.; Neerincx, M.; Zwetsloot-Schonk, B. An online lifestyle diary with a persuasive computer assistant providing feedback on self-management. Technol. Health Care 2009, 17, 253–267. [Google Scholar] [PubMed]
- Martins, R.; McNeil, D. Review of motivational interviewing in promoting health behaviors. Clin. Psychol. Rev. 2009, 29, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Flattum, C.; Story, M.; Feldman, S.; Petrich, C. Dietary approaches to healthy weight management for adolescents: The new moves model. Adolesc. Med. 2008, 19, 421–430. [Google Scholar]
- Hardcastle, S.; Taylor, A.; Bailey, M.; Castle, R. A randomised controlled trial on the effectiveness of a primary health care based counselling intervention on physical activity, diet and chd risk factors. Patient Educ. Couns. 2008, 70, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Barlow, S.; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef] [PubMed]
- Webber, K.; Tate, D.; Quintiliani, L. Motivational interviewing in internet groups: A pilot study for weight loss. J. Am. Diet. Assoc. 2008, 108, 1029–1032. [Google Scholar] [CrossRef] [PubMed]
- Keller, J. Motivational design of instruction. In Instructional-Design Theories and Models: An Overview of Their Current Status; Reigeluth, C., Ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1983; pp. 386–434. [Google Scholar]
- Keller, J. Keller’s ARCS model of motivational design. Available online: http://www.arcsmodel.com/ (accessed on 17 May 2010).
- Rodriguez, J. Culturally competent dietetics: Increasing awareness, improving care. J. Am. Diet. Assoc. 2010, 110, S7. [Google Scholar] [CrossRef] [PubMed]
- Speck, M. Best practice in professional development for sustained educational change. ERS Spectr. 1996, 14, 33–41. [Google Scholar]
- Knowles, M.; Holton, E.; Swanson, R. The Adult Learner; Gulf Publishing: Houston, TX, USA, 1998. [Google Scholar]
- Brookfield, S. Understanding and Facilitating Adult Learning; Jossey Bass: San Francisco, CA, USA, 1986. [Google Scholar]
- Zemel, M.B. Role of calcium and dairy products in energy partitioning and weight management. Am. J. Clin. Nutr. 2004, 79, 907S–912S. [Google Scholar] [PubMed]
- Rolls, B.J.; Ello-Martin, J.; Tohill, B. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutr. Rev. 2004, 62, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Domel, S.; Baranowski, T.; Leonard, S.; Al, E. Defining the year 2000 fruit and vegetable goal. J. Am. Coll. Nutr. 1993, 12, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Faith, M.; Scanlon, K.; Birch, L.; Francis, L.; Sherry, B. Parent-child feeding strategies and their relationships to child eating and weight status. Obes. Res. 2004, 12, 1711–1722. [Google Scholar] [CrossRef] [PubMed]
- Pierce, J. World Internet Project Report Finds Large Percentages of Non-Users, and Significant Gender Disparities in Going Online. Available online: http://worldinternetproject.com/_files/_News/37/wip2010_long_press_release_v2.pdf (accessed on 5 August 2015).
- Horrigan, J. Broadband Adoption and Use in America; Federal Communications Commission: Washington, DC, USA, 2010. [Google Scholar]
- American Academy of Pediatrics. The role of preschool home-visiting programs in improving children’s developmental and health outcomes. Pediatrics 2009, 123, 598–603. [Google Scholar]
- Haire-Joshu, D.; Elliott, M.; Cairo, N.; Hessler, K.; Nanney, M.; Hale, N.; Boehmer, T.; Kreuter, M.; Brownson, R. High 5 for kids: The impact of a home visiting program on fruit and vegetable intake of parents and their preschool children. Prev. Med. 2008, 47, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Schardt, C.; Garrison, J. Continuing Education and Knowledge Retention: A Comparison of Online and Face-to-face Deliveries. Available online: http://works.bepress.com/julie_garrison/1/ (accessed on 5 August 2015).
- O’Connor, T.; Jago, R.; Baranowski, T. Engaging parents to increase youth physical activity: A systematic review. Am. J. Prev. Med. 2009, 37, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Child Care Aware of America. Child Care in America: 2014 State Fact Sheets; Child Care Aware of America: Arlington, VA, USA, 2014. [Google Scholar]
- Munoz, K.; Krebs-Smith, S.; Ballard-Barbash, R.; Cleveland, L. Food intakes of US children and adolescents compared with recommendations. Pediatrics 1997, 100, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Gleason, P.; Suitor, C. Nutrition and Evaluation. Changes in Children’s Diets: 1989–1991 to 1994–1996; USDA Food and Nutrition Service, Office of Analysis: Alexandria, VA, USA, 2001. [Google Scholar]
- Guenther, P.; Juan, W.; Lino, M.; Hiza, H.; Fungwe, T.; Lucas, R. Diet Quality of Low-income and Higher Income Americans in 2003–04 as Measured by the Healthy Eating Index-2005: Nutrition Insight 42. Available online: http://www.cnpp.usda.gov/sites/default/files/nutrition_insights_uploads/Insight42.pdf (accessed on 5 August 2015).
- Lorson, B.; Melgar-Quinonez, H.; Taylor, C. Correlates of fruit and vegetable intakes in US children. J. Acad. Nutr. Diet. 2009, 109, 474–478. [Google Scholar] [CrossRef] [PubMed]
- Putnam, J.; Allshouse, J.; Kantor, L.S. US per capita food supply trends: More calories, refined carbohydrates, and fats. FoodReview 2002, 25, 2–15. [Google Scholar]
- French, S.A.; Story, M.; Jeffrey, R. Environmental influences on eating and physical activity. Annu. Rev. Public Health 2001, 22, 309–335. [Google Scholar] [CrossRef] [PubMed]
- Stookey, J.D. Energy density, energy intake and weight status in a large free-living sample of Chinese adults: Exploring the underlying roles of fat, protein, carbohydrate, fiber and water intakes. Eur. J. Clin. Nutr. 2001, 55, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Westerterp-Plantenga, M.S. Analysis of energy density of food in relation to energy intake regulation in human subjects. Br. J. Nutr. 2001, 85, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Popkin, B.M. The nutrition transition: New trends in the global diet. Nutr. Rev. 1997, 55, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Harnack, L.; Jeffery, R.; Boutelle, K. Temporal trends in energy intake in the United States: An ecologic perspective. Am. J. Clin. Nutr. 2000, 71, 1478–1484. [Google Scholar] [PubMed]
- Friedman, L.; Snetselaar, L.; Stumbo, P.; van Horn, L.; Singh, B.; Barton, B. Influence of intervention on beverage choice trends in the dietary intervention study in children (DISC). J. Am. Diet. Assoc. 2007, 107, 586–594. [Google Scholar] [CrossRef] [PubMed]
- McAleese, J.; Rankin, L. Garden-based nutrition education affects fruit and vegetable consumption on sixth-grade adolescents. J. Am. Diet. Assoc. 2007, 107, 662–665. [Google Scholar] [CrossRef] [PubMed]
- Sandeno, C.; Wolf, G.; Drake, T.; Reicks, M. Behavioral strategies to increase fruit and vegetable intake by fourth- through sixth-grade students. J. Am. Diet. Assoc. 2000, 100, 828–830. [Google Scholar] [CrossRef]
- Kruger, J.; Yore, M.; Solera, M.; Moeti, R. Prevalence of fruit and vegetable consumption and physical activity by race/ethnicity—United States, 2005. Morb. Mortal. Wkly. Rep. 2007, 56, 301–304. [Google Scholar]
- Blanck, H.; Galuska, D.; Gillespie, C.; Khan, L.; Serdula, M.; Solera, M.; Mokdad, A.; Cohen, L. Fruit and vegetable consumption among adults—United States, 2005. Morb. Mortal. Wkly. Rep. 2007, 56, 213–217. [Google Scholar]
- Kennedy, E.; Powell, R. Changing eating patterns of american children: A view from 1996. J. Am. Coll. Nutr. 1997, 16, 524–529. [Google Scholar] [PubMed]
- Krebs-Smith, S.; Cook, A.; Subar, A.; Cleveland, L.; Friday, J.; Kahle, L. Fruit and vegetable intakes of children and adolescents in the United States. Arch. Pediatr. Adolesc. Med. 1996, 150, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Story, M.; Resnick, M.; Blum, R. Correlates of inadequate fruit and vegetable consumption among adolescents. Prev. Med. 1996, 25, 497–495. [Google Scholar] [CrossRef] [PubMed]
- Lakkula, A.; Zanovec, M.; Silverman, L.; Murphy, E.; Tuuri, G. Black children with high preferences for fruits and vegetables are at less risk of being at risk of overweight or overweight. J. Am. Diet. Assoc. 2008, 108, 1912–1915. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.; Hodges, V.; Gillham, M. Normal weight adults consumer more fiber and fruit than their age and height-matched overweight/obese counterparts. J. Am. Diet. Assoc. 2006, 106, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.; Graubard, B. Energy dense diets reported by american adults: Association with food group intake, nutrient intake, and body weight. Int. J. Obes. 2005, 29, 950–956. [Google Scholar] [CrossRef] [PubMed]
- French, S.A.; Lin, B.; Guthrie, J. National trends in soft drink consumption among children and adolescents age 6 to 17 years: Prevalence, amounts, and sources, 1977/1978 to 1994/1998. J. Am. Diet. Assoc. 2003, 103, 1326–1331. [Google Scholar] [CrossRef]
- Nielsen, S.J.; Siega-Riz, A.M.; Popkin, B.M. Trends in energy intake in U.S. Between 1977 and 1996: Similar shifts seen across age groups. Obes. Res. 2002, 10, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, L.; Schwartz, M.; Brownell, K. Effect of soft drink consumption on nutrition and health: A systematic review and meta-analysis. Am. J. Public Health 2007, 97, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Ariza, A.; Chen, E.; Binns, H.; Christoffel, K. Risk factors for overweight in five- to six-year-old hispanic-american children: A pilot study. J. Urban Health Bull. N. Y. Acad. Med. 2004, 81, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Rampersaud, G.C.; Bailey, L.B.; Kauwell, G.P.A. National survey beverage consumption data for children and adolescents indicate the need to encourage a shift toward more nutritive beverages. J. Am. Diet. Assoc. 2003, 103, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.A.; Nielsen, S.J.; Popkin, B.M. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am. J. Clin. Nutr. 2004, 79, 537–543. [Google Scholar] [PubMed]
- Malik, V.; Popkin, B.; Bray, G.; Després, J.; Hu, F. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010, 121, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics. Prevention of pediatric overweight and obesity. Pediatrics 2003, 112, 424–430. [Google Scholar]
- Friorito, L.; Marini, M.; Mitchell, D.; Smiciklas-Wright, H.; Birch, L. Girls’ early sweetened carbonated beverage intake predicts different patterns of beverage and nutrient intake across childhood and adolescence. J. Am. Diet. Assoc. 2010, 110, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.; Peterson, K.; Gortmaker, S. Relation between consumption of sugar-sweetened drinks and childhood obesity: A prospective, observational analysis. Lancet 2001, 357, 505–508. [Google Scholar] [CrossRef]
- St-Onge, M.; Keller, K.L.; Heymsfield, S.B. Changes in childhood food consumption patterns: A cause for concern in light of increasing body weights. Am. J. Clin. Nutr. 2003, 78, 1068–1073. [Google Scholar] [PubMed]
- Raben, A.; Vasilaras, T.; Moller, A.; Astrup, A. Sucrose compared with artificial sweeteners: Different effects on ad libitum food intake and body weight after 10 weeks of supplementation in overweight subjects. Am. J. Clin. Nutr. 2002, 76, 721–729. [Google Scholar] [PubMed]
- Deshmukh-Taskar, P.; Nicklas, T.; O’Neil, C.; Keast, D.; Radcliffe, J. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: The national health and nutrition examination survey 1999–2006. J. Am. Diet. Assoc. 2010, 110, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Affenito, S. Breakfast: A missed opportunity. J. Am. Diet. Assoc. 2007, 107, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Utter, J.; Scragg, R.; Mhurchu, C.; Schaaf, D. At-home breakfast consumption among New Zealand children: Associations with body mass index and related nutrition behaviors. J. Am. Diet. Assoc. 2007, 107, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Albertson, A.; Affenito, S.; Bauserman, R.; Holschuh, N.; Eldridge, A.; Barton, B. The relationship of ready-to-eat cereal consumption to nutrient intake, blood lipids, and body mass index of children as they age through adolescence. J. Am. Diet. Assoc. 2009, 109, 1557–1565. [Google Scholar] [CrossRef] [PubMed]
- Albertson, A.; Thompson, D.; Franko, D.; Holschuh, N.; Bauserman, R.; Barton, B. Prospective associations among cereal intake in childhood and adiposity, lipid levels, and physical activity during late adolescence. J. Am. Diet. Assoc. 2009, 109, 1775–1780. [Google Scholar] [CrossRef] [PubMed]
- Rosado, J.; Arellano, M.; Montemayor, K.; García, O.; Caamaño, M. An increase of cereal intake as an approach to weight reduction in children is effective only when accompanied by nutrition education: A randomized control trial. Nutr. J. 2008, 7, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Dietrich, M.; Brown, C.; Clark, C.; Block, G. The effect of breakfast type on total daily energy intake and body mass index: Results from the third national health and nutrition examination survey (NHANES III). J. Am. Coll. Nutr. 2003, 22, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Barton, B.; Eldridge, A.; Thompson, D.; Affenito, S.; Striegel-Moore, R.; Franko, D.; Albertson, A.; Crockett, S. The relationship of breakfast and cereal consumption of nutrient intake and body mass index: The national heart, lung and blood institute growth and health study. J. Am. Diet. Assoc. 2005, 105, 1383–1389. [Google Scholar] [CrossRef] [PubMed]
- Rampersaud, G.; Pereira, M.; Girard, B.; Adams, J.; Metzl, J. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J. Am. Diet. Assoc. 2005, 105, 743–760. [Google Scholar] [CrossRef] [PubMed]
- Worobey, H.; Worobey, J. Efficacy of a preschool breakfast programme in balancing nutrient intake. Int. J. Food Sci. Nutr. 1999, 50, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Worobey, J.; Worobey, H. The impact of a two-year school breakfast program for preschool-aged children on their nutrient intake and pre-academic performance. Child Study J. 1999, 29, 113–131. [Google Scholar]
- Byrd-Bredbenner, C.; Hayes, D.; Jana, L.; Martin-Stephenson, S.; Melendez-Klinger, S.; O’Neil, C. The role of breakfast in health: Definition and criteria for a quality breakfast. J Acad Nutr Diet 2104, 12, S8–S26. [Google Scholar]
- United States Department of Agriculture, Agricultural Research Service. What We Eat in America, NHANES, 2001–2002. Available online: http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/Table_5_BIA.pdf (accessed on 5 August 2015).
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. Dietary Guidelines for Americans, 6th ed.; United States Department of Agriculture: Washington, DC, USA, 2005. [Google Scholar]
- Harnack, L.; Walters, S.; Jacobs, D. Dietary intake and food sources of whole grains among US children and adolescents: Data from the 1994–1996 continuing survey of food intakes by individuals. J. Am. Diet. Assoc. 2003, 103, 1015–1019. [Google Scholar] [CrossRef]
- Young, L.; Nestle, M. The contribution of expanding portion sizes to the US obesity epidemic. Am. J. Public Health 2002, 92, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Young, L.; Nestle, M. Expanding portion sizes in the US marketplace: Implications for nutrition counseling. J. Am. Diet. Assoc. 2003, 103, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Smiciklas-Wright, H.; Mitchell, D.; Mickle, S.; Goldman, J.; Cook, A. Food commonly eaten in the United States, 1989–1991 and 1994–1996. J. Am. Diet. Assoc. 2003, 103, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.J.; Popkin, B.M. Patterns and trends in food portion sizes, 1977–1998. J. Am. Med. Assoc. 2003, 289, 450–453. [Google Scholar] [CrossRef]
- Burger, K.; Kern, M.; Coleman, K. Characteristics of self-selected portion size in young adults. J. Am. Diet. Assoc. 2007, 107, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Diliberti, N.; Bordi, P.L.; Conklin, M.T.; Roe, L.S.; Rolls, B.J. Increased portion size leads to increased energy intake in a restaurant meal. Obes. Res. 2004, 12, 562–568. [Google Scholar] [CrossRef] [PubMed]
- Rolls, B.J.; Roe, L.S.; Meengs, J.S.; Wall, D.E. Increasing the portion size of a sandwich increases energy intake. J. Am. Diet. Assoc. 2004, 104, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Wansink, B.; Park, S. At the movies: How external cues and perceived taste impact consumption volume. Food Q. Preferences 2001, 12, 69–74. [Google Scholar] [CrossRef]
- Kral, R.; Meengs, J.; Wall, D.; Roe, L.; Rolls, B. Effect of food intake on increasing portion size of all foods over two consecutive days. FASEB J. 2003, 17, A809. [Google Scholar]
- Rolls, B.; Roe, L.; Kral, R.; Meengs, J.; Wall, D. Increasing the portion size of a packaged snack increases energy intake in men and women. Appetite 2004, 42, 63–69. [Google Scholar] [CrossRef]
- Rolls, B.J.; Morris, E.; Roe, L. Portion size of food affects energy intake in normal-weight and overweight men and women. Am. J. Clin. Nutr. 2002, 76, 1207–1213. [Google Scholar] [PubMed]
- Schwartz, J.; Byrd-Bredbenner, C. Portion distortion: Typical portion sizes selected by young adults. J. Am. Diet. Assoc. 2006, 106, 1412–1418. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Byrd-Bredbenner, C. The ability of young adults to estimate portion size and calorie content. Top. Clin. Nutr. 2006, 21, 114–121. [Google Scholar] [CrossRef]
- Nestle, M. Increasing portion sizes in American diets: More calories, more obesity. J. Am. Diet. Assoc. 2003, 103, 39–40. [Google Scholar] [CrossRef] [PubMed]
- Martin-Biggers, J.; Spaccarotella, K.; Berhaupt-Glickstein, A.; Hongu, N.; Worobey, J.; Byrd-Bredbenner, C. Come and get it! A discussion of the family mealtime environment. Adv. Nutr. 2014, 5, 235–247. [Google Scholar] [CrossRef] [PubMed]
- Martin-Biggers, J.; Spaccarotella, K.; Hongu, N.; Worobey, J.; Byrd-Bredbenner, C. Translating it into real life: Cognitions, barriers and supports for key weight-related behaviors of parents of preschoolers. BMC Public Health 2015, 15, 189. [Google Scholar] [CrossRef] [PubMed]
- Fulkerson, J.; Larson, N.; Horning, M.; Neumark-Sztainer, D. A review of associations between family or shared meal frequency and dietary and weight status outcomes across the lifespan. J. Nutr. Educ. Behav. 2014, 46, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Taveras, E.; Rifas-Shiman, S.; Berkey, C.; Rockett, H.; Field, A.; Frazier, A.; Colditz, G.; Gillman, M. Family dinner and adolescent overweight. Obes. Res. 2005, 13, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Byrd-Bredbenner, C. Food preparation knowledge and attitudes of young adults: Implications for nutrition practice. Top. Clin. Nutr. 2004, 19, 154–163. [Google Scholar] [CrossRef]
- Williamson, D.M.; Gravani, R.B.; Lawless, H.T. Correlating food safety knowledge with home food-preparation practices. Food Technol. 1992, 48, 94–100. [Google Scholar]
- Videon, T.M.; Manning, C.K. Influences on adolescent eating patterns: The importance of family meals. J. Adolesc. Health 2003, 32, 365–373. [Google Scholar] [CrossRef]
- Gillman, M.; Rifas-Shiman, S.; Frazier, L.; Rockett, H.; Camargo, C.; Field, A.; Berkey, C.; Colditz, G. Family dinner and diet quality among older children and adolescents. Arch. Fam. Med. 2000, 9, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Hannan, P.J.; Story, M.; Croll, J.; Perry, C. Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. J. Am. Diet. Assoc. 2003, 103, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Boutelle, K.N.; Lytle, L.A.; Murray, D.M.; Birnbaum, A.S. Perceptions of the family mealtime environment and adolescent mealtime behavior: Do adults and adolescents agree? J. Nutr. Educ. 2001, 33, 128–133. [Google Scholar] [CrossRef]
- Fulkerson, J.A.; Neumark-Sztainer, D.; Story, M.; Gurvich, O.; Kubik, M.Y.; Garwick, A.; Dudovitz, B. The healthy home offerings via the mealtime environment (home) plus study: Design and methods. Contemp. Clin. Trials 2014, 38, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Worobey, J. Early family mealtime experiences and eating attitudes in normal weight, underweight and overweight females. Eat. Weight Disord. 2002, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Ayala, G.; Baquero, B.; Arrendondo, E.; Campbell, N.; Larios, M.; Elder, J. Association between family variables and Mexican American children’s dietary behaviors. J. Nutr. Educ. Behav. 2007, 39, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Taras, H.; Sallis, J.; Nader, P.; Nelson, J. Children’s television-viewing habits and the family environment. Am. J. Disabil. Child. 1990, 144, 357–359. [Google Scholar] [CrossRef]
- Worobey, J.; Islas-Lopez, M.; Hoffman, D. Maternal behavior and infant weight gain in the first year. J. Nutr. Educ. Behav. 2009, 41, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Byrd-Bredbenner, C.; Maurer Abbot, J.; Cussler, E. Relationship of social cognitive theory concepts to mothers’ dietary intake and BMI. Matern. Child Nutr. 2010, in press. [Google Scholar] [CrossRef] [PubMed]
- Coon, K.; Goldberg, J.; Rogers, B.; Tucker, K. Relationships between use of television during meals and children’s food consumption patterns. Pediatrics 2001, 107, e7. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.; Cullen, K.; Baranowski, T. BMI related to the number of meals eaten watching TV as reported by 4th to 6th grade students: Demographic differences. J. Am. Diet. Assoc. 2000, 100, A38. [Google Scholar]
- Newman, J.; Taylor, A. Effect of a means and contingency on young children’s food preferences. J. Exp. Child Psychol. 1992, 53, 200–216. [Google Scholar] [CrossRef]
- Birch, L.; Birch, D.; Marlin, D.; Kramer, L. Effects of instrumental consumption on children’s food preference. Appetite 1982, 3, 125–134. [Google Scholar] [CrossRef]
- Birch, L.; Marlin, D.; Rotter, J. Eating as the “means” activity in a contingency: Effects on young children’s food preference. Child Dev. 1984, 55, 431–439. [Google Scholar] [CrossRef]
- Fisher, J.; Birch, L. Restricting access to palatable food affects children’s behavioral response, food selection, and intake. Am. J. Clin. Nutr. 1999, 69, 1264–1272. [Google Scholar] [PubMed]
- Johnson, S.; Birch, L. Parents’ and children’s adiposity and eating style. Pediatrics 1994, 94, 653–661. [Google Scholar] [PubMed]
- Constanzo, P.; Woody, E. Domaine specific parenting styles and their impact on the child’s development of particular deviance; the example of obesity proneness. J. Soc. Clin. Psychol. 1985, 3, 425–445. [Google Scholar] [CrossRef]
- Fisher, J.; Birch, L. Parents’ restrictive feeding practices are associated with young girls’ negative self-evaluation about eating. J. Am. Diet. Assoc. 2000, 100, 1341–1346. [Google Scholar] [CrossRef]
- Birch, L.; Fisher, J. Development of eating behaviors among children and adolescents. Pediatrics 1998, 101, 539–549. [Google Scholar] [PubMed]
- Rhee, K.; Appugliese, D.; Prisco, A.; Kaciroti, N.; Corwyn, R.; Bradley, R.; Lumeng, J. Controlling maternal feeding practices associated with decreased dieting behavior in sixth-grade children. J. Am. Diet. Assoc. 2010, 110, 619–623. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.; Schwartz, M. If you are good you can have a cookie: How memories of childhood food rules link to adult eating behaviors. Eat. Behav. 2003, 4, 283–293. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Media Education in the Practice Setting. An Overview of the Media and the Pediatrician’s Role. Available online: http://www.aap.org/advocacy/mmcamp.htm (accessed on 5 January 2003).
- Mendoza, J.; Zimmerman, F.; Christakis, D. Television viewing, computer use, obesity, and adiposity in us preschool children. Int. J. Behav. Nutr. Phys. Act. 2007, 4, 44. [Google Scholar] [CrossRef] [PubMed]
- Crespo, C.; Smit, E.; Troiano, R.P.; Bartlett, S.; Macera, C.; Andersen, R. Television watching, energy intake, and obesity in us children. Arch. Pediatr. Adolesc. Med. 2001, 155, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Janz, K.; Dawson, J.; Mahoney, L. Tracking physical fitness and physical activity from childhood to adolescence: The Muscatine study. Med. Sci. Sports Exerc. 2000, 32, 1250–1257. [Google Scholar] [CrossRef] [PubMed]
- Saelens, B.; Sallis, J.; Nader, P.; Broyles, S.; Berry, C.; Taras, H. Home environmental influences on children’s television watching from early to middle childhood. Dev. Behav. Pediatr. 2002, 23, 127–132. [Google Scholar] [CrossRef]
- Goldberg, M.; Gorn, G.; Gibson, W. TV messages for snack and breakfast foods: Do they influence children’s preferences. J. Consum. Res. 1978, 5, 73–81. [Google Scholar] [CrossRef]
- Kattelmann, K.; White, A.; Nitzke, S.; Boeckner, L.; Greene, G.; Horacek, T.; Hoerr, S.; Phillips, B.; Colby, S.; Byrd-Bredbenner, C.; et al. Development of a Randomized Trial Guided by the Process of Precede-proceed for Prevention of Excessive Weight Gain in Communities of Young Adults. Available online: http://www.reeis.usda.gov/web/crisprojectpages/217242.html (accessed on 5 August 2015).
- Maurer Abbot, J.; Byrd-Bredbenner, C. Development of a Self-directed Home Kitchen Makeover for Mothers of Young Children. Available online: http://ncsu.edu/ffci/publications/2009/v14-n1-2009-spring/abbot.php (accessed on 5 August 2015).
- McGinnis, J.; Kraak, V. Food Marketing to Children and Youth. Threat or Opportunity? The National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Peterson, P.; Jeffrey, D.; Bridgwater, C.; Dawson, B. How pronutrition television programming affects children’s dietary habits. Dev. Psychol. 1984, 20, 55–63. [Google Scholar] [CrossRef]
- Scammon, D.; Christopher, C. Nutrition education with children via television: A review. J. Advert. Res. 1981, 10, 26–36. [Google Scholar] [CrossRef]
- Taras, H.; Sallis, J.; Patterson, T.; Nader, P.; Nelson, J. Television’s influence on children’s diet and physical activity. J. Dev. Behav. Pediatr. 1989, 10, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Goran, M.; Treuth, M. Energy expenditure, physical activity, and obesity in children. Pediatr. Clin. N. Am. 2001, 48, 31–53. [Google Scholar] [CrossRef]
- Bar-Or, O.; Foreyt, J.; Bouchard, C.; Al, E. Physical activity, genetic, and nutritional considerations in childhood weight management. Med. Sci. Sports Exerc. 1998, 30, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Poirier, P.; Despres, J. Exercise in weight management of obesity. Cardiol. Clin. 2001, 19, 459–470. [Google Scholar] [CrossRef]
- Landers, D.; Arent, S. Physical activity and mental health. In The Handbook of Sport Psychology, 2nd ed.; Singer, R., Hausenblaus, H., Janelle, C., Eds.; Wiley: New York, NY, USA, 2001; pp. 740–765. [Google Scholar]
- National Center for Education Statistics. Household Education Survey Parent Survey. Available online: http://nces.ed.gov/nhes/dataproducts.asp#1999dp (accessed on 7 May 2010).
- U.S. Department of Health and Human Services. National Institutes of Health. We can! Ways to Enhance Children’S Activity & Nutrition. Available online: http://www.nhlbi.nih.gov/health/public/heart/obesity/wecan/ (accessed on 5 August 2015).
- Veitch, J.; Salmon, J.; Ball, K. Individual, social and physical environmental correlates of children’s active free-play: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Hongu, N. Indoor Activities for You and Your Child. Extension, Families, Food and Fitness. Available online: http://www.extension.org/pages/Indoor_Activities_for_You_and_Your_Child (accessed on 12 June 2010).
- Duncan, M. The Effect of 6-weeks Active Video Games on Body Mass Index and Physical Activity during School Recess. Available online: http://www.slideshare.net/gamercize/the-effect-of-6weeks-active-video-games-on-body-mass-index-and-physical-activity-during-school-recess (accessed on 5 August 2015).
- Lanningham-Foster, L.; Jensen, T.; Foster, R.; Redmond, A.; Walker, B.; Heinz, D.; Levine, J. Energy expenditure of sedentary screen time compared with active screen time for children. Pediatrics 2006, 118, e1831–e1835. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.; Killen, J.; Kraemer, H.; Wilson, D.; Matheson, D.; Haskell, W.; Pruitt, L.; Powell, T.; Owens, A.; Thompson, N.; et al. Dance and reducing television viewing to prevent weight gain in african-american girls: The stanford fems pilot study. Ethn. Dis. 2003, 13, S65–S77. [Google Scholar] [PubMed]
- Golem, D.; Martin-Biggers, J.; Koenings, M.; Finn Davis, K.; Byrd-Bredbenner, C. An integrative review of sleep for nutrition professionals. Adv. Nutr. 2014, 5, 742–759. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, L. Who’s Minding Thekids? Child Care Arrangements: Spring 2011; U.S. Census Bureau: Washington, DC, USA, 2013. [Google Scholar]
- Freedman, M.; Alvarez, K. Early childhood feeding: Assessing knowledge, attitude, and practices of multi-ethnic child-care providers. J. Am. Diet. Assoc. 2009, 109, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Note 1: The final R & D version of the HomeStyles guides are available at HealthyHomeStyles.com/About/ResearchDev.
- Gump, D. Headline writing. Journal. Mass Commun. Q. 2006, 83, 939–940. [Google Scholar]
- McGlaughlin, F.; Powell, J.; Doty, T. Headline Optimization: How Testing 10 Headlines Revealed a 3-letter Word that Improved Conversion more than Major Changes. Available online: http://www.marketingexperiments.com/marketing-optimization/optimizing-headlines.html (accessed on 5 August 2015).
- Malkin, A.; Wornina, K.; Chrisler, J. Women and weight: Gendered messages on magazine covers. Sex Roles 1999, 40, 647–655. [Google Scholar] [CrossRef]
- Lee, D. Make the cover a sales tool. Folio Mag. Mag. Manag. 1998, 27, 9–10. [Google Scholar]
- Martin-Biggers, J.; Beluska, K.; Quick, V.; Tursia, M.; Byrd-Bredbenner, C. Cover lines using positive, urgent, unique language entice moms to read health communications. J. Health Commun. 2015, 20, 766–772. [Google Scholar] [CrossRef] [PubMed]
- Healey, K.; Thombs, D. Fruit-vegetable consumption self-efficacy in youth. Am. J. Health Behav. 1997, 21, 172–177. [Google Scholar]
- Schwartz, J.; Byrd-Bredbenner, C. Formative evaluation in health education: An exploratory study of the usefulness of the cognitive response method. Health Educ. 2006, 106, 32–41. [Google Scholar] [CrossRef]
- Shepherd, S.; Sims, L. Employing cognitive response analysis to examine message acceptance in nutrition education. J. Nutr. Educ. 1990, 22, 215–219. [Google Scholar] [CrossRef]
- Note 2: The HomeStyles guides are available at HealthyHomeStyles.com/About/eBook/English and HealthyHomeStyles.com/About/eBook/Spanish.
- Agency for Healthcare Research and Quality. AHRQ Activities Using Community-based Participatory Research to Address Health Care Disparities. Available online: http://www.ahrq.gov/research/findings/factsheets/minority/cbprbrief/index.html (accessed on 27 February 2015).
- Whitlock, E.; O’Connor, E.; Williams, S.; Beil, T.; Lutz, K. Effectiveness of Weight Management in Children and Adolescents; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Stice, E.; Shaw, H.; Marti, C.N. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychol. Bull. 2006, 132, 667–691. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.; Carroll, M.; Flegal, K. High body mass index for age among US children and adolescents, 2003–2006. JAMA 2008, 299, 2401–2405. [Google Scholar] [CrossRef] [PubMed]
- Crockett, S.; Sims, L. Environmental influences in children’s eating. J. Nutr. Educ. 1995, 27, 235–249. [Google Scholar] [CrossRef]
- Patrick, H.; Nicklas, T. A review of family and social determinants of children’s eating patterns and diet quality. J. Am. Coll. Nutr. 2005, 24, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, J.; Harden, A.; Rees, R.; Brunton, G.; Garcia, J.; Oliver, S.; Oakley, A. Young people and healthy eating: A systematic review of research on barriers and facilitators. Health Educ. Res. 2006, 21, 239–257. [Google Scholar] [CrossRef] [PubMed]
- Story, M.; Neumark-Sztainer, D.; French, S. Individual and environmental influences on adolescent eating behaviors. J. Am. Diet. Assoc. 2002, 102, S40–S51. [Google Scholar] [CrossRef]
- Byrd-Bredbenner, C.; Maurer Abbot, J. Improving the nutritional quality of the home food environment using self-directed home kitchen makeovers. Forum Fam. Consum. Issues 2009, 14, 1–8. [Google Scholar]
- Evans, A.; Dave, J.; Tanner, A.; Duhe, S.; Condrasky, M.; Wilson, D.; Griffin, S.; Palmer, M.; Evans, M. Changing the home nutrition environment: Effects of a nutrition and media literacy pilot intervention. Fam. Commun. Health 2006, 2006, 43–54. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martin-Biggers, J.; Spaccarotella, K.; Delaney, C.; Koenings, M.; Alleman, G.; Hongu, N.; Worobey, J.; Byrd-Bredbenner, C. Development of the Intervention Materials for the HomeStyles Obesity Prevention Program for Parents of Preschoolers. Nutrients 2015, 7, 6628-6669. https://doi.org/10.3390/nu7085301
Martin-Biggers J, Spaccarotella K, Delaney C, Koenings M, Alleman G, Hongu N, Worobey J, Byrd-Bredbenner C. Development of the Intervention Materials for the HomeStyles Obesity Prevention Program for Parents of Preschoolers. Nutrients. 2015; 7(8):6628-6669. https://doi.org/10.3390/nu7085301
Chicago/Turabian StyleMartin-Biggers, Jennifer, Kim Spaccarotella, Colleen Delaney, Mallory Koenings, Gayle Alleman, Nobuko Hongu, John Worobey, and Carol Byrd-Bredbenner. 2015. "Development of the Intervention Materials for the HomeStyles Obesity Prevention Program for Parents of Preschoolers" Nutrients 7, no. 8: 6628-6669. https://doi.org/10.3390/nu7085301
APA StyleMartin-Biggers, J., Spaccarotella, K., Delaney, C., Koenings, M., Alleman, G., Hongu, N., Worobey, J., & Byrd-Bredbenner, C. (2015). Development of the Intervention Materials for the HomeStyles Obesity Prevention Program for Parents of Preschoolers. Nutrients, 7(8), 6628-6669. https://doi.org/10.3390/nu7085301





