The Impact of a Prolonged Multivitamin Shortage on Home Parenteral Nutrition Patients: A Single-Center Retrospective Cohort Study with Case Reports of Wernicke’s Encephalopathy
Abstract
1. Introduction
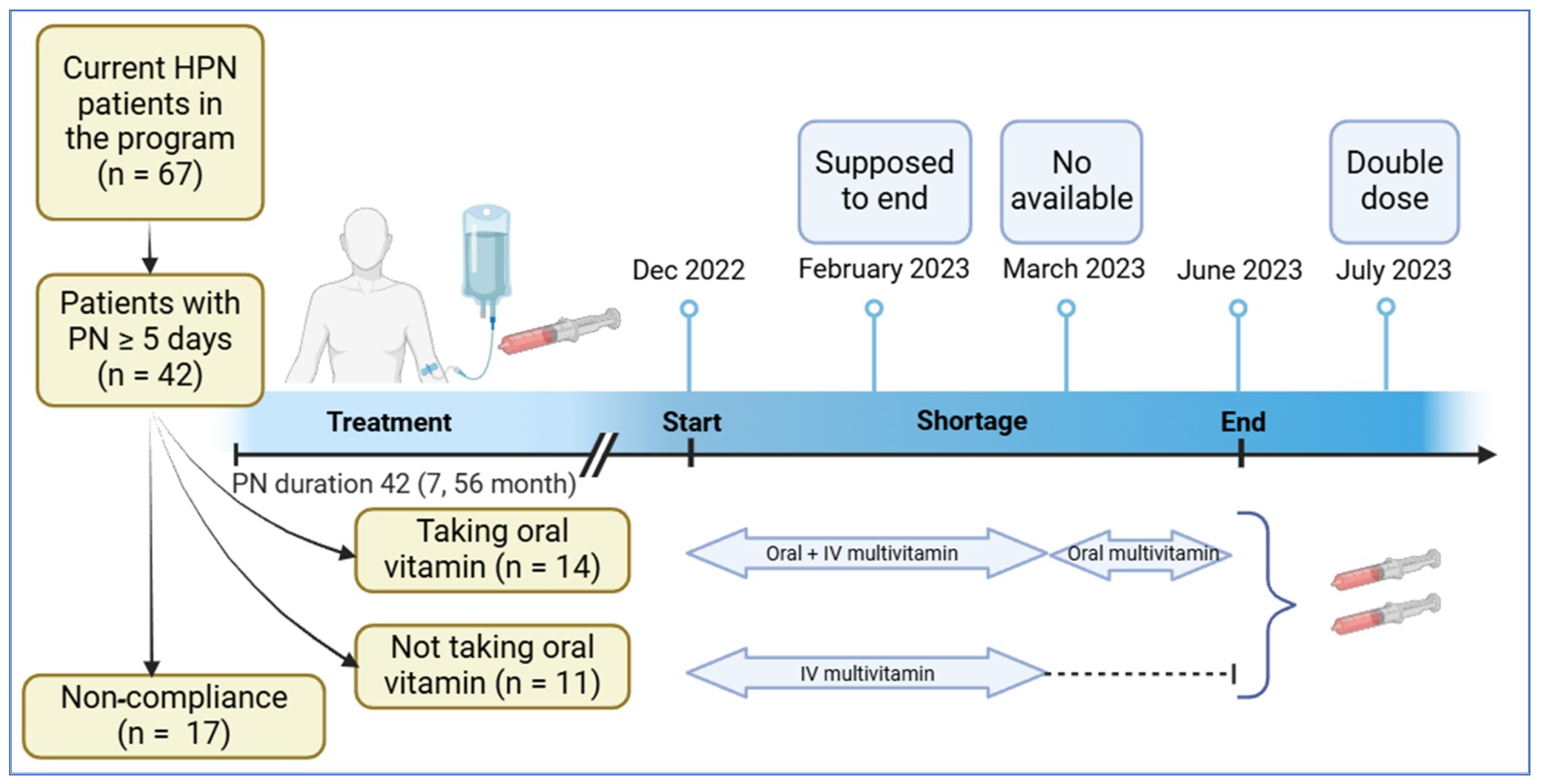
2. Materials and Methods
3. Results
3.1. Results from Retrospective Cohort Study
3.2. Case Reports of Patients Who Required Hospitalization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ASPEN | American Society for Parenteral and Enteral Nutrition |
| CDC | Centers for Disease Control and Prevention |
| DRIs | Dietary reference intakes |
| ESPEN | European Society for Clinical Nutrition and Metabolism |
| ETKA | Erythrocyte transketolase activity |
| G-tube | Gastrostomy tube |
| HPN | Home parenteral nutrition |
| IV | Intravenous |
| MRI | Magnetic resonance imaging |
| PN | Parenteral nutrition |
| WE | Wernicke’s encephalopathy |
References
- Winkler, M.F.; Hagan, E.; Wetle, T.; Smith, C.; Maillet, J.O.; Touger-Decker, R. An exploration of quality of life and the experience of living with home parenteral nutrition. JPEN J. Parenter. Enter. Nutr. 2010, 34, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Allan, P.; Lal, S. Intestinal failure: A review. F1000Research 2018, 7, 85. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L. Definitions of intestinal failure and the short bowel syndrome. Best Pract. Res. Clin. Gastroenterol. 2016, 30, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Yeh, D.D.; Ortiz-Reyes, L.A.; Chang, Y.; Quraishi, S.A. Impact of nationwide essential trace element shortages: A before-after, single-center analysis of hospitalized adults receiving home parenteral nutrition therapy. Nutr. Clin. Pract. 2022, 37, 442–450. [Google Scholar] [CrossRef]
- Drug Product Database Online Query. Canada. 2006. Available online: https://health-products.canada.ca/dpd-bdpp/dispatch-repartition (accessed on 1 April 2025).
- Jin, J.; Mulesa, L.; Carrilero Rouillet, M. Trace Elements in Parenteral Nutrition: Considerations for the Prescribing Clinician. Nutrients 2017, 9, 440. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Lactic acidosis traced to thiamine deficiency related to nationwide shortage of multivitamins for total parenteral nutrition—United States, 1997. MMWR Morb. Mortal. Wkly. Rep. 1997, 46, 523–528. [Google Scholar]
- Plogsted, S.; Adams, S.C.; Allen, K.; Cober, M.P.; Greaves, J.; Mogensen, K.M.; Ralph, A.; Ward, C.; Ybarra, J.; Holcombe, B. Parenteral Nutrition Amino Acids Product Shortage Considerations. Nutr. Clin. Pract. 2016, 31, 560–561. [Google Scholar] [CrossRef]
- Palm, E.; Dotson, B. Copper and Zinc Deficiency in a Patient Receiving Long-Term Parenteral Nutrition During a Shortage of Parenteral Trace Element Products. JPEN J. Parenter. Enter. Nutr. 2015, 39, 986–989. [Google Scholar] [CrossRef]
- Mirtallo, J.M.; Holcombe, B.; Kochevar, M.; Guenter, P. Parenteral nutrition product shortages: The A.S.P.E.N. strategy. Nutr. Clin. Pract. 2012, 27, 385–391. [Google Scholar] [CrossRef]
- Hahn, J.S.; Berquist, W.; Alcorn, D.M.; Chamberlain, L.; Bass, D. Wernicke encephalopathy and beriberi during total parenteral nutrition attributable to multivitamin infusion shortage. Pediatrics 1998, 101, E10. [Google Scholar] [CrossRef]
- Penitzka, S.; Schönenberger, K.A.; Huwiler, V.V.; Reber, E.; Stanga, Z.; Mühlebach, S. Impact of Parenteral Multivitamins Shortage in Switzerland. Clin. Nutr. ESPEN 2023, 54, 625. [Google Scholar] [CrossRef]
- Hoo, F.-W.; Chang, C.-T.; Amran, M.H.H. Multivitamin Product Shortage: Experience in a Tertiary Referral Hospital in Malaysia. Malays. J. Pharm. 2024, 10, 1. [Google Scholar] [CrossRef]
- 2021 Parenteral Nutrition Multivitamin Product Shortage Considerations. 2021. Available online: https://nutritioncare.org/PN-MVdosingconsiderations (accessed on 1 December 2022).
- Berger, M.M.; Shenkin, A.; Schweinlin, A.; Amrein, K.; Augsburger, M.; Biesalski, H.K.; Bischoff, S.C.; Casaer, M.P.; Gundogan, K.; Lepp, H.L.; et al. ESPEN micronutrient guideline. Clin. Nutr. 2022, 41, 1357–1424. [Google Scholar] [CrossRef] [PubMed]
- Plogsted, S.; Adams, S.C.; Allen, K.; Cober, M.P.; Greaves, J.; Mogensen, K.M.; Ralph, A.; Ward, C.; Ybarra, J.; Holcombe, B.; et al. Parenteral Nutrition Multivitamin Product Shortage Considerations. Nutr. Clin. Pract. 2016, 31, 556–559. [Google Scholar] [CrossRef]
- ASPEN. Parenteral Nutrition Product Shortage Recommendations: Intravenous Multivitamins. Available online: https://nutritioncare.org/wp-content/uploads/2024/12/Intravenous-Multivitamin-Shortage-Recommendations.pdf (accessed on 1 December 2024).
- Jeppesen, P.B.; Mortensen, P.B. Intestinal failure defined by measurements of intestinal energy and wet weight absorption. Gut 2000, 46, 701–706. [Google Scholar] [CrossRef]
- Shaw, C.; Bassett, R.L.; Fox, P.S.; Schmeler, K.M.; Overman, M.J.; Wallace, M.J.; Gupta, S.; Tam, A. Palliative venting gastrostomy in patients with malignant bowel obstruction and ascites. Ann. Surg. Oncol. 2013, 20, 497–505. [Google Scholar] [CrossRef]
- Hanson, C.; Thoene, M.; Wagner, J.; Collier, D.; Lecci, K.; Anderson-Berry, A. Parenteral nutrition additive shortages: The short-term, long-term and potential epigenetic implications in premature and hospitalized infants. Nutrients 2012, 4, 1977–1988. [Google Scholar] [CrossRef]
- Lykstad, J.; Sharma, S. Biochemistry, Water Soluble Vitamins. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Kim, W.J.; Kim, M.M. Wernicke’s Encephalopathy Presenting with Bilateral Complete Horizontal and Downward Gaze Palsy in a Malnourished Patient. Korean J. Ophthalmol. 2017, 31, 372–374. [Google Scholar] [CrossRef]
- Zuccoli, G.; Pipitone, N. Neuroimaging findings in acute Wernicke’s encephalopathy: Review of the literature. AJR Am. J. Roentgenol. 2009, 192, 501–508. [Google Scholar] [CrossRef]
- Parenteral, A.S.f.; Nutrition, E. Deaths associated with thiamine-deficient total parenteral nutrition. Morb. Mortal. Wkly. Rep. 1989, 38, 43–46. [Google Scholar]
- Perko, R.; Harreld, J.H.; Helton, K.J.; Sabin, N.D.; Haidar, C.E.; Wright, K.D. What goes around comes around? Wernicke encephalopathy and the nationwide shortage of intravenous multivitamins revisited. J. Clin. Oncol. 2012, 30, e318–e320. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stillhart, C.; Vucicevic, K.; Augustijns, P.; Basit, A.W.; Batchelor, H.; Flanagan, T.R.; Gesquiere, I.; Greupink, R.; Keszthelyi, D.; Koskinen, M.; et al. Impact of gastrointestinal physiology on drug absorption in special populations—An UNGAP review. Eur. J. Pharm. Sci. 2020, 147, 105280. [Google Scholar] [CrossRef] [PubMed]
- Campagnutta, E.; Cannizzaro, R.; Gallo, A.; Zarrelli, A.; Valentini, M.; De Cicco, M.; Scarabelli, C. Palliative treatment of upper intestinal obstruction by gynecological malignancy: The usefulness of percutaneous endoscopic gastrostomy. Gynecol. Oncol. 1996, 62, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Thampy, S.; Najran, P.; Mullan, D.; Laasch, H.U. Safety and Efficacy of Venting Gastrostomy in Malignant Bowel Obstruction: A Systematic Review. J. Palliat. Care 2020, 35, 93–102. [Google Scholar] [CrossRef]
- O’Malley, G.F.; O’Malley, R. Wernicke Encephalopathy. Available online: https://www.merckmanuals.com/en-ca/professional/special-subjects/illicit-drugs-and-intoxicants/wernicke-encephalopathy (accessed on 1 December 2024).
- Thomson, A.D.; Guerrini, I.; Marshall, E.J. Wernicke’s Encephalopathy: Role of Thiamine. Pract. Gastroenterol. 2009, 33, 21–30. [Google Scholar]
- Pironi, L.; Boeykens, K.; Bozzetti, F.; Joly, F.; Klek, S.; Lal, S.; Lichota, M.; Mühlebach, S.; Van Gossum, A.; Wanten, G.; et al. ESPEN practical guideline: Home parenteral nutrition. Clin. Nutr. 2023, 42, 411–430. [Google Scholar] [CrossRef]
- Worthington, P.; Balint, J.; Bechtold, M.; Bingham, A.; Chan, L.N.; Durfee, S.; Jevenn, A.K.; Malone, A.; Mascarenhas, M.; Robinson, D.T.; et al. When Is Parenteral Nutrition Appropriate? JPEN J. Parenter. Enter. Nutr. 2017, 41, 324–377. [Google Scholar] [CrossRef]
- Nakamura, Z.M.; Tatreau, J.R.; Rosenstein, D.L.; Park, E.M. Clinical Characteristics and Outcomes Associated with High-Dose Intravenous Thiamine Administration in Patients with Encephalopathy. Psychosomatics 2018, 59, 379–387. [Google Scholar] [CrossRef]
- Culkin, A.; Brundrett, D.; Pearson, M.; Gabe, S. A one size vial does not fit all: An evaluation of the micronutrient status of adult patients receiving home parenteral nutrition (HPN). Clin. Nutr. ESPEN 2023, 57, 676–682. [Google Scholar] [CrossRef]
| Variables | Overall (n = 25) | Vitamins Taken (n = 14) | Vitamins Not Taken (n = 11) | p-Value |
|---|---|---|---|---|
| Age (years) | 57 (42, 68) | 64 (55, 70) | 43 (21, 67) | 0.037 |
| Female | 17 (68%) | 12 (85.71%) | 5 (45.45%) | 0.081 |
| Height (cm) | 163 (158, 172) | 164 (162, 169.5) | 159 (152, 175) | 0.57 |
| Weight (kg) | 55.5 (48, 68.2) | 61.6 (53, 74.4) | 48.9 (40.6, 68.2) | 0.12 |
| BMI (kg/m2) | 20.7 (18.7, 23.6) | 21.35 (20.2, 24.8) | 187 (16, 21.6) | 0.08 |
| Indication for PN | ||||
| SBS | 15 (60%) | 8 (57.14%) | 7 (63.64%) | 0.63 |
| GI dysmotility | 5 (20%) | 4 (28.57%) | 1 (9.09%) | |
| Malignancy | 5 (20%) | 2 (14.29%) | 3 (27.27%) | |
| Some oral intakes | 17 (68%) | 10 (71.4%) | 7 (63.63%) | 0.86 |
| Use of venting G tube | 2 (8%) | 1 (7.14%) | 1 (9.09%) | 1.00 |
| TC (kcal/d) | 1542 (1368, 1792) | 1516 (1400, 1735) | 1545 (1334, 1800) | 0.87 |
| Protein (g/d) | 75 (60, 95) | 75 (65, 95) | 75 (55, 95) | 0.51 |
| Lipid (g/d) | 50 (45, 55) | 50 (45, 55) | 45 (40, 60) | 0.36 |
| Dextrose (g/d) | 250 (200, 260) | 250 (200, 260) | 225 (210, 280) | 0.91 |
| PN (d/week) | 7 (6, 7) | 7 (6, 7) | 7 (7, 7) | 0.07 |
| PN duration (months) | 42 (7, 56) | 52.5 (20, 83) | 9 (6, 42) | 0.02 |
| PN volume (mL) | 1800 (1680, 2400) | 2000 (1650, 2580) | 1800 (1710, 2200) | 0.39 |
| Overall (n = 25) | Vitamins Taken (n = 14) | Vitamins Not Taken (n = 11) | p-Value | |
|---|---|---|---|---|
| Symptom reported | 17 (68%) | 9 (64.29%) | 8 (72.73%) | 1.00 |
| Hospitalization | 3 (12%) | 2 (14.29%) | 1 (9.09%) | 1.00 |
| Diagnosed deficiency | 2 (8%) | 2 (14.29%) | 0 (0%) | 0.50 |
| Baseline Level | After Shortage Concluded | Change | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Vitamins Taken | N | Not Taken | p | N | Vitamins Taken | N | Not Taken | p | N | Vitamins Taken | N | Not Taken | p | |
| Glucose (mmol/L) | 14 | 5.15 (4.8, 5.7) | 11 | 6.0 (5.3, 6.3) | 0.03 | 13 | 5.90 (5.20, 6.40) | 11 | 5.50 (5.20, 6.40) | 0.77 | 13 | 0.4 (−0.5, 2.3) | 11 | −0.2 (−0.80, 1.10) | 0.3 |
| BUN (mmol/L) | 14 | 8.40 (5.6, 11.1) | 9 | 7.70 (6.3, 10.5) | 0.75 | 13 | 6.30 (5.20, 9.70) | 8 | 8.00 (5.25, 11.70) | 0.83 | 13 | −0.3 (−1.1, 0.1) | 8 | −0.65 (−1.70, 1.30) | 0.64 |
| Creatinine (μmol/L) | 14 | 87 (61, 122) | 11 | 60 (57, 81) | 0.14 | 13 | 88 (61, 107) | 11 | 61 (48, 86) | 0.12 | 13 | −4 (−22, 10) | 11 | 4 (−12, 9) | 0.28 |
| Sodium (mmol/L) | 14 | 139.5 (137, 141) | 11 | 136 (135, 138) | 0.05 | 13 | 140 (136, 141) | 11 | 135 (135, 137) | 0.04 | 13 | 0 (−4, 2) | 11 | −1 (−2, 2) | 0.82 |
| Potassium (mmol/L) | 14 | 3.95 (3.80, 4.30) | 11 | 4.10 (3.80, 4.50) | 0.89 | 13 | 3.90 (3.60, 4.60) | 11 | 4.20 (3.80, 4.80) | 0.41 | 13 | −0.1 (−0.4, 0.4) | 11 | 0.30 (0.10, 0.40) | 0.31 |
| Bicarbonate (mmol/L) | 11 | 23 (20, 27) | 8 | 25 (23.5, 28) | 0.32 | 10 | 23.5 (20, 26) | 8 | 24 (23, 24.5) | 0.93 | 10 | 0 (−0.9, 1) | 7 | −2 (−8, −1) | 0.04 |
| Chloride (mmol/L) | 14 | 105 (101, 107) | 11 | 105 (103, 106) | 0.72 | 13 | 103 (102, 107) | 11 | 105 (102, 107) | 0.95 | 13 | 0 (−3, 3) | 11 | −1 (−4, 1) | 0.6 |
| Calcium (mmol/L) | 13 | 2.26 (2.21, 2.51) | 11 | 2.22 (2.14, 2.33) | 0.47 | 13 | 2.36 (2.22, 2.47) | 11 | 2.35 (2.12, 2.42) | 0.79 | 12 | 0.02 (−0.16, 0.16) | 11 | 0.05 (−0.05, 0.18) | 0.88 |
| Mg (mmol/L) | 14 | 0.82 (0.78, 0.93) | 11 | 0.82 (0.76, 0.96) | 0.91 | 13 | 0.89 (0.82, 0.91) | 11 | 0.80 (0.76, 0.90) | 0.27 | 13 | −0.01 (−0.12, 0.08) | 11 | 0.01 (−0.13, 0.07) | 0.75 |
| Phosphate (mmol/L) | 14 | 1.18 (1.03, 1.31) | 11 | 1.12 (0.93, 1.36) | 0.48 | 13 | 1.10 (0.97, 1.18) | 11 | 1.23 (1.03, 1.34) | 0.16 | 13 | −0.06 (−0.24, 0.05) | 11 | 0.10 (−0.12, 0.28) | 0.12 |
| ALT (U/L) | 14 | 22 (16, 38) | 11 | 20 (12, 49) | 0.83 | 13 | 27 (14, 31) | 11 | 12 (10, 24) | 0.1 | 13 | −5 (−13, 3) | 11 | −6 (−39, −2) | 0.21 |
| ALP (U/L) | 14 | 91 (74, 147) | 11 | 111 (79, 407) | 0.6 | 13 | 117 (92, 140) | 11 | 105 (72, 232) | 0.98 | 13 | 7 (−4, 14) | 11 | 3 (−53, 82) | 0.98 |
| GGT (U/L) | 14 | 39 (14, 84) | 9 | 33 (23, 150) | 0.47 | 12 | 42.5 (16, 102) | 9 | 29 (22, 64) | 0.97 | 12 | −0.5 (−16.5, 2.5) | 9 | −1 (−25, 5) | 0.67 |
| Bilirubin (μmol/L) | 14 | 7.0 (4.0, 12.0) | 11 | 6.0 (5.0, 9.0) | 0.87 | 13 | 8.0 (4.0, 13.0) | 11 | 7.0 (5.0, 11.0) | 0.73 | 13 | 0.0 (−1.0, 1.0) | 11 | 1.00 (−6.00, 4.00) | 0.66 |
| Albumin (g/L) | 14 | 37.0 (34.0, 39.0) | 11 | 33.0 (26.0, 42.0) | 0.46 | 13 | 39.0 (34.0, 42.0) | 11 | 32.0 (31.0, 39.0) | 0.28 | 13 | 1.6 (−4.0, 3.0) | 11 | 0.0 (−4.0, 7.0) | 1 |
| Vitamin A (μmol/L) | 10 | 1.75 (1.00, 2.10) | 6 | 1.50 (1.30, 2.20) | 0.62 | 6 | 1.90 (1.20, 2.80) | 5 | 1.90 (1.60, 2.30) | 1 | 6 | 0.1 (−0.10, 0.2) | 4 | −0.00 (−0.60, 0.90) | 1 |
| Vitamin D (μmol/L) | 11 | 58.0 (35.0, 73.0) | 6 | 38.5 (21.0, 57.2) | 0.08 | 8 | 62.5 (45.5, 85.8) | 5 | 40.4 (31.0, 53.0) | 0.24 | 7 | 0.0 (−1.0, 9.7) | 4 | 4.5 (−2.5, 14.2) | 0.57 |
| PTH (pmol/L) | 10 | 5.95 (3.40, 9.30) | 4 | 2.40 (1.85, 4.35) | 0.07 | 4 | 7.25 (5.35, 8.25) | 3 | 5.40 (1.80, 6.20) | 0.16 | 3 | 2.10 (0.30, 2.40) | 2 | 1.20 (−0.40, 2.80) | 1 |
| Vitamin E (μmol/L) | 1 | 33 (33, 33) | 2 | 33 (32, 34) | N/A | 5 | 39.0 (36.0, 41.7) | 5 | 31.9 (28.0, 33.5) | 0.12 | 0 | NA | 1 | −4.0 (−4.0, −4.0) | N/A |
| INR | 14 | 1.10 (1.00, 1.16) | 10 | 1.05 (1.00, 1.20) | 0.85 | 13 | 1.00 (1.00, 1.10) | 9 | 1.20 (1.10, 1.20) | 0.04 | 13 | 0.0 (−0.1, 0.0) | 8 | 0.10 (0.00, 0.15) | 0.03 |
| B12 (pmol/L) | 11 | 544 (352, 871) | 8 | 574 (402.5, 762.5) | 0.93 | 11 | 414 (363, 835) | 7 | 465 (269, 598) | 0.29 | 10 | −143.5 (−213, −30) | 7 | −66 (−266, 1) | 0.56 |
| Hemoglobin (g/L) | 14 | 115.5 (95, 121) | 10 | 101.5 (82, 125) | 0.56 | 13 | 122 (102, 128) | 10 | 100.5 (88, 141) | 0.57 | 13 | 2 (−8, 10) | 10 | 2 (−16, 16) | 0.93 |
| Platelets (×109/L) | 14 | 182.0 (164.0, 291.0) | 10 | 294.5 (215.0, 397.0) | 0.04 | 13 | 181.0 (167.0, 280.0) | 10 | 317.0 (251.0, 411.0) | 0.05 | 13 | −3.0 (−30.0, 38.0) | 10 | −1.0 (−93.0, 69.0) | 1 |
| WBC (×109/L) | 14 | 0 (0, 0) | 10 | 0 (0, 0) | 0.24 | 14 | 0 (0, 0) | 10 | 0 (0, 0) | 1 | 14 | 0 (0, 0) | 9 | 0 (0, 0) | 0.21 |
| Variable | Patient No. 1 | Patient No. 2 | Patient No. 3 |
|---|---|---|---|
| Age (years) | 59 | 70 | 56 |
| Sex | Female | Female | Female |
| Weight (kg) | 67.1 | 68.4 | 48.5 |
| Body Mass Index (kg/m2) | 25.25 | 25.74 | 20.88 |
| Indication for PN | High output entero-vaginal fistula | Short bowel syndrome in the context of hollow visceral myopathy | Malignant bowel obstruction secondary to metastatic ovarian cancer |
| Oral diet | No | Minimal oral diet | No |
| Oral multivitamin | Centrum | Vitafusion | Nature’s Bounty Liquid B Complex |
| Use of venting tube | None | 2–2.5 L/d | Substantial |
| Total calories (kcal/d) | 1920 | 1252 | 1654 |
| Protein (g/d) | 100 | 60 | 80 |
| Dextrose (g/d) | 280 | 180 | 260 |
| PN frequency (d/week) | 7 | 7 | 7 |
| Add-ins | Octreotide 300 mcg | Famotidine 20 mg | Famotidine 40 mg |
| Precipitate | Severe nausea and vomiting | None | None |
| Neurological symptoms | Dizziness, double vision and weakness | Diplopia, declining mobility and weakness, and dizziness | Vertigo, gait instability, and diplopia |
| MRI results | Abnormal FLAIR signal observed in the dorsal medial thalami, around the third ventricle, tectal plate, and periaqueductal gray matter, accompanied by subtle increased signal intensity and facilitated diffusion on diffusion-weighted imaging | Subtle increased FLAIR signal noted in the medial thalami, periaqueductal gray, with subtle enhancement through the dorsal midbrain/memory bodies | Interval growth of left inferior cerebellar lesion. Normalization of signal abnormalities dorsomedially in the thalami with equivocal persistent increased signal in the peri aqueductal matter |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Unhapipatpong, C.; Lam, N.C.; Wang, C.; Schwenger, K.J.P.; Arca, C.; Chin, K.-W.; MacGillivray, A.; Yuen, C.; Pang, I.; Allard, J.P. The Impact of a Prolonged Multivitamin Shortage on Home Parenteral Nutrition Patients: A Single-Center Retrospective Cohort Study with Case Reports of Wernicke’s Encephalopathy. Nutrients 2025, 17, 1500. https://doi.org/10.3390/nu17091500
Unhapipatpong C, Lam NC, Wang C, Schwenger KJP, Arca C, Chin K-W, MacGillivray A, Yuen C, Pang I, Allard JP. The Impact of a Prolonged Multivitamin Shortage on Home Parenteral Nutrition Patients: A Single-Center Retrospective Cohort Study with Case Reports of Wernicke’s Encephalopathy. Nutrients. 2025; 17(9):1500. https://doi.org/10.3390/nu17091500
Chicago/Turabian StyleUnhapipatpong, Chanita, Natalie C. Lam, Christopher Wang, Katherine J. P. Schwenger, Celeste Arca, Ka-Wai Chin, Ann MacGillivray, Clement Yuen, Ian Pang, and Johane P. Allard. 2025. "The Impact of a Prolonged Multivitamin Shortage on Home Parenteral Nutrition Patients: A Single-Center Retrospective Cohort Study with Case Reports of Wernicke’s Encephalopathy" Nutrients 17, no. 9: 1500. https://doi.org/10.3390/nu17091500
APA StyleUnhapipatpong, C., Lam, N. C., Wang, C., Schwenger, K. J. P., Arca, C., Chin, K.-W., MacGillivray, A., Yuen, C., Pang, I., & Allard, J. P. (2025). The Impact of a Prolonged Multivitamin Shortage on Home Parenteral Nutrition Patients: A Single-Center Retrospective Cohort Study with Case Reports of Wernicke’s Encephalopathy. Nutrients, 17(9), 1500. https://doi.org/10.3390/nu17091500






