Impact of Enteral Nutrition on Clinical Outcomes in Very Low Birth Weight Infants in the NICU: A Single-Center Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Statistical Analysis
3. Results
3.1. Study Population
3.2. Feeding Practices
3.3. Incidence of Morbidities
3.4. Main Outcome
3.5. Secondary Outcome
4. Discussion
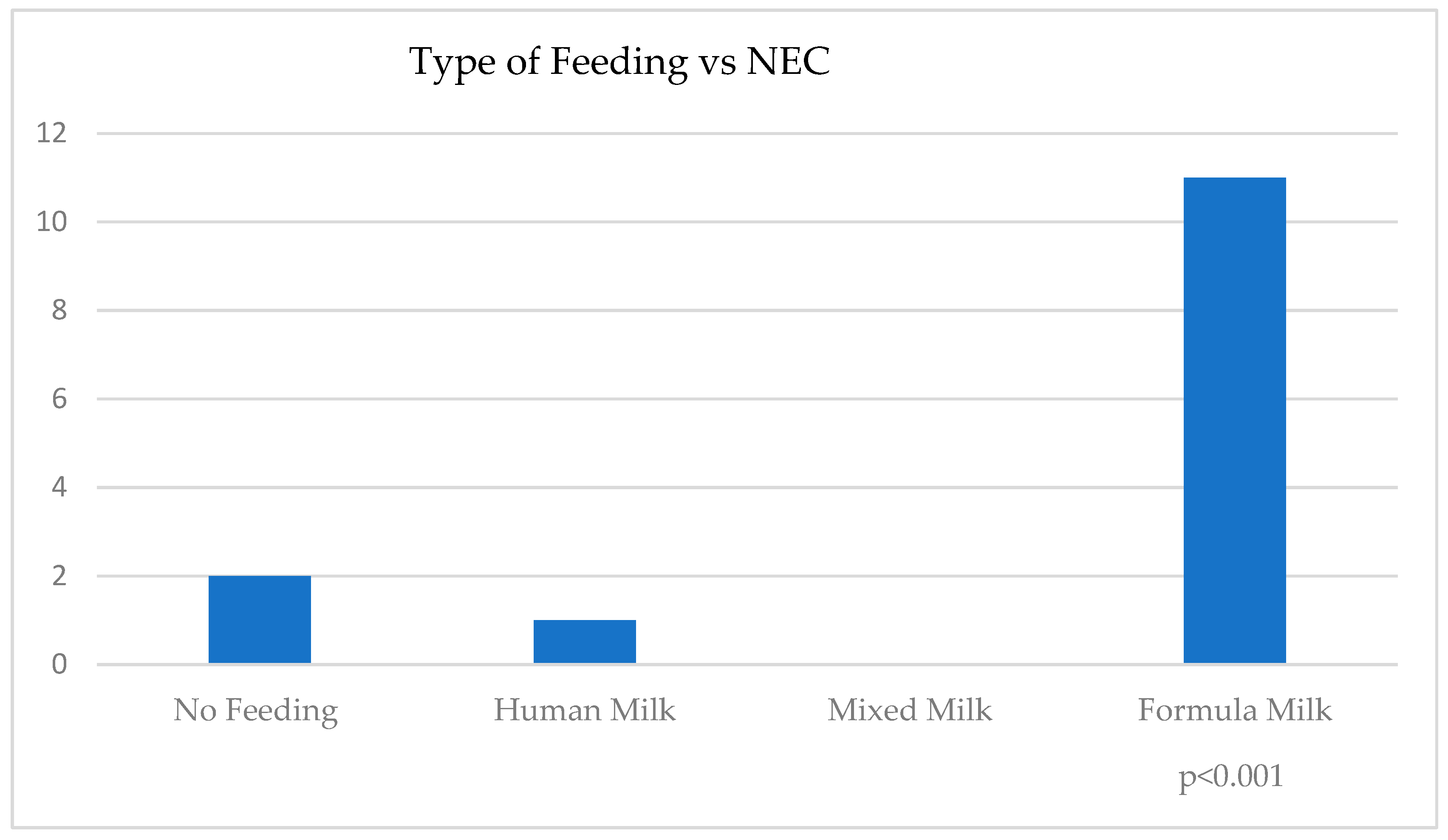
4.1. NEC
4.2. ROP
4.3. LOS
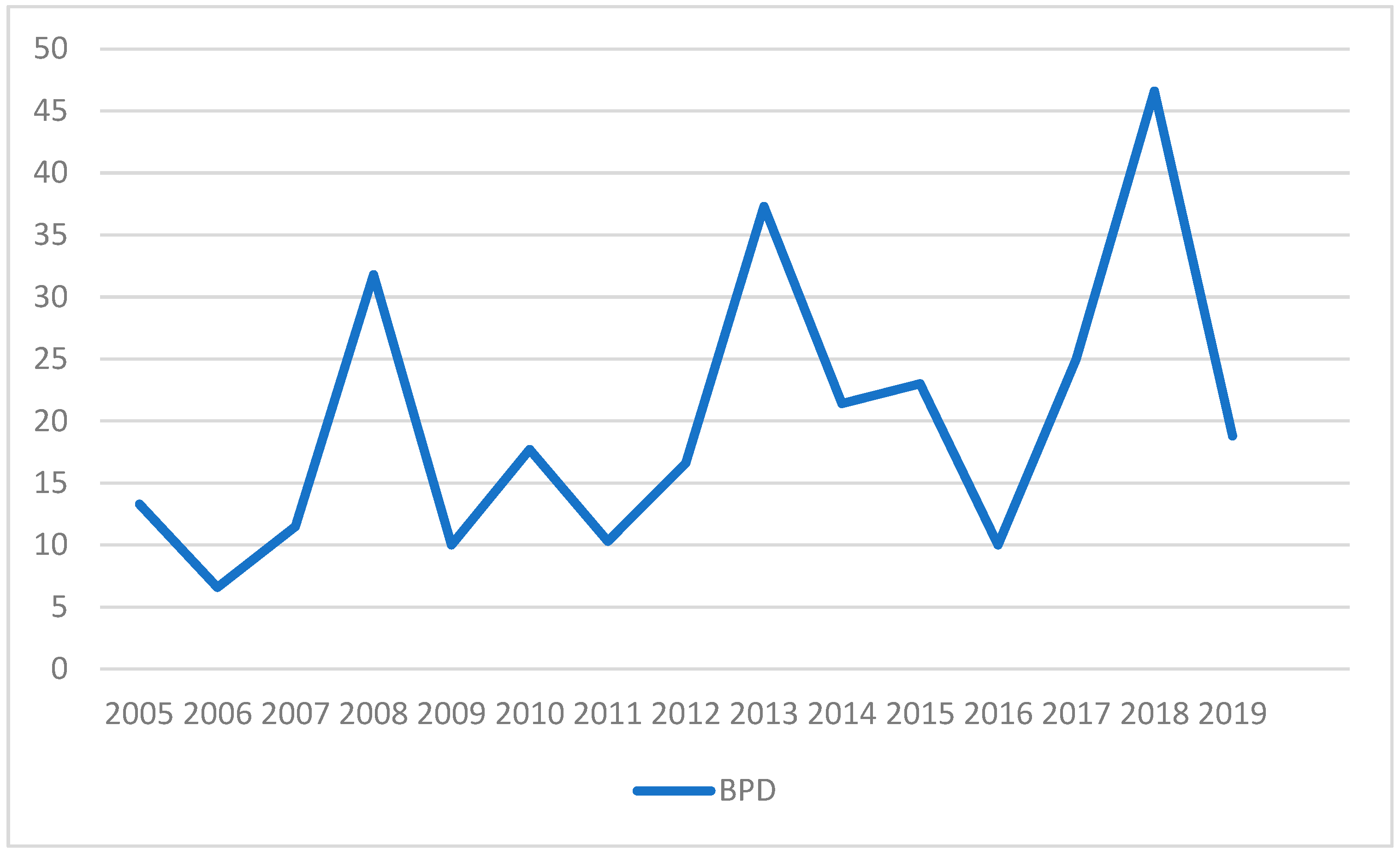
4.4. BPD
4.5. MOM Feeding
5. Conclusions
6. Strengths and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NICU | Neonatal Intensive Care Units |
| VLBW | Very Low Birth Weight Infants |
| RCT | Randomized Controlled Trials |
| NEC | Necrotizing Enterocolitis |
| LOS | Late-Onset Sepsis |
| ROP | Retinopathy Of Prematurity |
| BPD | Bronchopulmonary Dysplasia |
| MOM | Mother’s Own Milk |
| HM | Human Milk |
| DHM | Donor Human Milk |
| PF | Preterm Formula |
| VON | Vermont Oxford Network |
References
- Eidelman, A.I.; Schanler, R.J.; Johnston, M.; Landers, S.; Noble, L.; Szucs, K. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Tonkin, E.; Damarell, R.A.; McPhee, A.J.; Suganuma, M.; Suganuma, H.; Middleton, P.F.; Makrides, M.; Collins, C.T. A Systematic Review and Meta-Analysis of Human Milk Feeding and Morbidity in Very Low Birth Weight Infants. Nutrients 2018, 10, 707. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Parker, M.G.; Stellwagen, L.M.; Noble, L.; Kim, J.H.; Poindexter, B.B.; Puopolo, K.M.; Section on Breastfeeding, Committee on Nutrition, Committee on Fetus and Newborn. Promoting Human Milk and Breastfeeding for the Very Low Birth Weight Infant. Pediatrics 2021, 148, e2021054272. [Google Scholar] [CrossRef] [PubMed]
- United Nations International Children’s Emergency Fund/World Health Organization (UNICEF/WHO). Protecting, Promoting and Supporting Breastfeeding: The Baby-Friendly Hospital Initiative for Small, Sick and Preterm Newborns; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Hair, A.B.; Peluso, A.M.; Hawthorne, K.M.; Perez, J.; Smith, D.P.; Khan, J.Y.; O’Donnell, A.; Powers, R.J.; Lee, M.L.; Abrams, S.A. Beyond Necrotizing Enterocolitis Prevention: Improving Outcomes with an Exclusive Human Milk-Based Diet. Breastfeed. Med. 2016, 11, 70–74. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, B.; Xiu, W.; Dai, Y.; Yang, C. Protective effects of different doses of human milk on neonatal necrotizing enterocolitis. Medicine 2020, 99, e22166. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Patel, A.L.; Johnson, T.J.; Engstrom, J.L.; Fogg, L.F.; Jegier, B.J.; Bigger, H.R.; Meier, P.P. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J. Perinatol. 2013, 33, 514–519. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhou, J.; Shukla, V.V.; John, D.; Chen, C. Human Milk Feeding as a Protective Factor for Retinopathy of Prematurity: A Meta-analysis. Pediatrics 2015, 136, e1576–e1586. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, P.; Stolfi, I.; Pedicino, R.; Vagnarelli, F.; Mosca, F.; Pugni, L.; Bollani, L.; Pozzi, M.; Gomez, K.; Tzialla, C.; et al. Human milk feeding prevents retinopathy of prematurity (ROP) in preterm VLBW neonates. Early Hum. Dev. 2013, 89 (Suppl. 1), S64–S68. [Google Scholar] [CrossRef] [PubMed]
- Ginovart, G.; Gich, I.; Verd, S. Human milk feeding protects very low-birth-weight infants from retinopathy of prematurity: A pre-post cohort analysis. J. Matern. Fetal Neonatal Med. 2016, 29, 3790–3795. [Google Scholar] [CrossRef] [PubMed]
- Spiegler, J.; Preuß, M.; Gebauer, C.; Bendiks, M.; Herting, E.; Göpel, W.; German Neonatal Network (GNN); German Neonatal Network GNN. Does Breastmilk Influence the Development of Bronchopulmonary Dysplasia? J. Pediatr. 2016, 169, 76–80.e4. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Zhang, L.; Tang, J.; Shi, J.; Qu, Y.; Xiong, T.; Mu, D. Human milk as a protective factor for bronchopulmonary dysplasia: A systematic review and meta-analysis. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 104, F128–F136. [Google Scholar] [CrossRef]
- Villamor-Martínez, E.; Pierro, M.; Cavallaro, G.; Mosca, F.; Villamor, E. Mother’s own milk and bronchopulmonary dysplasia: A systematic review and meta-analysis. Front. Pediatr. 2019, 7, 224. [Google Scholar] [CrossRef]
- Anderson, J.W.; Johnstone, B.M.; Remley, D.T. Breast-feeding and cognitive development: A meta-analysis. Am. J. Clin. Nutr. 1999, 70, 525–535. [Google Scholar] [CrossRef] [PubMed]
- Vohr, B.R.; Poindexter, B.B.; Dusick, A.M.; McKinley, L.T.; Wright, L.L.; Langer, J.C.; Poole, W.K.; NICHD Neonatal Research Network. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics 2006, 118, e115–e123. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Shin, J.; McGee, M.; Unger, S.; Bando, N.; Sato, J.; Vandewouw, M.; Patel, Y.; Branson, H.M.; Paus, T.; et al. Intake of mother’s milk by very-low-birth-weight infants and variation in DNA methylation of genes involved in neurodevelopment at 5.5 years of age. Am. J. Clin. Nutr. 2022, 116, 1038–1048. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- World Health Organization/United Nations International Children’s Emergency Fund (WHO/UNICEF). Global Strategy for Infant and Young Child Feeding; WHO: Geneva, Switzerland, 2003. [Google Scholar]
- Picaud, J.C. Review highlights the importance of donor human milk being available for very low birth weight infants. Acta Paediatr. 2022, 111, 1127–1133. [Google Scholar] [CrossRef]
- Anand, R.J.; Leaphart, C.L.; Mollen, K.P.; Hackam, D.J. The role of the intestinal barrier in the pathogenesis of necrotizing enterocolitis. Shock 2007, 27, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Neu, J.; Walker, W.A. Necrotizing enterocolitis. N. Engl. J. Med. 2011, 364, 255–264. [Google Scholar] [CrossRef]
- Halpern, M.D.; Denning, P.W. The role of intestinal epithelial barrier function in the development of NEC. Tissue Barriers 2015, 3, e1000707. [Google Scholar] [CrossRef]
- Taylor, S.N.; Basile, L.A.; Ebeling, M.; Wagner, C.L. Intestinal permeability in preterm infants by feeding type: Mother’s milk versus formula. Breastfeed. Med. 2009, 4, 11–15. [Google Scholar] [CrossRef]
- Abrams, S.A.; Schanler, R.J.; Lee, M.L.; Rechtman, D.J. Greater mortality and morbidity in extremely preterm infants fed a diet containing cow milk protein products. Breastfeed. Med. 2014, 9, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Arslanoglu, S.; Corpeleijn, W.; Moro, G.; Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Domellöf, M.; Fewtrell, M.; Hojsak, I.; et al. Donor human milk for preterm infants: Current evidence and research directions. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 535–542. [Google Scholar] [PubMed]
- Perrin, M.T.; Belfort, M.B.; Hagadorn, J.I.; McGrath, J.M.; Taylor, S.N.; Tosi, L.M.; Brownell, E.A. The Nutritional Composition and Energy Content of Donor Human Milk: A Systematic Review. Adv. Nutr. 2020, 11, 960–970. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Quigley, M.; Embleton, N.D.; McGuire, W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst. Rev. 2019, 7, CD002971. [Google Scholar]
- Yang, R.; Chen, D.; Deng, Q.; Xu, X. The effect of donor human milk on the length of hospital stay in very low birthweight infants: A systematic review and meta-analysis. Int. Breastfeed. J. 2020, 15, 89. [Google Scholar] [CrossRef]
- Li, Y.; Chi, C.; Li, C.; Song, J.; Song, Z.; Wang, W.; Sun, J. Efficacy of Donated Milk in Early Nutrition of Preterm Infants: A Meta-Analysis. Nutrients 2022, 14, 1724. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cristofalo, E.A.; Schanler, R.J.; Blanco, C.L.; Sullivan, S.; Trawoeger, R.; Kiechl-Kohlendorfer, U.; Dudell, G.; Rechtman, D.J.; Lee, M.L.; Lucas, A.; et al. Randomized Trial of Exclusive Human Milk versus Preterm Formula Diets in Extremely Premature Infants. J. Pediatr. 2013, 163, 1592–1595. [Google Scholar]
- O’Connor, D.L.; Gibbins, S.; Kiss, A.; Bando, N.; Brennan-Donnan, J.; Ng, E.; Campbell, D.M.; Vaz, S.; Fusch, C.; Asztalos, E.; et al. Effect of Supplemental Donor Human Milk Compared With Preterm Formula on Neurodevelopment of Very Low-Birth-Weight Infants at 18 Months: A Randomized Clinical Trial. JAMA 2016, 316, 1897–1905. [Google Scholar] [CrossRef] [PubMed]
- Assad, M.; Elliott, M.J.; Abraham, J.H. Decreased cost and improved feeding villamor in VLBW infants fed an exclusive human milk diet. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2016, 36, 216–220. [Google Scholar]
- Trang, S.; Zupancic, J.A.; Unger, S.; Kiss, A.; Bando, N.; Wong, S.; Gibbins, S.; O’Connor, D.L.; GTA DoMINO Feeding Group. Cost-Effectiveness of Supplemental Donor Milk Versus Formula for Very Low Birth Weight Infants. Pediatrics 2018, 141, e20170737. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.J.; Berenz, A.; Wicks, J.; Esquerra-Zwiers, A.; Sulo, K.S.; Gross, M.E.; Szotek, J.; Meier, P.; Patel, A.L. The Economic Impact of Donor Milk in the Neonatal Intensive Care Unit. J. Pediatr. 2020, 224, 57–65.e4. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Silano, M.; Milani, G.P.; Fattore, G.; Agostoni, C. Donor human milk and risk of surgical necrotizing enterocolitis: A meta-analysis. Clin. Nutr. 2019, 38, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Garg, P.M.; Paschal, J.L.; Ansari, A.Y.; Block, D.; Inagaki, K.; Weitkamp, J.H. Clinical impact of NEC-associated sepsis on outcomes in preterm infants. Pediatr. Res. 2022, 92, 1705–1715. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Campos-Martinez, A.M.; Expósito-Herrera, J.; Gonzalez-Bolívar, M.; Fernández-Marin, E.; Uberos, J. Evaluation of Risk and Preventive Factors for Necrotizing Enterocolitis in Premature Newborns. A Systematic Review of the Literature. Front. Pediatr. 2022, 10, 874976. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Battersby, C.; Santhalingam, T.; Costeloe, K.; Modi, N. Incidence of Neonatal Necrotising Enterocolitis in High-Income Countries: A Systematic Review. Arch. Dis. Child. Fetal Neonatal Ed. 2018, 103, F182–F189. [Google Scholar]
- Analisi sulla Enterocolite Necrotizzante. Anni 2007–2013. Dati UTIN On-Line Regione Lazio—SIN 2015. Available online: https://www.regione.lazio.it/sites/default/files/2021-04/Enterocolite-Necrotizzante-Dati-UTIN-Anni-2007-2013%20.pdf (accessed on 25 February 2025).
- Società Italiana di Neonatologia. Italian Neonatal Network—INNSIN. Rapporto Anno 2021. Available online: https://www.sin-neonatologia.it/wp-content/uploads/2022/11/REPORT_INNSIN-2021_2020_2019.pdf (accessed on 25 February 2025).
- Singh, D.K.; Miller, C.M.; Orgel, K.A.; Dave, M.; Mackay, S.; Good, M. Necrotizing enterocolitis: Bench to bedside approaches and advancing our understanding of disease pathogenesis. Front. Pediatr. 2022, 10, 1107404. [Google Scholar] [CrossRef]
- Fredriksson, F.; Engstrand Lilja, H. Survival rates for surgically treated necrotising enterocolitis have improved over the last four decades. Acta Paediatr. 2019, 108, 1603–1608. [Google Scholar] [CrossRef]
- Jones, I.H.; Hall, N.J. Contemporary Outcomes for Infants with Necrotizing Enterocolitis-A Systematic Review. J. Pediatr. 2020, 220, 86–92.e3. [Google Scholar] [CrossRef] [PubMed]
- Good, M.; Sodhi, C.P.; Egan, C.E.; Afrazi, A.; Jia, H.; Yamaguchi, Y.; Lu, P.; Branca, M.F.; Ma, C.; Prindle, T.; et al. Breast milk protects against the development of necrotizing enterocolitis through inhibition of toll-like receptor 4 in the intestinal epithelium via activation of the epidermal growth factor receptor. Mucosal Immunol. 2015, 8, 1166–1179. [Google Scholar] [CrossRef]
- Chowning, R.; Radmacher, P.; Lewis, S.; Serke, L.; Pettit, N.; Adamkin, D.H. Aretrospective analysis of the effect of human milk on prevention of necrotizing enterocolitis and postnatal growth. J. Perinatol. 2016, 36, 221–224. [Google Scholar] [CrossRef]
- Nolan, L.S.; Parks, O.B.; Good, M. A Review of the Immunomodulating Components of Maternal Breast Milk and Protection Against Necrotizing Enterocolitis. Nutrients 2019, 12, 14. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zivkovic, A.M.; German, J.B.; Lebrilla, C.B.; Mills, D.A. Human milk glycobiome and its impact on the infant gastrointestinal microbiota. Proc. Natl. Acad. Sci. USA 2011, 108 (Suppl. 1), 4653–4658. [Google Scholar] [CrossRef] [PubMed]
- Laursen, M.F.; Pekmez, C.T.; Larsson, M.W.; Lind, M.V.; Yonemitsu, C.; Larnkjær, A.; Mølgaard, C.; Bode, L.; Dragsted, L.O.; Michaelsen, K.F.; et al. Maternal milk microbiota and oligosaccharides contribute to the infant gut microbiota assembly. ISME Commun. 2021, 1, 21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Walsh, C.; Lane, J.A.; van Sinderen, D.; Hickey, R.M. Human milk oligosaccharides: Shaping the infant gut microbiota and supporting health. J. Funct. Foods 2020, 72, 104074. [Google Scholar] [CrossRef]
- Quitadamo, P.A.; Palumbo, G.; Villani, A.; Savastano, M.; Ravidà, D.; Bisceglia, M.; Gentile, A.; Cristalli, P. Does the Opening of a Milk Bank in NICU Cancel the Incidence of NEC? J. Pediatr. Disord. Neonatal Care (JPDNC) 2018, 1, 104. [Google Scholar]
- Altobelli, E.; Angeletti, P.M.; Verrotti, A.; Petrocelli, R. The Impact of Human Milk on Necrotizing Enterocolitis: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 1322. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meier, P.P.; Engstrom, J.L.; Patel, A.L.; Jegier, B.J.; Bruns, N.E. Improving the use of human milk during and after the NICU stay. Clin. Perinatol. 2010, 37, 217–245. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Underwood, M.A. Human milk for the premature infant. Pediatr. Clin. N. Am. 2013, 60, 189–207. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hanford, J.; Mannebach, K.; Ohler, A.; Patten, M.; Pardalos, J. Rates of Comorbidities in Very Low Birth Weight Infants Fed an Exclusive Human Milk Diet Versus a Bovine Supplemented Diet. Breastfeed. Med. 2021, 16, 814–820. [Google Scholar] [CrossRef]
- Wang, M.; Gong, X.; Yu, L.; Song, F.; Li, D.; Fan, Q.; Zhang, T.; Yan, X. Early enteral nutrition with exclusive donor milk instead of formula milk affects the time of full enteral feeding for very low birth weight infants. Front. Nutr. 2024, 11, 1345768. [Google Scholar] [CrossRef]
- Lu, X.; Gao, Y.; Liu, C.; Pan, M.; Chen, X. Effect of Breast Milk on the Frequency of Bronchopulmonary Dysplasia in Very Low Birth Weight Premature Infants: A Meta-analysis. Breastfeed. Med. 2023, 18, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Moliner-Calderón, E.; Verd, S.; Leiva, A.; Ginovart, G.; Moll-McCarthy, P.; Figueras-Aloy, J. The role of human milk feeds on inotrope use in newborn infants with sepsis. Front. Pediatr. 2023, 11, 1172799. [Google Scholar] [CrossRef]
- Quitadamo, P.A.; Zambianco, F.; Palumbo, G.; Copetti, M.; Gentile, M.A.; Mondelli, A. Trend and Predictors of Breastmilk Feeding among Very-Low-Birth-Weight Infants in NICU and at Discharge. Nutrients 2023, 15, 3314. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Quitadamo, P.A.; Zambianco, F.; Palumbo, G.; Wagner, X.; Gentile, M.A.; Mondelli, A. Monitoring the Use of Human Milk, the Ideal Food for Very Low-Birth-Weight Infants-A Narrative Review. Foods 2024, 13, 649. [Google Scholar] [CrossRef]
- Rodrigues, C.; Severo, M.; Zeitlin, J.; Barros, H.; Portuguese EPICE (Effective Perinatal Intensive Care in Europe) Network. The Type of Feeding at Discharge of Very Preterm Infants: Neonatal Intensive Care Units Policies and Practices Make a Difference. Breastfeed. Med. 2018, 13, 50–59. [Google Scholar] [CrossRef]
- Dong, D.; Ru, X.; Huang, X.; Sang, T.; Li, S.; Wang, Y.; Feng, Q. A prospective cohort study on lactation status and breastfeeding challenges in mothers giving birth to preterm infants. Int. Breastfeed. J. 2022, 17, 6. [Google Scholar] [CrossRef]
- Boundy, E.O.; Perrine, C.G.; Nelson, J.M.; Hamner, H.C. Disparities in Hospital-Reported Breast Milk Use in Neonatal Intensive Care Units—United States, 2015. MMWR Morb. Mortal Wkly. Rep. 2017, 66, 1313–1317. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kalluri, N.S.; Burnham, L.A.; Lopera, A.M.; Stickney, D.M.; Combs, G.L.; Levesque, B.M.; Philipp, B.L.; Parker, M.G. A Quality Improvement Project to Increase Mother’s Milk Use in an Inner-City NICU. Pediatr. Qual. Saf. 2019, 4, e204. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dharel, D.; Singhal, N.; Wood, C.; Cieslak, Z.; Bacchini, F.; Shah, P.S.; Ye, X.Y.; Alshaikh, B.; Canadian Neonatal Network (CNN) and Canadian Preterm Birth Network (CPTBN) Investigators. Rates and Determinants of Mother’s Own Milk Feeding in Infants Born Very Preterm. J. Pediatr. 2021, 236, 21–27.e4. [Google Scholar] [CrossRef] [PubMed]
- Israel-Ballard, K.; LaRose, E.; Mansen, K. The global status of human milk banking. Matern. Child. Nutr. 2024, 20 (Suppl. S4), e13592. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on Optimal Feeding of Low Birth-Weight Infants in Low- and Middle-Income Countries; WHO Press: Geneva, Switzerland, 2011. [Google Scholar]
- World Health Organization. Donor Human Milk for Low-Birth-Weight Infants. 2019. Available online: https://www.who.int/tools/elena/interventions/donormilk-infants (accessed on 9 August 2023).
- Hepner, W.R., Jr.; Krause, A.C. Retrolental fibroplasia: Clinical observations. Pediatrics 1952, 10, 433–443. [Google Scholar] [PubMed]
- Lucas, A.; Gore, S.M.; Cole, T.J.; Bamford, M.F.; Dossetor, J.F.; Barr, I.; Dicarlo, L.; Cork, S.; Lucas, P.J. Multicentre trial on feeding low birthweight infants: Effects of diet on early growth. Arch. Dis. Child. 1984, 59, 722–730. [Google Scholar] [PubMed]
- Isaacs, E.B.; Fischl, B.R.; Quinn, B.T.; Chong, W.K.; Gadian, D.G.; Lucas, A. Impact of breast milk on intelligence quotient, brain size, and white matter development. Pediatr. Res. 2010, 67, 357–362. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miracle, D.J.; Meier, P.P.; Bennett, P.A. Mothers’ decisions to change from formula to mothers’ milk for very-low-birth-weight infants. J. Obstet. Gynecol. Neonatal Nurs. 2004, 33, 692–703. [Google Scholar] [CrossRef] [PubMed]
- Meier, P.P.; Johnson, T.J.; Patel, A.L.; Rossman, B. Evidence-Based Methods That Promote Human Milk Feeding of Preterm Infants: An Expert Review. Clin. Perinatol. 2017, 44, 1–22. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- O’Connor, D.L.; Kiss, A.; Tomlinson, C.; Bando, N.; Bayliss, A.; Campbell, D.M.; Daneman, A.; Francis, J.; Kotsopoulos, K.; Shah, P.S.; et al. Nutrient enrichment of human milk with human and bovine milk-based fortifiers for infants born weighing <1250 g: A randomized clinical trial. Am. J. Clin. Nutr. 2018, 108, 108–116. [Google Scholar] [CrossRef]
- Quigley, M.; Embleton, N.D.; Meader, N.; McGuire, W. Donor human milk for preventing necrotising enterocolitis in very preterm or very low-birthweight infants. Cochrane Database Syst. Rev. 2024, 9, CD002971. [Google Scholar] [CrossRef]
- Swanson, J.R.; Becker, A.; Fox, J.; Horgan, M.; Moores, R.; Pardalos, J.; Pinheiro, J.; Stewart, D.; Tonya Robinson, T. Implementing an exclusive human milk diet for preterm infants: Real-world experience in diverse NICUs. BMC Pediatr. 2023, 23, 237. [Google Scholar] [CrossRef]
- Yee, W.H.; Soraisham, A.S.; Shah, V.S.; Aziz, K.; Yoon, W.; Lee, S.K.; Canadian Neonatal Network. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics 2012, 129, e298–e304. [Google Scholar] [CrossRef] [PubMed]
- Fitzgibbons, S.C.; Ching, Y.; Yu, D.; Carpenter, J.; Kenny, M.; Weldon, C.; Lillehei, C.; Valim, C.; Horbar, J.D.; Jaksic, T. Mortality of necrotizing enterocolitis expressed by birth weight categories. J. Pediatr. Surg. 2009, 44, 1072–1075. [Google Scholar]
- Huston, R.K.; Markell, A.M.; McCulley, E.A.; Pathak, M.; Rogers, S.P.; Sweeney, S.L.; Dolphin, N.G.; Gardiner, S.K. Decreasing necrotizing enterocolitis and gastrointestinal bleeding in the neonatal intensive care unit: The role of donor human milk and exclusive human milk diets in infants _1500 g birth weight. Infant Child Adolesc. Nutr. 2014, 6, 86–93. [Google Scholar]
- Hair, A.B.; Rechtman, D.J.; Lee, M.L.; Niklas, V. Beyond necrotizing enterocolitis: Other clinical advantages of an exclusive human milk diet. Breastfeed. Med. 2018, 13, 408–411. [Google Scholar] [PubMed]
- Hylander, M.A.; Strobino, D.M.; Pezzullo, J.C.; Dhanireddy, R. Association of human milk feedings with a reduction in retinopathy of prematurity among very low birthweight infants. J. Perinatol. 2001, 21, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Green, B.F.; Pezzullo, J.C.; Bharwani, S.S.; Dhanireddy, R. Systematic review and meta-analysis of human milk intake and retinopathy of prematurity: A significant update. J. Perinatol. 2016, 36, 913–920. [Google Scholar] [CrossRef]
- Heller, C.D.; O’Shea, M.; Yao, Q.; Langer, J.; Ehrenkranz, R.A.; Phelps, D.L.; Poole, W.K.; Stoll, B.; Duara, S.; Oh, W.; et al. Human milk intake and retinopathy of prematurity in extremely low birth weight infants. Pediatrics 2007, 120, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Shirai, M.; Kokubo, M.; Takahashi, S.; Kajino, M.; Sakata, H.; Oki, J. Human milk reduces the risk of retinal detachment in extremely low-birthweight infants. Pediatr. Int. 2007, 49, 894–897. [Google Scholar] [CrossRef]
- Porcelli, P.J.; Weaver, R.G., Jr. The influence of early postnatal nutrition on retinopathy of prematurity in extremely low birth weight infants. Early Hum. Dev. 2010, 86, 391–396. [Google Scholar] [CrossRef]
- Fang, J.L.; Sorita, A.; Carey, W.A.; Colby, C.E.; Murad, H.M.; Alahdab, F. Interventions to prevent retinopathy of prematurity: A meta-analysis. Pediatrics 2016, 137, e20153387. [Google Scholar]
- de Silva, A.; Jones, P.W.; Spencer, S.A. Does human milk reduce infection rates in preterm infants? A systematic review. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, F509–F513. [Google Scholar] [CrossRef]
- Furman, L. Yes, human milk does reduce infection rates in very low birthweight infants. Arch. Dis. Child. Fetal Neonatal Ed. 2006, 91, F78. [Google Scholar] [PubMed] [PubMed Central]
- Corpeleijn, W.E.; de Waard, M.; Christmann, V.; van Goudoever, J.B.; Jansen-van der Weide, M.C.; Kooi, E.M.; Koper, J.F.; Kouwenhoven, S.M.; Lafeber, H.N.; Mank, E.; et al. Effect of Donor Milk on Severe Infections and Mortality in Very Low-Birth-Weight Infants: The Early Nutrition Study Randomized Clinical Trial. JAMA Pediatr. 2016, 170, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Kotha, R.; Konda, K.C.; Pandala, P.; Maddireddi, A. Effect of human milk enriched with human milk-based fortifier (HMBF) versus bovine milk-based fortifier (BMBF) on growth and morbidity among very low birth weight (VLBW) infants—A randomized controlled trial. J. Pediatr. Neonat. Individ. Med. 2022, 11, e110104. [Google Scholar] [CrossRef]
- Coyne, R.; Hughes, W.; Purtill, H.; McGrath, D.; Dunne, C.P.; Philip, R.K. Influence of an Early Human Milk Diet on the Duration of Parenteral Nutrition and Incidence of Late-Onset Sepsis in Very Low Birthweight (VLBW) Infants: A Systematic Review. Breastfeed. Med. 2024, 19, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Verd, S.; Porta, R.; Ginovart, G.; Avila-Alvarez, A.; García-Muñoz Rodrigo, F.; Izquierdo Renau, M.; Ventura, P.S. Human Milk Feeding Is Associated with Decreased Incidence of Moderate-Severe Bronchopulmonary Dysplasia in Extremely Preterm Infants. Children 2023, 10, 1267. [Google Scholar] [CrossRef]
- Thiess, T.; Lauer, T.; Woesler, A.; Neusius, J.; Stehle, S.; Zimmer, K.P.; Eckert, G.P.; Ehrhardt, H. Correlation of Early Nutritional Supply and Development of Bronchopulmonary Dysplasia in Preterm Infants <1000 g. Front. Pediatr. 2021, 9, 741365. [Google Scholar] [CrossRef]
- Morag, I.; Barkai, E.; Wazana, Y.; Elizur, A.; Levkovitz Stern, O.; Staretz-Chacham, O.; Pinchevski-Kadir, S.; Ofek Shlomai, N. Predictors of Developmental and Respiratory Outcomes Among Preterm Infants With Bronchopulmonary Dysplasia. Front. Pediatr. 2021, 9, 780518. [Google Scholar] [CrossRef]
- Martin, R.J.; Jobe, A.H.; Bancalari, E. What is BPD today and in the next 50 years? Am. J. Physiol. Lung Cell Mol. Physiol. 2021, 321, L974–L977. [Google Scholar] [CrossRef]
- Sindelar, R.; Shepherd, E.G.; Ågren, J.; Panitch, H.B.; Abman, S.H.; Nelin, L.D.; Bronchopulmonary Dysplasia Collaborative. Established severe BPD: Is there a way out? Change of ventilatory paradigms. Pediatr. Res. 2021, 90, 1139–1146. [Google Scholar] [CrossRef]
- Jensen, E.A.; Dysart, K.C.; Gantz, M.G.; Carper, B.; Higgins, R.D.; Keszler, M.; Laughon, M.M.; Poindexter, B.B.; Stoll, B.J.; Walsh, M.C.; et al. Association between Use of Prophylactic Indomethacin and the Risk for Bronchopulmonary Dysplasia in Extremely Preterm Infants. J. Pediatr. 2017, 186, 34–40.e2. [Google Scholar] [CrossRef]
- Starr, M.C.; Griffin, R.; Gist, K.M.; Segar, J.L.; Raina, R.; Guillet, R.; Nesargi, S.; Menon, S.; Anderson, N.; Askenazi, D.J. Neonatal Kidney Collaborative Research Committee. Association of Fluid Balance with Short- and Long-term Respiratory Outcomes in Extremely Premature Neonates. A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2248826. [Google Scholar]
- Schmidt, B.; Roberts, R.S.; Davis, P.; Doyle, L.W.; Barrington, K.J.; Ohlsson, A.; Solimano, A.; Tin, W.; Caffeine for Apnea of Prematurity Trial Group. Caffeine therapy for apnea of prematurity. N. Engl. J. Med. 2006, 354, 2112–2121. [Google Scholar] [CrossRef] [PubMed]
- Doyle, L.W.; Cheong, J.L.; Hay, S.; Manley, B.J.; Halliday, H.L. Late (≥7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst. Rev. 2021, 11, CD001145. [Google Scholar] [PubMed]
- Principi, N.; Di Pietro, G.M.; Esposito, S. Bronchopulmonary dysplasia: Clinical aspects and preventive and therapeutic strategies. J. Transl. Med. 2018, 16, 36. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Walsh, M.C.; Carlo, W.A.; Shankaran, S.; Laptook, A.R.; Sánchez, P.J.; Van Meurs, K.P.; Wyckoff, M.; et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993–2012. JAMA 2015, 314, 1039–1051. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jensen, E.A.; Edwards, E.M.; Greenberg, L.T.; Soll, R.F.; Ehret, D.E.; Horbar, J.D. Severity of Bronchopulmonary Dysplasia Among Very Preterm Infants in the United States. Pediatrics 2021, 148, e2020030007. [Google Scholar] [CrossRef]
- Giannì, M.L.; Roggero, P.; Colnaghi, M.R.; Piemontese, P.; Amato, O.; Orsi, A.; Morlacchi, L.; Mosca, F. The role of nutrition in promoting growth in pre-term infants with bronchopulmonary dysplasia: A prospective non-randomised interventional cohort study. BMC Pediatr. 2014, 14, 235. [Google Scholar] [CrossRef]
- Merino-Hernández, A.; Palacios-Bermejo, A.; Ramos-Navarro, C.; Caballero-Martín, S.; González-Pacheco, N.; Rodríguez-Corrales, E.; Sánchez-Gómez de Orgaz, M.C.; Sánchez-Luna, M. Effect of Donated Premature Milk in the Prevention of Bronchopulmonary Dysplasia. Nutrients 2024, 16, 859. [Google Scholar] [CrossRef]
- Yang, J.; Li, J.; Wang, H.; Chen, X.; Yang, C.; ChaoMu, L.; Cao, A.; Xiong, X. Human milk and bronchopulmonary dysplasia have a dose-dependent effect: A cohort study. BMJ Paediatr. Open 2025, 9, e002727. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhu, Z.; Yuan, L.; Wang, J.; Li, Q.; Yang, C.; Gao, X.; Chen, S.; Han, S.; Liu, J.; Wu, H.; et al. Mortality and Morbidity of Infants Born Extremely Preterm at Tertiary Medical Centers in China From 2010 to 2019. JAMA Netw. Open 2021, 4, e219382. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Petrova, A.; Eccles, S.; Mehta, R. Role of the Proportional Intake of Fortified Mother’s Own Milk in the Weight Gain Pattern of Their Very-Preterm-Born Infants. Nutrients 2020, 12, 1571. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lund, A.M.; Domellöf, M.; Pivodic, A.; Hellström, A.; Stoltz Sjöström, E.; Hansen-Pupp, I. Mother’s Own Milk and Its Relationship to Growth and Morbidity in a Population-based Cohort of Extremely Preterm Infants. J. Pediatr. Gastroenterol. Nutr. 2022, 74, 292–300. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- El-Fadeel, H.; Velumula, P.; Lulic-Botica, M.; Natarajan, G.; Thomas, R.; Botica, G.; Bajaj, M. Effect of an exclusive human milk diet on feeding tolerance in preterm infants. J. Perinatol. 2022, 42, 1070–1075. [Google Scholar] [CrossRef] [PubMed]


| Variable | ||
|---|---|---|
| N: 337 | Gestazional age, weeks {M(SD)} | 27.9 (2.51) |
| Birth weight, g {Median (SD)} | 1040 (266) | |
| Female {n (%)} | 172 (51) | |
| Multiple gestation {n (%)} | 118 (35) | |
| Type of delivery {n (%)} | ||
| - Vaginal delivery | 77 (22.8) | |
| - C-section | 123 (36.5) | |
| - Emergency C-section | 137 (40.7) | |
| Neonatal resuscitation {n (%)} | 313 (92.9) | |
| - ET | 163 (51.7) | |
| - Neopuff | 147 (46.7) | |
| - Other | 3 (0.9) | |
| Apgar 1′ {M(SD)} | 5 (1) | |
| Apgar 5′ {M(SD)} | 7 (1) | |
| Feeding {n (%)} | ||
| - Esclusive Human Milk | 182 (54.2) | |
| - Mixed Milk | 40 (11.9) | |
| - Preterm Formula | 112 (33.3) | |
| - No feeding | 3 (0.6) | |
| Mechanical ventilation hours {M(SD)} | ||
| - SIPPV/SIMV | 232 (360) | |
| - nIMV | 251 (346) | |
| - nCPAP | 299 (314) | |
| Any neonatal complication {n (%)} | ||
| - NEC | 14 (4.2) | |
| - BPD | 86 (25.5) | |
| - ROP | 82 (24.3) | |
| - LOS | 19 (5.6) |
| Subgroup | Sample n | Severe BPD n (%) | Severe ROP n (%) | Surgical NEC n (%) | LOS n (%) |
|---|---|---|---|---|---|
| MOM | 51 | 9 (17.6) | 2 (3.9) | 0 (0) | 4 (7.8) |
| PF | 110 | 20 (18.2) | 5 (4.5) | 11 (10) | 11 (10) |
| DHM | 75 | 16 (21.3%) | 0 (0) | 1 (1.3%) | 3 (4%) |
| HM escl. | 182 | 22 (12) | 5 (2.74) | 1 (0.5) | 3 (4) |
| Any MOM | 37 | 3 (8.1) | 2 (5.4) | 0 (0) | 1 (2.7) |
| Any HM | 40 | 5 (12.5) | 2 (5) | 0 (0) | 2 (5) |
| No Feeding | 3 | 2 |
| NNT Value | ||||
|---|---|---|---|---|
| NEC | LOS | Severe ROP | Severe BPD | |
| MOM vs. PF | 10 | 45 | 166 | 166 |
| DHM vs. PF | 11 | 26 | 22 | / |
| HM escl. vs. PF | 10 | 26 | 55 | 16 |
| Any MOM vs. PF | 10 | 13 | / | 9 |
| Any HM vs. PF | 10 | 20 | / | 17 |
| Spearman’s Rho | Type of Feeding (No Feeding/DHM + MOM/PF + MOM/ MOM/PF/DHM/MOM + PF/MOM + DHM/DHM + PF) | Feeding Class Human Milk/Mixed Milk/Formula Milk | |
|---|---|---|---|
| NEC | Correlation coefficient | 0.180 *** | 0.141 ** |
| p value | <0.001 | 0.010 | |
| LOS | Correlation coefficient | −0.110 * | |
| p value | Ns | 0.044 | |
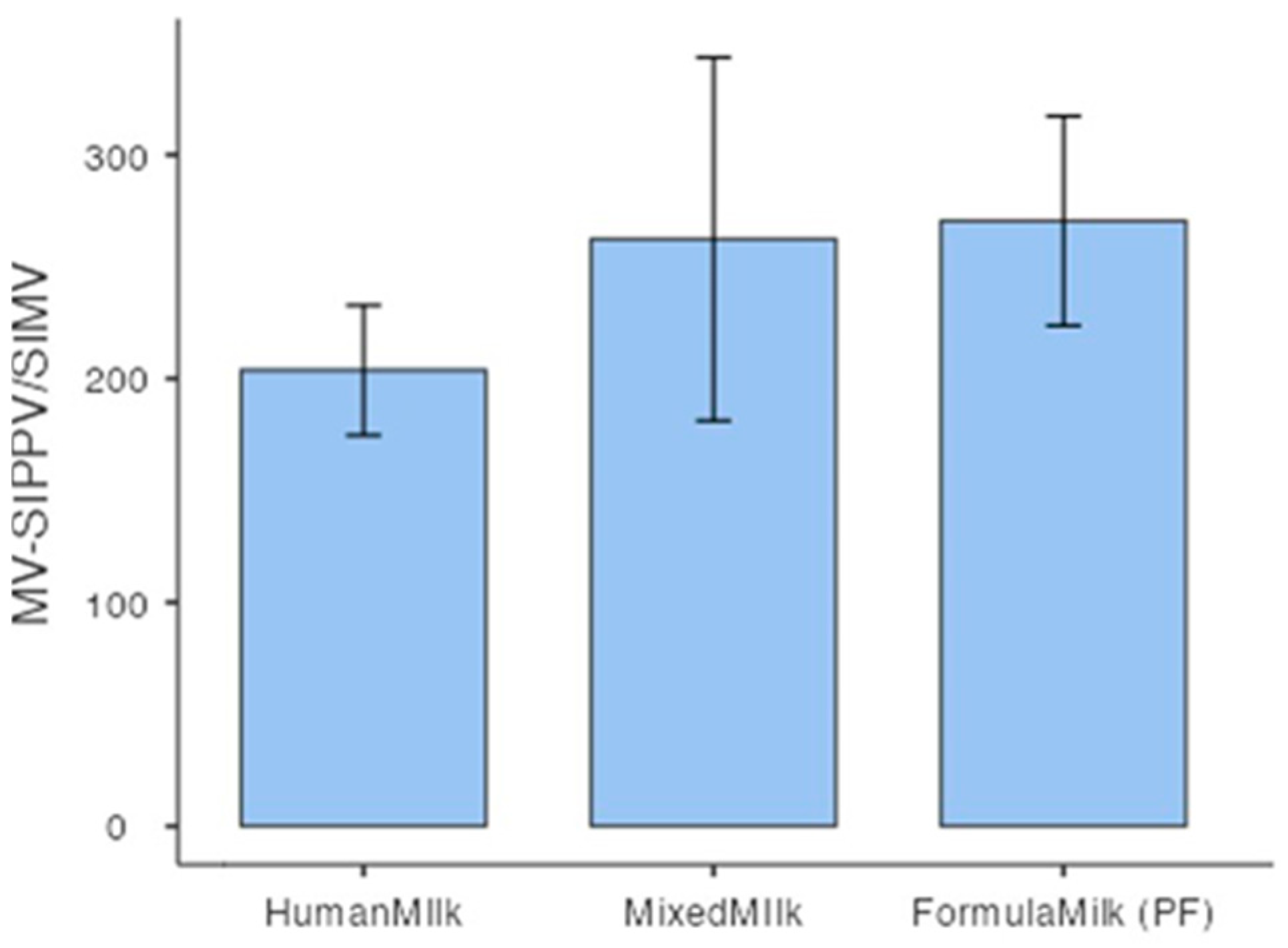
| MV—SIPPV/SIMV | Correlation coefficient | 0.173 ** | |
| p value | Ns | 0.009 | |
| Spearman’s Rho | Type of Feeding (No Feeding/DHM + MOM/PF + MOM/ MOM/PF/DHM/MOM + PF/MOM + DHM/DHM + PF) | Feeding Classis Human Milk/Mixed Milk/Formula Milk | |
|---|---|---|---|
| NEC | Correlation coefficient | 0.186 *** | 0.149 ** |
| p value | <0.001 | 0.007 | |
| LOS | Correlation coefficient | −0.118 * | |
| p value | Ns | 0.032 | |
| MOM/PF/DHM/HM escl./Any MOM | NEC | ROP | LOS | BPD |
|---|---|---|---|---|
| Correlation coefficient | <0.001 | 0.9551 | <0.001 | 0.1691 |
| MOM vs. PF | DHM vs. PF | HM Exclusive vs. PF | ANY MOM vs. DHM | |
|---|---|---|---|---|
| Chirurgical NEC | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| Severe ROP | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| LOS | p < 0.001 | p < 0.001 | ||
| Severe BPD | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| Spearman’s Rho | MV-SIPPV/SIMV | n-IMV | n-CPAP | N Trasfusions | Prenatal Steroids | |
|---|---|---|---|---|---|---|
| ROP | Correlation coefficient | −0.242 *** | −0.304 ** | −0.379 *** | −0.326 *** | −0.141 * |
| p-value | <0.001 | 0.001 | <0.001 | <0.001 | 0.010 |
| MV Duration Hours Media (Min–Max) | |
|---|---|
| HMB | 236 (1–1440) |
| PF | 338 (2–1440) |
| MOM + HMB | 158 (2–1344) |
| MOM | 218 (10–1464) |
| HM exclusive | 207 (12–1440) |
| MOM + BF | 233 (3–1320) |
| Spearman’s Rho | GA | BW | SIPPV/SIMV | n-IMV | n-CPAP | |
|---|---|---|---|---|---|---|
| BPD | Correlation coefficient | 0.487 *** | 0.460 *** | −0.443 *** | −0.437 *** | −0.455 *** |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| MOM% | PF% | DHM% | |
|---|---|---|---|
| 2005 | 8.3 | 58.3 | |
| 2006 | 16.6 | 60 | |
| 2007 | 2.6 | 57.7 | |
| 2008 | 9 | 72.7 | |
| 2009 | 9.7 | 74.2 | |
| 2010 | 14.7 | 67.6 | |
| 2011 | 6.6 | 63.3 | |
| 2012 | 1.8 | 94.4 | |
| 2013 | 9 | 65.2 | |
| 2014 | 14.2 | 42.8 | |
| 2015 | 15.3 | 23 | |
| 2016 | 36.3 | 18 | |
| 2017 | 35 | 15 | |
| 2018 | 46.6 | 40 | |
| 2019 | 43.7 | 25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quitadamo, P.A.; Comegna, L.; Zambianco, A.; Palumbo, G.; Gentile, M.A.; Mondelli, A. Impact of Enteral Nutrition on Clinical Outcomes in Very Low Birth Weight Infants in the NICU: A Single-Center Retrospective Cohort Study. Nutrients 2025, 17, 1138. https://doi.org/10.3390/nu17071138
Quitadamo PA, Comegna L, Zambianco A, Palumbo G, Gentile MA, Mondelli A. Impact of Enteral Nutrition on Clinical Outcomes in Very Low Birth Weight Infants in the NICU: A Single-Center Retrospective Cohort Study. Nutrients. 2025; 17(7):1138. https://doi.org/10.3390/nu17071138
Chicago/Turabian StyleQuitadamo, Pasqua Anna, Laura Comegna, Alessandra Zambianco, Giuseppina Palumbo, Maria Assunta Gentile, and Antonio Mondelli. 2025. "Impact of Enteral Nutrition on Clinical Outcomes in Very Low Birth Weight Infants in the NICU: A Single-Center Retrospective Cohort Study" Nutrients 17, no. 7: 1138. https://doi.org/10.3390/nu17071138
APA StyleQuitadamo, P. A., Comegna, L., Zambianco, A., Palumbo, G., Gentile, M. A., & Mondelli, A. (2025). Impact of Enteral Nutrition on Clinical Outcomes in Very Low Birth Weight Infants in the NICU: A Single-Center Retrospective Cohort Study. Nutrients, 17(7), 1138. https://doi.org/10.3390/nu17071138





