Healthful Plant-Based Dietary Patterns Associated with Reduced Adverse Effects of Air Pollution on COPD: Findings from a Large Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Basic Information of the Subject
2.3. Dietary Assessment and Calculation of Plant-Based Diet Indices
2.4. Air Pollution Estimates
2.5. Ascertainment of COPD
2.6. Missing Data
2.7. Statistical Analysis
3. Results
3.1. Characteristics of Participants
3.2. Characteristic Distribution of Air Pollution and Plant-Based Dietary Pattern
3.3. Associations Between COPD Risk and Air Pollution Exposure or Plant-Based Dietary Pattern
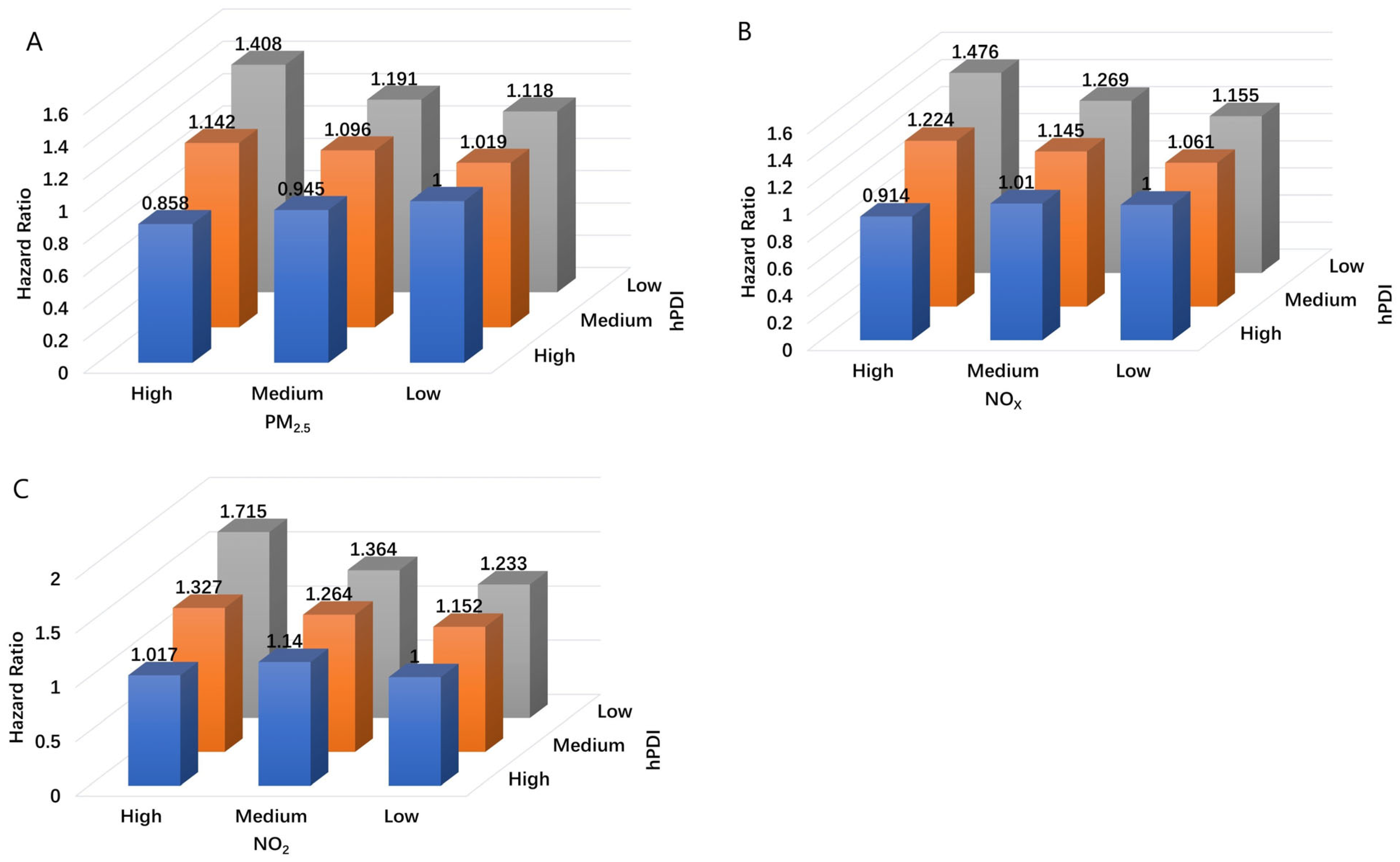
3.4. Combined Effects of Air Pollution Exposure and Plant-Based Dietary Pattern on COPD
3.5. Subgroup Analysis
3.6. Sensitive Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | body mass index |
| CI | confidence interval |
| COPD | chronic obstructive pulmonary disease |
| DASH | dietary approaches to stop hypertension diet |
| GBD | Global Burden of Disease |
| hPDI | healthful plant-based diet index |
| ICD | International Classification of Disease |
| MED | Mediterranean diet |
| NO2 | nitrogen dioxide |
| NOx | nitrogen oxides |
| PD | plant-based diet |
| PDI | plant-based diet index |
| PM | particulate matter |
| RERI | relative excess risks due to interaction |
| uPDI | unhealthful plant-based diet index |
References
- Christenson, S.A.; Smith, B.M.; Bafadhel, M.; Putcha, N. Chronic obstructive pulmonary disease. Lancet 2022, 399, 2227–2242. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhang, T.; Zhang, Y.; Chen, H.; Sang, S. Global burden of COPD attributable to ambient PM2.5 in 204 countries and territories, 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Sci. Total Environ. 2021, 796, 148819. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Carson-Chahhoud, K.; Noori, M.; Nejadghaderi, S.A.; Sullman, M.J.M.; Ahmadian Heris, J.; Ansarin, K.; Mansournia, M.A.; Collins, G.S.; Kolahi, A.-A.; et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990–2019: Results from the Global Burden of Disease Study 2019. BMJ 2022, 378, e069679. [Google Scholar] [CrossRef] [PubMed]
- Stolz, D.; Mkorombindo, T.; Schumann, D.M.; Agusti, A.; Ash, S.Y.; Bafadhel, M.; Bai, C.; Chalmers, J.D.; Criner, G.J.; Dharmage, S.C.; et al. Towards the elimination of chronic obstructive pulmonary disease: A Lancet Commission. Lancet 2022, 400, 921–972. [Google Scholar] [CrossRef]
- Schikowski, T.; Mills, I.C.; Anderson, H.R.; Cohen, A.; Hansell, A.; Kauffmann, F.; Krämer, U.; Marcon, A.; Perez, L.; Sunyer, J.; et al. Ambient air pollution: A cause of COPD? Eur. Respir. J. 2014, 43, 250–263. [Google Scholar] [CrossRef]
- Scoditti, E.; Massaro, M.; Garbarino, S.; Toraldo, D.M. Role of Diet in Chronic Obstructive Pulmonary Disease Prevention and Treatment. Nutrients 2019, 11, 1357. [Google Scholar] [CrossRef]
- Peña-Jorquera, H.; Cid-Jofré, V.; Landaeta-Díaz, L.; Petermann-Rocha, F.; Martorell, M.; Zbinden-Foncea, H.; Ferrari, G.; Jorquera-Aguilera, C.; Cristi-Montero, C. Plant-Based Nutrition: Exploring Health Benefits for Atherosclerosis, Chronic Diseases, and Metabolic Syndrome-A Comprehensive Review. Nutrients 2023, 15, 3244. [Google Scholar] [CrossRef]
- Varraso, R.; Dumas, O.; Boggs, K.M.; Willett, W.C.; Speizer, F.E.; Camargo, C.A. Processed Meat Intake and Risk of Chronic Obstructive Pulmonary Disease among Middle-aged Women. EClinicalMedicine 2019, 14, 88–95. [Google Scholar] [CrossRef]
- van Iersel, L.E.J.; Beijers, R.J.H.C.G.; Gosker, H.R.; Schols, A.M.W.J. Nutrition as a modifiable factor in the onset and progression of pulmonary function impairment in COPD: A systematic review. Nutr. Rev. 2022, 80, 1434–1444. [Google Scholar] [CrossRef]
- Cho, Y.; Chung, H.-K.; Kim, S.-S.; Shin, M.-J. Dietary patterns and pulmonary function in Korean women: Findings from the Korea National Health and Nutrition Examination Survey 2007–2011. Food Chem. Toxicol. 2014, 74, 177–183. [Google Scholar] [CrossRef]
- Medina-Remón, A.; Kirwan, R.; Lamuela-Raventós, R.M.; Estruch, R. Dietary patterns and the risk of obesity, type 2 diabetes mellitus, cardiovascular diseases, asthma, and neurodegenerative diseases. Crit. Rev. Food Sci. Nutr. 2018, 58, 262–296. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrova, K.; Koelman, L.; Rodrigues, C.E. Dietary patterns and biomarkers of oxidative stress and inflammation: A systematic review of observational and intervention studies. Redox Biol. 2021, 42, 101869. [Google Scholar] [CrossRef] [PubMed]
- Varraso, R.; Dumas, O.; Tabung, F.K.; Boggs, K.M.; Fung, T.T.; Hu, F.; Giovannucci, E.; Speizer, F.E.; Willett, W.C.; Camargo, C.A. Healthful and Unhealthful Plant-Based Diets and Chronic Obstructive Pulmonary Disease in U.S. Adults: Prospective Study. Nutrients 2023, 15, 765. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef]
- Sin, D.D.; Doiron, D.; Agusti, A.; Anzueto, A.; Barnes, P.J.; Celli, B.R.; Criner, G.J.; Halpin, D.; Han, M.K.; Martinez, F.J.; et al. Air pollution and COPD: GOLD 2023 committee report. Eur. Respir. J. 2023, 61, 2202469. [Google Scholar] [CrossRef]
- Fan, C.; Wang, W.; Wang, S.; Zhou, W.; Ling, L. Multiple dietary patterns and the association between long-term air pollution exposure with type 2 diabetes risk: Findings from UK Biobank cohort study. Ecotoxicol. Environ. Saf. 2024, 275, 116274. [Google Scholar] [CrossRef]
- Sudlow, C.; Gallacher, J.; Allen, N.; Beral, V.; Burton, P.; Danesh, J.; Downey, P.; Elliott, P.; Green, J.; Landray, M.; et al. UK Biobank: An Open Access Resource for Identifying the Causes of a Wide Range of Complex Diseases of Middle and Old Age. PLoS Med. 2015, 12, e1001779. [Google Scholar] [CrossRef]
- Piernas, C.; Perez-Cornago, A.; Gao, M.; Young, H.; Pollard, Z.; Mulligan, A.; Lentjes, M.; Carter, J.; Bradbury, K.; Key, T.J.; et al. Describing a new food group classification system for UK biobank: Analysis of food groups and sources of macro- and micronutrients in 208,200 participants. Eur. J. Nutr. 2021, 60, 2879–2890. [Google Scholar] [CrossRef]
- Qian, F.; Liu, G.; Hu, F.B.; Bhupathiraju, S.N.; Sun, Q. Association Between Plant-Based Dietary Patterns and Risk of Type 2 Diabetes. JAMA Intern. Med. 2019, 179, 1335–1344. [Google Scholar] [CrossRef]
- Beelen, R.; Hoek, G.; Vienneau, D.; Eeftens, M.; Dimakopoulou, K.; Pedeli, X.; Tsai, M.-Y.; Künzli, N.; Schikowski, T.; Marcon, A.; et al. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe—The ESCAPE project. Atmos. Environ. 2013, 72, 10–23. [Google Scholar] [CrossRef]
- Dirgawati, M.; Barnes, R.; Wheeler, A.J.; Arnold, A.-L.; McCaul, K.A.; Stuart, A.L.; Blake, D.; Hinwood, A.; Yeap, B.B.; Heyworth, J.S. Development of Land Use Regression models for predicting exposure to NO2 and NOx in Metropolitan Perth, Western Australia. Environ. Model. Softw. 2015, 74, 258–267. [Google Scholar] [CrossRef]
- Li, J.; Yang, L.; Yao, Y.; Gu, P.; Xie, Y.; Yin, H.; Xue, M.; Jiang, Y.; Dai, J.; Ma, J. Associations between long-term night shift work and incidence of chronic obstructive pulmonary disease: A prospective cohort study of 277,059 UK Biobank participants. BMC Med. 2024, 22, 16. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Cai, M.; Li, H.; Wang, X.; Tian, F.; Wu, Y.; Zhang, Z.; Lin, H. Risk/benefit tradeoff of habitual physical activity and air pollution on chronic pulmonary obstructive disease: Findings from a large prospective cohort study. BMC Med. 2022, 20, 70. [Google Scholar] [CrossRef]
- Knol, M.J.; VanderWeele, T.J.; Groenwold, R.H.H.; Klungel, O.H.; Rovers, M.M.; Grobbee, D.E. Estimating measures of interaction on an additive scale for preventive exposures. Eur. J. Epidemiol. 2011, 26, 433–438. [Google Scholar] [CrossRef]
- Knol, M.J.; VanderWeele, T.J. Recommendations for presenting analyses of effect modification and interaction. Int. J. Epidemiol. 2012, 41, 514–520. [Google Scholar] [CrossRef]
- Bates, D.V.; Hogg, J.C. Inhaled Carbon and Lung Function in Children. N. Engl. J. Med. 2006, 355, 1496–1497. [Google Scholar] [CrossRef]
- Harré, E.S.; Price, P.D.; Ayrey, R.B.; Toop, L.J.; Martin, I.R.; Town, G.I. Respiratory effects of air pollution in chronic obstructive pulmonary disease: A three month prospective study. Thorax 1997, 52, 1040. [Google Scholar] [CrossRef]
- Andersen, Z.J.; Hvidberg, M.; Jensen, S.S.; Ketzel, M.; Loft, S.; Sørensen, M.; Tjønneland, A.; Overvad, K.; Raaschou-Nielsen, O. Chronic obstructive pulmonary disease and long-term exposure to traffic-related air pollution: A cohort study. Am. J. Respir. Crit. Care Med. 2011, 183, 455–461. [Google Scholar] [CrossRef]
- Park, S.L.; Lichtensztajn, D.; Yang, J.; Wu, J.; Shariff-Marco, S.; Stram, D.O.; Inamdar, P.; Fruin, S.; Larsen, T.; Tseng, C.; et al. Ambient Air Pollution and COPD: The Multiethnic Cohort Study. Ann. Am. Thorac. Soc. 2025, 10, 1513. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, J.; Lu, W. Exposure to nitrogen dioxide and chronic obstructive pulmonary disease (COPD) in adults: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. 2018, 25, 15133–15145. [Google Scholar] [CrossRef]
- Fischer, A.; Johansson, I.; Blomberg, A.; Sundström, B. Adherence to a Mediterranean-like Diet as a Protective Factor Against COPD: A Nested Case-Control Study. COPD J. Chronic Obstr. Pulm. Dis. 2019, 16, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Gu, S.; Wang, X.; Qi, X. Associations of adherence to the DASH diet and the Mediterranean diet with chronic obstructive pulmonary disease among US adults. Front. Nutr. 2023, 10, 1031071. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Cho, S.W.; Park, Y.K. Long-term vegetarians have low oxidative stress, body fat, and cholesterol levels. Nutr. Res. Pr. 2012, 6, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Björkman, A.; Cai, K.; Liu, G.; Wang, C.; Li, Y.; Xia, H.; Sun, L.; Kristiansen, K.; Wang, J.; et al. Impact of a 3-Months Vegetarian Diet on the Gut Microbiota and Immune Repertoire. Front. Immunol. 2018, 9, 908. [Google Scholar] [CrossRef]
- Lim, C.C.; Hayes, R.B.; Ahn, J.; Shao, Y.; Silverman, D.T.; Jones, R.R.; Thurston, G.D. Mediterranean Diet and the Association Between Air Pollution and Cardiovascular Disease Mortality Risk. Circulation 2019, 139, 1766–1775. [Google Scholar] [CrossRef]
- Zhu, A.; Chen, H.; Shen, J.; Wang, X.; Li, Z.; Zhao, A.; Shi, X.; Yan, L.; Zeng, Y.; Yuan, C.; et al. Interaction between plant-based dietary pattern and air pollution on cognitive function: A prospective cohort analysis of Chinese older adults. Lancet Reg. Health West. Pac. 2022, 20, 100372. [Google Scholar] [CrossRef]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A.; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef]
- Kelly, F.J.; Fussell, J.C. Air pollution and public health: Emerging hazards and improved understanding of risk. Environ. Geochem. Health 2015, 37, 631–649. [Google Scholar] [CrossRef]
- Ling, S.H.; van Eeden, S.F. Particulate matter air pollution exposure: Role in the development and exacerbation of chronic obstructive pulmonary disease. Int. J. Chron. Obs. Pulmon Dis. 2009, 4, 233–243. [Google Scholar] [CrossRef]
- Li, X.Y.; Gilmour, P.S.; Donaldson, K.; MacNee, W. Free radical activity and pro-inflammatory effects of particulate air pollution (PM10) in vivo and in vitro. Thorax 1996, 51, 1216–1222. [Google Scholar] [CrossRef]
- Abbey, D.E.; Burchette, R.J.; Knutsen, S.F.; McDonnell, W.F.; Lebowitz, M.D.; Enright, P.L. Long-term particulate and other air pollutants and lung function in nonsmokers. Am. J. Respir. Crit. Care Med. 1998, 158, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C. Marine omega-3 fatty acids and inflammatory processes: Effects, mechanisms and clinical relevance. Biochim. Biophys. Acta 2015, 1851, 469–484. [Google Scholar] [CrossRef] [PubMed]
- Marsland, A.L.; Gianaros, P.J.; Kuan, D.C.H.; Sheu, L.K.; Krajina, K.; Manuck, S.B. Brain morphology links systemic inflammation to cognitive function in midlife adults. Brain Behav. Immun. 2015, 48, 195–204. [Google Scholar] [CrossRef] [PubMed]
| Variables a | All (n = 162,741) | Participants Without COPD (n = 158,061, 97.1%) | Participants with COPD (n = 4680, 2.9%) | p |
|---|---|---|---|---|
| Age | <0.001 | |||
| <60 years | 96,947 (59.6) | 95,441 (60.4) | 1506 (32.2) | |
| ≥60 years | 65,794 (40.4) | 62,620 (39.6) | 3174 (67.8) | |
| Sex | <0.001 | |||
| Female | 89,962 (55.3) | 87,892 (55.6) | 2070 (44.2) | |
| Male | 72,779 (44.7) | 70,169 (44.4) | 2610 (55.8) | |
| Ethnicity | <0.001 | |||
| White | 15,6397 (96.1) | 15,1852 (96.1) | 4545 (97.1) | |
| Others | 6344 (3.9) | 6209 (3.9) | 135 (2.9) | |
| Education level | <0.001 | |||
| Low | 40,005 (24.6) | 38,786 (24.5) | 1219 (26.0) | |
| Medium | 30,106 (18.5) | 29,161 (18.4) | 945 (20.2) | |
| High | 80,101 (49.2) | 78,560 (49.7) | 1541 (32.9) | |
| None of the above | 11,914 (7.3) | 10,985 (6.9) | 929 (19.9) | |
| Missing | 615 (0.4) | 569 (0.4) | 46 (1.0) | |
| Household income | <0.001 | |||
| <GBP 18,000 | 21,151 (13.0) | 19,814 (12.5) | 1337 (28.6) | |
| GBP 18,000–GBP 30,999 | 35,398 (21.8) | 34,093 (21.6) | 1305 (27.9) | |
| GBP 31,000–GBP 51,999 | 42,485 (26.1) | 41,569 (26.3) | 916 (19.6) | |
| GBP 52,000–GBP 100,000 | 36,885 (22.7) | 36,413 (23.0) | 472 (10.1) | |
| >GBP 100,000 | 11,009 (6.8) | 10,916 (6.9) | 93 (2.0) | |
| Missing | 15,813 (9.7) | 15,256 (9.7) | 557 (11.9) | |
| BMI | <0.001 | |||
| <25 kg/m2 | 62,161 (38.2) | 60,718 (38.4) | 1443 (30.8) | |
| 25–29.9 kg/m2 | 67,096 (41.2) | 65,262 (41.3) | 1834 (39.2) | |
| ≥30 kg/m2 | 33,029 (20.3) | 31,653 (20.0) | 1376 (29.4) | |
| Missing | 455 (0.3) | 428 (0.3) | 27 (0.6) | |
| Smoking | <0.001 | |||
| Never | 92,029 (56.5) | 91,001 (57.6) | 1028 (22.0) | |
| Previous | 58,486 (35.9) | 56,051 (35.5) | 2435 (52.0) | |
| Current | 11,829 (7.3) | 10,629 (6.7) | 1200 (25.6) | |
| Missing | 397 (0.2) | 380 (0.2) | 17 (0.4) | |
| Drinking | <0.001 | |||
| Never | 4800 (2.9) | 4656 (2.9) | 144 (3.1) | |
| Previous | 4713 (2.9) | 4442 (2.8) | 271 (5.8) | |
| Current | 153,091 (94.1) | 148,832 (94.2) | 4259 (91.0) | |
| Missing | 137 (0.1) | 131 (0.1) | 6 (0.1) |
| Model | Low | Medium, HR (95% CI) | High, HR (95% CI) | p-Trend a | per SD |
|---|---|---|---|---|---|
| PM2.5 | |||||
| Model 1 | 1 | 1.150 (1.069, 1.238) | 1.257 (1.158, 1.364) | <0.001 | 1.100 (1.070, 1.131) |
| Model 2 | 1 | 1.043 (0.969, 1.123) | 1.097 (1.009, 1.192) | 0.028 | 1.049 (1.019, 1.079) |
| PM2.5–10 | |||||
| Model 1 | 1 | 1.153 (1.072, 1.240) | 1.144 (1.053, 1.243) | 0.002 | 1.020 (0.992, 1.049) |
| Model 2 | 1 | 1.103 (1.026, 1.186) | 1.087 (1.000, 1.181) | 0.059 | 1.005 (0.977, 1.034) |
| PM10 | |||||
| Model 1 | 1 | 1.089 (1.014, 1.170) | 1.131 (1.043, 1.227) | 0.003 | 1.049 (1.020, 1.079) |
| Model 2 | 1 | 1.017 (0.946, 1.092) | 1.042 (0.960, 1.131) | 0.320 | 1.014 (0.985, 1.044) |
| NO2 | |||||
| Model 1 | 1 | 1.231 (1.144, 1.325) | 1.271 (1.169, 1.381) | <0.001 | 1.089 (1.059, 1.119) |
| Model 2 | 1 | 1.109 (1.030, 1.194) | 1.182 (1.086, 1.287) | <0.001 | 1.065 (1.034, 1.096) |
| NOx | |||||
| Model 1 | 1 | 1.193 (1.109, 1.284) | 1.259 (1.159, 1.367) | <0.001 | 1.097 (1.070, 1.125) |
| Model 2 | 1 | 1.070 (0.994, 1.152) | 1.129 (1.038, 1.227) | 0.005 | 1.063 (1.035, 1.092) |
| PDI | |||||
| Model 1 | 1 | 0.843 (0.788, 0.903) | 0.782 (0.722, 0.848) | <0.001 | 0.906 (0.881, 0.932) |
| Model 2 | 1 | 0.917 (0.856, 0.981) | 0.891 (0.821, 0.966) | 0.004 | 0.953 (0.926, 0.981) |
| hPDI | |||||
| Model 1 | 1 | 0.821 (0.768, 0.877) | 0.647 (0.596, 0.703) | <0.001 | 0.839 (0.816, 0.863) |
| Model 2 | 1 | 0.884 (0.827, 0.946) | 0.758 (0.697, 0.825) | <0.001 | 0.888 (0.862, 0.915) |
| uPDI | |||||
| Model 1 | 1 | 1.054 (0.980, 1.133) | 1.189 (1.097, 1.289) | <0.001 | 1.071 (1.041, 1.102) |
| Model 2 | 1 | 1.100 (1.023, 1.183) | 1.235 (1.139, 1.340) | <0.001 | 1.086 (1.055, 1.118) |
| Air Pollution | hPDI | Air Pollution Levels (HR (95% CI)) | RERI a | p for Interaction b | |||
|---|---|---|---|---|---|---|---|
| High | Medium | Low | High | Medium | |||
| Model 1 | |||||||
| PM2.5 | Low | 1.869 (1.596, 2.188) | 1.500 (1.295, 1.737) | 1.270 (1.069, 1.509) | 0.64 (0.38, 0.91) | 0.22 (−0.01, 0.45) | <0.001 |
| Medium | 1.389 (1.198, 1.611) | 1.290 (1.123, 1.482) | 1.084 (0.929, 1.263) | 0.35 (0.14, 0.55) | 0.19 (0.04, 0.35) | ||
| High | 0.958 (0.802, 1.145) | 1.013 (0.867, 1.182) | 1 | ||||
| NO2 | Low | 2.117 (1.793, 2.500) | 1.731 (1.486, 2.017) | 1.395 (1.167, 1.668) | 0.66 (0.36, 0.96) | 0.11 (−0.15, 0.37) | 0.002 |
| Medium | 1.522 (1.302, 1.780) | 1.489 (1.287, 1.722) | 1.221 (1.040, 1.432) | 0.24 (0.01, 0.47) | 0.044 (−0.17, 0.26) | ||
| High | 1.066 (0.887, 1.281) | 1.224 (1.043, 1.437) | 1 | ||||
| NOX | Low | 1.885 (1.604, 2.216) | 1.616 (1.394, 1.874) | 1.313 (1.103, 1.563) | 0.58 (0.30, 0.85) | 0.22 (−0.02, 0.46) | 0.003 |
| Medium | 1.454 (1.250, 1.691) | 1.358 (1.180, 1.563) | 1.122 (0.961, 1.311) | 0.33 (0.12, 0.55) | 0.15 (−0.04, 0.34) | ||
| High | 0.998 (0.834, 1.194) | 1.086 (0.929, 1.270) | 1 | ||||
| Model 2 | |||||||
| PM2.5 | Low | 1.408 (1.200, 1.652) | 1.191 (1.027, 1.381) | 1.118 (0.940, 1.329) | 0.44 (0.21, 0.67) | 0.13 (−0.08, 0.34) | 0.001 |
| Medium | 1.142 (0.983, 1.326) | 1.096 (0.954, 1.259) | 1.019 (0.874, 1.188) | 0.26 (0.07, 0.45) | 0.13 (−0.05, 0.31) | ||
| High | 0.858 (0.717, 1.026) | 0.945 (0.809, 1.104) | 1 | ||||
| NO2 | Low | 1.715 (1.450, 2.028) | 1.364 (1.169, 1.592) | 1.233 (1.030, 1.475) | 0.48 (0.21, 0.75) | 0.00 (−0.24, 0.25) | 0.005 |
| Medium | 1.327 (1.133, 1.553) | 1.264 (1.092, 1.462) | 1.152 (0.982, 1.352) | 0.15 (−0.07, 0.38) | −0.03 (−0.24, 0.17) | ||
| High | 1.017 (0.846, 1.223) | 1.140 (0.971, 1.338) | 1 | ||||
| NOX | Low | 1.476 (1.253, 1.739) | 1.269 (1.093, 1.473) | 1.155 (0.970, 1.377) | 0.41 (0.17, 0.66) | 0.11 (−0.11, 0.33) | 0.005 |
| Medium | 1.224 (1.052, 1.425) | 1.145 (0.994, 1.318) | 1.061 (0.908, 1.240) | 0.24 (0.04, 0.44) | 0.07 (−0.12, 0.26) | ||
| High | 0.914 (0.764, 1.095) | 1.010 (0.863, 1.181) | 1 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, T.; Zhao, C.; Fang, X.; Zhao, J.; Chao, W.; Bo, Y.; Zhou, L. Healthful Plant-Based Dietary Patterns Associated with Reduced Adverse Effects of Air Pollution on COPD: Findings from a Large Cohort Study. Nutrients 2025, 17, 1055. https://doi.org/10.3390/nu17061055
Wang T, Zhao C, Fang X, Zhao J, Chao W, Bo Y, Zhou L. Healthful Plant-Based Dietary Patterns Associated with Reduced Adverse Effects of Air Pollution on COPD: Findings from a Large Cohort Study. Nutrients. 2025; 17(6):1055. https://doi.org/10.3390/nu17061055
Chicago/Turabian StyleWang, Tianrun, Chenyu Zhao, Xiaoqi Fang, Jia Zhao, Wangzhe Chao, Yacong Bo, and Liting Zhou. 2025. "Healthful Plant-Based Dietary Patterns Associated with Reduced Adverse Effects of Air Pollution on COPD: Findings from a Large Cohort Study" Nutrients 17, no. 6: 1055. https://doi.org/10.3390/nu17061055
APA StyleWang, T., Zhao, C., Fang, X., Zhao, J., Chao, W., Bo, Y., & Zhou, L. (2025). Healthful Plant-Based Dietary Patterns Associated with Reduced Adverse Effects of Air Pollution on COPD: Findings from a Large Cohort Study. Nutrients, 17(6), 1055. https://doi.org/10.3390/nu17061055





