Nutritionist-Guided Video Intervention Improves Adherence to Mediterranean Diet and Reduces the Rate of Gestational Diabetes Mellitus: A Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
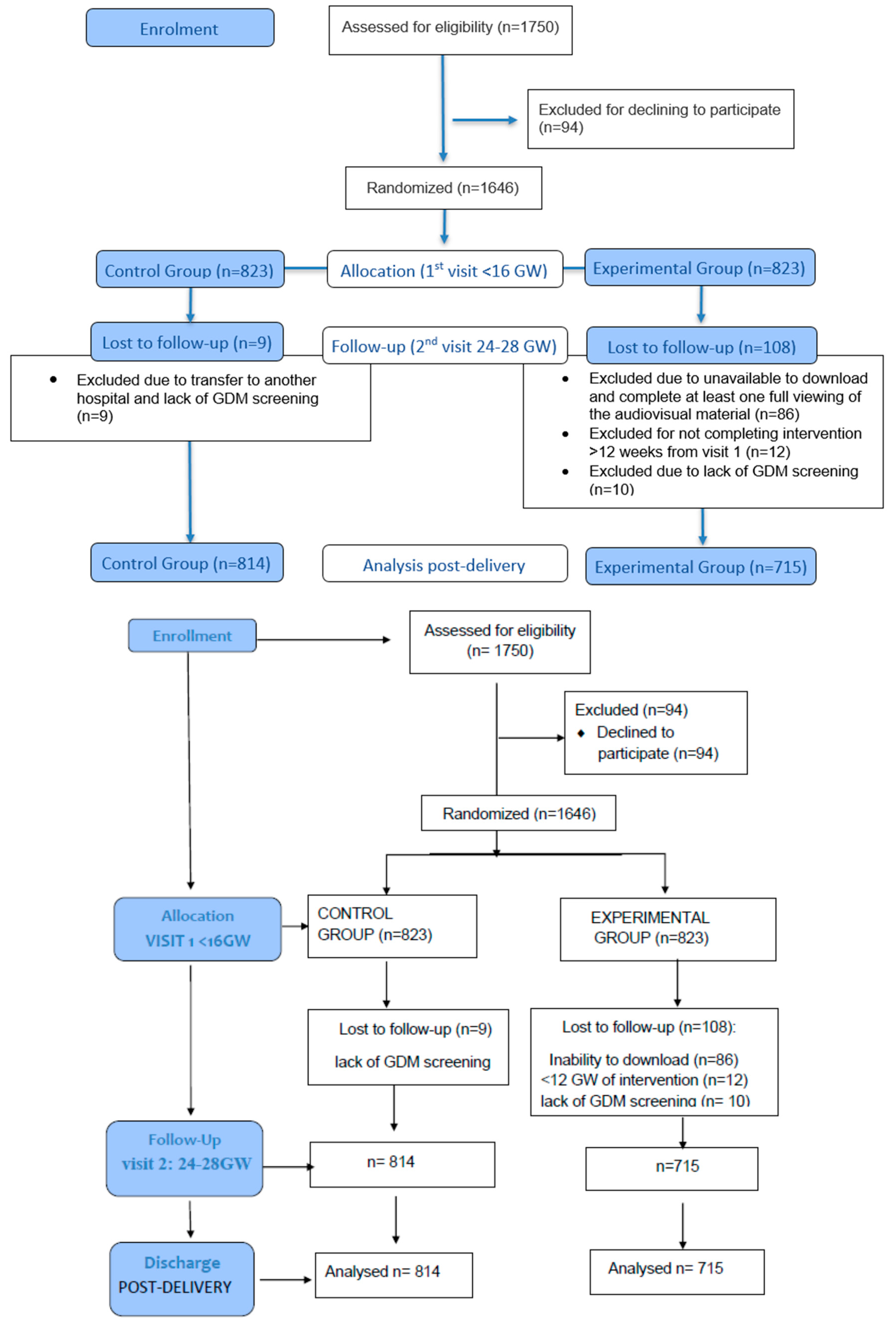
2.1. Study Design
2.2. Setting and Population
2.3. Randomization and Allocation
2.4. Intervention and Follow-Up
- -
- Mediterranean diet adherence: a minimum of 3 servings per day of dairy products. Fruit and vegetables should be eaten daily, with at least 12 servings of each of these groups per week. Whole fruit should be prioritized over juices. Extra virgin olive oil (EVOO) should be used as the main fat. No less than four tablespoons per day are recommended, including both raw for dressing dishes and homemade vegetable stir-fries with this olive oil. This will avoid commercial sauces. A handful of nuts is recommended every day, mainly pistachios. Pregnant women should be encouraged to choose whole foods instead of refined ones (>5 days per week). The recommendation for legumes consumption is 3 servings per week and the recommendation for consumption of oily fish is, at least, three servings per week, including canned fish, mainly small ones. Avoidance of processed foods (<2 days per week) was recommended, and instead consume white meats such as chicken, turkey, or rabbit over red meats. Commercial confectionery and processed snacks should be avoided (<2 days per week). Drinking regular water should be prioritized over sugary drinks such as soft drinks, milkshakes, and juices, which should be avoided (<2 portions per week). In addition, the video provided several meal ideas with images to make it more appealing. The aim was to increase adherence and simplify the intervention recommendations.
- -
- Physical activity recommendations included moderate strength training adapted to pregnancy, an active lifestyle with ≥1 h/day walking, stair climbing, and avoiding prolonged sitting.
2.5. Clinical Outcomes
2.6. Data Collection and Variables
- -
- Clinical history: personal and family history of diabetes, hypertension, dyslipidemia, obesity, obstetric history, medications, supplements, smoking status.
- -
- Anthropometric and clinical data: pregestational weight and height, body mass index (BMI), blood pressure.
- -
- Biochemical parameters: Blood and urine samples were obtained after an overnight fast of at least 8 h. Fasting plasma glucose (mmol/L) was determined in serum by the glucose–hexokinase method using an AU5800 analyzer (Beckman Coulter Diagnostics, Brea, CA, USA). Glycated hemoglobin (HbA1c, %) was measured by ion-exchange high-performance liquid chromatography (HPLC) on a Tosoh G8 analyzer (Tosoh Co., Tokyo, Japan). The method is standardized against the International Federation of Clinical Chemistry, with an imprecision of 1.23% for 32.23 mmol/mol (5.1% NGSP) and 1.36% for 85.24 mmol/mol (10% NGSP). Fasting serum insulin (μIU/mL) was quantified by chemiluminescence immunoassay (IMMULITE 2000 Xpi, Siemens Healthcare Diagnostics, Munich, Germany). Inter-assay CVs were 6.3% at 11 μIU/mL and 5.9% at 21 μIU/mL. Insulin resistance was estimated using the homeostasis model assessment (HOMA-IR): glucose (mmol/L) × insulin (μIU/mL)/22.7. All laboratory methods were subject to monthly external quality assurance by the Spanish Society of Clinical Chemistry (SEQC), which also performed regular method validation and review.
- -
- Dietary adherence using adapted 14-point MEDAS (12-point score; range 0–12).
- -
- Physical activity was assessed using the IPAQ, which records time spent walking, stair climbing, aerobic activities and moderate-intensity exercise. Daily walking time (minutes/week) and stair climbing (number of floors per day, >5 days/week) were specifically recorded, together with the frequency of aerobic and moderate-intensity exercise.
- -
- To assess patient satisfaction, at the end of the dietary questionnaires, participants in the experimental group were asked whether the information provided in the video had been clear and whether they found it useful. This exploratory assessment aimed to collect feedback for the potential improvement of the educational video.
2.7. Sample Size Calculation
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sweeting, A.; Hannah, W.; Backman, H.; Catalano, P.; Feghali, M.; Herman, W.H.; Hivert, M.-F.; Immanuel, J.; Meek, C.; Oppermann, M.L. Epidemiology and management of gestational diabetes. Lancet 2024, 404, 175–192. [Google Scholar] [CrossRef]
- Wang, H.; Li, N.; Chivese, T.; Werfalli, M.; Sun, H.; Yuen, L.; Hoegfeldt, C.A.; Powe, C.E.; Immanuel, J.; Karuranga, S.; et al. IDF Diabetes Atlas: Estimation of Global and Regional Gestational Diabetes Mellitus Prevalence for 2021 by International Association of Diabetes in Pregnancy Study Group’s Criteria. Diabetes Res. Clin. Pract. 2022, 183, 109050. Available online: https://www.diabetesresearchclinicalpractice.com/article/S0168-8227(21)00409-5/fulltext (accessed on 30 June 2025). [CrossRef]
- Prevalencia de Diabetes Mellitus Gestacional (DMG). Atlas de la Diabetes. Available online: https://diabetesatlas.org/es/data-by-indicator/hyperglycaemia-in-pregnancy-hip-20-49-y/prevalence-of-gestational-diabetes-mellitus-gdm/ (accessed on 1 July 2025).
- Paulo, M.S.; Abdo, N.M.; Bettencourt-Silva, R.; Al-Rifai, R.H. Gestational Diabetes Mellitus in Europe: A Systematic Review and Meta-Analysis of Prevalence Studies. Front. Endocrinol. 2021, 12, 691033. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee. 15. Management of Diabetes in Pregnancy: Standards of Care in Diabetes—2025. Diabetes Care 2024, 48 (Suppl. S1), S306–S320. [Google Scholar] [CrossRef]
- Dolatkhah, N.; Hajifaraji, M.; Shakouri, S.K. Nutrition Therapy in Managing Pregnant Women with Gestational Diabetes Mellitus: A Literature Review. J. Fam. Reprod. Health 2018, 12, 57–72. [Google Scholar]
- Popova, P.V.; Pustozerov, E.A.; Tkachuk, A.S.; Grineva, E.N. Improving nutrition for the prevention of gestational diabetes: Current status and perspectives. World J. Diabetes 2021, 12, 1494–1506. [Google Scholar] [CrossRef] [PubMed]
- Takele, W.W.; Vesco, K.K.; Josefson, J.; Redman, L.M.; Hannah, W.; Bonham, M.P.; Chen, M.; Chivers, S.C.; Fawcett, A.J.; Grieger, J.A.; et al. Effective interventions in preventing gestational diabetes mellitus: A systematic review and meta-analysis. Commun. Med. 2024, 4, 75. [Google Scholar] [CrossRef]
- Xu, J.; Lin, X.; Fang, Y.; Cui, J.; Li, Z.; Yu, F.; Tian, L.; Guo, H.; Lu, X.; Ding, J.; et al. Lifestyle interventions to prevent adverse pregnancy outcomes in women at high risk for gestational diabetes mellitus: A randomized controlled trial. Front. Immunol. 2023, 14, 1191184. [Google Scholar] [CrossRef]
- Assaf-Balut, C.; García de la Torre, N.; Durán, A.; Fuentes, M.; Bordiú, E.; Del Valle, L.; Familiar, C.; Ortolá, A.; Jiménez, I.; Herraiz, M.A.; et al. A Mediterranean diet with additional extra virgin olive oil and pistachios reduces the incidence of gestational diabetes mellitus (GDM): A randomized controlled trial: The St. Carlos GDM prevention study. PLoS ONE 2017, 12, e0185873. [Google Scholar] [CrossRef]
- Duran, A.; Torrejón, M.J.; Runkle, I.; Calle-Pascual, A.L. Response to Comment on Duran et al. Introduction of IADPSG Criteria for the Screening and Diagnosis of Gestational Diabetes Mellitus Results in Improved Pregnancy Outcomes at a Lower Cost in a Large Cohort of Pregnant Women: The St. Carlos Gestational Diabetes Study. Diabetes Care 2014;37:2442-2450. Diabetes Care 2015, 38, e41–e42. [Google Scholar]
- de la Torre, N.G.; Assaf-Balut, C.; Jiménez Varas, I.; Del Valle, L.; Durán, A.; Fuentes, M.; del Prado, N.; Bordiú, E.; Valerio, J.J.; Herraiz, M.A.; et al. Effectiveness of Following Mediterranean Diet Recommendations in the Real World in the Incidence of Gestational Diabetes Mellitus (GDM) and Adverse Maternal-Foetal Outcomes: A Prospective, Universal, Interventional Study with a Single Group. The St Carlos Study. Nutrients 2019, 11, 1210. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidance on Global Monitoring for Diabetes Prevention and Control: Framework, Indicators and Application. 2024. Available online: https://cdn.who.int/media/docs/default-source/ncds/ncd-surveillance/guidance-on-global-monitoring-for-diabetes.pdf?sfvrsn=ccb261b8_4 (accessed on 1 October 2025).
- Leblalta, B.; Kebaili, H.; Sim, R.; Lee, S.W.H. Digital health interventions for gestational diabetes mellitus: A systematic review and meta-analysis of randomised controlled trials. PLoS Digit Health 2022, 1, e0000015. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.L.; Félix, B.; Nunes, F.; Santos, I. Systematic development and refinement of a user-centered evidence-based digital toolkit for supporting self-care in gestational diabetes mellitus. Sci. Rep. 2025, 15, 12009. [Google Scholar] [CrossRef]
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International Association of Diabetes and Pregnancy Study Groups Recommendations on the Diagnosis and Classification of Hyperglycemia in Pregnancy. Diabetes Care 2010, 33, 676–682. [Google Scholar] [CrossRef]
- Obstetrics & Gynecology. Available online: https://journals.lww.com/greenjournal/abstract/2020/06000/gestational_hypertension_and_preeclampsia__acog.46.aspx (accessed on 15 September 2025).
- Villar, J.; Cheikh Ismail, L.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef]
- Adamkin, D.H. Committee on Fetus and Newborn. Postnatal Glucose Homeostasis in Late-Preterm and Term Infants. Pediatrics 2011, 127, e20103851. [Google Scholar] [CrossRef]
- GDM and Maternal-Foetal Adverse Outcomes Rates After Providing Lifestyle Recommendations Based on a Motivational Video Early in Pregnancy. The St Carlos TELE_MED_DIET Study. Zenodo. 2025. Available online: https://zenodo.org/records/16419364 (accessed on 3 September 2025).
- Melero, V.; García de la Torre, N.; Assaf-Balut, C.; Jiménez, I.; del Valle, L.; Durán, A.; Bordiú, E.; Valerio, J.J.; A Herraiz, M.; Izquierdo, N.; et al. Effect of a Mediterranean Diet-Based Nutritional Intervention on the Risk of Developing Gestational Diabetes Mellitus and Other Maternal-Fetal Adverse Events in Hispanic Women Residents in Spain. Nutrients 2020, 12, 3505. [Google Scholar] [CrossRef]
- Sharma, S.; Esposito, S.; Di Castelnuovo, A.; Gialluisi, A.; De Domenico, P.; de Gaetano, G.; Bonaccio, M.; Iacoviello, L. Impact of Mediterranean Diet Adherence During Pregnancy on Preeclampsia, Gestational Diabetes Mellitus, and Excessive Gestational Weight Gain: A Systematic Review of Observational Studies and Randomized Controlled Trials. Nutrients 2025, 17, 1723. [Google Scholar] [CrossRef]
- HAl Wattar, B.; Dodds, J.; Placzek, A.; Beresford, L.; Spyreli, E.; Moore, A.; Carreras, F.J.G.; Austin, F.; Murugesu, N.; Roseboom, T.J.; et al. Mediterranean-style diet in pregnant women with metabolic risk factors (ESTEEM): A pragmatic multicentre randomised trial. PLoS Med. 2019, 16, e1002857. [Google Scholar] [CrossRef]
- Tieu, J.; Shepherd, E.; Middleton, P.; Crowther, C.A. Dietary advice interventions in pregnancy for preventing gestational diabetes mellitus. Cochrane Database Syst. Rev. 2017, 1, CD006674. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, E.; Gomersall, J.C.; Tieu, J.; Han, S.; Crowther, C.A.; Middleton, P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst. Rev. 2017, 11, CD010443. [Google Scholar] [CrossRef] [PubMed]
| Experimental Group | Control Group | p Value | |
|---|---|---|---|
| N | 715 | 814 | |
| Age (years) | 31.88 ± 5.56 | 32.41 ± 5.79 | 0.776 |
| PP-BW (kg) | 64.68 ± 13.09 | 64.50 ±12.78 | 0.279 |
| PP-BMI (kg/m2) | 24.8 ± 4.9 | 24.3 ± 4.7 | 0.048 |
| sBP (mm Hg) | 113.7 ± 11.9 | 116.3 ± 12.1 | 0.001 |
| dBP (mm Hg) | 76.2 ± 8.4 | 74.9 ± 8.9 | 0.005 |
| FSG (mg/dL) | 82.5 ± 5.8 | 81.7 ± 6.0 | 0.080 |
| HbA1c % | 5.2 ± 0.3 | 5.2 ± 0.3 | 0.114 |
| Primiparous n (%) | 278 (38.9) | 352 (43.2) | 0.301 |
| Prior GDM | 54 (7.6) | 69 (8.5) | 0.285 |
| Prior Miscarriage | 274 (38.3) | 300 (36.9) | 0.093 |
| Never Smoker (%) | 509 (71.2) | 577 (71.1) | 0.186 |
| Ethnicity: Caucasian Latin American | 0.000 | ||
| 331 (46.3) | 459 (56.4) | ||
| 370 (51.7) | 328 (40.3) | ||
| Educational status: Low High | 26 (3.6) | 38 (4.6) | 0.052 |
| 433 (62.3) | 506 (62.3) | ||
| Occupation | 534 (74.9) | 627 (77.2) | 0.309 |
| MEDAS Score | 7.3 ± 2.4 | 7.6 ± 2.3 | 0.169 |
| At Baseline | 24–28 GW | Mean Diferencies (95% CI) | p Value | ||
|---|---|---|---|---|---|
| Medas Score | Control Group | 7.6 ± 2.3 | 7.2 ± 2.3 | −0.22 (−0.30; −0.14) | 0.001 |
| Experimental Group | 7.3 ± 2.4 | 7.7 ± 2.3 | 0.41 (0.23; 0.60) | 0.001 | |
| p value | 0.169 | 0.001 | 0.001 | ||
| Numbers of floors climbed per day. (>5 days a week) | Control Group | 4.5 + 5.4 | 3.7 + 6.0 | −0.8 (−0.5; −1) | 0.001 |
| Experimental Group | 4.7 + 6.0 | 4.8 + 5.6 | 0.6 (0.3; 0.8) | 0.001 | |
| p value | 0.011 | 0.006 | 0.001 | ||
| Walking daily (>5 days) min per week | Control Group | 546 + 412 | 462 + 342 | −84 (−61; −106) | 0.001 |
| Experimental Group | 586 + 450 | 494 + 373 | −93 (−66; −121) | 0.001 | |
| p value | 0.072 | 0.098 | 0.075 | ||
| Pieces of fruit per week | Control Group | 11 ± 9 | 16 ± 9 | 4 (4; 5) | 0.001 |
| Experimental Group | 10 ± 9 | 16 ± 9 | 5 (4; 5) | 0.001 | |
| p value | 0.046 | 0.970 | 0.045 | ||
| EVOO > 40 mL /day N (%) or increase ml/day | Control Group | 371 (45.7) | 490 (60.3) | 5.8 (−7.1; 10.3) | 0.001 |
| Experimental Group | 310 (43.4) | 482 (67.4) | 6.7 (−3.4; 5.7) | 0.001 | |
| p value | 0.194 | 0.007 | 0.004 | ||
| Pistachio/Nuts (serving/weeks) | Control Group | 2.3 ± 2.5 | 2.3 ± 2.6 | −0.3 (−0.4; −0.2) | 0.001 |
| Experimental Group | 2.2 ± 2.5 | 3.0 ± 2.7 | 0.4 (−0.2; 0.8) | 0.001 | |
| p value | 0.229 | 0.011 | 0.001 | ||
| Juice or sugar drinks (serving per week) | Control Group | 3.0 ± 5.6 | 2.9 ± 4.5 | −0.1 (−0.5; 1) | 0.001 |
| Experimental Group | 3.8 ± 6.4 | 2.1 ± 5.6 | −0.7 (0.3; 1.1) | 0.001 | |
| p value | 0.007 | 0.001 | 0.001 | ||
| Bakery/commercial confectionery servings per week | Control Group | 3.1 ± 3.1 | 3.1 ± 2.8 | −0.0 (−0.3; 0.1) | 0.001 |
| Experimental Group | 3.1 ± 3.8 | 2.9 ± 2.6 | −0.2 (−0.4; −0.1) | 0.001 | |
| p value | 0.095 | 0.095 | 0.045 | ||
| Maternal weight gain (Pregestational TO (kg)) | Control Group | 1.0 ± 2.4 | 5.4 ± 3.1 | 6.4 (−0.57; 8.77) | 0.001 |
| Experimental Group | 1.2 ± 2.7 | 4.9 ± 2.3 | 6.2 (0.73; 7.65) | 0.001 | |
| p value | 0.186 | 0.444 | 0.081 | ||
| Experimental Group | Control Group | p | |
|---|---|---|---|
| N | 715 | 814 | |
| Maternal outcomes | |||
| GDM | 148 (20.7) | 204 (25.1) | 0.025 |
| Insulin treatment | 22 (14.9) | 51(17.3) | 0.060 |
| Pregnancy-induced hypertension | 17 (2.6) | 44 (5.6) | 0.004 |
| Preeclampsia | 14 (2.2) | 30 (3.8) | 0.051 |
| Delivery | |||
| Vaginal eutocic | 474 (77.9) | 590 (74.6) | 0.189 |
| Cesarean section | 116 (19.1) | 179 (22.8) | |
| Emergency-CS | 80 (13.1) | 110 (13.9) | 0.418 |
| Episiotomy | 85 (14.4) | 147 (19.0) | 0.015 |
| Perineal Trauma (any tears grade) | 284 (482) | 349 (44.9) | 0.233 |
| Neonatal outcomes | |||
| Gestational Age at birth (weeks) | 38.9 ± 1.6 | 39.0 ± 1.6 | 0.415 |
| <37 GW | 34 (5.6) | 38 (5.0) | 0.324 |
| Birthweight (g) | 3240 ± 434 | 3238 ± 481 | 0.800 |
| Centile | 50.6 ± 27.8 | 50.1 ± 27.4 | 0.774 |
| Length (cm) | 49.7 ± 2.4 | 49.7 ± 2.4 | 0.967 |
| Centile | 59.3 ± 28.4 | 58.4 ± 29.4 | 0.614 |
| LGA > 90 percentile | 50 (9.1) | 61 (7.9) | 0.240 |
| SGA < 10 percentile | 39 (7.1) | 53 (6.8) | 0.459 |
| Apgar Score at 1 min | 8.6 ± 1.7 | 8.6 ± 1.1 | 0.378 |
| Apgar Score at 5 min | 9.7 ± 1.0 | 9.8 ± 0.8 | 0.129 |
| Hypoglycemia | 20 (3.7) | 39 (5.0) | 0.152 |
| NICU/observation | 32 (5.9) | 75 (9.7) | 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín-O’Connor, R.; Ramos-Levi, A.M.; Saviron-Cornudella, R.; López-Plaza, B.; Larrad-Sainz, A.; Barabash, A.; Marcuello-Foncillas, C.; Jiménez-Varas, I.; Diaz-Perez, A.; de Miguel, P.; et al. Nutritionist-Guided Video Intervention Improves Adherence to Mediterranean Diet and Reduces the Rate of Gestational Diabetes Mellitus: A Randomized Clinical Trial. Nutrients 2025, 17, 3533. https://doi.org/10.3390/nu17223533
Martín-O’Connor R, Ramos-Levi AM, Saviron-Cornudella R, López-Plaza B, Larrad-Sainz A, Barabash A, Marcuello-Foncillas C, Jiménez-Varas I, Diaz-Perez A, de Miguel P, et al. Nutritionist-Guided Video Intervention Improves Adherence to Mediterranean Diet and Reduces the Rate of Gestational Diabetes Mellitus: A Randomized Clinical Trial. Nutrients. 2025; 17(22):3533. https://doi.org/10.3390/nu17223533
Chicago/Turabian StyleMartín-O’Connor, Rocío, Ana M. Ramos-Levi, Ricardo Saviron-Cornudella, Bricia López-Plaza, Angélica Larrad-Sainz, Ana Barabash, Clara Marcuello-Foncillas, Inés Jiménez-Varas, Angel Diaz-Perez, Paz de Miguel, and et al. 2025. "Nutritionist-Guided Video Intervention Improves Adherence to Mediterranean Diet and Reduces the Rate of Gestational Diabetes Mellitus: A Randomized Clinical Trial" Nutrients 17, no. 22: 3533. https://doi.org/10.3390/nu17223533
APA StyleMartín-O’Connor, R., Ramos-Levi, A. M., Saviron-Cornudella, R., López-Plaza, B., Larrad-Sainz, A., Barabash, A., Marcuello-Foncillas, C., Jiménez-Varas, I., Diaz-Perez, A., de Miguel, P., Rubio-Herrera, M. A., Matía-Martín, P., & Calle-Pascual, A. L. (2025). Nutritionist-Guided Video Intervention Improves Adherence to Mediterranean Diet and Reduces the Rate of Gestational Diabetes Mellitus: A Randomized Clinical Trial. Nutrients, 17(22), 3533. https://doi.org/10.3390/nu17223533






