Association Between Intensity of Physical Activity in Pregnancy and Gestational Diabetes in a Multi-Ethnic Population: Results from the PROMOTE Cohort Study
Abstract
1. Introduction
1.1. Background/Rationale
1.2. Aim
2. Methods
2.1. Overall Study Design and Population
2.2. Data Collection for Baseline Characteristics
2.3. Data Collection for Physical Activity
2.4. Data Collection for Gestational Diabetes
2.5. Study Size
2.6. Statistical Methods
2.7. Ethics
3. Results
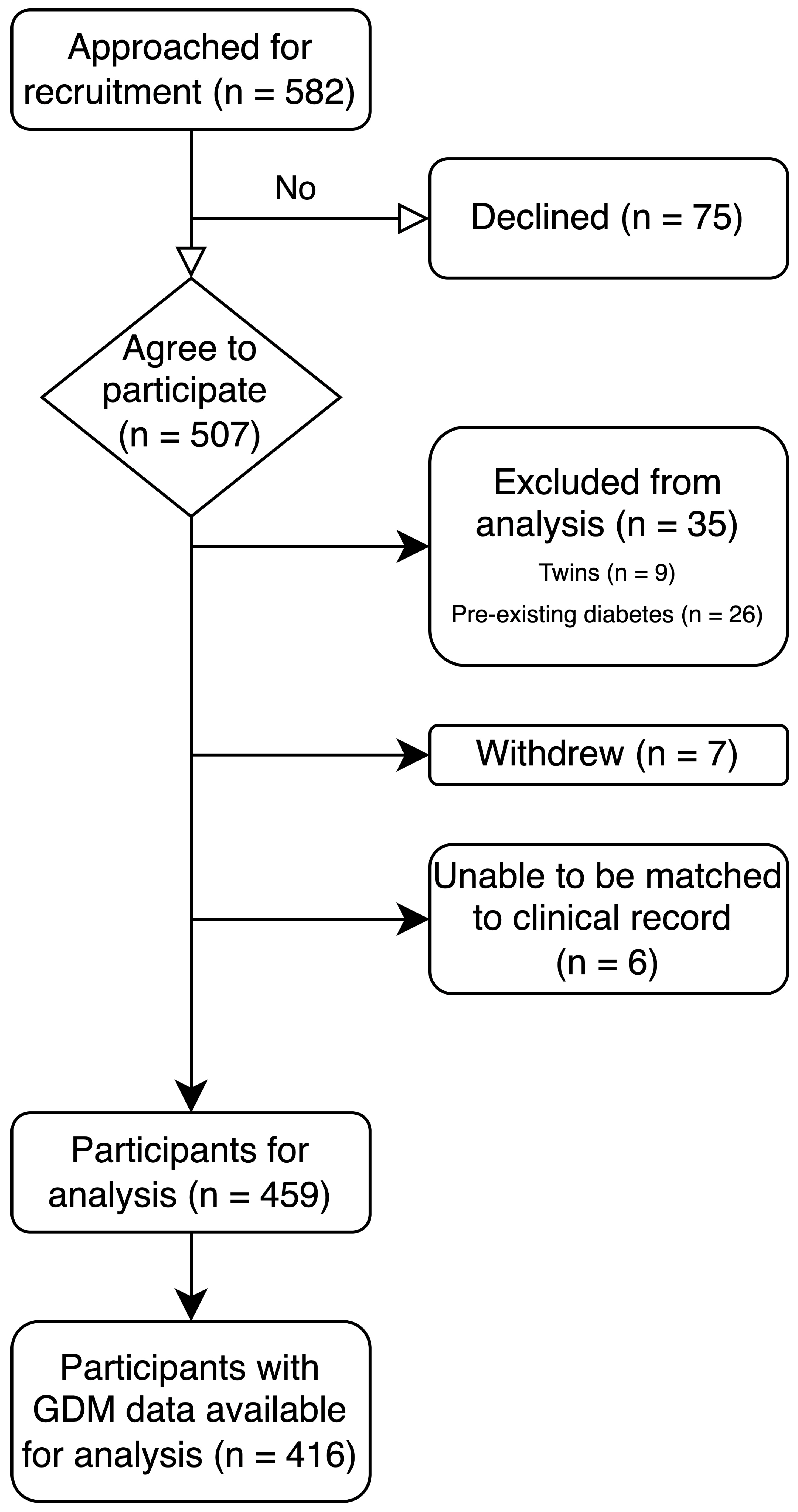
3.1. Participants
3.2. Baseline and Sociodemographic Characteristics
3.3. Physical Activity Length, Duration and Intensity
3.4. Characteristics Associated with Physical Activity Behaviours
3.5. Physical Activity Behaviours Associated with Gestational Diabetes
3.6. Physical Activity Behaviours and OGTT Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yang, X.; Li, H.; Zhao, Q.; Han, R.; Xiang, Z.; Gao, L. Clinical Practice Guidelines That Address Physical Activity and Exercise During Pregnancy: A Systematic Review. J. Midwifery Womens Health 2022, 67, 53–68. [Google Scholar] [CrossRef]
- Dipietro, L.; Evenson, K.R.; Bloodgood, B.; Sprow, K.; Troiano, R.P.; Piercy, K.L.; Vaux-Bjerke, A.; Powell, K.E. Benefits of Physical Activity during Pregnancy and Postpartum: An Umbrella Review. Med. Sci. Sports Exerc. 2019, 51, 1292–1302. [Google Scholar] [CrossRef]
- Ribeiro, M.M.; Andrade, A.; Nunes, I. Physical exercise in pregnancy: Benefits, risks and prescription. J. Perinat. Med. 2022, 50, 4–17. [Google Scholar] [CrossRef]
- Teede, H.J.; Bailey, C.; Moran, L.J.; Bahri Khomami, M.; Enticott, J.; Ranasinha, S.; Rogozinska, E.; Skouteris, H.; Boyle, J.A.; Thangaratinam, S.; et al. Association of Antenatal Diet and Physical Activity-Based Interventions With Gestational Weight Gain and Pregnancy Outcomes: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2022, 182, 106–114. [Google Scholar] [CrossRef]
- Laredo-Aguilera, J.A.; Gallardo-Bravo, M.; Rabanales-Sotos, J.A.; Cobo-Cuenca, A.I.; Carmona-Torres, J.M. Physical Activity Programs during Pregnancy Are Effective for the Control of Gestational Diabetes Mellitus. Int. J. Environ. Res. Public Health 2020, 17, 6151. [Google Scholar] [CrossRef]
- Mijatovic-Vukas, J.; Capling, L.; Cheng, S.; Stamatakis, E.; Louie, J.; Cheung, N.W.; Markovic, T.; Ross, G.; Senior, A.; Brand-Miller, J.C.; et al. Associations of Diet and Physical Activity with Risk for Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis. Nutrients 2018, 10, 698. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.; Busch, S.; Wang, R.; Sivak, A.; Davenport, M.H. Physical activity before and during pregnancy and maternal mental health: A systematic review and meta-analysis of observational studies. J. Affect. Disord. 2022, 309, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; van der Waerden, J.; Melchior, M.; Bolze, C.; El-Khoury, F.; Pryor, L. Physical activity during pregnancy and postpartum depression: Systematic review and meta-analysis. J. Affect. Disord. 2019, 246, 29–41. [Google Scholar] [CrossRef]
- Davenport, M.H.; Marchand, A.A.; Mottola, M.F.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Sobierajski, F.; James, M.; Meah, V.L.; et al. Exercise for the prevention and treatment of low back, pelvic girdle and lumbopelvic pain during pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 90–98. [Google Scholar] [CrossRef]
- Brown, J.; Ceysens, G.; Boulvain, M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database Syst. Rev. 2017, 6, CD012202. [Google Scholar] [CrossRef]
- Davenport, M.H.; Ruchat, S.M.; Poitras, V.J.; Jaramillo Garcia, A.; Gray, C.E.; Barrowman, N.; Skow, R.J.; Meah, V.L.; Riske, L.; Sobierajski, F.; et al. Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 1367–1375. [Google Scholar] [CrossRef]
- Keating, N.; Coveney, C.; McAuliffe, F.M.; Higgins, M.F. Aerobic or Resistance Exercise for Improved Glycaemic Control and Pregnancy Outcomes in Women with Gestational Diabetes Mellitus: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10791. [Google Scholar] [CrossRef]
- The International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta-analysis of individual participant data from randomised trials. BMJ 2017, 358, j3119. [Google Scholar] [CrossRef]
- Grau González, A.; Sánchez Del Pino, A.; Amezcua-Prieto, C.; Møller Luef, B.; Anne Vinter, C.; Stener Jorgensen, J.; García-Valdés, L. An umbrella review of systematic reviews on interventions of physical activity before pregnancy, during pregnancy, and postpartum to control and/or reduce weight gain. Int. J. Gynaecol. Obstet. 2024, 166, 915–931. [Google Scholar] [CrossRef]
- He, L.; Soh, K.L.; Huang, F.; Khaza’ai, H.; Geok, S.K.; Vorasiha, P.; Chen, A.; Ma, J. The impact of physical activity intervention on perinatal depression: A systematic review and meta-analysis. J. Affect. Disord. 2023, 321, 304–319. [Google Scholar] [CrossRef] [PubMed]
- Heslehurst, N.; Hayes, L.; Jones, D.; Newham, J.; Olajide, J.; McLeman, L.; McParlin, C.; de Brun, C.; Azevedo, L. The effectiveness of smoking cessation, alcohol reduction, diet and physical activity interventions in changing behaviours during pregnancy: A systematic review of systematic reviews. PLoS ONE 2020, 15, e0232774. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Magny-Normilus, C.; McMahon, E.; Whittemore, R. Systematic Review of Lifestyle Interventions for Gestational Diabetes Mellitus in Pregnancy and the Postpartum Period. J. Obs. Gynecol. Neonatal Nurs. 2022, 51, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Morales-Suárez-Varela, M.; Clemente-Bosch, E.; Peraita-Costa, I.; Llopis-Morales, A.; Martínez, I.; Llopis-González, A. Maternal Physical Activity During Pregnancy and the Effect on the Mother and Newborn: A Systematic Review. J. Phys. Act. Health 2021, 18, 130–147. [Google Scholar] [CrossRef]
- Taliento, C.; Piccolotti, I.; Sabattini, A.; Tormen, M.; Cappadona, R.; Greco, P.; Scutiero, G. Effect of Physical Activity during Pregnancy on the Risk of Hypertension Disorders and Gestational Diabetes: Evidence Generated by New RCTs and Systematic Reviews. J. Clin. Med. 2024, 13, 2198. [Google Scholar] [CrossRef]
- Fuller, H.; Moore, J.B.; Iles, M.M.; Zulyniak, M.A. Ethnic-specific associations between dietary consumption and gestational diabetes mellitus incidence: A meta-analysis. PLoS Glob. Public Health 2022, 2, e0000250. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Physical Activity During Pregnancy 2011–12; AIHW: Canberra, Australia, 2019. [Google Scholar]
- Samarawickrama, A.; Rhou, Y.J.J.; Melov, S.; Elhindi, J.; Patel, S.; Flood, V.; Smith, B.J.; Usherwood, T.; McNab, J.; McClean, M.; et al. Improving maternal and PeRinatal Outcomes aMong wOmen with and without obEsity (PROMOTE): Protocol for a prospective pregnancy cohort study. BMJ Open 2025, 15, e090930. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Gillies, J.C.P.; Dozois, D.J.A. Chapter 22—The Depression Anxiety Stress Scale: Features and applications. In The Neuroscience of Depression; Martin, C.R., Hunter, L.-A., Patel, V.B., Preedy, V.R., Rajendram, R., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 219–228. [Google Scholar]
- Australian Institute of Health and Welfare. The Active Australia Survey: A Guide and Manual for Implementation, Analysis and Reporting; AIHW: Canberra, Australia, 2003. [Google Scholar]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Nankervis, A.; McIntyre, H.D.; Moses, R.; Ross, G.P.; Callaway, L.; Porter, C.; Jeffries, W.; Boorman, C.; De Vries, B.; McElduff, A.; et al. ADIPS Consensus Guidelines for the Testing and Diagnosis of Hyperglycaemia in Pregnancy in Australia and New Zealand, Modified 2014; Australasian Diabetes in Pregnancy Society: Sydney, Australia, 2014. [Google Scholar]
- Smith, B.J.; Cheung, N.W.; Bauman, A.E.; Zehle, K.; McLean, M. Postpartum physical activity and related psychosocial factors among women with recent gestational diabetes mellitus. Diabetes Care 2005, 28, 2650–2654. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Physical Activity; AIHW: Canberra, Australia, 2024. [Google Scholar]
- Brown, W.J.; Hayman, M.; Haakstad, L.A.H.; Mielke, G.I.; Mena, G.P.; Lamerton, T.; Green, A.; Keating, S.E.; Gomes, G.A.O.; Coombes, J.S. Evidence-Based Physical Activity Guidelines for Pregnant Women. Report for the Australian Government Department of Health; Australian Government Department of Health: Canberra, Australia, 2020. [Google Scholar]
- Brown, J.; Alwan, N.A.; West, J.; Brown, S.; McKinlay, C.J.; Farrar, D.; Crowther, C.A. Lifestyle interventions for the treatment of women with gestational diabetes. Cochrane Database Syst. Rev. 2017, 5, Cd011970. [Google Scholar] [CrossRef]
- McGill, B.; Lees, D.; Salisbury, J.; Reynolds, T.; Davidson, S.; Dorney, E.; Jeong, S.Y.; O’Hara, B.J. Impact Evaluation of the Get Healthy in Pregnancy Program: Evidence of Effectiveness. Healthcare 2023, 11, 2424. [Google Scholar] [CrossRef]
- Marschner, S.; Chow, C.; Thiagalingam, A.; Simmons, D.; McClean, M.; Pasupathy, D.; Smith, B.J.; Flood, V.; Padmanabhan, S.; Melov, S.; et al. Effectiveness of a customised mobile phone text messaging intervention supported by data from activity monitors for improving lifestyle factors related to the risk of type 2 diabetes among women after gestational diabetes: Protocol for a multicentre randomised controlled trial (SMART MUMS with smart phones 2). BMJ Open 2021, 11, e054756. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Ecological Systems Theory; JAI: Greenwich, CT, USA, 1989; Volume 6. [Google Scholar]
- Tsironikos, G.I.; Zakynthinos, G.E.; Tatsioni, A.; Tsolaki, V.; Kagias, I.G.; Potamianos, P.; Bargiota, A. Gestational Metabolic Risk: A Narrative Review of Pregnancy-Related Complications and of the Effectiveness of Dietary, Exercise and Lifestyle Interventions during Pregnancy on Reducing Gestational Weight Gain and Preventing Gestational Diabetes Mellitus. J. Clin. Med. 2024, 13, 3462. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, E.; Gomersall, J.C.; Tieu, J.; Han, S.; Crowther, C.A.; Middleton, P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst. Rev. 2017, 11, Cd010443. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.; Cahalin, L.; Buman, M.; Ross, R. The current state of physical activity assessment tools. Prog. Cardiovasc. Dis. 2015, 57, 387–395. [Google Scholar] [CrossRef]
- Smith, T.O.; McKenna, M.C.; Salter, C.; Hardeman, W.; Richardson, K.; Hillsdon, M.; Hughes, C.A.; Steel, N.; Jones, A.P. A systematic review of the physical activity assessment tools used in primary care. Fam. Prac. 2017, 34, 384–391. [Google Scholar] [CrossRef]
- Althoff, T.; Sosič, R.; Hicks, J.L.; King, A.C.; Delp, S.L.; Leskovec, J. Large-scale physical activity data reveal worldwide activity inequality. Nature 2017, 547, 336–339. [Google Scholar] [CrossRef]
- Caputo, E.L.; Feter, N.; Alberton, C.L.; Leite, J.S.; Rodrigues, A.N.; Dumith, S.C.; Silva, M.C.D. Reliability of a smartphone application to measure physical activity. Res. Sports Med. 2022, 30, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, S.; Ghanvatkar, S.; Kankanhalli, A. Personalization of Intervention Timing for Physical Activity: Scoping Review. JMIR Mhealth Uhealth 2022, 10, e31327. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Long, H. The Effect of Smartphone App-Based Interventions for Patients With Hypertension: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2020, 8, e21759. [Google Scholar] [CrossRef] [PubMed]
| Maternal | All Participants (n = 459) | Participants with GDM Data Available (n = 416) | |
|---|---|---|---|
| Age, median (range) | 33 (21–43) | 32 (21–43) | |
| 20–24 years, n (%) | 21 (4.5) | 22 (5) | |
| 25–34 years, n (%) | 265 (58) | 252 (61) | |
| 35–39 years, n (%) | 143 (31) | 119 (29) | |
| 40+ years, n (%) | 30 (6.5) | 21 (5) | |
| Parity, n (%) | |||
| Para 0 | 140 (30.5) | 120 (29) | |
| Para 1 | 217 (47) | 199 (48) | |
| Para 2 | 68 (15) | 65 (16) | |
| Para 3 | 26 (6) | 25 (6) | |
| Para 4+ | 8 (1.7) | 7 (1.7) | |
| BMI kg/m2, mean (range) | 25.3 (16.8–50.9) | 26.5 (16.8–50.9) | |
| ≤18.5 | 10 (2) | 8 (2) | |
| 18.5–25 | 211 (45) | 195 (47) | |
| 25–30 | 138 (30) | 127 (31) | |
| ≥30 | 100 (22) | 86 (21) | |
| Smoking status, n (%) | 9 (2) | 9 (2) | |
| Reported alcohol use in pregnancy, n (%) | 0 (0) | 0 (0) | |
| Medical history | |||
| Hypertension, n (%) | 7 (1.5) | 6 (1.4) | |
| Diabetes | Excluded | Excluded | |
| Sociodemographic | |||
| Self-reported ethnicity, n (%) | |||
| Middle Eastern | 81 (18) | 79 (19) | |
| South-East Asian | 77 (17) | 69 (16.5) | |
| South Asian | 172 (37) | 153 (37) | |
| White | 90 (20) | 79 (19) | |
| Other | 39 (8.5) | 36 (8.7) | |
| Country of birth, n (%) | |||
| Australia | 143 (31) | 131 (33) | |
| Overseas | 316 (69) | 285 (67) | |
| Number of people in household, median (range) | 3 (1–12) | 3 (1–12) | |
| Number of children in household, median (range) | 1 (0–12) | 1 (0–12) | |
| Education level completed, n (%) | Available for 457 | Available for 414 | |
| Incomplete high school | 10 (2) | 10 (2.4) | |
| Completed high school | 38 (8.3) | 36 (8.7) | |
| TAFE * certificate/diploma | 82 (18) | 74 (18) | |
| University/tertiary institute | 317 (69) | 285 (68) | |
| Other | 4 (0.8) | 3 (0.7) | |
| Prefer not to say/did not answer | 6 (1.3) | 6 (1.4) | |
| Household income bracket AUD, n (%) | Available for 454 | Available for 411 | |
| <50,000 | 23 (5) | 22 (5) | |
| 50–100,000 | 96 (21) | 85 (20) | |
| 100–200,000 | 153 (33) | 139 (33) | |
| >200,000 | 75 (16.5) | 64 (15) | |
| Don’t know/prefer not to say | 107 (23.5) | 101 (24) | |
| Missing | 12 | 12 | |
| Pregnancy | |||
| Gestational age at recorded first visit in weeks, mean (range) | 6.2 (5–13) | 6.2 (5–13) | |
| Mode of conception, n (%) | |||
| Spontaneous | 435 (95) | 395 (94) | |
| IVF | 20 (4.4) | 17 (4) | |
| Ovulation induction | 3 (0.6) | 3 (0.7) | |
| Natural fertility services | 1 (0.2) | 1 (0.2) | |
| Edinburgh perinatal depression screening score, n (%) | Available for 455 | Available for 412 | |
| Score range 0–9 | 406 (89) | 371 (90) | |
| Score range 10–12 | 31 (7) | 27 (6.5) | |
| Score range ≥ 13 or response to Q10 on self-harm | 18 (4) | 14 (3.4) | |
| History of GDM, n (%) | 63 (18) # | 54 (18) # |
| Physical Activity Levels | n (%) | |
|---|---|---|
| By Category | Sufficiently active | 179 (39) |
| Low active | 206 (45) | |
| Inactive | 73 (16) | |
| By Intensity | Any walking | 430 (94) |
| Any moderate | 85 (19) | |
| Any vigorous | 74 (16) | |
| Any moderate/vigorous | 133 (25) |
| Physical Activity Levels | GDM (n = 104; 25%) | NO GDM (n = 312; 75%) | p | |
|---|---|---|---|---|
| By Category | Inactive | 15 (14%) | 51 (16%) | 0.624 |
| Low active | 51 (49%) | 136 (44%) | ||
| Sufficiently active | 38 (37%) | 125 (40%) | ||
| By Duration | Total exercise (minutes per week) | 113 (40–195) | 120 (30–240) | 0.671 |
| Walking (minutes per week) | 80 (30–180) | 90 (30–180) | 0.915 | |
| By Intensity | Walking (any) | 89 (86%) | 278 (89%) | 0.429 |
| Moderate (any) | 15 (14%) | 60 (19%) | 0.338 | |
| Vigorous (any) | 10 (10%) | 53 (17%) | 0.097 | |
| Moderate/vigorous (any) | 21 (20%) | 95 (30%) | 0.058 |
| Physical Activity Levels | Unadjusted | Adjusted * | |||
|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | ||
| By Category | Inactive | Ref. | Ref. | Ref. | Ref. |
| Low active | 1.28 (0.67–2.53) | 0.470 | 1.07 (0.55–2.19) | 0.839 | |
| Sufficiently active | 1.03 (0.53–2.09) | 0.924 | 0.90 (0.45–1.87) | 0.782 | |
| By Intensity | Any walking | 0.73 (0.38–1.43) | 0.336 | 0.63 (0.32–1.28) | 0.185 |
| Any moderate | 0.71 (0.37–1.28) | 0.271 | 0.70 (0.36–1.30) | 0.275 | |
| Any vigorous | 0.52 (0.24–1.02) | 0.073 | 0.59 (0.27–1.20) | 0.165 | |
| Any moderate or vigorous | 0.58 (0.33–0.97) | 0.045 | 0.59 (0.33–1.01) | 0.061 |
| Physical Activity Level | Fasting Glucose | 1 Hour Glucose | 2 Hour Glucose | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| By Category | p = 0.096 | p = 0.125 | p = 0.665 | |
| Inactive | 4.32 (0.52) | 7.80 (2.16) | 6.65 (1.79) | |
| Low active | 4.47 (0.49) | 8.21 (2.12) | 6.86 (1.93) | |
| Sufficiently active | 4.44 (0.41) | 7.79 (1.85) | 6.72 (1.77) | |
| By Intensity | Any walking | p = 0.292 | p = 0.559 | p = 0.708 |
| Yes | 4.44 (0.47) | 7.96 (2.02) | 6.76 (1.85) | |
| No | 4.37 (0.44) | 8.16 (2.14) | 6.87 (1.81) | |
| Any moderate | p = 0.245 | p = 0.369 | p = 0.428 | |
| Yes | 4.38 (0.42) | 7.78 (2.04) | 6.62 (1.81) | |
| No | 4.44 (0.47) | 8.02 (2.03) | 6.81 (1.86) | |
| Any vigorous | p = 0.409 | p < 0.001 | p = 0.316 | |
| Yes | 4.39 (0.38) | 7.25 (1.68) | 6.59 (1.52) | |
| No | 4.44 (0.48) | 8.11 (2.07) | 6.81 (1.90) | |
| Any moderate or vigorous? | p = 0.187 | p = 0.002 | p = 0.109 | |
| Yes | 4.39 (0.38) | 7.49 (1.87) | 6.55 (1.66) | |
| No | 4.45 (0.49) | 8.17 (2.06) | 6.86 (1.91) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samarawickrama, A.; Elhindi, J.; Rhou, Y.J.J.; Melov, S.J.; Flood, V.; McNab, J.; McLean, M.; Cheung, N.W.; Smith, B.J.; Usherwood, T.; et al. Association Between Intensity of Physical Activity in Pregnancy and Gestational Diabetes in a Multi-Ethnic Population: Results from the PROMOTE Cohort Study. Nutrients 2025, 17, 3500. https://doi.org/10.3390/nu17223500
Samarawickrama A, Elhindi J, Rhou YJJ, Melov SJ, Flood V, McNab J, McLean M, Cheung NW, Smith BJ, Usherwood T, et al. Association Between Intensity of Physical Activity in Pregnancy and Gestational Diabetes in a Multi-Ethnic Population: Results from the PROMOTE Cohort Study. Nutrients. 2025; 17(22):3500. https://doi.org/10.3390/nu17223500
Chicago/Turabian StyleSamarawickrama, Ania (Lucewicz), James Elhindi, Yoon Ji Jina Rhou, Sarah J. Melov, Vicki Flood, Justin McNab, Mark McLean, Ngai Wah Cheung, Ben J. Smith, Tim Usherwood, and et al. 2025. "Association Between Intensity of Physical Activity in Pregnancy and Gestational Diabetes in a Multi-Ethnic Population: Results from the PROMOTE Cohort Study" Nutrients 17, no. 22: 3500. https://doi.org/10.3390/nu17223500
APA StyleSamarawickrama, A., Elhindi, J., Rhou, Y. J. J., Melov, S. J., Flood, V., McNab, J., McLean, M., Cheung, N. W., Smith, B. J., Usherwood, T., Pasupathy, D., & on behalf of the PROMOTE Study Team. (2025). Association Between Intensity of Physical Activity in Pregnancy and Gestational Diabetes in a Multi-Ethnic Population: Results from the PROMOTE Cohort Study. Nutrients, 17(22), 3500. https://doi.org/10.3390/nu17223500







