Abstract
Background. The literature suggests that deficits in mentalization, operationalized as reflective functioning, are associated with emotional and behavioral dysregulation, including emotional eating and uncontrolled eating. These eating behaviors may be intensified by food addiction, yet its moderating role within this framework has not been thoroughly investigated. This study examined whether the relationship between deficits in reflective functioning and uncontrolled eating is mediated by emotional eating, and whether food addiction diagnosis moderates this pathway. Methods. A cross-sectional survey was administered to 559 adults from the general population. Participants completed self-report measures assessing reflective functioning (RFQ-8), emotional and uncontrolled eating (TFEQ-R-18), and food addiction (YFAS 2.0). A moderated mediation model was tested using conditional process analysis with 10,000 bootstrap resamples. Results. Deficits in reflective functioning were positively associated with emotional eating (β = 0.155, p < 0.001), which in turn were associated with uncontrolled eating (β = 1.314, p < 0.001). Food addiction diagnosis significantly moderated the relationship between emotional eating and uncontrolled eating (β = 0.744, p < 0.001). Specifically, individuals with food addiction exhibited a stronger association between emotional eating and uncontrolled eating compared to those without food addiction. The indirect effect from reflective functioning to uncontrolled eating via emotional eating was significantly stronger among individuals with food addiction than those without. The overall model explained 57.3% of the variance in uncontrolled eating. Conclusions. Food addiction diagnosis amplifies the pathway from emotional eating to uncontrolled eating, originating from deficits in reflective functioning. These findings highlight the clinical importance of targeting mentalization processes and emotional eating in interventions for disordered eating behaviors, particularly among individuals with food addiction.
1. Introduction
Disordered eating behaviors involving excessive food intake encompass a spectrum of atypical eating patterns characterized by dysfunctional responses to food-related cues, which can lead to harmful consequences, such as overweight, obesity and cardiovascular issues [1,2]. Often, these maladaptive eating patterns appear to be linked by certain recurring transdiagnostic factors (e.g., emotion dysregulation, impulsivity, childhood trauma) [3,4], as well as by behaviors, signs, and symptoms associated with a possible addiction to food and eating [5]. Research on eating behaviors has identified various forms of excessive consumption, ranging from persistent, repetitive, and compulsive grazing to episodes of overeating and binge eating [5,6,7,8].
Scientific studies highlighted that the development and maintenance of disordered eating behaviors are multifaceted, resulting from a complex interplay of genetic, behavioral, social, and psychological factors [9,10,11,12]: the literature has identified numerous risk factors and triggering cues [13,14], although the nature of their interrelationships and their specific contributions remain not fully understood.
According to infancy research and the attachment theory, previous studies have identified several risk factors for disordered eating behaviors, particularly early traumatic experiences such as emotional maltreatment [15,16,17,18,19] and insecure attachment to primary caregivers [15,20,21]. These early traumatic adversities are consistently linked to a heightened vulnerability to disordered eating patterns [15,17]. Individuals exposed to such experiences often develop attachment insecurities, which are associated with both eating-related difficulties [20,22] and broader psychopathology [23,24]. The literature indicates that childhood maltreatment may disrupt the attachment system [25,26], leading to impaired self-regulation and a fragmented sense of self due to emotionally mis-attuned caregiver relationships (i.e., insecure attachment) [27,28,29,30,31]—that would normally allow the child to use the parent as a secure base. Furthermore, these relational disruptions can hinder the development of core interpersonal capacities, including mentalization [25,32,33].
The construct of mentalization, often referred to as reflective functioning, is closely tied to early child–caregiver relationships [34,35]. Reflective functioning refers to the ability to interpret and make sense of one’s own behavior and that of others by attributing it to underlying mental states, including emotions, thoughts, intentions, and desires [36]. More specifically, reflective functioning involves understanding human actions by attributing them to underlying mental states such as thoughts, beliefs, feelings, and emotions [37,38]. This capacity enables individuals to ascribe meaning to others’ behaviors and experiences without relying entirely on external validation or cues [36,37].
However, when reflective functioning is underdeveloped or impaired, this foundational interpersonal capacity remains compromised [37]. Reflective functioning, when dysfunctional, can be seen as an automatic and unconscious process that negatively affects a person’s ability to interpret and regulate behavior [39], undermining the individual’s capacity to inhibit impulsive or dysregulated responses, particularly in emotionally charged situations [40]. Uncertain or impaired mentalization is often associated with poor emotion regulation difficulties with self-monitoring, impulse control, and a disrupted sense of self-agency [37,41,42,43]. A compromised reflective function often results in a rigid, distorted understanding of mental states leading individuals experiencing reality in a different, prementalized manner [15,25,44]. In such states, people experience a breakdown between internal feelings and external reality [25,44], especially during times of distress, making it difficult to distinguish between emotional experiences and actual events [28,40]. In these cases, internal states are perceived as disorganizing and overwhelming [28,37].
Consequently, individuals with impaired reflective functioning may seek to defend themselves from these distressing or threatening emotions [39,45,46] by relying on maladaptive coping strategies [41,42,47] that provide an immediate relief [32,48]—such as emotionally driven, compulsive, disordered eating behaviors [7,49,50].
Previous research has identified failures in reflective functioning as a key feature in individuals with disordered eating behaviors [15,17,51,52], including emotional eating, overeating, and loss of control over eating. So, in response to emotionally distressing or psychologically dysregulating experiences, these individuals may turn toward more tangible or bodily-based coping strategies (e.g., focusing on their physical body) [15] or external regulators such as food [51,53], in a compensatory effort to manage psychological and emotional discomfort and restore a sense of balance.
Thus, when faced with internal states perceived as aversive—such as anxiety, anger, intrusive thoughts, or feelings of uncontrollability—individuals with low reflective functioning may resort to impulsive and emotionally-driven eating behaviors.
Indeed, as levels of psychological stress or arousal increase, these individuals tend to rely on more primitive, unconscious, and automatic regulation strategies that promise immediate relief [32,48]—such as substance use or compulsive, emotionally driven eating behaviors. In these situations, the urge to escape intolerable emotional states can culminate in emotional eating [54,55,56] that consists in a powerful, overwhelming compulsion to eat (see e.g., [57,58]). Consequently, the more this emotion regulation strategy is effective in proving relief to discomfort, the more the individual will rely on it, and the more this process will tend to be reinforced and maintained [17]. This, in turn, may potentially lead the individual to develop a dependence/addiction on this external regulator (in this case, food) for emotion regulation, reinforcing dysfunctional emotional eating behaviors.
However, when highly stressful or traumatic events occur, individuals may feel engulfed by unbearable affective states and milder emotional regulation strategies—like emotional eating—prove to be insufficient [25,46]. As a result, they may turn to more intense and maladaptive responses—such as binge eating or compulsive, uncontrolled eating—in an attempt to fully suppress or numb the intense negative emotional experience [49,59,60,61]. These uncontrolled eating behaviors differ from emotional eating in their severity because they imply the loss of control over eating.
However, the relationship from emotional eating to uncontrolled eating may be influenced by another key construct, food addiction (FA), which could foster engagement in dysregulated eating behaviors [49] and which in recent years has gained increasing attention in both clinical practice and research related to eating disorders and dysfunctional eating behaviors [62,63,64,65]. Recent research has highlighted that certain individuals may develop signs of addiction to highly palatable and processed foods (HPFs) high in sugar, fat, and salt [66,67,68], which are particularly activating for brain circuits and neurotransmitters involved in reward and pleasure, similar to brain circuitry implicated in substance addiction [69,70,71,72].
Individuals diagnosed with FA may exhibit the core behavioral patterns typically associated with addiction—such as tolerance, withdrawal, and craving—which in turn may foster, reinforce, and maintain overeating and uncontrolled food intake behaviors [17,49]. FA appears to be a highly complex and multifaceted construct, it encompasses several facets, including impulsivity, emotional dysregulation, and poor dietary control [60,73,74,75]. FA also appears to have a transdiagnostic nature; it is observed in individuals with anorexia nervosa, bulimia nervosa, and binge eating disorder, as well as in clinical populations and in the general population [76]. It should also be acknowledged that food addiction is not confined to evident episodes of binge eating or overeating; it may also appear in more subtle and ongoing behaviors, such as grazing [6,7].
However, FA is still relatively poorly understood, as its etiology remains largely unclear [5]. Some recent studies have linked FA to experiences of physical, sexual, and emotional trauma during childhood [17,77,78,79]. Furthermore, a recent study by Rossi et al. (2025) has also associated FA with deficits in individuals’ reflective functioning [17].
Studies show that individuals diagnosed with FA—both from clinical samples and the general population—tend to exhibit a greater number and intensity of dysregulated eating behaviors compared to those without a diagnosis [80].
Relying on this evidence, it is therefore plausible to hypothesize that the strength of the association between emotional eating and uncontrolled eating may be moderated by the presence of an FA diagnosis. In other words, the strength of the relationship between emotional eating and uncontrolled eating may be moderated by whether or not the individual is diagnosed with FA.
However, this hypothesis still lacks robust empirical validation. Indeed, despite the extensive literature, the relationship between maladaptive eating behaviors and FA remains not fully understood—especially when considering early experiences with caregivers during childhood. Moreover, previous studies have often overlooked the underlying mechanisms that might link psychological factors rooted in early development (such as mentalization/reflective functioning), uncontrolled eating behaviors, and FA.
Consequently, based on these theoretical premises, the present research aims to examine a moderated mediation model in which deficits in reflective functioning (X) predict uncontrolled eating behaviors (Y) through emotional eating (M), with the presence of a FA diagnosis (W) moderating the whole model—this being the primary hypothesis. This model seeks to clarify how impaired mentalization may lead to maladaptive eating patterns and explore the amplifying effect of FA on these relationship.
H1.
Deficits in reflective functioning, dysfunctional eating behaviors (emotional eating and uncontrolled eating), and FA diagnosis are positively correlated;
H2.
Individuals diagnosed with FA will show higher levels of reflective functioning deficits, emotional eating and uncontrolled eating;
H3.
FA diagnosis will moderate the mediation model.
In other words, this study aimed to examine whether the relationship from (deficits in) reflective functioning to uncontrolled eating is mediated by emotional eating and whether this mediation pathway is moderated by the presence of a FA diagnosis. Specifically, it was hypothesized that individuals with greater deficits in reflective functioning would show increased emotional eating behaviors, which would in turn predict higher levels of uncontrolled eating. Furthermore, it was expected that the presence of a FA diagnosis would strengthen the association between emotional eating and uncontrolled eating, thereby amplifying the indirect pathway from (deficits in) reflective functioning to uncontrolled eating behaviors. With exploratory aims, the moderating effect of FA was also tested from (deficits in) reflective functioning to emotional eating, and from (deficits in) reflective functioning to uncontrolled eating.
2. Methods and Materials
2.1. Procedure
Participants were recruited from the general population using a snowball sampling approach [81], primarily through social media platforms, in line with previous studies [50,73,82]. To be eligible, individuals had to meet the following criteria: (A) be 18 years of age or older, (B) have Italian as their native language, (C) provide fully completed responses, and (D) signed and submit an online informed consent form. Ethical approval for the study was granted by the Ethics Committee of the University of Padua (protocol number 3558).
2.2. Sample Size Determination
The required sample size was determined a priori using a Monte Carlo simulation conducted in R (v 4.3.2), following general recommendations for power analysis in path analysis according to Muthén and Muthén (2002) [83]. The model specified a moderated mediation structure, including conditional indirect effect depending on the level of a binary moderator (0 = no FA, 1 = presence of FA). In line with previous studies (e.g., [15,17,49]) and the guidelines of Cohen (1988), path coefficients were set to small-to-moderate standardized values [84]. A Type I error rate (α) of 0.05 was adopted, and the desired statistical power (1 − β) was set to 0.80 [84]. Datasets were generated and analyzed using the lavaan package in R. Results indicated that a minimum sample size of 350 participants would yield an estimated power of 0.82 to detect the moderated indirect effect.
2.3. Measures
A demographic questionnaire was administered to gather information on participants’ age, biological sex, educational attainment, marital status, and employment status. Participants were also asked to report whether they had received a diagnosis of an eating disorder (ED) and to provide their weight and height, which were used to compute their body mass index (BMI).
2.3.1. Reflective Functioning Questionnaire 8 (RFQ-8)
The RFQ-8 [85] was utilized to measure participants’ mentalization operationalized as reflective functioning—i.e., their ability to understand their own and others’ mental states. This instrument includes 8 items rated on a 7-point Likert scale, from “completely disagree” (=1) to “completely agree” (=7), asking respondents to indicate their agreement with statements about mentalizing abilities. The RFQ-8 assesses two contrasting aspects: certainty and uncertainty about mental states. In this study, the uncertainty scale (RFQ8u) was used to capture deficits in mentalization/reflective functioning, with higher scores indicating greater impairment. The Italian version of the RFQ-8 [86] was employed, demonstrating good internal consistency: RFQ8u, McDonald’s omega = 0.791.
2.3.2. The Three-Factor Eating Questionnaire Revised 18 (TFEQ-R-18)
The TFEQ-R-18 [87] was use to assess key cognitive and behavioral dimensions associated with eating behaviors: cognitive restraint (CR), uncontrolled eating (UE), and emotional eating (EE). It consists of 18 items, each rated on a 4-point Likert scale, where higher scores reflect greater tendencies in the respective domains. The CR subscale captures individuals’ efforts and preoccupations with regulating their food intake to control body weight and shape—consequently, since its content was not relevant to the aims of the present study, this subscale was not used for the statistical analyses. The EE subscale measures the tendency to eat in response to emotional states, whether positive or negative, such as distress or other negative emotions. The UE subscale, on the other hand, assesses the difficulty in maintaining control over eating behaviors, often leading to overeating episodes. For this research, the Italian adaptation of the TFEQ-R-18 was employed [88]. The internal consistency, evaluated through McDonald’s omega, was 0.870 for the EE subscale and 0.822 for the UE subscale.
2.3.3. The Yale Food Addiction Scale 2.0 (YFAS 2.0)
The YFAS 2.0 [80,89] is a self-report instrument developed to assess the occurrence of FA symptoms over the previous 12 months. It includes 35 items rated on an 8-point Likert scale and is based on the DSM-5 criteria for substance use disorders (SUD) [62]. In particular, diagnostic criteria are: (A) consumed larger amount and for a longer period than intended; (B) much time/activity to obtain, use, recover; (C) social activities given up or reduced; (D) withdrawal symptoms; (E) Failure to fulfil major role obligation; (F) use despite knowledge of adverse consequences; (G) tolerance; (H) craving; (I) persistent desire or unsuccessful attempts to quit; (J) use in physically hazardous situations; (K) Social or interpersonal problems. FA can be evaluated through two scoring methods: (I) the symptom count, which tallies the number of criteria met, and (II) the diagnostic score, which classifies severity into No FA, mild, moderate, or severe FA depending on the level of impairment or distress. According to previous research [80], in this study, the aggregated diagnostic score was used. Thus, participants were classified as (A) non-food addicted (i.e., No FA = 0) or (B) food addicted (mild, moderate and severe FA = 1). The Italian version of the YFAS 2.0 [80,90] was used, showing good internal consistency: McDonald’s omega for categorical data = 0.875.
2.4. Statistical Analysis
Statistical analyses were performed with the R software (v. 4.3.2). The following packages were used: interactions, lavaan, lme4, process for R, psych, and tidyverse.
First (H1), the Pearson correlation coefficient (r) was computed to evaluate the strength of the relationships between variables [91,92] and interpreted using Cohen’s benchmarks [84]: r < 0.10, trivial; r from 0.10 to 0.30, small; r from 0.30 to 0.50, moderate; r > 0.50, large.
Second (H2), a Multivariate Analysis of Variance (MANOVA) was conducted to explore potential differences across FA diagnosis groups (No diagnosis of FA vs. FA Diagnosis—independent variable) on the three scales of the mediation model (i.e., reflective functioning, emotional eating, and uncontrolled eating—dependent variables) considered simultaneously. Wilks’ Lambda (Λ) was used to evaluate the overall multivariate effect [91,93] and interpreted using partial eta squared (η2p), classified as small (0.011–0.059), moderate (0.060–0.139), or large (>0.140). Effect sizes for bivariate comparisons were interpreted using Hedge’s g (g), classified as small (≈0.2), moderate (≈0.50), or large (≈0.80) [84].
Third (H3), in line with previous studies, before testing the hypothesized conditional process model (moderated mediation), preliminary analyses were performed. Then, a conditional process analysis (moderated mediation; 10,000 bootstrap resamples) with observed variables was performed [92,94,95,96,97,98,99]. The maximum likelihood (ML) estimator was used to conduct the statistical analyses. Following previous studies, two analytical steps were carried out. First, a simple mediation model was specified: ‘(deficits in) reflective functioning’ (X) was hypothesized to influence ‘uncontrolled eating’ (Y) through ‘emotional eating’ (M). Second, a conditional process model was tested: while maintaining the same mediation structure, the path from ‘emotional eating’ (M) to ‘uncontrolled eating’ (Y) was moderated by ‘(diagnosis of) FA’ (W), a binary variable coded as absence (=0) versus presence (=1) of FA diagnosis [92,100,101,102] (see Figure 1).
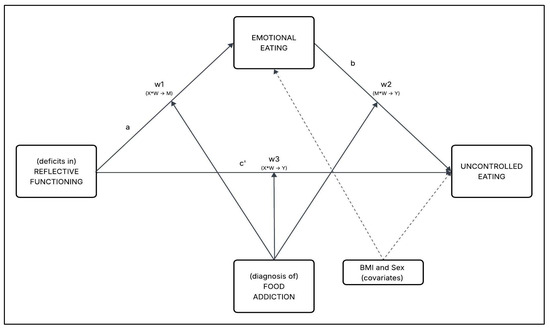
Figure 1.
Path model–conceptual representation.
The moderating effect of ‘(diagnosis of) FA’ (W) was examined by estimating the conditional effects at each level of the moderator (W = 0 and W = 1) within a single conditional process model, using 95% confidence intervals (95%CI) [92,95]. Given the categorical nature of the moderator, the analyses focused on comparing the magnitude and significance of the direct and indirect effects across the two groups. The interaction term between ‘emotional eating’ (M) and ‘(diagnosis of) food addiction’ (W) was specifically tested to assess whether the effects on ‘uncontrolled eating’ (Y) differed depending on the presence (W = 1) or absence (W = 0) of the FA diagnosis. Lastly, the index of moderated mediation (IMM) was computed to assess the difference between the two conditional indirect effects. All regression coefficients reported in the results section are unstandardized (β) for sake of interpretability.
3. Results
3.1. Participants
A sample of 559 participants were recruited. The sample comprised 162 males (29%) and 397 females (71%), aged from 18 to 72 years (mean = 34.87, SD = 14.98) and a BMI ranging from 15.62 to 50.68 (mean = 23.11; SD = 4.15). Further details are reported in Table 1.
3.2. Preliminary Analysis
Before testing the main hypotheses, the prevalence of food addiction and bivariate associations among study variables was examined. In accordance with the YFAS 2.0 scoring procedure, out of the total sample, 69 (12.3%) participants had a diagnosis of FA, while 490 (87.7%) participants did not have a diagnosis of FA.
The correlation analyses showed that the psychological variables included in the moderated mediation model were positively associated, supporting hypothesis 1 (H1)—as shown in Table 2. Moreover, all correlation values remained below the critical threshold of |0.80| and permitting the continuation of the statistical analyses. As hypothesized, deficits in reflective functioning were positively associated with emotional eating (r = 0.278, p < 0.001), uncontrolled eating (r = 0.259, p < 0.001), and FA symptoms (r = 0.222, p < 0.001). Furthermore, consistent with the literature, variables related to dysfunctional eating behavior were positively associated with each other—with a moderate to strong effect size. Indeed, emotional eating was positively associated with uncontrolled eating (r = 0.721, p < 0.001), and FA symptoms (r = 0.485, p < 0.001). Lastly, uncontrolled eating was positively associated with FA symptoms (r = 0.505, p < 0.001). These preliminary findings confirmed the appropriateness of including all variables in the subsequent moderated mediation model.

Table 1.
Samples descriptive statistics.
Table 1.
Samples descriptive statistics.
| Descriptives | ||
|---|---|---|
| Age (M, SD) | 34.87 | 14.98 |
| BMI (M, SD) | 23.11 | 4.15 |
| Gender (n, %) | ||
| Male | 162 | 29% |
| Female | 397 | 71% |
| Civil Status (n, %) | ||
| Single | 181 | 32.4% |
| In a relationship | 210 | 37.6% |
| Married | 136 | 24.3% |
| Separated/divorced | 22 | 3.9% |
| Widowed | 10 | 1.8% |
| Education (n, %) | ||
| Middle school degree | 37 | 6.6% |
| High school degree | 220 | 39.4% |
| Bachelor degree | 268 | 47.9% |
| Master/Ph.D. | 34 | 6.1% |
| Work Status (n, %) | ||
| Student | 227 | 40.6% |
| Full-time worker | 198 | 35.4% |
| Part-time worker | 42 | 7.5% |
| Entrepreneurs | 47 | 8.4% |
| Unemployed | 11 | 2.0% |
| Retired | 34 | 6.1% |
| BMI Class (n, %) | ||
| Severely underweight (<16) | 1 | 0.2% |
| Underweight (16–18.49) | 37 | 6.6% |
| Normal weight (18.5–24.99) | 387 | 69.2% |
| Overweight (25–29.99) | 99 | 17.7% |
| Class I obesity (30–34.99) | 29 | 5.2% |
| Class II obesity (35–39.99) | 3 | 0.5% |
| Class III obesity (>40) | 3 | 0.5% |
| ED Diagnosis (n, %) | ||
| No ED | 508 | 90.8% |
| Anorexia Nervosa | 22 | 3.9% |
| Bulimia Nervosa | 10 | 1.8% |
| Binge Eating Disorder | 12 | 2.1% |
| ED No Otherwise Specified | 7 | 1.3% |
Note: M = mean; SD = standard deviation; n = number of individual in each category; % percentage.

Table 2.
Descriptive statistics, correlations among variables.
Table 2.
Descriptive statistics, correlations among variables.
| Descriptives | Correlations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | SK | K | 1 | 2 | 3 | 4 | 5 | ||
| 1 | (deficits in) Reflective functioning | 2.63 | 3.28 | 1.66 | 2.82 | - | ||||
| 2 | Emotional eating | 6.30 | 2.59 | 0.39 | −0.83 | 0.278 | - | |||
| 3 | Uncontrolled eating | 17.50 | 5.74 | 0.64 | −0.26 | 0.259 | 0.721 | - | ||
| 4 | YFAS2 Symptom Count | 1.35 | 2.35 | 2.02 | 3.49 | 0.222 | 0.485 | 0.505 | - | |
| 5 | Body Mass Index | 23.11 | 4.15 | 1.77 | 6.11 | 0.062 § | 0.273 | 0.204 | 0.289 | - |
Note: all correlations are statistically significant with p < 0.001, except for § p > 0.050 ns. M = mean, SD = standard deviation, SK = skewness, K = kurtosis.
3.3. MANOVA Results
The raw score of each variable was almost normally distributed and their relationships were substantially linear. The Box’s M was statistically significant (M = 31.304, F = 5.132, p < 0.001)—however, it should be noted that MANOVA is robust to violations of assumptions [91,93]. Thus, considering these results, the MANOVA was performed. A statistically significant multivariate effect was found: Λ = 0.752, F = 60.998, p < 0.001; η2p = 0.248 (large effect size). In line with Hypothesis 2 (H2), a statistically significant between groups difference for the RFQ8u scale [t = −5.775, p < 0.001; g = −0.742 (moderate effect size)], the emotional eating scale of the TEFRQ-18 [t = −10.786, p < 0.001; g = −1.385 (large effect size)], and the uncontrolled eating scale of the TEFRQ-18 [t = −12.742, p < 0.001; g = −1.636 (large effect size)]. Results are reported in Table 3 and Figure 2. Overall, these findings indicate that individuals with a diagnosis of FA exhibited significantly higher levels of reflective functioning deficits, emotional eating, and uncontrolled eating compared to those without FA diagnosis, with effect sizes ranging from moderate to large.

Table 3.
MANOVA results.
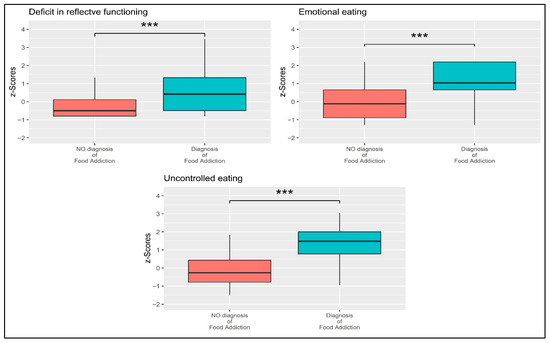
Figure 2.
Boxplots showing the mean differences between participants without and with a diagnosis of FA. Note: *** = p < 0.001.
3.4. Moderated Mediation Analysis
To test the main hypothesis (H3), a conditional process analysis was conducted to examine whether the relationship between reflective functioning deficits and uncontrolled eating is mediated by emotional eating, and whether this mediation pathway is moderated by the presence of a FA diagnosis. The moderated mediation analysis (Figure 3) supported the hypothesized results, as detailed below and summarized in Table 4.
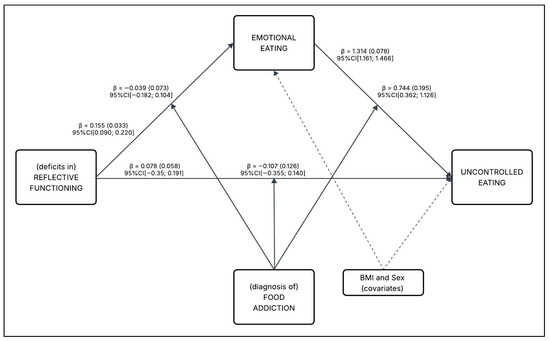
Figure 3.
Path model with unstandardized regression coefficients, standard errors, and 95% confidence intervals.

Table 4.
Summary of standardized (β*) and unstandardized (β) parameter estimates with 95% Confidence Intervals of the tested model (Figure 3).
3.4.1. Direct Effects and Main Associations
The direct paths in the model were first examined, controlling for covariates. As hypothesized, (deficits in) reflective functioning (X) were positively associated with emotional eating (M), path a: β = 0.155 (SE = 0.033), 95%CI [0.090; 0.220]. This indicates that greater deficits in reflective functioning were associated with higher levels of emotional eating. In addition, diagnosis of FA (W) was statistically associated (main effect) with emotional eating (M), path v1: β = 2.516 (SE = 0.431), 95%CI [1.669; 3.364]. This suggests that a FA diagnosis was associated with increased emotional eating, independent of reflective functioning.
Moreover, emotional eating (M) statistically positively predicted uncontrolled eating (Y), path b: β = 1.314 (SE = 0.078), 95%CI [1.161; 1.466]. This strong association confirms that higher emotional eating was linked to greater uncontrolled eating behaviors. However, diagnosis of FA (W) was not statistically associated (main effect) with uncontrolled eating (Y), path v2: β = −2.236 (SE = 1.753), 95%CI[−5.679; 1.207].
At the same time, controlling for emotional eating (M), (deficit in) reflective functioning (X) was no more statistically associated with uncontrolled eating (Y), path c’: β = 0.078 (SE = 0.058), 95%CI[−0.035; 0.191]—suggesting a complete mediation, wherein the effect of reflective functioning on uncontrolled eating was fully explained through emotional eating. The full model (including all direct effects, covariates, and interactions) explained 57.3% of the variance in uncontrolled eating (R2 = 0.573).
3.4.2. Moderation Effects
Whether FA diagnosis moderated any of the pathways in the model was then tested. Out of the three interactions performed (w1, w2, w3), only the interaction between emotional eating (M) and diagnosis of FA (W) on uncontrolled eating (Y) was statistically significant (path w2: β = 0.744 (SE = 0.195), 95%CI [0.362; 1.126]). This indicates that the strength of the relationship between emotional eating and uncontrolled eating was dependent on whether a FA diagnosis was present. The non-significant interactions (w1 and w3) are detailed in Section 3.5.
3.4.3. Conditional Indirect Effects
Finally, the indirect effects of reflective functioning on uncontrolled eating through emotional eating were examined separately for individuals with and without FA diagnosis. Considering the presence of a dichotomous moderator—namely, the diagnosis of FA (0 = absent vs. 1 = present)—the moderated mediation analysis yielded two distinct indirect effects [(deficit in) reflective functioning → emotional eating → uncontrolled eating], one for each level of the moderator.
Considering the overall model—thus, including also the non-statistically significant interactions (paths w1 and w3)—when the moderator was equal to 0 (=FA diagnosis: absent) the total indirect effect was: β = 0.204 (SE = 0.046), 95%CI [0.119; 0.300]. Conversely, when the moderator was equal to 1 (=FA diagnosis: endorsed) the total indirect effect was: β = 0.239 (SE = 0.125), 95%CI [0.006; 0.498]. The IMM test for the difference between both conditional indirect effects (including the three moderations—w1, w2, w3) of the overall model was equal to 0.035 (0.133), 95%CI[−0.214; 0.309]—meaning that no difference between the conditional indirect effects was observed because two out of three moderations were not statistically significant.
However, given that only one moderation was significant, the model was respecified to include only the statistically significant interaction (path w2). In this more parsimonious model, when the moderator was equal to 0 (=FA diagnosis: absent) the total indirect effect was: β = 0.262 (SE = 0.043), 95%CI [0.183; 0.353]. Conversely, when the moderator was equal to 1 (=FA diagnosis: endorsed) the total indirect effect was: β = 0.402 (SE = 0.069), 95%CI [0.276; 0.544]. The IMM of this respecified model was equal to 0.141 (0.043), 95%CI [0.060; 0.229], suggesting that the indirect effect was significantly stronger when the FA diagnosis was endorsed. In practical terms, the pathway from reflective functioning deficits to uncontrolled eating (via emotional eating) was amplified by approximately 53% in individuals with FA diagnosis compared to those without.
3.5. Probing Interaction
Considering the whole model, the simple slope analysis was used to deepen the moderation effect of the conditional process model presented in Figure 1 and Figure 3.
The moderation analyses for w1 and w3 examined the effect of FA diagnosis (W) as a moderator. Specifically, w1 tested the relationship from (deficits in) reflective functioning (X) to emotional eating (M), controlling for covariates, while w3 tested the relationship from X to uncontrolled eating (Y), controlling for M and covariates. Both interactions were not statistically significant (w1: β = −0.039, SE = 0.073, 95%CI [−0.182; 0.104]; w3: β = −0.107, SE = 0.126, 95%CI [−0.355; 0.140]) and were therefore not further examined. This indicates that the effects of (deficits in) reflective functioning on emotional eating and uncontrolled eating were not conditioned by FA diagnosis.
Conversely, the moderation analysis (w2) involved the moderating effect of the diagnosis of FA (W) on the relationship between emotional eating (M) and uncontrolled eating (Y), controlling for (deficit in) reflective functioning (X) and covariates: β = 0.744 (SE = 0.195) 95%CI [0.362; 1.126]. The change in explained variance (ΔR2) of the moderated mediation model due to this interaction was equal to 1.1% [ΔR2 = 0.011; F = 14.622, p < 0.001].
A deeper analysis was conducted on the two slopes. The simple slope analysis showed the effects at different levels of a binary moderator (0 = absent vs. 1 = endorsed)—Figure 4. On one hand, the simple slope analysis showed that the effect of emotional eating (M) on uncontrolled eating was minor when the diagnosis of FA was absent (moderator = 0): β = 1.314 (SE = 0.078), 95%CI [1.161; 1.466]. On the other hand, the effect was greater when the diagnosis of FA was present (moderator = 1): β = 2.057 (SE = 0.180), 95%CI [1.703; 2.412]). An additional statistical test was conducted to confirm the difference between the two slope coefficients. This direct comparison between the slopes indicated that the effect of emotional eating (M) on uncontrolled eating (Y) significantly differed as a function of FA diagnosis [t = 3.787, p < 0.001]—confirming once more a stronger association observed when the diagnosis of FA was present.
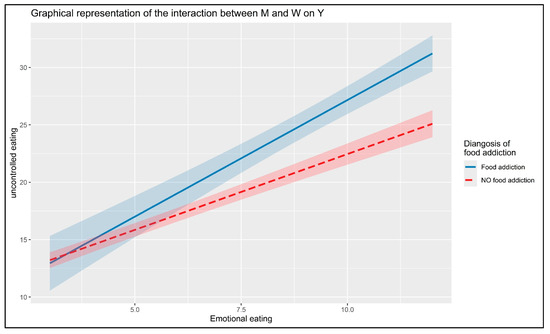
Figure 4.
Interaction between emotional eating and diagnosis of food addiction of uncontrolled eating.
4. Discussion
In recent years, a growing number of studies have focused on the crucial role of psychological factors rooted in early life experiences—such as childhood maltreatment, attachment patterns, and deficits in reflective functioning—which may underlie the development of disordered eating behaviors [15,17]. At the same time, although still limited, a steadily increasing body of research has suggested that maladaptive eating behaviors may be intensified by the presence of a key factor like FA [5,49,103,104]. However, to date, no model has been tested that integrates all these variables while highlighting the strengthening role of FA.
The aim of the present study was therefore to address this gap in the literature by testing a moderated mediation model, in which deficits in reflective functioning were linked to uncontrolled eating behaviors through emotional eating—a dysfunctional internal regulation strategy. Furthermore, it was hypothesized that the presence of a FA diagnosis would moderate these relationships. Understanding these mechanisms can help to clarify the psychological processes underlying uncontrolled eating behaviors, which often stem from basic strategies for regulating internal states and may be exacerbated by conditions that are frequently overlooked or underestimated in clinical practice—such as a diagnosis of FA. Moreover, shedding light on the psychological dynamics associated with FA can contribute to the development of more effective interventions for individuals struggling with obesity and disordered eating behaviors related to overeating. In turn, this could inform the design of timely psychological treatments and encourage further exploration of their effects on other constructs within research settings.
4.1. Reflective Functioning and Emotional Eating
One of the main findings of this study was that deficits in reflective functioning were positively associated with emotional eating—although the strength of this association was modest. However, this result is fully consistent with the (still limited) existing literature. This finding replicates prior research [15] and supports the idea that individuals with deficits in mentalization tend to rely on external regulation strategies involving external objects—such as food.
Deficits in reflective functioning, often linked to traumatic childhood experiences, hinder the development of secure attachment and the ability to mentalize emotional states, particularly during stressful situations [15,105,106,107,108]. Under such conditions, individuals may shift from controlled mentalization to more automatic, limbic-driven responses [25,32,48,107,108], creating a need for external objects like food to manage distressing psychological states. Consequently, emotional eating becomes a compensatory response to this unmet need for internal self-regulation.
4.2. The Pathway from Emotional Eating to Uncontrolled Eating
Moreover, among the main findings of the study, the tested model confirmed the expected relationship between emotional eating and uncontrolled eating [5,8,55]. These results are in line with previous studies that have highlighted the role of emotional eating as a first strategy to externally regulate internal cognitive and emotional states [57,58,59,61] that could lead to more intense and dysregulated eating pattern [49,60].
It is important to note that this progression is particularly evident when considering the characteristics of the measurement tools used. The emotional eating scale of the TFEQ-18-R captures the tendency to turn to food in response to negative or uncontrollable emotions. In contrast, the uncontrolled eating scale measures the extent to which individuals engage in actual episodes of loss-of-control eating (not limited to binge eating but also including other eating behaviors such as grazing), which represent behaviors that are qualitatively and quantitatively more severe than emotional eating.
The present findings are particularly relevant when considering the specific characteristics of highly palatable and processed foods (HPFs)—foods high in sugar, fat, and salt—which are particularly implicated in FA symptoms as they may trigger addictive-like responses [69]. The synergistic effects of sugar and fat macronutrients activate reward pathways in ways that single macronutrients do not [109,110]. The hyperpalatable nature of these foods may be especially problematic for individuals with deficits in reflective functioning, as they may be less able to cognitively regulate their responses to food cues. Furthermore, the combination of high sugar and fat content can lead to rapid fluctuations in blood glucose and subsequent cravings, potentially exacerbating the cycle from emotional eating to uncontrolled eating behaviors [70]. This suggests that interventions targeting FA might benefit from addressing not only psychological mechanisms but also the specific nutritional composition of foods consumed.
4.3. The Amplifying Role of Food Addiction
Finally, the main finding of the study concerns the moderating role of FA diagnosis. The research partially confirmed the proposed hypothesis: FA diagnosis moderated the relationship between emotional eating and uncontrolled eating (starting from deficits in reflective functioning)—w2. Specifically, the presence of a FA diagnosis appeared to act as an amplifying factor in the enactment of maladaptive eating behaviors, originating from dysfunctional coping strategies (e.g., emotional eating) associated with the inability to self-regulate.
Findings suggest that individuals with a FA diagnosis were significantly more likely to engage in uncontrolled eating behaviors (e.g., grazing, binge eating). This was further supported by the slope analysis, which showed that participants with FA exhibited a stronger association—a steeper slope—between emotional eating and uncontrolled eating, indicating a higher intensity of behavioral dysregulation when this addictive component was present. Specifically, the interaction (w2) showed that, controlling for deficits in reflective functioning, emotional eating led to higher levels of uncontrolled eating; however, individuals who endorsed FA diagnosis exhibited uncontrolled eating scores that were 0.744 points higher compared to those who did not endorse this diagnosis.
4.4. Specificity of Food Addiction’s Moderating Role
Additionally, the results indicated that FA diagnosis did not significantly moderate either the relationship between deficits in reflective functioning and emotional eating (w1) or the relationship between deficits in reflective functioning and uncontrolled eating (w3). This lack of significance can be interpreted through several theoretical and methodological considerations that provide important insights into the specificity of FA’s moderating role within the proposed model.
From a theoretical perspective, deficits in reflective functioning likely represent a more fundamental and transdiagnostic vulnerability factor that operates independently of FA diagnosis. Being rooted in early caregiver relationships, reflective functioning influences eating behaviors through primitive and automatic mechanisms that do not appear to interact with specific food-related addictive characteristics. Impaired reflective functioning serves as a common prerequisite predisposing individuals to regulation strategies requiring external objects—both emotional eating and uncontrolled eating. This interpretation aligns with research suggesting that deficits in reflective functioning constitute a “fertile ground” for various forms of psychopathology [32], including eating disorders [15,51,53,111,112,113] and addictive behaviors [17,31,40,114,115].
From a methodological standpoint, the dichotomous nature of the moderator variable and relatively low FA prevalence (12.3%) may have limited statistical power for detecting subtle moderation effects. However, the significant w2 interaction demonstrated sufficient sensitivity to identify robust effects, supporting the premise that FA’s influence is most pronounced at specific transition points rather than uniformly across all pathways. These findings highlight FA as a specific amplifying factor rather than a general moderator, emphasizing the temporal and mechanistic specificity of addictive processes in eating behavior research.
In summary, FA appeared to act as a moderator only at specific stages of the dysfunctional eating continuum—specifically during the transition from emotional eating to uncontrolled eating (w2), rather than in initial stages originating from reflective functioning deficits (w1 and w3). This pattern aligns with theoretical models suggesting that addictive characteristics emerge when compensatory behaviors fail to provide adequate emotional regulation, requiring more intense strategies [49,60]. While FA captures core addiction-related aspects [80,89], these elements may not directly condition fundamental mechanisms translating reflective functioning deficits into stronger use of external regulation strategies (emotional eating), but rather amplify their intensity and consequent behaviors. Therefore, FA could play a specific key role as a promoting factor and/or reinforcement between the use of external regulators in response to negative emotions and the engagement in dysfunctional and uncontrolled eating behavior [17].
This finding aligns with the theoretical premise of the study, which posits that deficits in reflective functioning may serve as a predisposing risk factor for the development of dysfunctional facets related to eating behavior (such as emotional eating). When an individual lacks the ability to regulate internal emotional states, they may seek gratification through external objects—such as HPFs that are strongly associated with food addiction [116,117,118,119,120]. When emotional food intake fails to achieve the desired internal regulation, the behavior may escalate, overwhelming the individual and culminating in uncontrolled eating—an outcome that is particularly intensified in the presence of a FA diagnosis.
4.5. Neurobiological Considerations and Weight Implications
The potential role of neurobiological factors should also be considered Deficits in reflective functioning have been associated with altered prefrontal cortex activity, particularly in regions implicated in executive control and emotion regulation [108].
When these top-down regulatory mechanisms are compromised, individuals may become more reliant on limbic-driven responses to emotional distress, including maladaptive behaviors such as food-seeking [72]. The presence of a FA diagnosis may further exacerbate this dysregulation by sensitizing reward pathways and diminishing the capacity to resist food-related cues [116], thereby fostering self-reinforcing cycles of problematic eating.
This mechanism may have important implications for weight management. The pathway from deficits in reflective functioning to uncontrolled eating—mediated by emotional eating and amplified by FA—represents a psychological risk profile that could contribute to weight gain over time. Prospective studies have demonstrated that emotional eating consistently predicts weight gain in adults, with individuals showing higher emotional eating scores experiencing greater increases in BMI and waist circumference over time [121,122]. Notably, the stronger effect observed among individuals with FA diagnosis (considering only the respecified model, β = 0.262 vs. β = 0.402) suggests that this subgroup may be particularly vulnerable to adverse weight-related outcomes [122], as FA symptoms have been linked to impaired control over eating behavior and greater psychological distress [123]. However, given the cross-sectional nature of this study, causal inferences about weight trajectories cannot be drawn. Future longitudinal research is therefore warranted to clarify how these psychological pathways may contribute to weight changes across time.
Lastly, the controversy surrounding FA and its role in obesity development is particularly relevant to these findings. HPFs [68,124] are particularly activating for brain circuits, as evidenced by research showing their role in FA symptoms [65,66,67]. In pediatric populations, the concern is particularly acute as children’s developing brains may be more susceptible to the rewarding properties of these foods [125]. Children with early trauma or attachment difficulties—conditions associated with impaired reflective functioning [15,17,25]—may be especially vulnerable to developing problematic relationships with food [126]. However, the complexity of neurobiological and environmental mechanisms warrants caution in interpretation and highlights the need for further investigation. Future studies should continue to explore the interplay between HPFs consumption, psychological vulnerabilities, and long-term health outcomes across diverse populations.
4.6. Strength, Limitations, and Future Research
This study is not without limitations. First, due to the cross-sectional design, causal inferences cannot be drawn. However, the research was grounded in a well-established theoretical framework, which informed both the formulation of hypotheses and the structure of the analytical model. It is also worth noting that some variables examined—particularly those linked to developmental history and early-life experiences—are inherently stable over time and, within the constraints of statistical modeling, should be considered as predictors [77,127].
Second, the study relied exclusively on self-report questionnaires, without the inclusion of clinical interviews or behavioral observations, which would offer a more nuanced assessment of reflective functioning deficits and a more accurate diagnosis of FA. The reliance on self-report measures may introduce common method variance and recall bias, particularly for retrospective assessments. Additionally, the snowball sampling approach and online administration may have introduced selection and response biases compared to randomized sampling and clinical assessments. Nonetheless, all questionnaires employed—such as the YFAS 2.0—are psychometrically sound and widely recognized for their validity and reliability in capturing the constructs under investigation.
Third, the relatively narrow scope of variables considered represents a limitation. Constructs such as impulsivity, difficulties in emotional regulation, and attachment insecurity—known to be associated with disordered eating and addictive behaviors—were not included but warrant attention in subsequent studies. Future studies may also consider relational and social factors (e.g., social support) contributing to mental health outcomes [128,129]. Future research should also incorporate physiological measures such as cortisol levels, neuroimaging data examining prefrontal-limbic connectivity, and metabolic markers to examine biological mechanisms underlying these psychological pathways. Additionally, genetic factors related to dopamine functioning and food reward sensitivity warrant investigation.
Fourth, the sample showed a slight gender imbalance, with female participants being overrepresented. This highlights the importance of considering gender and ethnicity-related factors in future research. Although the sample size was adequate and diverse, the findings can only be generalized to the Italian population and may be subject to sampling biases. Future studies should aim to recruit more representative samples or replicate the findings in clinical populations, such as individuals with diagnosed eating disorders or obesity.
Fifth, as noted in previous studies, the use of two scales targeting food-related constructs (YFAS 2.0 and the UE scale from the TFEQ-18-R) introduces the possibility of semantic overlap, which could potentially inflate correlations. However, this risk appears minimal in the present study, as observed correlations remained below critical thresholds [91,130,131], and the instruments measure conceptually distinct dimensions of eating behavior. Specifically, the YFAS 2.0 assesses hallmark symptoms of FA—including tolerance, withdrawal, and cravings—whereas the uncontrolled eating scale captures patterns of dysregulated eating, such as excessive food intake and impaired control over eating [73,132]. Furthermore, FA is not limited to overt episodes of binge eating or overeating; it can also manifest in more subtle and persistent patterns, such as grazing [6,7,133].
Finally, although the percentage of participants with FA diagnosis is consistent with available data for the general population, it remains low (12.3%; 69 participants). While sample size was calculated a priori using Monte Carlo simulation, this limited number may have influenced results. Future studies could consider increasing sample size to achieve greater power for participants with FA diagnosis. Despite these limitations, the theoretical grounding, validated instruments, and robust statistical approach support the reliability of conclusions within these methodological constraints.
However, the study presents several noteworthy strengths. Most importantly, it is anchored in a coherent and well-articulated theoretical model, which informed both the design and the statistical approach. The use of validated instruments and a relatively large, heterogeneous sample adds further robustness to the findings. To the best of our knowledge, this is the first study to examine the interplay between reflective functioning and disordered eating behaviors while specifically highlighting the moderating role of FA. Finally, by emphasizing the contribution of psychological processes to patterns of overeating and reduced dietary control, the findings resonate with foundational principles of contemporary therapeutic approaches—such as mentalization-based treatment (MBT) [44,134,135].
4.7. Clinical Implications
This study offers important contributions for both scientific research and clinical application. On the clinical front, the findings support the integration of therapeutic strategies grounded in contemporary, evidence-based psychotherapies—such as MBT [136,137,138]. Specifically, the results indicate that clinical interventions might benefit from focusing on strengthening individuals’ capacity to manage the emotional and behavioral outcomes associated with deficits in reflective functioning. Addressing maladaptive cognitive patterns, difficulties in emotion regulation, and dysfunctional behaviors may foster greater psychological well-being and reduce the incidence of disordered eating behaviors linked to FA. These interventions could be particularly effective when integrated with structured treatment protocols designed for such conditions [44,134,135,139,140,141,142,143,144].
Building on these therapeutic approaches, the findings suggest several specific intervention targets. The moderating role of FA diagnosis indicates that treatments should be stratified based on individual risk profiles, with individuals showing FA symptoms requiring interventions that incorporate craving management and trigger identification strategies. The stronger association between emotional eating and uncontrolled eating observed in individuals with FA diagnosis (β = 2.057 vs. β = 1.314) highlights the importance of early intervention targeting emotional eating patterns to prevent progression to more severe dysregulated behaviors. Furthermore, the results support multi-level interventions addressing underlying psychological processes, behavioral patterns, and environmental factors, with prevention programs focusing on developing emotional regulation skills before problematic patterns become entrenched.
From a research standpoint, the study deepens current knowledge by empirically supporting the association between reflective functioning and FA [17]. This contributes to a growing body of literature and lays the groundwork for future investigations exploring these psychological mechanisms. Moreover, the findings highlight the critical role played by deficits in reflective functioning, emotional eating, and the presence of FA diagnosis in mediating and moderating the path to uncontrolled eating behaviors. By clarifying these associations, the study provides clinicians with a conceptual basis for developing focused interventions aimed at individuals displaying dysregulated eating behaviors.
5. Conclusions
This research advances the understanding of maladaptive eating patterns—specifically emotional eating, uncontrolled eating, and FA—in relation to impairments in reflective functioning. As far as we are aware, it represents the first attempt to explore this specific pathway, particularly highlighting the moderating influence of FA. These insights may open new directions for the development of targeted interventions addressing disordered eating behaviors connected to FA symptoms and diagnosis. The results suggest that deficits in reflective functioning are directly linked to problematic eating behaviors, and that this relationship is further moderated by the presence of FA diagnosis.
Author Contributions
A.A.R. conceived the study, wrote the manuscript, and performed the analysis. A.T. and A.S. wrote part of the manuscript and contributed to the interpretation of the results. A.T. created the graphical abstract. L.D.R. and S.M. revised the manuscript critically for important intellectual content. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no funds or financial support for the research, authorship, and/or publication of this article.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the University of Padua (no. 3558); approval date 1 October 2023.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on a reasonable request due to privacy and ethical restrictions.
Conflicts of Interest
The author declares no conflicts of interest.
References
- Pereira, R.F.; Alvarenga, M. Disordered Eating: Identifying, Treating, Preventing, and Differentiating It From Eating Disorders. Diabetes Spectr. 2007, 20, 141–148. [Google Scholar] [CrossRef]
- Ágh, T.; Kovács, G.; Supina, D.; Pawaskar, M.; Herman, B.K.; Vokó, Z.; Sheehan, D.V. A Systematic Review of the Health-Related Quality of Life and Economic Burdens of Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2016, 21, 353–364. [Google Scholar] [CrossRef]
- Rossi, A.A.; Pietrabissa, G.; Tagliagambe, A.; Scuderi, A.; Montecchiani, L.; Castelnuovo, G.; Mannarini, S.; Dalla Ragione, L. Many Facets of Eating Disorders: Profiling Key Psychological Features of Anorexia Nervosa and Binge Eating Disorder. Behav. Sci. 2023, 13, 276. [Google Scholar] [CrossRef]
- Garner, D.; Olmsted, M.; Bohr, Y.; Garfinkel, P. The Eating Attitudes Test: Psychometric Features and Clinical Correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; Brownell, K.D.; Gold, M.S.; Potenza, M.N. (Eds.) Food & Addiction: A Comprehensive Handbook, 2nd ed.; Oxford University Press: Oxford, NY, USA, 2024; ISBN 978-0-19-067105-1. [Google Scholar]
- Rossi, A.A.; Mannarini, S.; Semonella, M.; Castelnuovo, G.; Pietrabissa, G. The Association between Grazing and Food Addiction: The Italian Version of the Repetitive Eating Questionnaire (Rep(Eat)-Q) and Its Relationships with Food Addiction Criteria. Nutrients 2024, 16, 949. [Google Scholar] [CrossRef] [PubMed]
- Conceição, E.M.; Mitchell, J.E.; Engel, S.G.; Machado, P.P.P.; Lancaster, K.; Wonderlich, S.A. What Is “Grazing”? Reviewing Its Definition, Frequency, Clinical Characteristics, and Impact on Bariatric Surgery Outcomes, and Proposing a Standardized Definition. Surg. Obes. Relat. Dis. 2014, 10, 973–982. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Brownell, K.D. Eating Disorders and Obesity: A Comprehensive Handbook; Guilford Press: New York, NY, USA, 2005; ISBN 978-1-59385-236-8. [Google Scholar]
- Leon, G.R.; Keel, P.K.; Klump, K.L.; Fulkerson, J.A. The Future of Risk Factor Research in Understanding the Etiology of Eating Disorders. Psychopharmacol. Bull. 1997, 33, 405–411. [Google Scholar]
- Weissman, R.S. The Role of Sociocultural Factors in the Etiology of Eating Disorders. Psychiatr. Clin. 2019, 42, 121–144. [Google Scholar] [CrossRef]
- Hetherington, M.M. Eating Disorders: Diagnosis, Etiology, and Prevention. Nutrition 2000, 16, 547–551. [Google Scholar] [CrossRef]
- Stice, E.; South, K.; Shaw, H. Future Directions in Etiologic, Prevention, and Treatment Research for Eating Disorders. J. Clin. Child Adolesc. Psychol. 2012, 41, 845–855. [Google Scholar] [CrossRef]
- Hilbert, A.; Pike, K.M.; Goldschmidt, A.B.; Wilfley, D.E.; Fairburn, C.G.; Dohm, F.-A.; Walsh, B.T.; Striegel Weissman, R. Risk Factors across the Eating Disorders. Psychiatry Res. 2014, 220, 500–506. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. Cognitive Behaviour Therapy for Eating Disorders: A “Transdiagnostic” Theory and Treatment. Behav. Res. Ther. 2003, 41, 509–528. [Google Scholar] [CrossRef]
- Musetti, A.; Gagliardini, G.; Lenzo, V.; Cella, S. From Childhood Emotional Maltreatment to Disordered Eating: A Path Analysis. Psychoanal. Psychol. 2023, 40, 90–98. [Google Scholar] [CrossRef]
- Vanderlinden, J.; Palmisano, G.L. Trauma and Eating Disorders: The State of the Art; Springer Publishing Company: Berlin/Heidelberg, Germany, 2024; ISBN 978-0-8261-7264-8. [Google Scholar]
- Rossi, A.A.; Tagliagambe, A.; Scuderi, A.; Dalla Ragione, L.; Mannarini, S. The Path from Childhood Emotional Maltreatment to Disordered Eating Behaviors: The Role of Reflective Functioning and Food Addiction. Nutrients 2025, 17, 1863. [Google Scholar] [CrossRef]
- Kimber, M.; McTavish, J.R.; Couturier, J.; Boven, A.; Gill, S.; Dimitropoulos, G.; MacMillan, H.L. Consequences of Child Emotional Abuse, Emotional Neglect and Exposure to Intimate Partner Violence for Eating Disorders: A Systematic Critical Review. BMC Psychol. 2017, 5, 33. [Google Scholar] [CrossRef] [PubMed]
- Mills, P.; Newman, E.F.; Cossar, J.; Murray, G. Emotional Maltreatment and Disordered Eating in Adolescents: Testing the Mediating Role of Emotion Regulation. Child Abuse Negl. 2015, 39, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Tasca, G.A. Attachment and Eating Disorders: A Research Update. Attach. Adulthood 2019, 25, 59–64. [Google Scholar] [CrossRef]
- Tasca, G.A.; Ritchie, K.; Zachariades, F.; Proulx, G.; Trinneer, A.; Balfour, L.; Demidenko, N.; Hayden, G.; Wong, A.; Bissada, H. Attachment Insecurity Mediates the Relationship between Childhood Trauma and Eating Disorder Psychopathology in a Clinical Sample: A Structural Equation Model. Child. Abuse Negl. 2013, 37, 926–933. [Google Scholar] [CrossRef]
- Jewell, T.; Collyer, H.; Gardner, T.; Tchanturia, K.; Simic, M.; Fonagy, P.; Eisler, I. Attachment and mentalization and their association with child and adolescent eating pathology: A systematic review. Int. J. Eat. Disord. 2016, 49, 354–373. [Google Scholar] [CrossRef]
- Midolo, L.R.; Santoro, G.; Ferrante, E.; Pellegriti, P.; Russo, S.; Costanzo, A.; Schimmenti, A. Childhood Trauma, Attachment and Psychopathology: A Correlation Network Approach. Mediterr. J. Clin. Psychol. 2020, 8, 1–25. [Google Scholar] [CrossRef]
- Schimmenti, A. The Trauma Factor: Examining the Relationships among Different Types of Trauma, Dissociation, and Psychopathology. J. Trauma. Dissociation 2018, 19, 552–571. [Google Scholar] [CrossRef]
- Garon-Bissonnette, J.; Dubois-Comtois, K.; St-Laurent, D.; Berthelot, N. A Deeper Look at the Association between Childhood Maltreatment and Reflective Functioning. Attach. Hum. Dev. 2023, 25, 368–389. [Google Scholar] [CrossRef]
- Cyr, C.; Euser, E.M.; Bakermans-Kranenburg, M.J.; Van Ijzendoorn, M.H. Attachment Security and Disorganization in Maltreating and High-Risk Families: A Series of Meta-Analyses. Dev. Psychopathol. 2010, 22, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Target, M. Attachment and Reflective Function: Their Role in Self-Organization. Dev. Psychopathol. 1997, 9, 679–700. [Google Scholar] [CrossRef] [PubMed]
- Musetti, A.; Starcevic, V.; Boursier, V.; Corsano, P.; Billieux, J.; Schimmenti, A. Childhood Emotional Abuse and Problematic Social Networking Sites Use in a Sample of Italian Adolescents: The Mediating Role of Deficiencies in Self-Other Differentiation and Uncertain Reflective Functioning. J. Clin. Psychol. 2021, 77, 1666–1684. [Google Scholar] [CrossRef] [PubMed]
- Adshead, G. Personal Responsibility, Abnormality, and Ethics: Psychotherapy as Moral Understanding. Psychiatry 2008, 7, 225–227. [Google Scholar] [CrossRef]
- Fonagy, P.; Luyten, P. A Developmental, Mentalization-Based Approach to the Understanding and Treatment of Borderline Personality Disorder. Dev. Psychopathol. 2009, 21, 1355–1381. [Google Scholar] [CrossRef]
- Santoro, G.; Musetti, A.; Costanzo, A.; Schimmenti, A. Self-Discontinuity in Behavioral Addictions: A Psychodynamic Framework. Addict. Behav. Rep. 2025, 21, 100601. [Google Scholar] [CrossRef]
- Luyten, P.; Campbell, C.; Allison, E.; Fonagy, P. The Mentalizing Approach to Psychopathology: State of the Art and Future Directions. Annu. Rev. Clin. Psychol. 2020, 16, 297–325. [Google Scholar] [CrossRef]
- Penner, F.; Gambin, M.; Sharp, C. Childhood Maltreatment and Identity Diffusion among Inpatient Adolescents: The Role of Reflective Function. J. Adolesc. 2019, 76, 65–74. [Google Scholar] [CrossRef]
- Fonagy, P.; Target, M. Playing with Reality: I. Theory of Mind and the Normal Development of Psychic Reality. Int. J. Psychoanal. 1996, 77 Pt 2, 217–233. [Google Scholar]
- Target, M.; Fonagy, P. Playing with Reality: II. The Development of Psychic Reality from a Theoretical Perspective. Int. J. Psychoanal. 1996, 77, 459–479. [Google Scholar]
- Fonagy, P.; Target, M.; Steele, H.; Steele, M. Reflective-Functioning Manual Version 5 for Application to Adult Attachment Interviews. Available online: https://discovery.ucl.ac.uk/id/eprint/1461016/ (accessed on 1 April 2025).
- Fonagy, P.; Gergely, G.; Jurist, E.; Target, M. Affect Regulation, Mentalization, and the Development of the Self; Other Press: New Yore, NY, USA, 2002. [Google Scholar]
- Fonagy, P.; Bateman, A.W. Adversity, Attachment, and Mentalizing. Compr. Psychiatry 2016, 64, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Musetti, A.; Brazzi, F.; Folli, M.C.; Plazzi, G.; Franceschini, C. Childhood Trauma, Reflective Functioning, and Problematic Mobile Phone Use Among Male and Female Adolescents. Open Psychol. J. 2020, 13, 242–252. [Google Scholar] [CrossRef]
- Handeland, T.B.; Kristiansen, V.R.; Lau, B.; Håkansson, U.; Øie, M.G. High Degree of Uncertain Reflective Functioning in Mothers with Substance Use Disorder. Addict. Behav. Rep. 2019, 10, 100193. [Google Scholar] [CrossRef] [PubMed]
- Cosenza, M.; Ciccarelli, M.; Nigro, G. The Steamy Mirror of Adolescent Gamblers: Mentalization, Impulsivity, and Time Horizon. Addict. Behav. 2019, 89, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Morosan, L.; Fonseca-Pedrero, E.; Debbané, M. Network Analysis of Reflective Functioning and Conduct Problems During Adolescence. Psychol. Violence 2020, 10, 300–311. [Google Scholar] [CrossRef]
- Fonagy, P.; Target, M. Mentalization and the Changing Aims of Child Psychoanalysis. Psychoanal. Dialogues 1998, 8, 87–114. [Google Scholar] [CrossRef]
- Allen, J.G.; Fonagy, P.; Bateman, A.W. Mentalizing in Clinical Practice. In Mentalizing in Clinical Practice; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2008; pp. 20–403. ISBN 978-1-58562-306-8. [Google Scholar]
- Cicchetti, D.; Toth, S.L. Child Maltreatment. Annu. Rev. Clin. Psychol. 2005, 1, 409–438. [Google Scholar] [CrossRef]
- Lorenzini, N.; Campbell, C.; Fonagy, P. Mentalization and Its Role in Processing Trauma. In Approaches to Psychic Trauma: Theory and Practice; Rowman & Littlefield: Lanham, MD, USA, 2019; pp. 403–422. ISBN 978-1-4422-5814-3. [Google Scholar]
- Panzeri, A.; Bottesi, G.; Ghisi, M.; Scalavicci, C.; Spoto, A.; Vidotto, G. Emotional Regulation, Coping, and Resilience in Informal Caregivers: A Network Analysis Approach. Behav. Sci. 2024, 14, 709. [Google Scholar] [CrossRef]
- Musetti, A.; Pingani, L.; Zagaria, A.; Uberti, D.; Meli, S.; Lenzo, V.; Gori, A.; Franceschini, C.; Galeazzi, G.M. Insecure Adult Attachment and Reflective Functioning as Mechanisms of the Relationship between Traumatic Life Events and Suicidal Ideation: A Path Analysis. Front. Psychol. 2022, 13, 985148. [Google Scholar] [CrossRef]
- Rossi, A.A. Tying Food Addiction to Uncontrolled Eating: The Roles of Eating-Related Thoughts and Emotional Eating. Nutrients 2025, 17, 369. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Pietrabissa, G.; Gearhardt, A.N.; Musetti, A.; Castelnuovo, G.; Mannarini, S. Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT). Nutrients 2023, 15, 1378. [Google Scholar] [CrossRef] [PubMed]
- Gagliardini, G.; Gullo, S.; Tinozzi, V.; Baiano, M.; Balestrieri, M.; Todisco, P.; Schirone, T.; Colli, A. Mentalizing Subtypes in Eating Disorders: A Latent Profile Analysis. Front. Psychol. 2020, 11, 564291. [Google Scholar] [CrossRef] [PubMed]
- Santoro, G.; Cannavò, M.; Schimmenti, A.; Barberis, N. Childhood Trauma and Eating Disorder Risk among Young Adult Females: The Mediating Role of Mentalization. Dev. Psychopathol. 2025, 1–8. [Google Scholar] [CrossRef]
- Gagliardini, G.; Pandolfi, G.; Colli, A. Attachment, Mentalization, Emotion Dysregulation, and Empathy in Eating Disorders: Comparing Anorexic and Bulimic Patients. J. Nerv. Ment. Dis. 2024, 212, 370. [Google Scholar] [CrossRef]
- Tan, C.C.; Chow, C.M. Stress and Emotional Eating: The Mediating Role of Eating Dysregulation. Personal. Individ. Differ. 2014, 66, 1–4. [Google Scholar] [CrossRef]
- Macht, M.; Simons, G. Emotional Eating. In Emotion Regulation and Well-Being; Nyklíček, I., Vingerhoets, A., Zeelenberg, M., Eds.; Springer: New York, NY, USA, 2011; pp. 281–295. ISBN 978-1-4419-6953-8. [Google Scholar]
- Stark, M.L. Katariina Emotional Eating and Eating Disorder Psychopathology. Eat. Disord. 2001, 9, 251–259. [Google Scholar] [CrossRef]
- Whiteside, U.; Chen, E.; Neighbors, C.; Hunter, D.; Lo, T.; Larimer, M. Difficulties Regulating Emotions: Do Binge Eaters Have Fewer Strategies to Modulate and Tolerate Negative Affect? Eat. Behav. 2007, 8, 162–169. [Google Scholar] [CrossRef]
- Goldbacher, E.M.; Grunwald, H.E.; LaGrotte, C.A.; Klotz, A.A.; Oliver, T.L.; Musliner, K.L.; VanderVeur, S.S.; Foster, G.D. Factor Structure of the Emotional Eating Scale in Overweight and Obese Adults Seeking Treatment. Appetite 2012, 59, 610–615. [Google Scholar] [CrossRef][Green Version]
- Frayn, M.; Knäuper, B. Emotional Eating and Weight in Adults: A Review. Curr. Psychol. 2018, 37, 924–933. [Google Scholar] [CrossRef]
- Nasirzadeh, Y.; Kantarovich, K.; Wnuk, S.; Okrainec, A.; Cassin, S.E.; Hawa, R.; Sockalingam, S. Binge Eating, Loss of Control over Eating, Emotional Eating, and Night Eating After Bariatric Surgery: Results from the Toronto Bari-PSYCH Cohort Study. Obes. Surg. 2018, 28, 2032–2039. [Google Scholar] [CrossRef] [PubMed]
- Meule, A.; Richard, A.; Schnepper, R.; Reichenberger, J.; Georgii, C.; Naab, S.; Voderholzer, U.; Blechert, J. Emotion Regulation and Emotional Eating in Anorexia Nervosa and Bulimia Nervosa. Eat. Disord. 2021, 29, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Meule, A.; Gearhardt, A.N. Food Addiction in the Light of DSM-5. Nutrients 2014, 6, 3653–3671. [Google Scholar] [CrossRef]
- Brewerton, T.D. Food Addiction as a Proxy for Eating Disorder and Obesity Severity, Trauma History, PTSD Symptoms, and Comorbidity. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2017, 22, 241–247. [Google Scholar] [CrossRef]
- Davis, C.; Curtis, C.; Levitan, R.D.; Carter, J.C.; Kaplan, A.S.; Kennedy, J.L. Evidence That ‘Food Addiction’ Is a Valid Phenotype of Obesity. Appetite 2011, 57, 711–717. [Google Scholar] [CrossRef]
- Schulte, E.M.; Wadden, T.A.; Allison, K.C. An Evaluation of Food Addiction as a Distinct Psychiatric Disorder. Int. J. Eat. Disord. 2020, 53, 1610–1622. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; DiFeliceantonio, A.G. Highly Processed Foods Can Be Considered Addictive Substances Based on Established Scientific Criteria. Addiction 2023, 118, 589–598. [Google Scholar] [CrossRef]
- Schiestl, E.T.; Rios, J.M.; Parnarouskis, L.; Cummings, J.R.; Gearhardt, A.N. A Narrative Review of Highly Processed Food Addiction across the Lifespan. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 106, 110152. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Schulte, E.M. Is Food Addictive? A Review of the Science. Annu. Rev. Nutr. 2021, 41, 387–410. [Google Scholar] [CrossRef]
- Schulte, E.M.; Avena, N.M.; Gearhardt, A.N. Which Foods May Be Addictive? The Roles of Processing, Fat Content, and Glycemic Load. PLoS ONE 2015, 10, e0117959. [Google Scholar] [CrossRef]
- Avena, N.M.; Rada, P.; Hoebel, B.G. Evidence for Sugar Addiction: Behavioral and Neurochemical Effects of Intermittent, Excessive Sugar Intake. Neurosci. Biobehav. Rev. 2008, 32, 20–39. [Google Scholar] [CrossRef]
- Davis, C.; Loxton, N.J.; Levitan, R.D.; Kaplan, A.S.; Carter, J.C.; Kennedy, J.L. ‘Food Addiction’ and Its Association with a Dopaminergic Multilocus Genetic Profile. Physiol. Behav. 2013, 118, 63–69. [Google Scholar] [CrossRef]
- Volkow, N.D.; Wise, R.A.; Baler, R. The Dopamine Motive System: Implications for Drug and Food Addiction. Nat. Rev. Neurosci. 2017, 18, 741–752. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Mannarini, S.; Castelnuovo, G.; Pietrabissa, G. Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients 2023, 15, 104. [Google Scholar] [CrossRef] [PubMed]
- Ben-Porat, T.; Weiss, R.; Sherf-Dagan, S.; Rottenstreich, A.; Kaluti, D.; Khalaileh, A.; Abu Gazala, M.; Zaken Ben-Anat, T.; Mintz, Y.; Sakran, N.; et al. Food Addiction and Binge Eating During One Year Following Sleeve Gastrectomy: Prevalence and Implications for Postoperative Outcomes. Obes. Surg. 2021, 31, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Aloi, M.; Liuzza, M.T.; Rania, M.; Carbone, E.A.; Filippis, R.d.; Gearhardt, A.N.; Segura-Garcia, C. Using Latent Class Analysis to Identify Different Clinical Profiles According to Food Addiction Symptoms in Obesity with and without Binge Eating Disorder. J. Behav. Addict. 2024, 13, 262–275. [Google Scholar] [CrossRef]
- Meule, A.; Gearhardt, A.N. Ten Years of the Yale Food Addiction Scale: A Review of Version 2.0. Curr. Addict. Rep. 2019, 6, 218–228. [Google Scholar] [CrossRef]
- Guney, N.; Snaychuk, L.A.; Kim, H.S. An Investigation into the Relationship between Adverse Childhood Experiences and Food Addiction: The Role of Urgency and Emotion Dysregulation. Psychiatry Res. Commun. 2025, 5, 100206. [Google Scholar] [CrossRef]
- Hoover, L.V.; Yu, H.P.; Duval, E.R.; Gearhardt, A.N. Childhood Trauma and Food Addiction: The Role of Emotion Regulation Difficulties and Gender Differences. Appetite 2022, 177, 106137. [Google Scholar] [CrossRef]
- Lin, X.; Wang, X.; Wang, C.; Wu, J.; Yang, W.; Wang, J.; Yang, Y.; Zhang, R.; Hu, J.; Wang, F.; et al. Bidirectional Mediation of Psychological Distress and Food Addiction Influenced by Childhood Trauma among Adolescents. J. Affect. Disord. 2025, 375, 448–455. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Mannarini, S.; Fabbricatore, M.; Imperatori, C.; Innamorati, M.; Gearhardt, A.N.; Castelnuovo, G. Structural Validity, Measurement Invariance, Reliability and Diagnostic Accuracy of the Italian Version of the Yale Food Addiction Scale 2.0 in Patients with Severe Obesity and the General Population. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2021, 26, 345–366. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.P. Snowball Sampling: Introduction. In Wiley StatsRef: Statistics Reference Online; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2014; ISBN 978-1-118-44511-2. [Google Scholar]
- Consoli, S.; Rossi, A.; Thompson, L.Y.; Volpi, C.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Assessing Psychometric Properties of the Italian Version of the Heartland Forgiveness Scale. Front. Psychol. 2020, 11, 596501. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B.O. How to Use a Monte Carlo Study to Decide on Sample Size and Determine Power. Struct. Equ. Model. Multidiscip. J. 2002, 9, 599–620. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Fonagy, P.; Luyten, P.; Moulton-Perkins, A.; Lee, Y.W.; Warren, F.; Howard, S.; Ghinai, R.; Fearon, P.; Lowyck, B. Development and Validation of a Self-Report Measure of Mentalizing: The Reflective Functioning Questionnaire. PLoS ONE 2016, 11, 0158678. [Google Scholar] [CrossRef]
- Morandotti, N.; Brondino, N.; Merelli, A.; Boldrini, A.; Vidovich, G.Z.; Ricciardo, S.; Abbiati, V.; Ambrosi, P.; Caverzasi, E.; Fonagy, P.; et al. The Italian Version of the Reflective Functioning Questionnaire: Validity Data for Adults and Its Association with Severity of Borderline Personality Disorder. PLoS ONE 2018, 13, 0206433. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, J.; Persson, L.-O.; Sjöström, L.; Sullivan, M. Psychometric Properties and Factor Structure of the Three-Factor Eating Questionnaire (TFEQ) in Obese Men and Women. Results from the Swedish Obese Subjects (SOS) Study. Int. J. Obes. 2000, 24, 1715–1725. [Google Scholar] [CrossRef]
- Rossi, A.A.; Pietrabissa, G.; Castelnuovo, G.; Mannarini, S. Cognitive Restraint, Uncontrolled Eating, and Emotional Eating. The Italian Version of the Three Factor Eating Questionnaire—Revised 18 (TFEQ–R–18): A Three—Step Validation Study. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2024, 29, 16. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Development of the Yale Food Addiction Scale Version 2.0. Psychol. Addict. Behav. 2016, 30, 113–121. [Google Scholar] [CrossRef]
- Aloi, M.; Rania, M.; Rodríguez Muñoz, R.C.; Jiménez Murcia, S.; Fernández-Aranda, F.; De Fazio, P.; Segura-Garcia, C. Validation of the Italian Version of the Yale Food Addiction Scale 2.0 (I-YFAS 2.0) in a Sample of Undergraduate Students. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2017, 22, 527–533. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 7th ed.; Pearson: Harlow, UK, 2019. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: Third Edition: A Regression-Based Approach, 3rd ed.; The Guilford Press: New York, NY, USA, 2022. [Google Scholar]
- Howell, D.C. Statistical Methods for Psychology; Wadsworth, Cengage Learning: Belmont, CA, USA, 2013. [Google Scholar]
- Hayes, A.F. Partial, Conditional, and Moderated Moderated Mediation: Quantification, Inference, and Interpretation. Commun. Monogr. 2018, 85, 4–40. [Google Scholar] [CrossRef]
- Hayes, A.F.; Rockwood, N.J. Conditional Process Analysis: Concepts, Computation, and Advances in the Modeling of the Contingencies of Mechanisms. Am. Behav. Sci. 2020, 64, 19–54. [Google Scholar] [CrossRef]
- Iacobucci, D. Mediation Analysis; SAGE Publications, Inc.: London, UK, 2008; ISBN 978-1-4129-8496-6. [Google Scholar]
- Weston, R.; Gore, P.A. A Brief Guide to Structural Equation Modeling. Couns. Psychol. 2006, 34, 719–751. [Google Scholar] [CrossRef]
- McDonald, R.P.; Ho, M.-H.R. Principles and Practice in Reporting Structural Equation Analyses. Psychol. Methods 2002, 7, 64–82. [Google Scholar] [CrossRef]
- Frazier, P.A.; Tix, A.P.; Barron, K.E. Testing Moderator and Mediator Effects in Counseling Psychology Research. J. Couns. Psychol. 2004, 51, 115–134. [Google Scholar] [CrossRef]
- Daniel, R.M.; De Stavola, B.L.; Cousens, S.N.; Vansteelandt, S. Causal Mediation Analysis with Multiple Mediators. Biometrics 2015, 71, 1–14. [Google Scholar] [CrossRef]
- Mackinnon, D.P. Introduction to Statistical Mediation Analysis; Routledge: New York, NY, USA, 2012; pp. 1–477. [Google Scholar]
- VanderWeele, T.; Vansteelandt, S. Mediation Analysis with Multiple Mediators. Epidemiol. Methods 2014, 2, 95–115. [Google Scholar] [CrossRef]
- Schulte, E.M.; Gearhardt, A.N. Associations of Food Addiction in a Sample Recruited to Be Nationally Representative of the United States. Eur. Eat. Disord. Rev. 2018, 26, 112–119. [Google Scholar] [CrossRef]
- Schulte, E.M.; Gearhardt, A.N. Attributes of the Food Addiction Phenotype within Overweight and Obesity. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2020, 26, 2043–2049. [Google Scholar] [CrossRef]
- Bartholomew, K.; Horowitz, L.M. Attachment Styles among Young Adults: A Test of a Four-Category Model. J. Pers. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef]
- Mikulincer, M.; Shaver, P.R.; Pereg, D. Attachment Theory and Affect Regulation: The Dynamics, Development, and Cognitive Consequences of Attachment-Related Strategies. Motiv. Emot. 2003, 27, 77–102. [Google Scholar] [CrossRef]
- Luyten, P.; Fonagy, P. Mentalizing and Trauma. In Handbook of Mentalizing in Mental Health Practice; American Psychiatric Association Publishing: Washington, DC, USA, 2019. [Google Scholar]
- Luyten, P.; Fonagy, P. The Neurobiology of Mentalizing. Personal. Disord. Theory Res. Treat. 2015, 6, 366–379. [Google Scholar] [CrossRef]
- Small, D.M.; DiFeliceantonio, A.G. Processed Foods and Food Reward. Science 2019, 363, 346–347. [Google Scholar] [CrossRef] [PubMed]
- DiFeliceantonio, A.G.; Coppin, G.; Rigoux, L.; Thanarajah, S.E.; Dagher, A.; Tittgemeyer, M.; Small, D.M. Supra-Additive Effects of Combining Fat and Carbohydrate on Food Reward. Cell Metab. 2018, 28, 33–44.e3. [Google Scholar] [CrossRef] [PubMed]
- Sacchetti, S.; Robinson, P.; Bogaardt, A.; Clare, A.; Ouellet-Courtois, C.; Luyten, P.; Bateman, A.; Fonagy, P. Reduced Mentalizing in Patients with Bulimia Nervosa and Features of Borderline Personality Disorder: A Case-Control Study. BMC Psychiatry 2019, 19, 134. [Google Scholar] [CrossRef] [PubMed]
- Santoro, G.; Midolo, L.R.; Costanzo, A.; Schimmenti, A. The Vulnerability of Insecure Minds: The Mediating Role of Mentalization in the Relationship between Attachment Styles and Psychopathology. Bull. Menn. Clin. 2021, 85, 358–384. [Google Scholar] [CrossRef]
- Kuipers, G.S.; van Loenhout, Z.; van der Ark, L.A.; Bekker, M.H. Attachment Insecurity, Mentalization and Their Relation to Symptoms in Eating Disorder Patients. Attach. Hum. Dev. 2016, 18, 250–272. [Google Scholar] [CrossRef]
- Ciccarelli, M.; Nigro, G.; D’Olimpio, F.; Griffiths, M.D.; Cosenza, M. Mentalizing Failures, Emotional Dysregulation, and Cognitive Distortions Among Adolescent Problem Gamblers. J. Gambl. Stud. 2021, 37, 283–298. [Google Scholar] [CrossRef]
- Schimmenti, A.; Bifulco, A. Toward a Better Understanding of the Relationship between Childhood Trauma and Psychiatric Disorders: Measurement and Impact on Addictive Behaviors. Psychiatry Investig. 2015, 12, 415–416. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Food Addiction: An Examination of the Diagnostic Criteria for Dependence. J. Addict. Med. 2009, 3, 1–7. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Hebebrand, J. The Concept of “Food Addiction” Helps Inform the Understanding of Overeating and Obesity: Debate Consensus. Am. J. Clin. Nutr. 2021, 113, 274–276. [Google Scholar] [CrossRef]
- Al-Jawaldeh, A.; Abbass, M.M.S. Unhealthy Dietary Habits and Obesity: The Major Risk Factors Beyond Non-Communicable Diseases in the Eastern Mediterranean Region. Front. Nutr. 2022, 9, 817808. [Google Scholar] [CrossRef]
- Agüera, Z.; Lozano-Madrid, M.; Mallorquí-Bagué, N.; Jiménez-Murcia, S.; Menchón, J.M.; Fernández-Aranda, F. A Review of Binge Eating Disorder and Obesity. Neuropsychiatrie 2021, 35, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Castelnuovo, G.; Pietrabissa, G.; Manzoni, G.M.; Corti, S.; Ceccarini, M.; Borrello, M.; Giusti, E.M.; Novelli, M.; Cattivelli, R.; Middleton, N.A.; et al. Chronic Care Management of Globesity: Promoting Healthier Lifestyles in Traditional and mHealth Based Settings. Front. Psychol. 2015, 6, 1557. [Google Scholar] [CrossRef] [PubMed]
- Konttinen, H. Emotional Eating and Obesity in Adults: The Role of Depression, Sleep and Genes. Proc. Nutr. Soc. 2020, 79, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Konttinen, H.; van Strien, T.; Männistö, S.; Jousilahti, P.; Haukkala, A. Depression, Emotional Eating and Long-Term Weight Changes: A Population-Based Prospective Study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 28. [Google Scholar] [CrossRef]
- Pape, M.; Herpertz, S.; Schroeder, S.; Seiferth, C.; Färber, T.; Wolstein, J.; Steins-Loeber, S. Food Addiction and Its Relationship to Weight- and Addiction-Related Psychological Parameters in Individuals With Overweight and Obesity. Front. Psychol. 2021, 12, 736454. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-Processed Foods: What They Are and How to Identify Them. Public. Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Stice, E.; Yokum, S.; Burger, K.S. Elevated Reward Region Responsivity Predicts Future Substance Use Onset But Not Overweight/Obesity Onset. Biol. Psychiatry 2013, 73, 869–876. [Google Scholar] [CrossRef]
- Ravichandran, S.; Sood, R.; Das, I.; Dong, T.; Figueroa, J.D.; Yang, J.; Finger, N.; Vaughan, A.; Vora, P.; Selvaraj, K.; et al. Early Life Adversity Impacts Alterations in Brain Structure and Food Addiction in Individuals with High BMI. Sci. Rep. 2024, 14, 13141. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S.; Watkins, E.R. A Heuristic for Developing Transdiagnostic Models of Psychopathology: Explaining Multifinality and Divergent Trajectories. Perspect. Psychol. Sci. 2011, 6, 589–609. [Google Scholar] [CrossRef]
- Panzeri, A.; Bettinardi, O.; Bottesi, G.; Bertolotti, G.; Brambatti, L.; Monfredo, M.; Mignemi, G.; Bruno, G.; Vidotto, G.; Spoto, A.; et al. Assessment of Perceived Support in the Context of Emergency: Development and Validation of the Psycho-Social Support Scale. Curr. Psychol. 2022, 42, 22514–22525. [Google Scholar] [CrossRef]
- Bennett, K.M.; Panzeri, A.; Derrer-Merk, E.; Butter, S.; Hartman, T.K.; Mason, L.; McBride, O.; Murphy, J.; Shevlin, M.; Gibson-Miller, J.; et al. Predicting Resilience during the COVID-19 Pandemic in the United Kingdom: Cross-Sectional and Longitudinal Results. PLoS ONE 2023, 18, e0283254. [Google Scholar] [CrossRef] [PubMed]
- Panzeri, A.; Castelnuovo, G.; Spoto, A. Assessing Discriminant Validity through Structural Equation Modeling: The Case of Eating Compulsivity. Nutrients 2024, 16, 550. [Google Scholar] [CrossRef] [PubMed]
- Rönkkö, M.; Cho, E. An Updated Guideline for Assessing Discriminant Validity. Organ. Res. Methods 2022, 25, 6–14. [Google Scholar] [CrossRef]
- Ruddock, H.K.; Christiansen, P.; Halford, J.C.G.; Hardman, C.A. The Development and Validation of the Addiction-like Eating Behaviour Scale. Int. J. Obes. 2017, 41, 1710–1717. [Google Scholar] [CrossRef]
- Krupa, H.; Gearhardt, A.N.; Lewandowski, A.; Avena, N.M. Food Addiction. Brain Sci. 2024, 14, 952. [Google Scholar] [CrossRef]
- Bateman, A.; Fonagy, P.; Campbell, C.; Luyten, P.; Debbané, M. Cambridge Guide to Mentalization-Based Treatment (MBT); Cambridge Guides to the Psychological Therapies; Cambridge University Press: Cambridge, UK, 2023. [Google Scholar]
- Allen, J.G.; Fonagy, P. Handbook of Mentalization—Based Treatment; John Wiley & Sons, Ltd.: West Sussex, UK, 2006; ISBN 978-0-470-71298-6. [Google Scholar]
- Robinson, P.; Hellier, J.; Barrett, B.; Barzdaitiene, D.; Bateman, A.; Bogaardt, A.; Clare, A.; Somers, N.; O’Callaghan, A.; Goldsmith, K.; et al. The NOURISHED Randomised Controlled Trial Comparing Mentalisation-Based Treatment for Eating Disorders (MBT-ED) with Specialist Supportive Clinical Management (SSCM-ED) for Patients with Eating Disorders and Symptoms of Borderline Personality Disorder. Trials 2016, 17, 549. [Google Scholar] [CrossRef]
- Robinson, P.; Skårderud, F.; Sommerfeldt, B. Hunger: Mentalization-Based Treatments for Eating Disorders; Springer: Berlin/Heidelberg, Germany, 2018; ISBN 978-3-319-95121-8. [Google Scholar]
- Salucci, K.G.; Austin, A. Mentalisation-Based Therapy for Eating Disorder Treatment: Protocol for a Systematic Review. BMJ Open 2025, 15, e097639. [Google Scholar] [CrossRef]
- O’Hea, E.L.; Edwards-Hampton, S.A.; Beall Brown, D.L.; Sonneville, K.R.; Ziedonis, D.M.; Gearhardt, A.N. The Food Addiction Clinical Treatment (FACT) Manual: A Harm Reduction Treatment Approach. Behav. Sci. 2024, 14, 557. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Rossi, A.; Borrello, M.; Manzoni, G.M.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Development and Validation of a Self-Determination Theory-Based Measure of Motivation to Exercise and Diet in Children. Front. Psychol. 2020, 11, 1299. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, G.; Sorgente, A.; Rossi, A.; Simpson, S.; Riva, G.; Manzoni, G.M.; Prochaska, J.O.; Prochaska, J.M.; Cattivelli, R.; Castelnuovo, G. Stages of Change in Obesity and Weight Management: Factorial Structure of the Italian Version of the University of Rhode Island Change Assessment Scale. Eat. Weight Disord. Stud. Anorex. Bulim. Obes. 2017, 22, 361–367. [Google Scholar] [CrossRef]
- Zeeck, A.; Lau, I.; Endorf, K.; Schaefer, L.; Euler, S.; Lahmann, C.; Hartmann, A. Mentalizing in Psychotherapeutic Processes of Patients with Eating Disorders. Front. Psychiatry 2024, 15, 1367863. [Google Scholar] [CrossRef]
- Sonntag, M.; Russell, J. The Mind-in-Mind Study: A Pilot Randomised Controlled Trial That Compared Modified Mentalisation Based Treatment with Supportive Clinical Management for Patients with Eating Disorders without Borderline Personality Disorder. Eur. Eat. Disord. Rev. 2022, 30, 206–220. [Google Scholar] [CrossRef]
- Zeeck, A.; Endorf, K.; Euler, S.; Schaefer, L.; Lau, I.; Flösser, K.; Geiger, V.; Meier, A.F.; Walcher, P.; Lahmann, C.; et al. Implementation of Mentalization-Based Treatment in a Day Hospital Program for Eating Disorders—A Pilot Study. Eur. Eat. Disord. Rev. 2021, 29, 783–801. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).