Composite Meal-Related Behaviors and Health Indicators: Insight from Large-Scale Nationwide Data on Korean Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Categorization Based on Dietary Behaviors
2.3. Sociodemographic Characteristics and Clinical Variables
2.4. Assessment of Sedentary Time
2.5. Biochemical Markers
2.6. Assessment of Nutrient Intake
2.7. Statistical Analysis
3. Results
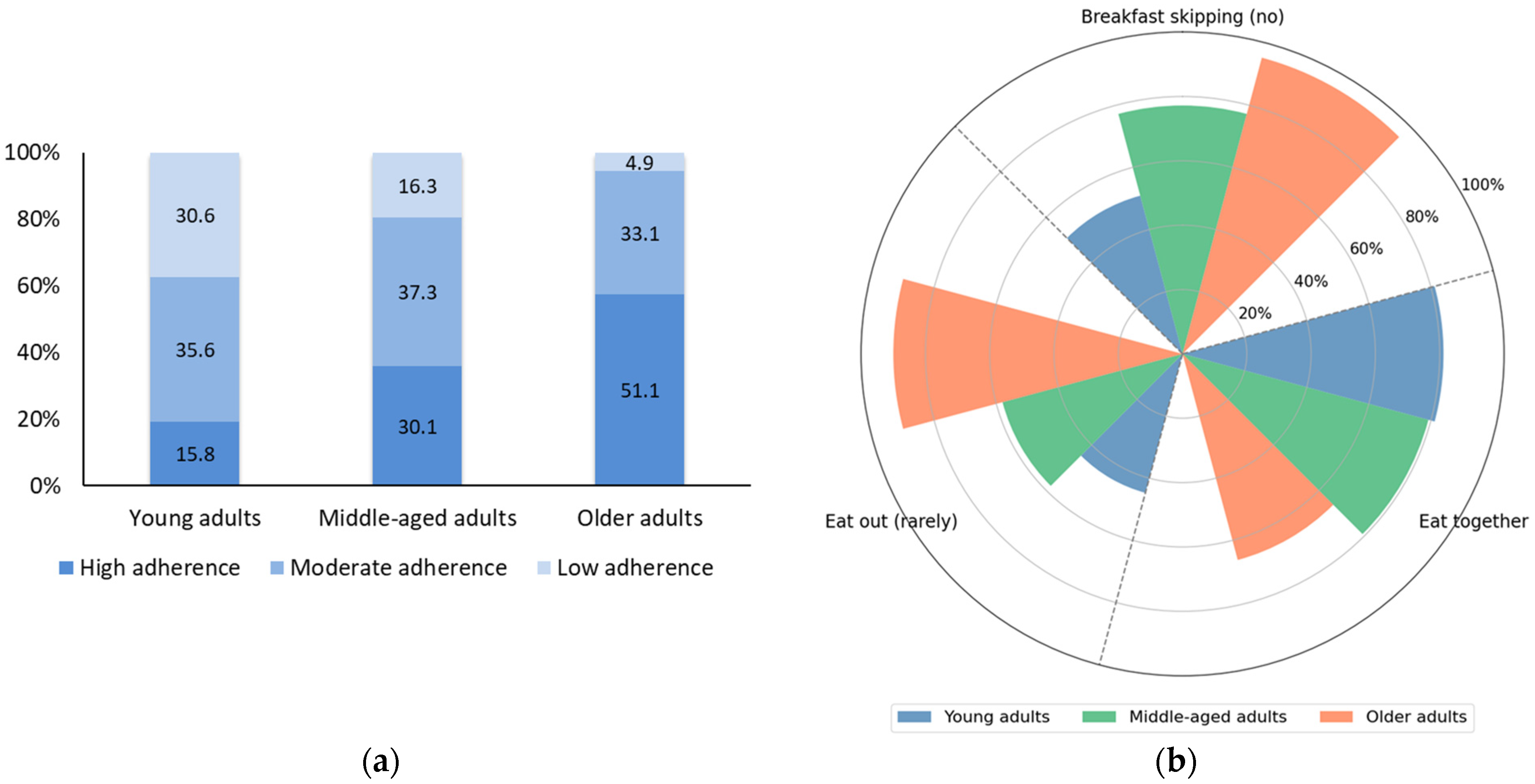
3.1. Differences in Dietary Behaviors Across Age Groups
3.2. Comparison of Health Outcomes by Meal-Related Behavior Groups
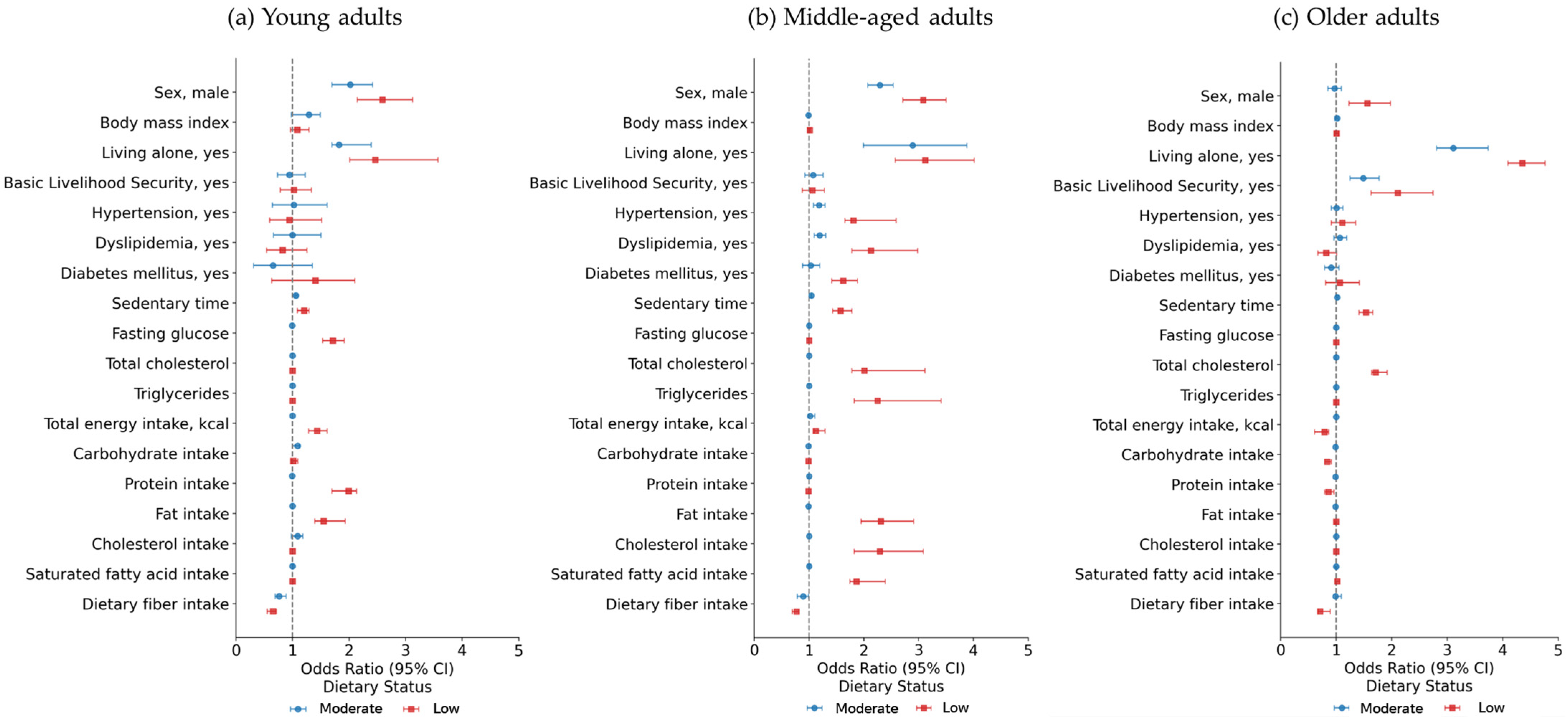
3.3. Predictors of Poorer Dietary Status
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ueno, S.; Aung, M.N.; Yuasa, M.; Ishtiaq, A.; Khin, E.T.; Latt, T.S.; Moolphate, S.; Sato, S.; Tanigawa, T. Association Between Dietary Habits and Type 2 Diabetes Mellitus in Yangon, Myanmar: A Case-Control Study. Int. J. Environ. Res. Public Health 2021, 18, 11056. [Google Scholar] [CrossRef]
- King, D.E.; Xiang, J. A Relationship Between Mortality and Eating Breakfast and Fiber. J. Am. Board Fam. Med. 2021, 34, 678–687. [Google Scholar] [CrossRef] [PubMed]
- Ofori-Asenso, R.; Owen, A.J.; Liew, D. Skipping Breakfast and the Risk of Cardiovascular Disease and Death: A Systematic Review of Prospective Cohort Studies in Primary Prevention Settings. J. Cardiovasc. Dev. Dis. 2019, 6, 30. [Google Scholar] [CrossRef] [PubMed]
- Ishizuka, R.; Otaki, N.; Tai, Y.; Yamagami, Y.; Tanaka, K.; Morikawa, M.; Iki, M.; Kurumatani, N.; Saeki, K.; Obayashi, K. Breakfast Skipping and Declines in Cognitive Score Among Community-Dwelling Older Adults: A Longitudinal Study of the HEIJO-KYO Cohort. J. Geriatr. Psychiatry Neurol. 2023, 36, 316–322. [Google Scholar] [CrossRef]
- Utter, J.; Larson, N.; Berge, J.M.; Eisenberg, M.E.; Fulkerson, J.A.; Neumark-Sztainer, D. Family meals among parents: Associations with nutritional, social and emotional wellbeing. Prev. Med. 2018, 113, 7–12. [Google Scholar] [CrossRef]
- Ishikawa, M.; Takemi, Y.; Yokoyama, T.; Kusama, K.; Fukuda, Y.; Nakaya, T.; Nozue, M.; Yoshiike, N.; Yoshiba, K.; Hayashi, F.; et al. “Eating Together” Is Associated with Food Behaviors and Demographic Factors of Older Japanese People Who Live Alone. J. Nutr. Health Aging 2017, 21, 662–672. [Google Scholar] [CrossRef]
- Kant, A.K.; Whitley, M.I.; Graubard, B.I. Away from home meals: Associations with biomarkers of chronic disease and dietary intake in American adults, NHANES 2005–2010. Int. J. Obes. 2015, 39, 820–827. [Google Scholar] [CrossRef]
- Du, Y.; Rong, S.; Sun, Y.; Liu, B.; Wu, Y.; Snetselaar, L.G.; Wallace, R.B.; Bao, W. Association Between Frequency of Eating Away-From-Home Meals and Risk of All-Cause and Cause-Specific Mortality. J. Acad. Nutr. Diet. 2021, 121, 1741–1749.e1. [Google Scholar] [CrossRef] [PubMed]
- Hengeveld, L.M.; Wijnhoven, H.A.H.; Olthof, M.R.; Brouwer, I.A.; Simonsick, E.M.; Kritchevsky, S.B.; Houston, D.K.; Newman, A.B.; Visser, M. Prospective Associations of Diet Quality with Incident Frailty in Older Adults: The Health, Aging, and Body Composition Study. J. Am. Geriatr. Soc. 2019, 67, 1835–1842. [Google Scholar] [CrossRef]
- Lim, J.; Kim, J.-S.; Kim, Y. Association Between Physical Activity and Metabolic Syndrome in Korean Adults and Older Adults: Using Accelerometer Data from the Korea National Health and Nutrition Examination Survey, 2014–2017. Exerc. Sci. 2022, 31, 357–363. [Google Scholar] [CrossRef]
- Qiu, B.; Zhu, R.; Huang, X.; Qi, Z.; Zhang, L. Associations between eating alone, its transition and depressive symptoms among Chinese middle-aged and older adults: Evidence from two national cohorts. BMC Psychiatry 2024, 24, 458. [Google Scholar] [CrossRef]
- Adams, J.; Goffe, L.; Brown, T.; Lake, A.A.; Summerbell, C.; White, M.; Wrieden, W.; Adamson, A.J. Frequency and socio-demographic correlates of eating meals out and take-away meals at home: Cross-sectional analysis of the UK national diet and nutrition survey, waves 1–4 (2008–12). Int. J. Behav. Nutr. Phys. Act. 2015, 12, 51. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Kang, M.; Lim, H. Age-specific association between meal-skipping patterns and the risk of hyperglycemia in Korean adults: A national cross-sectional study using the KNHANES data. BMC Public Health 2024, 24, 1697. [Google Scholar] [CrossRef]
- Kelly, S.; Martin, S.; Kuhn, I.; Cowan, A.; Brayne, C.; Lafortune, L. Barriers and Facilitators to the Uptake and Maintenance of Healthy Behaviours by People at Mid-Life: A Rapid Systematic Review. PLoS ONE 2016, 11, e0145074. [Google Scholar] [CrossRef]
- Bhawra, J.; Kirkpatrick, S.I.; Hall, M.G.; Vanderlee, L.; White, C.M.; Hammond, D. Patterns and correlates of nutrition knowledge across five countries in the 2018 international food policy study. Nutr. J. 2023, 22, 19. [Google Scholar] [CrossRef] [PubMed]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J. Acad. Nutr. Diet. 2013, 113, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Korea Disease Control and Prevention Agency. Korea Health Statistics 2022: Korea National Health and Nutrition Examination Survey (KNHANES IX-1). Available online: https://knhanes.kdca.go.kr/knhanes/archive/wsiStatsClct.do (accessed on 15 June 2025).
- Ju, S.Y. Changes in Eating-Out Frequency according to Sociodemographic Characteristics and Nutrient Intakes Among Korean Adults. Iran. J. Public Health 2020, 49, 46–55. [Google Scholar] [CrossRef]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Bechard, L.E.; Bergelt, M.; Neudorf, B.; DeSouza, T.C.; Middleton, L.E. Using the Health Belief Model to Understand Age Differences in Perceptions and Responses to the COVID-19 Pandemic. Front. Psychol. 2021, 12, 609893. [Google Scholar] [CrossRef]
- Murray, C.B.; Patel, K.V.; Twiddy, H.; Sturgeon, J.A.; Palermo, T.M. Age differences in cognitive-affective processes in adults with chronic pain. Eur. J. Pain 2021, 25, 1041–1052. [Google Scholar] [CrossRef]
- Park, S.; Kim, H.J.; Kim, S.; Rhee, S.Y.; Woo, H.G.; Lim, H.; Cho, W.; Yon, D.K. National Trends in Physical Activity Among Adults in South Korea Before and During the COVID-19 Pandemic, 2009–2021. JAMA Netw. Open 2023, 6, e2316930. [Google Scholar] [CrossRef]
- Konikowska, K.; Bombala, W.; Szuba, A.; Rozanska, D.; Regulska-Ilow, B. Metabolic Syndrome Is Associated with Low Diet Quality Assessed by the Healthy Eating Index-2015 (HEI-2015) and Low Concentrations of High-Density Lipoprotein Cholesterol. Biomedicines 2022, 10, 2487. [Google Scholar] [CrossRef]
- Lumley, T.; Diehr, P.; Emerson, S.; Chen, L. The importance of the normality assumption in large public health data sets. Annu. Rev. Public Health 2002, 23, 151–169. [Google Scholar] [CrossRef]
- Rice, J.A. Mathematical Statistics and Data Analysis, 3rd ed.; Cengage Learning: Belmont, CA, USA, 2006. [Google Scholar]
- Coelho-Junior, H.J.; Calvani, R.; Azzolino, D.; Picca, A.; Tosato, M.; Landi, F.; Cesari, M.; Marzetti, E. Protein Intake and Sarcopenia in Older Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 8718. [Google Scholar] [CrossRef] [PubMed]
- Bjornwall, A.; Sydner, Y.M.; Koochek, A.; Neuman, N. Eating Alone or Together Among Community-Living Older People-A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 3495. [Google Scholar] [CrossRef]
- Tani, Y.; Kondo, N.; Takagi, D.; Saito, M.; Hikichi, H.; Ojima, T.; Kondo, K. Combined effects of eating alone and living alone on unhealthy dietary behaviors, obesity and underweight in older Japanese adults: Results of the JAGES. Appetite 2015, 95, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wellard-Cole, L.; Davies, A.; Allman-Farinelli, M. Contribution of foods prepared away from home to intakes of energy and nutrients of public health concern in adults: A systematic review. Crit. Rev. Food Sci. Nutr. 2022, 62, 5511–5522. [Google Scholar] [CrossRef] [PubMed]
- Suliga, E.; Koziel, D.; Ciesla, E.; Gluszek, S. Association between dietary patterns and metabolic syndrome in individuals with normal weight: A cross-sectional study. Nutr. J. 2015, 14, 55. [Google Scholar] [CrossRef]
- Livingstone, K.M.; Sexton-Dhamu, M.J.; Pendergast, F.J.; Worsley, A.; Brayner, B.; McNaughton, S.A. Energy-dense dietary patterns high in free sugars and saturated fat and associations with obesity in young adults. Eur. J. Nutr. 2022, 61, 1595–1607. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Hoffmann, G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: A systematic review and meta-analysis of cohort studies. J. Acad. Nutr. Diet. 2015, 115, 780–800.e5. [Google Scholar] [CrossRef]
- Mozaffarian, D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity: A Comprehensive Review. Circulation 2016, 133, 187–225. [Google Scholar] [CrossRef]
- Artegoitia, V.M.; Krishnan, S.; Bonnel, E.L.; Stephensen, C.B.; Keim, N.L.; Newman, J.W. Healthy eating index patterns in adults by sex and age predict cardiometabolic risk factors in a cross-sectional study. BMC Nutr. 2021, 7, 30. [Google Scholar] [CrossRef]
- Dittmann, A.; Werner, L.; Horz, L.; Luft, T.; Finkbeiner, F.; Storcksdieck Genannt Bonsmann, S. Sociodemographic and behavioural differences between frequent and non-frequent users of convenience food in Germany. Front. Nutr. 2024, 11, 1369137. [Google Scholar] [CrossRef] [PubMed]
- Hughes, G.; Bennett, K.M.; Hetherington, M.M. Old and alone: Barriers to healthy eating in older men living on their own. Appetite 2004, 43, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Bowman, S.A. Television-viewing characteristics of adults: Correlations to eating practices and overweight and health status. Prev. Chronic Dis. 2006, 3, A38. [Google Scholar] [PubMed]
- Patterson, R.; McNamara, E.; Tainio, M.; de Sa, T.H.; Smith, A.D.; Sharp, S.J.; Edwards, P.; Woodcock, J.; Brage, S.; Wijndaele, K. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: A systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018, 33, 811–829. [Google Scholar] [CrossRef]
- Sisson, S.B.; Shay, C.M.; Broyles, S.T.; Leyva, M. Television-viewing time and dietary quality among U.S. children and adults. Am. J. Prev. Med. 2012, 43, 196–200. [Google Scholar] [CrossRef]
- Thorp, A.A.; McNaughton, S.A.; Owen, N.; Dunstan, D.W. Independent and joint associations of TV viewing time and snack food consumption with the metabolic syndrome and its components; a cross-sectional study in Australian adults. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 96. [Google Scholar] [CrossRef]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef]
- Wagner, A.; Dallongeville, J.; Haas, B.; Ruidavets, J.B.; Amouyel, P.; Ferrieres, J.; Simon, C.; Arveiler, D. Sedentary behaviour, physical activity and dietary patterns are independently associated with the metabolic syndrome. Diabetes Metab. 2012, 38, 428–435. [Google Scholar] [CrossRef]
- Nouri, M.; Gerami, S.; Borazjani, M.; Rajabzadeh-Dehkordi, M.; Askarpour, M.; Najafi, M.; Faghih, S. Diet quality indices and their relationship with dyslipidemia in adults: A cross-sectional study. Clin. Nutr. ESPEN 2023, 58, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Asakura, K.; Suga, H.; Sasaki, S.; Three-generation Study of Women on Diets and Health Study Group. High protein intake is associated with low prevalence of frailty among old Japanese women: A multicenter cross-sectional study. Nutr. J. 2013, 12, 164. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Argiles, J.M.; Evans, W.J.; Bhasin, S.; Cella, D.; Deutz, N.E.; Doehner, W.; Fearon, K.C.; Ferrucci, L.; Hellerstein, M.K.; et al. Nutritional recommendations for the management of sarcopenia. J. Am. Med. Dir. Assoc. 2010, 11, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.; Park, H. Physical Activity and Eating Habits Are Related to Chronic Disease in the Basic Livelihood Security Program. Nutrients 2025, 17, 462. [Google Scholar] [CrossRef]
| Variable | Very Good (n = 2436) | Good (n = 5501) | Poor (n = 4731) | p-Value |
|---|---|---|---|---|
| Age, year | 31.4 ± 6.2 a,b | 29.5 ± 6.6 c | 29.0 ± 6.2 | <0.001 # |
| Sex, female | 1787 (73.4) d | 3023 (55.0) | 2188 (46.2) e | <0.001 $ |
| BMI, kg/m2 | 23.1 ± 4 b | 23.3 ± 4.2 c | 23.7 ± 4.3 | <0.001 # |
| BMI group, n (%) | <0.001 $ | |||
| Underweight | 184 (8.2) | 390 (7.8) | 277 (6.5) e | |
| Normal | 1067 (47.5) d | 2252 (45.3) | 1813 (42.6) | |
| Overweight | 381 (17.0) | 829 (16.7) | 754 (17.7) | |
| Obese | 615 (27.4) e | 1499 (30.2) | 1415 (33.2) d | |
| Living alone, yes | 40 (1.6) e | 237 (4.3) e | 805 (17.0) d | <0.001 $ |
| Basic Livelihood Security, yes | 115 (4.7) | 256 (4.7) | 254 (5.4) | 0.215 $ |
| Hypertension, yes | 31 (1.4) | 86 (1.8) | 92 (2.2) | 0.049 $ |
| Dyslipidemia, yes | 40 (1.8) | 101 (2.1) | 103 (2.5) | 0.153 $ |
| Diabetes mellitus, yes | 14 (0.6) | 38 (0.8) | 31 (0.7) | 0.773 $ |
| Sedentary time, hour/day | 8.2 ± 3.5 a,b | 9.0 ± 3.5 c | 9.5 ± 3.6 | <0.001 # |
| Fasting glucose, mg/dL | 91.8 ± 16.7 b | 92.1 ± 13.8 c | 93.5 ± 15.9 | <0.001 # |
| Total cholesterol, mg/dL | 184.7 ± 34.0 b | 185.6 ± 34.0 c | 187.7 ± 33.5 | <0.001 # |
| Triglycerides, mg/dL | 105.5 ± 85.9 a,b | 112.8 ± 92.2 c | 121.1 ± 107.7 | <0.001 # |
| Total energy intake, kcal | 1977.4 ± 873.0 a,b | 2102.4 ± 992.7 c | 2170.7 ± 1127.4 | <0.001 # |
| Carbohydrate intake, g | 284.1 ± 121.5 | 286.1 ± 126.6 | 280.6 ± 128.3 | 0.09 # |
| Protein intake, g | 75.0 ± 42.1 a,b | 79.6 ± 46.1 c | 82.1 ± 52.1 | <0.001 # |
| Fat intake, g | 52.5 ± 35.3 a,b | 58.8 ± 41.3 c | 62.9 ± 51.1 | <0.001 # |
| Cholesterol intake, mg | 292.8 ± 246.3 b | 303.2 ± 246 c | 315.8 ± 274.9 | <0.001 # |
| Saturated fatty acid intake, g | 16.8 ± 12.5 a,b | 19.0 ± 14.6 c | 20.5 ± 18.2 | <0.001 # |
| Dietary fiber intake, g | 22.5 ± 12.3 b | 21.8 ± 12 c | 20.6 ± 11.6 | <0.001 # |
| Variable | Very Good (n = 7648) | Good (n = 9471) | Poor (n = 4149) | p-Value |
|---|---|---|---|---|
| Age, year | 54.0 ± 7.3 a,b | 51.9 ± 7 c | 50.2 ± 6.8 | <0.001 # |
| Sex, female | 5498 (71.9) d | 4875 (51.5) | 1909 (46.0) e | <0.001 $ |
| BMI, kg/m2 | 24.0 ± 3.4 a,b | 24.2 ± 3.4 | 24.3 ± 3.5 | <0.001 # |
| BMI group, n (%) | <0.001 $ | |||
| Underweight | 174 (2.4) | 210 (2.4) | 96 (2.5) | |
| Normal | 2779 (38.7) d | 3108 (35.8) | 1307 (34.2) e | |
| Overweight | 1676 (23.3) | 2100 (24.2) | 898 (23.5) | |
| Obese | 2553 (35.5) e | 3272 (37.7) | 1519 (39.8) d | |
| Living alone, yes | 167 (2.2) e | 862 (9.1) | 785 (18.9) d | <0.001 $ |
| Basic Livelihood Security, yes | 394 (5.2) e | 568 (6.0) | 301 (7.3) d | <0.001 $ |
| Hypertension, yes | 1644 (18.7) e | 1810 (20.6) | 727 (22.7) d | <0.001 $ |
| Dyslipidemia, yes | 1724 (17.7) e | 1766 (20.1) | 689 (23.8) d | <0.001 $ |
| Diabetes mellitus, yes | 655 (7.5) | 760 (8.7) | 293 (9.0) d | 0.027 $ |
| Sedentary time, hour/day | 7.3 ± 3.3 a,b | 7.8 ± 3.5 c | 8.3 ± 3.6 | <0.001 # |
| Fasting glucose, mg/dL | 101.9 ± 23.5 a,b | 102.8 ± 24.3 | 103.8 ± 27.3 | <0.001 # |
| Total cholesterol, mg/dL | 196.3 ± 38.3 b | 197.1 ± 37.2 c | 199.8 ± 38.3 | <0.001 # |
| Triglycerides, mg/dL | 132.5 ± 95.0 a,b | 145.6 ± 123.0 c | 151.3 ± 125.2 | <0.001 # |
| Total energy intake, kcal | 1860.1 ± 759.7 a,b | 2025.9 ± 895.7 | 1989.7 ± 900.6 | <0.001 # |
| Carbohydrate intake, g | 293.2 ± 122.2 a,b | 300.5 ± 124.9 c | 282.5 ± 119.6 | <0.001 # |
| Protein intake, g | 66.8 ± 32.3 a,b | 73.4 ± 43.4 | 71.6 ± 37.9 | <0.001 # |
| Fat intake, g | 40.2 ± 27.7 a,b | 45.8 ± 32.2 c | 47.5 ± 34.7 | <0.001 # |
| Cholesterol intake, mg | 224.0 ± 198.1 a,b | 254.2 ± 235.1 | 256.8 ± 226.6 | <0.001 # |
| Saturated fatty acid intake, g | 12.1 ± 9.5 a,b | 14.0 ± 10.8 c | 14.8 ± 11.9 | <0.001 # |
| Dietary fiber intake, g | 28.4 ± 15.0 a,b | 27.8 ± 14.3 c | 25.0 ± 13.0 | <0.001 # |
| Variable | Very Good (n = 7690) | Good (n = 4976) | Poor (n = 730) | p-Value |
|---|---|---|---|---|
| Age, year | 72.9 ± 5.0 a,b | 73.5 ± 5.1 c | 71.9 ± 5.2 | <0.001 # |
| Sex, female | 3949 (51.4) | 3240 (65.1) d | 412 (56.4) | <0.001 $ |
| BMI, kg/m2 | 24.0 ± 3.2 a,b | 24.2 ± 3.2 | 24.4 ± 3.3 | <0.001 # |
| BMI group, n (%) | 0.041 | |||
| Underweight | 208 (2.9) | 117 (2.5) | 25 (3.7) | |
| Normal | 2499 (36.1) d | 1519 (34.0) | 240 (31.3) | |
| Overweight | 1802 (23.9) | 1173 (25.4) | 179 (25.8) | |
| Obese | 2617 (37.1) | 1801 (38.1) | 235 (39.2) | |
| Living alone, yes | 250 (3.3) e | 2482 (49.9) | 385 (52.7) d | <0.001 $ |
| Basic Livelihood Security, yes | 518 (6.7) e | 767 (15.4) | 152 (20.9) d | <0.001 $ |
| Hypertension, yes | 4022 (55.1) e | 2797 (58.9) d | 368 (56.7) | <0.001 $ |
| Dyslipidemia, yes | 2473 (33.9) | 1669 (35.2) | 250 (36.5) | 0.197 $ |
| Diabetes mellitus, yes | 1574 (21.6) e | 1151 (24.3) d | 140 (20.4) | 0.001 $ |
| Sedentary time, hour/day | 8.1 ± 3.6 a,b | 8.8 ± 3.8 | 9.0 ± 4.0 | <0.001 # |
| Fasting glucose, mg/dL | 107.5 ± 25.7 a | 108.8 ± 27.5 | 108.3 ± 30.9 | 0.029 # |
| Total cholesterol, mg/dL | 180.1 ± 39 a,b | 182.4 ± 39.9 c | 187.5 ± 40.9 | <0.001 # |
| Triglycerides, mg/dL | 129.3 ± 73.7 | 130.8 ± 77.9 | 133.7 ± 110.2 | 0.277 # |
| Total energy intake, kcal | 1659.0 ± 658.5 a,b | 1557.5 ± 670.3 | 1556.1 ± 735.2 | <0.001 # |
| Carbohydrate intake, g | 284.8 ± 112.2 a,b | 266.5 ± 112.2 | 258.1 ± 124.2 | <0.001 # |
| Protein intake, g | 56.1 ± 27.8 a,b | 52.4 ± 28.8 | 53.1 ± 30.5 | <0.001 # |
| Fat intake, g | 28.3 ± 21.3 a | 26.8 ± 22.3 | 28.9 ± 23.6 | <0.001 # |
| Cholesterol intake, mg | 147.6 ± 158.0 | 142.0 ± 163.7 c | 158.6 ± 175.9 | 0.017 # |
| Saturated fatty acid intake, g | 8.2 ± 6.7 | 8.0 ± 7.0 c | 8.8 ± 7.6 | 0.003 # |
| Dietary fiber intake, g | 26.7 ± 14.8 a,b | 24.2 ± 14.4 c | 22.3 ± 14.1 | <0.001 # |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, S.; Park, H. Composite Meal-Related Behaviors and Health Indicators: Insight from Large-Scale Nationwide Data on Korean Adults. Nutrients 2025, 17, 2982. https://doi.org/10.3390/nu17182982
Bae S, Park H. Composite Meal-Related Behaviors and Health Indicators: Insight from Large-Scale Nationwide Data on Korean Adults. Nutrients. 2025; 17(18):2982. https://doi.org/10.3390/nu17182982
Chicago/Turabian StyleBae, Seongryu, and Hyuntae Park. 2025. "Composite Meal-Related Behaviors and Health Indicators: Insight from Large-Scale Nationwide Data on Korean Adults" Nutrients 17, no. 18: 2982. https://doi.org/10.3390/nu17182982
APA StyleBae, S., & Park, H. (2025). Composite Meal-Related Behaviors and Health Indicators: Insight from Large-Scale Nationwide Data on Korean Adults. Nutrients, 17(18), 2982. https://doi.org/10.3390/nu17182982







