Influence of Adherence to the Mediterranean Diet on Vascular Health and Healthy Aging in Women: Assessment Using CAVI
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Ethical Considerations
2.4. Variables and Measuring Instruments
2.4.1. Vascular Aging
2.4.2. Arterial Stiffness
2.4.3. Mediterranean Diet
2.4.4. Descriptives
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Characteristics of the Subjects Included with and Without Healthy Vascular Aging
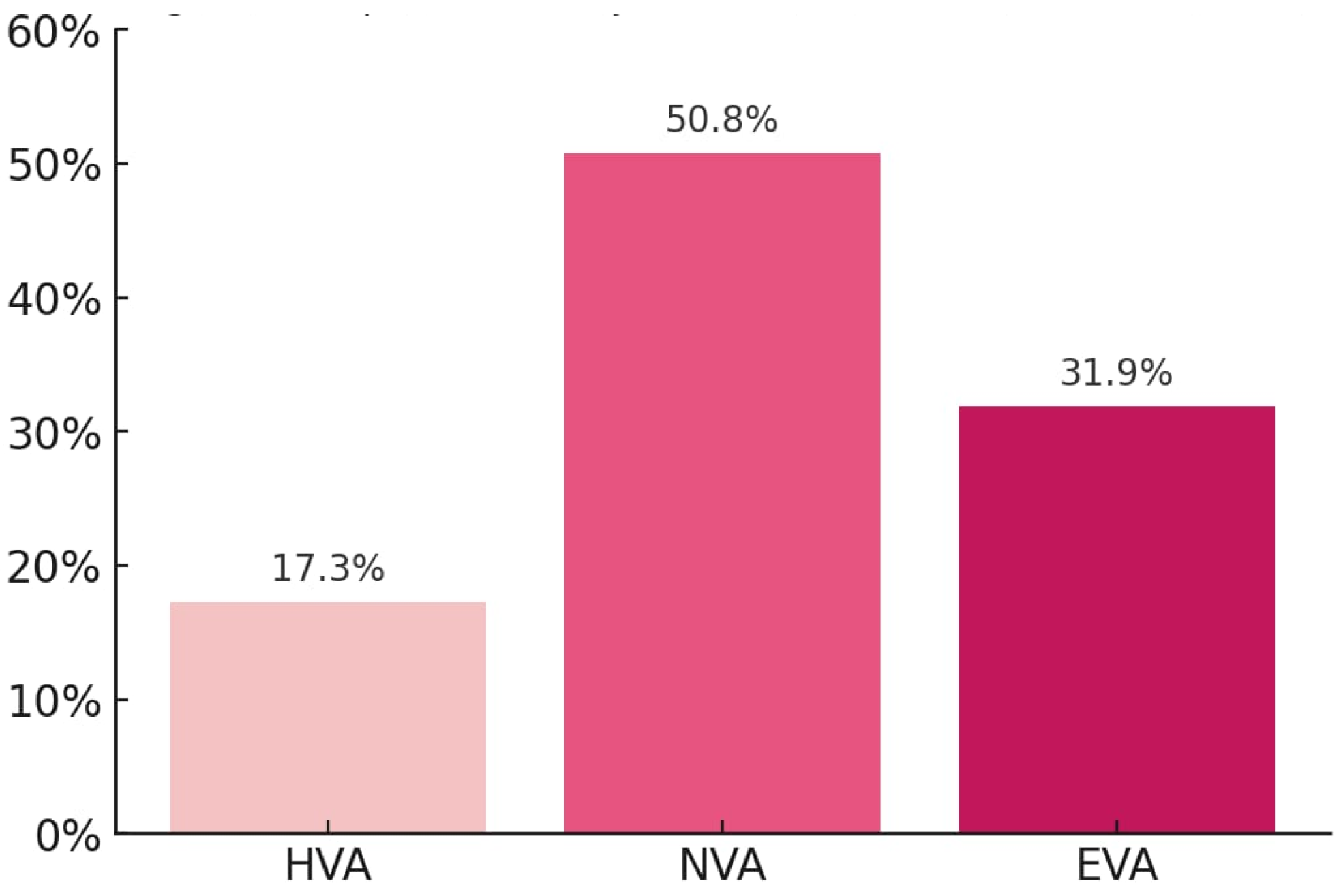
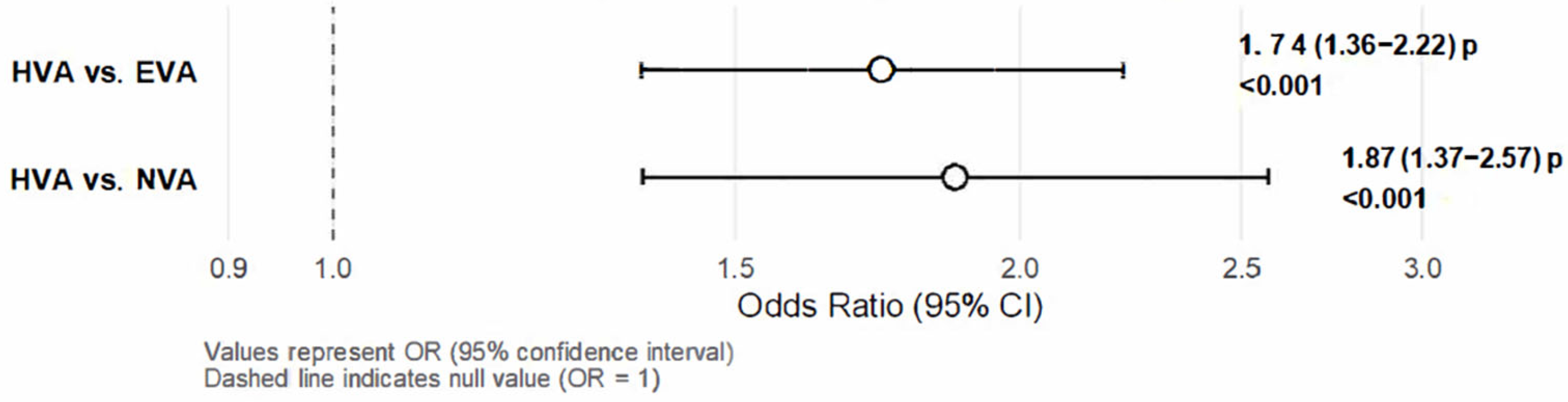
3.3. Association Between CAVI and MD Overall and by Sex Multinomial Logistic Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of Variance |
| BMI | Body Mass Index |
| CAVI | Cardio-Ankle Vascular Index |
| DBP | Diastolic blood pressure |
| EVA | Accelerated Vascular Aging |
| HDL-C | High-density Lipoprotein Cholesterol |
| HVA | Healthy Vascular Aging |
| LDL-C | Low-density Lipoprotein Cholesterol |
| MD | Mediterranean diet |
| NVA | Normal Vascular Aging |
| PCOS | Polycystic Ovary Syndrome |
| SBP | Systolic Blood Pressure |
References
- Martínez-Rodríguez, A.; Cuestas-Calero, B.J.; Martínez-Olcina, M.; Marcos-Pardo, P.J. Benefits of Adding an Aquatic Resistance Interval Training to a Nutritional Education on Body Composition, Body Image Perception and Adherence to the Mediterranean Diet in Older Women. Nutrients 2021, 13, 2712. [Google Scholar] [CrossRef]
- Vogel, B.; Acevedo, M.; Appelman, Y.; Merz, C.N.B.; Chieffo, A.; Figtree, G.A.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.H.E.M.; et al. The Lancet women and cardiovascular disease Commission: Reducing the global burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef]
- Colpani, V.; Baena, C.P.; Jaspers, L.; van Dijk, G.M.; Farajzadegan, Z.; Dhana, K.; Tielemans, M.J.; Voortman, T.; Freak-Poli, R.; Veloso, G.G.V.; et al. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: A systematic review and meta-analysis. Eur. J. Epidemiol. 2018, 33, 831–845. [Google Scholar] [CrossRef]
- Alonso-Domínguez, R.; Sánchez-Aguadero, N.; Patino-Alonso, M.C.; Agudo-Conde, C.; de Cabo-Laso, Á.; Gómez-Sánchez, M.; Gómez-Sánchez, L.; Rodríguez-Sánchez, E.; García-Ortiz, L.; Gómez-Marcos, M.A.; et al. Association between measurements of arterial stiffness and target organ damage in a general Spanish population. Ann. Med. 2021, 53, 345–356. [Google Scholar] [CrossRef]
- Maier, J.A.; Andrés, V.; Castiglioni, S.; Giudici, A.; Lau, E.S.; Nemcsik, J.; Seta, F.; Zaninotto, P.; Catalano, M.; Hamburg, N.M. Aging and Vascular Disease: A Multidisciplinary Overview. J. Clin. Med. 2023, 12, 5512. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.; Verma, H.K.; Lakkakula, S.; Merchant, N.; Kadir, F.; Rahman, S.; Jeffree, M.S.; Lakkakula, B.V.K.S.; Rao, P.V. Biomarkers of Oxidative Stress Tethered to Cardiovascular Diseases. Oxidative Med. Cell. Longev. 2022, 2022, 9154295. [Google Scholar] [CrossRef]
- Jebari-Benslaiman, S.; Galicia-García, U.; Larrea-Sebal, A.; Olaetxea, J.R.; Alloza, I.; Vandenbroeck, K.; Benito-Vicente, A.; Martín, C. Pathophysiology of Atherosclerosis. Int. J. Mol. Sci. 2022, 23, 3346. [Google Scholar] [CrossRef] [PubMed]
- Giani, A.; Micciolo, R.; Zoico, E.; Mazzali, G.; Zamboni, M.; Fantin, F. Cardio-Ankle Vascular Index and Aging: Differences between CAVI and CAVI0. J. Clin. Med. 2023, 12, 6726. [Google Scholar] [CrossRef]
- Silva, T.R.; Oppermann, K.; Reis, F.M.; Spritzer, P.M. Nutrition in Menopausal Women: A Narrative Review. Nutrients 2021, 13, 2149. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef] [PubMed]
- Menotti, A.; Puddu, P.E.; Kromhout, D.; Kafatos, A.; Tolonen, H. Coronary heart disease mortality trends during 50 years as explained by risk factor changes: The European cohorts of the Seven Countries Study. Eur. J. Prev. Cardiol. 2020, 27, 988–998. [Google Scholar] [CrossRef]
- Poorolajal, J.; Mohammadi, Y.; Fattahi-Darghlou, M.; Almasi-Moghadam, F. The association between major gastrointestinal cancers and red and processed meat and fish consumption: A systematic review and meta-analysis of the observational studies. PLoS ONE 2024, 19, e0305994. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Simonetta, I.; Daidone, M.; Mogavero, A.; Ortello, A.; Pinto, A. Metabolic and Vascular Effect of the Mediterranean Diet. Int. J. Mol. Sci. 2019, 20, 4716. [Google Scholar] [CrossRef]
- Richardson, L.A.; Izuora, K.; Basu, A. Mediterranean Diet and Its Association with Cardiovascular Disease Risk Factors: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 12762. [Google Scholar] [CrossRef]
- Mehta, L.S.; Velarde, G.P.; Lewey, J.; Sharma, G.; Navas-Acien, A.; Fretts, A.M.; Magwood, G.S.; Yang, E.; Blumenthal, R.S.; Brown, R.-M.; et al. Cardiovascular Disease Risk Factors in Women: The Impact of Race and Ethnicity: A Scientific Statement From the American Heart Association. Circulation 2023, 147, 1471–1487. [Google Scholar] [CrossRef]
- Guan, C.; Zahid, S.; Minhas, A.S.; Ouyang, P.; Vaught, A.; Baker, V.L.; Michos, E.D. Polycystic ovary syndrome: A “risk-enhancing” factor for cardiovascular disease. Fertil. Steril. 2022, 117, 924–935. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Marcos, M.A.; Martinez-Salgado, C.; Gonzalez-Sarmiento, R.; Hernandez-Rivas, J.M.; Sanchez-Fernandez, P.L.; Recio-Rodriguez, J.I.; Rodriguez-Sanchez, E.; García-Ortiz, L. Association between different risk factors and vascular accelerated ageing (EVA study): Study protocol for a cross-sectional, descriptive observational study. BMJ Open 2016, 6, e011031. [Google Scholar] [CrossRef] [PubMed]
- Martí, R.; Parramon, D.; García-Ortiz, L.; Rigo, F.; Gómez-Marcos, M.A.; Sempere, I.; García-Regalado, N.; Recio-Rodriguez, J.I.; Agudo-Conde, C.; Feuerbach, N.; et al. Improving interMediAte Risk management. MARK study. BMC Cardiovasc. Disord. 2011, 11, 61. [Google Scholar] [CrossRef]
- Recio-Rodríguez, J.I.; Martín-Cantera, C.; González-Viejo, N.; Gómez-Arranz, A.; Arietaleanizbeascoa, M.S.; Schmolling-Guinovart, Y.; Maderuelo-Fernandez, J.A.; Pérez-Arechaederra, D.; Rodriguez-Sanchez, E.; Gómez-Marcos, M.A.; et al. Effectiveness of a smartphone application for improving healthy lifestyles, a randomized clinical trial (EVIDENT II): Study protocol. BMC Public Health 2014, 14, 254. [Google Scholar] [CrossRef]
- Gómez-Sánchez, M.; Patino-Alonso, M.C.; Gómez-Sánchez, L.; Recio-Rodríguez, J.I.; Rodríguez-Sánchez, E.; Maderuelo-Fernández, J.A.; García-Ortiz, L.; Gómez-Marcos, M.A. Reference values of arterial stiffness parameters and their association with cardiovascular risk factors in the Spanish population. The EVA Study. Rev. Española Cardiol. 2020, 73, 43–52. [Google Scholar] [CrossRef]
- Ji, H.; Teliewubai, J.; Lu, Y.; Xiong, J.; Yu, S.; Chi, C.; Li, J.; Blacher, J.; Zhang, Y.; Xu, Y. Vascular aging and preclinical target organ damage in community-dwelling elderly. J. Hypertens. 2018, 36, 1391–1398. [Google Scholar] [CrossRef]
- Niiranen, T.J.; Lyass, A.; Larson, M.G.; Hamburg, N.M.; Benjamin, E.J.; Mitchell, G.F.; Vasan, R.S. Prevalence, Correlates, and Prognosis of Healthy Vascular Aging in a Western Community-Dwelling Cohort. Hypertension 2017, 70, 267–274. [Google Scholar] [CrossRef]
- Nilsson, P.M.; Laurent, S.; Cunha, P.G.; Olsen, M.H.; Rietzschel, E.; Franco, O.H.; Ryliškytė, L.; Strazhesko, I.; Vlachopoulos, C.; Chen, C.-H.; et al. Characteristics of healthy vascular ageing in pooled population-based cohort studies. J. Hypertens. 2018, 36, 2340–2349. [Google Scholar] [CrossRef]
- Gomez-Sanchez, M.; Gomez-Sanchez, L.; Patino-Alonso, M.C.; Cunha, P.G.; Recio-Rodriguez, J.I.; Alonso-Dominguez, R.; Sanchez-Aguadero, N.; Rodriguez-Sanchez, E.; Maderuelo-Fernandez, J.A.; Garcia-Ortiz, L.; et al. Vascular aging and its relationship with lifestyles and other risk factors in the general Spanish population: Early Vascular Ageing Study. J. Hypertens. 2020, 38, 1110–1122. [Google Scholar] [CrossRef]
- Namekata, T.; Suzuki, K.; Ishizuka, N.; Shirai, K. Establishing baseline criteria of cardio-ankle vascular index as a new indicator of arteriosclerosis: A cross-sectional study. BMC Cardiovasc. Disord. 2011, 11, 51. [Google Scholar] [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A Short Screener Is Valid for Assessing Mediterranean Diet Adherence Among Older Spanish Men and Women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Theodoridis, X.; Chourdakis, M.; Papaemmanouil, A.; Chaloulakou, S.; Georgakou, A.V.; Chatzis, G.; Triantafyllou, A. The Effect of Diet on Vascular Aging: A Narrative Review of the Available Literature. Life 2024, 14, 267. [Google Scholar] [CrossRef] [PubMed]
- Laporte, M.A.L.; Coutinho, T. Vascular Aging in Women. Can. J. Cardiol. 2024, 40, 1493–1495. [Google Scholar] [CrossRef]
- O’Neill, S.M.; Travers, C.M.; Otahal, P.; Khoo, S.K.; Sharman, J.E. Menopause and accelerated aortic stiffness. Maturitas 2024, 180, 107900. [Google Scholar] [CrossRef] [PubMed]
- Vallée, A. Menopause and arterial stiffness index: Insights from the women’s UK Biobank cohort. Maturitas 2025, 198, 108608. [Google Scholar] [CrossRef]
- Gavilán-Carrera, B.; Aguilera-Fernández, V.; Amaro-Gahete, F.J.; Rosales-Castillo, A.; Soriano-Maldonado, A.; Vargas-Hitos, J.A. Association of the Mediterranean diet with arterial stiffness, inflammation, and medication use in women with systemic lupus erythematosus: An exploratory study. J. Nutr. Biochem. 2024, 134, 109759. [Google Scholar] [CrossRef]
- Gil-Gutiérrez, R.; Medina-Martínez, I.; Quesada-Caballero, M.; de la Hera-Fernández, F.J.; Zamora-Pasadas, M.; Cantarero-Villanueva, I.; Albendín-García, L.; Parola, V.; Rueda-Medina, B.; Correa-Rodríguez, M. EFINUTRILES Study: Integrative Extra Virgin Olive Oil and Multimodal Lifestyle Interventions for Cardiovascular Health and SLE Management. Nutrients 2025, 17, 1076. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, A.; Nakamura, Y.; Kagiyama, N.; Sato, E.; Fujita, W.; Kaneko, T.; Minamino, T. Low Arterial Stiffness by Pulse Wave Analysis and Aortic Diseases. Circ. Rep. 2025, 7, 481–485. [Google Scholar] [CrossRef]
- Hersant, J.; Kruger, R.; Bianchini, E.; Königstein, K.; Sinha, M.D.; Hidvégi, E.V.; Kodithuwakku, V.; Mill, J.G.; Diaz, A.; Zócalo, Y.; et al. Measuring early vascular aging in youth: An expert consensus document from the Youth Vascular Consortium. J. Hypertens. 2025. [Google Scholar] [CrossRef] [PubMed]
- Shirai, K. Analysis of vascular function using the cardio–ankle vascular index (CAVI). Hypertens. Res. 2011, 34, 684–685. [Google Scholar] [CrossRef]
- Pagidipati, N.J.; Taub, P.R.; Ostfeld, R.J.; Kirkpatrick, C.F. Dietary patterns to promote cardiometabolic health. Nat. Rev. Cardiol. 2025, 22, 38–46. [Google Scholar] [CrossRef]
- Seth, C.; Schmid, V.; Mueller, S.; Haykowsky, M.; Foulkes, S.J.; Halle, M.; Wernhart, S. Diabetes, obesity, and cardiovascular disease—What is the impact of lifestyle modification? Herz 2025, 50, 240–245. [Google Scholar] [CrossRef]
- Rodríguez Núñez, S.; Rubín-García, M.; Martín-Sánchez, V.; Álvarez-Álvarez, L.; Molina, A.J. Mediterranean Diet, Obesity-Related Metabolic Cardiovascular Disorders, and Environmental Sustainability: A Systematic Review. Nutrients 2025, 17, 2005. [Google Scholar] [CrossRef]
- Estruch, R. Anti-inflammatory effects of the Mediterranean diet: The experience of the PREDIMED study. Proc. Nutr. Soc. 2010, 69, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Hu, F.B.; Martínez-González, M.A.; Fitó, M.; Bulló, M.; Estruch, R.; Ros, E.; Corella, D.; Recondo, J.; Gómez-Gracia, E.; et al. Olive oil intake and risk of cardiovascular disease and mortality in the PREDIMED Study. BMC Med. 2014, 12, 78. [Google Scholar] [CrossRef] [PubMed]
- Frank, G.; Pala, B.; Gualtieri, P.; Tocci, G.; La Placa, G.; Di Renzo, L. Adherence to Mediterranean Diet and Implications for Cardiovascular Risk Prevention. Nutrients 2025, 17, 1991. [Google Scholar] [CrossRef]
- Fujie, S.; Horii, N.; Kajimoto, H.; Yamazaki, H.; Inoue, K.; Iemitsu, K.; Uchida, M.; Arimitsu, T.; Shinohara, Y.; Sanada, K.; et al. Impact of resistance training and chicken intake on vascular and muscle health in elderly women. J. Cachexia Sarcopenia Muscle 2025, 16. [Google Scholar] [CrossRef]
- Zupo, R.; Castellana, F.; Lisco, G.; Corbo, F.; Crupi, P.; Sardone, R.; Catino, F.; Perna, S.; Gesualdo, L.; Lozupone, M.; et al. The Effect of a Mediterranean Diet on Arterial Stiffness: A Systematic Review. Nutrients 2025, 17, 1192. [Google Scholar] [CrossRef] [PubMed]
- Hauner, D.; Günther, J.; Schederecker, F.; Donik, L.; Meyer, D.; Hermsdörfer, J.; Friedl, T.W.; Rack, B.; Beckmann, M.W.; Janni, W.; et al. Effect of a comprehensive lifestyle intervention program on body weight and health behavior in women with breast cancer: Results from a randomized controlled trial. Clin. Nutr. 2024, 43, 1937–1951. [Google Scholar] [CrossRef] [PubMed]

| Total (n = 1468) | 30–40 (n = 69) | 40–50 (n = 143) | 50–60 (n = 434) | 60–70 (n = 583) | 70–80 (n = 239) | p Value | |
|---|---|---|---|---|---|---|---|
| Mediterranean Diet | |||||||
| MD (total score) | 6.03 ± 1.98 | 6.74 ± 0.24 | 6.36 ± 0.17 | 5.89 ± 0.09 | 5.87 ± 0.08 | 6.27 ± 0.13 | <0.001 |
| Adherence to MD, n (%) | 880 (59.9) | 31 (44.9) | 73 (51.0) | 265 (61.1) | 377 (64.7) | 134 (56.1) | 0.001 |
| Conventional risk factors | |||||||
| Age, (years) | 60.09 ± 9.71 | 35.97 ± 0.30 | 45.89 ± 0.21 | 55.51 ± 0.12 | 64.57 ± 0.10 | 72.93 ± 0.16 | <0.001 |
| SBP, (mmHg) | 128.72 ± 20.55 | 102.73 ± 2.31 | 117.96 ± 1.60 | 127.93 ± 0.92 | 131.07 ± 0.79 | 135.91 ± 1.24 | <0.001 |
| DBP, (mmHg) | 79.64 ± 10.84 | 68.86 ± 1.25 | 76.23 ± 0.87 | 82.23 ± 0.50 | 80.51 ± 0.43 | 77.98 ± 0.67 | <0.001 |
| Hypertension, n (%) | 1309 (89.2) | 68 (98.6) | 134 (93.7) | 383 (88.2) | 516 (88.5) | 208 (87.0) | 0.025 |
| Antihypertensive drugs, n (%) | 654 (44.6) | 1 (1.4) | 22 (15.4) | 175 (40.3) | 291 (49.9) | 165 (69.0) | <0.001 |
| Total cholesterol, (mg/dL) | 220.54 ± 42.47 | 182.13 ± 4.94 | 203.10 ± 3.43 | 226.35 ± 1.97 | 226.02 ± 1.70 | 218.16 ± 2.66 | <0.001 |
| LDL cholesterol, (mg/dL) | 132.53 ± 35.94 | 102.74 ± 4.28 | 122.60 ± 2.94 | 138.77 ± 1.70 | 135.61 ± 1.45 | 128.14 ± 2.27 | <0.001 |
| HDL cholesterol, (mg/dL) | 57.27 ± 15.77 | 61.98 ± 1.91 | 57.16 ± 1.32 | 56.87 ± 0.76 | 56.65 ± 0.65 | 58.20 ± 1.01 | 0.09 |
| Triglycerides, (mg/dL) | 122.63 ± 68.62 | 76.61 ± 8.18 | 101.79 ± 5.65 | 132.05 ± 3.24 | 125.33 ± 2.80 | 124.55 ± 4.36 | <0.001 |
| Dyslipidemia, n (%) | 1076 (73.3) | 19 (17.5) | 71 (49.7) | 317 (73.0) | 477 (81.8) | 192 (80.3) | <0.001 |
| Lipid–lowering drugs. n (%) | 429 (29.2) | 1 (1.4) | 13 (9.1) | 98 (22.6) | 207 (35.5) | 110 (46.9) | <0.001 |
| FPG, (mg/dL) | 100.24 ± 32.30 | 83.80 ± 3.82 | 85.64 ± 2.65 | 102.15 ± 1.53 | 103.40 ± 1.32 | 102.58 ± 2.05 | <0.001 |
| HbA1c | 5.93 ± 1.07 | 5.26 ± 0.13 | 5.39 ± 0.09 | 5.98 ± 0.05 | 6.07 ± 0.04 | 6.01 ± 0.07 | <0.001 |
| Diabetes mellitus, n (%) | 306 (20.8) | 2 (2.9) | 5 (3.5) | 92 (21.2) | 147 (25.2) | 60 (25.1) | <0.001 |
| Hypoglycemic drugs, n (%) | 234 (15.9) | 2 (2.9) | 4 (2.8) | 66 (15.2) | 107 (18.4) | 55 (23.0) | <0.001 |
| Weight, kg | 70.20 ± 13.31 | 63.91 ± 1.59 | 70.46 ± 1.10 | 71.31 ± 0.63 | 71.03 ± 0.55 | 67.81 ± 0.85 | <0.001 |
| Height, cm | 157.11 ± 6.67 | 162.10 ± 0.76 | 161.25 ± 0.53 | 158.24 ± 0.30 | 155.82 ± 0.26 | 154.29 ± 0.41 | <0.001 |
| BMI, (kg/m2) | 28.47 ± 5.30 | 24.35 ± 0.63 | 27.11 ± 0.43 | 28.49 ± 0.25 | 29.27 ± 0.21 | 28.48 ± 0.34 | <0.001 |
| WC, cm | 94.33 ± 12.90 | 82.84 ± 1.51 | 90.61 ± 1.06 | 93.61 ± 0.60 | 96.48 ± 0.52 | 95.91 ± 0.81 | <0.001 |
| Obesity, n (%) | 495 (33.7) | 9 (13.0) | 38 (26.6) | 152 (35.0) | 213 (36.5) | 83 (34.7) | 0.001 |
| Arterial stiffness | |||||||
| CAVI, m/second | 8.37 ± 1.24 | 6.58 ± 0.12 | 7.18 ± 0.09 | 8.10 ± 0.05 | 8.70 ± 0.04 | 9.29 ± 0.07 | <0.001 |
| (a) | ||||
| HVA (n = 254) | NVA (n = 746) | EVA (n = 468) | p Value | |
| Mediterranean Diet | ||||
| MD (total score) | 6.34 ± 0.12 | 6.12 ± 0.07 | 5.72 ± 0.09 | <0.001 |
| Adherence to MD, n (%) | 138 (34.3) | 419 (56.2) | 323 (69.0) | <0.001 |
| Conventional risk factors | ||||
| Age, (years) | 58.67 ± 0.61 | 60.39 ± 0.36 | 60.38 ± 0.45 | 0.038 |
| SBP, (mmHg) | 124.81 ± 1.27 | 127.02 ± 0.74 | 133.54 ± 0.94 | <0.001 |
| DBP, (mmHg) | 78.43 ± 0.67 | 78.67 ± 0.39 | 81.84 ± 0.50 | <0.001 |
| Hypertension, n (%) | 236 (92.9) | 672 (90.1) | 401 (85.7) | <0.006 |
| Antihypertensive drugs, n (%) | 112 (44.1) | 325 (43.6) | 217 (46.4) | 0.625 |
| Total cholesterol, (mg/dL) | 217.47 ± 2.66 | 218.39 ± 1.55 | 225.65 ± 1.96 | 0.007 |
| LDL cholesterol, (mg/dL) | 131.33 ± 2.27 | 131.50 ± 1.32 | 134.84 ± 1.67 | 0.246 |
| HDL cholesterol, (mg/dL) | 57.85 ± 0.99 | 57.43 ± 0.58 | 56.70 ± 0.73 | 0.598 |
| Triglycerides, (mg/dL) | 116.89 ± 4.30 | 120.62 ± 2.51 | 128.96 ± 3.17 | <0.041 |
| Dyslipidemia, n (%) | 165 (65.0) | 536 (71.8) | 375 (80.1) | <0.001 |
| Lipid–lowering drugs. n (%) | 61 (24.0) | 220 (29.5) | 148 (31.6) | 0.097 |
| FPG, (mg/dL) | 88.54 ± 2.00 | 100.10 ± 1.16 | 106.79 ± 1.47 | <0.001 |
| HbA1c | 5.47 ± 0.07 | 5.94 ± 0.04 | 6.16 ± 0.05 | <0.001 |
| Diabetes mellitus, n (%) | 0 (0.0) | 172 (23.1) | 134 (28.6) | <0.001 |
| Hypoglycemic drugs, n (%) | 0 (0.0) | 133 (17.8) | 101 (21.6) | <0.001 |
| Weight, kg | 73.85 ± 0.83 | 70.05 ± 0.48 | 68.45 ± 0.61 | <0.001 |
| Height, cm | 156.68 ± 0.42 | 154.86 ± 0.24 | 157.75 ± 0.31 | <0.004 |
| BMI, (kg/m2) | 30.08 ± 0.33 | 28.53 ± 0.19 | 27.52 ± 0.24 | <0.001 |
| WC, cm | 95.49 ± 0.81 | 94.22 ± 0.47 | 93.87 ± 0.60 | 0.262 |
| Obesity, n (%) | 11 (43.7) | 259 (34.7) | 125 (26.7) | <0.001 |
| Arterial stiffness | ||||
| CAVI, m/second | 6.95 ± 0.06 | 8.19 ± 0.03 | 9.44 ± 0.04 | <0.001 |
| (b) | ||||
| HVA vs. NVA | HVA vs. EVA | NVA vs. EVA | ||
| Mediterranean Diet | ||||
| Total cholesterol, (mg/dL) | 0.767 | 0.013 | 0.004 | |
| Triglycerides, (mg/dL) | 0.454 | 0.024 | 0.039 | |
| FPG, (mg/dL) | <0.001 | <0.001 | <0.001 | |
| HbA1c | <0.001 | <0.001 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llamas-Ramos, I.; Llamas-Ramos, R.; Rodríguez, M.C.; Rodríguez-Sánchez, E.; Gómez-Marcos, M.A.; Gómez-Sánchez, M.; Gómez-Sánchez, L. Influence of Adherence to the Mediterranean Diet on Vascular Health and Healthy Aging in Women: Assessment Using CAVI. Nutrients 2025, 17, 2963. https://doi.org/10.3390/nu17182963
Llamas-Ramos I, Llamas-Ramos R, Rodríguez MC, Rodríguez-Sánchez E, Gómez-Marcos MA, Gómez-Sánchez M, Gómez-Sánchez L. Influence of Adherence to the Mediterranean Diet on Vascular Health and Healthy Aging in Women: Assessment Using CAVI. Nutrients. 2025; 17(18):2963. https://doi.org/10.3390/nu17182963
Chicago/Turabian StyleLlamas-Ramos, Inés, Rocío Llamas-Ramos, María Cortés Rodríguez, Emiliano Rodríguez-Sánchez, Manuel A. Gómez-Marcos, Marta Gómez-Sánchez, and Leticia Gómez-Sánchez. 2025. "Influence of Adherence to the Mediterranean Diet on Vascular Health and Healthy Aging in Women: Assessment Using CAVI" Nutrients 17, no. 18: 2963. https://doi.org/10.3390/nu17182963
APA StyleLlamas-Ramos, I., Llamas-Ramos, R., Rodríguez, M. C., Rodríguez-Sánchez, E., Gómez-Marcos, M. A., Gómez-Sánchez, M., & Gómez-Sánchez, L. (2025). Influence of Adherence to the Mediterranean Diet on Vascular Health and Healthy Aging in Women: Assessment Using CAVI. Nutrients, 17(18), 2963. https://doi.org/10.3390/nu17182963







