The Accuracy of Potassium Content on Food Labels in Canada
Abstract
1. Introduction
2. Materials and Methods
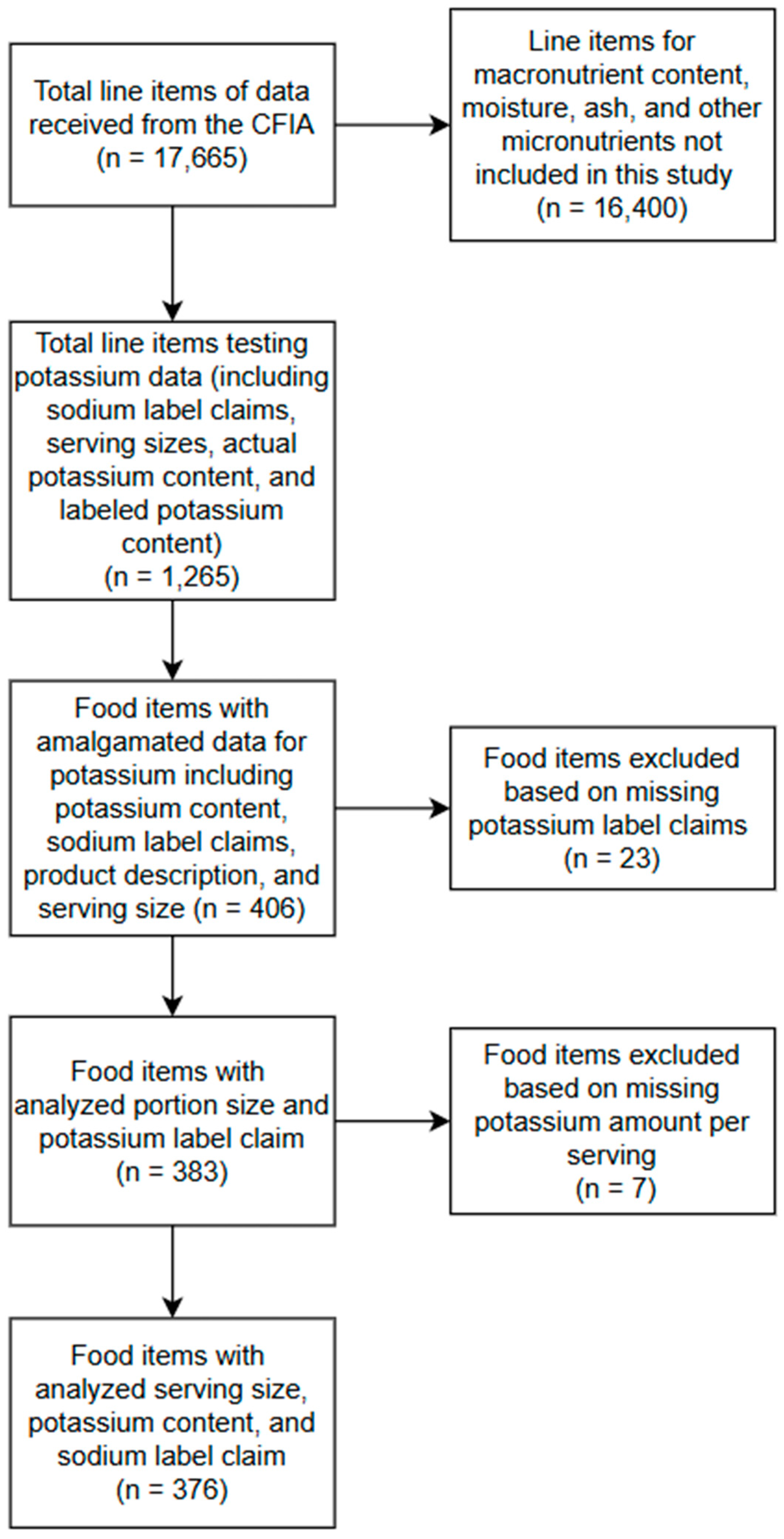
2.1. Study Design
2.2. CFIA Compliance Testing
2.3. Product Categorization
2.4. Statistical Analysis
3. Results
3.1. Number of Products Sampled
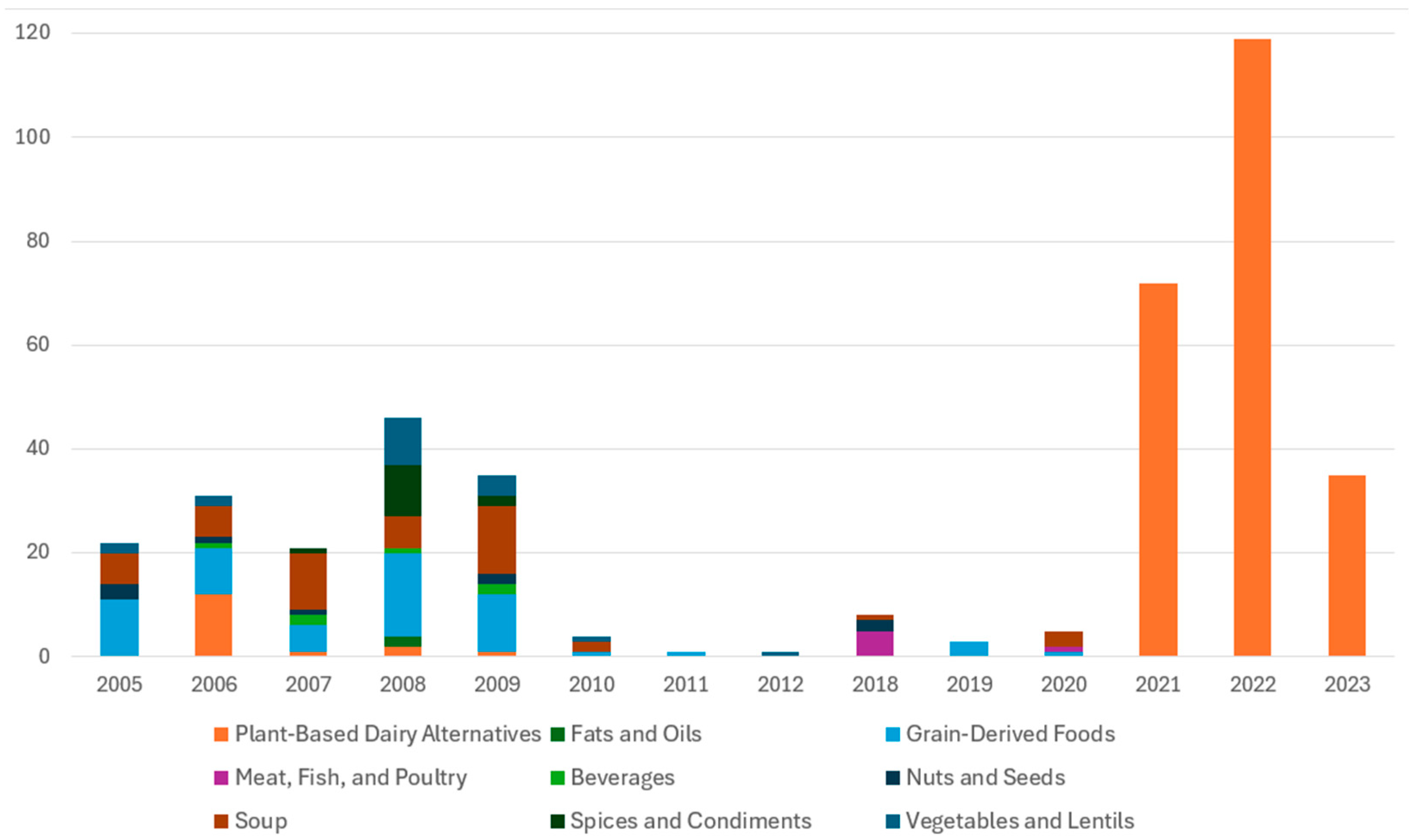
3.2. Types of Products Sampled
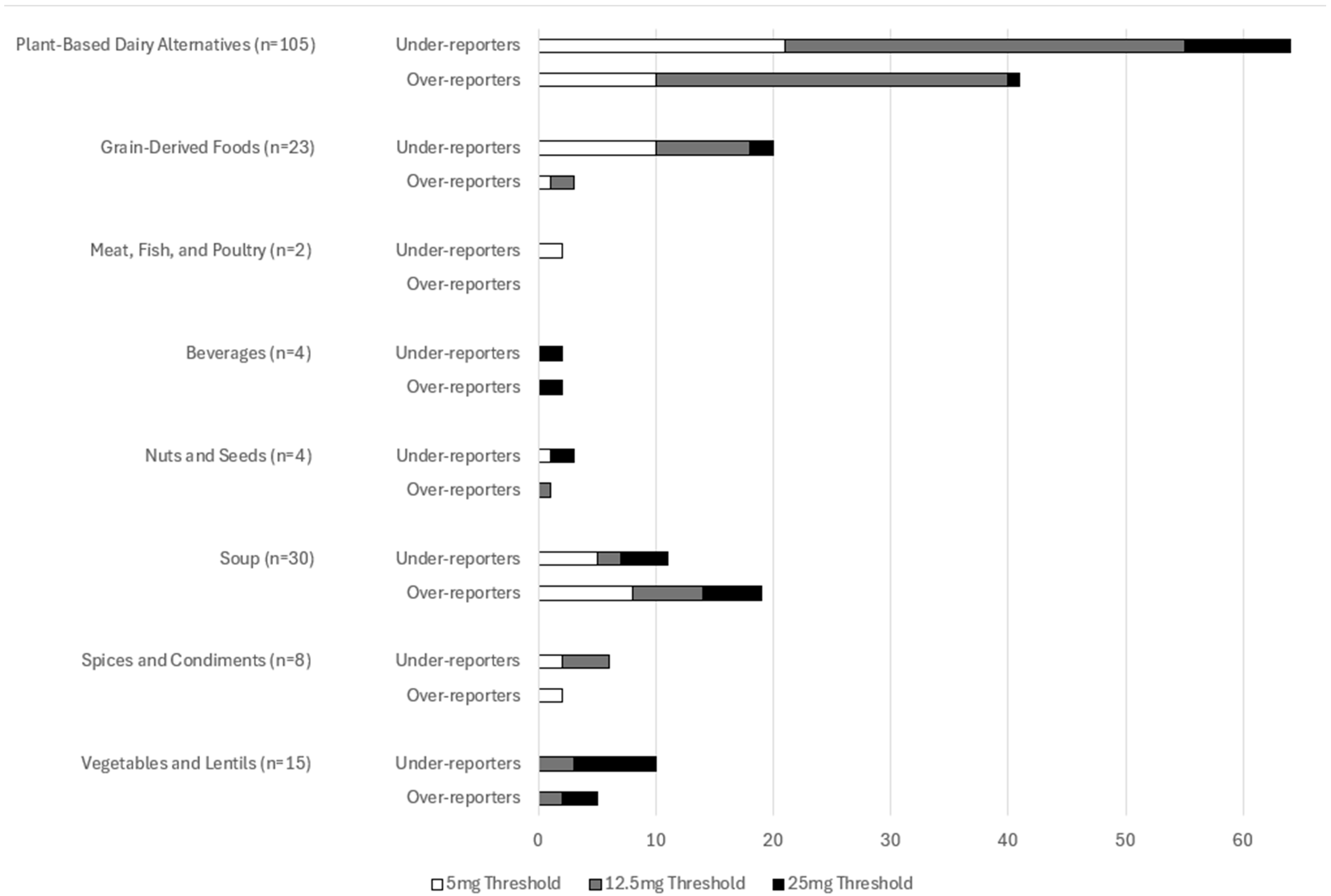
3.3. Products Meeting CFIA Compliance Standards
3.4. Levels of Agreement Between Analyzed and Labeled Potassium Content
3.5. Absolute Differences Between Labeled and Analyzed Potassium Content
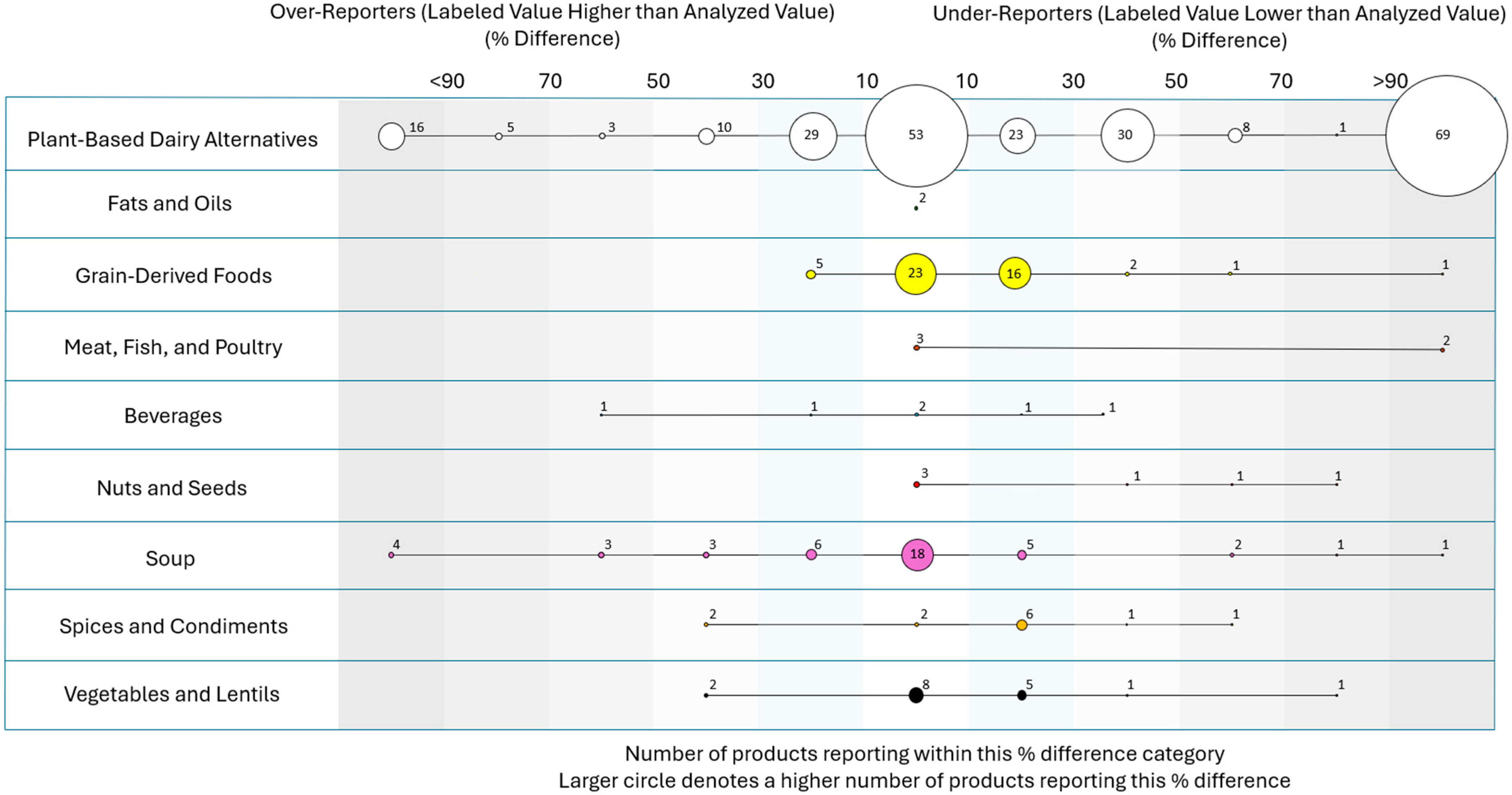
3.6. Percentage Differences Between Labeled and Analyzed Potassium Content
3.7. The Impact of Sample Year on Potassium
3.8. Sodium-Related Label Claims
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CFIA | Canadian Food Inspection Agency |
| CI | Confidence Interval |
| SD | Standard Deviation |
| mg | Milligram |
References
- Aburto, N.J.; Hanson, S.; Gutierrez, H.; Hooper, L.; Elliott, P.; Cappuccio, F.P. Effect of increased potassium intake on cardiovascular risk factors and disease: Systematic review and meta-analyses. BMJ 2013, 346, f1378. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.-J.; Lee, H.S.; Park, G.; Lee, J.-W. Association between dietary sodium, potassium, and the sodium-to-potassium ratio and mortality: A 10-year analysis. Front. Nutr. 2022, 9, 1053585. [Google Scholar] [CrossRef]
- Rabi, D.M.; McBrien, K.A.; Sapir-Pichhadze, R.; Nakhla, M.; Ahmed, S.B.; Dumanski, S.M.; Butalia, S.; Leung, A.A.; Harris, K.C.; Cloutier, L. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can. J. Cardiol. 2020, 36, 596–624. [Google Scholar] [CrossRef]
- D’Elia, L.; Barba, G.; Cappuccio, F.P.; Strazzullo, P. Potassium Intake, Stroke, and Cardiovascular Disease. J. Am. Coll. Cardiol. 2011, 57, 1210–1219. [Google Scholar] [CrossRef]
- Rosano, G.M.C.; Tamargo, J.; Kjeldsen, K.P.; Lainscak, M.; Agewall, S.; Anker, S.D.; Ceconi, C.; Coats, A.J.S.; Drexel, H.; Filippatos, G. Expert consensus document on the management of hyperkalaemia in patients with cardiovascular disease treated with renin angiotensin aldosterone system inhibitors: Coordinated by the Working Group on Cardiovascular Pharmacotherapy of the European Society of Cardiology. Eur. Heart J.–Cardiovasc. Pharmacother. 2018, 4, 180–188. [Google Scholar]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.-J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J. KDOQI clinical practice guideline for nutrition in CKD: 2020 update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Tobe, S.W.; Bajaj, H.S.; Tangri, N.; Jain, R.; Pham, T.; Beaudin, V.; McFarlane, P. Chronic Kidney Disease in Diabetes: A Clinical Practice Guideline. Can. J. Diabetes 2025, 49, 73–86.e14. [Google Scholar] [CrossRef] [PubMed]
- Viviana Viola, G.C.; Bianchi, F.; Croce, E.; Ceretti, E. Are Food Labels Effective as a Means of Health Prevention? J. Public Health Res. 2016, 5, jphr.2016.768. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, L.; Arcand, J.; L’Abbe, M.; Deng, M.; Duhaney, T.; Campbell, N. Accuracy of Canadian Food Labels for Sodium Content of Food. Nutrients 2014, 6, 3326–3335. [Google Scholar] [CrossRef]
- Regulations Amending the Food and Drug Regulations (Nutrition Labelling, Other Labelling Provisions and Food Colours). Government of Canada: Ottawa, ON, Canada, 2016. Available online: https://gazette.gc.ca/rp-pr/p2/2016/2016-12-14/html/sor-dors305-eng.html (accessed on 16 August 2025).
- Regulations and Compliance: Nutrition Labelling. Government of Canada, 2024. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/nutrition-labelling/regulations-compliance.html (accessed on 16 August 2025).
- Voluntary Sodium Reduction Goals: Target Mean and Upper Bound Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods: Guidance for Industry; US Department of Health and Human Services Food and Drug Administration Centre for Food Safety and Applied Nutrition: College Park, MD, USA, 2021.
- Picard, K.; Mager, D.R.; Senior, P.A.; Richard, C. Potassium-based sodium substitutes impact the sodium and potassium content of foods. J. Ren. Nutr. 2025, 35, 64–71. [Google Scholar] [CrossRef]
- Braschi, A.; Gill, L.; Naismith, D.J. Partial substitution of sodium with potassium in white bread: Feasibility and bioavailability. Int. J. Food Sci. Nutr. 2009, 60, 507–521. [Google Scholar] [CrossRef]
- Nutrition Labelling Compliance Test. Canadian Food Inspection Agency, Government of Canada, 2024. Available online: https://inspection.canada.ca/food-labels/labelling/industry/nutrition-labelling/additional-information/compliance-test/eng/1409949165321/1409949250097?chap=2#s10c2 (accessed on 27 August 2025).
- Monteiro, C.A.; Cannon, G.; Moubarac, J.-C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.C.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Health. Sodium Intake of Canadians in 2017. Health Canada Publications, 2018. Available online: https://www.canada.ca/content/dam/hc-sc/documents/services/publications/food-nutrition/sodium-intake-canadians-2017/2017-sodium-intakes-report-eng.pdf (accessed on 27 August 2025).
- Picard, K.; Picard, C.; Mager, D.R.; Richard, C. Potassium content of the American food supply and implications for the management of hyperkalemia in dialysis: An analysis of the Branded Product Database. Semin. Dial. 2024, 37, 307–316. [Google Scholar] [CrossRef]
- Islam, N.; Shafiee, M.; Vatanparast, H. Trends in the consumption of conventional dairy milk and plant-based beverages and their contribution to nutrient intake among Canadians. J. Hum. Nutr. Diet. 2021, 34, 1022–1034. [Google Scholar] [CrossRef]
- Health Canada Food Sampling and Testing Terminology. Government of Canada, Canadian Food Inspection Agency, 2019. Available online: https://inspection.canada.ca/en/food-safety-industry/food-chemistry-and-microbiology/food-safety-testing-reports-and-journal-articles/terminology (accessed on 16 August 2025).
- Fabiansson, S.U. Precision in nutritional information declarations on food labels in Australia. Asia Pac. J. Clin. Nutr. 2006, 15, 451–458. [Google Scholar]
- Parpia, A.S.; Darling, P.B.; L’Abbé, M.R.; Goldstein, M.B.; Arcand, J.; Cope, A.; Shaikh, A.-S. The accuracy of Canadian Nutrient File data for reporting phosphorus, potassium, sodium, and protein in selected meat, poultry, and fish products. Can. J. Public Health 2018, 109, 150–152. [Google Scholar] [CrossRef] [PubMed]
- D’Elia, L. Potassium Intake and Human Health. Nutrients 2024, 16, 833. [Google Scholar] [CrossRef] [PubMed]
- Hypertension Canada Organizational Position Statement: Dietary Potassium. 2019. Available online: https://hypertension.ca/wp-content/uploads/2019/01/Position-Statement-on-Dietary-Potassium-Hypertension-Canada-January-2019.pdf (accessed on 6 June 2025).
- Ahmed, M.; Ng, A.P.; L’Abbe, M.R. Nutrient intakes of Canadian adults: Results from the Canadian Community Health Survey (CCHS)–2015 Public Use Microdata File. Am. J. Clin. Nutr. 2021, 114, 1131–1140. [Google Scholar] [CrossRef]
- Hunter, R.W.; Bailey, M.A. Hyperkalemia: Pathophysiology, risk factors and consequences. Nephrol. Dial. Transplant. 2019, 34 (Suppl. 3), iii2–iii11. [Google Scholar] [CrossRef] [PubMed]
- Sevamontree, C.; Jintajirapan, S.; Phakdeekitcharoen, P.; Phakdeekitcharoen, B. The Prevalence and Risk Factors of Hyperkalemia in the Outpatient Setting. Int. J. Nephrol. 2024, 2024, 5694131. [Google Scholar] [CrossRef]
- Van Boemmel-Wegmann, S.; Bauer, C.; Schuchhardt, J.; Hartenstein, A.; James, G.; Pessina, E.; Beeman, S.; Edfors, R.; Pecoits-Filho, R. Hyperkalemia Incidence in Patients with Non-Dialysis Chronic Kidney Disease: A Large Retrospective Cohort Study from United States Clinical Care. Kidney Med. 2024, 6, 100879. [Google Scholar] [CrossRef]
- Betts, K.A.; Woolley, J.M.; Mu, F.; McDonald, E.; Tang, W.; Wu, E.Q. The prevalence of hyperkalemia in the United States. Curr. Med. Res. Opin. 2018, 34, 971–978. [Google Scholar] [CrossRef]
- Moranne, O.; Froissart, M.; Rossert, J.; Gauci, C.; Boffa, J.-J.; Haymann, J.P.; M’rad, M.B.; Jacquot, C.; Houillier, P.; Stengel, B.; et al. Timing of onset of CKD-related metabolic complications. J. Am. Soc. Nephrol. 2009, 20, 164–171. [Google Scholar] [CrossRef]
- Gilligan, S.; Raphael, K.L. Hyperkalemia and hypokalemia in CKD: Prevalence, risk factors, and clinical outcomes. Adv. Chronic Kidney Dis. 2017, 24, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P.; Matsushita, K.; Sang, Y.; Brunskill, N.J.; Carrero, J.J.; Chodick, G.; Hasegawa, T.; Heerspink, H.L.; Hirayama, A.; Landman, G.W.D.; et al. Serum potassium and adverse outcomes across the range of kidney function: A CKD Prognosis Consortium meta-analysis. Eur. Heart J. 2018, 39, 1535–1542. [Google Scholar] [CrossRef]
- Agiro, A.; Mu, F.; Cook, E.; Greatsinger, A.; Chen, J.; Zhao, A.; Louden, E.; Colman, E.; Desai, P.; Chertow, G.M. Hyperkalemia and the Risks of Adverse Cardiovascular Outcomes in Patients with Chronic Kidney Disease. J. Am. Heart Assoc. 2025, 14, e035256. [Google Scholar] [CrossRef]
- Kanda, E.; Rastogi, A.; Murohara, T.; Lesén, E.; Agiro, A.; Arnold, M.; Chen, G.; Yajima, T.; Järbrink, K.; Pollack, C.V. Clinical impact of suboptimal RAASi therapy following an episode of hyperkalemia. BMC Nephrol. 2023, 24, 18. [Google Scholar] [CrossRef] [PubMed]
- Canadian Nutrient File. Government of Canada, 2018; Volume 2021. Available online: https://food-nutrition.canada.ca/cnf-fce/index-eng.jsp (accessed on 16 August 2025).
- Hoy, M.K.; Goldman, J.D.; Moshfegh, A. Potassium Intake of the U.S. Population: What We Eat in America, NHANES 2017-2018. In FSRG Dietary Data Briefs; United States Department of Agriculture (USDA): Beltsville, MD, USA, 2010. Available online: http://www.ncbi.nlm.nih.gov/books/NBK587683/ (accessed on 16 August 2025).
- Noori, N.; Kalantar-Zadeh, K.; Kovesdy, C.P.; Murali, S.B.; Bross, R.; Nissenson, A.R.; Kopple, J.D. Dietary potassium intake and mortality in long-term hemodialysis patients. Am. J. Kidney Dis. 2010, 56, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Guidance for the Food Industry on Reducing Sodium in Processed Foods. Government of Canada, Food Directorate Health Products, 2012. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/legislation-guidelines/guidance-documents/guidance-food-industry-reducing-sodium-processed-foods-2012.html (accessed on 16 August 2025).
- Voluntary Sodium Reduction Targets for Processed Foods 2020–2025. Government of Canada, 2022. Available online: https://www.canada.ca/en/health-canada/services/publications/food-nutrition/sodium-reduced-targets-2020-2025.html (accessed on 16 August 2025).
- Guide to Developing Accurate Nutrient Value. Health Canada, 2007; p. 103. Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/hpfb-dgpsa/pdf/label-etiquet/guide-nutri_val_tc-tm-eng.pdf (accessed on 16 August 2025).
- Picard, K.; Morris, A. Potassium Food Additives and Dietary Management of Serum Potassium: Proposed Best-Practice Recommendations. J. Ren. Nutr. 2025, 35, 221–228. [Google Scholar] [CrossRef]
- Nutrition Labelling—Table of Reference Amounts for Food. Health Canada, 2024. Available online: https://www.canada.ca/en/health-canada/services/technical-documents-labelling-requirements/nutrition-labelling-table-reference-amounts-food.html#b (accessed on 16 August 2025).
| Product Class | Product Subclasses |
|---|---|
| Dairy Analogs (n = 243) | Plant-Based Milks (n = 16) |
| |
| Plant-Based Cheese (n = 226) Pudding (n = 1) | |
| Fats and Oils (n = 2) | Extra Virgin Olive Oil (n = 2) |
| Grain-Derived Foods (n = 58) | Cereals (n = 15) |
| |
| Cookies and Crackers (n = 26) | |
| |
| Pasta and Rice (n = 5) | |
| |
| Grain-Based Snack Goods (e.g., popcorn) (n = 2) Breads and Bread Products (n = 10) | |
| |
| Meat, Fish, and Poultry (n = 5) | Sausages (n = 2) |
| |
| Canned Salmon and Tuna (n = 3) | |
| |
| Non-alcoholic Beverages (n = 6) | Soda (n = 3) |
| |
| Juice (n = 1) Coconut Water (n = 1) Breakfast Drink Mix (n = 1) | |
| Nuts and Seeds (n = 9) | Peanut Butter (n = 4) |
| |
| Sunflower and Pumpkin Seeds (n = 3) | |
| |
| Almonds and Soy Nuts (n = 2) | |
| |
| Soups (n = 50) | Broth (n = 32) |
| |
| Canned Soups and Soup Mixes (n = 18) | |
| |
| Spices and Condiments (n = 13) | Gravy, Sauces, and Condiments (n = 9) |
| |
| Spice Blends (n = 4) | |
| |
| Vegetable- and Lentil-Based Products (n = 19) | Lentils or Beans (n = 5) |
| |
| Vegetable Juices (n = 10) | |
| |
| Plantain Chips (n = 1) Canned Tomatoes (n = 1) Seasoned Ground Soy/Simulated Meat Product (n = 1) |
| Sodium Content Claim | Mean Analyzed Potassium Content, mg per Serving (SD) | Mean Labeled Potassium Content, mg per Serving (SD) | Difference, mg per Serving (SD) | p-Value | N of Accurate Reporters | N of Inaccurate Reports |
|---|---|---|---|---|---|---|
| No Sodium-Related Claim (n = 292) | 93 (137) | 77 (118) | 14 (60) | <0.001 | 120 (41%) | 172 (59%) |
| Sodium Content Claim (n = 97) | 268 (318) | 254 (300) | 14 mg (77) | <0.001 | 55 (62%) | 34 (38%) |
| 354 (319 mg) | 322 (304 mg) | 31 (86) | 0.038 | 25 (71.4%) | 10 (28.6%) |
| 442 (513) | 428 (540) | 13 (40) | 0.377 | 7 (87.5%) | 1 (12.5%) |
| 173 (245) | 171 (210) | 2 (73) | 0.865 | 23 (50%) | 23 (50%) |
| 176 (126) | 108 (51) | 69 (164) | 0.275 | 7 (87.5%) | 1 (12.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Picard, K.; Renouf, D.; Draheim, S.; Picard, C.; Wong, M.M.Y. The Accuracy of Potassium Content on Food Labels in Canada. Nutrients 2025, 17, 2935. https://doi.org/10.3390/nu17182935
Picard K, Renouf D, Draheim S, Picard C, Wong MMY. The Accuracy of Potassium Content on Food Labels in Canada. Nutrients. 2025; 17(18):2935. https://doi.org/10.3390/nu17182935
Chicago/Turabian StylePicard, Kelly, Dani Renouf, Sarah Draheim, Christopher Picard, and Michelle M. Y. Wong. 2025. "The Accuracy of Potassium Content on Food Labels in Canada" Nutrients 17, no. 18: 2935. https://doi.org/10.3390/nu17182935
APA StylePicard, K., Renouf, D., Draheim, S., Picard, C., & Wong, M. M. Y. (2025). The Accuracy of Potassium Content on Food Labels in Canada. Nutrients, 17(18), 2935. https://doi.org/10.3390/nu17182935






