Plant-Based Dietary Patterns and the Risk of Cardiovascular Disease in Middle-Aged Korean Adults: A Community-Based Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
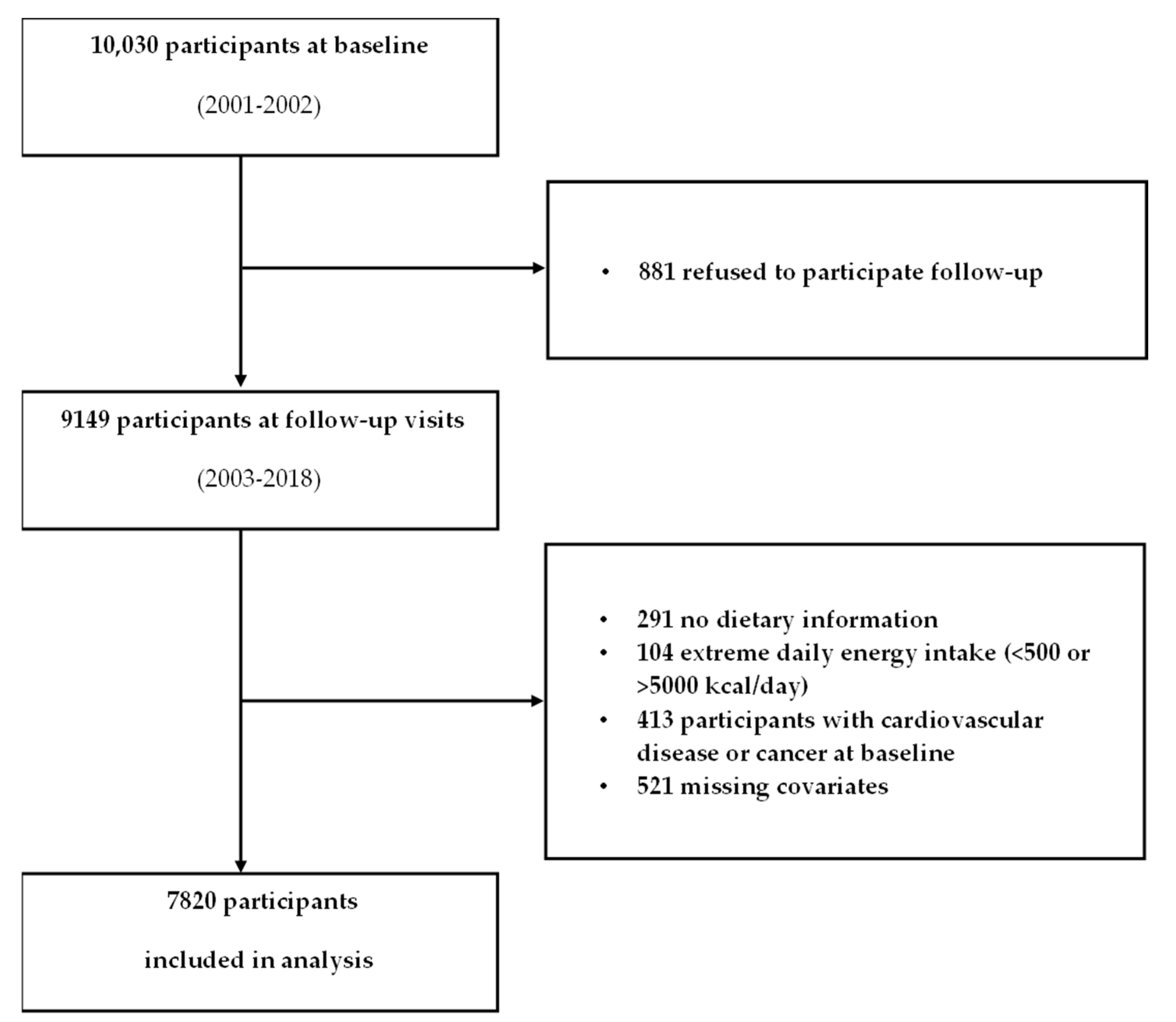
2.1. Study Design and Population
2.2. Calculation of Plant-Based Diet Index Scores
2.3. Ascertainment of Cardiovascular Disease
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Nutrient Intakes Across Quartiles of Plant-Based Diet Indices
3.3. Association of Plant-Based Diet Indices with CVD
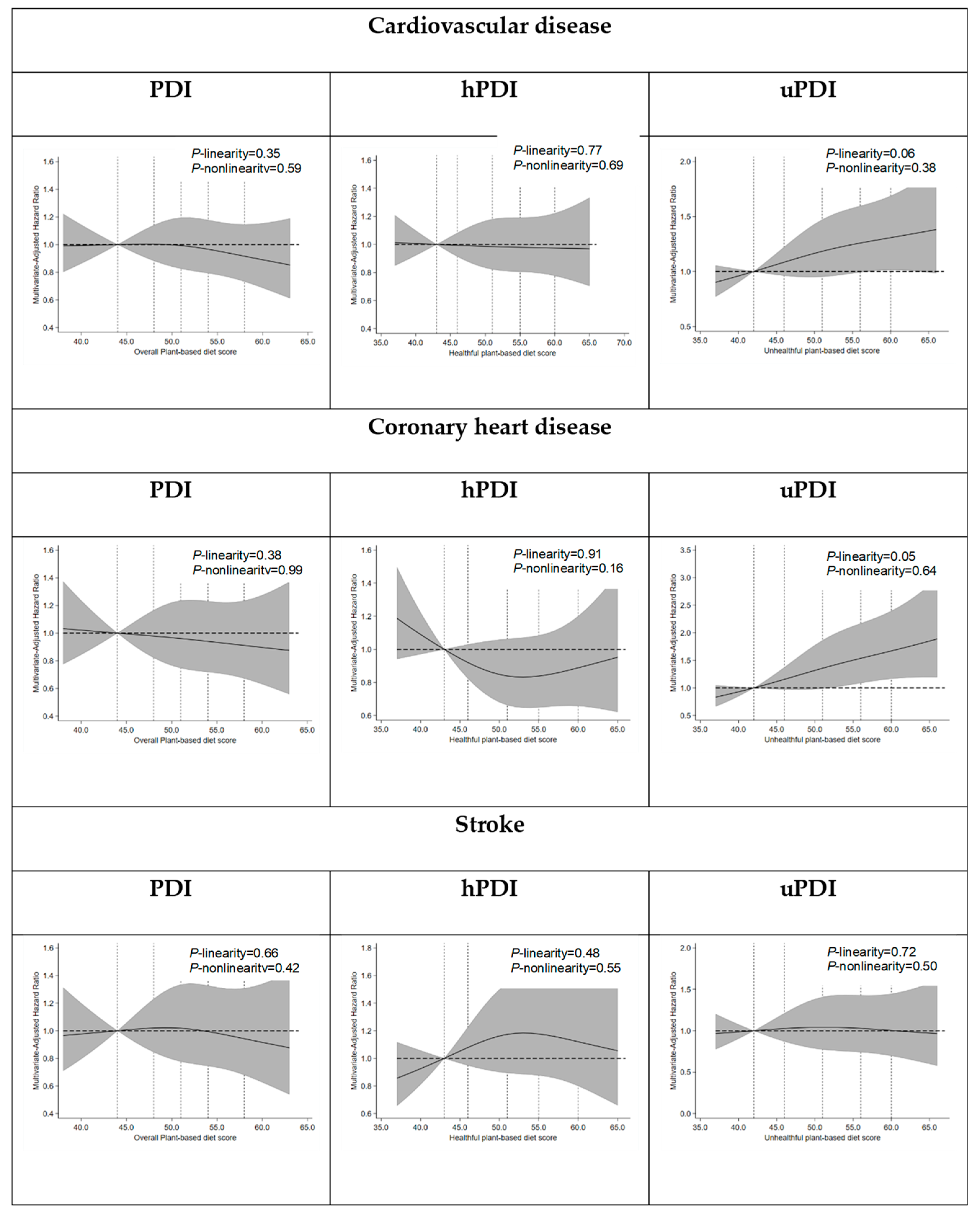
3.4. Exploratory and Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PDI | Overall Plant-based Diet Index |
| hPDI | Healthful Plant-based Diet Index |
| uPDI | Unhealthful Plant-based Diet Index |
References
- Mensah, G.A.; Fuster, V.; Murray, C.J.L.; Roth, G.A. Global Burden of Cardiovascular Diseases and Risks, 1990–2022. J. Am. Coll. Cardiol. 2023, 82, 2350–2473. [Google Scholar] [CrossRef]
- Seo, A.R.; Hwang, T.Y. Relationship between Dietary Patterns and Cardiovascular Disease Risk in Korean Older Adults. Int. J. Environ. Res. Public Health 2021, 18. [Google Scholar] [CrossRef]
- Satija, A.; Hu, F.B. Plant-based diets and cardiovascular health. Trends Cardiovasc. Med. 2018, 28, 437–441. [Google Scholar] [CrossRef]
- Springmann, M.; Godfray, H.C.; Rayner, M.; Scarborough, P. Analysis and valuation of the health and climate change cobenefits of dietary change. Proc. Natl. Acad. Sci. USA 2016, 113, 4146–4151. [Google Scholar] [CrossRef]
- Sleiman, D.; Al-Badri, M.R.; Azar, S.T. Effect of mediterranean diet in diabetes control and cardiovascular risk modification: A systematic review. Front. Public Health 2015, 3, 69. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Pozo, V.A.; Guevara-Ramírez, P.; Paz-Cruz, E.; Tamayo-Trujillo, R.; Cadena-Ullauri, S.; Frias-Toral, E.; Simancas-Racines, D.; Altuna-Roshkova, Y.; Reytor-González, C.; Zambrano, A.K.J.F.; et al. The role of the Mediterranean diet in prediabetes management and prevention: A review of molecular mechanisms and clinical outcomes. Food Agric. Immunol. 2024, 35, 2398042. [Google Scholar] [CrossRef]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.J.; Forouhi, N.G.; Ye, Z.; Buijsse, B.; Arriola, L.; Balkau, B.; Barricarte, A.; Beulens, J.W.; Boeing, H.; Büchner, F.L.; et al. Fruit and vegetable intake and type 2 diabetes: EPIC-InterAct prospective study and meta-analysis. Eur. J. Clin. Nutr. 2012, 66, 1082–1092. [Google Scholar] [CrossRef]
- Micha, R.; Penalvo, J.L.; Cudhea, F.; Imamura, F.; Rehm, C.D.; Mozaffarian, D. Association Between Dietary Factors and Mortality From Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA 2017, 317, 912–924. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G.; Lampousi, A.M.; Knuppel, S.; Iqbal, K.; Schwedhelm, C.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of type 2 diabetes mellitus: A systematic review and meta-analysis of prospective studies. Eur. J. Epidemiol. 2017, 32, 363–375. [Google Scholar] [CrossRef]
- Ma, H.; Wang, X.; Li, X.; Heianza, Y.; Qi, L. Adding Salt to Foods and Risk of Cardiovascular Disease. J. Am. Coll. Cardiol. 2022, 80, 2157–2167. [Google Scholar] [CrossRef] [PubMed]
- Satija, A.; Bhupathiraju, S.N.; Spiegelman, D.; Chiuve, S.E.; Manson, J.E.; Willett, W.; Rexrode, K.M.; Rimm, E.B.; Hu, F.B. Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults. J. Am. Coll. Cardiol. 2017, 70, 411–422. [Google Scholar] [CrossRef]
- Kim, H.; Caulfield, L.E.; Garcia-Larsen, V.; Steffen, L.M.; Coresh, J.; Rebholz, C.M. Plant-Based Diets Are Associated With a Lower Risk of Incident Cardiovascular Disease, Cardiovascular Disease Mortality, and All-Cause Mortality in a General Population of Middle-Aged Adults. J. Am. Heart Assoc. 2019, 8, e012865. [Google Scholar] [CrossRef]
- Weston, L.J.; Kim, H.; Talegawkar, S.A.; Tucker, K.L.; Correa, A.; Rebholz, C.M. Plant-based diets and incident cardiovascular disease and all-cause mortality in African Americans: A cohort study. PLoS Med. 2022, 19, e1003863. [Google Scholar] [CrossRef]
- Kouvari, M.; Tsiampalis, T.; Chrysohoou, C.; Georgousopoulou, E.; Skoumas, J.; Mantzoros, C.S.; Pitsavos, C.S.; Panagiotakos, D.B. Quality of plant-based diets in relation to 10-year cardiovascular disease risk: The ATTICA cohort study. Eur. J. Nutr. 2022, 61, 2639–2649. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.S.; Tresserra-Rimbau, A.; Karavasiloglou, N.; Jennings, A.; Cantwell, M.; Hill, C.; Perez-Cornago, A.; Bondonno, N.P.; Murphy, N.; Rohrmann, S.; et al. Association of Healthful Plant-based Diet Adherence with Risk of Mortality and Major Chronic Diseases Among Adults in the UK. JAMA Netw. Open 2023, 6, e234714. [Google Scholar] [CrossRef]
- Kim, Y.; Han, B.G. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int. J. Epidemiol. 2017, 46, e20. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Ahn, Y.; Kwon, E.; Shim, J.E.; Park, M.K.; Joo, Y.; Kimm, K.; Park, C.; Kim, D.H. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur. J. Clin. Nutr. 2007, 61, 1435–1441. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-J.; Lyu, J.; Lee, K.; Lee, H.-J.; Park, H.-Y. Nutrition survey methods and food composition database update of the Korean Genome and Epidemiology Study. Epidemiol. Health 2024, 46, e2024042. [Google Scholar] [CrossRef]
- Kim, J.; Giovannucci, E. Healthful Plant-Based Diet and Incidence of Type 2 Diabetes in Asian Population. Nutrients 2022, 14, 3078. [Google Scholar] [CrossRef]
- Kim, H.; Lee, K.; Rebholz, C.M.; Kim, J. Plant-based diets and incident metabolic syndrome: Results from a South Korean prospective cohort study. PLoS Med. 2020, 17, e1003371. [Google Scholar] [CrossRef]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, S1220–S1228. [Google Scholar] [CrossRef]
- Hu, F.B.; Stampfer, M.J.; Rimm, E.; Ascherio, A.; Rosner, B.A.; Spiegelman, D.; Willett, W.C. Dietary fat and coronary heart disease: A comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am. J. Epidemiol. 1999, 149, 531–540. [Google Scholar] [CrossRef]
- Suh, S.; Baek, J.; Bae, J.C.; Kim, K.-N.; Park, M.K.; Kim, D.K.; Cho, N.H.; Lee, M.-K. Sex Factors in the Metabolic Syndrome as a Predictor of Cardiovascular Disease. Endocrinol. Metab. 2014, 29, 522–529. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef]
- Jang, M.; Won, J.; Choi, H.; Kim, S.; Park, W.; Kim, D.; Jung, S.; Kim, B. Effects of Physical Activity on Fractures in Adults: A Community-Based Korean Cohort Study. Korean J. Sports Med. 2017, 35, 97–102. [Google Scholar] [CrossRef]
- Grambsch, P.M.; Therneau, T.M. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994, 81, 515–526. [Google Scholar] [CrossRef]
- Zhang, S.; Jiang, Y.; Wang, H.; Liu, Q.; He, X.; Pan, M.; Chen, Y.; Xiong, J.; Chen, Z.; Liu, P.; et al. Associations between plant-based diets and cardiovascular disease, frailty, and cognitive dysfunction in middle and old age: A systematic review and meta-analysis of cohort studies. Food Funct. 2025, 16, 4061–4084. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Andrews, K.G.; Engell, R.E.; Mozaffarian, D. Global, regional and national consumption of major food groups in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open 2015, 5, e008705. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1. [Google Scholar] [CrossRef]
- Baden, M.Y.; Shan, Z.; Wang, F.; Li, Y.; Manson, J.E.; Rimm, E.B.; Willett, W.C.; Hu, F.B.; Rexrode, K.M. Quality of Plant-Based Diet and Risk of Total, Ischemic, and Hemorrhagic Stroke. Neurology 2021, 96, e1940–e1953. [Google Scholar] [CrossRef]
- Petrie, J.R.; Guzik, T.J.; Touyz, R.M. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 2018, 34, 575–584. [Google Scholar] [CrossRef]
- Alfaddagh, A.; Martin, S.S.; Leucker, T.M.; Michos, E.D.; Blaha, M.J.; Lowenstein, C.J.; Jones, S.R.; Toth, P.P. Inflammation and cardiovascular disease: From mechanisms to therapeutics. Am. J. Prev. Cardiol. 2020, 4, 100130. [Google Scholar] [CrossRef]
- Micha, R.; Shulkin, M.L.; Peñalvo, J.L.; Khatibzadeh, S.; Singh, G.M.; Rao, M.; Fahimi, S.; Powles, J.; Mozaffarian, D. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS ONE 2017, 12, e0175149. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Nan, F.; Liang, H.; Shu, P.; Fan, X.; Song, X.; Hou, Y.; Zhang, D. Excessive intake of sugar: An accomplice of inflammation. Front. Immunol. 2022, 13, 988481. [Google Scholar] [CrossRef]
- Alba, B.K.; Stanhewicz, A.E.; Dey, P.; Bruno, R.S.; Kenney, W.L.; Alexander, L.M. Controlled feeding of an 8-d, high-dairy cheese diet prevents sodium-induced endothelial dysfunction in the cutaneous microcirculation of healthy, older adults through reductions in superoxide. J. Nutr. 2020, 150, 55–63. [Google Scholar] [CrossRef]
- Kieffer, D.A.; Piccolo, B.D.; Vaziri, N.D.; Liu, S.; Lau, W.L.; Khazaeli, M.; Nazertehrani, S.; Moore, M.E.; Marco, M.L.; Martin, R.J.; et al. Resistant starch alters gut microbiome and metabolomic profiles concurrent with amelioration of chronic kidney disease in rats. Am. J. Physiol. Ren. Physiol. 2016, 310, F857–F871. [Google Scholar] [CrossRef] [PubMed]
- Price, N.L.; Gomes, A.P.; Ling, A.J.; Duarte, F.V.; Martin-Montalvo, A.; North, B.J.; Agarwal, B.; Ye, L.; Ramadori, G.; Teodoro, J.S.; et al. SIRT1 is required for AMPK activation and the beneficial effects of resveratrol on mitochondrial function. Cell Metab. 2012, 15, 675–690. [Google Scholar] [CrossRef] [PubMed]
| PDI | hPDI | uPDI | ||||
|---|---|---|---|---|---|---|
| Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | |
| Sample size, n (1) | 2425 | 1922 | 1963 | 1913 | 2099 | 1633 |
| Median score (range) | 46 (31–48) | 57 (55–70) | 44 (29–46) | 59 (56–74) | 43 (30–46) | 60 (57–75) |
| Women, n (%) | 1129 (46.6) | 1083 (56.4) | 765 (39.1) | 1215 (63.5) | 1359 (64.8) | 678 (41.5) |
| Age, years | 50.3 ± 8.5 | 53.4 ± 9.0 | 50.3 ± 8.8 | 53.2 ± 8.7 | 49.9 ± 8.1 | 53.1 ± 9.0 |
| Residential area, n (%) | ||||||
| Rural, Ansung | 1055 (43.5) | 1045 (54.4) | 772 (39.3) | 1022 (53.4) | 569 (27.1) | 1161 (71.1) |
| Urban, Ansan | 1370 (56.5) | 877 (45.6) | 1191 (60.7) | 891 (46.6) | 1530 (72.9) | 742 (28.9) |
| Income (KRW/month), n (%) | ||||||
| <1,000,000 | 646 (26.6) | 772 (40.2) | 527 (26.9) | 716 (37.4) | 422 (20.1) | 735 (45.0) |
| 1,000,000 to <2,000,000 | 737 (30.4) | 545 (28.4) | 583 (29.7) | 584 (30.5) | 587 (28.0) | 505 (30.9) |
| 2,000,000 to <3,000,000 | 522 (21.5) | 315 (16.4) | 423 (21.6) | 313 (16.4) | 514 (24.5) | 222 (13.6) |
| ≥3,000,000 | 520 (21.4) | 290 (15.1) | 430 (21.9) | 300 (15.7) | 576 (27.4) | 171 (10.5) |
| Education level, n (%) | ||||||
| ≤Elementary school | 571 (23.6) | 784 (40.8) | 504 (25.7) | 714 (37.3) | 401 (19.1) | 679 (41.6) |
| Middle school | 557 (23.0) | 444 (23.1) | 445 (22.7) | 433 (22.6) | 437 (20.8) | 407 (24.9) |
| High school | 848 (35.0) | 511 (26.6) | 655 (33.4) | 548 (28.7) | 843 (40.2) | 398 (24.4) |
| ≥College | 449 (18.5) | 183 (9.5) | 359 (18.3) | 218 (11.4) | 418 (19.9) | 149 (9.1) |
| Smoking (packs/year) | 10.0 ± 15.6 | 9.0 ± 16.0 | 12.4 ± 16.6 | 7.2 ± 19.5 | 6.4 ± 13.5 | 11.8 ± 17.1 |
| Alcohol intake (g/day) | 11.7 ± 23.7 | 7.5 ± 20.1 | 13.0 ± 24.6 | 7.2 ± 19.5 | 8.4 ± 21.1 | 10.3 ± 21.9 |
| Hypertension status, n (%) | ||||||
| Hypertensive | 693 (28.6) | 654 (34.0) | 556 (28.3) | 671 (35.1) | 586 (27.9) | 553 (33.9) |
| Normotensive | 1732 (71.4) | 1268 (66.0) | 1407 (71.7) | 1242 (64.9) | 1513 (72.1) | 1080 (66.1) |
| Family history of CVD, n (%) | ||||||
| Yes | 379 (15.6) | 272 (14.2) | 317 (16.2) | 272 (14.2) | 343 (16.3) | 223 (13.7) |
| No | 2046 (84.4) | 1650 (85.9) | 1646 (83.9) | 1641 (85.8) | 1756 (83.7) | 1410 (86.3) |
| Body mass index, kg/m2 | 24.4 ± 3.1 | 24.9 ± 3.2 | 24.4 ± 3.1 | 24.9 ± 3.2 | 24.8 ± 3.1 | 24.4 ± 3.2 |
| Physical activity, METs/day | 22.8 ± 14.1 | 26.0 ± 15.1 | 23.0 ± 14.3 | 24.6 ± 14.7 | 20.6 ± 12.1 | 28.1 ± 16.1 |
| Total energy intake, kcal/day | 1959.2 ± 519.0 | 1879.8 ± 468.9 | 1817.6 ± 518.8 | 2009.8 ± 471.8 | 1807.4 ± 482.4 | 2006.4 ± 527.4 |
| Healthy plant foods, serv/d (2) | 10.4 ± 4.9 | 14.2 ± 5.5 | 9.3 ± 4.4 | 14.7 ± 5.6 | 14.2 ± 5.0 | 9.5 ± 4.9 |
| Unhealthy plant foods, serv/d (3) | 7.2 ± 3.2 | 9.2 ± 3.6 | 9.5 ± 3.4 | 6.7 ± 3.2 | 6.4 ± 2.7 | 10.1 ± 3.7 |
| Animal foods, serv/d (4) | 4.4 ± 2.4 | 3.1 ± 2.0 | 4.4 ± 2.3 | 3.1 ± 2.0 | 4.4 ± 2.2 | 2.9 ± 2.0 |
| PDI | hPDI | uPDI | ||||
|---|---|---|---|---|---|---|
| Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | Quartile 1 | Quartile 4 | |
| (n = 2425) | (n = 1922) | (n = 1963) | (n = 1913) | (n = 2099) | (n = 1633) | |
| Total energy intake, kcal/day | 1959.2 ± 519.0 | 1886.9 ± 474.3 | 1817.6 ± 518.8 | 2009.8 ± 471.8 | 1807.4 ± 482.4 | 2006.4 ± 527.4 |
| Carbohydrate, %E | 68.8 ± 6.1 | 74.0 ± 5.0 | 69.5 ± 6.1 | 73.5 ± 5.4 | 68.8 ± 5.2 | 74.4 ± 5.7 |
| Protein, %E | 13.8 ± 2.1 | 12.9 ± 1.8 | 13.6 ± 2.1 | 13.0 ± 1.9 | 14.5 ± 1.8 | 12.0 ± 1.7 |
| Fat, %E | 16.1 ± 4.8 | 12.3 ± 4.0 | 15.7 ± 4.8 | 12.4 ± 4.2 | 16.0 ± 4.1 | 12.2 ± 4.7 |
| Vitamin A, μg RE | 241.7 ± 113.1 | 296.8 ± 138.1 | 270.2 ± 123.9 | 261.6 ± 138.2 | 295.5 ± 125.3 | 239.9 ± 122.0 |
| Vitamin E, mg | 4.4 ± 1.2 | 4.9 ± 1.3 | 4.61 ± 1.21 | 4.63 ± 1.35 | 5.2 ± 1.2 | 4.1 ± 1.2 |
| Vitamin B1, mg | 0.61 ± 0.12 | 0.61 ± 0.10 | 0.61 ± 0.11 | 0.61 ± 0.11 | 0.64 ± 0.10 | 0.57 ± 0.11 |
| Vitamin B2, mg | 0.52 ± 0.12 | 0.49 ± 0.12 | 0.52 ± 0.12 | 0.48 ± 0.13 | 0.58 ± 0.12 | 0.43 ± 0.10 |
| Niacin, mg | 7.9 ± 1.5 | 8.0 ± 1.3 | 8.1 ± 1.4 | 7.7 ± 1.3 | 8.6 ± 1.3 | 7.1 ± 1.2 |
| Vitamin B6, mg | 0.87 ± 0.15 | 0.95 ± 0.16 | 0.90 ± 0.15 | 0.90 ± 0.17 | 1.0 ± 0.1 | 0.8 ± 0.2 |
| Folate, μg | 110.0 ± 33.0 | 141.6 ± 39.7 | 119.2 ± 37.1 | 130.0 ± 41.0 | 135.9 ± 36.2 | 112.3 ± 37.5 |
| Vitamin C, mg | 52.8 ± 27.7 | 73.6 ± 29.4 | 56.4 ± 23.1 | 67.5 ± 34.1 | 70.1 ± 28.6 | 54.4 ± 27.1 |
| Calcium, mg | 239.9 ± 83.8 | 247.4 ± 79.9 | 245.8 ± 81.8 | 235.5 ± 84.6 | 284.0 ± 85.3 | 197.6 ± 68.7 |
| Phosphorus, mg | 515.9 ± 75.4 | 517.0 ± 72.4 | 511.8 ± 73.8 | 518.0 ± 75.7 | 566.5 ± 71.4 | 457.3 ± 59.0 |
| Sodium, mg | 1421.5 ± 515.8 | 1829.8 ± 633.9 | 1758.1 ± 632.7 | 1479.2 ± 581.9 | 1567.9 ± 559.2 | 1662.3 ± 632.3 |
| Potassium, mg | 1189.7 ± 289.8 | 1418.5 ± 310.6 | 1257.1 ± 293.3 | 1316.3 ± 339.7 | 1459.6 ± 303.3 | 1115.1 ± 272.0 |
| Iron, mg | 5.2 ± 1.1 | 5.9 ± 1.2 | 5.2 ± 1.2 | 5.8 ± 1.2 | 6.2 ± 1.1 | 4.7 ± 1.0 |
| Zinc, μg | 4.6 ± 1.0 | 4.3 ± 0.7 | 4.43 ± 0.94 | 4.37 ± 0.78 | 4.8 ± 1.1 | 4.0 ± 0.8 |
| Fiber, g | 3.0 ± 0.8 | 4.1 ± 1.0 | 3.2 ± 0.9 | 3.8 ± 1.1 | 3.7 ± 1.0 | 3.3 ± 1.0 |
| Cholesterol, mg | 102.6 ± 44.8 | 66.0 ± 37.2 | 100.1 ± 45.1 | 67.8 ± 39.3 | 107.4 ± 41.7 | 60.1 ± 37.2 |
| Quartiles of Plant-Based Diet Index Scores | p-Trend (1) | ||||
|---|---|---|---|---|---|
| Quartile 1 | Quartile 2 | Quartile 3 | Quartile 4 | ||
| Cardiovascular disease (n = 597) | |||||
| Overall plant-based diet index | |||||
| Median score (range) | 46 (31–48) | 50 (49–51) | 53 (52–54) | 57 (55–70) | |
| Cases/total | 174/2425 | 139/1826 | 119/1647 | 165/1922 | |
| Person-years | 30,521 | 23,188 | 21,432 | 24,608 | |
| Age, sex adjusted | Reference | 0.98 (0.79–1.23) | 0.87 (0.69–1.10) | 1.01 (0.81–1.25) | 0.846 |
| Multivariable adjusted * | Reference | 0.98 (0.78–1.22) | 0.86 (0.68–1.09) | 0.99 (0.80–1.24) | 0.779 |
| Healthful plant-based diet index | |||||
| Median score | 44 (29–46) | 49 (47–51) | 53 (52–55) | 59 (56–74) | |
| Cases/total | 135/1963 | 179/2258 | 129/1686 | 154/1913 | |
| Person-years | 23,991 | 29,071 | 21,948 | 24,741 | |
| Age, sex adjusted | Reference | 1.05 (0.84–1.31) | 0.98 (0.76–1.24) | 1.02 (0.81–1.29) | 0.986 |
| Multivariable adjusted * | Reference | 1.07 (0.86–1.35) | 1.00 (0.78–1.28) | 1.06 (0.83–1.35) | 0.796 |
| Unhealthful plant-based diet index | |||||
| Median score | 43 (30–46) | 49 (47–51) | 54 (52–56) | 60 (57–75) | |
| Cases/total | 135/2099 | 150/2069 | 163/2019 | 149/1633 | |
| Person-years | 27,579 | 26,709 | 25,350 | 20,113 | |
| Age, sex adjusted | Reference | 0.99 (0.78–1.25) | 1.04 (0.82–1.31) | 1.18 (0.93–1.50) | 0.151 |
| Multivariable adjusted * | Reference | 0.99 (0.78–1.25) | 1.07 (0.84–1.36) | 1.25 (0.97–1.62) | 0.07 |
| Coronary heart disease (n = 314) | |||||
| Overall plant-based diet index | |||||
| Median score (range) | 46 (31–48) | 50 (49–51) | 53 (52–54) | 57 (55–70) | |
| Cases/total | 94/2425 | 66/1834 | 66/1636 | 88/1925 | |
| Person-years | 30,901 | 23,738 | 21,433 | 25,036 | |
| Age, sex adjusted | Reference | 0.86 (0.62–1.17) | 0.91 (0.66–1.25) | 1.00 (0.74–1.34) | 0.962 |
| Multivariable adjusted * | Reference | 0.85 (0.62–1.17) | 0.90 (0.66–1.24) | 0.97 (0.72–1.30) | 0.88 |
| Healthful plant-based diet index | |||||
| Median score | 44 (29–46) | 49 (47–51) | 53 (52–55) | 59 (56–74) | |
| Cases/total | 76/1962 | 88/2257 | 66/1683 | 84/1918 | |
| Person-years | 24,264 | 29,489 | 22,207 | 25,147 | |
| Age, sex adjusted | Reference | 0.92 (0.68–1.26) | 0.90 (0.65–1.26) | 1.00 (0.73–1.37) | 0.963 |
| Multivariable adjusted * | Reference | 0.92 (0.67–1.25) | 0.90 (0.65–1.26) | 0.99 (0.72–1.37) | 0.997 |
| Unhealthful plant-based diet index | |||||
| Median score | 43 (30–46) | 49 (47–51) | 54 (52–56) | 60 (57–75) | |
| Cases/total | 60/2099 | 79/2074 | 88/2011 | 87/1636 | |
| Person-years | 27,904 | 27,156 | 25,611 | 20,436 | |
| Age, sex adjusted | Reference | 1.18 (0.84–1.65) | 1.28 (0.92–1.79) | 1.56 (1.12–2.19) | 0.008 |
| Multivariable adjusted * | Reference | 1.19 (0.84–1.67) | 1.31 (0.93–1.85) | 1.62 (1.12–2.33) | 0.008 |
| Stroke (n = 287) | |||||
| Overall plant-based diet index | |||||
| Median score (range) | 46 (32–48) | 50 (49–51) | 53 (52–54) | 57 (55–70) | |
| Cases/total | 85/2426 | 69/1836 | 57/1637 | 76/1921 | |
| Person-years | 31,034 | 23,812 | 21,689 | 25,163 | |
| Age, sex adjusted | Reference | 0.99 (0.72–1.36) | 0.86 (0.61–1.20) | 0.95 (0.69–1.30) | 0.611 |
| Multivariable adjusted * | Reference | 0.98 (0.71–1.36) | 0.85 (0.61–1.20) | 0.97 (0.71–1.33) | 0.705 |
| Healthful plant-based diet index | |||||
| Median score | 44 (29–46) | 49 (47–51) | 53 (52–55) | 59 (56–74) | |
| Cases/total | 65/1971 | 85/2251 | 64/1684 | 73/1914 | |
| Person-years | 24,531 | 29,583 | 22,352 | 25,232 | |
| Age, sex adjusted | Reference | 1.05 (0.76–1.46) | 1.03 (0.73–1.45) | 1.03 (0.73–1.45) | 0.922 |
| Multivariable adjusted * | Reference | 1.11 (0.80–1.53) | 1.09 (0.77–1.55) | 1.13 (0.79–1.60) | 0.511 |
| Unhealthful plant-based diet index | |||||
| Median score | 43 (30–46) | 49 (47–51) | 54 (52–56) | 60 (57–75) | |
| Cases/total | 71/2094 | 75/2077 | 82/2022 | 59/1627 | |
| Person-years | 27,881 | 27,325 | 25,837 | 20,654 | |
| Age, sex adjusted | Reference | 1.05 (0.76–1.46) | 1.03 (0.73–1.45) | 1.03 (0.73–1.45) | 0.427 |
| Multivariable adjusted * | Reference | 0.93 (0.66–1.29) | 1.03 (0.74–1.45) | 0.97 (0.66–1.42) | 0.964 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, C.; Han, B.; Lee, Y. Plant-Based Dietary Patterns and the Risk of Cardiovascular Disease in Middle-Aged Korean Adults: A Community-Based Prospective Cohort Study. Nutrients 2025, 17, 2805. https://doi.org/10.3390/nu17172805
Park C, Han B, Lee Y. Plant-Based Dietary Patterns and the Risk of Cardiovascular Disease in Middle-Aged Korean Adults: A Community-Based Prospective Cohort Study. Nutrients. 2025; 17(17):2805. https://doi.org/10.3390/nu17172805
Chicago/Turabian StylePark, Chaeyoung, Boeun Han, and Yujin Lee. 2025. "Plant-Based Dietary Patterns and the Risk of Cardiovascular Disease in Middle-Aged Korean Adults: A Community-Based Prospective Cohort Study" Nutrients 17, no. 17: 2805. https://doi.org/10.3390/nu17172805
APA StylePark, C., Han, B., & Lee, Y. (2025). Plant-Based Dietary Patterns and the Risk of Cardiovascular Disease in Middle-Aged Korean Adults: A Community-Based Prospective Cohort Study. Nutrients, 17(17), 2805. https://doi.org/10.3390/nu17172805






