Prematurity and Low Birth Weight Among Food-Secure and Food-Insecure Households: A Comparative Study in Surabaya, Indonesia
Highlights
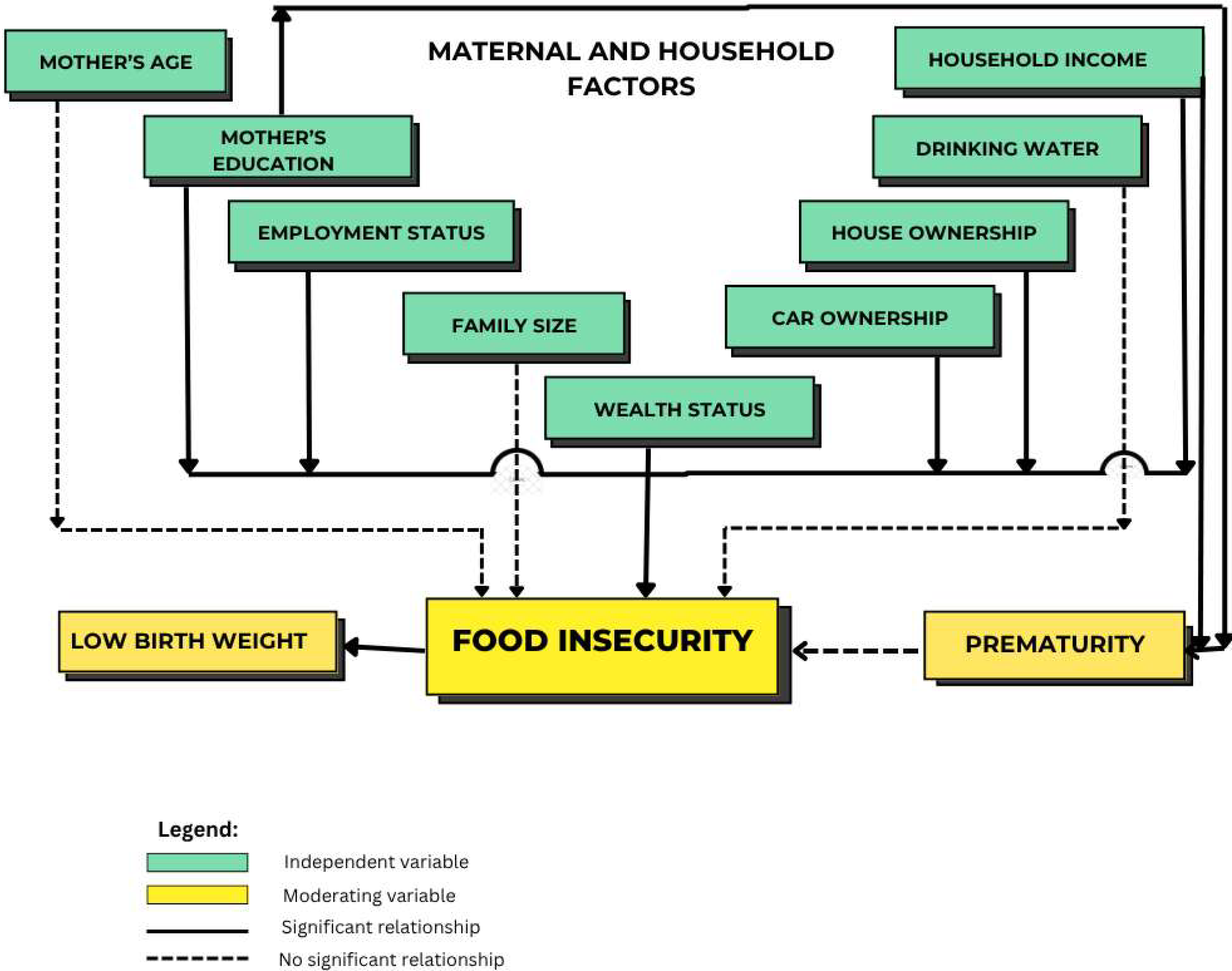
- Prematurity was not associated with household food insecurity. Nevertheless, maternal education, employment status, and household income were associated with household food insecurity.
- Children from food-insecure households had a lower risk of low birth weight than those from food-secure households. This unusual finding warrants additional examination of the context-specific protective factors or interventions that might impact birth outcomes.
- Low birth weight outcomes may potentially be attributed to maternal health interventions (i.e., nutrition education, food aids, cash transfer) that aim to lessen the impact of food insecurity during pregnancy.
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Design
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Study Population
3.2. Factors Associated with Prematurity, Low Birth Weight, and Household Food Insecurity
4. Discussion
4.1. Low Birth Weight in Food-Secure and Food-Insecure Households
4.2. Prematurity in Food-Secure and Food-Insecure Households
4.3. Comparison of Findings in Food-Secure and Food-Insecure Households
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LBW | Low birth weight |
| CI | Confidence interval |
| AOR | Adjusted odds ratio |
| SDG | Sustainable development goal |
| FAO | Food and Agriculture Organization |
| WHO | World Health Organization |
| FIES-SM | Food insecurity experience scale survey module |
| IUGR | Intra-uterine growth restriction |
| IYCF | Infant and young child feeding |
| SD | Standard deviation |
| PET | Polyethylene terephthalate |
References
- World Health Organization. Preterm Birth. Available online: https://www.who.int/news-room/fact-sheets/detail/preterm-birth (accessed on 11 February 2025).
- Born Too Soon: Decade of Action on Preterm Birth. Available online: https://www.who.int/publications/i/item/9789240073890 (accessed on 15 February 2025).
- SKI 2023 Dalam Angka-Badan Kebijakan Pembangunan Kesehatan|BKPK Kemenkes. Available online: https://www.badankebijakan.kemkes.go.id/ski-2023-dalam-angka/ (accessed on 7 January 2025).
- Data Warehouse-UNICEF DATA. Available online: https://data.unicef.org/resources/data_explorer/unicef_f/?ag=UNICEF&df=GLOBAL_DATAFLOW&ver=1.0&dq=IDN.CME_MRM0.&startPeriod=1970&endPeriod=2024 (accessed on 7 January 2025).
- Sampurna, M.T.A.; Handayani, K.D.; Utomo, M.T.; Angelika, D.; Etika, R.; Harianto, A.; Mapindra, M.P.; Mahindra, M.P.; Efendi, F.; Kaban, R.K.; et al. Determinants of Neonatal Deaths in Indonesia: A National Survey Data Analysis of 10,838 Newborns. Heliyon 2023, 9, e12980. [Google Scholar] [CrossRef] [PubMed]
- Dinas Kesehatan Provinsi Jawa Timur. Profil Kesehatan Provinsi Jawa Timur Tahun 2023; Dinas Kesehatan Provinsi Jawa Timur: Surabaya, Indonesia, 2023. [Google Scholar]
- Asma, K.M.; Misu, F.; Islam, M.A. The Impact of Social Safety Net Programs on Poverty, Food Security and Standard of Living in Bangladesh. Int. J. Community Soc. Dev. 2022, 5, 71–96. [Google Scholar] [CrossRef]
- UNICEF-WHO. Low Birthweight Estimates: Levels and Trends 2000–2015|UNICEF. Available online: https://www.unicef.org/reports/UNICEF-WHO-low-birthweight-estimates-2019 (accessed on 11 February 2025).
- Pusdekar, Y.V.; Patel, A.B.; Kurhe, K.G.; Bhargav, S.R.; Thorsten, V.; Garces, A.; Goldenberg, R.L.; Goudar, S.S.; Saleem, S.; Esamai, F.; et al. Rates and Risk Factors for Preterm Birth and Low Birthweight in the Global Network Sites in Six Low- and Low Middle-Income Countries. Reprod. Health 2020, 17, 187. [Google Scholar] [CrossRef] [PubMed]
- Wulandari, R.D.; Laksono, A.D.; Matahari, R. Policy to Decrease Low Birth Weight in Indonesia: Who Should Be the Target? Nutrients 2023, 15, 465. [Google Scholar] [CrossRef]
- Martinson, M.L.; Choi, K.H. Low Birth Weight and Childhood Health: The Role of Maternal Education. Ann. Epidemiol. 2019, 39, 39–45.e2. [Google Scholar] [CrossRef]
- Alam, M.J.; Islam, M.M.; Maniruzzaman, M.; Ahmed, N.A.M.F.; Tawabunnahar, M.; Rahman, M.J.; Roy, D.C.; Mydam, J. Socioeconomic Inequality in the Prevalence of Low Birth Weight and Its Associated Determinants in Bangladesh. PLoS ONE 2022, 17, e0276718. [Google Scholar] [CrossRef]
- Singh, D.; Manna, S.; Barik, M.; Rehman, T.; Kanungo, S.; Pati, S. Prevalence and Correlates of Low Birth Weight in India: Findings from National Family Health Survey 5. BMC Pregnancy Childbirth 2023, 23, 456. [Google Scholar] [CrossRef]
- Uwimana, G.; Elhoumed, M.; Gebremedhin, M.A.; Azalati, M.M.; Nan, L.; Zeng, L. Association between Quality Antenatal Care and Low Birth Weight in Rwanda: A Cross-Sectional Study Design Using the Rwanda Demographic and Health Surveys Data. BMC Health Serv. Res. 2023, 23, 558. [Google Scholar] [CrossRef]
- Aryastami, N.K.; Shankar, A.; Kusumawardani, N.; Besral, B.; Jahari, A.B.; Achadi, E. Low Birth Weight Was the Most Dominant Predictor Associated with Stunting among Children Aged 12-23 Months in Indonesia. BMC Nutr. 2017, 3, 16. [Google Scholar] [CrossRef]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2022; WHO: Geneva, Switzerland, 2022; 209p. [Google Scholar] [CrossRef]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2023; WHO: Geneva, Switzerland, 2023; 316p. [Google Scholar] [CrossRef]
- Pangan, D.K.; Pertanian, K.; WFP. Food Security and Vulnerability Atlas of Indonesia 2015; Dewan Ketahanan Pangan, Kementerian Pertanian and World Food Programme (WFP): Rome, Italy, 2015. [Google Scholar]
- Dinagde, D.D.; Wada, H.W.; Chewaka, M.T. Household Food Insecurity and Associated Factors among Postpartum Women in Southern Ethiopia: A Community Based Cross Sectional Study. Sci. Rep. 2024, 14, 4003. [Google Scholar] [CrossRef]
- Fan, H.C.; Chang, Y.M.; Lee, J.Y.; Wang, D.S.; Chen, C.M.; Hu, S.W.; Chiang, K.L.; Kuo, F.C. The Prevalence and Risk Analysis of Cerebral Palsy and Other Neuro-Psychological Comorbidities in Children with Low Birth Weight in Taiwan: A Nationwide Population-Based Cohort Study. J. Clin. Med. 2024, 13, 3480. [Google Scholar] [CrossRef]
- Ramadhani, D.N.A.M.; Budhiastuti, U.R.; Murti, B. Meta-Analysis of the Effect of Exposure to Indoor Cigarette Smoke in Pregnant Women on the Risk of Infants Low Birth Weight. J. Epidemiol. Public Health 2023, 8, 469–477. [Google Scholar] [CrossRef]
- Lee, J.; Costello, S.; Balmes, J.R.; Holm, S.M. The Association between Ambient PM2.5 and Low Birth Weight in California. Int. J. Environ. Res. Public Health 2022, 19, 13554. [Google Scholar] [CrossRef] [PubMed]
- Gebreslasie, K.Z.; Weldemariam, S.; Gebre, G.; Zenebe, D.; Mehari, M.; Birhane, A.; Dewey, R.S. Intimate Partner Violence during Pregnancy and Risks of Low Birth Weight and Preterm Birth in Hospitals of Tigray, Northern Ethiopia. Sci. Rep. 2024, 14, 1363. [Google Scholar] [CrossRef] [PubMed]
- Bachwenkizi, J.; Liu, C.; Meng, X.; Zhang, L.; Wang, W.; van Donkelaar, A.; Martin, R.V.; Hammer, M.S.; Chen, R.; Kan, H. Maternal Exposure to Fine Particulate Matter and Preterm Birth and Low Birth Weight in Africa. Environ. Int. 2022, 160, 107053. [Google Scholar] [CrossRef]
- Kaforau, L.S.K.; Tessema, G.A.; Jancey, J.; Dhamrait, G.; Bugoro, H.; Pereira, G. Prevalence and Risk Factors of Adverse Birth Outcomes in the Pacific Island Region: A Scoping Review. Lancet Reg. Health West. Pac. 2022, 21, 100402. [Google Scholar] [CrossRef]
- Kang, H. Sample Size Determination and Power Analysis Using the G*Power Software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef]
- International Committee of Medical Journal Editors. Uniform Requirements for Manuscripts Submitted to Biomedical Journals. JAMA 1997, 277, 927–934. [Google Scholar] [CrossRef]
- Kiernan, M.; Baiocchi, M.T. Casting New Light on Statistical Power: An Illuminating Analogy and Strategies to Avoid Underpowered Trials. Am. J. Epidemiol. 2022, 191, 1500. [Google Scholar] [CrossRef]
- FAO. Analyse the Data|Voices of the Hungry|Food and Agriculture Organization of the United Nations. Available online: https://www.fao.org/in-action/voices-of-the-hungry/analyse-data/en/ (accessed on 11 June 2025).
- Bater, J.; Lauer, J.M.; Ghosh, S.; Webb, P.; Agaba, E.; Bashaasha, B.; Turyashemererwa, F.M.; Shrestha, R.; Duggan, C.P. Predictors of Low Birth Weight and Preterm Birth in Rural Uganda: Findings from a Birth Cohort Study. PLoS ONE 2020, 15, e0235626. [Google Scholar] [CrossRef]
- de Freitas Rocha, A.R.; de Souza de Morais, N.; Azevedo, F.M.; de Castro Morais, D.; Priore, S.E. Maternal Food Insecurity Increases the Risk of Low Birth Weight Babies: Systematic Review and Meta-Analysis. Acta Paediatr. 2024, 113, 2180–2188. [Google Scholar] [CrossRef] [PubMed]
- Terfa, Z.G.; Nantanda, R.; Lesosky, M.; Devereux, G.; Obasi, A.; Mortimer, K.; Khan, J.A.M.; Rylance, J.; Niessen, L. Household Food Insecurity, Maternal Nutrition, Environmental Risks and Infants’ Health Outcomes: Protocol of the IMPALA Birth Cohort Study in Uganda. BMJ Open 2022, 12, e050729. [Google Scholar] [CrossRef] [PubMed]
- Masitoh, S.; Wurisastuti, T.; Riyadina, W.; Ronoatmodjo, S. The Level of Household Food Insecurity Is Associated with the Risk of Infectious Diseases among Toddlers in Indonesia: A Cross-Sectional Study. Osong Public Health Res. Perspect. 2025, 16, 261. [Google Scholar] [CrossRef] [PubMed]
- Borji, M.; Moradi, M.; Otaghi, M.; Tartjoman, A. Tartjoman Relationship between Nutritional Status, Food Insecurity, and Causes of Hospitalization of Children with Infectious Diseases. J. Compr. Ped 2018, 9, e63870. [Google Scholar] [CrossRef]
- Chakraborty, R.; Armijos, R.X.; Beidelman, E.T.; Rosenberg, M.; Margaret Weigel, M. Household Food and Water Insecurity and Its Association with Diarrhoea, Respiratory Illness, and Stunting in Ecuadorian Children under 5 Years. Matern. Child. Nutr. 2024, 20, e13683. [Google Scholar] [CrossRef]
- Guruge, G.N.D.; Young, S.M.; Perera, K.M.N.; Dharmaratne, S.D.; Gunathunga, M.W. Evaluating the Effectiveness of a Community-Based Health Promotion Intervention on Knowledge Improvement Regarding Low Birth Weight and Its Determinants among Antenatal Couples in Sri Lanka. Discov. Public Health 2024, 21, 1–15. [Google Scholar] [CrossRef]
- Leroy, J.L.; Koch, B.; Roy, S.; Gilligan, D.; Ruel, M. Social Assistance Programs and Birth Outcomes: A Systematic Review and Assessment of Nutrition and Health Pathways. J. Nutr. 2021, 151, 3841–3855. [Google Scholar] [CrossRef]
- Dolati, S.; Barzegar, A.; Mohammadi-Nasrabadi, F.; Abdollahi, M.; Khodayari-Zarnaq, R. Cash Transfer Program on Pregnancy Outcomes and Infant Growth in Deprived Pregnant and Lactating Mothers in Iran: A Field Trial. BMC Public Health 2025, 25, 2219. [Google Scholar] [CrossRef]
- Garrity, K.; Krzyzanowski Guerra, K.; Hart, H.; Al-Muhanna, K.; Kunkler, E.C.; Braun, A.; Poppe, K.I.; Johnson, K.; Lazor, E.; Liu, Y.; et al. Local Food System Approaches to Address Food and Nutrition Security among Low-Income Populations: A Systematic Review. Adv. Nutr. 2024, 15, 100156. [Google Scholar] [CrossRef]
- Falcão, I.R.; Ribeiro-Silva, R.d.C.; Fiaccone, R.L.; Alves, F.J.O.; Rocha, A.d.S.; Ortelan, N.; Silva, N.J.; Rebouças, P.; Pinto Júnior, E.P.; De Almeida, M.F.; et al. Participation in Conditional Cash Transfer Program During Pregnancy and Birth Weight–Related Outcomes. JAMA Netw. Open 2023, 6, e2344691. [Google Scholar] [CrossRef]
- Kheirouri, S.; Alizadeh, M. Maternal Dietary Diversity during Pregnancy and Risk of Low Birth Weight in Newborns: A Systematic Review. Public Health Nutr. 2021, 24, 4671. [Google Scholar] [CrossRef]
- Ruan, X.; Chen, K.; Li, Z.; Wei, J.; Chen, Y.; Zou, Q.; Peng, Y.; Luo, M.; Sun, M.; Wang, T.; et al. The Impact of Maternal Health and Lifestyle on Low Birth Weight: A Prospective Cohort Study. Ital. J. Pediatr. 2025, 51, 217. [Google Scholar] [CrossRef]
- Richterman, A.; Raymonville, M.; Hossain, A.; Millien, C.; Joseph, J.P.; Jerome, G.; Franke, M.F.; Ivers, L.C. Food Insecurity as a Risk Factor for Preterm Birth: A Prospective Facility-Based Cohort Study in Rural Haiti. BMJ Glob. Health 2020, 5, e002341. [Google Scholar] [CrossRef]
- Montemor, M.S.; Demarque, G.F.; Rodrigues, A.S.; Francisco, R.P.V.; de Carvalho, M.H.B. Association between Preterm Births and Socioeconomic Development: Analysis of National Data. BMC Public Health 2022, 22, 2014. [Google Scholar] [CrossRef]
- Ahmed, A.M.; Pullenayegum, E.; McDonald, S.D.; Beltempo, M.; Premji, S.S.; Pole, J.D.; Bacchini, F.; Shah, P.S.; Pechlivanoglou, P. Association between Preterm Birth and Economic and Educational Outcomes in Adulthood: A Population-Based Matched Cohort Study. PLoS ONE 2024, 19, e0311895. [Google Scholar] [CrossRef] [PubMed]
- Granés, L.; Torà-Rocamora, I.; Palacio, M.; De La Torre, L.; Llupià, A. Maternal Educational Level and Preterm Birth: Exploring Inequalities in a Hospital-Based Cohort Study. PLoS ONE 2023, 18, e0283901. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Jia, C.; Luo, X.; Sun, Y.; Zuo, W.; Wu, Y.; Wu, Y.; Kaierdebieke, A.; Lin, Z. The Impact of Higher Education on Health Literacy: A Comparative Study between Urban and Rural China. Sustainability 2022, 14, 12142. [Google Scholar] [CrossRef]
- Prasetyo, Y.B.; Permatasari, P.; Susanti, H.D. The Effect of Mothers’ Nutritional Education and Knowledge on Children’s Nutritional Status: A Systematic Review. Int. J. Child Care Educ. Policy 2023, 17, 11. [Google Scholar] [CrossRef]
- Adhikari, T.; Sahu, D.; Nair, S.; Saha, K.B.; Sharma, R.K.; Pandey, A. Factors Associated with Utilization of Antenatal Care Services among Tribal Women: A Study of Selected States. Indian J. Med. Res. 2016, 144, 58–66. [Google Scholar] [CrossRef]
- Ade, A.D.; Guthi, V.R.; Kondagunta, N.; Kumar, D.S.S.; Deekala, R.; Vallepalli, C.; Prathyusha, T.V.D. Improving Access to Utilize the Healthcare Services Facilitated by ASHAs, ANMs and Medical Officers of PHC among Scheduled Tribe Pregnant Women: An Interventional Study. J. Fam. Med. Prim. Care 2024, 13, 3856–3863. [Google Scholar] [CrossRef]
- Areba, A.S.; Akiso, D.E.; Haile, A.; Abire, B.G.; Kanno, G.G.; Tirore, L.L.; Abame, D.E. Factors Associated with Food Insecurity among Pregnant Women in Gedeo Zone Public Hospitals, Southern Ethiopia. Front. Public Health 2024, 12, 1399185. [Google Scholar] [CrossRef] [PubMed]
- Lemi, T.B.; Ababor, G.N.; Abdulahi, M. Relationship between Household Food Insecurity and Minimum Dietary Diversity among Pregnant Women Attending Antenatal Care at Public Health Facilities in Fiche Town, Oromia Region, Central Ethiopia: A Facility-Based Cross-Sectional Study. BMJ Open 2025, 15, e088621. [Google Scholar] [CrossRef] [PubMed]
- Zinga, J.; McKay, F.H.; Lindberg, R.; van der Pligt, P. Experiences of Food-Insecure Pregnant Women and Factors Influencing Their Food Choices. Matern. Child Health J. 2022, 26, 1434–1441. [Google Scholar] [CrossRef] [PubMed]
- Cheah Whye Lian, P.; Beng Chin, T.; Whye Lian, C.; Leh Shii, L. Demographic Characteristics Are Associated with Children’s Nutritional Status: Findings from a Pilot Study on Food Insecure Households in Simunjan District, Sarawak. Malays. J. Nutr. 2023, 29, 467–480. [Google Scholar] [CrossRef]
- Abdullah, N.A.; Nasution, Z.; Bariah, S.; Hamid, A. Impact of Pandemic COVID-19 towards Food Insecurity and Dietary Diversity Among B40 Mothers Living in Urban Areas in Selangor. Malays. J. Med. Health Sci. 2024, 20, 3–11. [Google Scholar] [CrossRef]
- Das Shuvo, S.; Hossain, M.S.; Riazuddin, M.; Mazumdar, S.; Roy, D. Factors Influencing Low-Income Households’ Food Insecurity in Bangladesh during the COVID-19 Lockdown. PLoS ONE 2022, 17, e0267488. [Google Scholar] [CrossRef]
- UNICEF. Child Food Poverty: Nutrition Deprivation in Early Childhood-UNICEF DATA. Available online: https://data.unicef.org/resources/child-food-poverty-report-2024/ (accessed on 7 April 2025).
- Shahzad, M.A.; Qing, P.; Rizwan, M.; Razzaq, A.; Faisal, M. COVID-19 Pandemic, Determinants of Food Insecurity, and Household Mitigation Measures: A Case Study of Punjab, Pakistan. Healthcare 2021, 9, 621. [Google Scholar] [CrossRef]
- Lukwa, A.T.; Siya, A.; Zablon, K.N.; Azam, J.M.; Alaba, O.A. Socioeconomic Inequalities in Food Insecurity and Malnutrition among Under-Five Children: Within and between-Group Inequalities in Zimbabwe. BMC Public Health 2020, 20, 1199. [Google Scholar] [CrossRef]
- Ali, D.; Saha, K.K.; Nguyen, P.H.; Diressie, M.T.; Ruel, M.T.; Menon, P.; Rawat, R. Household Food Insecurity Is Associated with Higher Child Undernutrition in Bangladesh, Ethiopia, and Vietnam, but the Effect Is Not Mediated by Child Dietary Diversity. J. Nutr. 2013, 143, 2015–2021. [Google Scholar] [CrossRef]
- Leonard, K.; Dela Luna, G.; Theresa, M.; Talavera, M. Influences of Wealth Index, Family Size, Food Security, and Diet Diversity Status in the Growth of Filipino School-Age Children in Farming Households. J. Hum. Ecol. Sustain. 2022, 1. [Google Scholar] [CrossRef]
- Aghamohammadi, V.; Nasiri, K.; Bazyar, H.; Mohammadi, E.; Moghaddam, H.R.; Masoudi, M.R.; Ivanbagha, R.; Behzad, A.; Ezzati, M. Association of Household Food Insecurity with Stunting and Underweight Among Iranian Children Aged 2–5 Years Old. Iran. J. Pediatr. 2024, 34, e145493. [Google Scholar] [CrossRef]
- Aden, E.H.; Mohammed, S.A. Household Food Insecurity and Its Association with Nutritional Status of Children 6–59 Months of Age in Kebridehar City|Aden|Indonesian Food and Nutrition Progress. Available online: https://jurnal.ugm.ac.id/ifnp/article/view/90356/40460 (accessed on 7 April 2025).
| Characteristics | Mean (±SD) | Food Insecure | Food Secure | Total | Chi-Square (p-Value) |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Maternal and household factors | |||||
| Mother’s age: | 32.79 (±6.21) | 0.51 | |||
| Teen Mothers | 0 (0.00) | 1 (0.15) | 1 (0.15) | ||
| Young Adult Mothers | 87 (13.24) | 133 (20.24) | 220 (33.49) | ||
| Mature Adult Mothers | 123 (18.72) | 213 (32.42) | 336 (51.14) | ||
| Advanced Age Mothers | 43 (6.54) | 57 (8.68) | 100 (15.22) | ||
| Maternal education: | <0.001 * | ||||
| Low Education | 93 (14.16) | 90 (13.70) | 183 (27.85) | ||
| Medium Education | 141 (21.46) | 235 (35.77) | 376 (57.23) | ||
| High Education | 19 (2.89) | 79 (12.02) | 98 (14.92) | ||
| Mother’s employment status: | <0.001 * | ||||
| Not employed | 166 (25.27) | 213 (32.42) | 379 (57.69) | ||
| Employed | 87 (13.24) | 191 (29.07) | 278 (42.31) | ||
| Family size: | 0.25 | ||||
| Small Family | 51 (7.76) | 63 (9.59) | 114 (17.35) | ||
| Medium Family | 170 (25.88) | 279 (42.47) | 449 (68.34) | ||
| Large Family | 32 (4.87) | 62 (9.44) | 94 (14.31) | ||
| Monthly household income: | <0.001 * | ||||
| Low income | 231 (35.16) | 319 (48.55) | 550 (83.71) | ||
| Medium income | 20 (3.04) | 67 (10.20) | 87 (13.24) | ||
| High income | 2 (0.30) | 18 (2.74) | 20 (3.04) | ||
| Drinking water: | 0.52 | ||||
| Tap water | 54 (8.22) | 69 (10.50) | 123 (18.72) | ||
| Mineral water (in glass/PET bottle) | 185 (28.16) | 316 (48.10) | 501 (76.26) | ||
| Borehole | 11 (1.67) | 15 (2.28) | 26 (3.95) | ||
| Springwater | 3 (0.46) | 4 (0.61) | 7 (1.07) | ||
| House ownership: | 0.01 ** | ||||
| Yes | 67 (10.20) | 146 (22.22) | 213 (32.42) | ||
| No | 186 (28.31) | 258 (39.27) | 444 (67.58) | ||
| Car ownership: | <0.001 * | ||||
| Yes | 10 (1.52) | 73 (11.11) | 83 (12.63) | ||
| No | 243 (36.99) | 331 (50.38) | 574 (87.37) | ||
| Wealth status (self-assessment): | <0.001 * | ||||
| Rather better off | 74 (11.26) | 128 (19.48) | 202 (30.75) | ||
| Average | 164 (24.96) | 272 (41.40) | 436 (66.36) | ||
| Rather worse off | 15 (2.28) | 4 (0.61) | 19 (2.89) | ||
| Prematurity: | 37.33 (±2.40) | 0.51 | |||
| Preterm birth | 108 (16.44) | 183 (27.85) | 291 (44.29) | ||
| Normal birth | 145 (22.07) | 221 (33.64) | 366 (55.71) | ||
| Birth weight: | 3.05 (±0.48) | 0.07 | |||
| Low birth weight | 17 (2.59) | 44 (6.70) | 61 (9.28) | ||
| Normal birth weight | 236 (35.92) | 360 (54.79) | 596 (90.72) | ||
| Characteristics | Prematurity | LBW | ||||
|---|---|---|---|---|---|---|
| Normaln (%) | Preterm Birthn (%) | p Value | No LBWn (%) | LBWn (%) | p Value | |
| Child gender: | 0.71 | 0.64 | ||||
| Boy | 184 (28.01) | 142 (21.61) | 294 (44.75) | 32 (4.87) | ||
| Girl | 182 (27.70) | 149 (22.68) | 302 (45.97) | 29 (4.41) | ||
| Household food insecurity: | 0.51 | 0.07 | ||||
| Food-secure | 221 (33.64) | 183 (27.85) | 360 (54.79) | 44 (6.70) | ||
| Food-insecure | 108 (22.07) | 253 (16.44) | 236 (35.92) | 17 (2.59) | ||
| Mother’s age: | 0.57 | 0.97 | ||||
| Teen Mothers | 0 (0.00) | 1 (0.20) | 1 (0.20) | 0 (0.00) | ||
| Young Adult Mothers | 127 (19.30) | 93 (14.20) | 199 (30.30) | 21 (3.20) | ||
| Mature Adult Mothers | 182 (27.70) | 154 (23.40) | 306 (46.60) | 30 (4.57) | ||
| Advanced Age Mothers | 57 (8.68) | 43 (6.50) | 90 (13.70) | 10 (1.52) | ||
| Maternal education: | 0.008 | 0.11 | ||||
| Low Education | 86 (13.09) | 97 (14.76) | 159 (24.20) | 24 (3.65) | ||
| Medium Education | 216 (32.88) | 160 (24.35) | 347 (52.82) | 29 (4.41) | ||
| High Education | 64 (9.74) | 34 (5.18) | 90 (13.70) | 8 (1.22) | ||
| Mother’s employment status: | 0.87 | 0.09 | ||||
| Not employed | 210 (31.96) | 169 (25.72) | 350 (53.27) | 29 (4.41) | ||
| Employed | 156 (23.74) | 122 (18.57) | 246 (37.44) | 32 (4.87) | ||
| Family size: | 0.76 | 0.66 | ||||
| Small Family: 3 members | 67 (10.20) | 47 (7.15) | 106 (16.13) | 8 (1.22) | ||
| Medium Family: 4–6 members | 248 (37.75) | 201 (30.59) | 405 (61.64) | 44 (6.70) | ||
| Large Family: more than 6 members | 51 (7.76) | 43 (6.54) | 85 (12.94) | 9 (1.37) | ||
| Monthly household income: | 0.09 | 0.79 | ||||
| Low income | 315 (47.95) | 235 (35.77) | 498 (75.80) | 52 (7.91) | ||
| Medium income | 39 (5.94) | 48 (7.31) | 79 (12.02) | 8 (1.22) | ||
| High income | 12 (1.83) | 8 (1.22) | 19 (2.89) | 1 (0.15) | ||
| Drinking water: | 0.12 | 0.32 | ||||
| Tap water | 63 (9.59) | 60 (9.13) | 113 (17.20) | 10 (1.52) | ||
| Mineral water (in glass/PET bottle) | 284 (43.23) | 217 (33.03) | 456 (69.41) | 45 (6.85) | ||
| Borehole | 17 (2.59) | 9 (1.37) | 21 (3.20) | 5 (0.76) | ||
| Springwater | 2 (0.30) | 5 (0.76) | 6 (0.91) | 1 (0.15) | ||
| House ownership: | 0.003 | 0.43 | ||||
| Yes | 119 (18.11) | 94 (14.31) | 196 (29.83) | 17 (2.59) | ||
| No | 247 (37.6) | 197 (29.98) | 400 (60.88) | 44 (6.7) | ||
| Car ownership: | 0.32 | 0.13 | ||||
| Yes | 42 (6.39) | 41 (6.24) | 79 (12.02) | 4 (0.61) | ||
| No | 324 (49.32) | 250 (38.05) | 517 (78.69) | 57 (8.68) | ||
| Wealth status: | 0.23 | 0.83 | ||||
| Rather better off | 115 (17.50) | 87 (13.24) | 183 (27.85) | 19 (2.89) | ||
| Average | 237 (36.07) | 199 (30.29) | 395 (60.12) | 41 (6.24) | ||
| Rather worse off | 14 (2.13) | 5 (0.76) | 18 (2.74) | 1 (0.15) | ||
| Characteristics | Prematurity | Low Birth Weight (LBW) | ||
|---|---|---|---|---|
| COR (95%CI) | AOR (95%CI) ** | COR (95%CI) | AOR (95%CI) ** | |
| Household Food Insecurity: | ||||
| Food secure | 1 | 1 | 1 | 1 |
| Food insecure | 0.90 (0.66–1.23) | 0.89 (0.63–1.25) | 0.59 (0.33–1.06) | 0.54 (0.29–0.99) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alristina, A.D.; Mahrouseh, N.; Irawan, A.S.; Laili, R.D.; Zimonyi-Bakó, A.V.; Feith, H.J. Prematurity and Low Birth Weight Among Food-Secure and Food-Insecure Households: A Comparative Study in Surabaya, Indonesia. Nutrients 2025, 17, 2479. https://doi.org/10.3390/nu17152479
Alristina AD, Mahrouseh N, Irawan AS, Laili RD, Zimonyi-Bakó AV, Feith HJ. Prematurity and Low Birth Weight Among Food-Secure and Food-Insecure Households: A Comparative Study in Surabaya, Indonesia. Nutrients. 2025; 17(15):2479. https://doi.org/10.3390/nu17152479
Chicago/Turabian StyleAlristina, Arie Dwi, Nour Mahrouseh, Anggi Septia Irawan, Rizky Dzariyani Laili, Alexandra Vivien Zimonyi-Bakó, and Helga Judit Feith. 2025. "Prematurity and Low Birth Weight Among Food-Secure and Food-Insecure Households: A Comparative Study in Surabaya, Indonesia" Nutrients 17, no. 15: 2479. https://doi.org/10.3390/nu17152479
APA StyleAlristina, A. D., Mahrouseh, N., Irawan, A. S., Laili, R. D., Zimonyi-Bakó, A. V., & Feith, H. J. (2025). Prematurity and Low Birth Weight Among Food-Secure and Food-Insecure Households: A Comparative Study in Surabaya, Indonesia. Nutrients, 17(15), 2479. https://doi.org/10.3390/nu17152479






