Associations Among Sleep Duration, Physical Activity, and Nutrient Intake in Korean Adults
Abstract
1. Introduction
2. Methods
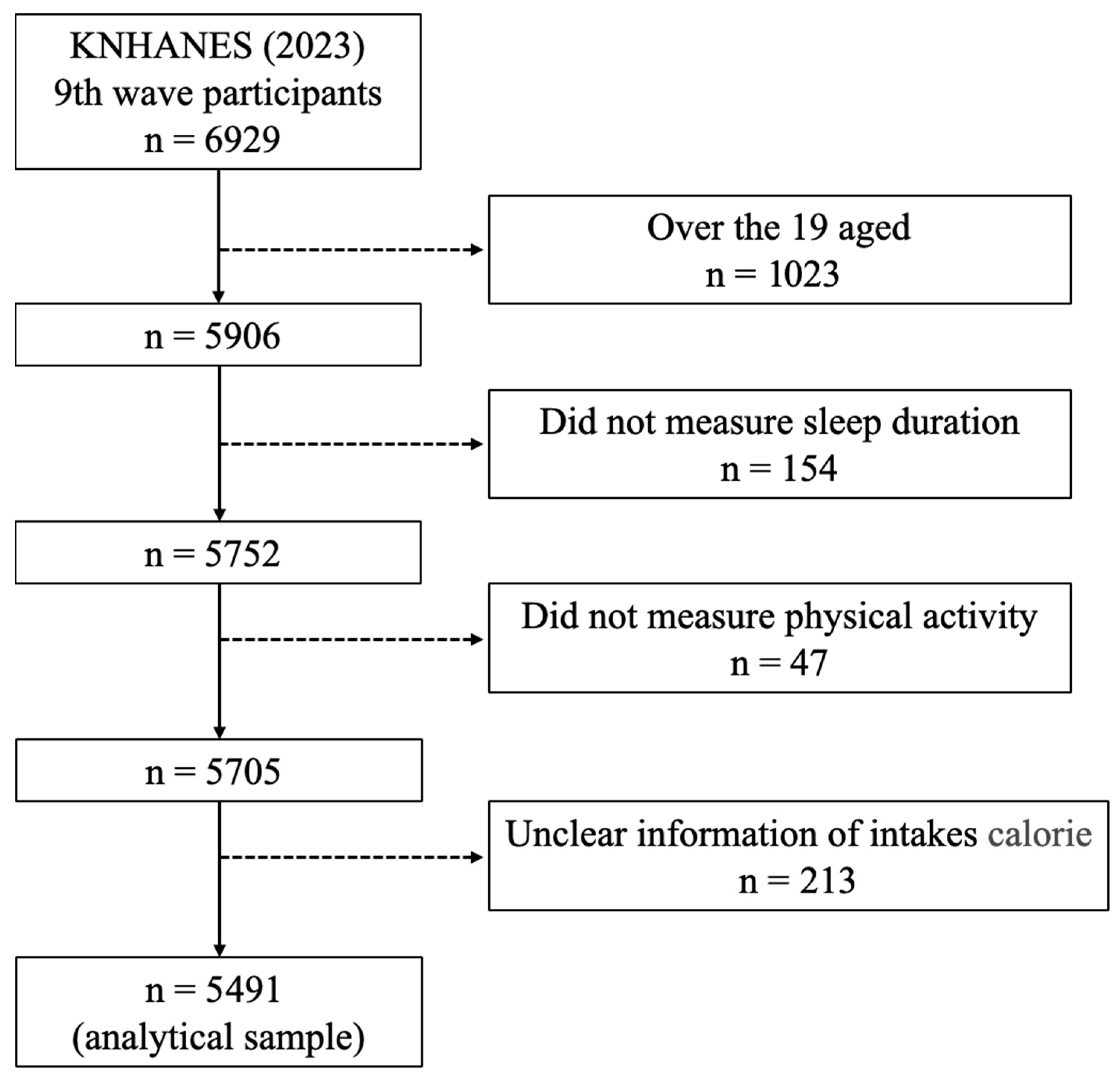
2.1. Participation
2.2. Sleep Duration
2.3. Level of Physical Activity
2.4. Assessment of Vitamin D, Carbohydrate, Protein, and Fat Intake
2.5. Statistical Analysis
3. Results
3.1. Physical Activity Levels
3.2. Vitamin D, Carbohydrate, Protein, and Fat Intake
3.3. Relationship Between Protein Intake, Physical Activity, and Sleep Duration
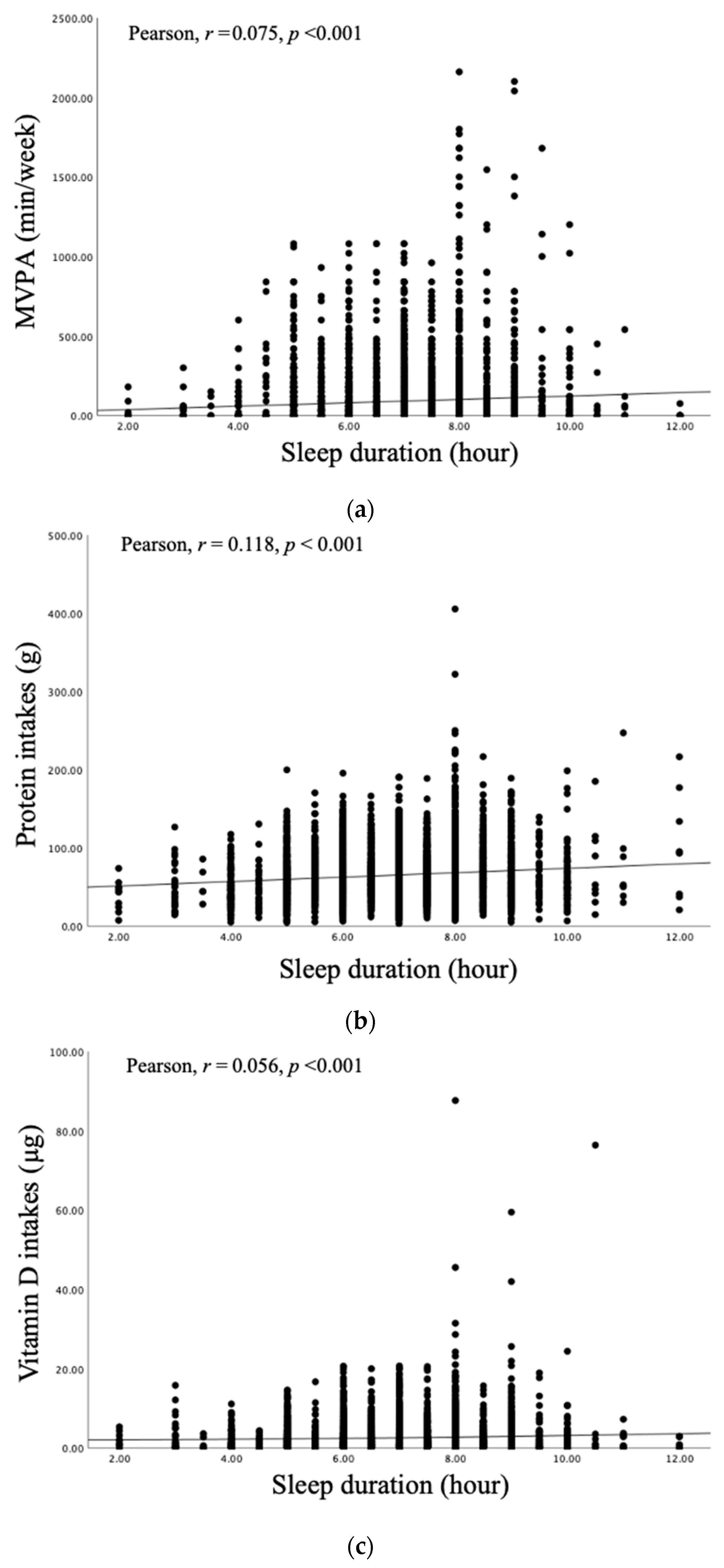
3.4. Correlation Coefficients Between Sleep Duration and Physical Activity, Protein, and Vitamin D
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vestergaard, C.L.; Skogen, J.C.; Hysing, M.; Harvey, A.G.; Vedaa, Ø.; Sivertsen, B. Sleep duration and mental health in young adults. Sleep Med. 2024, 115, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Fernandez-Mendoza, J.; Liao, D.; Bixler, E.O. Insomnia with objective short sleep duration: The most biologically severe phenotype of the disorder. Sleep Med. Rev. 2013, 17, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Nôga, D.A.; Meth, E.M.E.S.; Pacheco, A.P.; Tan, X.; Cedernaes, J.; van Egmond, L.T.; Xue, P.; Benedict, C. Habitual Short Sleep Duration, Diet, and Development of Type 2 Diabetes in Adults. JAMA Netw. Open 2024, 7, e241147. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Koemel, N.A.; Biswas, R.K.; Ahmadi, M.N.; Allman-Farinelli, M.; Trost, S.G.; Inan-Eroglu, E.; Del Pozo Cruz, B.; Bin, Y.S.; Postnova, S.; et al. Minimum and optimal combined variations in sleep, physical activity, and nutrition in relation to all-cause mortality risk. BMC Med. 2025, 23, 111. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Grosso, G.; Castellano, S.; Galvano, F.; Caraci, F.; Ferri, R. Association between diet and sleep quality: A systematic review. Sleep Med. Rev. 2021, 57, 101430. [Google Scholar] [CrossRef] [PubMed]
- Zuraikat, F.M.; Makarem, N.; Liao, M.; St-Onge, M.P.; Aggarwal, B. Measures of Poor Sleep Quality Are Associated with Higher Energy Intake and Poor Diet Quality in a Diverse Sample of Women from the Go Red for Women Strategically Focused Research Network. J. Am. Heart Assoc. 2020, 9, e014587. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.T.; Lee, E. Physical activity, body weight, and liver function as factors increasing Insomnia index among Korean adults: A cross-sectional analysis. Sleep Breath. 2024, 28, 2639–2645. [Google Scholar] [CrossRef] [PubMed]
- da Costa, B.G.G.; Chaput, J.P.; Lopes, M.V.V.; Malheiros, L.E.A.; Silva, K.S. How do adolescents with short sleep duration spend their extra waking hours? A device-based analysis of physical activity and sedentary behaviour in a Brazilian sample. Sleep Sci. 2021, 14, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, L.Z.; de Farias, J.M.; de Lima, T.R.; Schäfer, A.A.; Meller, F.O.; Silva, D.A.S. Physical Activity and Sleep in Adults and Older Adults in Southern Brazil. Int. J. Environ. Res. Public Health 2023, 20, 1461. [Google Scholar] [CrossRef] [PubMed]
- Lamon, S.; Morabito, A.; Arentson-Lantz, E.; Knowles, O.; Vincent, G.E.; Condo, D.; Alexander, S.E.; Garnham, A.; Paddon-Jones, D.; Aisbett, B. The effect of acute sleep deprivation on skeletal muscle protein synthesis and the hormonal environment. Physiol. Rep. 2021, 9, e14660. [Google Scholar] [CrossRef] [PubMed]
- Tipton, K.D.; Wolfe, R.R. Exercise, protein metabolism, and muscle growth. Int. J. Sport Nutr. Exerc. Metab. 2001, 11, 109–132. [Google Scholar] [CrossRef] [PubMed]
- Precenzano, F.; Ruberto, M.; Parisi, L.; Salerno, M.; Maltese, A.; Verde, D.; Tripi, G.; Romano, P.; Folco, A.D.; Filippo, T.D.; et al. Sleep habits in children affected by autism spectrum disorders: A preliminary case-control study. Acta Medica Mediterr. 2017, 33, 405–409. [Google Scholar]
- Korea Centers for Disease Control and Prevention Agency. The 9th Korea National Health and Nutrition Examination Survey. Available online: https://knhanes.kdca.go.kr/knhanes/main.do (accessed on 25 May 2025).
- U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020 Sleep Health. 2020. Available online: https://www.cdc.gov/nchs/data/hpdata2020/hp2020mcr-c38-sh.pdf (accessed on 9 May 2025).
- Lim, S.T.; Jung, Y.Z.; Akama, T.; Lee, E. Physical Activity Amount and Cognitive Impairment in Korean Elderly Population. Brain Sci. 2020, 10, 804. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Kim, I.D.; Lim, S.T. Physical activity and protein-intake strategies to prevent sarcopenia in older people. Int. Health 2025, 17, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare, The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2020; Ministry of Health and Welfare, The Korean Nutrition Society: Sejong, Republic of Korea, 2020. [Google Scholar]
- Sateia, M.J. International classification of sleep disorders-third edition: Highlights and modifications. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Short, M.A.; Booth, S.A.; Omar, O.; Ostlundh, L.; Arora, T. The relationship between sleep duration and mood in adolescents: A systematic review and meta-analysis. Sleep Med. Rev. 2020, 52, 101311. [Google Scholar] [CrossRef] [PubMed]
- Bloomberg, M.; Brocklebank, L.; Hamer, M.; Steptoe, A. Joint associations of physical activity and sleep duration with cognitive ageing: Longitudinal analysis of an English cohort study. Lancet Healthy Longev. 2023, 4, e345–e353. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Chen, Y.; Feng, H.; Zhou, M.; Chan, J.W.Y.; Liu, Y.; Kong, A.P.S.; Tan, X.; Wing, Y.K.; Liang, Y.Y.; et al. Association of accelerometer-measured sleep duration and different intensities of physical activity with incident type 2 diabetes in a population-based cohort study. J. Sport Health Sci. 2024, 13, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Xin, S.; Luan, D.; Zou, Z.; Liu, M.; Bai, X.; Gao, Q. Association of physical activity, sedentary time, and sleep duration on the health-related quality of life of college students in Northeast China. Health Qual. Life Outcomes 2019, 17, 124. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Biddle, S.J.H.; Lee, J.T.; Duolikun, N.; Zhang, L.; Wang, Z.; Zhao, Y. The prevalence of multimorbidity and its association with physical activity and sleep duration in middle aged and elderly adults: A longitudinal analysis from China. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 77. [Google Scholar] [CrossRef] [PubMed]
- Monda, V.; Salerno, M.; Fiorenzo, M.; Villano, I.; Viggiano, A.; Sessa, F.; Triggiani, A.I.; Cibelli, G.; Valenzano, A.; Marsala, G.; et al. Role of Sex Hormones in the Control of Vegetative and Metabolic Functions of Middle-Aged Women. Front. Physiol. 2017, 8, 773. [Google Scholar] [CrossRef] [PubMed]
- Aubertin-Leheudre, M.; Lord, C.; Khalil, A.; Dionne, I.J. Six months of isoflavone supplement increases fat-free mass in obese-sarcopenic postmenopausal women: A randomized double-blind controlled trial. Eur. J. Clin. Nutr. 2007, 61, 1442–1444. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Jackson, N.; Gerstner, J.R.; Knutson, K.L. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite 2013, 64, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Santana, A.A.; Pimentel, G.D.; Romualdo, M.; Oyama, L.M.; Santos, R.V.; Pinho, R.A.; de Souza, C.T.; Rodrigues, B.; Caperuto, E.C.; Lira, F.S. Sleep duration in elderly obese patients correlated negatively with intake fatty. Lipids Health Dis. 2012, 11, 99. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, D.L.; Dokkedal-Silva, V.; Fernandes, G.L.; Kim, L.J.; Tufik, S.; Andersen, M.L. Sleep duration as an independent factor associated with vitamin D levels in the EPISONO cohort. J. Clin. Sleep Med. 2021, 17, 2439–2449. [Google Scholar] [CrossRef] [PubMed]
- Sutanto, C.N.; Loh, W.W.; Toh, D.W.K.; Lee, D.P.S.; Kim, J.E. Association Between Dietary Protein Intake and Sleep Quality in Middle-Aged and Older Adults in Singapore. Front. Nutr. 2022, 9, 832341. [Google Scholar] [CrossRef] [PubMed]
- Bossan, F.M.; Dos Anjos, L.A.; Wahrlich, V.; Ferriolli, E.; Pfrimer, K. Comparison of total daily energy expenditure with dietary reference intakes values in a sample of urban, relatively active Brazilian adults: A doubly labeled water study. Am. J. Hum. Biol. 2024, 36, e24027. [Google Scholar] [CrossRef] [PubMed]
- Majid, M.S.; Ahmad, H.S.; Bizhan, H.; Hosein, H.Z.M.; Mohammad, A. The effect of vitamin D supplement on the score and quality of sleep in 20–50 year-old people with sleep disorders compared with control group. Nutr. Neurosci. 2018, 21, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Kou, T.; Zhuang, B.; Ren, Y.; Dong, X.; Wang, Q. The Association between Vitamin D Deficiency and Sleep Disorders: A Systematic Review and Meta-Analysis. Nutrients 2018, 10, 1395. [Google Scholar] [CrossRef] [PubMed]
- Muscogiuri, G.; Barrea, L.; Scannapieco, M.; Di Somma, C.; Scacchi, M.; Aimaretti, G.; Savastano, S.; Colao, A.; Marzullo, P. The lullaby of the sun: The role of vitamin D in sleep disturbance. Sleep Med. 2019, 54, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Eyles, D.W.; Smith, S.; Kinobe, R.; Hewison, M.; McGrath, J.J. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J. Chem. Neuroanat. 2005, 29, 21–30. [Google Scholar] [CrossRef] [PubMed]
- van Vliet, S.; Burd, N.A.; van Loon, L.J. The Skeletal Muscle Anabolic Response to Plant-versus Animal-Based Protein Consumption. J. Nutr. 2015, 145, 1981–1991. [Google Scholar] [CrossRef] [PubMed]
- Chandel, N.S. Carbohydrate Metabolism. Cold Spring Harb. Perspect. Biol. 2021, 13, a040568. [Google Scholar] [CrossRef] [PubMed]
| Variable | Male (n = 2347) | Female (n = 3144) | ||
|---|---|---|---|---|
| ≥8 h (n = 776) | <8 h (n = 1571) | ≥8 h (n = 927) | <8 h (n = 2217) | |
| Age (years) | 51.92 ± 18.18 | 54.73 ± 16.06 | 48.46 ± 17.16 | 56.04 ± 15.45 |
| Height (cm) | 170.89 ± 6.80 | 170.43 ± 6.75 | 157.39 ± 6.32 | 157.37 ± 6.33 |
| Weight (kg) | 71.70 ± 12.97 | 71.62 ± 12.27 | 58.83 ± 10.42 | 58.64 ± 9.76 |
| BMI (kg/m2) | 24.47 ± 3.62 | 24.58 ± 3.46 | 23.35 ± 3.91 | 23.67 ± 3.68 |
| WC (cm) | 88.00 ± 9.95 | 88.24 ± 9.60 | 79.53 ± 10.87 | 81.18 ± 10.15 |
| SBP (mmHg) | 122.07 ± 13.53 | 121.67 ± 14.83 | 114.77 ± 16.50 | 118.49 ± 16.36 |
| DBP (mmHg) | 75.99 ± 9.35 | 75.62 ± 9.50 | 71.70 ± 9.34 | 72.55 ± 9.00 |
| Sleep duration (h) | 8.47 ± 0.72 | 6.43 ± 0.90 | 8.78 ± 0.58 | 6.27 ± 1.03 |
| Variable | Male (n = 2347) | p-Value | Female (n = 3144) | p-Value | ||
|---|---|---|---|---|---|---|
| ≥8 h (n = 776) | <8 h (n = 1571) | ≥8 h (n = 927) | <8 h (n = 2217) | |||
| MPA (min/week) | 102.33 ± 220.3 | 82.17 ± 152.90 | 0.026 | 71.96 ± 186.67 | 57.53 ± 123.00 | 0.011 |
| VPA (min/week) | 29.89 ± 109.94 | 21.33 ± 74.33 | 0.010 | 14.06 ± 61.36 | 10.48 ± 43.86 | 0.066 |
| MVPA (min/week) | 132.22 ± 269.29 | 103.50 ± 184.97 | 0.003 | 86.02 ± 204.02 | 68.01 ± 135.86 | 0.004 |
| Variable | Male (n = 2347) | p-Value | Female (n = 3144) | p-Value | ||
|---|---|---|---|---|---|---|
| ≥8 h (n = 776) | <8 h (n = 1571) | ≥8 h (n = 927) | <8 h (n = 2217) | |||
| Vitamin D (µg) | 3.13 ± 5.21 | 2.76 ± 3.17 | 0.029 | 2.63 ± 4.42 | 2.28 ± 2.80 | 0.008 |
| Carbohydrates (g) | 285.86 ± 113.28 | 285.53 ± 104.36 | 0.944 | 228.19 ± 96.37 | 227.29 ± 92.33 | 0.806 |
| Protein (g) | 79.13 ± 40.21 | 73.18 ± 28.54 | <0.001 | 60.32 ± 29.74 | 57.52 ± 27.66 | 0.011 |
| Fats (g) | 55.20 ± 42.86 | 50.89 ± 32.29 | 0.007 | 43.76 ± 28.40 | 41.08 ± 28.13 | 0.015 |
| Unadjusted | Adjusted a | |||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Physical activity Protein intake below KDRIs Protein intake above the KDRIs | 1.00 1.59 (1.388–1.823) | <0.001 | 1.00 1.35 (1.169–1.554) | <0.001 |
| Sleep duration Protein intake below KDRIs Protein intake above the KDRIs | 1.00 1.12 (1.070–1.162) | <0.001 | 1.00 1.06 (1.010–1.103) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.; Lim, S.-T. Associations Among Sleep Duration, Physical Activity, and Nutrient Intake in Korean Adults. Nutrients 2025, 17, 2324. https://doi.org/10.3390/nu17142324
Lee E, Lim S-T. Associations Among Sleep Duration, Physical Activity, and Nutrient Intake in Korean Adults. Nutrients. 2025; 17(14):2324. https://doi.org/10.3390/nu17142324
Chicago/Turabian StyleLee, Eunjae, and Seung-Taek Lim. 2025. "Associations Among Sleep Duration, Physical Activity, and Nutrient Intake in Korean Adults" Nutrients 17, no. 14: 2324. https://doi.org/10.3390/nu17142324
APA StyleLee, E., & Lim, S.-T. (2025). Associations Among Sleep Duration, Physical Activity, and Nutrient Intake in Korean Adults. Nutrients, 17(14), 2324. https://doi.org/10.3390/nu17142324







