Targeted Outreach by an Insurance Company Improved Dietary Habits and Urine Sodium/Potassium Ratios Among High-Risk Individuals with Lifestyle-Related Diseases
Abstract
1. Introduction
2. Materials and Methods
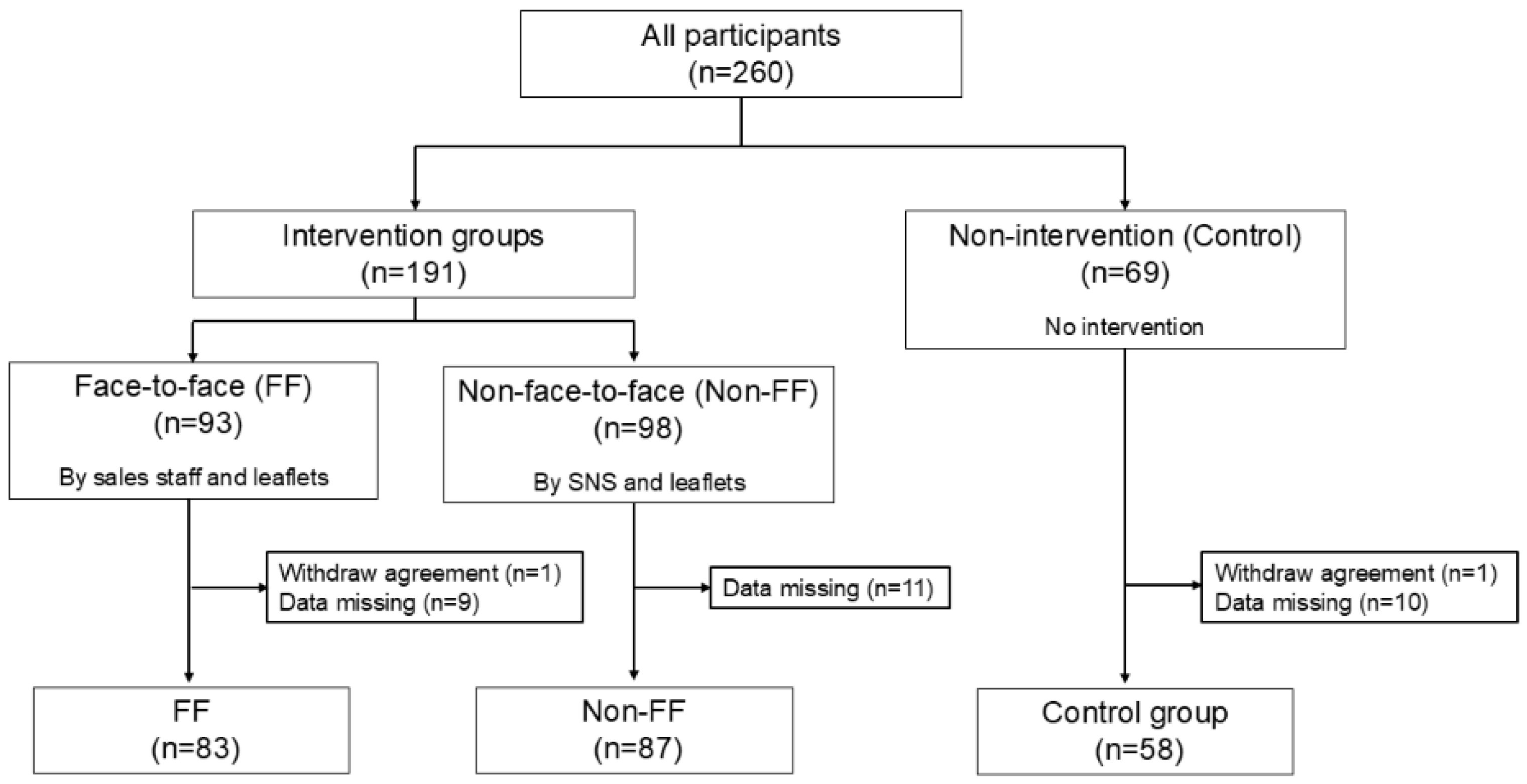
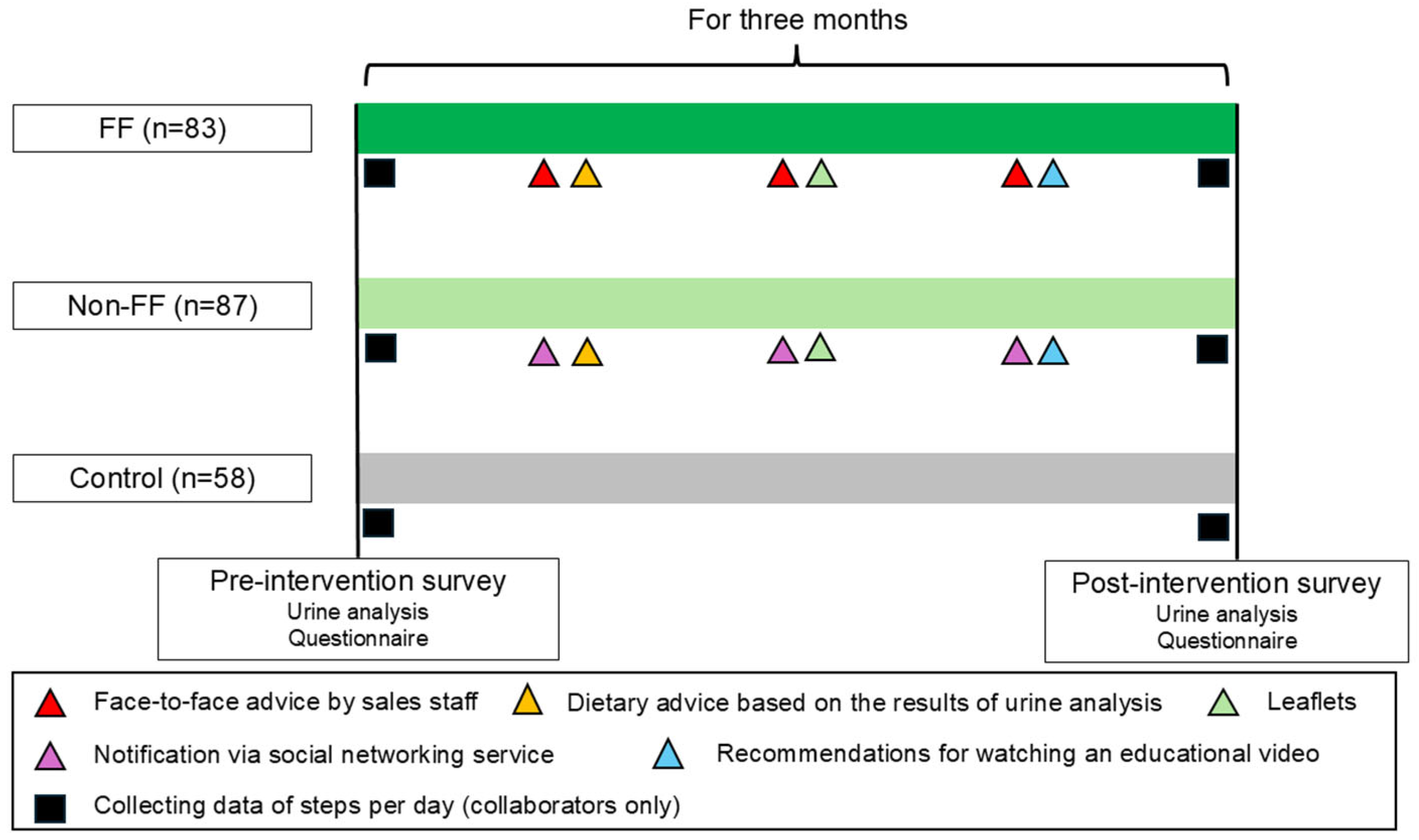
2.1. Study Design and Settings
2.2. Intervention Strategies
2.3. Data Collection and Processing
2.4. Statistical Analyses
3. Results
3.1. Baseline Characteristics of the Three Groups
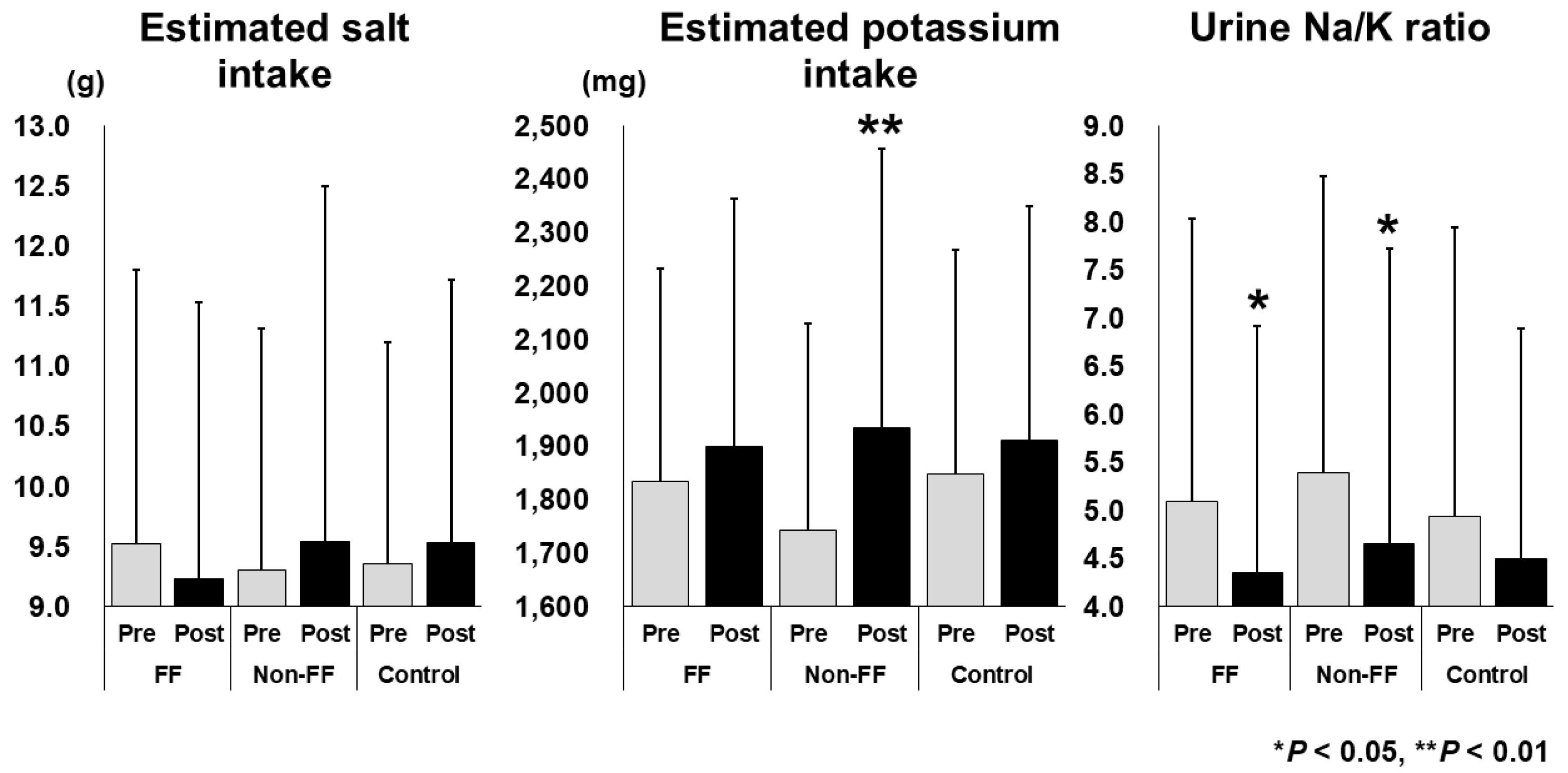
3.2. Changes in Estimated Salt and Potassium Intake and the Urine Na/K Ratio
3.3. Factors Associated with a Decrease in the Urine Na/K Ratio
3.4. Differences Between the Participants Who Watched or Did Not Watch the Educational Video
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FF | Face-to-face |
| Non-FF | Non-face-to-face |
| SNS | Social networking sites |
| BMI | Body mass index |
References
- Katsimardou, A.; Imprialos, K.; Stavropoulos, K.; Sachinidis, A.; Doumas, M.; Athyros, V. Hypertension in Metabolic Syndrome: Novel Insights. Curr. Hypertens. Rev. 2020, 16, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Dzau, V.J.; Hodgkinson, C.P. Precision Hypertension. Hypertension 2024, 81, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Otani, K.; Haruyama, R.; Gilmour, S. Prevalence and Correlates of Hypertension among Japanese Adults, 1975 to 2010. Int. J. Environ. Res. Public Health 2018, 15, 1645. [Google Scholar] [CrossRef]
- Carey, R.M.; Moran, A.E.; Whelton, P.K. Treatment of Hypertension: A Review. JAMA 2022, 328, 1849–1861. [Google Scholar] [CrossRef]
- Graudal, N.; Hubeck-Graudal, T.; Jürgens, G.; Taylor, R.S. Dose-response relation between dietary sodium and blood pressure: A meta-regression analysis of 133 randomized controlled trials. Am. J. Clin. Nutr. 2019, 109, 1273–1278. [Google Scholar] [CrossRef]
- Aburto, N.J.; Hanson, S.; Gutierrez, H.; Hooper, L.; Elliott, P.; Cappuccio, F.P. Effect of increased potassium intake on cardiovascular risk factors and disease: Systematic review and meta-analyses. BMJ 2013, 346, f1378. [Google Scholar] [CrossRef] [PubMed]
- Tabara, Y.; Takahashi, Y.; Kumagai, K.; Setoh, K.; Kawaguchi, T.; Takahashi, M.; Muraoka, Y.; Tsujikawa, A.; Gotoh, N.; Terao, C.; et al. Descriptive epidemiology of spot urine sodium-to-potassium ratio clarified close relationship with blood pressure level: The Nagahama study. J. Hypertens. 2015, 33, 2407–2413. [Google Scholar] [CrossRef]
- Kogure, M.; Nakaya, N.; Hirata, T.; Tsuchiya, N.; Nakamura, T.; Narita, A.; Suto, Y.; Honma, Y.; Sasaki, H.; Miyagawa, K.; et al. Sodium/potassium ratio change was associated with blood pressure change: Possibility of population approach for sodium/potassium ratio reduction in health checkup. Hypertens. Res. 2021, 44, 225–231. [Google Scholar] [CrossRef]
- Hisamatsu, T.; Kogure, M.; Tabara, Y.; Hozawa, A.; Sakima, A.; Tsuchihashi, T.; Yoshita, K.; Hayabuchi, H.; Node, K.; Takemi, Y.; et al. Practical use and target value of urine sodium-to-potassium ratio in assessment of hypertension risk for Japanese: Consensus Statement by the Japanese Society of Hypertension Working Group on Urine Sodium-to-Potassium Ratio. Hypertens. Res. 2024, 47, 3288–3302. [Google Scholar] [CrossRef]
- Nakaji, S.; Murashita, K.; Mikami, T.; Tamada, Y.; Uemura, N. Strategies for promoting health in society utilizing quality-of-life check-ups: A protocol paper. Prevent. Med. Res. 2024, 1, 43–54. [Google Scholar] [CrossRef]
- Yamagishi, K.; Iso, H. The criteria for metabolic syndrome and the national health screening and education system in Japan. Epidemiol. Health 2017, 39, e2017003. [Google Scholar] [CrossRef]
- Jane, M.; Hagger, M.; Foster, J.; Ho, S.; Pal, S. Social media for health promotion and weight management: A critical debate. BMC Public Health 2018, 18, 932. [Google Scholar] [CrossRef] [PubMed]
- Halling Ullberg, O.; Toivanen, S.; Tillander, A.; Bälter, K. Workplace health promotion to facilitate physical activity among office workers in Sweden. Front. Public Health 2023, 11, 1175977. [Google Scholar] [CrossRef]
- Glowacki, E.M.; Centeio, E.E.; Van Dongen, D.J.; Carson, R.L.; Castelli, D.M. Health Promotion Efforts as Predictors of Physical Activity in Schools: An Application of the Diffusion of Innovations Model. J. Sch. Health 2016, 86, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Symes, L.; Hadgraft, N.; Marsh, P.; Nuttman, S.; Kingsley, J. ‘Surrounding yourself with beauty’: Exploring the health promotion potential of a rural garden appreciation group. Health Promot. Int. 2023, 38, daad010. [Google Scholar] [CrossRef]
- Kai, Y.; Fujii, Y.; Takashi, N.; Yoshiba, K.; Muramatsu-Noguchi, Y.; Noda, T.; Jindo, T.; Kidokoro, T.; Yajima, Y.; Kasuga, J.; et al. Promoting health and productivity management in small companies through outreach-based public-private partnership: The Yokohama Linkworker Project. Front. Public Health 2024, 12, 1345771. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.N.; Lambert, E.V.; da Silva, R.; Greyling, M.; Nossel, C.; Noach, A.; Derman, W.; Gaziano, T. The association between medical costs and participation in the vitality health promotion program among 948,974 members of a South African health insurance company. Am. J. Health Promot. 2010, 24, 199–204. [Google Scholar] [CrossRef]
- Patel, D.N.; Nossel, C.; Alexander, E.; Yach, D. Innovative business approaches for incenting health promotion in sub-Saharan Africa: Progress and persisting challenges. Prog. Cardiovasc. Dis. 2013, 56, 356–362. [Google Scholar] [CrossRef]
- Mantzari, E.; Vogt, F.; Shemilt, I.; Wei, Y.; Higgins, J.P.; Marteau, T.M. Personal financial incentives for changing habitual health-related behaviors: A systematic review and meta-analysis. Prev. Med. 2015, 75, 75–85. [Google Scholar] [CrossRef]
- Nakamura, K.; Ogata, T. Locomotive Syndrome: Definition and Management. Clin. Rev. Bone Miner. Metab. 2016, 14, 56–67. [Google Scholar] [CrossRef]
- Tanaka, T.; Okamura, T.; Miura, K.; Kadowaki, T.; Ueshima, H.; Nakagawa, H.; Hashimoto, T. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J. Hum. Hypertens. 2002, 16, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Raphadu, T.T.; Mphekgwana, P.M.; Matshipi, M.; Monyeki, K.D. A Longitudinal Investigation on the Effects of Sodium and Potassium Intake on the Development of Hypertension and Abdominal Obesity from Childhood to Young Adulthood amongst Ellisras Rural Population, South Africa. Children 2023, 10, 1330. [Google Scholar] [CrossRef]
- Mirmiran, P.; Gaeini, Z.; Bahadoran, Z.; Ghasemi, A.; Norouzirad, R.; Tohidi, M.; Azizi, F. Urinary sodium-to-potassium ratio: A simple and useful indicator of diet quality in population-based studies. Eur. J. Med. Res. 2021, 26, 3. [Google Scholar] [CrossRef] [PubMed]
- Eakin, E.G.; Lawler, S.P.; Vandelanotte, C.; Owen, N. Telephone interventions for physical activity and dietary behavior change: A systematic review. Am. J. Prev. Med. 2007, 32, 419–434. [Google Scholar] [CrossRef] [PubMed]
- Valmorbida, J.L.; Sangalli, C.N.; Leffa, P.S.; Baratto, P.S.; Rauber, F.; Mennella, J.A.; Vitolo, M.R. Sodium Intake Tracked from Infancy and Salt Taste Preference during Adolescence: Follow-up of a Randomized Controlled Field Trial in Brazil. Curr. Dev. Nutr. 2023, 7, 100011. [Google Scholar] [CrossRef]
- Kimura, T.; Kobayashi, H.; Nakayama, E.; Kakihana, W. Seasonality in physical activity and walking of healthy older adults. J. Physiol. Anthropol. 2015, 34, 33. [Google Scholar] [CrossRef]
- Mitsui, T.; Barajima, T.; Kanachi, M.; Shimaoka, K. Daily walking activity among male office workers in a rural town in northern Japan. J. Physiol. Anthropol. 2010, 29, 43–46. [Google Scholar] [CrossRef][Green Version]
- Gehlbach, H.; Artino, A.R., Jr. The Survey Checklist (Manifesto). Acad. Med. 2018, 93, 360–366. [Google Scholar] [CrossRef]
| Dietary behaviors |
| I’m careful not to avoid excessive energy intake. |
| I’m careful not to eat too much salt. |
| I’m careful not to get too fat. |
| I try to consume an adequate intake of potassium, vitamins, minerals, and fiber. |
| I try to maintain an appropriate carbohydrate intake. |
| Locomotor activities |
| I perform regular gymnastics/stretching. |
| I’m aware of standing up, moving, standing tall, etc., regularly. |
| I regularly do aerobic exercise (walking, running, and aquabics, etc.). |
| I usually do strength training. |
| I try to incorporate a little exercise into my daily life, such as using the stairs or doing squats during breaks. |
| FF (n = 83) | Non-FF (n = 87) | Control (n = 58) | |
|---|---|---|---|
| Professional/technical workers | 18 (21.7%) | 21 (24.1%) | 14 (24.1%) |
| Manager | 5 (6.0%) | 1 (1.1%) | 5 (8.6%) |
| Clerk | 16 (19.3%) | 19 (21.8%) | 15 (25.9%) |
| Sales worker | 3 (3.6%) | 11 (12.6%) | 3 (5.2%) |
| Service worker | 10 (12.0%) | 17 (19.5%) | 8 (13.8%) |
| Security worker | 2 (2.4%) | 1 (1.1%) | 3 (5.2%) |
| Construction and civil engineering | 4 (4.8%) | 2 (2.3%) | 1 (1.7%) |
| Agriculture | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Forestry | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Fishing | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Transport and communications | 7 (8.4%) | 9 (10.3%) | 3 (5.2%) |
| Production process and laborers | 7 (8.4%) | 0 (0.0%) | 4 (6.9%) |
| Housewives | 0 (0.0%) | 1 (1.1%) | 0 (0.0%) |
| None | 2 (2.4%) | 1 (1.1%) | 0 (0.0%) |
| Others | 9 (10.8%) | 4 (4.6%) | 2 (3.4%) |
| FF (n = 83) | Non-FF (n = 87) | Control (n = 58) | p Value | |
|---|---|---|---|---|
| Male | 54 (65.0%) | 50 (57.4%) | 41 (70.6%) | 0.253 |
| Age (years) | 43.9 ± 10.0 | 43.4 ± 10.9 | 43.4 ± 10.1 | 0.983 |
| BMI (kg/m2) | 25.2 ± 4.5 | 24.3 ± 4.7 | 26.0 ± 4.0 | 0.041 * |
| Estimated salt intake (g/day) | 9.52 ± 2.28 | 9.30 ± 2.00 | 9.35 ± 1.84 | 0.942 |
| Estimated potassium intake (mg/day) | 1835.5 ± 396.5 | 1743.0 ± 386.8 | 1849.2 ± 419.0 | 0.167 |
| Urine Na/K ratio | 5.10 ± 2.93 | 5.39 ± 3.08 | 4.94 ± 3.00 | 0.658 |
| <2.0 | 8 (9.6%) | 3 (3.4%) | 5 (8.6%) | |
| ≧2.0, <4.0 | 27 (32.5%) | 30 (34.5%) | 20 (34.5%) | |
| ≧ 4.0 | 48 (57.8%) | 54 (62.1%) | 33 (56.9%) | |
| Present treatment of lifestyle disease | 20 (24.1%) | 22 (25.3%) | 20 (34.5%) | 0.347 |
| Past treatment of lifestyle disease | 21 (25.3%) | 22 (25.3%) | 17 (29.3%) | 0.835 |
| Previous suggestions of hypertension | 16 (19.3%) | 22 (25.3%) | 15 (25.9%) | 0.560 |
| Total scores in the lifestyle questionnaire | ||||
| Dietary behavior | 13.1 ± 4.6 | 13.6 ± 4.4 | 13.7 ± 4.5 | 0.624 |
| Locomotor activity | 15.0 ± 5.0 | 14.7 ± 4.9 | 15.0 ± 4.8 | 0.328 |
| Number of participants who cooperated with step counting | 33 (39.7%) | 46 (52.8%) | 26 (44.8%) | |
| Steps per day | 3825.8 ± 2446.8 | 4876.9 ± 3080.8 | 4397.0 ± 2970.2 | 0.328 |
| Urine Na/K Ratio | ||||
|---|---|---|---|---|
| Decreased (n =128) | Not Decreased (n = 100) | p Value | ||
| Interventional groups | ||||
| FF | 51 (39.8%) | 32 (32.0%) | ||
| Non-FF | 49 (38.3%) | 38 (38.0%) | 0.300 | |
| Control | 28 (21.9%) | 30 (30.0%) | ||
| Age | 43.0 ± 10.6 | 44.3 ± 9.9 | 0.324 | |
| Sex | ||||
| Male | 82 (64.1%) | 63 (63.0%) | 0.869 | |
| Female | 46 (35.9%) | 37 (37.0%) | ||
| BMI (kg/m2) | 24.8 ± 4.4 | 25.3 ± 4.6 | 0.478 | |
| Past treatment of lifestyle disease | 29 (22.7%) | 31 (31.0%) | 0.156 | |
| Present treatment of lifestyle disease | 33 (25.8%) | 29 (29.0%) | 0.588 | |
| Recent suggestion of hypertension | 30 (23.4%) | 23 (23.0%) | 0.938 | |
| Total scores in lifestyle questionnaire (baseline) | ||||
| Dietary behaviors | 13.2 ± 4.4 | 13.8 ± 4.6 | 0.435 | |
| Locomotor activities | 15.1 ± 5.0 | 14.6 ± 4.9 | 0.382 | |
| The number of participants who answered the post-interventional questionnaire | 224 | 224 | ||
| Whether the leaflets had been read | ||||
| Almost all/partially | 92 (41.1%) | 68 (30.4%) | 0.458 | |
| None | 33 (14.7%) | 31 (13.8%) | ||
| Whether the video had been watched | ||||
| Almost all/partially | 82 (36.6%) | 50 (22.3%) | 0.029 * | |
| None | 43 (19.2%) | 49 (21.9%) | ||
| Affected by | ||||
| Urinalysis | 96 (42.9%) | 67 (29.9%) | 0.134 | |
| Leaflets | 63 (28.1%) | 46 (20.5%) | 1.000 | |
| Video | 58 (25.9%) | 37 (16.5%) | 0.842 | |
| Constant | Partial Regression Coefficient | Significant Probability | Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Watched the educational video | –0.131 | 0.625 | 0.023 * | 1.869 | 1.089–3.206 |
| Pre-Intervention | Post-Intervention | p Value | |
|---|---|---|---|
| Estimated salt intake (g/d) | 9.44 ± 2.00 | 9.36 ± 2.61 | 0.482 |
| Estimated potassium intake (mg/d) | 1786.4 ± 401.5 | 1920.3 ± 506.4 | 0.007 * |
| Urine Na/K ratio | 5.28 ± 2.85 | 4.49 ± 2.83 | 0.001 ** |
| BMI (kg/m2) | 24.5 ± 4.6 | 24.6 ± 4.6 | 0.476 |
| Total points of dietary behavior | 13.3 ± 4.3 | 14.9 ± 3.7 | <0.001 ** |
| Total points of locomotor activity | 14.6 ± 5.0 | 13.9 ± 4.6 | 0.045 * |
| Numbers of individuals who answered the question on the number of steps | 63 (47.4%) | 59 (44.6%) | |
| Steps per day | 4542.9 ± 2940.6 | 4483.7 ± 3124.3 | 0.590 |
| Watched (n = 132) | Did Not Watch (n = 92) | p Value | |
|---|---|---|---|
| Age | 44.1 ± 10.7 | 42.8 ± 9.7 | 0.305 |
| Sex | |||
| Male | 82 (62.1%) | 61 (66.3%) | 0.573 |
| Female | 50 (37.9%) | 31 (33.7%) | |
| BMI (baseline) (kg/m2) | 24.5 ± 4.6 | 25.8 ± 4.2 | 0.018 * |
| BMI (after the intervention period) (kg/m2) | 24.6 ± 4.6 | 25.8 ± 4.3 | 0.021 * |
| Past treatment of lifestyle disease | 31 (23.5%) | 25 (27.2%) | 0.530 |
| Recent suggestion of hypertension | 28 (21.2%) | 22 (23.9%) | 0.369 |
| Recent suggestion of other lifestyle diseases | 63 (47.7%) | 55 (59.8%) | 0.530 |
| The type of intervention | 0.075 | ||
| Face-to-face | 62 (47.0%) | 20 (21.7%) | |
| Non-face-to-face | 70 (53.0%) | 14 (15.2%) | 0.251 |
| Recent suggestion of hypertension | 28 (21.2%) | 22 (23.9%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, S.; Fukui, J.; Otsu, A.; Yokoyama, S.; Tanaka, T.; Sawada, K.; Nakaji, S.; Tamada, Y.; Murashita, K.; Mikami, T. Targeted Outreach by an Insurance Company Improved Dietary Habits and Urine Sodium/Potassium Ratios Among High-Risk Individuals with Lifestyle-Related Diseases. Nutrients 2025, 17, 2152. https://doi.org/10.3390/nu17132152
Tanaka S, Fukui J, Otsu A, Yokoyama S, Tanaka T, Sawada K, Nakaji S, Tamada Y, Murashita K, Mikami T. Targeted Outreach by an Insurance Company Improved Dietary Habits and Urine Sodium/Potassium Ratios Among High-Risk Individuals with Lifestyle-Related Diseases. Nutrients. 2025; 17(13):2152. https://doi.org/10.3390/nu17132152
Chicago/Turabian StyleTanaka, Sunao, Junji Fukui, Akira Otsu, Shintaro Yokoyama, Tsukasa Tanaka, Kaori Sawada, Shigeyuki Nakaji, Yoshinori Tamada, Koichi Murashita, and Tatsuya Mikami. 2025. "Targeted Outreach by an Insurance Company Improved Dietary Habits and Urine Sodium/Potassium Ratios Among High-Risk Individuals with Lifestyle-Related Diseases" Nutrients 17, no. 13: 2152. https://doi.org/10.3390/nu17132152
APA StyleTanaka, S., Fukui, J., Otsu, A., Yokoyama, S., Tanaka, T., Sawada, K., Nakaji, S., Tamada, Y., Murashita, K., & Mikami, T. (2025). Targeted Outreach by an Insurance Company Improved Dietary Habits and Urine Sodium/Potassium Ratios Among High-Risk Individuals with Lifestyle-Related Diseases. Nutrients, 17(13), 2152. https://doi.org/10.3390/nu17132152






