Nutrition Education Among Community-Dwelling Polish Seniors—A Pilot Study of Diet Quality, Health Status, and Public Health Interventions
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Research Tool and Data Collection
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Profile and BMI Classification
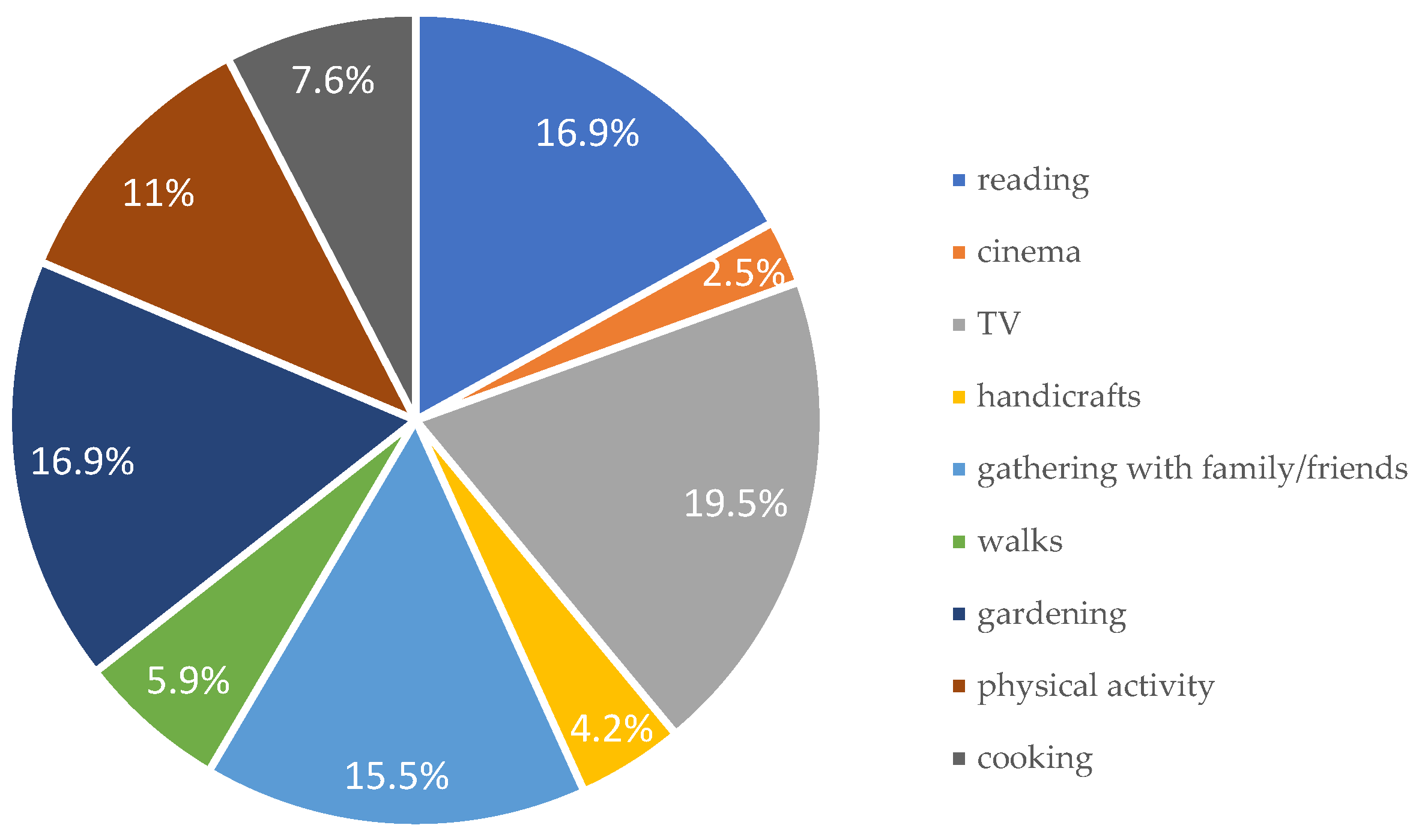
3.2. Lifestyle Patterns, Health Perception, and Physical Activity
3.3. Dietary Habits, Meal Frequency, and Diet Quality Index (pHDI/nHDI)
3.4. Seniors’ Views on Nutrition and Health Education
4. Discussion
4.1. Lifestyle and Nutrition in Healthy Aging
4.2. Dietary Behaviors and Nutritional Risks
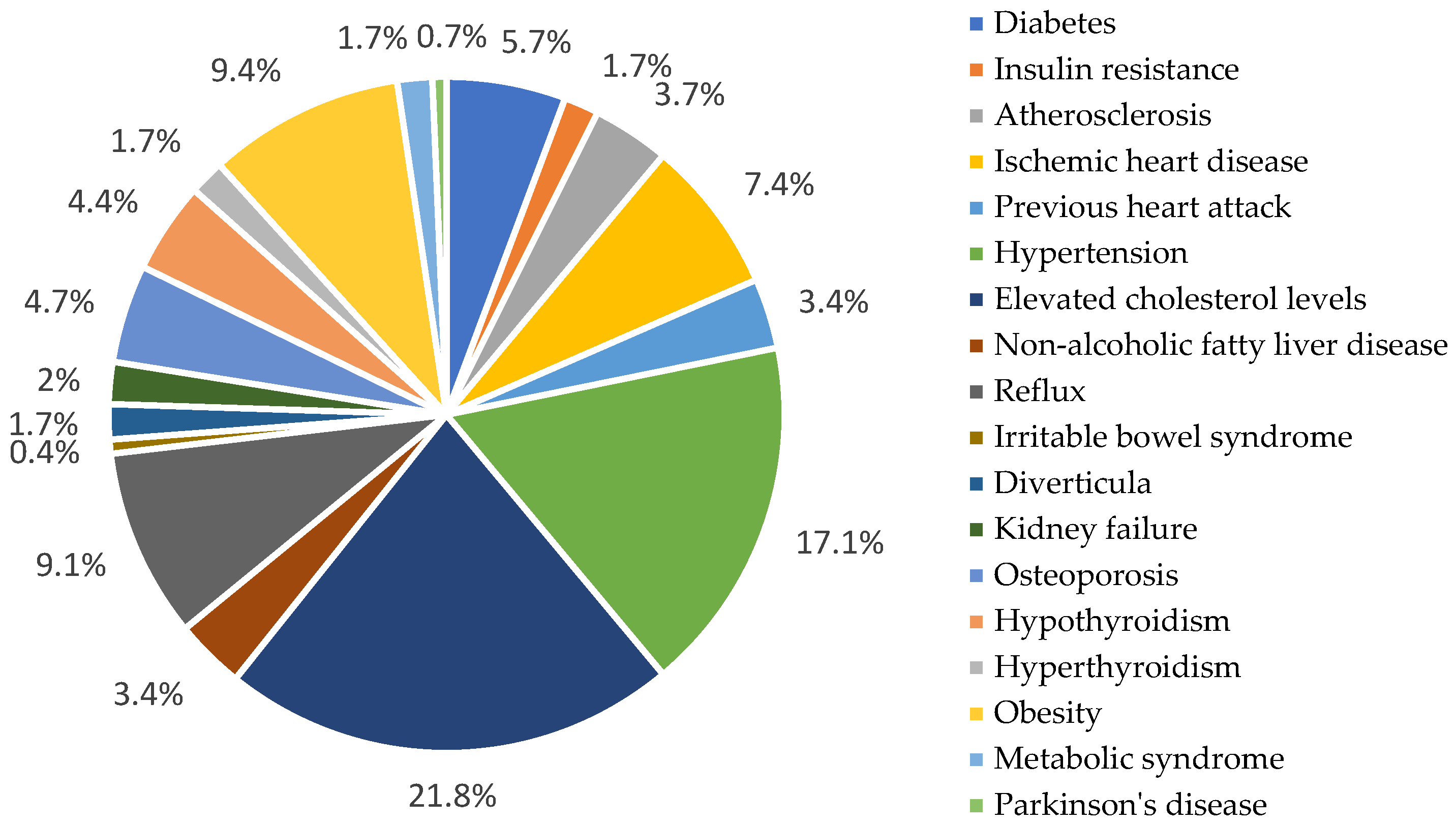
4.3. Diet Quality as a Predictor of Diet-Related Diseases
4.4. Effectiveness and Reach of Nutritional Education
5. Study Limitation
- (1)
- Include larger, probabilistically selected samples;
- (2)
- Apply mixed-method or longitudinal approaches;
- (3)
- Incorporate clinical and functional health measures;
- (4)
- Target underrepresented groups, including rural and socially isolated individuals.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO, World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 10 March 2025).
- Contento, I. Edukacja Żywieniowa; PWN: Warszawa, Poland, 2012; p. 14. [Google Scholar]
- Pew Research Center. Growing Old in America: Expectations vs. Reality. 29 June 2009. Available online: https://core.ac.uk/download/pdf/71351636.pdf (accessed on 10 March 2025).
- GUS. Pojęcia Stosowane w Statystyce Publicznej. Available online: https://stat.gov.pl/metainformacje/slownik-pojec/pojecia-stosowane-w-statystyce-publicznej (accessed on 10 March 2025).
- GUS. Sytuacja Osób Starszych w Polsce w 2023 Roku. Available online: https://stat.gov.pl/obszary-tematyczne/osoby-starsze/osoby-starsze/sytuacja-osob-starszych-w-polsce-w-2023-roku,2,6.html# (accessed on 10 March 2025).
- Eurostat. Ageing Europe-Looking at the Lives of Older People in the EU. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_statistics_on_population_developments (accessed on 10 March 2025).
- Petersen, K.S.; Kris-Etherton, P.M. Diet quality assessment and the relationship between diet quality and cardiovascular disease risk. Nutrients 2021, 13, 4305. [Google Scholar] [CrossRef] [PubMed]
- Szostak-Węgierek, D. Żywienie Osób Starszych; PZWL: Warszawa, Poland, 2020; p. 27. [Google Scholar]
- Śliż, D.; Mamcarz, A. Medycyna Stylu Życia; PZWL: Warszawa, Poland, 2021; p. 337. [Google Scholar]
- GUS. Trwanie Życia w 2023r. 30 July 2024; p. 26. Available online: https://stat.gov.pl/obszary-tematyczne/ludnosc/trwanie-zycia/trwanie-zycia-w-2023-roku,2,18.html (accessed on 10 March 2025).
- Lewandowicz-Umyszkiewicz, M.; Wieczorowska-Tobis, K. Nowe kryteria diagnozowania niedożywienia New criteria for the diagnosis of malnutrition. Geriatria 2019, 13, 101–105. [Google Scholar]
- Saffel-Shrier, S.; Johnson, M.A.; Francis, S.L. Position of the Academy of Nutrition and Dietetics and the Society for Nutrition Education and Behavior: Food and nutrition programs for community-residing older adults. J. Nutr. Educ. Behav. 2019, 51, 781–797. [Google Scholar] [CrossRef] [PubMed]
- Majdua, G.J.I.; Gatar, M.M.; Hakami, M.M.O.; Alhazmi, G.; Alnuman, H.I.; Masmali, A.A.M. The Role of Nutrition Education and Health Education in Public Health. J. Int. Crisis Risk Commun. Res. 2024, 7, 359–364. [Google Scholar]
- Khurshid, F.; Waris, W.; Khurshid, A. Nutritional Considerations for Older Adults: Promoting Healthy Aging and Preventing Age-Related Diseases. J. Regen. Med. 2024, 13, 1000299. [Google Scholar]
- World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- KomPan®. Kwestionariusz Do Badania Poglądów i Zwyczajów Żywieniowych Oraz Procedura Opracowania Danych, 2nd ed.; KomPan®: Olsztyn, Poland, 2020. [Google Scholar]
- Wadolowska, L.; Stasiewicz, B. The manual for developing nutritional data from the KomPAN® Questionare. In KomPAN® Dietary Habits and Nutrition Beliefs Questionare and the Manual for Developing Nutritional Data; Gawecki, J., Ed.; The Committee of Human Nutrition, Polish Academy of Sciences: Olsztyn, Poland, 2020; pp. 35–56. [Google Scholar]
- Jarosz, M.; Rychlik, E.; Stoś, K.; Charzewska, J. Normy Żywienia Dla Populacji Polski i ich Zastosowanie; National Institute of Public Health–National Institute of Hygiene–National Research Institute: Warsaw, Poland, 2020. [Google Scholar]
- Gajda, R.; Jeżewska-Zychowicz, M.; Raczkowska, E.; Rak, K.; Szymala-Pędzik, M.; Noculak, Ł.; Sobieszczańska, M. Association of Dietary Patterns, Suspected Sarcopenia, and Frailty Syndrome among Older Adults in Poland—A Cross-Sectional Study. Nutrients 2024, 16, 3090. [Google Scholar] [CrossRef]
- Ręklewski, M. Statystyka Opisowa. Teoria i Przykłady; Państwowa Uczelnia Zawodowa We Włocławku: Włocławek, Poland, 2020; p. 95. [Google Scholar]
- Stephen, B. Causal role of high body mass index in multiple chronic diseases: A systematic review and meta-analysis of Mendelian randomization studies. BMC Med. 2021, 19, 320. [Google Scholar]
- Tańska, M.; Babicz-Zielińska, E.; Komorpowska-Szczepańska, W. Zwyczaje żywieniowe osób starszych i ich wpływ na występowanie nadwagi i otyłości. Fam. Med. Prim. Care Rev. 2013, 178–180. [Google Scholar]
- Klimek, E.; Kamińska, A. Żywienie osób w Podeszłym Wieku, Medycyna Praktyczna. 2021. Available online: https://www.mp.pl/geriatria/wytyczne/27138 (accessed on 11 March 2025).
- Kotowska, A.; Sochacka, K.; Wiśniewski, R.; Lachowicz-Wiśniewska, S. Dietary Habits of Young Poles and Their Selected Determinants: A Review and Implications for Public Health. Nutrients 2024, 16, 3561. [Google Scholar] [CrossRef]
- Narodowe Centrum Edukacji Żywieniowej. Zasady Żywienia Seniorów. Available online: https://ncez.pzh.gov.pl/seniorzy/zasady-zywienia-seniorow/ (accessed on 10 March 2025).
- Charzewska, J. Dlaczego Osoby Starsze Powinny Spożywać Mleko i Fermentowane Napoje Mleczne; Narodow Centrum Edukacji Żywieniowej: Warszawa, Poland, 2018. [Google Scholar]
- Guantario, B.; Giribaldi, M.; Devirgiliis, C.; Finamore, A.; Colombino, E.; Capucchio, M.T.; Evangelista, R.; Motta, V.; Zinno, P.; Cirrincione, S.; et al. A comprehensive evaluation of the impact of bovine milk containing different beta-casein profiles on gut health of ageing mice. Nutrients 2020, 12, 2147. [Google Scholar] [CrossRef] [PubMed]
- Visioli, F.; Strata, A. Milk, dairy products, and their functional effects in humans: A narrative review of recent evidence. Adv. Nutr. 2014, 5, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Wierzbicka, J.; Brukwicka, I.; Kopański, Z.; Rowiński, J.; Furmanik, F. Wybrane Aspekty Procesu Starzenia Się Człowieka. 2017. Available online: http://jchc.eu/numery/2017_2/201721.pdf (accessed on 11 March 2025).
- Drywień, M.E.; Kuć, A. Specyfika zachowań żywieniowych osób starszych pochodzących ze środowiska wiejskiego. Kosmos 2019, 68, 303–310. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Izquierdo, M.; de Souto Barreto, P.; Arai, H.; Bischoff-Ferrari, H.A.; Cadore, E.L.; Cesari, M.; Chen, L.K.; Coen, P.M.; Courneya, K.S.; Duque, G.; et al. Global consensus on optimal exercise recommendations for enhancing healthy longevity in older adults (ICFSR). J. Nutr. Health Aging 2025, 29, 100401. [Google Scholar] [CrossRef]
- Taylor, D. Physical activity is medicine for older adults. Postgrad. Med. J. 2014, 90, 26–32. [Google Scholar] [CrossRef]
- Wieczorkowska-Tobis, K.; Talarska, D. Pomyślna Starość; Wydawnictwo Uniwersytetu Medycznego: Poznań, Poland, 2010. [Google Scholar]
- Głowacka, P. The Psychological Aspect of the Aging Process. p. 121. Available online: https://www.researchgate.net/publication/305755083_Psychologiczny_aspekt_procesu_starzenia (accessed on 10 March 2025).
- Adamska, E.; Ostrowska, L.; Adamska, E.; Maliszewska, K.; Citko, A.; Waszczeniuk, M.; Przystupa, W.; Majewski, R.; Wasilewska, A.; Milewski, R.; et al. Różnice w nawykach i preferencjach żywieniowych osób dorosłych w zależności od wieku. Rocz. Państwowego Zakładu Hig. 2012, 63, 73–81. [Google Scholar]
- Jędrusek-Golińska, A.; Waszkowiak, K.; Szymandera-Buszka, K.; Kobus-Cisowska, J.; Kmiecik, D.; Górecka, D. Wybrane zachowania prozdrowotne ludzi starszych z terenu Wielkopolski (badania wstępne). Bromat. Chem. Toksykol. 2016, 3, 490–494. [Google Scholar]
- Śmidowicz, A.; Reguła, J. Analiza zachowań żywieniowych predysponujących do rozwoju chorób żywieniowozależnych u osób po 40. roku życia. Forum Zaburzeń Metab. 2016, 7, 44–50. [Google Scholar]
- Suliga, E. Zachowania zdrowotne związane z żywieniem osób dorosłych i starszych. Hygeia Public Health 2010, 45, 44–48. [Google Scholar]
- Dymarska, E.; Janczar-Smuga, M. Water as an Essential Nutrient in the Diet of the Elderly. Prace Naukowe Uniwersytetu Ekonomicznego We Wrocławiu. 2016. No. 461. Available online: https://dbc.wroc.pl/Content/36606/PDF/Dymarska_Woda_Jako_Niezbedny_Skladnik_Pokarmowy_w_Zywieniu_2016.pdf (accessed on 10 March 2025).
- Barrio-Cortes, J.; Castaño-Reguillo, A.; Beca-Martínez, M.T.; Bandeira-de Oliveira, M.; López-Rodríguez, C.; Jaime-Sisó, M.Á. Chronic diseases in the geriatric population: Morbidity and use of primary care services according to risk level. BMC Geriatr. 2021, 21, 278. [Google Scholar] [CrossRef]
- WHO. World Health Statistics 2024. Available online: https://iris.who.int/bitstream/handle/10665/376869/9789240094703-eng.pdf?sequence=1 (accessed on 10 March 2025).
- Chen, Z.; Klimentidis, Y.C.; Bea, J.W.; Ernst, K.C.; Hu, C.; Jackson, R.; Thomson, C.A. Body mass index, waist circumference, and mortality in a large multiethnic postmenopausal cohort—Results from the Women’s Health Initiative. J. Am. Geriatr. Soc. 2017, 65, 1907–1915. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.B. Weight and body mass index in old age: Do they still matter? J. Am. Geriatr. Soc. 2017, 65, 1898. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.D.; Chen, Q.F.; Yang, W.; Zuluaga, M.; Targher, G.; Byrne, C.D.; Valenti, L.; Luo, F.; Katsouras, C.S.; Thaher, O.; et al. Burden of disease attributable to high body mass index: An analysis of data from the Global Burden of Disease Study 2021. EClinicalMedicine 2024, 76, 102848. [Google Scholar] [CrossRef] [PubMed]
- Wnęk, D. Otyłość–Przyczyny i Konsekwencje, Medycyna Praktyczna. Available online: https://www.mp.pl/pacjent/dieta/odchudzanie/wprowadzenie/290855,otylosc-przyczyny-i-konsekwencje (accessed on 10 March 2025).
- Malczyk, E.; Malczyk, A.; Misiarz, M.; Kwapisz, A. Ocena jakości diety osób dorosłych aktywnych zawodowo za pomocą indeksu ogólnej jakości diety (DQI). Med. Ogólna I Nauk. O Zdrowiu 2024, 30, 240–246. [Google Scholar] [CrossRef]
- Mursu, J.; Steffen, L.M.; Meyer, K.A.; Duprez, D.; Jacobs, D.R., Jr. Diet quality indexes and mortality in postmenopausal women: The Iowa Women’s Health Study. Am. J. Clin. Nutr. 2013, 98, 444–453. [Google Scholar] [CrossRef]
- Kolarzyk, E.; Kwiatkowski, J.; Skop-Lewandowska, A. Assessment of diet quality among occupationally active adults using the Diet Quality Index (DQI). Med. Ogólna Nauk. Zdrowiu 2024, 30, 240–246. [Google Scholar]
- Gacek, M. Zachowania żywieniowe słuchaczek uniwersytetu trzeciego wieku ze środowiska krakowskiego–wybrane uwarunkowania. Med. Ogólna I Nauk. O Zdrowiu 2018, 24, 257. [Google Scholar] [CrossRef]
- Augustowski, K.; Augustyński, K. Świadomość Osób Starszych na Teamt Właściwego Odżywiania. Available online: https://www.augustowscy-dietetycy.pl/wp-content/uploads/2015/09/%C5%9AWIADOMO%C5%9A%C4%86-OS%C3%93B-STARSZYCH-NA-TEMAT.pdf (accessed on 10 March 2025).
- Greenlaw, C.L. Describing Nutrition Education Needs of Older Adults at Congregate Meal Sites and Community Settings. Master’s Thesis, Cornell University, Ithaca, NY, USA, 2018. [Google Scholar]
- Sandri, E.; Amigo-Bravo, M.; Werner, L.U. Influence of health education on nutrition and lifestyle habits in the Spanish population: A descriptive cross-sectional study. Int. J. Vitam. Nutr. Res. 2025, 95, 28112. [Google Scholar] [CrossRef]
- Morony, S.; Lamph, E.; Muscat, D.; Nutbeam, D.; Dhillon, H.M.; Shepherd, H.; McCaffery, K.J. Improving health literacy through adult basic education in Australia. Health Promot. Int. 2018, 33, 867–877. [Google Scholar] [CrossRef]
- Nakamura, S.; Inayama, T.; Harada, K.; Arao, T. Reduction in vegetable intake disparities with a web-based nutrition education intervention among lower-income adults in Japan: Randomized controlled trial. J. Med. Internet Res. 2017, 19, e377. [Google Scholar] [CrossRef]
- Kim, S.Y.; Jeon, S.W.; Lee, M.Y.; Shin, D.W.; Lim, W.J.; Shin, Y.C.; Oh, K.S. The association between physical activity and anxiety symptoms for general adult populations: An analysis of the dose-response relationship. Psychiatry Investig. 2019, 17, 29–34. [Google Scholar] [CrossRef] [PubMed]
- González-Padilla, E.A.; Dias, J.; Ramne, S.; Olsson, K.; Nälsén, C.; Sonestedt, E. Association between added sugar intake and micronutrient dilution: A cross-sectional study in two adult Swedish populations. Nutr. Metab. 2020, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.U.; Lee, E.H.; Hwang, S.T.; Hong, S.H.; Kim, J.H. The Beck Depression Inventory: Psychometric properties in Korean adult populations. Korean J. Clin. Psychol. 2019, 38, 300–307. [Google Scholar] [CrossRef]
- Tanaka, H.; Katanoda, K.; Togawa, K.; Kobayashi, Y. Educational inequalities in all-cause and cause-specific mortality in Japan: National census-linked mortality data for 2010–15. Int. J. Epidemiol. 2024, 53, dyae031. [Google Scholar] [CrossRef]
- Paulionis, L. The changing face of food and nutrition in Canada and the United States: Opportunities and challenges for older adults. J. Nutr. Elder. 2008, 27, 277–295. [Google Scholar] [CrossRef]




| Profile Number | Type of Indicator | Quality Profiles | Participation of Participants (N = 151) | |
|---|---|---|---|---|
| N | % | |||
| 1 | Low pHDI-10 and low nHDI-14 | L-QI † | 90 | 60 |
| 2 | Moderate pHDI-10 and low nHDI-14 | M-QI †† | 45 | 30 |
| 3 | High pHDI-10 and low nHDI-14 | H-QI ††† | 16 | 11 |
| Characteristics | N = 151 | |
|---|---|---|
| Gender | Female | 91 |
| Male | 60 | |
| Age | <60 | 0 |
| 60–65 | 82 | |
| 66–70 | 40 | |
| 71–80 | 23 | |
| >80 | 6 | |
| Place of residence | Village | 23 |
| Small town | 41 | |
| City | 87 | |
| Residential status | Live alone | 35 |
| Live with a partner | 56 | |
| Live with children | 24 | |
| Multigenerational family | 24 | |
| Care institution | 12 | |
| Employment activity | Yes | 57 |
| No | 94 | |
| Marital status | Single | 15 |
| In a relationship | 83 | |
| Widowed | 49 | |
| Other | 4 | |
| Education | Primary | 3 |
| Vocational | 12 | |
| Secondary | 60 | |
| High | 76 | |
| Body mass index (kg/m2) | <23.0 | 9 |
| 23.0–29.9 | 86 | |
| ≥30.0 | 60 | |
| Characteristics | Profile of Diet Quality Index | p | Cramér’s V | ||||||
|---|---|---|---|---|---|---|---|---|---|
| L-QI a | M-QI b | H-QI c | |||||||
| N = 90 | 60% | N = 45 | 30% | N = 16 | 11% | ||||
| Gender | Female ab,bc,ac | 59 | 39 | 30 | 20 | 14 | 9 | 0.213 | 0.085 |
| Male ab,bc,ac | 31 | 21 | 15 | 10 | 2 | 1 | |||
| Age | 60–65 ab,bc,ac | 25 | 17 | 45 | 30 | 12 | 8 | <0.0001 | 0.451 |
| 66–70 ab,bc,ac | 38 | 25 | 0 | 0 | 2 | 1 | |||
| 71–80 ab,bc,ac | 21 | 14 | 0 | 0 | 2 | 1 | |||
| >80 ab,bc,ac | 6 | 4 | 0 | 0 | 0 | 0 | |||
| Place of residence | Village ab,bc,ac | 13 | 9 | 0 | 0 | 10 | 7 | <0.0001 | 0.409 |
| Small town ab,bc,ac | 30 | 20 | 5 | 3 | 6 | 4 | |||
| City ab,bc,ac | 47 | 31 | 40 | 26 | 0 | 0 | |||
| Residential status | Live alone ab,bc,ac | 35 | 23 | 0 | 0 | 0 | 0 | <0.0001 | 0.411 |
| Live with A partner ab,bc,ac | 40 | 26 | 10 | 7 | 6 | 4 | |||
| Live with children ab,bc,ac | 5 | 3 | 9 | 6 | 10 | 7 | |||
| Multigenerational family ab,bc,ac | 18 | 12 | 6 | 4 | 0 | 0 | |||
| Care institution ab,bc,ac | 12 | 8 | 0 | 0 | 0 | 0 | |||
| Employment activity | Yes ab,bc,ac | 48 | 32 | 9 | 6 | 0 | 0 | <0.0001 | 0.392 |
| No ab,bc,ac | 42 | 28 | 36 | 24 | 16 | 11 | |||
| Marital status | Single ab,bc,ac | 14 | 9 | 1 | 1 | 0 | 0 | 0.017 | 0.177 |
| In a relationship ab,bc,ac | 49 | 32 | 22 | 15 | 12 | 8 | |||
| Widowed ab,bc,ac | 24 | 16 | 21 | 14 | 4 | 3 | |||
| Other ab,bc,ac | 4 | 3 | 0 | 0 | 0 | 0 | |||
| Education | Primary ab,bc,ac | 3 | 2 | 0 | 0 | 0 | 0 | <0.0001 | 0.474 |
| Vocational ab,bc,ac | 10 | 7 | 2 | 1 | 0 | 0 | |||
| Secondary ab,bc,ac | 57 | 38 | 0 | 0 | 3 | 2 | |||
| High ab,bc,ac | 20 | 13 | 43 | 28 | 13 | 9 | |||
| BMI (kg/m2) | <23.0 ab,bc,ac | 3 | 2 | 6 | 4 | 0 | 0 | 0.0005 | 0229 |
| 23.0–29.9 ab,bc,ac | 50 | 33 | 20 | 13 | 16 | 11 | |||
| ≥30.0 ab,bc,ac | 41 | 27 | 19 | 13 | 0 | 0 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szreiter, A.; Lachowicz-Wiśniewska, S. Nutrition Education Among Community-Dwelling Polish Seniors—A Pilot Study of Diet Quality, Health Status, and Public Health Interventions. Nutrients 2025, 17, 2103. https://doi.org/10.3390/nu17132103
Szreiter A, Lachowicz-Wiśniewska S. Nutrition Education Among Community-Dwelling Polish Seniors—A Pilot Study of Diet Quality, Health Status, and Public Health Interventions. Nutrients. 2025; 17(13):2103. https://doi.org/10.3390/nu17132103
Chicago/Turabian StyleSzreiter, Anna, and Sabina Lachowicz-Wiśniewska. 2025. "Nutrition Education Among Community-Dwelling Polish Seniors—A Pilot Study of Diet Quality, Health Status, and Public Health Interventions" Nutrients 17, no. 13: 2103. https://doi.org/10.3390/nu17132103
APA StyleSzreiter, A., & Lachowicz-Wiśniewska, S. (2025). Nutrition Education Among Community-Dwelling Polish Seniors—A Pilot Study of Diet Quality, Health Status, and Public Health Interventions. Nutrients, 17(13), 2103. https://doi.org/10.3390/nu17132103









