Social Factors, Dietary Intake and the Nutritional Status of Community-Dwelling Chinese Older Adults: A Scoping Review
Abstract
1. Introduction
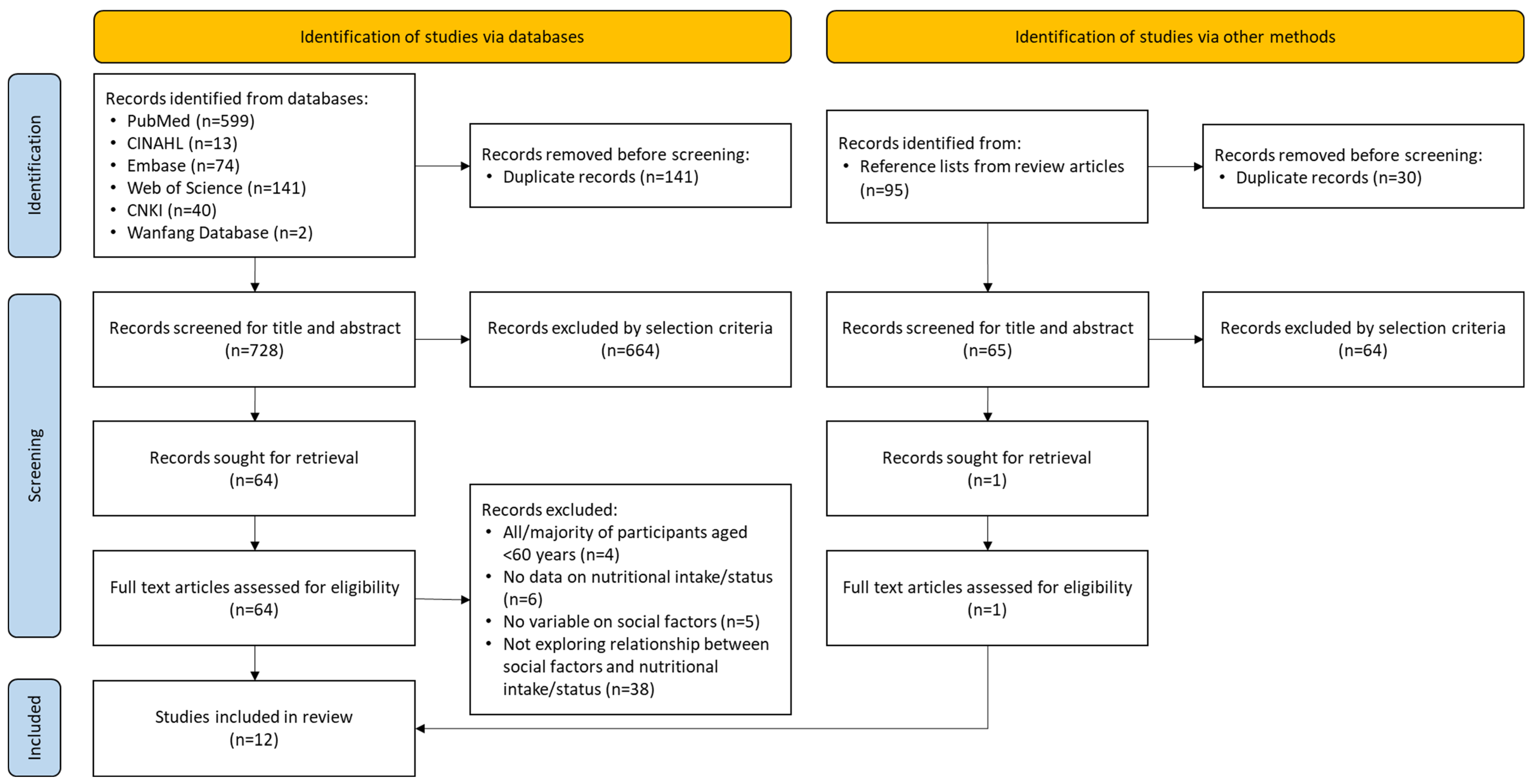
2. Methods
- What are the social factors relating to dietary intake or nutritional status among community-dwelling Chinese older adults?
- How do the social factors relate to dietary intake or nutritional status among community-dwelling Chinese older adults?
3. Results
3.1. Characteristics of the Studies
3.2. Measures Used in the Included Studies
3.3. Quality of the Studies
3.4. Relationships Between Social Factors and Dietary Intake/Nutritional Status
3.4.1. Marital Status
3.4.2. Living Arrangement
3.4.3. Eating Arrangement
3.4.4. Loneliness, Low Social Support, and Social Isolation
3.4.5. Social Frailty
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MNA | Mini Nutritional Assessment |
| AA | Anorexia of ageing |
| BMI | Body mass index |
| DDS | Diet Diversity Score |
| DETERMINE | Disease, Eating poorly, Tooth loss/mouth pain, Economic hardship, Reduced social contact, Multiple medicines, Involuntary weight loss/gain, Needs assistance in self-care, Elder years above age 80 |
| ESPEN | European Society of Parenteral and Enteral Nutrition and Metabolism |
| FFQ | Food Frequency Questionnaire |
| OR | Odds ratio |
| WC | Waist circumference |
References
- Holmes, S. Barriers to effective nutritional care for older adults. Nurs. Stand. 2006, 21, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in older adults—Recent advances and remaining challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef] [PubMed]
- McTigue, K.M.; Hess, R.; Ziouras, J. Obesity in older adults: A systematic review of the evidence for diagnosis and treatment. Obesity 2006, 14, 1485–1497. [Google Scholar] [CrossRef] [PubMed]
- Guigoz, Y.; Vellas, B. Nutritional assessment in older adults: MNA® 25 years of a screening tool & a reference standard for care and research; what next? J. Nutr. Health Aging 2021, 25, 528–583. [Google Scholar] [CrossRef]
- Khaleghi, A.A.; Salari, N.; Darvishi, N.; Bokaee, S.; Jafari, S.; Hemmati, M.; Mohammadi, M. Global prevalence of obesity in the older adults: A meta-analysis. Public Health Pract. 2025, 9, 100585. [Google Scholar] [CrossRef]
- Payette, H.; Gray-Donald, K.; Cyr, R.; Boutier, V. Predictors of dietary intake in a functionally dependent elderly population in the community. Am. J. Public Health 1995, 85, 677–683. [Google Scholar] [CrossRef]
- Volkert, D. Malnutrition in the elderly—Prevalence, causes and corrective strategies. Clin. Nutr. 2002, 21, 110–112. [Google Scholar] [CrossRef]
- Agarwal, E.; Miller, M.; Yaxley, A.; Isenring, E. Malnutrition in the elderly: A narrative review. Maturitas 2013, 76, 296–302. [Google Scholar] [CrossRef]
- Walker-Clarke, A.; Walase, L.; Meye, C. Psychosocial factors influencing the eating behaviours of older adults: A systematic review. Ageing Res. Rev. 2022, 77, 101597. [Google Scholar] [CrossRef]
- Besora-Moreno, M.; Llauradó, E.; Tarro, L.; Solà, R. Social and economic factors and malnutrition or the risk of malnutrition in the elderly: A systematic review and meta-analysis of observational studies. Nutrients 2020, 12, 737. [Google Scholar] [CrossRef]
- Poggiogalle, E.; Kiesswetter, E.; Romano, M.; Saba, A.; Sinesio, F.; Polito, A.; Moneta, E.; Ciarapica, D.; Migliaccio, S.; Suwalska, A. Psychosocial and cultural determinants of dietary intake in community-dwelling older adults: A Determinants of Diet and Physical Activity systematic literature review. Nutrition 2021, 85, 111131. [Google Scholar] [CrossRef] [PubMed]
- Wild, H.; Baek, Y.; Shah, S.; Gasevic, D.; Owen, A. The socioecological correlates of meal skipping in community-dwelling older adults: A systematic review. Nutr. Rev. 2022, 81, 168–179. [Google Scholar] [CrossRef] [PubMed]
- Beller, J.; Wagner, A. Loneliness and Health: The Moderating Effect of Cross-Cultural Individualism/Collectivism. J. Aging Health 2020, 32, 1516–1527. [Google Scholar] [CrossRef] [PubMed]
- Fischler, C. Commensality, society and culture. Soc. Sci. Inf. 2011, 50, 528–548. [Google Scholar] [CrossRef]
- Bildtgard, T. What It Means to “Eat Well” in France and Sweden. Food Foodways 2010, 18, 209–232. [Google Scholar] [CrossRef]
- Björnwall, A.; Mattsson Sydner, Y.; Koochek, A.; Neuman, N. Perceptions and experiences of eating alone among community-living retired Swedes: Loss, routine and independence. Appetite 2023, 186, 106570. [Google Scholar] [CrossRef]
- Renzaho, A.M.; Burns, C. Post-migration food habits of sub-Saharan African migrants in Victoria: A cross-sectional study. Nutr. Diet. 2006, 63, 91–102. [Google Scholar] [CrossRef]
- Phull, S.; Wills, W.; Dickinson, A. Is it a pleasure to eat together? Theoretical reflections on conviviality and the Mediterranean diet. Sociol. Compass 2015, 9, 977–986. [Google Scholar] [CrossRef]
- Yiengprugsawan, V.; Banwell, C.; Takeda, W.; Dixon, J.; Seubsman, S.-a.; Sleigh, A.C. Health, happiness and eating together: What can a large Thai cohort study tell us? Glob. J. Health Sci. 2015, 7, 270. [Google Scholar] [CrossRef]
- Cho, W.; Takeda, W.; Oh, Y.; Aiba, N.; Lee, Y. Perceptions and practices of commensality and solo-eating among Korean and Japanese university students: A cross-cultural analysis. Nutr. Res. Pract. 2015, 9, 523–529. [Google Scholar] [CrossRef]
- Ma, G. Food, eating behavior, and culture in Chinese society. J. Ethn. Foods 2015, 2, 195–199. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Aromataris, E.; Munn, Z. JBI Manual for Evidence Synthesis. Available online: https://synthesismanual.jbi.global (accessed on 7 April 2023).
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Systematic reviews of etiology and risk. In JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2020. [Google Scholar]
- Bian, D.; Li, X.; Xiao, Y.; Song, K.; Wang, L.; Shen, J.; Aimaiti, M.; Ma, X.; Shi, C.; Li, G. Relationship between social support, sarcopenia, and cognitive impairment in chinese community-dwelling older adults. J. Nutr. Health Aging 2023, 27, 726–733. [Google Scholar] [CrossRef]
- Cui, G.H.; Zhang, S.K.; Zhang, X.C.; Li, S.J. Development and validation of a nomogram for predicting anorexia of aging in older people. Appetite 2024, 201, 107606. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Li, S.; Zheng, Y. Predictors of nutritional status among community-dwelling older adults in Wuhan, China. Public Health Nutr. 2009, 12, 1189–1196. [Google Scholar] [CrossRef]
- Li, Y.X.; Xiang, Q.; Song, Q.H.; Liang, R.; Deng, L.H.; Dong, B.R.; Yue, J.R. Longitudinal associations between social support and sarcopenia: Findings from a 5-year cohort study in Chinese aged ≥50 years. J. Nutr. Health Aging 2024, 28, 100014. [Google Scholar] [CrossRef]
- Song, X.; Zhang, W.; Hallensleben, C.; Versluis, A.; van der Kleij, R.; Jiang, Z.; Chavannes, N.H.; Gobbens, R.J.J. Associations between obesity and multidimensional frailty in older Chinese people with hypertension. Clin. Interv. Aging 2020, 15, 811–820. [Google Scholar] [CrossRef]
- Tang, H.; Xu, H.; Guo, Q.; Hu, Y.; Han, Y.; Ding, K.; Wen, X. Risk assessment and influencing factors of malnutrition among community-dwelling older adults in Minhang District of Shanghai. J. Environ. Occup. Med. 2023, 40, 1068–1073. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, T.; Yuan, B.; Han, B. Association between physical and mental health of urban elderly women without social security. Chin. J. Gerontol. 2013, 12, 2858–2861. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, C.; Luan, W. Social isolation, depression, nutritional status and quality of life during COVID-19 among Chinese community-dwelling older adults: A cross-sectional study. BMJ Open 2023, 13, e072305. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.-M.; Li, S.; Claytor, L.; Partridge, J.; Goates, S. Prevalence and predictors of malnutrition in elderly Chinese adults: Results from the China Health and Retirement Longitudinal Study. Public Health Nutr. 2018, 21, 3129–3134. [Google Scholar] [CrossRef] [PubMed]
- Pek, K.; Chew, J.; Lim, J.P.; Yew, S.; Tan, C.N.; Yeo, A.; Ding, Y.Y.; Lim, W.S. Social Frailty Is Independently Associated with Mood, Nutrition, Physical Performance, and Physical Activity: Insights from a Theory-Guided Approach. Int. J. Environ. Res. Public Health 2020, 17, 4239. [Google Scholar] [CrossRef]
- Yap, K.B.; Niti, M.; Ng, T.P. Nutrition screening among community-dwelling older adults in Singapore. Singap. Med. J. 2007, 48, 911–916. [Google Scholar]
- Huang, Y.-C.; Cheng, H.-L.; Wahlqvist, M.L.; Lo, Y.-T.C.; Lee, M.-S. Gender differences in longevity in free-living older adults who eat-with-others: A prospective study in Taiwan. BMJ Open 2017, 7, e016575. [Google Scholar] [CrossRef]
- Bunt, S.; Steverink, N.; Olthof, J.; Van Der Schans, C.; Hobbelen, J. Social frailty in older adults: A scoping review. Eur. J. Ageing 2017, 14, 323–334. [Google Scholar] [CrossRef]
- Björnwall, A.; Mattsson Sydner, Y.; Koochek, A.; Neuman, N. Eating Alone or Together among Community-Living Older People—A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 3495. [Google Scholar] [CrossRef]
- McAlpine, S.; Harper, J.; McMurdo, M.; Bolton-Smith, C.; Hetherington, M. Nutritional supplementation in older adults: Pleasantness, preference and selection of sip-feeds. Br. J. Health Psychol. 2003, 8, 57–66. [Google Scholar] [CrossRef]
- Nakata, R.; Kawai, N. The “social” facilitation of eating without the presence of others: Self-reflection on eating makes food taste better and people eat more. Physiol. Behav. 2017, 179, 23–29. [Google Scholar] [CrossRef]
- McHugh Power, J.E.; Lee, O.; Aspell, N.; McCormack, E.; Loftus, M.; Connolly, L.; Lawlor, B.; Brennan, S. RelAte: Pilot study of the effects of a mealtime intervention on social cognitive factors and energy intake among older adults living alone. Br. J. Nutr. 2016, 116, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Veazie, S.; Gilbert, J.; Winchell, K.; Paynter, R.; Guise, J.-M. Addressing Social Isolation to Improve the Health of Older Adults: A Rapid Review; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2019.
- Cattan, M.; White, M.; Bond, J.; Learmouth, A. Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing Soc. 2005, 25, 41–67. [Google Scholar] [CrossRef]
- Xiao, S. The theoretical basis and research application of the Social Support Rating Scale. J. Clin. Psychiatry 1994, 4, 98–100. [Google Scholar]
- Bessa, B.; Ribeiro, O.; Coelho, T. Assessing the social dimension of frailty in old age: A systematic review. Arch. Gerontol. Geriatr. 2018, 78, 101–113. [Google Scholar] [CrossRef]
- Kuroda, A.; Tanaka, T.; Hirano, H.; Ohara, Y.; Kikutani, T.; Furuya, H.; Obuchi, S.P.; Kawai, H.; Ishii, S.; Akishita, M. Eating alone as social disengagement is strongly associated with depressive symptoms in Japanese community-dwelling older adults. J. Am. Med. Dir. Assoc. 2015, 16, 578–585. [Google Scholar] [CrossRef]
- Sahyoun, N.R.; Pratt, C.A.; Anderson, A. Evaluation of nutrition education interventions for older adults: A proposed framework. J. Am. Diet. Assoc. 2004, 104, 58–69. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Q.; Cohen, N.L.; Marra, M.V.; Woolf, K.; Gilbride, J.; Francis, S.L. Community priorities for healthy eating in older adults. J. Nutr. Gerontol. Geriatr. 2017, 36, 75–91. [Google Scholar] [CrossRef]
- Walton, K.; do Rosario, V.A.; Pettingill, H.; Cassimatis, E.; Charlton, K. The impact of home-delivered meal services on the nutritional intake of community living older adults: A systematic literature review. J. Hum. Nutr. Diet. 2020, 33, 38–47. [Google Scholar] [CrossRef]
- You, J.; Fung, H.; Vitaliano, P. The pattern of social support seeking and its socio-demographic variations among older adults in China. Eur. J. Ageing 2020, 17, 341–348. [Google Scholar] [CrossRef]
- Boulton, E.; Kneale, D.; Stansfield, C.; Heron, P.N.; Sutcliffe, K.; Hayanga, B.; Hall, A.; Bower, P.; Casey, D.; Craig, D. Rapid systematic review of systematic reviews: What befriending, social support and low intensity psychosocial interventions, delivered remotely, may reduce social isolation and loneliness among older adults and how? F1000Research 2021, 9, 1368. [Google Scholar] [CrossRef]
- Lai, D.W.; Li, J.; Ou, X.; Li, C.Y. Effectiveness of a peer-based intervention on loneliness and social isolation of older Chinese immigrants in Canada: A randomized controlled trial. BMC Geriatr. 2020, 20, 356. [Google Scholar] [CrossRef] [PubMed]

| Population | Social Factors | Dietary Intake/Nutritional Status | ||
|---|---|---|---|---|
| Community-dwelling Independent living Free-living | Chinese | Aged Old* Elder* Senior* Geriatric* | Social factors Social interaction Social isolation Social support Home environment Loneliness Alone Friends Companion* Commensal* | Nutritional status Malnutrition Undernutrition Nutrition* Diet* Eating Body weight Body Mass Index Body mass BMI Food Meals |
| Reference | Origin | Aims | Study Design | Population | Measures of Dietary Intake/Nutritional Status | Measures of Social Factors | Key Findings Related to Nutritional Status and Social Factors |
|---|---|---|---|---|---|---|---|
| Bian et al. (2023) [27] | China | To explore the correlation between social support, sarcopenia, and cognitive impairment in Chinese older adults | Cross-sectional | 720 Chinese community-dwelling older adults aged ≥65 years | Sarcopenia | Social Support Rate Scale | There was a negative association between older adults with higher levels of social support and sarcopenia. |
| Cui et al. (2024) [28] | China | To develop a nomogram for predicting the risk of AA among older people | Cross-sectional | 2144 community-dwelling older adults aged ≥60 years in Jinan city | Simplified Nutritional Appetite Questionnaire | UCLA Loneliness Scale, living arrangement | Lonely older adults were more likely to have AA than non-lonely older adults (OR = 1.930). Older adults living alone were more likely to have AA than those who were not living alone (OR = 1.649). |
| Han et al. (2009) [29] | China | To examine the levels of nutritional and functional status; to identify the relationships between nutrition, demographic characteristics, and functional status; and to explore the predictors contributing to poor nutrition for older adults | Cross-sectional | 162 community-dwelling older adults aged ≥65 years in Wuhan | MNA | Marital status, living arrangement | Widowed participants were more likely to suffer from poor nutrition. Living arrangement was not associated with nutritional status. |
| Huang et al. (2017) [38] | Taiwan | To evaluate whether daily frequency of eating with others is associated with all-cause mortality | Cohort study | 1984 free-living Taiwanese older men and women aged ≥65 | BMI, FFQ, DDS (calculated from a 24-h recall) | Eating arrangement | Female participants who did not eat with others had the lowest BMI. Male participants who ate only once daily with others had the lowest DDS. Female participants who did not eat with others had the lowest DDS. Male participants who did not eat with others ate the most meat and the least vegetables. Female participants who did not eat with others ate the least meat, least seafood, fewest eggs, and least vegetables. |
| Li et al. (2024) [30] | China | To investigate longitudinal associations between overall social support and its sub domains with the risk of sarcopenia | Cohort study | 1905 community-dwelling adults aged ≥50 years in west China | Sarcopenia | Social Support Rating Scale | Participants with higher scores for overall social support, subjective support, and support utilization at baseline were less likely to develop sarcopenia during the 5-year follow up (adjusted OR = 0.87, 0.88, and 0.87, respectively). |
| Pek et al. (2020) [36] | Singapore | To understand the impact of social frailty on pertinent outcomes | Cross-sectional | 229 community-dwelling adults aged ≥50 years (mean age 67.22; 92.6% Chinese) | MNA, serum albumin level | Social frailty | Socially frail participants had the lowest MNA scores. Socially pre-frail participants had the lowest serum albumin level. Socially frail participants were more likely to have poor nutritional status (adjusted OR = 8.35). |
| Song et al. (2020) [31] | China | To investigate the prevalence of multidimensional frailty, and to explore the relationship of general and abdominal obesity to multidimensional frailty in community-dwelling older people with hypertension | Cross-sectional | 995 community-dwelling Chinese older people with hypertension aged ≥65 years | Consumption of breakfast, BMI, WC | Social frailty | Participants who did not have breakfast scored higher in social frailty. Overweight or obese participants scored higher in social frailty. Centrally obese participants scored higher in social frailty. |
| Tang et al. (2023) [32] | China | To evaluate the risk of malnutrition among the community-dwelling elderly and explore its influencing factors | Cross-sectional | 950 seniors aged ≥65 years in Shanghai | Risk Assessment of Malnutrition in the Elderly | Marital status, living arrangement | Unmarried seniors were more likely to have malnutrition (OR = 1.755). Seniors living alone were more likely to have malnutrition (OR = 2.28). |
| Wang et al. (2013) [33] | China | To understand the physical and psychological health of older adults without social insurance, and to analyze their correlation and the factors affecting them | Cross-sectional | 243 community-dwelling females aged ≥60 and over without social insurance in Beijing | BMI, WC | UCLA Loneliness Scale | Higher BMI was associated with lower loneliness (no participants were underweight). |
| Wang et al. (2023) [34] | China | To investigate the relationship between social isolation, depression, nutritional status, and quality of life among community-dwelling older adults during COVID-19 | Cross-sectional | 406 community-dwelling older adults aged ≥ in Shanghai | Risk Assessment of Malnutrition in the Elderly | Lubben Social Network Scale | Social isolation was weakly associated with malnutrition risk (r = 0.14). |
| Wei et al. (2018) [35] | China | To provide a nationally representative estimate of the prevalence of malnutrition in elderly Chinese adults and to determine predictors of malnutrition in this population | Cross-sectional | 6394 community-dwelling Chinese adults aged ≥ 0 years | ESPEN definition of malnutrition (BMI, weight loss) | Marital status | Married participants were less likely to be malnourished (OR = 0.54). |
| Yap et al. (2007) [37] | Singapore | To describe the responses to the DETERMINE checklist and the nutritional risk level of community-dwelling older Chinese in Singapore | Cross-sectional | 2605 community-dwelling older Chinese aged ≥55 years (mean age 66.0) | DETERMINE (nutritional risk) | Marital status, living arrangement | Single/divorced/widowed participants were more likely to be at a higher nutritional risk (adjusted OR = 1.46). Participants who lived alone were more likely to be at a higher nutritional risk (adjusted OR = 2.05). |
| Study | Risk of Bias Domains * | % Yes | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| Bian 2023 [27] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Cui 2024 [28] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Han 2009 [29] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Pek 2020 [36] | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | 87.5 |
| Song 2020 [31] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Tang 2023 [32] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Wang 2013 [33] | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 87.5 |
| Wang 2023 [34] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Wei 2018 [35] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Yap 2007 [37] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Study | Risk of Bias Domains * | % Yes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| Huang 2017 [38] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | 100 |
| Li 2024 [30] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| No Significant Associations | Associated with Poor Dietary Intake/Nutritional Status | |
|---|---|---|
| Single * | [29,35,37] | |
| Living alone | [29] | [28,32,37] |
| Eating alone | [38] | |
| Loneliness/low social support/social isolation | [27,28,30,33,34] | |
| Social frailty | [31,36] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsang, J.P.Y.; Cheung, D.S.K.; Liu, J.Y.W. Social Factors, Dietary Intake and the Nutritional Status of Community-Dwelling Chinese Older Adults: A Scoping Review. Nutrients 2025, 17, 2019. https://doi.org/10.3390/nu17122019
Tsang JPY, Cheung DSK, Liu JYW. Social Factors, Dietary Intake and the Nutritional Status of Community-Dwelling Chinese Older Adults: A Scoping Review. Nutrients. 2025; 17(12):2019. https://doi.org/10.3390/nu17122019
Chicago/Turabian StyleTsang, Joyce P. Y., Daphne S. K. Cheung, and Justina Y. W. Liu. 2025. "Social Factors, Dietary Intake and the Nutritional Status of Community-Dwelling Chinese Older Adults: A Scoping Review" Nutrients 17, no. 12: 2019. https://doi.org/10.3390/nu17122019
APA StyleTsang, J. P. Y., Cheung, D. S. K., & Liu, J. Y. W. (2025). Social Factors, Dietary Intake and the Nutritional Status of Community-Dwelling Chinese Older Adults: A Scoping Review. Nutrients, 17(12), 2019. https://doi.org/10.3390/nu17122019







