C-Reactive Protein to Albumin Ratio Predicts Early Mortality in Hospitalized Older Patients, Independent of the Admission Diagnosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Methods
2.3. Statistics
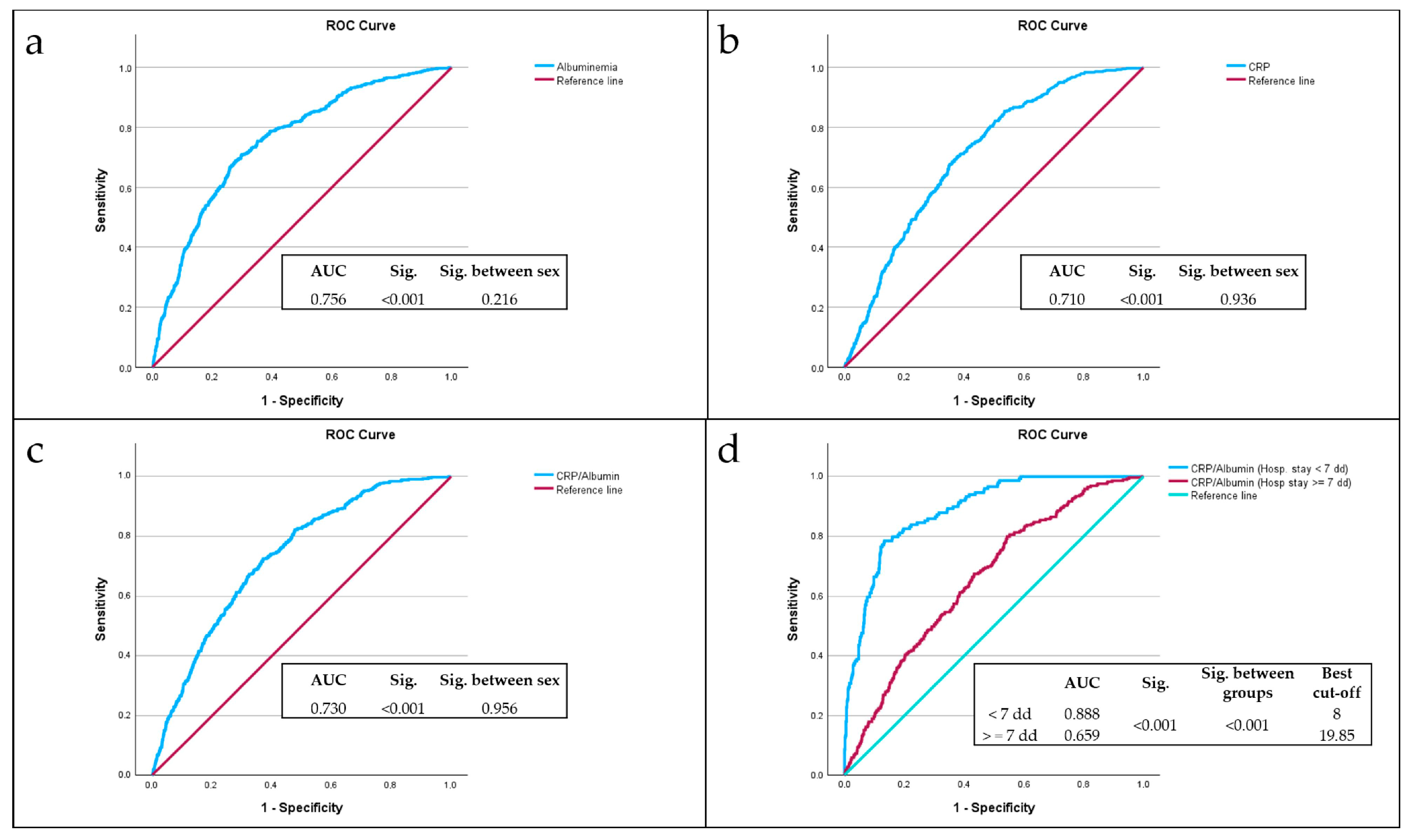
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 6 May 2025).
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cereda, E.; Cruz-Jentoft, A.; Goisser, S.; de Groot, L.; Großhauser, F.; Kiesswetter, E.; Norman, K.; et al. Management of Malnutrition in Older Patients—Current Approaches, Evidence and Open Questions. J. Clin. Med. 2019, 8, 974. [Google Scholar] [CrossRef] [PubMed]
- Sanson, G.; Bertocchi, L.; Dal Bo, E.; Di Pasquale, C.L.; Zanetti, M. Identifying reliable predictors of protein-energy malnutrition in hospitalized frail older adults: A prospective longitudinal study. Int. J. Nurs. Stud. 2018, 82, 40–48. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Walston, J.; Hadley, E.C.; Ferrucci, L.; Guralnik, J.M.; Newman, A.B.; Studenski, S.A.; Ershler, W.B.; Harris, T.; Fried, L.P. Research agenda for frailty in older adults: Toward a better understanding of physiology and etiology: Summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 991–1001. [Google Scholar] [CrossRef]
- Eeles, E.M.; White, S.V.; O’Mahony, S.M.; Bayer, A.J.; Hubbard, R.E. The impact of frailty and delirium on mortality in older inpatients. Age Ageing 2012, 41, 412–416. [Google Scholar] [CrossRef]
- Garagnani, P.; Capri, M.; Salvioli, S.; Santoro, A.; Morsiani, C.; Franceschi, C.; Monti, D.; Conte, M.; Grignolio, A. The Continuum of aging and age-related diseases: Common mechanisms but different rates. Front. Med. 2018, 5, 61. [Google Scholar]
- Pisano, C.; Polisano, D.; Balistreri, C.R.; Altieri, C.; Nardi, P.; Bertoldo, F.; Trombetti, D.; Asta, L.; Ferrante, M.S.; Buioni, D.; et al. Role of cachexia and fragility in the patient candidate for cardiac surgery. Nutrients 2021, 13, 517. [Google Scholar] [CrossRef]
- Petermann-Rocha, F.; Pell, J.P.; Celis-Morales, C.; Ho, F.K. Frailty, sarcopenia, cachexia and malnutrition as comorbid conditions and their associations with mortality: A prospective study from UK Biobank. J. Public Health 2022, 44, e172–e180. [Google Scholar] [CrossRef]
- Slee, A.; Birch, D.; Stokoe, D. The relationship between malnutrition risk and clinical outcomes in a cohort of frail older hospital patients. Clin. Nutr. ESPEN 2016, 15, 57–62. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 6 May 2025).
- Lee, S.B.; Oh, J.H.; Park, J.H.; Choi, S.P.; Wee, J.H. Differences in youngest-old, middle-old, and oldest-old patients who visit the emergency department. Clin. Exp. Emerg. Med. 2018, 5, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Guigoz, Y. The mini nutritional assessment (MNA) review of the literature e what does it tell us? J. Nutr. Health Aging 2006, 10, 466–485. [Google Scholar]
- Wolf, C.; Jauch, K.-W.; Bischoff, S.C.; Lochs, H.; Weimann, A.; Schindler, K.; Frieling, T.; Bolder, U.; Schütz, T.; Pirlich, M.; et al. The German hospital malnutrition study. Clin. Nutr. 2006, 25, 563–572. [Google Scholar]
- Banks, M.; Ash, S.; Bauer, J.; Gaskill, D. Prevalence of malnutrition in adults in Queensland public hospitals and residential aged care facilities. Nutr. Diet. 2007, 64, 172–178. [Google Scholar] [CrossRef]
- Kondrup, J.; Sorensen, J.M. The magnitude of the problem of malnutrition in Europe. Nestle Nutr. Workshop Ser. Clin. Perform. Program 2009, 12, 1–14. [Google Scholar]
- Waitzberg, D.L.; Caiaffa, W.T.; Correia, M.I.T.D. Hospital malnutrition: The Brazilian national survey (IBRANUTRI): A study of 4000 patients. Nutrition 2001, 17, 573–580. [Google Scholar] [CrossRef]
- Aghdassi, E.; McArthur, M.; Liu, B.; McGeer, A.; Simor, A.; Allard, J.P. Dietary intake of elderly living in Toronto long-term care facilities: Comparison to the dietary reference intake. Rejuvenation Res. 2007, 10, 301–309. [Google Scholar] [CrossRef]
- Singh, H.; Watt, K.; Veitch, R.; Cantor, M.; Duerksen, D.R. Malnutrition is prevalent in hospitalized medical patients: Are housestaff identifying the malnourished patient? Nutrition 2006, 22, 350–354. [Google Scholar] [CrossRef]
- Villalon, L.; Laporte, M.; Carrier, N. Nutrition screening for seniors in health care facilities: A survey of health professionals. Can. J. Diet. Pract. Pract. Res. 2011, 72, 162–169. [Google Scholar] [CrossRef]
- Willich, S.N.; Rossnagel, K.; Lochs, H.; Schütz, T.; Pirlich, M.; Kemps, M.; Luhman, N.; Lübke, H.J.; Minko, N. Social risk factors for hospital malnutrition. Nutrition 2005, 21, 295–300. [Google Scholar]
- Amaral, T.F.; Matos, L.C.; Teixeira, M.A.; Tavares, M.M.; Alvares, L.; Antunes, A. Undernutrition and associated factors among hospitalized patients. Clin. Nutr. 2010, 29, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Johansen, N.; Plum, L.M.; Bak, L.; Larsen, I.H.; Martinsen, A.; Andersen, J.R.; Baernthsen, H.; Bunch, E.; Lauesen, N. Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin. Nutr. 2002, 21, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Lou, W.; Gramlich, L.; Jeejeebhoy, K.N.; Laporte, M.; Allard, J.P.; Davidson, B.; Keller, H.; Bernier, P.; Teterina, A.; Duerksen, D.R.; et al. Decline in nutritional status is associated with prolonged length of stay in hospitalized patients admitted for 7 days or more: A prospective cohort study. Clin. Nutr. 2016, 35, 144–152. [Google Scholar]
- Omran, M.L.; Morley, J.E. Evaluation of protein-energy malnutrition in older people, Part II: Laboratory evaluation. Nutrition 2000, 16, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Lowrie, E.; Lew, N. Death risk in hemodialysis patients: The predictive value of commonly measured variables and an evaluation of death rate differences between facilities. Am. J. Kidney Dis. 1990, 15, 458–482. [Google Scholar] [CrossRef]
- United States Renal Data System. Combined conditions and correlation with mortality risk among 3399 incident hemodialysis patients. Am. J. Kidney Dis. 1992, 20 (Suppl. S2), 32. [Google Scholar]
- Guijarro, C.; Massy, Z.A.; Wiederkehr, M.R.; Ma, J.Z.; Kasiske, B.L. Serum albumin and mortality after renal transplantation. Am. J. Kidney Dis. 1996, 27, 117–123. [Google Scholar] [CrossRef]
- Tal, S.; Guller, V.; Shavit, Y.; Stern, F.; Malnick, S. Mortality predictors in hospitalized elderly patients. Q. Jour Med. 2011, 104, 933–938. [Google Scholar] [CrossRef]
- Lyons, O.; Whelan, B.; Bennett, K.; O’Riordan, D.; Silke, B. Serum albumin as an outcome predictor in hospital emergency medical admissions. Eur. J. Int. Med. 2010, 21, 17–20. [Google Scholar] [CrossRef]
- Marik, P.E. The treatment of hypoalbuminemia in the critically ill patient. Heart Lung 1993, 22, 166–170. [Google Scholar]
- Haller, C. Hypoalbuminemia in Renal Failure. Pathogenesis and Therapeutic Considerations. Kidney Blood Press Res. 2005, 28, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Namendys-Silva, S.A.; Gonzalez-Herrera, M.O.; Herrera-Gomez, A. Hypoalbuminemia in Critically Ill patients With Cancer: Incidence and Mortality. Am. J. Hosp. Palliat. Med. 2011, 28, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Oster, H.S.; Dolev, Y.; Kehat, O.; Weis-Meilik, A.; Mittelman, M. Serum Hypoalbuminemia Is a Long-Term Prognostic Marker in Medical Hospitalized Patients, Irrespective of the Underlying Disease. J. Clin. Med. 2022, 11, 1207. [Google Scholar] [CrossRef]
- Akirov, A.; Masri-Iraqi, H.; Atamna, A.; Shimon, I. Low Albumin Levels Are Associated with Mortality Risk in Hospitalized Patients. Am. J. Med. 2017, 130, 1465.e11–1465.e19. [Google Scholar] [CrossRef]
- Goldwasser, P.; Feldman, J. Association of serum albumin and mortality risk. J. Clin. Epidemiol. 1997, 50, 693–703. [Google Scholar] [CrossRef]
- Carriere, I.; Dupuy, A.-M.; Lacroux, A.; Cristol, J.-P.; Delcourt, C.; Pathologies Oculaires Liées à l’Age Study Group. Biomarkers of Inflammation and Malnutrition Associated with Early Death in Healthy Elderly People. J. Am. Geriatr. Soc. 2008, 56, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Knaus, W.A.; Wagner, D.P.; Draper, E.A.; Zimmerman, J.E.; Bergner, M.; Bastos, P.G.; Sirio, C.A.; Murphy, D.J.; Lotring, T.; Damiano, A.; et al. The APACHE III prognostic system-risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991, 100, 1619. [Google Scholar] [CrossRef]
- Phillips, A.; Shaper, A.G.; Whincup, P.H. Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet 1989, 2, 1434–1436. [Google Scholar] [CrossRef]
- Gillum, R.F.; Makuc, D.M. Serum albumin, coronary heart disease, and death. Am. Heart J. 1992, 123, 507–513. [Google Scholar] [CrossRef]
- Klonoff-Cohen, H.; Barrett-Connor, E.L.; Edelstein, S.L. Albumin levels as a predictor of mortality in the healthy elderly. J. Clin. Epidemiol. 1992, 45, 207–212. [Google Scholar] [CrossRef]
- Corti, M.C.; Guralnik, J.M.; Salive, M.E.; Sorkin, J.D. Serum albumin level and physical disability as predictors of mortality in older persons. J. Am. Med. Assoc. 1994, 272, 1036–1042. [Google Scholar] [CrossRef]
- Law, M.R.; Morris, J.K.; Wald, N.J.; Hale, A.K. Serum albumin and mortality in the BUPA study. Int. J. Epidemiol. 1994, 23, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Kuller, L.H.; Eichner, J.E.; Orchard, T.J.; Grandits, G.A.; McCallum, L.; Tracy, R.P. The relation between serum albumin and risk of coronary heart disease in the multiple risk factor intervention trial. Am. J. Epidemiol. 1991, 134, 1266–1277. [Google Scholar] [CrossRef] [PubMed]
- Cabrerizo, S.; Cuadras, D.; Gomez-Busto, F.; Artaza-Artabe, I.; Marin-Ciancas, F.; Malafarina, V. Serum albumin and health in older people: Review and meta-analysis. Maturitas 2015, 81, 17–27. [Google Scholar] [CrossRef]
- Devran, Ö.; Karakurt, Z.; Adıgüzel, N.; Güngör, G.; Moçin, Ö.Y.; Balcı, M.K.; Saltürk, C.; Takır, H.B.; Kargın, F.; Yılmaz, A. C-reactive protein as a predictor of mortality in patients affected with severe sepsis in intensive care unit. Multidiscip. Respir. Med. 2012, 7, 47. [Google Scholar] [CrossRef]
- Lobo, S.M.; Lobo, F.R.; Bota, D.P.; Lopes-Ferreira, F.; Soliman, H.M.; Mélot, C.; Vincent, J.L. C-reactive protein levels correlate with mortality and organ failure in critically ill patients. Chest 2003, 123, 2043–2049. [Google Scholar] [CrossRef]
- Prieto, M.F.; Kilstein, J.; Bagilet, D.; Pezzotto, S.M. C-reactive protein as a marker of mortality in intensive care unit. Med. Intensiv. 2008, 32, 424–430. [Google Scholar]
- Marsik, C.; Kazemi-Shirazi, L.; Schickbauer, T.; Winkler, S.; Joukhadar, C.; Wagner, O.F.; Endler, G. C-Reactive Protein and All-Cause Mortality in a Large Hospital-Based Cohort. Clin. Chem. 2008, 54, 343–349. [Google Scholar] [CrossRef]
- Cao, J.J.; Arnold, A.M.; Manolio, T.A.; Polak, J.F.; Psaty, B.M.; Hirsch, C.H.; Kuller, L.H.; Cushman, M. Association of carotid artery intima-media thickness, plaques, and C-reactive protein with future cardiovascular disease and all-cause mortality: The Cardiovascular Health Study. Circulation 2007, 116, 32–38. [Google Scholar] [CrossRef]
- Currie, C.J.; Poole, C.D.; Conway, P. Evaluation of the association between the first observation and the longitudinal change in C-reactive protein, and all-cause mortality. Heart 2008, 94, 457–462. [Google Scholar] [CrossRef]
- Zacho, J.; Tybjærg-Hansen, A.; Nordestgaard, B.G. C-reactive protein and all-cause mortality—The Copenhagen City Heart Study. Eur. Heart J. 2010, 31, 1624–1632. [Google Scholar] [CrossRef] [PubMed]
- Jellinge, M.E.; Henriksen, D.P.; Hallas, P.; Brabrand, M. Hypoalbuminemia Is a Strong Predictor of 30-Day All-Cause Mortality in Acutely Admitted Medical Patients: A Prospective, Observational, Cohort Study. PLoS ONE 2014, 9, e105983. [Google Scholar] [CrossRef] [PubMed]
- Quispe, E.A.; Li, X.M.; Yi, H. Comparison and relationship of thyroid hormones, il-6, il-10 and albumin as mortality predictors in case-mix critically ill patients. Cytokine 2016, 81, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Povoa, P. C-reactive protein: A valuable marker of sepsis. Intensive Care Med. 2002, 28, 235–243. [Google Scholar] [CrossRef]
- Oh, T.K.; Ji, E.; Na, H.-s.; Min, B.; Jeon, Y.-T.; Do, S.-H.; Song, I.-A.; Park, H.-P.; Hwang, J.-W. C-Reactive Protein to Albumin Ratio Predicts 30-Day and 1-Year Mortality in Postoperative Patients after Admission to the Intensive Care Unit. J. Clin. Med. 2018, 7, 39. [Google Scholar] [CrossRef]
- Dominguez de Villota, E.; Mosquera, J.M.; Rubio, J.J.; Galdos, P.; Diez Balda, V.; de la Serna, J.L.; Tomas, M.I. Association of a low serum albumin with infection and increased mortality in critically ill patients. Intensive Care Med. 1980, 7, 19–22. [Google Scholar] [CrossRef]
- Kim, M.H.; Ahn, J.Y.; Song, J.E.; Choi, H.; Ann, H.W.; Kim, J.K.; Kim, J.H.; Jeon, Y.D.; Kim, S.B.; Jeong, S.J.; et al. The C-reactive protein/albumin ratio as an independent predictor of mortality in patients with severe sepsis or septic shock treated with early goal-directed therapy. PLoS ONE 2015, 10, e0132109. [Google Scholar] [CrossRef]
- Ranzani, O.T.; Zampieri, F.G.; Forte, D.N.; Azevedo, L.C.; Park, M. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS ONE 2013, 8, e59321. [Google Scholar] [CrossRef]
- Yu, Y.; Wu, W.; Dong, Y.; Li, L. C-Reactive Protein-to-Albumin Ratio Predicts Sepsis and Prognosis in Patients with Severe Burn Injury. Mediat. Inflamm. 2021, 2021, 6621101. [Google Scholar] [CrossRef]
- Kurniawan, R.B.; Oktafia, P.; Saputra, P.B.T.; Purwati, D.D.; Saputra, M.E.; Maghfirah, I.; Faizah, N.N.; Oktaviono, Y.H.; Alkaff, F.F. The roles of C-reactive protein-albumin ratio as a novel prognostic biomarker in heart failure patients: A systematic review. Curr. Probl. Cardiol. 2024, 49, 102475. [Google Scholar] [CrossRef]
- Iwata, M.; Kuzuya, M.; Kitagawa, Y.; Iguchi, A. Prognostic value of serum albumin combined with serum C-reactive protein levels in older hospitalized patients: Continuing importance of serum albumin. Aging Clin. Exp. Res. 2006, 18, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Savina, C.; Ricciardi, L.M.; Coletti, C.; Paolini, M.; Scavone, L.; De Felice, M.R.; Laviano, A.; Fanelli, F.R.; Cannella, C. Predicting the outcome of artificial nutrition by clinical and functional indices. Nutrition 2009, 25, 11–19. [Google Scholar] [CrossRef]
- Oh, T.K.; Song, I.-A.; Lee, J.H. Clinical usefulness of C-reactive protein to albumin ratio in predicting 30-day mortality in critically ill patients: A retrospective analysis. Sci. Rep. 2018, 8, 14977. [Google Scholar] [CrossRef] [PubMed]
- Llop-Talaveron, J.; Badia-Tahull, M.B.; Leiva-Badosa, E. An inflammation-based prognostic score, the C-reactive protein/albumin ratio predicts the morbidity and mortality of patients on parenteral nutrition. Clin. Nutr. 2018, 37, 1575–1583. [Google Scholar] [CrossRef]
- Procopio, A.D.; Cherubini, A.; Bonfigli, A.R.; Olivieri, F.; Balistreri, C.R.; Burattini, M.; Cecchini, S.; Capalbo, M.; Fedecostante, M.; Spannella, F.; et al. Inflammation scores based on C-reactive protein and albumin predict mortality in hospitalized older patients independent of the admission diagnosis. Immun. Ageing 2024, 21, 67. [Google Scholar]
- Baune, B.T.; Rothermundt, M.; Ladwig, K.H.; Meisinger, C.; Berger, K. Systemic inflammation (Interleukin 6) predicts all-cause mortality in men: Results from a 9-year follow-up of the MEMO Study. Age 2011, 33, 209–217. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Cummings, P. The Relative Merits of Risk Ratios and Odds Ratios. Arch. Pediatr. Adolesc. Med. 2009, 163, 438. [Google Scholar] [CrossRef]
- Neugarten, B.L. Age groups in American society and the rise of the young-old. Ann. Am. Acad. Political Soc. Sci. 1974, 415, 187–198. [Google Scholar] [CrossRef]
- Forman, D.E.; Berman, A.D.; McCabe, C.H.; Baim, D.S.; Wei, J.Y. PTCA in the elderly: The “young-old” versus the “old-old”. J. Am. Geriatr. Soc. 1992, 40, 19–22. [Google Scholar] [CrossRef]
- Grande, E.; Grippo, F.; Frova, L.; Pantosti, A.; Pezzotti, P.; Fedeli, U. The increase of sepsis-related mortality in Italy: A nationwide study, 2003–2015. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 1701–1708. [Google Scholar] [CrossRef]
- National Institute of Statistics. Available online: https://esploradati.istat.it/databrowser/#/it/dw/categories/IT1,Z0810HEA,1.0/HEA_DEATH/DCIS_CMORTEM (accessed on 6 May 2025).

| Male | Female | Effect Size Cohen’s h | Sig. (99% CIs) | |
| Subjects N (%) | 1316 (47.3%) | 1464 (52.7%) | 0.11 | 0.004 (0.001–0.008) |
| Male | Female | Effect Size Cohen’s d | Sig. (99% CIs) | |
| Age at hospitalization (Mean ± SD) | 79 ± 8 | 82 ± 8 | 0.32 | <0.001 (0.000–0.002) |
| LOS (Mean ± SD) | 11 ± 7 | 11 ± 7 | 0.01 | 0.947 (0.936–0.958) |
| Albuminemia (Mean ± SD) | 3.05 ± 0.6 | 3.03 ± 0.6 | 0.02 | 0.751 (0.730–0.772) |
| CRP (Mean ± SD) | 80.1 ± 89 | 73.2 ± 88 | 0.08 | <0.001 (0.000–0.002) |
| CRP/Alb ratio (Mean ± SD) | 31.3 ± 38 | 29.2 ± 40 | 0.05 | 0.476 (0.452–0.501) |
| Male | Female | Effect Size Cohen’s h | Sig. (99% CIs) | |
|---|---|---|---|---|
| Young old N (%) (65–74 years old) | 382 (56.9%) | 289 (43.1%) | 0.28 | <0.001 (0.000–0.002) |
| Old N (%) (75–84 years old) | 551 (49.4%) | 565 (50.6%) | 0.02 | 0.705 (0.682–0.727) |
| Very Old N (%) (85 + years old) | 383 (38.6%) | 610 (61.4%) | 0.46 | <0.001 (0.000–0.002) |
| Length of Stay | ||
|---|---|---|
| Age at admission | Partial correlation | −0.015 |
| Significance (2-tailed) | 0.441 | |
| CRP | Partial correlation | 0.148 |
| Significance (2-tailed) | <0.001 | |
| Albuminemia | Partial correlation | −0.189 |
| Significance (2-tailed) | <0.001 | |
| CRP/Alb ratio | Partial correlation | 0.150 |
| Significance (2-tailed) | <0.001 | |
| Deceased | |
|---|---|
| Severe Sepsis N (%) | 221 (49.8%) |
| Pulmonary edema and respiratory failure N (%) | 44 (9.9%) |
| Any respiratory infection and inflammation with complications N (%) | 43 (9.7%) |
| Pleural effusion with complications N (%) | 19 (4.3%) |
| Heart failure and shock N (%) | 19 (4.3%) |
| Malignant neoplasms of digestive system with complications N (%) | 9 (2.0%) |
| Any infectious disease N (%) | 9 (2.0%) |
| Severe renal failure N (%) | 8 (1.8%) |
| All other causes N (%) | 72 (16.2%) |
| Total number of deaths N (%) | 444 (100.0%) |
| Deceased | Non-Deceased | Effect Size Cohen’s h | Sig. (99% CIs) | |
| Subjects N (%) | 444 (16%) | 2336 (84%) | 1.50 | <0.001 (0.000–0.002) |
| Deceased | Non-Deceased | Effect Size Phi Coefficient | Sig. | |
| Male N (%) | 221 (49.8%) | 1095 (46.9%) | 0.02 | 0.276 |
| Female N (%) | 223 (50.2%) | 1241 (53.1%) | ||
| Deceased | Non-Deceased | Effect Size Cohen’s d | Sig. (99% CIs) | |
| Age at hospitalization (Mean ± SD) | 84 ± 8 | 80 ± 8 | 0.411 | <0.001 (0.000–0.002) |
| LOS (Mean ± SD) | 12 ± 10 | 11 ± 7 | 0.098 | 0.003 (0.000–0.005) |
| Albuminemia (Mean ± SD) | 2.6 ± 0.6 | 3.1 ± 0.6 | −0.955 | <0.001 (0.000–0.002) |
| CRP (Mean ± SD) | 123.6 ± 95.9 | 67.5 ± 84.1 | 0.651 | <0.001 (0.000–0.002) |
| CRP/Alb ratio (Mean ± SD) | 54.8 ± 47.8 | 25.6 ± 35.8 | 0.771 | <0.001 (0.000–0.002) |
| OR | 95% CIs | Sig. | |
|---|---|---|---|
| LOS >= 7 days | 5.13 | 2.38–12.62 | <0.001 |
| LOS < 7 days | 15 | 3.99–81.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capurso, C.; Lo Buglio, A.; Bellanti, F.; Serviddio, G. C-Reactive Protein to Albumin Ratio Predicts Early Mortality in Hospitalized Older Patients, Independent of the Admission Diagnosis. Nutrients 2025, 17, 1984. https://doi.org/10.3390/nu17121984
Capurso C, Lo Buglio A, Bellanti F, Serviddio G. C-Reactive Protein to Albumin Ratio Predicts Early Mortality in Hospitalized Older Patients, Independent of the Admission Diagnosis. Nutrients. 2025; 17(12):1984. https://doi.org/10.3390/nu17121984
Chicago/Turabian StyleCapurso, Cristiano, Aurelio Lo Buglio, Francesco Bellanti, and Gaetano Serviddio. 2025. "C-Reactive Protein to Albumin Ratio Predicts Early Mortality in Hospitalized Older Patients, Independent of the Admission Diagnosis" Nutrients 17, no. 12: 1984. https://doi.org/10.3390/nu17121984
APA StyleCapurso, C., Lo Buglio, A., Bellanti, F., & Serviddio, G. (2025). C-Reactive Protein to Albumin Ratio Predicts Early Mortality in Hospitalized Older Patients, Independent of the Admission Diagnosis. Nutrients, 17(12), 1984. https://doi.org/10.3390/nu17121984









