The Association of Food Insecurity and Risk of Mortality: A Systematic Review and Meta-Analysis of Large-Scale Cohorts
Abstract
1. Introduction
2. Methods
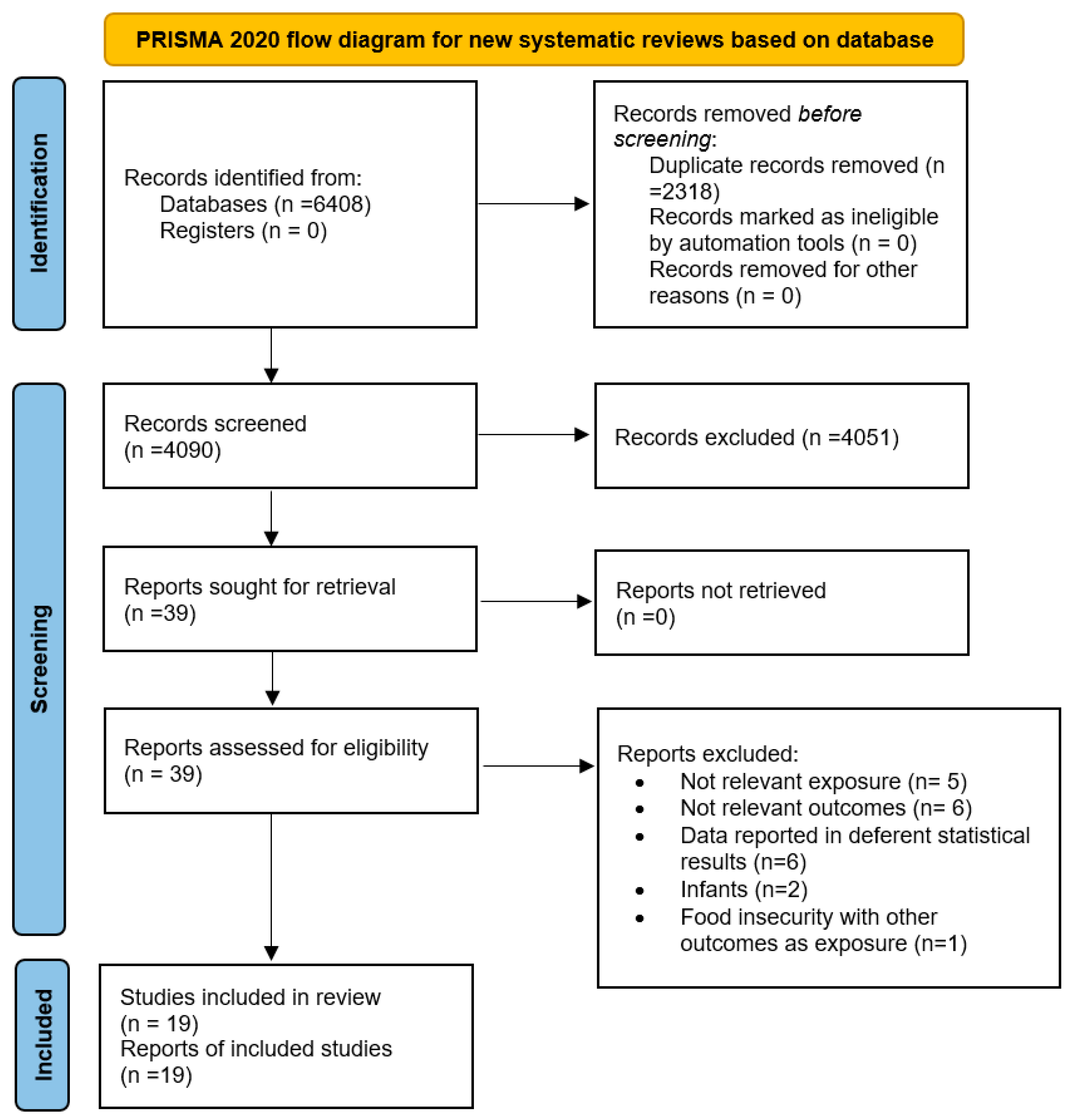
2.1. Literature Search and Selection
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analyses and Data Synthesis
2.6. Quality of Evidence
3. Results
3.1. Study Characteristics
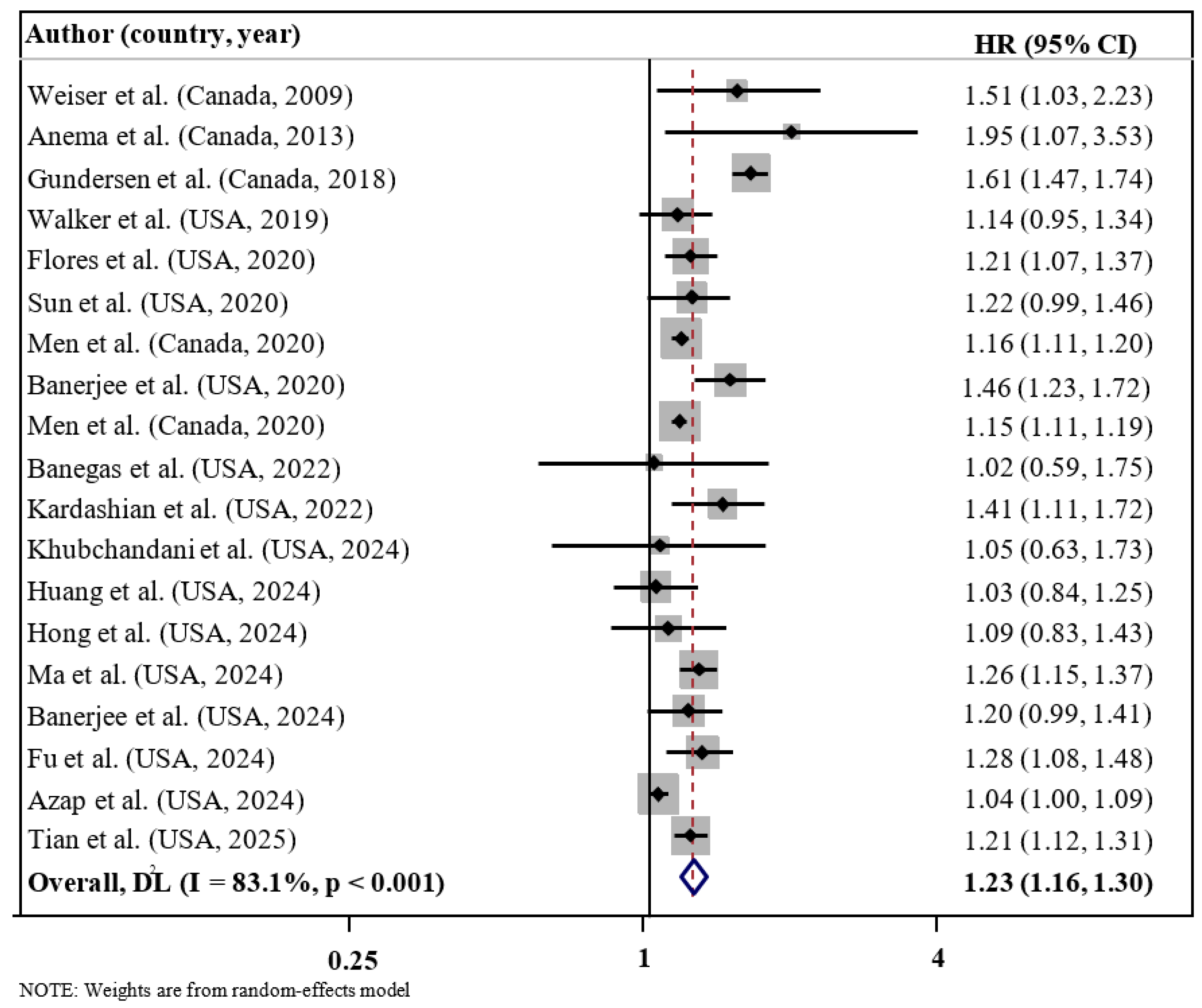
3.2. FI and Risk of Mortality
3.3. Meta-Regression Analysis
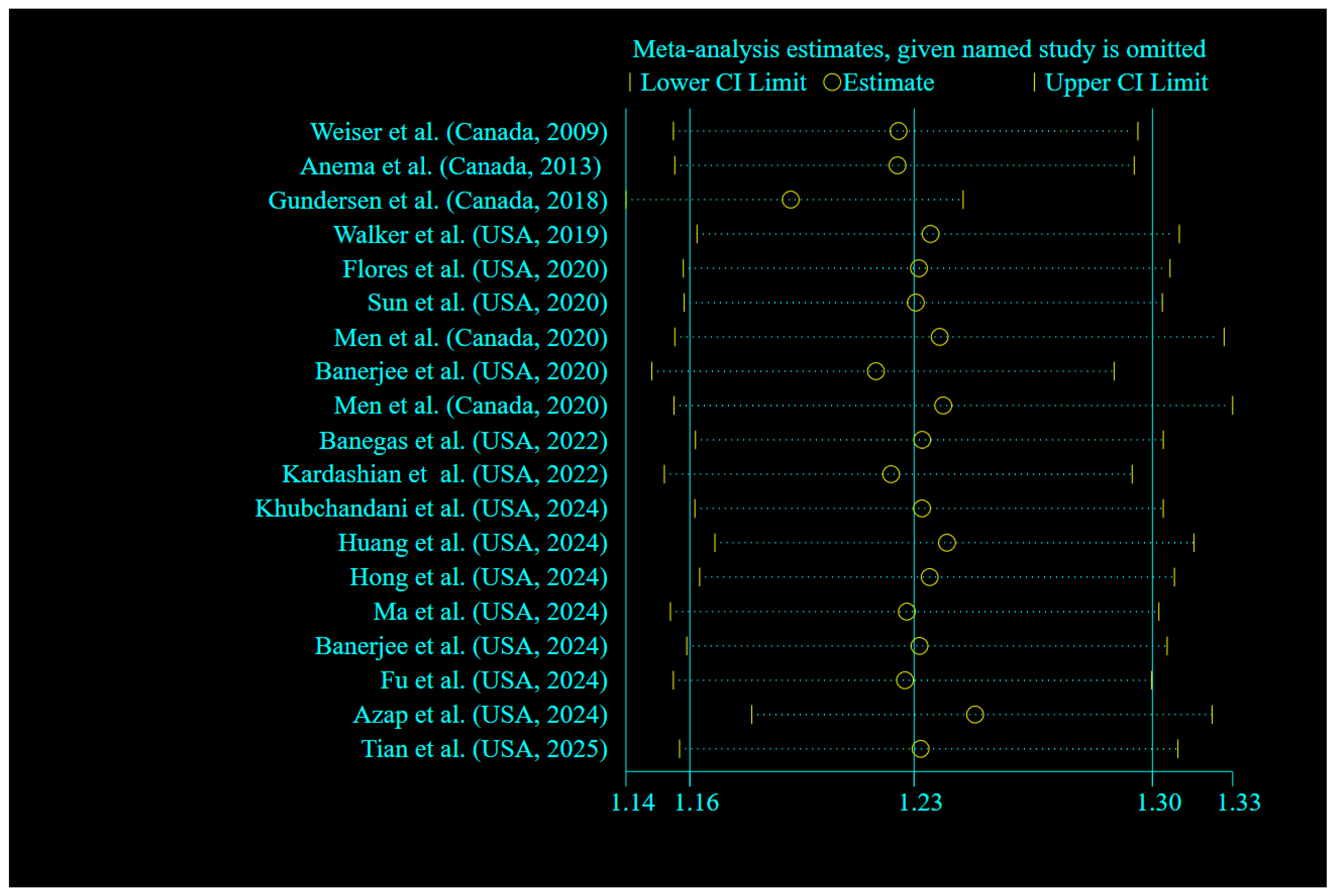
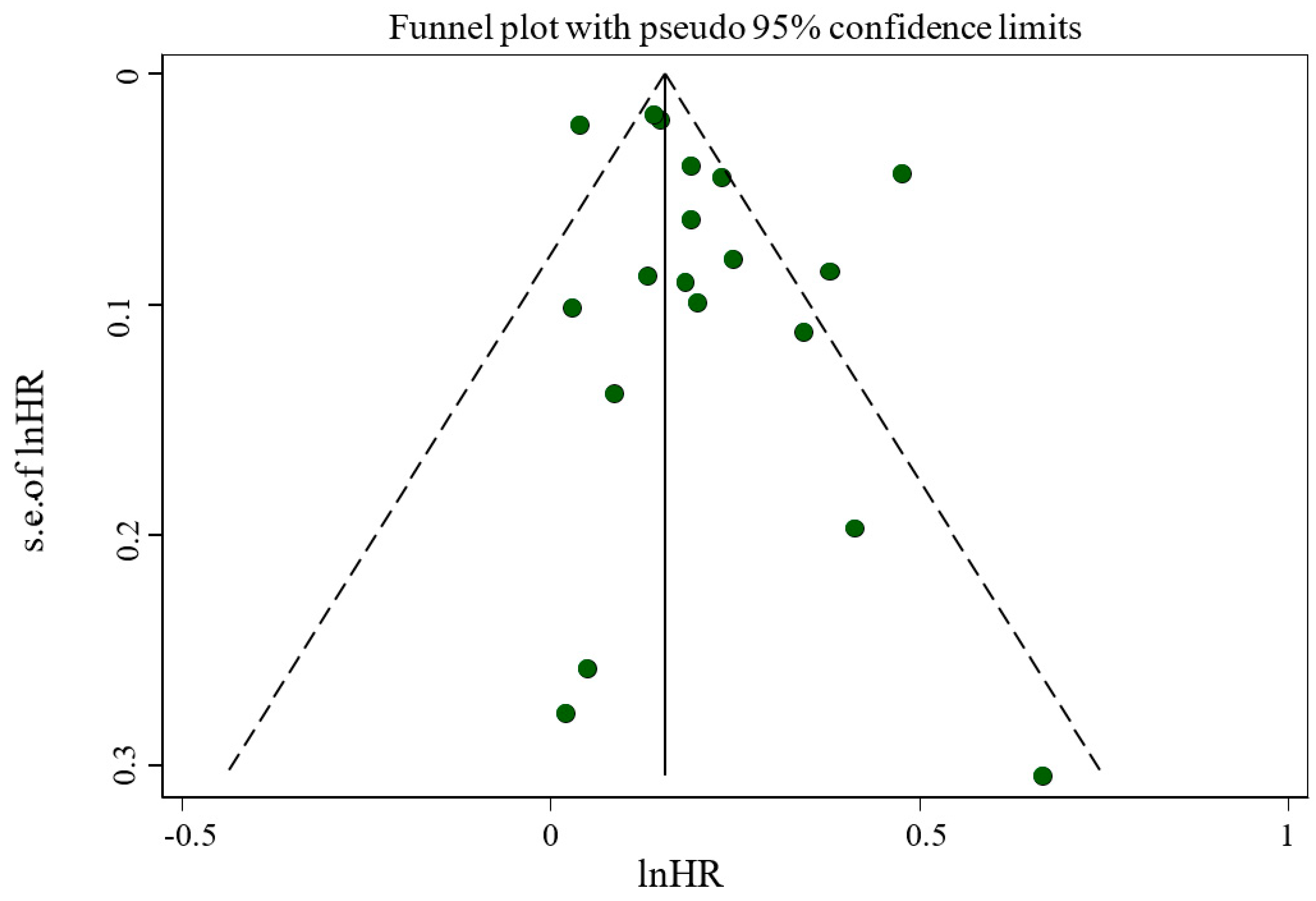
3.4. Sensitivity Analyses and Publication Bias
3.5. Quality of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2021; USDA: Washington, DC, USA, 2022.
- Cumpston, M.; Li, T.; Page, M.; Chandler, J.; Welch, V.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.; Ali, A. Global food insecurity and its association with malnutrition. Emerg. Chall. Agric. Food Sci. 2023, 2. [Google Scholar]
- Medicine, B.M.C. Food insecurity: A neglected public health issue requiring multisectoral action. BMC Med. 2023, 21, 130. [Google Scholar] [CrossRef]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Odoms-Young, A.; Brown, A.G.M.; Agurs-Collins, T.; Glanz, K. Food Insecurity, Neighborhood Food Environment, and Health Disparities: State of the Science, Research Gaps and Opportunities. Am. J. Clin. Nutr. 2024, 119, 850–861. [Google Scholar] [CrossRef]
- Porras-Pérez, E.; Romero-Cabrera, J.L.; Díaz-Cáceres, A.; Serrán-Jiménez, A.; Arenas-Montes, J.; Peña-Orihuela, P.J.; De-Castro-Burón, I.; García-Ríos, A.; Torres-Peña, J.D.; Malagón, M.M.; et al. Food Insecurity and Its Cardiovascular Implications in Underresourced Communities. J. Am. Heart Assoc. 2025, 14, e037457. [Google Scholar] [CrossRef]
- Levi, R.; Bleich, S.N.; Seligman, H.K. Food Insecurity and Diabetes: Overview of Intersections and Potential Dual Solutions. Diabetes Care 2023, 46, 1599–1608. [Google Scholar] [CrossRef]
- Royer, M.F.; Rosas, L.G.; King, A.C. Food insecurity and cardiovascular disease risk factors among U.S. adults. BMC Public Health 2025, 25, 817. [Google Scholar] [CrossRef]
- Mazloomi, S.N.; Talebi, S.; Kazemi, M.; Ghoreishy, S.M.; Moosavian, S.P.; Amirian, P.; Mohammadi, H.; Nouri-Majd, S.; Marx, W.; Hojjati Kermani, M.A.; et al. Food insecurity is associated with the sleep quality and quantity in adults: A systematic review and meta-analysis. Public Health Nutr. 2023, 26, 792–802. [Google Scholar] [CrossRef]
- Lopes, S.O.; Abrantes, L.C.; Azevedo, F.M.; Morais, N.D.; Morais, D.D.; Gonçalves, V.S.; Fontes, E.A.; Franceschini, S.D.; Priore, S.E. Food Insecurity and Micronutrient Deficiency in Adults: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 1074. [Google Scholar] [CrossRef]
- Moradi, S.; Arghavani, H.; Issah, A.; Mohammadi, H.; Mirzaei, K. Food insecurity and anaemia risk: A systematic review and meta-analysis. Public Health Nutr. 2018, 21, 3067–3079. [Google Scholar] [CrossRef]
- Chen, K.Y.; Blackford, A.L.; Hussaini, S.Q. County-Level Food Insecurity to Predict Cancer Incidence and Mortality in the United States, 2015–2020; American Society of Clinical Oncology: Alexandria, VA, USA, 2023. [Google Scholar]
- Moradi, S.; Mirzababaei, A.; Mohammadi, H.; Moosavian, S.P.; Arab, A.; Jannat, B.; Mirzaei, K. Food insecurity and the risk of undernutrition complications among children and adolescents: A systematic review and meta-analysis. Nutrition 2019, 62, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Pourmotabbed, A.; Moradi, S.; Babaei, A.; Ghavami, A.; Mohammadi, H.; Jalili, C.; Symonds, M.E.; Miraghajani, M. Food insecurity and mental health: A systematic review and meta-analysis. Public Health Nutr. 2020, 23, 1778–1790. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, D.A.; Kreider, R.B.; Petro, J.L.; Romance, R.; García-Sillero, M.; Benítez-Porres, J.; Vargas-Molina, S. Creatine Enhances the Effects of Cluster-Set Resistance Training on Lower-Limb Body Composition and Strength in Resistance-Trained Men: A Pilot Study. Nutrients 2021, 13, 2303. [Google Scholar] [CrossRef]
- Kohanmoo, A.; Hashemzadeh, M.; Teymouri, M.; Zare, M.; Akhlaghi, M. Food insecurity is associated with low diet quality and unhealthy cooking and eating habits in Iranian women. J. Health Popul. Nutr. 2024, 43, 42. [Google Scholar] [CrossRef]
- Anema, A.; Chan, K.; Chen, Y.; Weiser, S.; Montaner, J.S.; Hogg, R.S. Relationship between food insecurity and mortality among HIV-positive injection drug users receiving antiretroviral therapy in British Columbia, Canada. PLoS ONE 2013, 8, e61277. [Google Scholar] [CrossRef] [PubMed]
- Azap, L.; Woldesenbet, S.; Akpunonu, C.C.; Alaimo, L.; Endo, Y.; Lima, H.A.; Yang, J.; Munir, M.M.; Moazzam, Z.; Huang, E.S.; et al. The Association of Food Insecurity and Surgical Outcomes Among Patients Undergoing Surgery for Colorectal Cancer. Dis. Colon Rectum 2024, 67, 577–586. [Google Scholar] [CrossRef]
- Banegas, M.P.; Dickerson, J.F.; Zheng, Z.; Murphy, C.C.; Tucker-Seeley, R.; Murphy, J.D.; Yabroff, K.R. Association of Social Risk Factors with Mortality among US Adults with a New Cancer Diagnosis. JAMA Netw. Open 2022, 5, E2233009. [Google Scholar] [CrossRef]
- Flores, M.W.; Lê Cook, B.; Mullin, B.; Halperin-Goldstein, G.; Nathan, A.; Tenso, K.; Schuman-Olivier, Z. Associations between neighborhood-level factors and opioid-related mortality: A multi-level analysis using death certificate data. Addiction 2020, 115, 1878–1889. [Google Scholar] [CrossRef]
- Fu, P.; Wen, J.; Duan, X.; Hu, X.; Chen, F.; Yuan, P. Association between adult food insecurity and mortality among adults aged 20–79 years with diabetes: A population-based retrospective cohort study. Diabet Med 2024, 41, e15268. [Google Scholar] [CrossRef]
- Gundersen, C.; Tarasuk, V.; Cheng, J.; De Oliveira, C.; Kurdyak, P. Food insecurity status and mortality among adults in Ontario, Canada. PLoS ONE 2018, 13, e0202642. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Wei, T.; Huang, Y.; Zhang, A.; Zhang, H.; Zhang, Z.; Xu, Y.; Pan, H.; Kong, L.; Li, Y. Association between social determinants of health and survival among the US cancer survivors population. BMC Med. 2024, 22, 343. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Banerjee, S.; Kopera-Frye, K.; Gonzales-Lagos, R.; Onukogu, C. Food insecurity and mortality risk among adults with Chronic Kidney Disease: A longitudinal cohort study of NHANES. Nutrire 2024, 49, 52. [Google Scholar] [CrossRef]
- Men, F.; Gundersen, C.; Urquia, M.L.; Tarasuk, V. Association between household food insecurity and mortality in Canada: A population-based retrospective cohort study. CMAJ 2020, 192, E53–E60. [Google Scholar] [CrossRef]
- Sun, Y.; Liu, B.; Rong, S.; Du, Y.; Xu, G.; Snetselaar, L.G.; Wallace, R.B.; Bao, W. Food insecurity is associated with cardiovascular and all-cause mortality among adults in the united states. J. Am. Heart Assoc. 2020, 9, e014629. [Google Scholar] [CrossRef]
- Tian, L.; Jaeger, B.C.; Marshall, A.N.; Dorans, K.S.; Bell, C.N.; Theall, K.P.; Chen, J.; He, J.; Bundy, J.D. Comparison of Associations of Food Security Instruments and Mediators with Premature All-Cause and Cardiovascular Disease Death in US Adults. Circ. Cardiovasc. Qual. Outcomes 2025, e011209. [Google Scholar] [CrossRef]
- Walker, R.J.; Chawla, A.; Garacci, E.; Williams, J.S.; Mendez, C.; Ozieh, M.N.; Egede, L.E. Assessing the relationship between food insecurity and mortality among U.S. adults. Ann. Epidemiol. 2019, 32, 43–48. [Google Scholar] [CrossRef]
- Weiser, S.D.; Fernandes, K.A.; Brandson, E.K.; Lima, V.D.; Anema, A.; Bangsberg, D.R.; Montaner, J.S.; Hogg, R.S. The association between food insecurity and mortality among HIV-infected individuals on HAART. J. Acquir. Immune Defic. Syndr. 2009, 52, 342–349. [Google Scholar] [CrossRef]
- Tian, F.; Shen, Q.; Hu, Y.; Ye, W.; Valdimarsdóttir, U.A.; Song, H.; Fang, F. Association of stress-related disorders with subsequent risk of all-cause and cause-specific mortality: A population-based and sibling-controlled cohort study. Lancet Reg. Health–Eur. 2022, 18, 100402. [Google Scholar] [CrossRef]
- Men, F.; Tarasuk, V. Severe food insecurity associated with mortality among lower-income Canadian adults approaching eligibility for public pensions: A population cohort study. BMC Public Health 2020, 20, 1484. [Google Scholar] [CrossRef]
- Banerjee, S.; Radak, T.; Khubchandani, J.; Dunn, P. Food Insecurity and Mortality in American Adults: Results from the NHANES-Linked Mortality Study. Health Promot. Pract. 2021, 22, 204–214. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Oxford: 2000. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 3 April 2025).
- Symons, M.; Moore, D. Hazard rate ratio and prospective epidemiological studies. J. Clin. Epidemiol. 2002, 55, 893–899. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; p. 4. [Google Scholar]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. Bmj 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. Bmj 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Banerjee, S.; Radak, T.; Khubchandani, J.; Gonzales-Lagos, R.; Dunn, P. Food insecurity and the risk of mortality among Hispanics with hypertension. Nutr. Metab. Cardiovasc. Dis. 2024, 34, 2555–2561. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.R.; Wang, R.; Case, S.; Jo, A.; Turner, K.; Ross, K.M. Association of food insecurity with overall and disease-specific mortality among cancer survivors in the US. Support. Care Cancer 2024, 32, 309. [Google Scholar] [CrossRef]
- Kardashian, A.; Dodge, J.L.; Terrault, N.A. Food Insecurity is Associated With Mortality Among U.S. Adults with Nonalcoholic Fatty Liver Disease and Advanced Fibrosis. Clin. Gastroenterol. Hepatol. 2022, 20, 2790–2799.e2794. [Google Scholar] [CrossRef]
- Ma, H.; Wang, X.; Li, X.; Heianza, Y.; Katzmarzyk, P.T.; Franco, O.H.; Qi, L. Food Insecurity and Premature Mortality and Life Expectancy in the US. JAMA Intern. Med. 2024, 184, 301–310. [Google Scholar] [CrossRef]
- Njoku, A.; Sawadogo, W.; Frimpong, P. Racial and ethnic disparities in cancer occurrence and outcomes in rural United States: A scoping review. Cancer Control 2024, 31, 10732748241261558. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.M.; Adrada, B.E. Hereditary Breast Cancer: BRCA Mutations and Beyond. Radiol. Clin. N. Am. 2024, 62, 627–642. [Google Scholar] [CrossRef]
- Possenti, I.; Martini, A.; Bagnardi, V.; Specchia, C.; Garavello, W.; Odone, A.; Smits, L.J.M.; Gallus, S.; Lugo, A. Association between cigarette smoking and nasopharyngeal cancer risk: A meta-analysis. Rhinology 2025, 63, 13–21. [Google Scholar] [CrossRef]
- Shin, S.; Fu, J.; Shin, W.-K.; Huang, D.; Min, S.; Kang, D. Association of food groups and dietary pattern with breast cancer risk: A systematic review and meta-analysis. Clin. Nutr. 2023, 42, 282–297. [Google Scholar] [CrossRef]
- Iwasaki, M.; Itoh, H.; Sawada, N.; Tsugane, S. Exposure to environmental chemicals and cancer risk: Epidemiological evidence from Japanese studies. Genes Environ. 2023, 45, 10. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-T.; Chiu, L.-T. The impact of psychological distress on cervical cancer. Cancers 2023, 15, 1100. [Google Scholar] [CrossRef]
- Bourgeois, A.; Horrill, T.; Mollison, A.; Stringer, E.; Lambert, L.K.; Stajduhar, K. Barriers to cancer treatment for people experiencing socioeconomic disadvantage in high-income countries: A scoping review. BMC Health Serv. Res. 2024, 24, 670. [Google Scholar] [CrossRef]
- Lombe, D.C.; Mwamba, M.; Msadabwe, S.; Bond, V.; Simwinga, M.; Ssemata, A.S.; Muhumuza, R.; Seeley, J.; Mwaka, A.D.; Aggarwal, A. Delays in seeking, reaching and access to quality cancer care in sub-Saharan Africa: A systematic review. BMJ Open 2023, 13, e067715. [Google Scholar] [CrossRef]
- Zanobini, P.; Bonaccorsi, G.; Giusti, M.; Minardi, V.; Possenti, V.; Masocco, M.; Garofalo, G.; Mereu, G.; Cecconi, R.; Lorini, C. Health literacy and breast cancer screening adherence: Results from the population of Tuscany, Italy. Health Promot. Int. 2023, 38, daad177. [Google Scholar] [CrossRef]
- Aljahdali, A.A. Food insecurity and ultra-processed food consumption in the Health and Retirement Study: Cross-sectional analysis. J. Nutr. Health Aging 2025, 29, 100422. [Google Scholar] [CrossRef]
- Chodur, G.; Singh, S.; Riordan, E.E.; Kalaydjian, S.; Martinez, S.M. Campus Food Pantry Use May Improve Daily Frequency of Fruit and Vegetable Intake Among California University Students Experiencing Food Insecurity. J. Acad. Nutr. Diet. 2024, 124, 225–232.e221. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, K.; Smith-Warner, S.A.; Rossato, S.L.; Khandpur, N.; Manson, J.E.; Qi, L.; Rimm, E.B.; Mukamal, K.J.; Willett, W.C.; Wang, M.; et al. Ultra-processed foods and cardiovascular disease: Analysis of three large US prospective cohorts and a systematic review and meta-analysis of prospective cohort studies. Lancet Reg. Health–Am. 2024, 37, 100859. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.K.; Tong, T.Y.N.; Watling, C.Z.; Reynolds, A.; Piernas, C.; Schmidt, J.A.; Papier, K.; Carter, J.L.; Key, T.J.; Perez-Cornago, A. Associations between types and sources of dietary carbohydrates and cardiovascular disease risk: A prospective cohort study of UK Biobank participants. BMC Med. 2023, 21, 34. [Google Scholar] [CrossRef] [PubMed]
- Men, F.; Tarasuk, V. Classification Differences in Food Insecurity Measures between the United States and Canada: Practical Implications for Trend Monitoring and Health Research. J. Nutr. 2022, 152, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Uppal, S. Food Insecurity Among Canadian Families; Statistics Canada=Statistique Canada. 2023. Available online: https://www150.statcan.gc.ca/n1/pub/75-006-x/2023001/article/00013-eng.htm (accessed on 3 April 2025).
- Byaro, M.; Mafwolo, G.; Ngereza, C. Does unemployment in sub-Saharan Africa have asymmetric effects on health? A panel quantile approach. J. Econ. Asymmetries 2023, 28, e00316. [Google Scholar] [CrossRef]
- Kanbay, M.; Tanriover, C.; Copur, S.; Peltek, I.B.; Mutlu, A.; Mallamaci, F.; Zoccali, C. Social isolation and loneliness: Undervalued risk factors for disease states and mortality. Eur. J. Clin. Investig. 2023, 53, e14032. [Google Scholar] [CrossRef]
- Johnstone, A.M.; Lonnie, M. Tackling diet inequalities in the UK food system: Is food insecurity driving the obesity epidemic? (The FIO Food project). Proc. Nutr. Soc. 2024, 83, 133–141. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, G.-C.; Sotres-Alvarez, D.; Perreira, K.M.; Daviglus, M.L.; Pirzada, A.; Gallo, L.C.; Llabre, M.M.; Cai, J.; Xue, X.; et al. General or Central Obesity and Mortality Among US Hispanic and Latino Adults. JAMA Netw. Open 2024, 7, e2351070. [Google Scholar] [CrossRef]
- Jia, J.; Carnethon, M.R.; Wong, M.; Lewis, C.E.; Schreiner, P.J.; Kandula, N.R. Food Insecurity and Incident Cardiovascular Disease Among Black and White US Individuals, 2000–2020. JAMA Cardiol. 2025, 10, 456–462. [Google Scholar] [CrossRef]
- Zhou, C.; Miao, H.; Zhao, Y.; Wan, X. Food insecurity increases the risk of overweight and chronic diseases in adolescents: A systematic review and meta-analysis. Food Sci. Hum. Wellness 2023, 12, 1937–1947. [Google Scholar] [CrossRef]
- Seligman, H.K.; Schillinger, D. Hunger and socioeconomic disparities in chronic disease. N. Engl. J. Med. 2010, 363, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Kent, K.; Schumacher, T.; Kocar, S.; Seivwright, A.; Visentin, D.; Collins, C.E.; Lester, L. Increasing food insecurity severity is associated with lower diet quality. Public Health Nutr. 2024, 27, e61. [Google Scholar] [CrossRef]
- Ranjit, N.; Macias, S.; Hoelscher, D. Factors related to poor diet quality in food insecure populations. Transl. Behav. Med. 2021, 10, 1297–1305. [Google Scholar] [CrossRef]
- Gold, S.L.; Kohler, D.; Freid, H.; Haskey, N.; Raman, M. Food Insecurity Is Common in Patients with Inflammatory Bowel Disease and Is Associated with Increased Ultra-Processed Food Intake. Nutrients 2024, 16, 3736. [Google Scholar] [CrossRef]
- Qasrawi, R.; Sgahir, S.; Nemer, M.; Halaikah, M.; Badrasawi, M.; Amro, M.; Vicuna Polo, S.; Abu Al-Halawa, D.; Mujahed, D.A.; Nasreddine, L.; et al. Investigating the Association between Nutrient Intake and Food Insecurity among Children and Adolescents in Palestine Using Machine Learning Techniques. Children 2024, 11, 625. [Google Scholar] [CrossRef] [PubMed]
- Suksatan, W.; Moradi, S.; Naeini, F.; Bagheri, R.; Mohammadi, H.; Talebi, S.; Mehrabani, S.; Hojjati Kermani, M.A.; Suzuki, K. Ultra-Processed Food Consumption and Adult Mortality Risk: A Systematic Review and Dose-Response Meta-Analysis of 207,291 Participants. Nutrients 2021, 14, 174. [Google Scholar] [CrossRef] [PubMed]
- Moradi, S.; Hojjati Kermani, M.A.; Bagheri, R.; Mohammadi, H.; Jayedi, A.; Lane, M.M.; Asbaghi, O.; Mehrabani, S.; Suzuki, K. Ultra-Processed Food Consumption and Adult Diabetes Risk: A Systematic Review and Dose-Response Meta-Analysis. Nutrients 2021, 13, 4410. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, Z.; Yang, H.; Qiu, P.; Wang, H.; Wang, F.; Zhao, Q.; Fang, J.; Nie, J. Consumption of ultra-processed foods and health outcomes: A systematic review of epidemiological studies. Nutr. J. 2020, 19, 86. [Google Scholar] [CrossRef]
- Rivera, N.; Du, S.; Bernard, L.; Kim, H.; Matsushita, K.; Rebholz, C.M. Ultra-Processed Food Consumption and Risk of Incident Hypertension in US Middle-Aged Adults. J. Am. Heart Assoc. 2024, 13, e035189. [Google Scholar] [CrossRef]
- Maldonado-Pereira, L.; Barnaba, C.; de Los Campos, G.; Medina-Meza, I.G. Evaluation of the nutritional quality of ultra-processed foods (ready to eat + fast food): Fatty acids, sugar, and sodium. J. Food Sci. 2022, 87, 3659–3676. [Google Scholar] [CrossRef] [PubMed]
- Menezes, C.A.; Magalhães, L.B.; da Silva, J.T.; da Silva Lago, R.M.R.; Gomes, A.N.; Ladeia, A.M.T.; Vianna, N.A.; Oliveira, R.R. Ultra-Processed Food Consumption Is Related to Higher Trans Fatty Acids, Sugar Intake, and Micronutrient-Impaired Status in Schoolchildren of Bahia, Brazil. Nutrients 2023, 15, 381. [Google Scholar] [CrossRef]
- Wakasugi, M.; Yokoseki, A.; Wada, M.; Momotsu, T.; Sato, K.; Kawashima, H.; Nakamura, K.; Onodera, O.; Narita, I. Vegetable and Fruit Intake Frequency and Mortality in Patients With and Without Chronic Kidney Disease: A Hospital-Based Cohort Study. J. Ren. Nutr. 2023, 33, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.; Junejo, R. Oxidative Stress in Cardiovascular Diseases. In Biomarkers of Oxidative Stress: Clinical Aspects of Oxidative Stress; Andreescu, S., Henkel, R., Khelfi, A., Eds.; Springer Nature: Cham, Switzerland, 2024; pp. 45–70. [Google Scholar] [CrossRef]
- Fraga, C.G.; Croft, K.D.; Kennedy, D.O.; Tomás-Barberán, F.A. The effects of polyphenols and other bioactives on human health. Food Funct. 2019, 10, 514–528. [Google Scholar] [CrossRef] [PubMed]
- Eggersdorfer, M.; Wyss, A. Carotenoids in human nutrition and health. Arch. Biochem. Biophys. 2018, 652, 18–26. [Google Scholar] [CrossRef]
- Yang, Z.; Zhang, Y.; Gao, J.; Yang, Q.; Qu, H.; Shi, J. Association between dietary magnesium and 10-year risk of a first hard atherosclerotic cardiovascular disease event. Am. J. Med. Sci. 2024, 368, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Peng, J.; Yang, C.; Zhang, W.; Cheng, Z.; Zheng, H. Magnesium intake and all-cause mortality after stroke: A cohort study. Nutr. J. 2023, 22, 54. [Google Scholar] [CrossRef]
- Borges, J.Y.V. The Inverse Association between Potassium Intake and Cardiovascular Disease Risk: A Systematic Review and Meta-Analysis of Prospective Cohort Studies from 2008–2023. Syst. Rev. 2024. [Google Scholar] [CrossRef]
- Ramezani, F.; Pourghazi, F.; Eslami, M.; Gholami, M.; Mohammadian Khonsari, N.; Ejtahed, H.-S.; Larijani, B.; Qorbani, M. Dietary fiber intake and all-cause and cause-specific mortality: An updated systematic review and meta-analysis of prospective cohort studies. Clin. Nutr. 2024, 43, 65–83. [Google Scholar] [CrossRef]
- Gibb, R.D.; McRorie, J.W., Jr.; Russell, D.A.; Hasselblad, V.; D’Alessio, D.A. Psyllium fiber improves glycemic control proportional to loss of glycemic control: A meta-analysis of data in euglycemic subjects, patients at risk of type 2 diabetes mellitus, and patients being treated for type 2 diabetes mellitus. Am. J. Clin. Nutr. 2015, 102, 1604–1614. [Google Scholar] [CrossRef]
- Akhlaghi, M. The role of dietary fibers in regulating appetite, an overview of mechanisms and weight consequences. Crit. Rev. Food Sci. Nutr. 2024, 64, 3139–3150. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Alam, M.J.; Marques, F.Z.; Mackay, C.R. A major mechanism for immunomodulation: Dietary fibres and acid metabolites. Semin. Immunol. 2023, 66, 101737. [Google Scholar] [CrossRef]
- Qi, X.; Li, Y.; Fang, C.; Jia, Y.; Chen, M.; Chen, X.; Jia, J. The associations between dietary fibers intake and systemic immune and inflammatory biomarkers, a multi-cycle study of NHANES 2015–2020. Front. Nutr. 2023, 10, 1216445. [Google Scholar] [CrossRef]
- Campos-Perez, W.; Martinez-Lopez, E. Effects of short chain fatty acids on metabolic and inflammatory processes in human health. Biochim. Biophys. Acta (BBA)-Mol. Cell Biol. Lipids 2021, 1866, 158900. [Google Scholar] [CrossRef]
- Cohn, J.S.; Kamili, A.; Wat, E.; Chung, R.W.S.; Tandy, S. Reduction in intestinal cholesterol absorption by various food components: Mechanisms and implications. Atheroscler. Suppl. 2010, 11, 45–48. [Google Scholar] [CrossRef]
- Sun, Y.; Zhang, H.; Qi, G.; Tian, W. Nutrient deficiency patterns and all-cause and cardiovascular mortality in older adults with hypertension: A latent class analysis. BMC Public Health 2024, 24, 1551. [Google Scholar] [CrossRef] [PubMed]
- Cannon, E.J.; Misialek, J.R.; Buckley, L.F.; Aboelsaad, I.A.F.; Ballantyne, C.M.; Leister, J.; Pankow, J.S.; Lutsey, P.L. Anemia, Iron Deficiency, and Cause-Specific Mortality: The Atherosclerosis Risk in Communities Study. Gerontology 2024, 70, 1023–1032. [Google Scholar] [CrossRef] [PubMed]
- Seligman, H.K.; Laraia, B.A.; Kushel, M.B. Food insecurity is associated with chronic disease among low-income NHANES participants. J. Nutr. 2010, 140, 304–310. [Google Scholar] [CrossRef]
- Vozoris, N.T.; Tarasuk, V.S. Household food insufficiency is associated with poorer health. J. Nutr. 2003, 133, 120–126. [Google Scholar] [CrossRef]
- Casagrande, S.S.; Bullard, K.M.; Siegel, K.R.; Lawrence, J.M. Food insecurity, diet quality, and suboptimal diabetes management among US adults with diabetes. BMJ Open Diabetes Res. Care 2022, 10, e003033. [Google Scholar] [CrossRef]
- Zangiabadi, S.; Alghalyini, B.; Zoubi, F.; Tamim, H. Effect of food insecurity on depression, anxiety, and stress among resettled Syrian refugees in Ontario. PLoS Glob. Public Health 2024, 4, e0002571. [Google Scholar] [CrossRef] [PubMed]
- Xia, W.; Jiang, H.; Di, H.; Feng, J.; Meng, X.; Xu, M.; Gan, Y.; Liu, T.; Lu, Z. Association between self-reported depression and risk of all-cause mortality and cause-specific mortality. J. Affect. Disord. 2022, 299, 353–358. [Google Scholar] [CrossRef]
- Szablewski, L. Insulin Resistance: The Increased Risk of Cancers. Curr. Oncol. 2024, 31, 998–1027. [Google Scholar] [CrossRef] [PubMed]
- Kerr, A.G.; Andersson, D.P.; Dahlman, I.; Rydén, M.; Arner, P. Adipose Insulin Resistance Associates With Dyslipidemia Independent of Liver Resistance and Involves Early Hormone Signaling. Arterioscler. Thromb. Vasc. Biol. 2023, 43, 1054–1065. [Google Scholar] [CrossRef]
- Zeng, J.; Zhang, T.; Yang, Y.; Wang, J.; Zheng, D.; Hou, Y.; Tong, Y.; Fan, X.; Wang, X.; Fang, Y. Association between a metabolic score for insulin resistance and hypertension: Results from National Health and Nutrition Examination Survey 2007–2016 analyses. Front. Endocrinol. 2024, 15, 1369600. [Google Scholar] [CrossRef] [PubMed]
- Arenas, D.J.; Zhou, S.; Thomas, A.; Wang, J.; Arroyo, G.V.; Bash, K. Negative health outcomes associated with food insecurity status in the United States of America: A systematic review of peer-reviewed studies. NutriXiv 2018. [Google Scholar] [CrossRef]
- Jones, A.; Ehsan, A.N.; Saha, S.; Huang, C.-C.; Pillai, N.; Hathi, P.; Vengadassalapathy, S.; Bhat, K.; Ganesh, P.; Chauhan, S.; et al. Incident Food Insecurity and Associated Risk Factors After Surgical Trauma. J. Surg. Res. 2025, 308, 174–182. [Google Scholar] [CrossRef]
- Ramirez-Santana, M. Limitations and Biases in Cohort Studies. In Cohort Studies in Health Sciences; Barría, R.M., Ed.; IntechOpen: Rijeka, Croatia, 2018. [Google Scholar] [CrossRef]
| Outcomes | Certainty Assessment | Effect | Certainty | Importance | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| № of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias | Mean Difference (95% CI) | |||
| Mortality | 19 | Cohort | not serious | serious | serious | not serious | not serious | 1.23 (1.16, 1.30) | ⨁⨁◯◯ LOW | IMPORTANT |
| Quality Score | Adjusted Variables | Main Results | Food Insecurity Assessment Method | Mortality Outcome | Population/ Age (Mean ± SD) /(Women/Men) | Study Design/Follow Up (years)/Source of Data/Health Status | Author (Year; Location) |
|---|---|---|---|---|---|---|---|
| +8/9 | Adherence, CD4 counts, and socioeconomic variables | Food insecurity was associated with increased risk of non-accidental mortality | Radimer/Cornell scale | Non-accidental mortality | N: 1119 41 ± 7.79 years (F: 9%; M: 91%) | Cohort 8.3 years BC drug treatment program HIV-infected individuals on HAART | Weiser et al. (Canada, 2009) [30] |
| +7/9 | NR | Food insecurity was associated with increased risk of mortality. | Radimer/Cornell scale | All-cause mortality | N: 354 38.3 ± 6.71 years (F: 16.9%; M: 83.1%) | Cohort 13 years Provincial HIV/AIDS drug treatment Program administrative database HIV-positive injection drug users | Anema et al. (2013, Canada) [18] |
| +8/9 | Age, gender, education level, homeownership, neighborhood-level income quintile, number of children in the household, and number of adults in the household | Food insecurity was not associated with increased risk of mortality | 18-item HFSSM | All-cause mortality | N: 90,368 51.3 ± 18.7 years (F: 54.9%; M: 45.1%) | Repeated cross-sectional Canada’s Canadian Community Health Survey Community-dwelling adults | Gundersen et al. (Canada, 2018) [23] |
| +8/9 | Demographics, comorbidities, lifestyle variables, and BMI | Food insecurity was associated with increased risk of all-cause mortality | 18-item HFSSM | Mortality | N: 20,918 NR (Mixed) | Cohort 4.5 years NHANES and NDI Community-dwelling adults | Walker et al. (USA, 2019) [29] |
| +8/9 | Age, and gender | Food insecurity was associated with increased risk of mortality, all-cause mortality, and cardiovascular disease mortality | 10-item HFSSM | Mortality All-cause mortality cardiovascular disease mortality | N: 25,247 46.5 ± 34.9 years (F: 52.1%; M: 47.9%) | Cohort 10.2 years NHANES linked mortality file Community-dwelling adults | Banerjee et al. (USA; 2020) [33] |
| +8/9 | Age at death, year of death, sex, race/ethnicity, marital status, education, veteran status, and nativity | Food insecurity was associated with increased risk of opioid-related mortality | NR | Opioid-related mortality | N: 11,818 NR (Mixed) | Cohort 3 years All-age death certificate data Community dwelling adults | Flores et al. (USA, 2020) [21] |
| +8/9 | Age, sex, household income, highest education in household, household type, housing tenure, acute care admission to hospital in the past 2 years, number of self-reported chronic conditions, smoker status, and past-year alcohol consumption history | Food insecurity was associated with increased risk of all-cause premature mortality and all causes of death, except cancers | 18-item HFSSM | All-cause premature mortality cause-specific premature mortality | N: 510,010 32.5 years (F: 54.5%; M: 55.5%) | Cohort 12 years CCHS and CVSD Community-dwelling adults | Men et al. (Canada, 2020) [26] |
| +8/9 | Age, sex, smoking, alcohol, chronic condition, homeowner, education, household type, and indigeneity | Food insecurity was associated with increased risk of pre-65 mortality | 18-item HFSSM | Mortality prior to 65 | N: 354,000 58 ± 3.2 years (F: 53.7%; M: 56.3%) | Cohort 7 years CCHS and CVSD Community-dwelling adults | Men et al. (Canada, 2020) [32] |
| +9/9 | Age, sex, race/ethnicity, education, income, smoking status, alcohol intake, physical activity levels, total energy intake, overall diet quality indicated by Healthy Eating Index 2010 score, baseline diabetes mellitus, hypertension, hypercholesterolemia, and BMI | Food insecurity was not associated with increased risk of cardiovascular disease mortality and stroke mortality | 10-item HFSSM | Cardiovascular disease mortality Stroke mortality | N: 21,178 57.4 ± 14.5 years (F: 47.9%; M: 52.1%) | Cohort 8.5 years NHANES linked mortality file Community-dwelling adults | Sun et al. (USA, 2020) [27] |
| +8/9 | Sex, sociodemographic, and metabolic risk factors | Food insecurity was associated with increased risk of mortality among participants with NAFLD and advanced fibrosis | 18-item HFSSM | All-cause mortality | Adults with NAFLD: N: 4518 48.5 years Adults with advanced fibrosis: N: 1470 65.5 years Total population (F: 51%; M: 49%) | Cohort 4.6 years NHANES linked mortality file Adults with nonalcoholic fatty liver disease (NAFLD) and advanced fibrosis | Kardashian et al. (USA, 2022) [44] |
| +9/9 | Age at diagnosis, sex, race and ethnicity, Elixhauser Comorbidity Index, educational attainment, median household income, Neighbourhood Deprivation Index, type of first-line cancer treatment, cancer type, tumor stage at diagnosis, insurance type, and days between YCLS survey and incident cancer diagnosis | Food insecurity was not associated with increased risk of mortality | Food insecurity was assessed using a single question | All-cause mortality | N: 1151 63.5 ± 18.7 years (F: 59.5%; M: 40.6%) | Cohort 3 years Social risk survey Adults with a new cancer diagnosis | Banegas et al. (2022, USA) [20] |
| +8/9 | Cancer type, cancer stage, urban status, region, marital status, age, sex, and Charlson Comorbidity Index | Food insecurity was associated with increased risk of mortality | 10-item HFSSM | Mortality | N: 46,296 75.6 ± 8.9 years (F: 51.5%; M: 48.5%) | Cohort 5 years Surveillance, Epidemiology, and End Results—Medicare database Patients undergoing surgery for colorectal cancer | Azap et al. (2024, USA) [19] |
| +9/9 | Sociodemographic (age, gender, poverty–income–ratio, marital status, and citizenship status) and health-related characteristics (COPD, diabetes, cardiovascular disease, chronic kidney disease) | Food insecurity was associated with increased risk of all-cause mortality among those with hypertension | 10-item HFSSM | All-cause mortality | Adults with hypertension: N: 1701 56.5 years (F: 55.8%; M: 44.2%) Adults without hypertension: N: 6462 37.8 years (F: 49.3%; M: 50.7%) | Cohort 8.5 years NHANES linked mortality file among adults with/without hypertension | Banerjee et al. (USA, 2024) [42] |
| +9/9 | Age, sex, race and ethnicity, educational attainment, family income, health insurance, marital status, total number of people in the household, immigration status, smoking, heavy drinking, unhealthy diet, physical inactivity, underlying psychological problems, routine place to go for health care, obesity, diabetes, hypertension, cardiovascular disease, and cancer | Food insecurity was associated with increased risk of all-cause premature mortality | 10-item HFSSM | All-cause premature mortality | N: 41,177 47.3 ± 42.6 years (F: 51.3%; M: 48.7%) | Cohort 9.3 years NHANES, and NDI Community-dwelling adults | Ma et al. (USA, 2024) [45] |
| +8/9 | Age, gender, race/ethnicity, education, federal poverty line, marital status, smoking habits, BMI category, diabetes, and CVD | Food insecurity was not associated with increased risk of all-cause mortality, cardiovascular disease mortality, and caner-specific mortality | 10-item HFSSM | All-cause mortality Cardiovascular disease mortality Caner-specific mortality | N: 5032 62.5 ± 21.28 years (F: 58%; M: 42%) | Cohort 6.8 years NHANES linked mortality file Cancer survivors | Hong et al. (USA, 2024) [43] |
| +8/9 | Age, gender, and race/ethnicity | Food insecurity was not associated with increased risk of all-cause mortality, caner-specific mortality, and non-cancer mortality | 18-item HFSSM | All-cause mortality Cancer-specific mortality Non-cancer mortality | N: 5163 NR (F: 57.7%; M: 42.3%) | Cohort 6.7 years NHANES and NDI Cancer survivors | Huang et al. (USA, 2024) [24] |
| +8/9 | Sociodemographic (i.e., age, gender, education, race, income) and health-related characteristics of participants (i.e., health insurance coverage, smoking, obesity, diabetes, and cardiovascular disease). | Individuals with food insecurity but without CKD did not have a higher risk of mortality. Those with both CKD and food insecurity had a significantly higher risk of mortality | 10-item HFSSM | Mortality | N: 13,512 63.6 ± 17.4 years (F: 53.5%; M: 46.5%) | Cohort 9 years NHANES and NDI Adults with chronic kidney disease | Khubchandani et al. (USA, 2024) [25] |
| +9/9 | Age, gender, race/ethnicity, educational level, family income–poverty ratio, smoking status, drinking status, physical activity status, BMI, diabetes, hypertension, heart failure, coronary heart disease, heart attack, stroke, insulin use, hypoglycaemic agents use and HbA1c, high-density lipoprotein, total cholesterol, and systolic and diastolic blood pressure | Food insecurity was associated with increased risk of all-cause mortality | 10-item HFSSM | All-cause mortality Cardiovascular disease mortality Cancer mortality | N: 5749 56.1 ± 12.7 years (F: 47.6%; M: 52.4%) | Cohort 8.5 years NHANES and NDI Adults with diabetes | Fu et al. (USA, 2024) [22] |
| +9/9 | NIHS: Age, sex, and race and ethnicity, stratified by survey cycles, employment, income to poverty ratio, home ownership, education status, health care access, insurance status, married or living with partner, smoking status, and supplemental nutrition assistance program enrollment. NHANES: Age, sex, and race and ethnicity, stratified by survey cycles, employment, income to poverty ratio, home ownership, education status, health care access, insurance status, married or living with partner, and smoking status, BMI, hemoglobin A1c, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, lipid medications, antihypertensive medications, sleep <6 or >8 h per day, and Patient Health Questionnaire-9. | NIHS: Food insecurity was associated with increased risk of all-cause premature mortality, and premature cardiovascular disease mortality NHANES: Food insecurity was not associated with increased risk of all-cause premature mortality and premature cardiovascular disease mortality | 10-item HFSSM 6-item HFSSM 2-item HFSSM | All-cause premature mortality Premature cardiovascular disease mortality | NIHS N: 218,136 44.1 years (F: 51%; M: 49%) NHANES N: 37,027 43.5 years (F: 50.8%; M: 49.1%) | Cohort NIHS and NDI (5 years follow-up) NHANES and NDI (7.8 years follow-up) Community-dwelling adults | Tian et al. (USA, 2025) [28] |
| Sub-Groups | Number of Effect Sizes | Hazard Ratio (95% CI), Pvalue | I2 (%), Pheterogeneity | Pbetween |
|---|---|---|---|---|
| Overall | 19 | 1.23 (1.16, 1.30), <0.001 | 83.1, <0.001 | |
| Level of food insecurity | 0.032 | |||
| Mild | 9 | 1.16 (1.10, 1.22), <0.001 | 0.0, <0.622 | |
| Moderate | 10 | 1.19 (1.07, 1.31), 0.001 | 83.2, <0.001 | |
| Sever | 10 | 1.52 (1.25, 1.86), <0.001 | 94.9, <0.001 | |
| Kind of mortality | <0.001 | |||
| All-cause mortality | 16 | 1.26 (1.18, 1.35), <0.001 | 82.0, <0.001 | |
| Cardiovascular-cause mortality | 7 | 1.24 (1.11, 1.39), <0.001 | 42.8, 0.106 | |
| Cancer-cause mortality | 4 | 1.04 (0.98, 1.11), 0.236 | 0.0, 0.444 | |
| Mean age | 0.023 | |||
| <55 years | 8 | 1.36 (1.21, 1.52), <0.001 | 87.7, <0.001 | |
| >55 years | 8 | 1.13 (1.06, 1.21), <0.001 | 60.4, <0.014 | |
| Not report | 3 | 1.15 (1.05, 1.26), 0.002 | 0.0, 0.339 | |
| Health status | <0.001 | |||
| Healthy population | 10 | 1.25 1.17, 1.34), <0.001 | 85.5, <0.001 | |
| HIV/AIDS patients | 2 | 1.63 (1.18, 2.25), 0.003 | 0.0, 0.481 | |
| Cancer patients | 2 | 1.04 (1.00, 1.09), 0.074 | 0.0, 0.944 | |
| Cancer survivors | 2 | 1.05 (0.89, 1.23), 0.574 | 0.0, 0.547 | |
| Other patients | 3 | 1.30 (1.15, 1.48), <0.001 | 0.0, 0.535 | |
| Food insecurity assessment tools | 0.214 | |||
| HFSSM scale | 15 | 1.22 (1.14, 1.30), <0.001 | 86.2, <0.001 | |
| Radimer/Cornell scale | 2 | 1.63 (1.18, 2.25), <0.001 | 0.0, 0.481 | |
| Other | 2 | 1.20 (1.06, 1.35), <0.001 | 0.0, 0.548 | |
| Age of mortality | 0.472 | |||
| Premature (before 75 years) | 3 | 1.19 (1.14, 1.25), <0.001 | 31.9, 0.194 | |
| Mature (after 75 years) | 16 | 1.24 (1.14, 1.35), <0.001 | 83.5, <0.001 | |
| Follow-up duration | 0.338 | |||
| <10 years | 15 | 1.18 (1.12, 1.22), <0.001 | 63.4, 0.001 | |
| >10 years | 4 | 1.30 (1.07, 1.58), 0.009 | 69.5, 0.020 | |
| Number of participants | 0.957 | |||
| <10,000 | 8 | 1.23 (1.11, 1.36), <0.001 | 26.0, 0.221 | |
| >10,000 | 11 | 1.23 (1.14, 1.32), <0.001 | 89.5, <0.001 | |
| Region | 0.268 | |||
| USA | 14 | 1.07 (0.93, 1.25), 0.349 | 75.8, <0.001 | |
| Canada | 5 | 1.19 (1.07, 1.32), 0.001 | 70.7, <0.001 | |
| COVID 19 pandemic period | 0.207 | |||
| Before (2019 and ago) | 4 | 1.45 (1.15, 1.84), 0.002 | 77.3, 0.004 | |
| During (2019 to 2023) | 7 | 1.19 (1.14, 1.25), <0.001 | 46.7, 0.081 | |
| After (2024 and after) | 8 | 1.16 (1.06, 1.26), 0.001 | 73.1, <0.001 | |
| Adjustments | ||||
| Body mass index | 0.730 | |||
| Yes | 7 | 1.22 (1.13, 1.32), <0.001 | 89.5, <0.001 | |
| No | 12 | 1.24 (1.17, 1.32), 0.311 | 0.0, 0.700 | |
| Smoking status | 0.470 | |||
| Yes | 10 | 1.17 (1.14, 1.20), <0.001 | 72.4, <0.001 | |
| No | 9 | 1.25 (1.05, 1.48), 0.010 | 92.5, <0.001 | |
| Physical activity | 0.751 | |||
| Yes | 4 | 1.24 (1.16, 1.32), <0.001 | 73.1, <0.001 | |
| No | 15 | 1.22 (1.14, 1.31), <0.001 | 86.8, <0.001 | |
| Alcohol intake | 0.733 | |||
| Yes | 4 | 1.20 (1.13, 1.28), 0.001 | 41.5, 0.163 | |
| No | 15 | 1.22 (1.12, 1.33), 0.001 | 86.8, <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jalili, C.; Moosavian, S.P.; Awlqadr, F.H.; Mehrabani, S.; Bagheri, R.; Sedighy, M.; Hodder, S.; Jalili, F.; Ali Hojjati Kermani, M.; Zamir Nasta, M.; et al. The Association of Food Insecurity and Risk of Mortality: A Systematic Review and Meta-Analysis of Large-Scale Cohorts. Nutrients 2025, 17, 1937. https://doi.org/10.3390/nu17111937
Jalili C, Moosavian SP, Awlqadr FH, Mehrabani S, Bagheri R, Sedighy M, Hodder S, Jalili F, Ali Hojjati Kermani M, Zamir Nasta M, et al. The Association of Food Insecurity and Risk of Mortality: A Systematic Review and Meta-Analysis of Large-Scale Cohorts. Nutrients. 2025; 17(11):1937. https://doi.org/10.3390/nu17111937
Chicago/Turabian StyleJalili, Cyrus, Seyedeh Parisa Moosavian, Farhang Hameed Awlqadr, Sanaz Mehrabani, Reza Bagheri, Matin Sedighy, Shirley Hodder, Faramarz Jalili, Mohammad Ali Hojjati Kermani, Maryam Zamir Nasta, and et al. 2025. "The Association of Food Insecurity and Risk of Mortality: A Systematic Review and Meta-Analysis of Large-Scale Cohorts" Nutrients 17, no. 11: 1937. https://doi.org/10.3390/nu17111937
APA StyleJalili, C., Moosavian, S. P., Awlqadr, F. H., Mehrabani, S., Bagheri, R., Sedighy, M., Hodder, S., Jalili, F., Ali Hojjati Kermani, M., Zamir Nasta, M., Moradi, S., & Dutheil, F. (2025). The Association of Food Insecurity and Risk of Mortality: A Systematic Review and Meta-Analysis of Large-Scale Cohorts. Nutrients, 17(11), 1937. https://doi.org/10.3390/nu17111937









