Association of Food-Specific Glycemic Load and Distinct Dietary Components with Gestational Diabetes Mellitus Within a Mediterranean Dietary Pattern: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
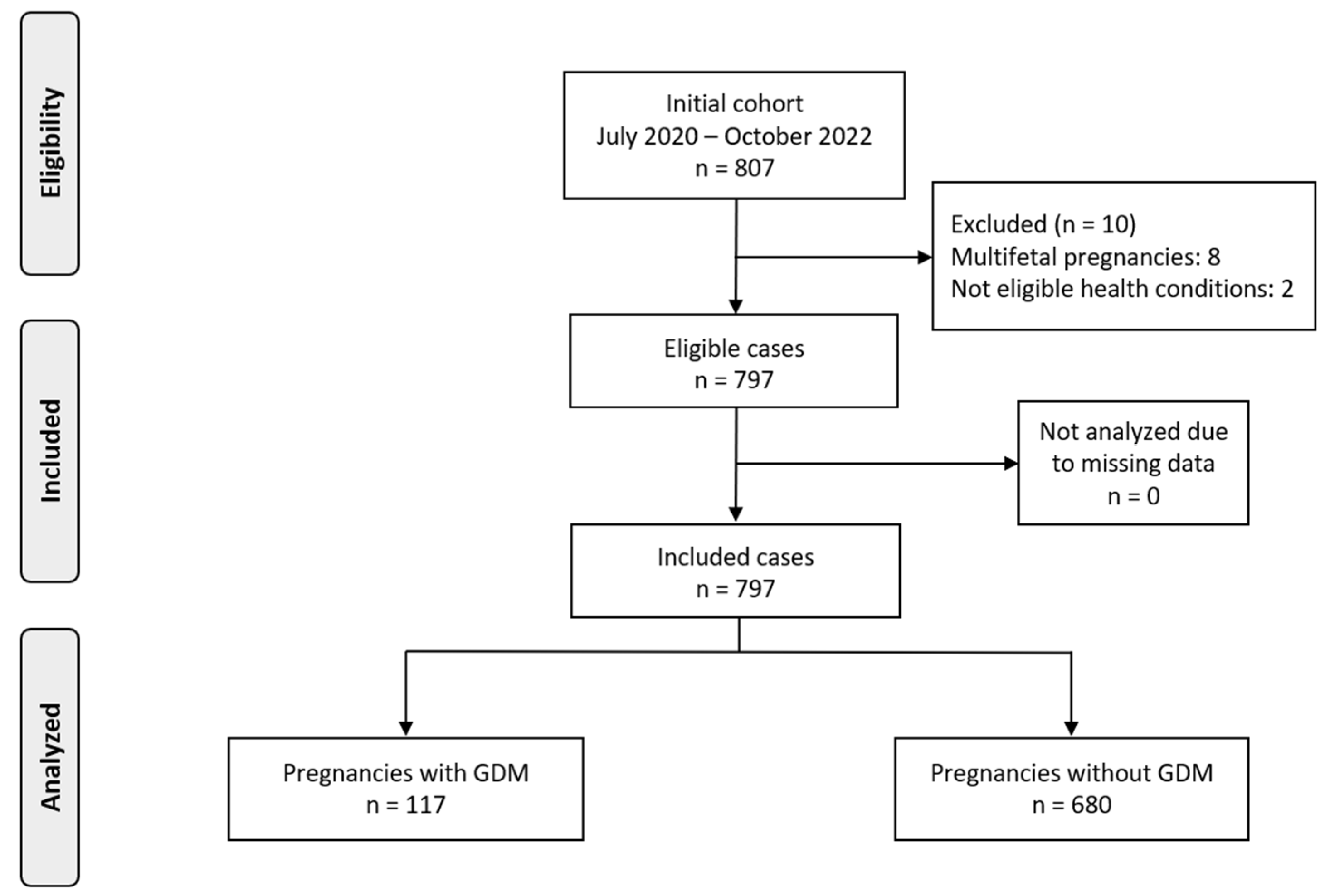
2.1. Population Characteristics
2.2. GDM Diagnosis
2.3. Food Groups from FFQ
2.4. Dietary Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Modzelewski, R.; Stefanowicz-Rutkowska, M.M.; Matuszewski, W.; Bandurska-Stankiewicz, E.M. Gestational diabetes mellitus—Recent literature review. J. Clin. Med. 2022, 11, 5736. [Google Scholar] [CrossRef] [PubMed]
- Vince, K.; Perković, P.; Matijević, R. What is known and what remains unresolved regarding gestational diabetes mellitus (GDM). J. Perinat. Med. 2020, 48, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Farahvar, S.; Walfisch, A.; Sheiner, E. Gestational diabetes risk factors and long-term consequences for both mother and offspring: A literature review. Expert Rev. Endocrinol. Metab. 2019, 14, 63–74. [Google Scholar] [CrossRef]
- Hivert, M.-F.; Backman, H.; Benhalima, K.; Catalano, P.; Desoye, G.; Immanuel, J.; McKinlay, C.J.; Meek, C.L.; Nolan, C.J.; Ram, U. Pathophysiology from preconception, during pregnancy, and beyond. Lancet 2024, 404, 158–174. [Google Scholar] [CrossRef] [PubMed]
- Mustad, V.A.; Huynh, D.T.; López-Pedrosa, J.M.; Campoy, C.; Rueda, R. The role of dietary carbohydrates in gestational diabetes. Nutrients 2020, 12, 385. [Google Scholar] [CrossRef]
- Louie, J.C.Y.; Markovic, T.P.; Ross, G.P.; Foote, D.; Brand-Miller, J.C. Timing of peak blood glucose after breakfast meals of different glycemic index in women with gestational diabetes. Nutrients 2012, 5, 1–9. [Google Scholar] [CrossRef]
- Zhang, Y.; Feng, H.; Li, X.; Chen, Q.; Shao, R.; Wang, C.; Gao, Y. Association of dietary glycemic index and glycemic load with the risk of gestational diabetes mellitus: A systematic review and dose-response meta-analysis. Gynecol. Endocrinol. 2024, 40, 2375564. [Google Scholar] [CrossRef]
- Agnoli, C.; Pounis, G.; Krogh, V. Dietary pattern analysis. In Analysis in Nutrition Research; Elsevier: Amsterdam, The Netherlands, 2019; pp. 75–101. [Google Scholar]
- Zhang, Y.; Xia, M.; Weng, S.; Wang, C.; Yuan, P.; Tang, S. Effect of Mediterranean diet for pregnant women: A meta-analysis of randomized controlled trials. J. Matern.-Fetal Neonatal Med. 2022, 35, 4824–4829. [Google Scholar] [CrossRef]
- Assaf-Balut, C.; García de la Torre, N.; Durán, A.; Fuentes, M.; Bordiú, E.; Del Valle, L.; Familiar, C.; Ortolá, A.; Jiménez, I.; Herraiz, M.A. A Mediterranean diet with additional extra virgin olive oil and pistachios reduces the incidence of gestational diabetes mellitus (GDM): A randomized controlled trial: The St. Carlos GDM prevention study. PLoS ONE 2017, 12, e0185873. [Google Scholar] [CrossRef]
- Fernández-González, E.; Martínez-González, M.Á.; Bes-Rastrollo, M.; Suescun-Elizalde, D.; Basterra-Gortari, F.J.; Santiago, S.; Gea, A. Association between pre-conceptional carbohydrate quality index and the incidence of gestational diabetes: The SUN cohort study. Br. J. Nutr. 2023, 129, 704–714. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Aminianfar, A.; Soltani, S.; Hajianfar, H.; Azadbakht, L.; Shahshahan, Z.; Esmaillzadeh, A. The association between dietary glycemic index and load and risk of gestational diabetes mellitus: A prospective study. Diabetes Res. Clin. Pract. 2020, 170, 108469. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Gong, Y.; Della Corte, K.; Yu, D.; Xue, H.; Shan, S.; Tian, G.; Liang, Y.; Zhang, J.; He, F. Relevance of dietary glycemic index, glycemic load and fiber intake before and during pregnancy for the risk of gestational diabetes mellitus and maternal glucose homeostasis. Clin. Nutr. 2021, 40, 2791–2799. [Google Scholar] [CrossRef]
- Tranidou, A.; Tsakiridis, I.; Magriplis, E.; Apostolopoulou, A.; Chroni, V.; Tsekitsidi, E.; Kalaitzopoulou, I.; Pazaras, N.; Chourdakis, M.; Dagklis, T. Maternal Macronutrient Intake and Associated Risk for Gestational Diabetes Mellitus: Results from the BORN2020 Study. Biomedicines 2024, 13, 57. [Google Scholar] [CrossRef] [PubMed]
- Coustan, D.R.; Lowe, L.P.; Metzger, B.E.; Dyer, A.R. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: Paving the way for new diagnostic criteria for gestational diabetes mellitus. Am. J. Obstet. Gynecol. 2010, 202, 654.e1–654.e6. [Google Scholar] [CrossRef]
- Apostolopoulou, A.; Magriplis, E.; Tsekitsidi, E.; Oikonomidou, A.C.; Papaefstathiou, E.; Tsakiridis, I.; Dagklis, T.; Chourdakis, M. Development and validation of a short culture-specific food frequency questionnaire for Greek pregnant women and their adherence to the Mediterranean diet. Nutrition 2021, 90, 111357. [Google Scholar] [CrossRef]
- Foster-Powell, K.; Holt, S.H.; Brand-Miller, J.C. International table of glycemic index and glycemic load values: 2002. Am. J. Clin. Nutr. 2002, 76, 5–56. [Google Scholar] [CrossRef]
- Khani, B.R.; Wolk, A.; Ye, W.; Terry, P. Reproducibility and validity of major dietary patterns among Swedish women assessed with a food-frequency questionnaire. J. Nutr. 2004, 134, 1541–1545. [Google Scholar] [CrossRef]
- Hu, J.; Oken, E.; Aris, I.M.; Lin, P.-I.D.; Ma, Y.; Ding, N.; Gao, M.; Wei, X.; Wen, D. Dietary patterns during pregnancy are associated with the risk of gestational diabetes mellitus: Evidence from a Chinese prospective birth cohort study. Nutrients 2019, 11, 405. [Google Scholar] [CrossRef]
- Schoenaker, D.A.; Soedamah-Muthu, S.S.; Callaway, L.K.; Mishra, G.D. Pre-pregnancy dietary patterns and risk of gestational diabetes mellitus: Results from an Australian population-based prospective cohort study. Diabetologia 2015, 58, 2726–2735. [Google Scholar] [CrossRef]
- Ebrahimi, S.; Ellery, S.J.; Leech, R.M.; van der Pligt, P.F. Associations between diet quality and dietary patterns and gestational diabetes mellitus in a low-risk cohort of pregnant women in Australia: A cross-sectional study. J. Hum. Nutr. Diet. 2024, 37, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Quan, W.; Zeng, M.; Jiao, Y.; Li, Y.; Xue, C.; Liu, G.; Wang, Z.; Qin, F.; He, Z.; Chen, J. Western dietary patterns, foods, and risk of gestational diabetes mellitus: A systematic review and meta-analysis of prospective cohort studies. Adv. Nutr. 2021, 12, 1353–1364. [Google Scholar] [CrossRef]
- Chen, Q.; Wu, W.; Yang, H.; Zhang, P.; Feng, Y.; Wang, K.; Wang, Y.; Wang, S.; Zhang, Y. A vegetable dietary pattern is associated with lowered risk of gestational diabetes mellitus in Chinese women. Diabetes Metab. J. 2020, 44, 887–896. [Google Scholar] [CrossRef] [PubMed]
- Jaworsky, K.; DeVillez, P.; Alexander, J.M.; Basu, A. Effects of an eating pattern including colorful fruits and vegetables on management of gestational diabetes: A randomized controlled trial. Nutrients 2023, 15, 3624. [Google Scholar] [CrossRef]
- Gao, Q.; Zhong, C.; Zhou, X.; Chen, R.; Xiong, T.; Hong, M.; Li, Q.; Kong, M.; Xiong, G.; Han, W. Inverse association of total polyphenols and flavonoids intake and the intake from fruits with the risk of gestational diabetes mellitus: A prospective cohort study. Clin. Nutr. 2021, 40, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Tryggvadottir, E.A.; Halldorsson, T.I.; Landberg, R.; Hrolfsdottir, L.; Birgisdottir, B.E.; Magnusdottir, O.K.; Hreidarsdottir, I.T.; Hardardottir, H.; Gunnarsdottir, I. Higher Alkylresorcinol concentrations, a consequence of Whole-Grain intake, are inversely associated with gestational diabetes mellitus in Iceland. J. Nutr. 2021, 151, 1159–1166. [Google Scholar] [CrossRef]
- Xu, J.; Wang, H.; Bian, J.; Xu, M.; Jiang, N.; Luo, W.; Zu, P.; Yin, W.; Zhu, P. Association between the maternal mediterranean diet and perinatal outcomes: A systematic review and meta-analysis. Adv. Nutr. 2024, 15, 100159. [Google Scholar] [CrossRef]
- Karamanos, B.; Thanopoulou, A.; Anastasiou, E.; Assaad-Khalil, S.; Albache, N.; Bachaoui, M.; Slama, C.B.; El Ghomari, H.; Jotic, A.; Lalic, N. Relation of the Mediterranean diet with the incidence of gestational diabetes. Eur. J. Clin. Nutr. 2014, 68, 8–13. [Google Scholar] [CrossRef]
- Olmedo-Requena, R.; Gómez-Fernández, J.; Amezcua-Prieto, C.; Mozas-Moreno, J.; Khan, K.S.; Jiménez-Moleón, J.J. Pre-pregnancy adherence to the Mediterranean diet and gestational diabetes mellitus: A case-control study. Nutrients 2019, 11, 1003. [Google Scholar] [CrossRef]
- Tsarna, E.; Eleftheriades, A.; Tsomi, E.; Ziogou, G.; Vakas, P.; Panoskaltsis, T.; Christopoulos, P. The Role of Diet during Pregnancy in Protecting against Gestational Diabetes Mellitus in a Population with Mediterranean Dietary Habits: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 1857. [Google Scholar] [CrossRef]
- Verbeke, W.; De Bourdeaudhuij, I. Dietary behaviour of pregnant versus non-pregnant women. Appetite 2007, 48, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Arista, D.M.; Amelia, R.; Fitriani, D.; Khotimah, H.; Ratnaningrum, S.D.; Irwanto, Y.; Nurseta, T. Gestational Diabetes Mellitus: An overview and its potential treatment with herbs. GSC Biol. Pharm. Sci. 2023, 23, 261–273. [Google Scholar] [CrossRef]
- Hinkle, S.N.; Laughon, S.K.; Catov, J.M.; Olsen, J.; Bech, B.H. First trimester coffee and tea intake and risk of gestational diabetes mellitus: A study within a national birth cohort. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 420–428. [Google Scholar] [CrossRef]
- Li, F.; Sun, H.; Dong, H.-L.; Zhang, Y.-Q.; Pang, X.-X.; Cai, C.-J.; Bai, D.; Wang, P.-P.; Yang, M.-Y.; Zeng, G. Starchy vegetable intake in the first trimester is associated with a higher risk of gestational diabetes mellitus: A prospective population-based study. J. Matern.-Fetal Neonatal Med. 2022, 35, 6794–6801. [Google Scholar] [CrossRef]
- Zhou, X.; Chen, R.; Zhong, C.; Wu, J.; Li, X.; Li, Q.; Cui, W.; Yi, N.; Xiao, M.; Yin, H. Fresh fruit intake in pregnancy and association with gestational diabetes mellitus: A prospective cohort study. Nutrition 2019, 60, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.-Q.; Lu, Y.; Xu, M.; Huang, J.; Su, Y.-X.; Zhang, C.-X. Excessive fruit consumption during the second trimester is associated with increased likelihood of gestational diabetes mellitus: A prospective study. Sci. Rep. 2017, 7, 43620. [Google Scholar] [CrossRef]
- Li, H.; Xie, S.; Zhang, X.; Xia, Y.; Zhang, Y.; Wang, L. Mid-pregnancy consumption of fruit, vegetable and fruit juice and the risk of gestational diabetes mellitus: A correlation study. Clin. Nutr. ESPEN 2021, 46, 505–509. [Google Scholar] [CrossRef]
- Goran, M.; Plows, J.; Ventura, E. Effects of consuming sugars and alternative sweeteners during pregnancy on maternal and child health: Evidence for a secondhand sugar effect. Proc. Nutr. Soc. 2019, 78, 262–271. [Google Scholar] [CrossRef]
- Huang, L.; Huang, Y.; Zhang, H.; Lyu, C. Correlation Analyses of the Consumption of Artificial Sweeteners During Pregnancy and the Incidence of Gestational Diabetes Mellitus. Diabetes Metab. Syndr. Obes. 2025, 18, 1527–1538. [Google Scholar] [CrossRef]
- Campos, P.; Rebolledo, N.; Durán, S.; Flores, M.; Reyes, M.; Garmendia, M.L. Association between consumption of non-nutritive sweeteners and gestational diabetes mellitus in Chilean pregnant women: A secondary data analysis of the CHiMINCs-II cohort. Nutrition 2024, 128, 112560. [Google Scholar] [CrossRef]
- Mahjoub, F.; Jemaa, H.B.; Sabeh, F.B.; Amor, N.B.; Gamoudi, A.; Jamoussi, H. Impact of nutrients and Mediterranean diet on the occurrence of gestational diabetes. Libyan J. Med. 2021, 16. [Google Scholar] [CrossRef]
- Pouladi, F.; Nozari, E.; Hosseinzadeh, F.; Hashemi, S. The protective association of dairy intake and the adverse impact of iron on gestational diabetes risk. Int. J. Vitam. Nutr. Res. 2024, 94, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Schoenaker, D.A.; Mishra, G.D.; Callaway, L.K.; Soedamah-Muthu, S.S. The role of energy, nutrients, foods, and dietary patterns in the development of gestational diabetes mellitus: A systematic review of observational studies. Diabetes Care 2016, 39, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Jacques, P.F.; Tucker, K.L. Are dietary patterns useful for understanding the role of diet in chronic disease? Am. J. Clin. Nutr. 2001, 73, 1–2. [Google Scholar] [CrossRef]
- Aune, D.; Ursin, G.; Veierød, M. Meat consumption and the risk of type 2 diabetes: A systematic review and meta- analysis of cohort studies. Diabetologia 2009, 52, 2277–2287. [Google Scholar] [CrossRef]
| Maternal Characteristics | GDM (N = 117) | Non-GDM (N = 680) | p-Value |
|---|---|---|---|
| Maternal Age (years) | 34.15 (±4.48) | 32.1 (±4.89) | p < 0.0001 * |
| Maternal Age > 35 (%) | 51 (43.59%) | 186 (27.35%) | p < 0.001 * |
| Pre-pregnancy BMI (kg/m2) | 23.7 (21.7, 28.5) | 22.7 (20.8, 26.02) | 0.004 * |
| Pre-pregnancy BMI < 18.5 (%) | 2 (1.71%) | 28 (4.12%) | 0.32 |
| Pre-pregnancy BMI 18.5–24.9 (%) | 69 (58.97%) | 438 (64.41%) | 0.31 |
| Pre-pregnancy BMI 25–29.9 (%) | 46 (39.32%) | 214 (31.47%) | 0.12 |
| Pre-pregnancy BMI ≥ 30 (%) | 25 (21.37%) | 75 (11.03%) | 0.003 * |
| BMI < 18.5 during pregnancy | 1 (0.855%) | 20 (2.94%) | 0.32 |
| BMI 18.5–24.9 during pregnancy | 66 (56.41%) | 422 (62.06%) | 0.29 |
| BMI 25–29.9 during pregnancy | 20 (17.09%) | 157 (23.09%) | 0.19 |
| BMI ≥ 30 during pregnancy | 30 (25.64%) | 81 (11.91%) | p < 0.001 * |
| Smoking (%) | 21 (17.95%) | 60 (8.82%) | 0.004 * |
| Parity | |||
| 0 | 60 (51.28%) | 347 (51.03%) | 1 |
| 1 | 44 (37.61%) | 253 (37.21%) | 1 |
| 2 | 12 (10.26%) | 69 (10.15%) | 1 |
| 3 | 1 (0.855%) | 9 (1.32%) | 1 |
| 4 | 0 (0%) | 2 (0.294%) | - |
| ART (%) | 11 (9.4%) | 48 (7.06%) | 0.48 |
| Thyroid Disease (%) | 13 (11.11%) | 93 (13.68%) | 0.54 |
| Time Period | Adherence to MD | GDM (N = 117) | Non-GDM (N = 680) | p-Value |
|---|---|---|---|---|
| Pre-pregnancy (A) | Total MD Score (median, IQR) | 4 (3, 6) | 5 (3, 6) | 0.58 |
| Low adherence (%) | N = 61 (52.14%) | N = 332 (48.82%) | 0.57 | |
| Medium adherence (%) | N = 19 (16.24%) | N = 141 (20.74%) | 0.32 | |
| High adherence (%) | N = 37 (31.62%) | N = 207 (30.44%) | 0.88 | |
| During pregnancy (B) | Total MD Score (median, IQR) | 5 (4, 6) | 5 (3, 6) | 0.45 |
| Low adherence (%) | N = 50 (42.74%) | N = 317 (46.62%) | 0.5 | |
| Medium adherence (%) | N = 30 (25.64%) | N = 159 (23.38%) | 0.68 | |
| High adherence (%) | N = 37 (31.62%) | N = 204 (30%) | 0.81 |
| Time Period | Factor | Dominant Food Groups | Pattern Type | Variance Explained (%) |
|---|---|---|---|---|
| A | Factor 1 | Non-refined products and grains, fruits, boiled salad, legumes, nuts and olives and oil | Whole plant-based | 6.79% |
| Factor 2 | Sugary sweets and sugar beverages, vegetables, nuts and olives and oil, animal fats, ultra processed foods and cold cuts and refined | Processed/sweet | 5.24% | |
| Factor 3 | Beverages | Beverage-heavy | 3.47% | |
| B | Factor 1 | Fresh juice, vegetables, fruits, legumes, nuts and olives and oil | Plant-rich with juice | 5.12% |
| Factor 2 | Sugary sweets and sugar beverages, animal fats, ultra processed foods and cold cuts and refined | Western/processed | 4.82% | |
| Factor 3 | Sugar alternatives | Sweetener-focused | 2.28% |
| MD Adherence | Time Period | Factor | Dominant Foods | Association | aOR (95% CI) | p-Value | Power (aOR) |
|---|---|---|---|---|---|---|---|
| High | Pre-pregnancy (A) | 3–A | Beverages | ↑ Risk | 1.96 (1.31–3.02) | 0.001 * | 1 |
| Medium | During pregnancy (B) | 1–B | Fresh juice, vegetables, fruits, legumes, nuts and olives and oil | ↑ Risk | 2.91 (1.50–6.24) | 0.003 * | 1 |
| Medium | During pregnancy (B) | 2–B | Sugary sweets & sugar beverages, animal fats, ultra processed foods & cold cuts & refined | ↓ Risk | 0.34 (0.17–0.64) | 0.001 * | 1 |
| Medium | During pregnancy (B) | 3–B | Sugar alternatives | ↑ Risk | 4.94 (1.48–19.36) | 0.014 * | 1 |
| Low | During pregnancy (B) | 3–B | Sugar alternatives | ↑ Risk | 2.16 (1.23–3.85) | 0.008 * | 1 |
| Time Period | MD Adherence | Food Group | aOR (95% CI) | p-Value | Power (aOR) |
|---|---|---|---|---|---|
| A | High | Boiled salad | 0.09 (0.01–0.73) | 0.032 * | 1 |
| B | High | Boiled salad | 0.11 (0.01–0.76) | 0.039 * | 1 |
| A | Medium | Ultra processed and Cold cuts and refined | 0.99 (0.99–0.99) | 0.037 * | 0.05 |
| B | Medium | Fruits | 1.03 (1, 1.07) | 0.022 * | 0.062 |
| A | Low | Non-refined products and grains | 1.02 (1.01–1.03) | <0.001 *** | 0.064 |
| B | Low | Non-refined products and grains | 1.01 (1, 1.02) | 0.005 ** | 0.057 |
| A | Low | Ultra processed and Cold cuts and refined | 0.99 (0.99–0.99) | 0.027 * | 0.05 |
| A | Non-stratified | Boiled salad | 0.19 (0.05–0.63) | 0.008 ** | 1 |
| A | Non-stratified | Non-refined products and grains | 1.01 (1.00–1.02) | 0.005 ** | 0.059 |
| A | Non-stratified | Ultra processed and Cold cuts and refined | 0.99 (0.99–0.99) | 0.021 * | 0.05 |
| B | Non-stratified | Non-refined products and grains | 1.01 (1.00–1.02) | 0.002 ** | 0.058 |
| B | Non-stratified | Ultra processed and Cold cuts and refined | 0.99 (0.99–0.99) | 0.037 * | 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tranidou, A.; Siargkas, A.; Magriplis, E.; Tsakiridis, I.; Kripouri, P.; Apostolopoulou, A.; Chourdakis, M.; Dagklis, T. Association of Food-Specific Glycemic Load and Distinct Dietary Components with Gestational Diabetes Mellitus Within a Mediterranean Dietary Pattern: A Prospective Cohort Study. Nutrients 2025, 17, 1917. https://doi.org/10.3390/nu17111917
Tranidou A, Siargkas A, Magriplis E, Tsakiridis I, Kripouri P, Apostolopoulou A, Chourdakis M, Dagklis T. Association of Food-Specific Glycemic Load and Distinct Dietary Components with Gestational Diabetes Mellitus Within a Mediterranean Dietary Pattern: A Prospective Cohort Study. Nutrients. 2025; 17(11):1917. https://doi.org/10.3390/nu17111917
Chicago/Turabian StyleTranidou, Antigoni, Antonios Siargkas, Emmanouela Magriplis, Ioannis Tsakiridis, Panagiota Kripouri, Aikaterini Apostolopoulou, Michail Chourdakis, and Themistoklis Dagklis. 2025. "Association of Food-Specific Glycemic Load and Distinct Dietary Components with Gestational Diabetes Mellitus Within a Mediterranean Dietary Pattern: A Prospective Cohort Study" Nutrients 17, no. 11: 1917. https://doi.org/10.3390/nu17111917
APA StyleTranidou, A., Siargkas, A., Magriplis, E., Tsakiridis, I., Kripouri, P., Apostolopoulou, A., Chourdakis, M., & Dagklis, T. (2025). Association of Food-Specific Glycemic Load and Distinct Dietary Components with Gestational Diabetes Mellitus Within a Mediterranean Dietary Pattern: A Prospective Cohort Study. Nutrients, 17(11), 1917. https://doi.org/10.3390/nu17111917








