Triathlon: Ergo Nutrition for Training, Competing, and Recovering
Abstract
1. Introduction
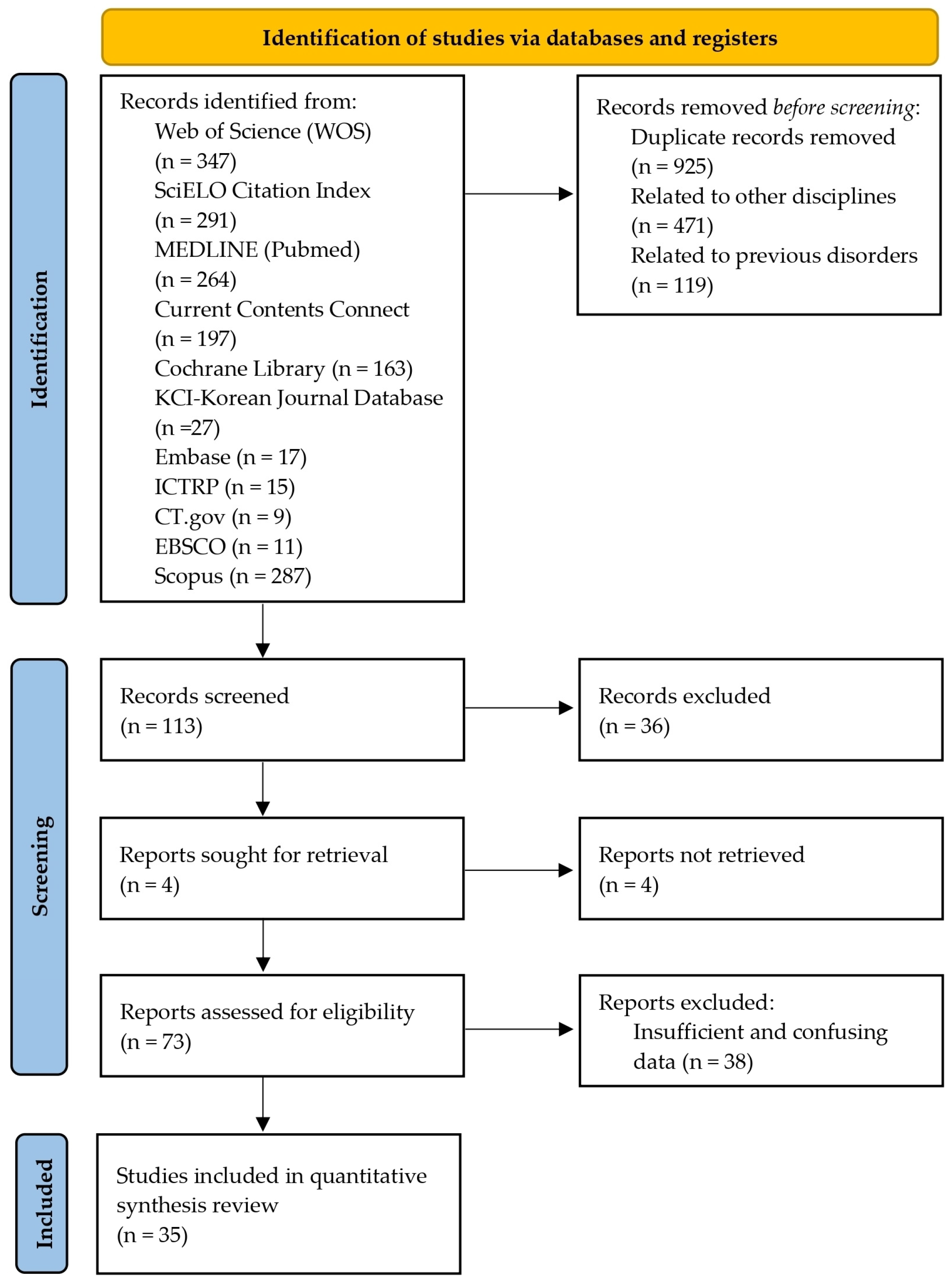
2. Materials and Methods
2.1. Sources of Information
2.2. Study Selection
2.3. Data Extraction
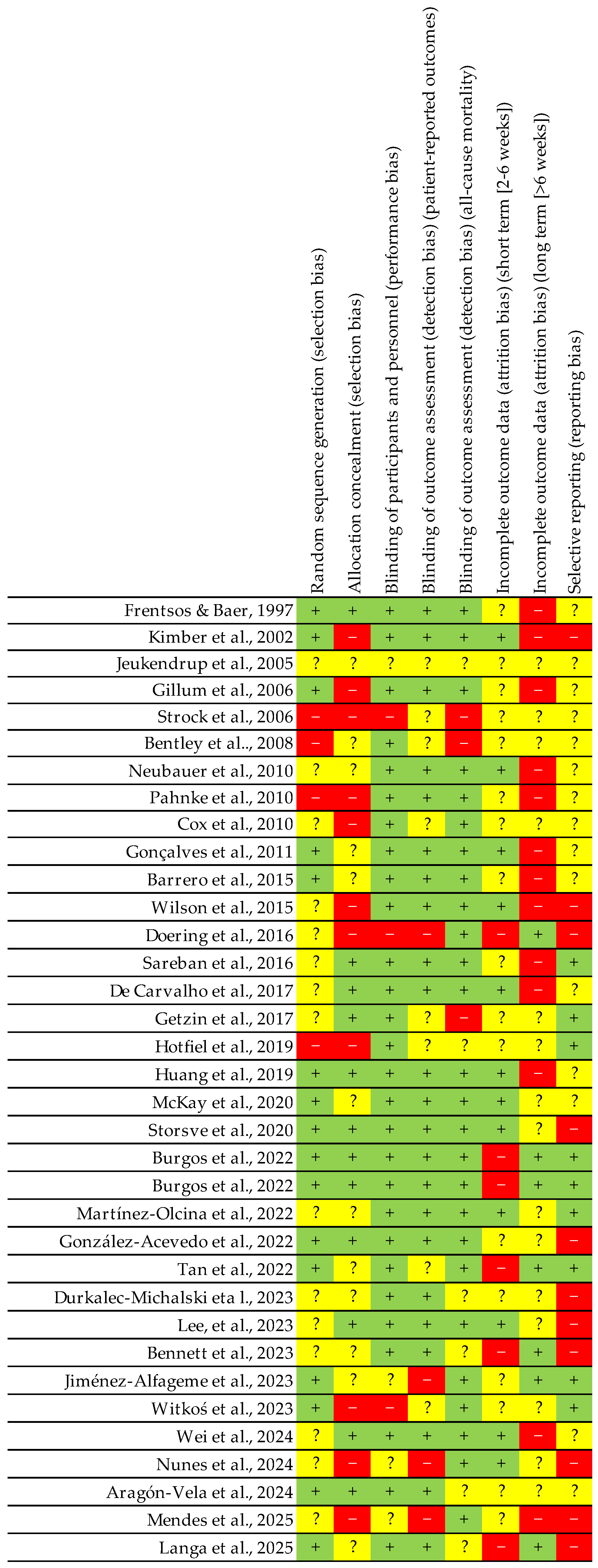
2.4. Assessing the Quality of Experiments: Risk of Bias
3. Results
3.1. Assessing the Quality of Experiments: Risk of Bias and Levels of Evidence
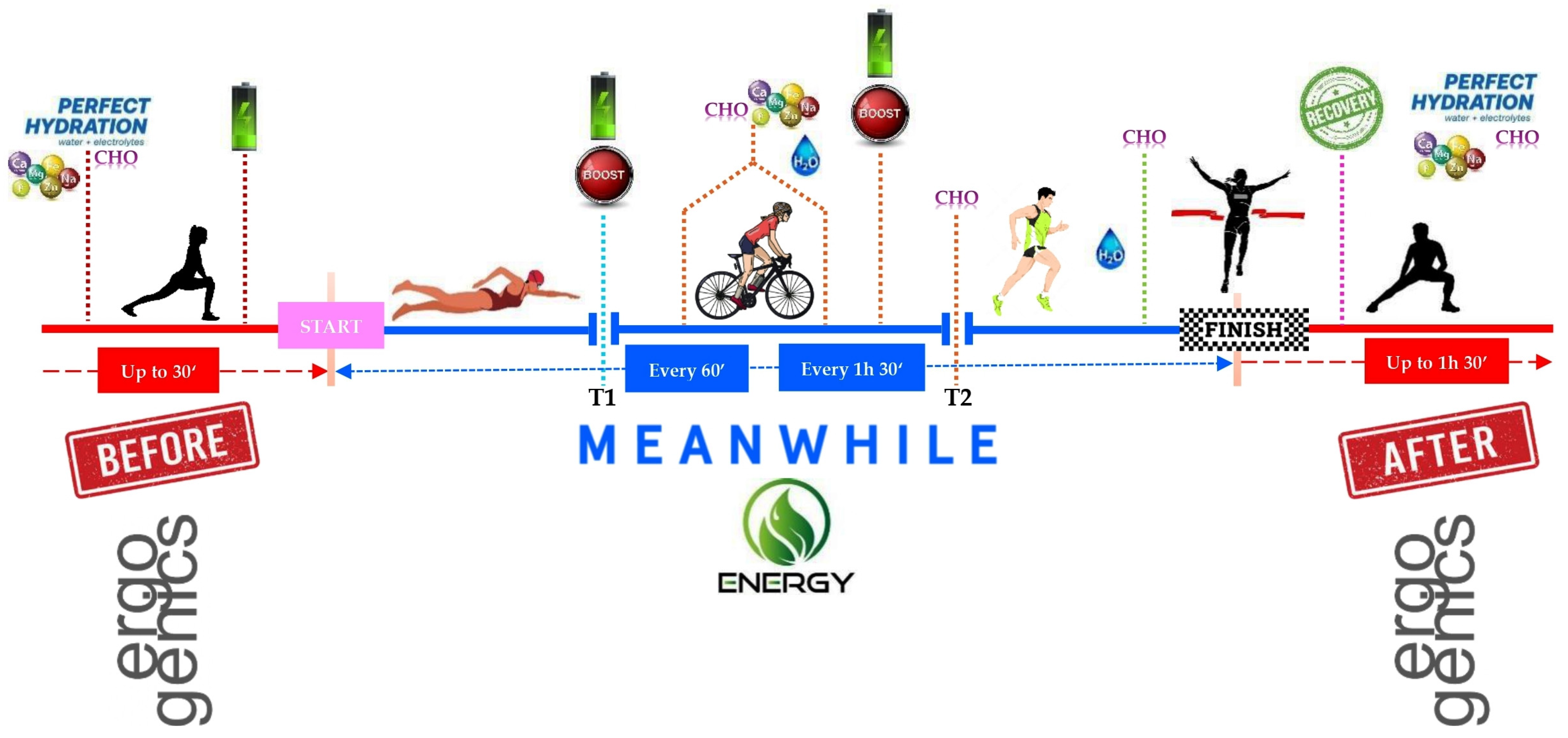
3.2. Nutritional Strategies
3.3. Recovery
3.4. Ergogenic Supplementation
4. Discussion
4.1. Nutritional Strategies
- Individualisation: Each athlete has different metabolic needs, GI tolerances and cultural or personal preferences [101].
- Previous practice: All strategies should be tested during long training sessions to avoid surprises in competition.
- Environmental factors: Altitude, temperature and humidity affect water and energy requirements. For example, hot environments increase water loss.
4.2. Recovery
- -
- Muscle repair: Intense activity can cause microlesions in muscle fibres, particularly following high-intensity or high-volume sessions [103]. The repair process requires protein synthesis, controlled inflammation, and the removal of residual metabolic products [104]. With regard to protein synthesis, Bentley et al. (2008) [58] also noted that protein intake is necessary for muscle recovery and glycogen resynthesis.
- -
- Glycogen replenishment: It is critical to replenish muscle and liver glycogen in order to maintain performance in subsequent sessions [90]. Post-exercise CHO ingestion accelerates this process [95]. Frentsos and Baer (1997) [53] reported that dietary strategies combining increased carbohydrate and protein intake can improve recovery rates. Jeukendrup et al. (2005) [55] recommended 1.0–1.2 g/kg CHO per hour for post-exercise recovery to optimise glycogen synthesis.
- -
- Restoring Fluid and Electrolyte Balance: The loss of fluids and electrolytes during exercise can affect neuromuscular and metabolic function [105]. Adequate hydration can help to prevent cramps and premature fatigue [106]. Jeukendrup et al. (2005) [55] have already suggested that drinks containing sodium (Na) at concentrations of 30–50 mmol/L facilitate water absorption and prevent hyponatraemia. Bentley et al. (2008) [58] pointed out that maintaining fluid balance before and after exercise is important for delaying fatigue and improving recovery. Aragón-Vela et al. (2024) [84] conducted a study on hydration using mineral-rich deep seawater (DSW) and found that DSW could help maintain muscle strength during isometric exercise.
- -
- -
- Training intensity and volume: Excessive training without adequate recovery can lead to overtraining syndrome, chronic fatigue and reduced performance [109].
- -
- -
- Nutrition: A balanced diet containing sufficient calories, protein, CHO and micronutrients is essential for facilitating repair processes [112].
- -
- -
- Post-exercise nutrition: It is recommended that you consume a combination of carbohydrates and proteins within the first few hours after exercise [115]. For example, a 3:1 or 4:1 ratio of CHO to protein can increase protein synthesis and replenish glycogen stores [116]. Faster muscle recovery can also be achieved by taking 3 g/day of citrulline (CIT) and 300 mg/day of nitrate-rich beetroot extract (BRG), which may promote faster recovery [73]. However, this does not prevent exercise-induced muscle damage (EIMD) [117].
- -
- Hydration: Maintaining electrolyte balance involves drinking fluids with electrolytes according to estimated losses [118].
- -
- Recovery techniques: Sports massage can reduce muscle soreness and improve circulation [119]; cryotherapy can reduce inflammation [120]; and gentle stretching can help maintain flexibility [121]. Post-exercise compression appears to reduce muscle damage (Hotfiel et al., 2019 [69]), while cold water immersion is effective in reducing delayed-onset muscle soreness (DOMS) and inflammation; however, it may interfere with muscle glycogen recovery [69].
- -
- Adequate sleep: Prioritising a good night′s sleep is key. Some research suggests that sleeping for 7–9 h promotes the anabolic processes necessary for recovery [122].
- -
- Inadequate recovery can result in:
- -
- Overtraining: A condition characterised by persistent fatigue, reduced performance, and hormonal imbalances [123].
- -
- Overuse injuries: Tendinitis, stress fractures and muscle injuries often occur when proper tissue repair is not permitted [124].
- -
- Impaired immune system: Increased susceptibility to respiratory infections and other illnesses [125].
4.3. Ergogenic Supplements: Scientific Evidence
- a.
- CHO
- b.
- Electrolytes
- c.
- Proteins and amino acids
- d.
- Creatine
- e.
- Caffeine
- f.
- Beta-alanine
- g.
- Nitrates
- -
- -
- Some studies have shown that nitrate supplementation can increase aerobic capacity and delay fatigue, enabling athletes to maintain a higher pace for longer [174], which is crucial in triathlons.
- -
- -
- There is stronger evidence in endurance sports such as cycling and running, but studies also suggest potential benefits in combined events such as triathlons [177].
- -
- Most studies utilise nitrate doses ranging from 300 to 600 milligrams, typically administered two to three hours prior to physical exertion, with the aim of optimising the nitrate′s effects. Examples of sources of nitrate include beetroot juice [178].
- -
- Although nitrate supplementation is generally considered safe at the recommended doses, it is advisable to consult a professional beforehand, particularly if you have pre-existing medical conditions [174].
- h.
- Taurine
- i.
- Probiotics
- j.
- Seawater
- k.
- Krill oil
- I.
- Carbohydrates: Consuming them during prolonged exercise significantly increases the time it takes to become fatigued [199].
- II.
- Electrolytes: Adequate replenishment prevents cramps and maintains neuromuscular function [134].
- III.
- Caffeine: Significant improvements in race times were observed when caffeine was administered in moderate doses [200].
- Decreased performance: A deficiency in carbohydrates can lead to a reduction in muscle and liver glycogen stores, which can subsequently affect endurance during the event.
- Lack of protein or micronutrients has been shown to lead to slower muscle recovery and an increased chance of injury.
- There is a risk of dehydration or hyponatraemia. Poor hydration management has been shown to increase the risk of dangerous complications.
- GI issues: It has been demonstrated that ingesting specific foods or supplements in quantities that exceed recommended levels can result in adverse effects during competitive events.
- The long-term health implications of the following factors must be given due consideration: It is important to note that malnutrition and deficiencies can affect athletes’ overall well-being.
5. Strengths, Limitations, Future Research Lines, Practical Applications
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| ∃ | there is |
| ∄ | there is not |
| - | reduction |
| [] | concentration |
| + | increase |
| < | lesser |
| > | greater |
| ≠ | differences |
| ± | similar |
| 1-MAT | 1-Min Abdominal Test |
| AA | amino acid |
| ABS | agriculture and biological sciences |
| aED | absolute energy deficit |
| aEI | absolute energy intake |
| Ae | Aerobic |
| AIS | Australian Institute of Sport |
| An | anaerobic |
| Anthp | anthropometry |
| aTEE | absolute total energy expenditure |
| B | balance |
| BC | body composition |
| BCAAs | branched-chain amino acids |
| BE | beet extract |
| BF | body fat |
| BI | biochemical indices |
| BM | body mass |
| BMI | BMI |
| BW | body weight |
| BP | blood pressure |
| C | cortisol |
| Ca | calcium |
| CCI | intraclass correlation coefficient |
| CFU | colony-forming units |
| CHO | carbohydrates |
| Ci | citrulline |
| CK | creatine kinase |
| CMJ | countermovement jump |
| Ct | Cooper test |
| CWI | Cold Water Immersion Therapy |
| Cu | Copper |
| DB | data base |
| DOMS | delayed onset muscle soreness |
| DMG | dimethylglycine |
| DSW | deep-sea water |
| DYN | Handgrip Dynamometer Test |
| E | energy |
| EB | energy balance |
| EC | energy consumption |
| ECW | extracellular water |
| EDM | endocrinology, diabetes and metabolism |
| EE | energy expenditure |
| EEE | Exercise Energy Expenditure |
| RER | respiratory exchange ratio |
| EI | Energy intake |
| EIMD | exercise-induced muscle damage |
| End | endurance |
| E-SOD | superoxide dismutase activity in erythrocytes |
| ExC | exercise capacities |
| F | fatigue |
| FAT | Female Athlete Triad |
| Fe | iron |
| FAS | Felt Arousal Scale |
| FS | Feeling Scale |
| FFM | fat free mass |
| FM | fat mass |
| FS | food science |
| Fs | sensation scale |
| G | glycogen |
| GI | gastrointestinal |
| GSH | glutathione |
| hg | height |
| h | hour |
| H | hydration |
| Hb | Hb |
| HIGH | High CHO availability |
| HJUMP | Horizontal Jump Test |
| H-LEA | high LEA |
| HS | heat stress |
| HI | high intensity |
| HIT | high-intensity training |
| Hn | hyponatraemia |
| HOMA2-IR | homeostasis model assessment for the insulin resistance |
| HR | heart rate |
| I | intensity |
| ICW | intracellular water |
| ICT | incremental cycling test |
| IC | inflammation cytokines |
| IE | intense exercise |
| IL-10 | cytokines |
| IL-6 | cytokines |
| IM | Iron Man |
| Int | intake |
| IR | injury-related |
| KI | kidney injury |
| L | laboratory |
| Lat | lactate |
| LD | long distance |
| LI | low intensity |
| LIT | low-intensity training |
| LEA | Low energy availability |
| LEAF-Q | low energy availability in females questionnaire |
| LLEA | low LEA |
| LOW | low CHO availability |
| M | master |
| Md | medicine |
| Mb | Myoglobin |
| MD | menstrual disorders |
| MDA | malondialdehyde |
| Mg | magnesium |
| mcN | macronutrients |
| MD&W | method of Durnin and Womersley |
| MD | muscle damage |
| MDA | malondialdehyde |
| Mg | magnesium |
| MgO | magnesium oxide |
| MM | muscle mass |
| MPO | myeloperoxidase |
| MUFA | monounsaturated fatty acids |
| N | nutrients |
| Nt | nutrition |
| N2 | nitrogen |
| Na | sodium |
| ND | nutrition and dietetics |
| NO | Nitric oxide |
| Nur | 24 h nitrogen excretion |
| O2 | oxygen |
| OG | organic chemistry |
| OGJ | organic grape juice |
| ORAC | oxygen radical absorbance capacity |
| OT | Olympic triathlon |
| P | performance |
| PAL | physical activity level |
| Ph | physiology |
| PHEOH | public health, environmental and occupational health |
| POMS | profile of mood states |
| PPROT | proteins of plant origin |
| Prdt | periodisation |
| Pt | proteins |
| PUFA | polyunsaturated fatty acids |
| PUFAn6 | n-6 polyunsaturated atty acids |
| PUFAn3 | n-3 polyunsaturated fatty acids |
| Rcv | recovery |
| RED-S | Relative Energy Deficiency in Sports |
| rED | relative energy deficit |
| REE | resting energy expenditure |
| rEI | Relative energy intake |
| RER | respiratory exchange rate |
| RPE | rate of perceived exertion |
| rTEE | relative total energy expenditure |
| s | speed |
| S | subjective/observational |
| SFA | saturated fatty acids |
| SL | sleep low |
| SM | sport medicine |
| SNKQ | Sports Nutrition Knowledge Questionnaire |
| Spp | supplementation |
| SS | sports supplements |
| ST | Sprint triathlon |
| St | strength |
| STR | sport therapy and rehabilitation |
| T | testosterone |
| Ta | Taurine |
| TBW | total body water |
| Texh | time to exhaustion |
| TEE | total energy expenditure |
| TL | train low |
| TNF-α | Cytokines |
| TRX | Thioredoxin |
| TT | Thirty-minute time trial |
| UE | ultra-endurance |
| V | volume |
| VAT | visceral adipose tissue |
| vC | vitamin C |
| vE | vitamin E |
| VO2max | maximum oxygen consumption |
| VO2 | oxygen consumption |
| VT | ventilatory threshold |
| WVT | workload expressed in watts |
| YP | young people |
| Zn | zinc |
References
- Cushman, D.M.; Dowling, N.; Ehn, M.; Kotler, D.H. Triathlon Considerations. Phys. Med. Rehabil. Clin. N. Am. 2022, 33, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.P.; Périard, J.D. Physiological Requirements of the Different Distances of Triathlon. In Triathlon Medicine; Springer: Cham, Switzerland, 2020; pp. 5–17. [Google Scholar] [CrossRef]
- Etxebarria, N.; Mujika, I.; Pyne, D.B. Training and Competition Readiness in Triathlon. Sports 2019, 7, 101. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, K.M.; Badenhorst, C.E.; Cripps, A.J.; Landers, G.J.; Merrells, R.J.; Bulsara, M.K.; Hoyne, G.F. Strength Training for Long-Distance Triathletes: Theory to Practice. Strength Cond. J. 2022, 44, 1–14. [Google Scholar] [CrossRef]
- Prieto-González, P.; Sedlacek, J. Effects of Running-Specific Strength Training, Endurance Training, and Concurrent Training on Recreational Endurance Athletes’ Performance and Selected Anthropometric Parameters. Int. J. Environ. Res. Public Health 2022, 19, 10773. [Google Scholar] [CrossRef]
- García-Giménez, A. Triathlon Performance: Physiological and Training Strategies from Super Sprint to Long Distance Events. Phys. Educ. Sport Through Centuries 2024, 11, 87–93. [Google Scholar] [CrossRef]
- Borrego-Sánchez, A.; Vinolo-Gil, M.J.; De-La-casa-almeida, M.; Rodríguez-Huguet, M.; Casuso-Holgado, M.J.; Martín-Valero, R. Effects of Training on Cardiorespiratory Fitness in Triathletes: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 13332. [Google Scholar] [CrossRef]
- Zamparo, P.; Cortesi, M.; Gatta, G. The Energy Cost of Swimming and Its Determinants. Eur. J. Appl. Physiol. 2020, 120, 41–66. [Google Scholar] [CrossRef]
- Husband, S.P.; Wainwright, B.; Wilson, F.; Crump, D.; Mockler, D.; Carragher, P.; Nugent, F.; Simms, C.K. Cycling Position Optimisation–A Systematic Review of the Impact of Positional Changes on Biomechanical and Physiological Factors in Cycling. J. Sports Sci. 2024, 42, 1477–1490. [Google Scholar] [CrossRef]
- Van Hooren, B.; Jukic, I.; Cox, M.; Frenken, K.G.; Bautista, I.; Moore, I.S. The Relationship Between Running Biomechanics and Running Economy: A Systematic Review and Meta-Analysis of Observational Studies. Sports Med. 2024, 54, 1269–1316. [Google Scholar] [CrossRef]
- Miguel-Ortega, Á.; Calleja-González, J.; Mielgo-Ayuso, J. Endurance in Long-Distance Swimming and the Use of Nutritional Aids. Nutrients 2024, 16, 3949. [Google Scholar] [CrossRef]
- Mugambi, L.T.; Okoth, M.W.; Abong, G.O.; Wamiti, J. Nutrition and Evidence-Based Foods for Enhancement of Athletic Performance. Galore Int. J. Health Sci. Res. 2023, 8, 53–65. [Google Scholar] [CrossRef]
- Miguel-Ortega, Á.; Calleja-Gonzalez, J.; Mielgo-Ayuso, J. Nutrition-Related Considerations for Health and Performance in Female Volleyball: A Narrative Review. J. Hum. Sport Exerc. 2023, 18, 462–477. [Google Scholar] [CrossRef]
- Burke, L.M.; Van Loon, L.J.C.; Hawley, J.A. Postexercise Muscle Glycogen Resynthesis in Humans. J. Appl. Physiol. 2017, 122, 1055–1067. [Google Scholar] [CrossRef]
- Vleck, V.; Millet, G.P.; Alves, F.B. The Impact of Triathlon Training and Racing on Athletes’ General Health. Sports Med. 2014, 44, 1659–1692. [Google Scholar] [CrossRef]
- Langa, D.; Naczyk, M.; Szymczak, R.K.; Karbowska, J.; Kochan, Z. A Preliminary Study of Nutrients Related to the Risk of Relative Energy Deficiency in Sport (RED-S) in Top-Performing Female Amateur Triathletes: Results from a Nutritional Assessment. Nutrients 2025, 17, 208. [Google Scholar] [CrossRef]
- Naderi, A.; Gobbi, N.; Ali, A.; Berjisian, E.; Hamidvand, A.; Forbes, S.C.; Koozehchian, M.S.; Karayigit, R.; Saunders, B. Carbohydrates and Endurance Exercise: A Narrative Review of a Food First Approach. Nutrients 2023, 15, 1367. [Google Scholar] [CrossRef]
- Purcell, L.K. Sport Nutrition for Young Athletes. Paediatr. Child Health 2013, 18, 200–202. [Google Scholar] [CrossRef]
- Jeejeebhoy, K.N. Nutritional Assessment. In Nutritional Care of the Patient with Gastrointestinal Disease; CRC Press: Boca Raton, FL, USA, 2015; pp. 1–14. [Google Scholar] [CrossRef]
- Cena, H.; Calder, P.C. Defining a Healthy Diet: Evidence for the Role of Contemporary Dietary Patterns in Health and Disease. Nutrients 2020, 12, 334. [Google Scholar] [CrossRef]
- Puri, S.; Shaheen, M.; Grover, B. Nutrition and Cognitive Health: A Life Course Approach. Front. Public Health 2023, 11, 1023907. [Google Scholar] [CrossRef]
- López Torres, O.; Fernández-Elías, V.E. Training and Nutrition for Performance: Males, Females, and Gender Differences. Nutrients 2024, 16, 3979. [Google Scholar] [CrossRef]
- Beck, K.; Thomson, J.S.; Swift, R.J.; von Hurst, P.R. Role of Nutrition in Performance Enhancement and Postexercise Recovery. Open Access J. Sports Med. 2015, 6, 259. [Google Scholar] [CrossRef] [PubMed]
- Jäger, R.; Kerksick, C.M.; Campbell, B.I.; Cribb, P.J.; Wells, S.D.; Skwiat, T.M.; Purpura, M.; Ziegenfuss, T.N.; Ferrando, A.A.; Arent, S.M.; et al. International Society of Sports Nutrition Position Stand: Protein and Exercise. J. Int. Soc. Sports Nutr. 2017, 14, 1–25. [Google Scholar] [CrossRef]
- Jeukendrup, A.E. Nutrition for Endurance Sports: Marathon, Triathlon, and Road Cycling. J. Sports Sci. 2011, 29 (Suppl. S1), 91–99. [Google Scholar] [CrossRef]
- Amawi, A.; AlKasasbeh, W.; Jaradat, M.; Almasri, A.; Alobaidi, S.; Hammad, A.A.; Bishtawi, T.; Fataftah, B.; Turk, N.; Saoud, H.; et al. Athletes’ Nutritional Demands: A Narrative Review of Nutritional Requirements. Front. Nutr. 2023, 10, 1331854. [Google Scholar] [CrossRef]
- Guest, N.S.; Horne, J.; Vanderhout, S.M.; El-Sohemy, A. Sport Nutrigenomics: Personalized Nutrition for Athletic Performance. Front. Nutr. 2019, 6, 8. [Google Scholar] [CrossRef]
- Kerksick, C.M.; Wilborn, C.D.; Roberts, M.D.; Smith-Ryan, A.; Kleiner, S.M.; Jäger, R.; Collins, R.; Cooke, M.; Davis, J.N.; Galvan, E.; et al. ISSN Exercise & Sports Nutrition Review Update: Research & Recommendations. J. Int. Soc. Sports Nutr. 2018, 15, 38. [Google Scholar] [CrossRef]
- Alfieri, A.; D’Angelo, S.; Mazzeo, F. Role of Nutritional Supplements in Sport, Exercise and Health. Nutrients 2023, 15, 4429. [Google Scholar] [CrossRef]
- Pence, J.C.; Martin, K.R.; Bloomer, R.J. Beyond Nutrition Recommendations: What Healthcare Professionals Should Know about Dietary Supplements to Best Serve Their Patients. Health 2021, 13, 334–346. [Google Scholar] [CrossRef]
- The Office of Dietary Supplements (ODS) of the National Institutes of Health (NIH). Dietary Supplements for Exercise and Athletic Performance—Health Professional Fact Sheet. Dietary Supplements for Exercise and Athletic Performance. Available online: https://ods.od.nih.gov/factsheets/ExerciseAndAthleticPerformance-HealthProfessional/#h2%0Ahttps://ods.od.nih.gov/factsheets/ExerciseAndAthleticPerformance-HealthProfessional/#h6 (accessed on 10 February 2025).
- Rowlands, D.S.; Houltham, S.D. Multiple-Transportable Carbohydrate Effect on Long-Distance Triathlon Performance. Med. Sci. Sports Exerc. 2017, 49, 1734–1744. [Google Scholar] [CrossRef]
- Knechtle, B.; Hernández Morales, N.P.; Ruvalcaba González, E.; Aguirre Gutierrez, A.A.; Noriega Sevilla, J.; Amézquita Gómez, R.; Estrada Robledo, A.R.; Marroquín Rodríguez, A.L.; Salas Fraire, O.; Andonie, J.L.; et al. Effect of a Multistage Ultraendurance Triathlon on Aldosterone, Vasopressin, Extracellular Water and Urine Electrolytes. Scott. Med. J. 2012, 57, 26–32. [Google Scholar] [CrossRef]
- Areces, F.; González-Millán, C.; Salinero, J.J.; Abian-Vicen, J.; Lara, B.; Gallo-Salazar, C.; Ruiz-Vicente, D.; Del Coso, J. Changes in Serum Free Amino Acids and Muscle Fatigue Experienced during a Half-Ironman Triathlon. PLoS ONE 2015, 10, e0138376. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Park, H.Y.; Kim, S.W.; Sun, Y.; Choi, J.H.; Seo, J.; Jung, Y.P.; Kim, A.J.; Kim, J.; Lim, K. Enhancing Supplemental Effects of Acute Natural Antioxidant Derived from Yeast Fermentation and Vitamin C on Sports Performance in Triathlon Athletes: A Randomized, Double-Blinded, Placebo-Controlled, Crossover Trial. Nutrients 2023, 15, 3324. [Google Scholar] [CrossRef] [PubMed]
- Potgieter, S.; Wright, H.H.; Smith, C. Caffeine Improves Triathlon Performance: A Field Study in Males and Females. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 228–237. [Google Scholar] [CrossRef]
- Houston, M.; Dolan, S.; Martin, S. The impact of physical, nutritional, and mental preparation on triathlon performance. J. Sports Med. Phys. Fit. 2011, 51, 583–594. [Google Scholar]
- Bonilla, D.A.; Boullosa, D.; Del Coso, J. Advances in Nutrition, Dietary Supplements and Ergogenic Aids for Athletic Performance: Trends and Future Prospects. Nutrients 2023, 15, 2246. [Google Scholar] [CrossRef]
- Miguel-Ortega, Á.; Calleja-González, J.; Mielgo-Ayuso, J. Nutrition-Related Considerations for Health and Performance in Female Basketball Players: A Narrative Review. J. Phys. Fit. Sports Med. 2023, 12, 119–132. [Google Scholar] [CrossRef]
- Escribano-Ott, I.; Calleja-González, J.; Mielgo-Ayuso, J. Ergo-Nutritional Intervention in Basketball: A Systematic Review. Nutrients 2022, 14, 638. [Google Scholar] [CrossRef]
- Brooke, N.K.; Cosio-Lima, L. Nutrition in Cycling. Phys. Med. Rehabil. Clin. N. Am. 2022, 33, 159–172. [Google Scholar] [CrossRef]
- Barrenetxea-Garcia, J.; Murua-Ruiz, A.; Mielgo-Ayuso, J.; Nuell, S.; Calleja-González, J.; de Villarreal, E.S. Recovery in Water Polo: How Much Do We Have to Know? A Systematic Review. J. Exerc. Rehabil. 2022, 18, 225–234. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; Clark, J.; et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- O’Connor, D.; Green, S.; Higgins, J.P. Defining the Review Question and Developing Criteria for Including Studies. In Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; Wiley: Hoboken, NJ, USA, 2008; pp. 81–94. [Google Scholar] [CrossRef]
- Horsley, T.; Dingwall, O.; Sampson, M. Checking Reference Lists to Find Additional Studies for Systematic Reviews. Cochrane Database Syst. Rev. 2011, 8, MR000026. [Google Scholar] [CrossRef] [PubMed]
- Gentles, S.J.; Charles, C.; Ploeg, J.; Ann McKibbon, K. Sampling in Qualitative Research: Insights from an Overview of the Methods Literature. Qual. Rep. 2015, 20, 1772–1789. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; Willey: Hoboken, NJ, USA, 2008; Volume 2010, pp. 1–649. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Kirby, R.S. Clinical Epidemiology: How to Do Clinical Practice Research, 3rd ed.; Lippincott Williams & Wilkins (LWW): Philadelphia, PA, USA, 2012. [Google Scholar] [CrossRef]
- Olivo, S.A.; Macedo, L.G.; Gadotti, I.C.; Fuentes, J.; Stanton, T.; Magee, D.J. Scales to Assess the Quality of Randomized Controlled Trials: A Systematic Review. Phys. Ther. 2008, 88, 156–175. [Google Scholar] [CrossRef]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the Quality of Reports of Randomized Clinical Trials: Is Blinding Necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Frentsos, J.A.; Baer, J.T. Increased Energy and Nutrient Intake during Training and Competition Improves Elite Triathletes’ Endurance Performance. Int. J. Sport Nutr. Exerc. Metab. 1997, 7, 61–71. [Google Scholar] [CrossRef]
- Kimber, N.E.; Ross, J.J.; Mason, S.L.; Speedy, D.B. Energy Balance During an Ironman Triathlon in Male and Female Triathletes. J. Sport Nutr. Exerc. Metab. 2002, 12, 47–62. [Google Scholar] [CrossRef]
- Jeukendrup, A.E.; Jentjens, R.L.; Moseley, L. Nutritional Considerations in Triathlon. Sports Med. 2005, 35, 163–181. [Google Scholar] [CrossRef]
- Gillum, T.L.; Dumke, C.L.; Ruby, B.C. Muscle Glycogenolysis and Resynthesis in Response to a Half Ironman Triathlon: A Case Study. Int. J. Sports Physiol. Perform. 2006, 1, 408–413. [Google Scholar] [CrossRef]
- Strock, G.A.; Cottrell, E.R.; Lohman, J.M. Triathlon. Phys. Med. Rehabil. Clin. N. Am. 2006, 17, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Bentley, D.J.; Cox, G.R.; Green, D.; Laursen, P.B. Maximising Performance in Triathlon: Applied Physiological and Nutritional Aspects of Elite and Non-Elite Competitions. J. Sci. Med. Sport 2008, 11, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Neubauer, O.; Reichhold, S.; Nics, L.; Hoelzl, C.; Valentini, J.; Stadlmayr, B.; Knasmller, S.; Wagner, K.H. Antioxidant Responses to an Acute Ultra-Endurance Exercise: Impact on DNA Stability and Indications for an Increased Need for Nutritive Antioxidants in the Early Recovery Phase. Br. J. Nutr. 2010, 104, 1129–1138. [Google Scholar] [CrossRef]
- Pahnke, M.D.; Trinity, J.D.; Zachwieja, J.J.; Stofan, J.R.; Hiller, W.D.; Coyle, E.F. Serum Sodium Concentration Changes Are Related to Fluid Balance and Sweat Sodium Loss. Med. Sci. Sports Exerc. 2010, 42, 1669–1674. [Google Scholar] [CrossRef]
- Cox, G.R.; Snow, R.J.; Burke, L.M. Race-Day Carbohydrate Intakes of Elite Triathletes Contesting Olympic-Distance Triathlon Events. Int. J. Sport Nutr. Exerc. Metab. 2010, 20, 299–306. [Google Scholar] [CrossRef][Green Version]
- Gonçalves, M.C.; Bezerra, F.F.; Eleutherio, E.C.D.A.; Bouskela, E.; Koury, J. Organic Grape Juice Intake Improves Functional Capillary Density and Postocclusive Reactive Hyperemia in Triathletes. Clinics 2011, 66, 1537–1541. [Google Scholar] [CrossRef]
- Barrero, A.; Erola, P.; Bescós, R. Energy Balance of Triathletes During an Ultra-Endurance Event. Nutrients 2015, 7, 209–222. [Google Scholar] [CrossRef]
- Wilson, P.B.; Rhodes, G.S.; Ingraham, S.J. Saccharide Composition of Carbohydrates Consumed During an Ultra-Endurance Triathlon. J. Am. Coll. Nutr. 2015, 34, 497–506. [Google Scholar] [CrossRef]
- Doering, T.M.; Reaburn, P.R.; Cox, G.; Jenkins, D.G. Comparison of Postexercise Nutrition Knowledge and Postexercise Carbohydrate and Protein Intake Between Australian Masters and Younger Triathletes. Int. J. Sport Nutr. Exerc. Metab. 2016, 26, 338–346. [Google Scholar] [CrossRef]
- Sareban, M.; Zügel, D.; Koehler, K.; Hartveg, P.; Zügel, M.; Schumann, U.; Steinacker, J.M.; Treff, G. Carbohydrate Intake in Form of Gel Is Associated with Increased Gastrointestinal Distress but Not with Performance Differences Compared with Liquid Carbohydrate Ingestion During Simulated Long-Distance Triathlon. Int. J. Sport Nutr. Exerc. Metab. 2016, 26, 114–122. [Google Scholar] [CrossRef][Green Version]
- De Carvalho, F.G.; Galan, B.S.M.; Santos, P.C.; Pritchett, K.; Pfrimer, K.; Ferriolli, E.; Papoti, M.; Marchini, J.S.; de Freitas, E.C. Taurine: A Potential Ergogenic Aid for Preventing Muscle Damage and Protein Catabolism and Decreasing Oxidative Stress Produced by Endurance Exercise. Front. Physiol. 2017, 8, 710. [Google Scholar] [CrossRef] [PubMed]
- Getzin, A.R.; Milner, C.; Harkins, M. Fueling the Triathlete: Evidence-Based Practical Advice for Athletes of All Levels. Curr. Sports Med. Rep. 2017, 16, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Hotfiel, T.; Mayer, I.; Huettel, M.; Hoppe, M.W.; Engelhardt, M.; Lutter, C.; Pöttgen, K.; Heiss, R.; Kastner, T.; Grim, C. Accelerating Recovery from Exercise-Induced Muscle Injuries in Triathletes: Considerations for Olympic Distance Races. Sports 2019, 7, 143. [Google Scholar] [CrossRef]
- Huang, W.C.; Wei, C.C.; Huang, C.C.; Chen, W.L.; Huang, H.Y. The Beneficial Effects of Lactobacillus Plantarum PS128 on High-Intensity, Exercise-Induced Oxidative Stress, Inflammation, and Performance in Triathletes. Nutrients 2019, 11, 353. [Google Scholar] [CrossRef]
- McKay, A.K.A.; Heikura, I.A.; Burke, L.M.; Peeling, P.; van Swelm, R.P.L.; Laarakkers, C.M.; Pyne, D.B.; Cox, G.R. Influence of Periodizing Dietary Carbohydrate on Iron Regulation and Immune Function in Elite Triathletes. Int. J. Sport Nutr. Exerc. Metab. 2020, 30, 34–41. [Google Scholar] [CrossRef]
- Storsve, A.B.; Johnsen, L.; Nyborg, C.; Melau, J.; Hisdal, J.; Burri, L. Effects of Krill Oil and Race Distance on Serum Choline and Choline Metabolites in Triathletes: A Field Study. Front. Nutr. 2020, 7, 133. [Google Scholar] [CrossRef]
- Burgos, J.; Viribay, A.; Fernández-Lázaro, D.; Calleja-González, J.; González-Santos, J.; Mielgo-Ayuso, J. Combined Effects of Citrulline Plus Nitrate-Rich Beetroot Extract Co-Supplementation on Maximal and Endurance-Strength and Aerobic Power in Trained Male Triathletes: A Randomized Double-Blind, Placebo-Controlled Trial. Nutrients 2022, 14, 40. [Google Scholar] [CrossRef]
- Burgos, J.; Viribay, A.; Calleja-gonzález, J.; Fernández-lázaro, D.; Olasagasti-ibargoien, J.; Seco-calvo, J.; Mielgo-ayuso, J. Long-Term Combined Effects of Citrulline and Nitrate-Rich Beetroot Extract Supplementation on Recovery Status in Trained Male Triathletes: A Randomized, Double-Blind, Placebo-Controlled Trial. Biology 2022, 11, 75. [Google Scholar] [CrossRef]
- Martínez-Olcina, M.; Miralles-Amorós, L.; Asencio-Mas, N.; Vicente-Martínez, M.; Yáñez-Sepúlveda, R.; Martínez-Rodríguez, A. Ingestion of Carbohydrate Solutions and Mouth Rinse on Mood and Perceptual Responses during Exercise in Triathletes. Gels 2022, 8, 50. [Google Scholar] [CrossRef]
- Acevedo, O.G.; Aragón-Vela, J.; De la Cruz Márquez, J.C.; Marín, M.M.; Casuso, R.A.; Huertas, J.R. Seawater Hydration Modulates IL-6 and Apelin Production during Triathlon Events: A Crossover Randomized Study. Int. J. Environ. Res. Public Health 2022, 19, 9581. [Google Scholar] [CrossRef]
- Tan, X.; Rogers, N.; Brown, N.; MacDonald, M.; Bowler, A.L.; Cox, G.R. The Impact of a ‘Remotely-Delivered’ Sports Nutrition Education Program on Dietary Intake and Nutrition Knowledge of Junior Elite Triathletes. Nutrients 2022, 14, 5203. [Google Scholar] [CrossRef] [PubMed]
- Durkalec-Michalski, K.; Główka, N.; Nowaczyk, P.M.; Laszczak, A.; Gogojewicz, A.; Suliburska, J. Do Triathletes Periodize Their Diet and Do Their Mineral Content, Body Composition and Aerobic Capacity Change During Training and Competition Periods? Nutrients 2023, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Bennett, S.; Tiollier, E.; Guibert, E.; Morales-Artacho, A.; Lalire, P.; Owens, D.J.; Morton, J.P.; Brocherie, F.; Louis, J. Environmental Heat Stress Offsets Adaptation Associated with Carbohydrate Periodization in Trained Male Triathletes. Scand. J. Med. Sci. Sport. 2023, 33, 1677–1689. [Google Scholar] [CrossRef]
- Jiménez-Alfageme, R.; Martínez-Sanz, J.M.; Romero-García, D.; Giménez-Monzo, D.; Hernández Aparicio, S.; Sanchez-Oliver, A.J.; Sospedra, I. Do Spanish Triathletes Consume Sports Supplements According to Scientific Evidence? An Analysis of the Consumption Pattern According to Sex and Level of Competition. Nutrients 2023, 15, 1330. [Google Scholar] [CrossRef]
- Witkoś, J.; Błażejewski, G.; Gierach, M. The Low Energy Availability in Females Questionnaire (LEAF-Q) as a Useful Tool to Identify Female Triathletes at Risk for Menstrual Disorders Related to Low Energy Availability. Nutrients 2023, 15, 650. [Google Scholar] [CrossRef]
- Wei, C.C.; Harris, M.B.; Ye, M.; Nicholls, A.; Alkhatib, A.; Dewi, L.; Huang, C.Y.; Kuo, C.H. Defecation After Magnesium Supplementation Enhances Cognitive Performance in Triathletes. Sports Med. Health Sci. 2024, 7, 102–108. [Google Scholar] [CrossRef]
- de Oliveira, V.N.; Andrade, M.S.; Sinisgalli, R.; Vancini, R.L.; de Conti Teixeira Costa, G.; Weiss, K.; Knechtle, B.; de Lira, C.A.B. Prevalence of Dietary Supplement Use Among Male Brazilian Recreational Triathletes: A Cross-Sectional Study. BMC Res. Notes 2024, 17, 8. [Google Scholar] [CrossRef]
- Aragón-Vela, J.; González-Acevedo, O.; De la Cruz-Márquez, J.C.; Rojas Ruíz, F.J.; Marín, M.M.; Casuso, R.A.; Plaza-Diaz, J.; Huertas, J.F.R. The Effects of Acute Deep Seawater Supplementation on Muscle Function after Triathlon. J. Clin. Med. 2024, 13, 2258. [Google Scholar] [CrossRef]
- Mendes, M.P.; Marinho, A.H.; Moura, F.A.; Bádue, G.S.; Ferreira, G.A.; de Araujo, G.G.; Lima-Silva, A.E.; Ataide-Silva, T. Self-Reported Carbohydrate Supercompensation and Supplementation Strategies Adopted by Olympic Triathlon Athletes. Braz. J. Med. Biol. Res. 2025, 58, e14189. [Google Scholar] [CrossRef]
- Ioniță-Mîndrican, C.B.; Ziani, K.; Mititelu, M.; Oprea, E.; Neacșu, S.M.; Moroșan, E.; Dumitrescu, D.E.; Roșca, A.C.; Drăgănescu, D.; Negrei, C. Therapeutic Benefits and Dietary Restrictions of Fiber Intake: A State of the Art Review. Nutrients 2022, 14, 2641. [Google Scholar] [CrossRef]
- Close, G.L.; Kasper, A.M.; Morton, J.P. From Paper to Podium: Quantifying the Translational Potential of Performance Nutrition Research. Sports Med. 2019, 49 (Suppl. S1), 25–37. [Google Scholar] [CrossRef] [PubMed]
- Heydenreich, J.; Kayser, B.; Schutz, Y.; Melzer, K. Total Energy Expenditure, Energy Intake, and Body Composition in Endurance Athletes Across the Training Season: A Systematic Review. Sports Med.-Open 2017, 3, 8. [Google Scholar] [CrossRef] [PubMed]
- Joyner, M.J.; Coyle, E.F. Endurance Exercise Performance: The Physiology of Champions. J. Physiol. 2008, 586, 35–44. [Google Scholar] [CrossRef]
- Murray, B.; Rosenbloom, C. Fundamentals of Glycogen Metabolism for Coaches and Athletes. Nutr. Rev. 2018, 76, 243–259. [Google Scholar] [CrossRef]
- Iwayama, K.; Seol, J.; Tokuyama, K. Exercise Timing Matters for Glycogen Metabolism and Accumulated Fat Oxidation over 24 H. Nutrients 2023, 15, 1109. [Google Scholar] [CrossRef]
- Mata, F.; Valenzuela, P.L.; Gimenez, J.; Tur, C.; Ferreria, D.; Domínguez, R.; Sanchez-Oliver, A.J.; Sanz, J.M.M. Carbohydrate Availability and Physical Performance: Physiological Overview and Practical Recommendations. Nutrients 2019, 11, 1084. [Google Scholar] [CrossRef]
- Hearris, M.A.; Hammond, K.M.; Fell, J.M.; Morton, J.P. Regulation of Muscle Glycogen Metabolism during Exercise: Implications for Endurance Performance and Training Adaptations. Nutrients 2018, 10, 298. [Google Scholar] [CrossRef]
- Cao, W.; He, Y.; Fu, R.; Chen, Y.; Yu, J.; He, Z. A Review of Carbohydrate Supplementation Approaches and Strategies for Optimizing Performance in Elite Long-Distance Endurance. Nutrients 2025, 17, 918. [Google Scholar] [CrossRef]
- Naderi, A.; Rothschild, J.A.; Santos, H.O.; Hamidvand, A.; Koozehchian, M.S.; Ghazzagh, A.; Berjisian, E.; Podlogar, T. Nutritional Strategies to Improve Post-Exercise Recovery and Subsequent Exercise Performance: A Narrative Review. Sports Med. 2025, 1–19. [Google Scholar] [CrossRef]
- Nakrani, M.N.; Wineland, R.H.; Anjum, F. Physiology, Glucose Metabolism; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Tiller, N.B.; Roberts, J.D.; Beasley, L.; Chapman, S.; Pinto, J.M.; Smith, L.; Wiffin, M.; Russell, M.; Sparks, S.A.; Duckworth, L.; et al. International Society of Sports Nutrition Position Stand: Nutritional Considerations for Single-Stage Ultra-Marathon Training and Racing. J. Int. Soc. Sports Nutr. 2019, 16, 50. [Google Scholar] [CrossRef]
- Craven, J.; Desbrow, B.; Sabapathy, S.; Bellinger, P.; McCartney, D.; Irwin, C. The Effect of Consuming Carbohydrate with and Without Protein on the Rate of Muscle Glycogen Re-Synthesis During Short-Term Post-Exercise Recovery: A Systematic Review and Meta-Analysis. Sports Med.-Open 2021, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, B.J.; Aragon, A.A.; Krieger, J.W. The Effect of Protein Timing on Muscle Strength and Hypertrophy: A Meta-Analysis. J. Int. Soc. Sports Nutr. 2013, 10, 53. [Google Scholar] [CrossRef] [PubMed]
- Kalogerakou, T.; Antoniadou, M. The Role of Dietary Antioxidants, Food Supplements and Functional Foods for Energy Enhancement in Healthcare Professionals. Antioxidants 2024, 13, 1508. [Google Scholar] [CrossRef]
- Martín-Rodríguez, A.; Belinchón-deMiguel, P.; Rubio-Zarapuz, A.; Tornero-Aguilera, J.F.; Martínez-Guardado, I.; Villanueva-Tobaldo, C.V.; Clemente-Suárez, V.J. Advances in Understanding the Interplay Between Dietary Practices, Body Composition, and Sports Performance in Athletes. Nutrients 2024, 16, 571. [Google Scholar] [CrossRef]
- Wang, L.; Meng, Q.; Su, C.H. From Food Supplements to Functional Foods: Emerging Perspectives on Post-Exercise Recovery Nutrition. Nutrients 2024, 16, 4081. [Google Scholar] [CrossRef]
- Stožer, A.; Vodopivc, P.; Bombek, L.K. Pathophysiology of Exercise-Induced Muscle Damage and Its Structural, Functional, Metabolic, and Clinical Consequences. Physiol. Res. 2020, 69, 565–598. [Google Scholar] [CrossRef]
- Jaiswal, N.; Gavin, M.; Loro, E.; Sostre-Colón, J.; Roberson, P.A.; Uehara, K.; Rivera-Fuentes, N.; Neinast, M.; Arany, Z.; Kimball, S.R.; et al. AKT Controls Protein Synthesis and Oxidative Metabolism via Combined MTORC1 and FOXO1 Signalling to Govern Muscle Physiology. J. Cachexia Sarcopenia Muscle 2022, 13, 495–514. [Google Scholar] [CrossRef]
- Kronfeld, D.S. Body Fluids and Exercise: Physiological Responses (PART I). J. Equine Vet. Sci. 2001, 21, 312–322. [Google Scholar] [CrossRef]
- Jung, A.P.; Bishop, P.A.; Al-Nawwas, A.; Dale, R.B. Influence of Hydration and Electrolyte Supplementation on Incidence and Time to Onset of Exercise-Associated Muscle Cramps. J. Athl. Train. 2005, 40, 71–75. [Google Scholar]
- Simpson, R.J.; Campbell, J.P.; Gleeson, M.; Krüger, K.; Nieman, D.C.; Pyne, D.B.; Turner, J.E.; Walsh, N.P. Can exercise affect immune function to increase susceptibility to infection? Exerc. Immunol. Rev. 2020, 26, 8–22. [Google Scholar]
- Pedersen, B.K.; Rohde, T.; Ostrowski, K. Recovery of the Immune System After Exercise. Acta Physiol. Scand. 1998, 162, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Myrick, K.M. Overtraining and Overreaching Syndrome in Athletes. J. Nurse Pract. 2015, 11, 1018–1022. [Google Scholar] [CrossRef]
- Morrison, M.; Halson, S.L.; Weakley, J.; Hawley, J.A. Sleep, Circadian Biology and Skeletal Muscle Interactions: Implications for Metabolic Health. Sleep Med. Rev. 2022, 66, 101700. [Google Scholar] [CrossRef]
- Chennaoui, M.; Vanneau, T.; Trignol, A.; Arnal, P.; Gomez-Merino, D.; Baudot, C.; Perez, J.; Pochettino, S.; Eirale, C.; Chalabi, H. How Does Sleep Help Recovery from Exercise-Induced Muscle Injuries? J. Sci. Med. Sport 2021, 24, 982–987. [Google Scholar] [CrossRef]
- Espinosa-Salas, S.; Gonzalez-Arias, M. Nutrition: Micronutrient Intake, Imbalances, and Interventions; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Sañudo, B.; Bartolomé, D.; Tejero, S.; Ponce-González, J.G.; Loza, J.P.; Figueroa, A. Impact of Active Recovery and Whole-Body Electromyostimulation on Blood-Flow and Blood Lactate Removal in Healthy People. Front. Physiol. 2020, 11, 310. [Google Scholar] [CrossRef]
- Li, S.; Kempe, M.; Brink, M.; Lemmink, K. Effectiveness of Recovery Strategies After Training and Competition in Endurance Athletes: An Umbrella Review. Sports Med.-Open 2024, 10, 55. [Google Scholar] [CrossRef]
- Margolis, L.M.; Allen, J.T.; Hatch-McChesney, A.; Pasiakos, S.M. Coingestion of Carbohydrate and Protein on Muscle Glycogen Synthesis After Exercise: A Meta-Analysis. Med. Sci. Sports Exerc. 2021, 53, 384–393. [Google Scholar] [CrossRef]
- Kerksick, C.; Harvey, T.; Stout, J.; Campbell, B.; Wilborn, C.; Kreider, R.; Kalman, D.; Ziegenfuss, T.; Lopez, H.; Landis, J.; et al. International Society of Sports Nutrition Position Stand: Nutrient Timing. J. Int. Soc. Sports Nutr. 2008, 5, 17. [Google Scholar] [CrossRef]
- Owens, D.J.; Twist, C.; Cobley, J.N.; Howatson, G.; Close, G.L. Exercise-Induced Muscle Damage: What Is It, What Causes It and What Are the Nutritional Solutions? Eur. J. Sport Sci. 2019, 19, 71–85. [Google Scholar] [CrossRef]
- Choi, D.H.; Cho, J.Y.; Koo, J.H.; Kim, T.K. Effects of Electrolyte Supplements on Body Water Homeostasis and Exercise Performance During Exhaustive Exercise. Appl. Sci. 2021, 11, 9093. [Google Scholar] [CrossRef]
- Weerapong, P.; Hume, P.A.; Kolt, G.S. The Mechanisms of Massage and Effects on Performance, Muscle Recovery and Injury Prevention. Sports Med. 2005, 35, 235–256. [Google Scholar] [CrossRef] [PubMed]
- Peake, J.M.; Roberts, L.A.; Figueiredo, V.C.; Egner, I.; Krog, S.; Aas, S.N.; Suzuki, K.; Markworth, J.F.; Coombes, J.S.; Cameron-Smith, D.; et al. The Effects of Cold Water Immersion and Active Recovery on Inflammation and Cell Stress Responses in Human Skeletal Muscle after Resistance Exercise. J. Physiol. 2017, 595, 695–711. [Google Scholar] [CrossRef]
- Page, P. Current Concepts in Muscle Stretching for Exercise and Rehabilitation. Int. J. Sports Phys. Ther. 2012, 7, 109–119. [Google Scholar] [PubMed]
- Charest, J.; Grandner, M.A. Sleep and Athletic Performance: Impacts on Physical Performance, Mental Performance, Injury Risk and Recovery, and Mental Health. Sleep Med. Clin. 2020, 15, 41–57. [Google Scholar] [CrossRef] [PubMed]
- Sharif, K. Chronic Fatigue Syndrome. In Autoimmune Disorders: Adjuvants and Other Risk Factors in Pathogenesis; Wiley: Hoboken, NJ, USA, 2024; pp. 107–115. [Google Scholar] [CrossRef]
- Aicale, R.; Tarantino, D.; Maffulli, N. Overuse Injuries in Sport: A Comprehensive Overview. J. Orthop. Surg. Res. 2018, 13, 309. [Google Scholar] [CrossRef]
- Patel, H.; Vanguri, P.; Kumar, D.; Levin, D. The Impact of Inadequate Sleep on Overtraining Syndrome in Male and Female College Athletes 18–22 Years Old: A Literature Review. Cureus 2024, 16, e56186. [Google Scholar] [CrossRef]
- Sandbakk, Ø.; Tønnessen, E.; Sandbakk, S.B.; Losnegard, T.; Seiler, S.; Haugen, T. Best-Practice Training Characteristics Within Olympic Endurance Sports as Described by Norwegian World-Class Coaches. Sport. Med. Open 2025, 11, 45. [Google Scholar] [CrossRef]
- Cintineo, H.P.; Bello, M.L.; Walker, A.J.; Chandler, A.J.; McFadden, B.A.; Arent, S.M. Monitoring Training, Performance, Biomarkers, and Psychological State Throughout a Competitive Season: A Case Study of a Triathlete. Eur. J. Appl. Physiol. 2024, 124, 1895–1910. [Google Scholar] [CrossRef]
- Mujika, I. Tapering for Triathlon Competition. J. Hum. Sport Exerc. 2011, 6, 264–270. [Google Scholar] [CrossRef]
- Nutrition, C. Ergogenic Aid—An Overview|ScienceDirect Topics. Available online: https://www.sciencedirect.com/topics/medicine-and-dentistry/ergogenic-aid (accessed on 8 May 2025).
- Kruseman, M.; Lecoultre, V.; Gremeaux, V. Nutrition for Long-Distance Triathletes: Facts and Myths. Ger. J. Sports Med. 2020, 71, 229–235. [Google Scholar] [CrossRef]
- Armstrong, L.E. Rehydration During Endurance Exercise: Challenges, Research, Options, Methods. Nutrients 2021, 13, 887. [Google Scholar] [CrossRef] [PubMed]
- Varillas-Delgado, D. Nutritional Status and Ergogenic Aids in Performance During Exercise and Sports. Nutrients 2025, 17, 1224. [Google Scholar] [CrossRef] [PubMed]
- Passe, D.H.; Horn, M.; Stofan, J.; Murray, R. Palatability and Voluntary Intake of Sports Beverages, Diluted Orange Juice, and Water During Exercise. Int. J. Sport Nutr. Exerc. Metab. 2004, 14, 272–284. [Google Scholar] [CrossRef]
- Burns, T.A. Electrolytes. In Pharmacology in Veterinary Anesthesia and Analgesia; Wiley: Hoboken, NJ, USA, 2024; pp. 362–369. [Google Scholar] [CrossRef]
- Krisher, L.; Dawson, J.B.; Yoder, H.; Pilloni, D.; Dally, M.; Johnson, E.C.; Jaramillo, D.; Cruz, A.; Asensio, C.; Newman, L.S. Electrolyte Beverage Intake to Promote Hydration and Maintain Kidney Function in Guatemalan Sugarcane Workers Laboring in Hot Conditions. J. Occup. Environ. Med. 2020, 62, e696–e703. [Google Scholar] [CrossRef]
- Crintea, I.N.; Cindrea, A.C.; Mederle, O.A.; Trebuian, C.I.; Timar, R. Electrolyte Imbalances and Metabolic Emergencies in Obesity: Mechanisms and Clinical Implications. Diseases 2025, 13, 69. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Sawka, M.N. Fluid and Electrolyte Needs for Training, Competition, and Recovery. J. Sports Sci. 2011, 29 (Suppl. S1), S39–S46. [Google Scholar] [CrossRef]
- Witard, O.C.; Hearris, M.; Morgan, P.T. Protein Nutrition for Endurance Athletes: A Metabolic Focus on Promoting Recovery and Training Adaptation. Sports Med. 2025, 1–16. [Google Scholar] [CrossRef]
- Drummond, M.J.; Rasmussen, B.B. Leucine-Enriched Nutrients and the Regulation of Mammalian Target of Rapamycin Signalling and Human Skeletal Muscle Protein Synthesis. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 222–226. [Google Scholar] [CrossRef]
- Kim, D.-H.; Kim, S.-H.; Jeong, W.-S.; Lee, H.-Y. Effect of BCAA Intake During Endurance Exercises on Fatigue Substances, Muscle Damage Substances, and Energy Metabolism Substances. J. Exerc. Nutr. Biochem. 2013, 17, 169–180. [Google Scholar] [CrossRef]
- Cava, E.; Yeat, N.C.; Mittendorfer, B. Preserving Healthy Muscle During Weight Loss. Adv. Nutr. 2017, 8, 511–519. [Google Scholar] [CrossRef]
- Xu, F.; Zeng, J.; Liu, X.; Lai, J.; Xu, J. Exercise-Induced Muscle Damage and Protein Intake: A Bibliometric and Visual Analysis. Nutrients 2022, 14, 4288. [Google Scholar] [CrossRef] [PubMed]
- Carbone, J.W.; Pasiakos, S.M. Dietary Protein and Muscle Mass: Translating Science to Application and Health Benefit. Nutrients 2019, 11, 1136. [Google Scholar] [CrossRef] [PubMed]
- Cintineo, H.P.; Arent, M.A.; Antonio, J.; Arent, S.M. Effects of Protein Supplementation on Performance and Recovery in Resistance and Endurance Training. Front. Nutr. 2018, 5, 83. [Google Scholar] [CrossRef]
- Blomstrand, E. A Role for Branched-Chain Amino Acids in Reducing Central Fatigue. J. Nutr. 2006, 136, 544S–547S. [Google Scholar] [CrossRef]
- Mikulski, T.; Dabrowski, J.; Hilgier, W.; Ziemba, A.; Krzeminski, K. Effects of Supplementation with Branched Chain Amino Acids and Ornithine Aspartate on Plasma Ammonia and Central Fatigue During Exercise in Healthy Men. Folia Neuropathol. 2015, 53, 377–386. [Google Scholar] [CrossRef]
- Luan, C.; Wang, Y.; Li, J.; Zhou, N.; Song, G.; Ni, Z.; Xu, C.; Tang, C.; Fu, P.; Wang, X.; et al. Branched-Chain Amino Acid Supplementation Enhances Substrate Metabolism, Exercise Efficiency and Reduces Post-Exercise Fatigue in Active Young Males. Nutrients 2025, 17, 1290. [Google Scholar] [CrossRef]
- Trexler, E.T.; Smith-Ryan, A.E.; Stout, J.R.; Hoffman, J.R.; Wilborn, C.D.; Sale, C.; Kreider, R.B.; Jäger, R.; Earnest, C.P.; Bannock, L.; et al. International Society of Sports Nutrition Position Stand: Beta-Alanine. J. Int. Soc. Sports Nutr. 2015, 12, 30. [Google Scholar] [CrossRef]
- Hormoznejad, R.; Zare Javid, A.; Mansoori, A. Effect of BCAA Supplementation on Central Fatigue, Energy Metabolism Substrate and Muscle Damage to the Exercise: A Systematic Review with Meta-Analysis. Sport Sci. Health 2019, 15, 265–279. [Google Scholar] [CrossRef]
- Mason, S.A.; Trewin, A.J.; Parker, L.; Wadley, G.D. Antioxidant Supplements and Endurance Exercise: Current Evidence and Mechanistic Insights. Redox Biol. 2020, 35, 101471. [Google Scholar] [CrossRef]
- Vitale, K.; Getzin, A. Nutrition and Supplement Update for the Endurance Athlete: Review and Recommendations. Nutrients 2019, 11, 1289. [Google Scholar] [CrossRef]
- Martinho, D.V.; Nobari, H.; Faria, A.; Field, A.; Duarte, D.; Sarmento, H. Oral Branched-Chain Amino Acids Supplementation in Athletes: A Systematic Review. Nutrients 2022, 14, 4002. [Google Scholar] [CrossRef] [PubMed]
- Mamerow, M.M.; Mettler, J.A.; English, K.L.; Casperson, S.L.; Arentson-Lantz, E.; Sheffield-Moore, M.; Layman, D.K.; Paddon-Jones, D. Dietary Protein Distribution Positively Influences 24-H Muscle Protein Synthesis in Healthy Adults. J. Nutr. 2014, 144, 876–880. [Google Scholar] [CrossRef] [PubMed]
- Wax, B.; Kerksick, C.M.; Jagim, A.R.; Mayo, J.J.; Lyons, B.C.; Kreider, R.B. Creatine for Exercise and Sports Performance, with Recovery Considerations for Healthy Populations. Nutrients 2021, 13, 1915. [Google Scholar] [CrossRef]
- Saito, S.; Cao, D.Y.; Okuno, A.; Li, X.; Peng, Z.; Kelel, M.; Tsuji, N.M. Creatine Supplementation Enhances Immunological Function of Neutrophils by Increasing Cellular Adenosine Triphosphate. Biosci. Microbiota Food Health 2022, 41, 185–194. [Google Scholar] [CrossRef]
- Doma, K.; Ramachandran, A.K.; Boullosa, D.; Connor, J. The Paradoxical Effect of Creatine Monohydrate on Muscle Damage Markers: A Systematic Review and Meta-Analysis. Sports Med. 2022, 52, 1623–1645. [Google Scholar] [CrossRef]
- Antonio, J.; Newmire, D.E.; Stout, J.R.; Antonio, B.; Gibbons, M.; Lowery, L.M.; Harper, J.; Willoughby, D.; Evans, C.; Anderson, D.; et al. Common Questions and Misconceptions about Caffeine Supplementation: What Does the Scientific Evidence Really Show? J. Int. Soc. Sports Nutr. 2024, 21, 2323919. [Google Scholar] [CrossRef]
- Naderi, A.; de Oliveira, E.P.; Ziegenfuss, T.N.; Willems, M.E.T. Timing, Optimal Dose and Intake Duration of Dietary Supplements with Evidence-Based Use in Sports Nutrition. J. Exerc. Nutr. Biochem. 2016, 20, 1–12. [Google Scholar] [CrossRef]
- Powers, M.E.; Arnold, B.L.; Weltman, A.L.; Perrin, D.H.; Mistry, D.; Kahler, D.M.; Kraemer, W.; Volek, J. Creatine Supplementation Increases Total Body Water Without Altering Fluid Distribution. J. Athl. Train. 2003, 38, 44–50. [Google Scholar]
- Lambrych, M. Caffeine. In Encyclopedia of Toxicology, Fourth Edition: Volume 1–9; StatPearls Publishing: Treasure Island, FL, USA, 2023; Volume 2, pp. 417–425. [Google Scholar] [CrossRef]
- Kreutzer, A.; Graybeal, A.J.; Moss, K.; Braun-Trocchio, R.; Shah, M. Caffeine Supplementation Strategies Among Endurance Athletes. Front. Sports Act. Living 2022, 4, 821750. [Google Scholar] [CrossRef]
- Graham, T.E.; Helge, J.W.; MacLean, D.A.; Kiens, B.; Richter, E.A. Caffeine Ingestion Does Not Alter Carbohydrate or Fat Metabolism in Human Skeletal Muscle during Exercise. J. Physiol. 2000, 529, 837–847. [Google Scholar] [CrossRef]
- Fiani, B.; Zhu, L.; Musch, B.L.; Briceno, S.; Andel, R.; Sadeq, N.; Ansari, A.Z. The Neurophysiology of Caffeine as a Central Nervous System Stimulant and the Resultant Effects on Cognitive Function. Cureus 2021, 13, e15032. [Google Scholar] [CrossRef] [PubMed]
- Guest, N.S.; VanDusseldorp, T.A.; Nelson, M.T.; Grgic, J.; Schoenfeld, B.J.; Jenkins, N.; Arent, S.M.; Antonio, J.; Stout, J.R.; Trexler, E.T.; et al. International Society of Sports Nutrition Position Stand: Caffeine and Exercise Performance. J. Int. Soc. Sports Nutr. 2021, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- Yang, A.; Palmer, A.A.; De Wit, H. Genetics of Caffeine Consumption and Responses to Caffeine. Psychopharmacology 2010, 211, 245–257. [Google Scholar] [CrossRef]
- Lara, B.; Ruiz-Moreno, C.; Salinero, J.J.; Coso, J. Del. Time Course of Tolerance to the Performance Benefits of Caffeine. PLoS ONE 2019, 14, e0210275. [Google Scholar] [CrossRef]
- Hobson, R.M.; Saunders, B.; Ball, G.; Harris, R.C.; Sale, C. Effects of β-Alanine Supplementation on Exercise Performance: A Meta-Analysis. Amino Acids 2012, 43, 25–37. [Google Scholar] [CrossRef]
- Wender, C.L.A.; Manninen, M.; O’Connor, P.J. The Effect of Chronic Exercise on Energy and Fatigue States: A Systematic Review and Meta-Analysis of Randomized Trials. Front. Psychol. 2022, 13, 907637. [Google Scholar] [CrossRef]
- Sweeney, K.M.; Wright, G.A.; Glenn Brice, A.; Doberstein, S.T. The Effect of Beta-Alanine Supplementation on Power Performance During Repeated Sprint Activity. J. Strength Cond. Res. 2010, 24, 79–87. [Google Scholar] [CrossRef]
- Cimadevilla-Fernández-Pola, E.; Martínez-Roldán, C.; Maté-Muñoz, J.L.; Guodemar-Pérez, J.; Sánchez-Calabuig, M.A.; García-Fernández, P.; Hervás-Pérez, J.P.; Hernández-Lougedo, J. Effects of β-Alanine Supplementation on Subjects Performing High-Intensity Functional Training. Nutrients 2024, 16, 2340. [Google Scholar] [CrossRef]
- Culbertson, J.Y.; Kreider, R.B.; Greenwood, M.; Cooke, M. Effects of Beta-Alanine on Muscle Carnosine and Exercise Performance: A Review of the Current Literature. Nutrients 2010, 2, 75–98. [Google Scholar] [CrossRef]
- Macuh, M.; Knap, B. Effects of Nitrate Supplementation on Exercise Performance in Humans: A Narrative Review. Nutrients 2021, 13, 3183. [Google Scholar] [CrossRef]
- Bentley, R.F.; Walsh, J.J.; Drouin, P.J.; Velickovic, A.; Kitner, S.J.; Fenuta, A.M.; Tschakovsky, M.E. Dietary Nitrate Restores Compensatory Vasodilation and Exercise Capacity in Response to a Compromise in Oxygen Delivery in the Noncompensator Phenotype. J. Appl. Physiol. 2017, 123, 594–605. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.M. Dietary Nitrate Supplementation and Exercise Performance. Sports Med. 2014, 44 (Suppl. S1), 35. [Google Scholar] [CrossRef] [PubMed]
- Husmann, F.; Bruhn, S.; Mittlmeier, T.; Zschorlich, V.; Behrens, M. Dietary Nitrate Supplementation Improves Exercise Tolerance by Reducing Muscle Fatigue and Perceptual Responses. Front. Physiol. 2019, 10, 404. [Google Scholar] [CrossRef]
- Tan, R.; Cano, L.; Lago-Rodríguez, Á.; Domínguez, R. The Effects of Dietary Nitrate Supplementation on Explosive Exercise Performance: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 762. [Google Scholar] [CrossRef]
- Calvo, J.L.; Alorda-Capo, F.; Pareja-Galeano, H.; Jiménez, S.L. Influence of Nitrate Supplementation on Endurance Cyclic Sports Performance: A Systematic Review. Nutrients 2020, 12, 1796. [Google Scholar] [CrossRef]
- Silva, K.V.C.; Costa, B.D.; Gomes, A.C.; Saunders, B.; Mota, J.F. Factors That Moderate the Effect of Nitrate Ingestion on Exercise Performance in Adults: A Systematic Review with Meta-Analyses and Meta-Regressions. Adv. Nutr. 2022, 13, 1866–1881. [Google Scholar] [CrossRef]
- Buzdağlı, Y.; Eyipınar, C.D.; Öget, F.; Şıktar, E.; Forbes, S.C.; Tekin, A. Taurine Supplementation Enhances Anaerobic Power in Elite Speed Skaters: A Double-Blind, Randomized, Placebo-Controlled, Crossover Study. Biol. Sport 2023, 40, 741–751. [Google Scholar] [CrossRef]
- Thirupathi, A.; Pinho, R.A.; Baker, J.S.; István, B.; Gu, Y. Taurine Reverses Oxidative Damages and Restores the Muscle Function in Overuse of Exercised Muscle. Front. Physiol. 2020, 11, 582449. [Google Scholar] [CrossRef]
- De Luca, A.; Pierno, S.; Camerino, D.C. Taurine: The Appeal of a Safe Amino Acid for Skeletal Muscle Disorders. J. Transl. Med. 2015, 13, 243. [Google Scholar] [CrossRef]
- Baliou, S.; Adamaki, M.; Ioannou, P.; Pappa, A.; Panayiotidis, M.I.; Spandidos, D.A.; Christodoulou, I.; Kyriakopoulos, A.M.; Zoumpourlis, V. Protective Role of Taurine against Oxidative Stress (Review). Mol. Med. Rep. 2021, 24, 605. [Google Scholar] [CrossRef]
- Kurtz, J.A.; VanDusseldorp, T.A.; Doyle, J.A.; Otis, J.S. Taurine in Sports and Exercise. J. Int. Soc. Sports Nutr. 2021, 18, 39. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Li, Z.; Pinho, R.A.; Gupta, R.C.; Ugbolue, U.C.; Thirupathi, A.; Gu, Y. The Dose Response of Taurine on Aerobic and Strength Exercises: A Systematic Review. Front. Physiol. 2021, 12, 700352. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, H.; Medlin, S.; Morehen, J.C. The Role of the Gut Microbiome and Probiotics in Sports Performance: A Narrative Review Update. Nutrients 2025, 17, 690. [Google Scholar] [CrossRef] [PubMed]
- Nami, Y.; Barghi, A.; Shahgolzari, M.; Salehian, M.; Haghshenas, B. Mechanism of Action and Beneficial Effects of Probiotics in Amateur and Professional Athletes. Food Sci. Nutr. 2024, 13, e4658. [Google Scholar] [CrossRef]
- Mazziotta, C.; Tognon, M.; Martini, F.; Torreggiani, E.; Rotondo, J.C. Probiotics Mechanism of Action on Immune Cells and Beneficial Effects on Human Health. Cells 2023, 12, 184. [Google Scholar] [CrossRef]
- Chandrasekaran, P.; Weiskirchen, S.; Weiskirchen, R. Effects of Probiotics on Gut Microbiota: An Overview. Int. J. Mol. Sci. 2024, 25, 6022. [Google Scholar] [CrossRef]
- Macarro, M.S.; Ávila-Gandía, V.; Pérez-piñero, S.; Cánovas, F.; García-muñoz, A.M.; Abellán-ruiz, M.S.; Victoria-montesinos, D.; Luque-rubia, A.J.; Climent, E.; Genovés, S.; et al. Antioxidant Effect of a Probiotic Product on a Model of Oxidative Stress Induced by High-intensity and Duration Physical Exercise. Antioxidants 2021, 10, 323. [Google Scholar] [CrossRef]
- Charitos, I.A.; Colella, M.; Carretta, D.M.; Santacroce, L. Probiotics, Gut Microbiota and Physical Activity: A Close Relationship. Sports Med. Health Sci. 2025; in press. [Google Scholar] [CrossRef]
- Wegierska, A.E.; Charitos, I.A.; Topi, S.; Potenza, M.A.; Montagnani, M.; Santacroce, L. The Connection Between Physical Exercise and Gut Microbiota: Implications for Competitive Sports Athletes. Sports Med. 2022, 52, 2355–2369. [Google Scholar] [CrossRef]
- Ansari, F.; Neshat, M.; Pourjafar, H.; Jafari, S.M.; Samakkhah, S.A.; Mirzakhani, E. The Role of Probiotics and Prebiotics in Modulating of the Gut-Brain Axis. Front. Nutr. 2023, 10, 1173660. [Google Scholar] [CrossRef]
- Aragón-Vela, J.; González-Acevedo, O.; Plaza-Diaz, J.; Casuso, R.A.; Huertas, J.R. Physiological Benefits and Performance of Sea Water Ingestion for Athletes in Endurance Events: A Systematic Review. Nutrients 2022, 14, 4609. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Bustamante-Sanchez, Á.; Mielgo-Ayuso, J.; Martínez-Guardado, I.; Martín-Rodríguez, A.; Tornero-Aguilera, J.F. Antioxidants and Sports Performance. Nutrients 2023, 15, 2371. [Google Scholar] [CrossRef] [PubMed]
- Drobnic, F.; Storsve, A.B.; Burri, L.; Ding, Y.; Banquells, M.; Riera, J.; Björk, P.; Ferrer-roca, V.; Domingo, J.C. Krill-Oil-Dependent Increases in HS-Omega-3 Index, Plasma Choline and Antioxidant Capacity in Well-Conditioned Power Training Athletes. Nutrients 2021, 13, 4237. [Google Scholar] [CrossRef] [PubMed]
- Jäger, R.; Heileson, J.L.; Abou Sawan, S.; Dickerson, B.L.; Leonard, M.; Kreider, R.B.; Kerksick, C.M.; Cornish, S.M.; Candow, D.G.; Cordingley, D.M.; et al. International Society of Sports Nutrition Position Stand: Long-Chain Omega-3 Polyunsaturated Fatty Acids. J. Int. Soc. Sports Nutr. 2025, 22, 2441775. [Google Scholar] [CrossRef]
- Fernández-Lázaro, D.; Arribalzaga, S.; Gutiérrez-Abejón, E.; Azarbayjani, M.A.; Mielgo-Ayuso, J.; Roche, E. Omega-3 Fatty Acid Supplementation on Post-Exercise Inflammation, Muscle Damage, Oxidative Response, and Sports Performance in Physically Healthy Adults—A Systematic Review of Randomized Controlled Trials. Nutrients 2024, 16, 2044. [Google Scholar] [CrossRef]
- Hasani, M.; Arabpour, Z.; Hasani, M.; Saeedi, A.; Khodabakhshi, A. Effect of Astaxanthin on Physical Activity Factors, Lipid Profile, Inflammatory Markers, and Antioxidants Indices in Athletic Men: A Systematic Review and Meta-Analysis. J. Funct. Foods 2024, 122, 106477. [Google Scholar] [CrossRef]
- Jeukendrup, A. A Step towards Personalized Sports Nutrition: Carbohydrate Intake during Exercise. Sports Med. 2014, 44 (Suppl. S1), S25–S33. [Google Scholar] [CrossRef]
- Wang, Z.; Qiu, B.; Gao, J.; Del Coso, J. Effects of Caffeine Intake on Endurance Running Performance and Time to Exhaustion: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 148. [Google Scholar] [CrossRef]
- Turnagöl, H.H.; Koșar Șükran, N.; Güzel, Y.; Aktitiz, S.; Atakan, M.M. Nutritional Considerations for Injury Prevention and Recovery in Combat Sports. Nutrients 2022, 14, 53. [Google Scholar] [CrossRef]
- Burke, L.M. Supplements for Optimal Sports Performance. Curr. Opin. Physiol. 2019, 10, 156–165. [Google Scholar] [CrossRef]
- Petróczi, A.; Naughton, D.P. Supplement Use in Sport: Is There a Potentially Dangerous Incongruence between Rationale and Practice? J. Occup. Med. Toxicol. 2007, 2, 4. [Google Scholar] [CrossRef]
- Perez-Montilla, J.J.; Cuevas-Cervera, M.; Gonzalez-Muñoz, A.; Garcia-Rios, M.C.; Navarro-Ledesma, S. Efficacy of Nutritional Strategies on the Improvement of the Performance and Health of the Athlete: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 4240. [Google Scholar] [CrossRef] [PubMed]
- Woźniak, K.; Hedesz, P.; Żuk-Łapan, A.; Jung, M.; Gardian-Baj, M.; Popczyńska, J.; Doryń, A.; Jung, M.; Babula, E.; Włodarczyk, A.; et al. Nutrition Strategies for Optimizing Performance and Health in Young Athletes. J. Educ. Health Sport 2024, 60, 11–33. [Google Scholar] [CrossRef]
- Sharma, S.K.; Gaur, S. Optimizing Nutritional Outcomes: The Role of AI in Personalized Diet Planning. Int. J. Res. Publ. Semin. 2024, 15, 107–116. [Google Scholar] [CrossRef]


| Research | Level |
|---|---|
| Frentsos and Baer, 1997 [53] | B |
| Kimber et al., 2002 [54] | A |
| Jeukendrup et al., 2005 [55] | A |
| Gillum et al., 2006 [56] | B |
| Strock et al., 2006 [57] | A |
| Bentley et al., 2008 [58] | A |
| Neubauer et al., 2010 [59] | A |
| Pahnke et al., 2010 [60] | A |
| Cox et al., 2010 [61] | A |
| Gonçalves et al., 2011 [62] | B |
| Barrero et al., 2015 [63] | A |
| Wilson et al., 2015 [64] | B |
| Doering et al., 2016 [65] | B |
| Sareban et al., 2016 [66] | A |
| De Carvalho et al., 2017 [67] | A |
| Getzin et al., 2017 [68] | A |
| Hotfiel et al., 2019 [69] | A |
| Huang et al., 2019 [70] | A |
| McKay et al., 2020 [71] | A |
| Storsve et al., 2020 [72] | A |
| Burgos et al., 2022 [73] | A |
| Burgos et al., 2022 [74] | A |
| Martínez-Olcina et al., 2022 [75] | A |
| González-Acevedo et al., 2022 [76] | A |
| Tan et al., 2022 [77] | A |
| Durkalec-Michalski eta l., 2023 [78] | A |
| Lee, et al., 2023 [35] | A |
| Bennett et al., 2023 [79] | A |
| Jiménez-Alfageme et al., 2023 [80] | A |
| Witkoś et al., (2023) [81] | B |
| Wei et al., 2024 [82] | B |
| de Oliveira et al., 2024 [83] | B |
| Aragón-Vela et al., 2024 [84] | A |
| Mendes et al., 2025 [85] | B |
| Langa et al., 2025 [16] | A |
| Knowledge Area | Journal | Q | Authors | Population | Age Ranges (Years) | Triathlon Type | Method | Intervention | Variables | Results Analysed | Main Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Md | Int. J. Sport Nutr. Exerc. Metab. | 1 | Frentsos and Baer, 1997 [53] | Elite 4 ♂/2 ♀ | 31.0 ± 3.0 | IM | DB | Modification of Int of N; + of Int of CHO; adjustment of Pt for post-exercise; regulation of Int of fats; plans for greater H | Total calories consumed; proportion of mcN scheduled for the test; moment of Int of the N | Composition of nutritional supplements; dietary Int; food Int patterns; competition dietary practices; | An adequate Int of N is necessary to improve the P of End |
| The + of Int of CHO allows you to delay the F and improve the End | |||||||||||
| The B between mcN favours Rcv | |||||||||||
| Md | Int. J. Sport Nutr. Exerc. Metab. | 1 | Kimber et al., 2002 [54] | 10 ♂–y 8 ♀ | 35.25 ± 8.3 | IM | DB | Laboratory test; incremental ramp test; MD&W [86] | hg; BW; %BF; FM; FFM; BMI; EI; EE; VO2; s; CHO intake | EI during cycling and running; mcN Int and Na; EE; EB | Despite the negative EB, the average EI seemed sufficient before reaching substrate depletion |
| CHO Int adequate to satisfy the maximum rates of plasma glucose oxidation by skeletal muscle | |||||||||||
| The increase in EI may have improved the performance of the ♂ | |||||||||||
| The increase in total CHO and EI were not related to faster completion times in ♀ | |||||||||||
| SM | Sport. Med. | 1 | Jeukendrup et al., 2005 [55] | - | - | - | DB | Ig strategies of CHO, H and Rcv | Int of CHO; H; synthesis of G; sporting P; medical problems | Loading of CHO; H; Post-exercise recovery | Nt is important for improving P and Rcv |
| Int of CHO and an H with Na help to maintain the E and prevent the Hn | |||||||||||
| A well-designed nutritional strategy optimises P and reduces health risks | |||||||||||
| SM | Int. J. Sports Physiol. Perform. | 2 | Gillum et al., 2006 [56] | 1 ♂ | 38 | LD | DB | Analysis of muscle G depletion and resynthesis before, during and after competition | Consumption of CHO, Pt and fats, energy excretion and oxidation of substrates, muscle G levels | BW; muscle G; CHO consumption | CHO intake is essential |
| Eccentric muscle damage from running can affect G resynthesis | |||||||||||
| STR | Phys. Med. Rehabil. Clin. N. Am. | 2 | Strock et al., 2006 [57] | Triathletes of diverse levels, from amateur to professional | - | - | S | Theoretical revision | Nt and H strategies; thermal problems and temperature regulation | Conditioning; nutritional aspects; thermoregulation; | Nutritional planning and adequate H are fundamental for the P and safety |
| STR | J. Sci. Med. Sport | 1 | Bentley et al., 2008 [58] | - | - | - | S | Analysis of strategies to improve P in running | EC; CHO; Pt; fluid loss; rest and recovery; V and I; thermal regulation; VO2max; lactate threshold | Adequate consumption of CHO pre- and post-test; Int of Pt post-exercise; H; sweating; electrolytes | Individual Nt, H and Rcv are needed to help the body readapt |
| Acclimatisation is important to avoid F and improve heat tolerance | |||||||||||
| Well-structured training is important (St, End, and s) | |||||||||||
| Md | Br. J. Nutr. | 1 | Neubauer et al., 2010 [59] | 42 ♂ | 35.3 ± 7.0 | IM | S | Free consumption during the competition | Endogenous and exogenous antioxidants in plasma; markers of oxidative stress; oxidative damage to DNA | Plasma antioxidant capacity; ORAC ratio and oxidative damage to DNA; carotenoids and α-tocopherol | The acute post-exercise antioxidant response of ultra-end can prevent oxidative damage to DNA |
| Need for nutritional antioxidants during Rcv | |||||||||||
| Special attention in the Rcv diet | |||||||||||
| STR | Med. Sci. Sports Exerc. | 1 | Pahnke et al., 2010 [60] | 26 ♂–20 ♀ | 46.65 ± 10.65 | IM | DB | [Na] in serum; BM; sweating; Int of Na and fluids | [Na] in serum and BW, pre/post-race; recording of fluids and [Na] during the race | Sweating analysis trial; Serum [Na]; race day results; Int during the race of mcN, Na, K, and fluid | The change in [Na] during the ultra-end exercise is related to the change in BMI and to the rate of Na loss through sweat |
| The rate of Na loss through sweat and the changes in serum Na were clear in ♂, but not so clear in ♀ | |||||||||||
| Although the ♀ compensated their Na losses better through Na Int, the ♀ consumed more liquids than the ♂ | |||||||||||
| This higher fluid Int in the ♀ may partly explain their slightly greater decrease in serum Na on the day of the race than in the ♂ | |||||||||||
| Md | Int. J. Sport Nutr. Exerc. Metab. | 1 | Cox et al., 2010 [61] | 36 ♂–15 ♀ elite | Under-23 | OT | S | Self-reported prerace and during-race nutrition data were collected at three separate OT events | CHO Int pre/post and during the race; race time; temperature and humidity during the race; differences in CHO Int according to gender | Nutrient-Int analysis | Elite triathletes usually comply with the Int recommendations of pre-race CHO, but have difficulties in achieving them during the race |
| Md | Clinics | 2 | Gonçalves et al., 2011 [62] | 10 ♂ | 34 ± 7 | - | DB | Measurement of blood parameters; capillary microcirculation | Glucose; insulin; uric acid; superoxide dismutase; functional capillary density; diameter of capillaries; resting erythrocyte flow velocity; time to reach peak velocity after occlusion; BW; %FM; %FFM; mcN | OGJ consumption for 20 days; HOMA2-IR index; uric acid; E-SOD; polyphenols; capillary density; peak erythrocyte flow velocity; time to reach peak s; diameter of afferent, efferent and apical capillaries; BW; %FM; %FFM | OGJ Int improved blood glucose, antioxidant capacity and microvascular function, without affecting BW or BC |
| The observed benefits can be attributed to a high polyphenol content, which could favour P and cardiovascular health | |||||||||||
| FS | Nutrients | 1 | Barrero et al., 2015 [63] | 11 ♂ | 36.8 ± 5.1 | UE | S | Nutrition record and H; physiological variables | EI and EE during competition; BM; TBW; ICW; ECW; Int of CHO, proteins and lipids; relationship of fluid loss and Int of CHO, with sports P | P; mcN Int; Fluid and Na Int; EB; BM and bioimpedance bioelectricity variables; relationship between racing P and parameters assessed during the race | E demands significantly > than Int |
| Loss of BM associated with fluid depletion and depletion of G and fat reserves | |||||||||||
| CHO supplementation was key for P, and ∃ the need for personalised strategies to optimise Pt Int and lipids | |||||||||||
| ND | J. Am. Coll. Nutr. | 2 | Wilson et al., 2015 [64] | 43 ♂–y 11 ♀ | 18–64 | UE | S | CHO Int and its impact on digestion | CHO Int; proportion of glucose and fructose in food and drink; Na Int, proteins, fats and caffeine | Participant characteristics; food composition and saccharide Int; GI distress and associations with saccharide Int | CHO consumption does not fulfil glucose–fructose recommendations |
| The higher consumption of glucose compared to fructose can lead to GI problems | |||||||||||
| Md | Int. J. Sport Nutr. Exerc. Metab. | 2 | Doering et al., 2016 [65] | 101 ♂–81 ♀ | 41.5 ± 7.5 | LD | S | Survey | Knowledge of recommended CHO and Pt post-exercise Int; actual consumption of CHO and Pt post-exercise; sources of information on Nt post-exercise; differences between age groups | Knowledge of post-exercise nutritional recommendations; post-exercise nutrition practices | Triathletes, regardless of age, have a poor understanding of the recommended post-exercise Nt |
| M have inadequate post-exercise dietary practices, consuming less CHO and Pt than recommended | |||||||||||
| Md | Int. J. Sport Nutr. Exerc. Metab. | 2 | Sareban et al., 2016 [66] | 9 triathletes | 38.6 ± 10.7 | LD | DB | CHO consumption during the test | Distance covered in the final race; RER; blood glucose and lactate; GI discomfort | Self-reported caloric Int during the 48-hr period before; P; fluid and CHO Int; glucose and lactate; RER; RPE; GI distress | The Int of CHO in gel does not improve the P in comparison with liquid CHO, but + GI discomfort |
| Ph | Front. Physiol. | 1 | De Carvalho et al., 2017 [67] | 10 ♂ | 30.9 ± 1.3 | LD | DB | Int Ta + low-fat chocolate milk | [Ta]; oxidative stress; protein metabolism; aerobic parameters | Oxidative stress and Pt metabolism marker levels; GSH; MDA; N ur; N2 B; vE; Urea; Creatinine | Supplementation with Ta did not improve Ae P, but it did improve oxidative stress and N2 balance, suggesting a possible protective effect on muscle catabolism |
| Md | Curr. Sports Med. Rep. | 3 | Getzin et al., 2017 [68] | - | - | DB | Int of CHO; special considerations for the obese triathlete | Distance; time; CHO Int differentiating between elite and non-elite triathletes and BM of each athlete | H; Int of CHO; caffeine; fluids; Na replacement; organic nitrates; exercise-induced GI syndrome; obesity | Reduction in the cost of O2 in the whole body, especially in low to moderate I exercise, improvement in tolerance and P; improvement in cognitive functioning | |
| Decrease in blood pressure due to the effect of NO on vascular control | |||||||||||
| STR | Sports | 1 | Hotfiel et al., 2019 [69] | Olympic level | - | OT | DB | Compression therapy; CWI; active regeneration; nutritional supplementation; sleep quality | Use of garments and intermittent pressure devices; CWI; impact of sleep quality and quantity on Rcv; active regeneration; supplementation with Pt, BCAAs, omega-3; H | EIMD; post-exercise compression; CWI; sleep pattern; supplementation with Pt and BCAAs; active regeneration | CWI is effective for the reduction of DOMS and inflammation, but could affect muscle G Rcv |
| A comprehensive approach that combines rest, nutrition and active Rcv optimises P | |||||||||||
| Personalisation is key, as each athlete responds≠ | |||||||||||
| Post-exercise compression appears to be effective in reducing MD, although there is no consensus on its impact on P | |||||||||||
| Muscle damage induced by EIMD affects P | |||||||||||
| Sleep is fundamental for muscle Rcv and injury prevention | |||||||||||
| Supplementation with Pt and BCAAs favours muscle repair and G resynthesis | |||||||||||
| Active regeneration, such as foam rolling and light pedalling after competition, may aid Rcv, but evidence is limited | |||||||||||
| ND | Am. J. Clin. Nutr. | 1 | Huang et al., 2019 [70] | 34 triathletes | 20.93 ± 0.93 | ST | DB | Daily supplementation with Lactobacillus plantarum PS128 capsules or placebo | CK, TRX, MPO), (TNF-α, IL-6, IL-10), (VO2max, Wingate), plasma amino acids; muscle F (lactate, ammonia), BC | BC Pre-Post SS; F and I-R BI; IC after IE; KI and MPO after IE; An and Ae ExC; Free AA Content after SS | Supplementation with L. plantarum PS128 + post-exercise Rcv |
| + levels of essential amino acids and maintains P after intensive exercise | |||||||||||
| Potential ergogenic aid for End athletes | |||||||||||
| Md | Int. J. Sport Nutr. Exerc. Metab. | 1 | McKay et al., 2020 [71] | 4 ♂–7 ♀ elite | 24.45 ± 2.5 | - | DB | CHO Prdt; inflammation and immune function; HIGH; LOW | HIGH; LOW; HIT; LIT; physiological and metabolic biomarkers; VO2max; HR; Int mcN; state of health | Effects of CHO Prdt on Fe regulation; inflammation and immune function; response to training and energy metabolism | CHO Prdt can be a useful tool for optimising adaptations to training with adequate management of the Fe Int |
| CHO PRT using the LOW strategy does not negatively affect inflammation or immune function | |||||||||||
| The restriction of nocturnal CHO + the post-exercise hepcidin response | |||||||||||
| Athletes in the LOW condition showed > dependence on fats as a source of E | |||||||||||
| The P in LI sessions was not affected by the CHO restriction | |||||||||||
| ND | Front. Nutr. | 1 | Storsve et al., 2020 [72] | 35 ♂–12 ♀ elite | 40.45 ± 8.6 | IM/OT | DB | Daily Spp before competition | Effect of krill oil supplementation on [choline] and its metabolites | Choline; betaine; DMG; other choline metabolites | Preventing [choline]—during long competitions, improving Rcv and P |
| FS | Nutrients | 1 | Burgos et al., 2022 [73] | 32 ♂ | 32.17 ± 4.87 | - | DB | Spp with Ci and/or BE rich in nitrates; physical tests | HJUMP; DYN; 1-MAT; Ct; Anthp | BC; somatotype; maximal St; End-St; Ae power | The combination of Ci and BE powers Ae |
| ABS | Biology (Basel) | 1 | Burgos et al., 2022 [74] | 32 ♂ | 34.37 ± 7.08 | - | DB | Supplementation | Dietary evaluation; hormones generated; Ct; Anthpc measurements | E and mcN Int; Anthp and BC; Ct; Serum EIMD markers; T-C status; T/C ratio | The combination of Ci-BE muscle damage markers |
| T/C | |||||||||||
| Rcv y la P | |||||||||||
| OG | Gels | 2 | Martínez-Olcina et al., 2022 [75] | 10 ♂ | 26.0 ± 8.7 | - | DB | Mouthwash | RPE; FS; FAS; POMS; blood glucose, sprints, and dietary habits | RPE; Fs; FAS; POMS; Int of CHO gel | Consumption of gel with CHO and mood |
| RPE, activation, blood glucose levels and P in Sprint | |||||||||||
| The level of activation over time | |||||||||||
| Pleasant sensation with a lower proportion in terms of RPE | |||||||||||
| PHEOH | Int. J. Environ. Res. Public Health | 2 | González-Acevedo et al., 2022 [76] | 10 ♂ | 38.8 ± 5.62 | - | DB | Specific H | Haematological measurements; cytokine and cytokine Pt | Anthp and physiological characteristics; alterations in blood cytokine and myokine Pt levels | H, keeping plasma V constant |
| Rcv time in End | |||||||||||
| Use of fats as a source of E and metabolic adaptation | |||||||||||
| FS | Nutrients | 1 | Tan et al., 2022 [77] | 12 ♂–9 ♀ elite | 18.9 ± 1.6 | - | S | Nutrition in training; H; mcN; micronutrients; supplements | SNKQ; dietary Int assessment | Sports nutrition knowledge; dietary Int; E; CHO; Pt; Fat; Ca; Fe | Nutritional knowledge and caloric intake to the demands of training |
| + Int of Ca and CHO, optimising P and health | |||||||||||
| FS | Nutrients | 1 | Durkalec-Michalski et al., 2023 [78] | 18 ♂–2 ♀ | 32 ± 7 | - | DB | An observational study carried out during two macrocycles of training specific to triathlon | Dietary record for three consecutive pre-test days; ICT to evaluate aerobic fitness; mineral content analysis | BM; h; BC; FM; FFM; TBW; EI; Pt; CHO; fat and dietary fibre Int; SFA; MUFA; PUFA; vitamins and minerals; Texh, VO2max; VO2VT; %VO2max_VT); HRmax; HRVT; WVT; niveles de Cu, Fe, Zn, Ca y Mg | E and nutritional values of the usual diets between training and competition |
| Fe content that may indicate an increase in nutritional needs during the competition period | |||||||||||
| Ae capacity during the competition period | |||||||||||
| Meaningful relationship between [Ca] and the absolute maximum uptake of O2 | |||||||||||
| % of maximum uptake of O2 in the VT | |||||||||||
| Lack of dietary periodisation based on training macrocycles | |||||||||||
| FS | Nutrients | 1 | Lee et al., 2023 [35] | 9 ♂–3 ♀ | 49.42 ± 5.9 | L | DB | Double-blind, crossover, placebo-controlled laboratory trial | [GSH]; superoxide dismutase, catalase, biological antioxidant potential | MF; skeletal muscle oxygenation; CF; BS; RPE | vC with natural antioxidant is more effective for metabolic function, skeletal muscle oxygenation, cardiac function, and antioxidant function in an End activity than a single SS of vC |
| SM | Scand. J. Med. Sci. Sport. | 1 | Bennett et al., 2023 [79] | 23 ♂ | 34 ± 7 | L | DB | Randomised control trial; battery of physiological tests; registered dietary intake; F qualification; H | V̇O2max; training program LIT and HIT; dietary Int; submaximal cycling test; TT | Training response; submaximal cycling test; TT; dietary Int | CHO Prdt improves metabolic adaptation, and the P |
| Prdt of CHO and HS did not provide additional benefits; in fact, it can impair the positive adaptations associated with the SL-TL diet | |||||||||||
| HS can compromise the oxidation capacity of CHO, which calls into question the effectiveness of training with low availability of CHO in warm conditions | |||||||||||
| FS | Nutrients | 1 | Jiménez-Alfageme et al., 2023 [80] | 165 ♂–67 ♀ | 34.79 ± 9.93 | - | S | Validated SS consumption questionnaire | SS consumption; BMI; type of SS; reasons for consumption; source of recommendation; sex; competitive level | SS consumed; distribution SS on sex, type, competitive level | Consumption of SS is high among triathletes |
| Professional nutritional advice is frequent | |||||||||||
| Considerable use of SS with little scientific evidence | |||||||||||
| 20% had or had had monthly MD that could indicate an immediate risk of LEA | |||||||||||
| 10% of participants were at physiological risk and of P related to RED-S | |||||||||||
| The number of reported injuries was higher in ♀ with MD, which may indicate that the lack of oestrogen can lead to a higher risk of injury | |||||||||||
| FS | Nutrients | 1 | Witkoś et al., 2023 [81] | 30 ♀ | 33.5 ± 9.2 | IM | DB | BC; LEAF-Q questionnaire | Incidence of injuries; GI problems; menstrual cycle disorders | hg; BM; BMI; FM; VAT; FFM; MM; TBW; ECW; monthly cycle disorders | LEAF-Q allowed for the early detection of FAT symptoms in several of the triathletes studied |
| 20% of the triathletes had or had had monthly cycle disorders that could indicate an immediate risk of LEA | |||||||||||
| 10% of the triathletes were at physiological and performance risk related to RED-S. The number of injuries reported in ♀ triathletes was higher in those ♀ with menstrual disorders compared to those ♀ without them, which may indicate that a lack of oestrogen can lead to a higher risk of injury | |||||||||||
| SM | Sport. Med. Heal. Sci. | 2 | Wei et al., 2024 [82] | 13 elite triathletes | 20.3 ± 0.5 | OT/ST | S | Stroop colour–word test | Identify metabolically active regions; haemodynamic measurements | Regions with high glucose uptake; Stroop colour–word test; haemodynamic changes | Connection between the rectum and cognitive P |
| Powerful intervention capable of improving cognitive P | |||||||||||
| SM | Med. Sci. Sports Exerc. | 1 | de Oliveira et al., 2024 [83] | 724 ♂ | 38 ± 10 | S | Questionnaire | Age, BMI, height, whether or not they take SS, nutritional advice, and the scope of this advice | Use of SS by categories; number of SS; amount of SS used; nutritionist guidance | The majority of triathletes took SS, 25% did not receive services from professionals | |
| Md | J. Clin. Med. | 1 | Aragón-Vela et al., 2024 [84] | 19 ♂ | 39.0 ± 4.25 | - | DB | DSW supplementation; compared with two additional H conditions: isotonic placebo and tap water | H; Isometric muscle St; CMJ | Anthp; time; BM; RPE; and temperature of the test; CMJ; isometric muscle St test | Preserve muscle St in isometric exercises post-exercise |
| CMJ | |||||||||||
| Delaying muscle F and preserving post-exercise muscle function in End | |||||||||||
| Ph | Braz. J. Med. Biol. Res. | 3 | Mendes et al., 2025 [85] | 61 ♂–11 ♀ | 34.5 ± 8.5 | OT | S | Survey conducted using an online questionnaire on the Google Forms platform. The questionnaire included multiple choice and open questions. | Amount of training; gastrointestinal discomfort when ingesting CHO; types of CHO, whether they had nutritional advice and the time of the competition; gender; strategy of CHO use; amount of CHO | 48.6% of triathletes reported having compensated for CHO before competitions. 86.1% of the triathletes had used CHO during competitions. Only two athletes ingested 60 g/h, and the average intake was 22.1 g/h | The quantities ingested were not always those recommended because only some of the participants received professional advice |
| FS | Nutrients | 1 | Langa et al., 2025 [16] | 20 ♀ | 5.5 ± 2.5 | IM | DB | Three-day food diary form; training diary; LEAF-Q | Baseline characteristics of high-P; dietary assessment; REE; EEE; PAL; TEE; LEA in females’ questionnaire | LEA in female’s questionnaire scores; diet; REE; aTEE; rTEE; aEI; rEI; aED; rED; LLEA; H-LEA; training load; dietary Int of mcN; PPROT; PUFA; PUFAn6; PUFAn3; MUFA; SFA; fibre Int; dietary Int of micronutrients—Fe and Ca | 30% of the participants were at risk of suffering RED-S, and 50% presented at least one symptom related to LEA |
| The diets consumed by triathletes who presented menstrual dysfunction, gastrointestinal symptoms and/or lesions were richer in fibre, differed in the type of Pt and in the proportion of fatty acids with respect to the diets of triathletes without LEA symptoms, who consumed more saturated fatty acids. | |||||||||||
| Diets rich in fibre and vegetable Pt may put ♀ at risk of RED-S. | |||||||||||
| The composition of dietary FM is essential for adequate E Int. Greater dependence on free fatty acids as E substrates |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miguel-Ortega, Á.; Rodríguez-Rodrigo, M.-A.; Mielgo-Ayuso, J.; Calleja-González, J. Triathlon: Ergo Nutrition for Training, Competing, and Recovering. Nutrients 2025, 17, 1846. https://doi.org/10.3390/nu17111846
Miguel-Ortega Á, Rodríguez-Rodrigo M-A, Mielgo-Ayuso J, Calleja-González J. Triathlon: Ergo Nutrition for Training, Competing, and Recovering. Nutrients. 2025; 17(11):1846. https://doi.org/10.3390/nu17111846
Chicago/Turabian StyleMiguel-Ortega, Álvaro, María-Azucena Rodríguez-Rodrigo, Juan Mielgo-Ayuso, and Julio Calleja-González. 2025. "Triathlon: Ergo Nutrition for Training, Competing, and Recovering" Nutrients 17, no. 11: 1846. https://doi.org/10.3390/nu17111846
APA StyleMiguel-Ortega, Á., Rodríguez-Rodrigo, M.-A., Mielgo-Ayuso, J., & Calleja-González, J. (2025). Triathlon: Ergo Nutrition for Training, Competing, and Recovering. Nutrients, 17(11), 1846. https://doi.org/10.3390/nu17111846









