The Impact of Flaxseed (Linum usitatissimum L.) Oil Supplementation on Human Health: A Human-Centric Evidence-Graded Approach
Abstract
1. Introduction
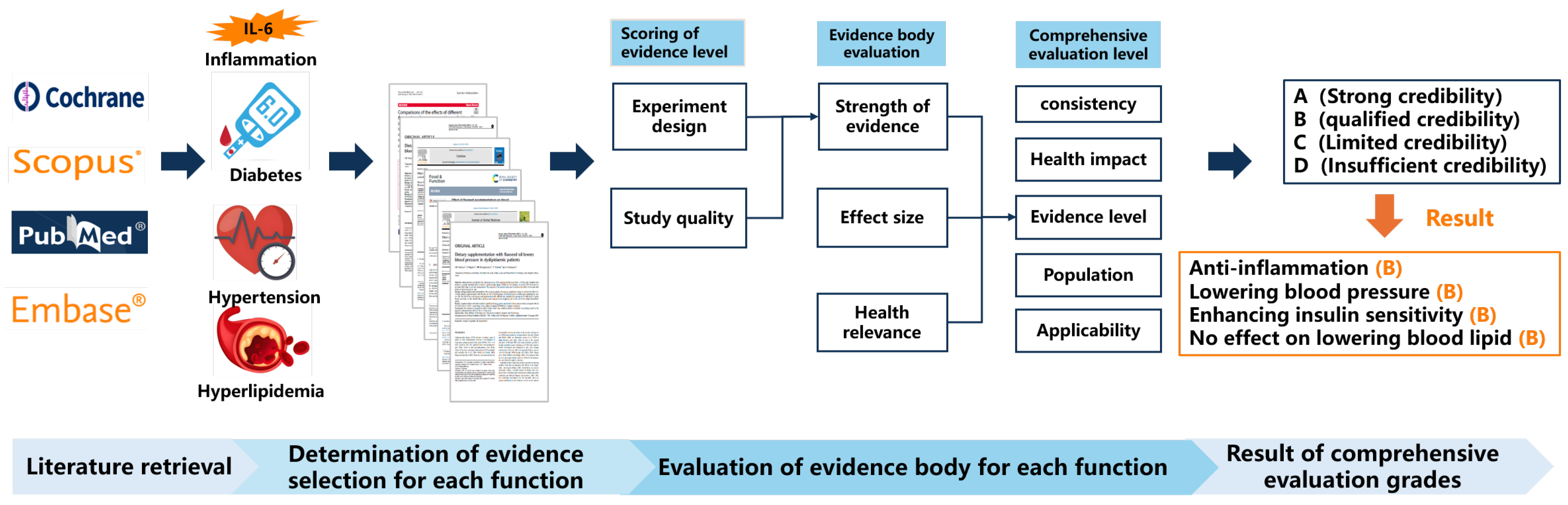
2. Methods
2.1. Literature Search
2.2. Inclusion Criteria and Exclusion
2.3. Evidence Quality Evaluation
3. Results
3.1. Literature Search and Screening
3.2. The Health Benefits of Flaxseed Oil Grading by Evidence Evaluation
3.2.1. Anti-Inflammation
3.2.2. Lowering Blood Pressure
3.2.3. Enhancing Insulin Sensitivity
3.2.4. No Effect on Lowering Blood Lipid
3.3. Uncertain Health Benefits of Flaxseed Oil
3.3.1. Reducing Waist Circumference
3.3.2. Improvement of Mood and Cognition
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Kauser, S.; Hussain, A.; Ashraf, S.; Fatima, G.; Javaria, S.; Abideen, Z.U.; Kabir, K.; Yaqub, S.; Akram, S.; Shehzad, A.; et al. Flaxseed (Linum usitatissimum); Phytochemistry, Pharmacological Characteristics and Functional Food Applications. Food Chem. Adv. 2024, 4, 100573. [Google Scholar] [CrossRef]
- Hirst, B.C.; Dibrov, E.; Hirst, S.D.; Pierce, G.N. Physiological and Pathological Considerations for the Use of Flaxseed as a Therapeutic Dietary Strategy. Rev. Cardiovasc. Med. 2023, 24, 149. [Google Scholar] [CrossRef]
- Shim, Y.Y.; Gui, B.; Wang, Y.; Reaney, M.J. Flaxseed (Linum usitatissimum L.) Oil Processing and Selected Products. Trends Food Sci. Tech. 2015, 43, 162–177. [Google Scholar] [CrossRef]
- Goyal, A.; Sharma, V.; Upadhyay, N.; Gill, S.; Sihag, M. Flax and Flaxseed Oil: An Ancient Medicine & Modern Functional Food. J. Food Sci. Technol. 2014, 51, 1633–1653. [Google Scholar] [PubMed]
- Nowak, W.; Jeziorek, M. The Role of Flaxseed in Improving Human Health. Healthcare 2023, 11, 395. [Google Scholar] [CrossRef]
- Calder, P.C. Mechanisms of Action of (n-3) Fatty Acids. J. Nutr. 2012, 142, 592S–599S. [Google Scholar] [CrossRef]
- Gertser, H. Can Adults Adequately Convert Alpha-Linolenic Acid to Eicosapentaenoic Acid and Docosahexaenoic Acid? Int. J. Vitam. Nutr. Res. 1998, 68, 159–173. [Google Scholar]
- World Health Organization. WHO Handbook for Guideline Development, 2nd ed.; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Akl, E.A.; Kennedy, C.; Konda, K.; Caceres, C.F.; Horvath, T.; Ayala, G.; Doupe, A.; Gerbase, A.; Wiysonge, C.S.; Segura, E.R.; et al. Using GRADE Methodology for the Development of Public Health Guidelines for the Prevention and Treatment of HIV and Other STIs Among Men Who Have Sex with Men and Transgender People. BMC Public Health 2012, 12, 386. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. Food and Health Evidence Based Review; People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- Chinese Nutrition Society. Chinese Dietary Guidelines; People’s Medical Publishing House: Beijing, China, 2022. [Google Scholar]
- Basch, E.; Mphil, S.B.; Collins, J.; Dacey, C.; Harrison, M.; Szapary, P. Flax and Flaxseed Oil (Linum usitatissimum): A Review. J. Soc. Integr. Oncol. 2007, 5, 92–105. [Google Scholar] [CrossRef]
- Yang, C.; Xia, H.; Wan, M.; Lu, Y.; Xu, D.; Yang, X.; Yang, L.; Sun, G. Comparisons of the Effects of Different Flaxseed Products Consumption on Lipid Profiles, Inflammatory Cytokines and Anthropometric Indices in Patients with Dyslipidemia Related Diseases: Systematic Review and a Dose–Response Meta-Analysis of Randomized Controlled Trials. Nutr. Metab. 2021, 18, 91. [Google Scholar]
- Askarpour, M.; Karimi, M.; Hadi, A.; Ghaedi, E.; Symonds, M.E.; Miraghajani, M.; Javadian, P. Effect of Flaxseed Supplementation on Markers of Inflammation and Endothelial Function: A Systematic Review and Meta-Analysis. Cytokine 2020, 126, 154922. [Google Scholar] [CrossRef]
- Jiang, W.; Liang, J.; Xiong, M.; Dong, Y. Efficacy of Flaxseed Oil Compared with Fish Oil Supplementation in the Treatment of Coronary Heart Disease: A Retrospective Study. J. Thorac. Dis. 2022, 14, 396. [Google Scholar] [CrossRef]
- Li, L.; Li, H.; Gao, Y.; Zhang, X.; Yang, M. Effect of Flaxseed Supplementation on Blood Pressure: A Systematic Review and Dose-Response Meta-Analysis of Randomized Clinical Trials. Food Funct. 2023, 14, 675–690. [Google Scholar] [CrossRef] [PubMed]
- Mahmudiono, T.; Jasim, S.A.; Karim, Y.S.; Bokov, D.O.; Abdelbasset, W.K.; Akhmedov, K.S.; Yasin, G.; Thangavelu, L.; Mustsfa, Y.F.; Shoukat, S.; et al. The Effect of Flaxseed Oil Consumption on Blood Pressure Among Patients with Metabolic Syndrome and Related Disorders: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Phytother. Res. 2022, 36, 3766–3773. [Google Scholar] [CrossRef]
- Paschos, G.K.; Magkos, F.; Panagiotakos, D.B.; Votteas, V.; Zampelas, A. Dietary Supplementation with Flaxseed Oil Lowers Blood Pressure in Dyslipidaemic Patients. Eur. J. Clin. Nutr. 2007, 61, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Kavyani, Z.; Pourfarziani, P.; Kakhki, A.M.J.; Ahrabi, S.S.; Moridpour, A.H.; Mollaghasemi, N.; Musazadeh, V.; Faghfouri, A.H. The Effect of Flaxseed Supplementation on Glycemic Control in Adults: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Funct. Foods 2023, 110, 105816. [Google Scholar] [CrossRef]
- Soleimani, Z.; Hashemdokht, F.; Bahmani, F.; Taghizadeh, F.; Memarzadeh, M.R.; Asemi, Z. Clinical and Metabolic Response to Flaxseed Oil Omega-3 Fatty Acids Supplementation in Patients with Diabetic Foot Ulcer: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Diabetes Complicat. 2017, 31, 1394–1400. [Google Scholar] [CrossRef]
- Hajiahmadi, S.; Nadjarzadeh, A.; Gharipour, M.; Hosseinzadeh, M.; Fallahzadeh, H.; Mohsenpour, M.A. Effect of Flaxseed Oil on Glycemic Control and Inflammatory Markers in Overweight Adults with Pre-Diabetes: A Double-Blind Randomized Controlled Clinical Trial. J. Herb. Med. 2020, 24, 100387. [Google Scholar] [CrossRef]
- Jamilian, M.; Khademi, L.; Vahedpoor, Z.; Bahmani, F.; Mahmoodi, S.; Taghizadeh, M.; Asemi, Z. Effects of Flaxseed Oil Omega-3 Fatty Acids Supplementation on Regression and Metabolic Status in Endometrial Hyperplasia: A Randomized, Double-Blind, Placebo-Controlled Trial. Int. J. Prev. Med. 2019, 10, 61. [Google Scholar]
- Hadi, A.; Askarpour, M.; Salamat, S.; Ghaedi, E.; Symonds, M.E.; Miraghajani, M. Effect of Flaxseed Supplementation on Lipid Profile: An Updated Systematic Review and Dose-Response Meta-Analysis of Sixty-Two Randomized Controlled Trials. Pharmacol. Res. 2020, 152, 104622. [Google Scholar] [CrossRef]
- Rezaei, S.; Sasani, M.R.; Akhlaghi, M.; Kohanmoo, A. Flaxseed Oil in the Context of a Weight Loss Programme Ameliorates Fatty Liver Grade in Patients with Non-Alcoholic Fatty Liver Disease: A Randomised Double-Blind Controlled Trial. Br. J. Nutr. 2020, 123, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Musazadeh, V.; Abolghasemian, M.; Kavyani, Z.; Moridpour, A.H.; Nazari, A.; Faghfouri, A.H. The Effects of Flaxseed (Linum usitatissimum) Supplementation on Anthropometric Indices: An Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials. Complement. Ther. Med. 2024, 84, 103066. [Google Scholar] [CrossRef]
- Gracious, B.L.; Chirieac, M.C.; Costescu, S.; Finucane, T.L.; Youngstrom, E.A.; Hibbeln, J.R. Randomized, Placebo-Controlled Trial of Flax Oil in Pediatric Bipolar Disorder. Bipolar Disord. 2010, 12, 142–154. [Google Scholar] [CrossRef]
- Poorbaferani, F.; Rouhani, M.H.; Heidari, Z.; Poorbaferani, M.; Safavi, S.M. Flaxseed Oil Supplementation on Severity of Depression and Brain-Derived Neurotrophic Factor: A Randomized, Double-Blind Placebo Controlled Clinical Trial. Int. J. Food Prop. 2020, 23, 1518–1526. [Google Scholar] [CrossRef]
- Ogawa, T.; Sawane, K.; Ookoshi, K.; Kawashima, R. Supplementation with Flaxseed Oil Rich in Alpha-Linolenic Acid Improves Verbal Fluency in Healthy Older Adults. Nutrients 2023, 15, 1499. [Google Scholar] [CrossRef]
- Liu, C.; Chu, D.; Kalantar-Zadeh, K.; George, J.; Young, H.A.; Liu, G. Cytokines: From Clinical Significance to Quantification. Adv. Sci. 2021, 8, 2004433. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Karapetyan, E.; Dutta, P.; Shaheen, M.; Vadgama, J.V. Inflammatory Cytokines Associated with Obesity, Type-2 Diabetes, and Hypertension Exacerbate Breast Cancer Risk in Underserved African American and Latin American Women. J. Clin. Med. 2024, 13, 1687. [Google Scholar] [CrossRef] [PubMed]
- Frostegård, J. Autoimmunity, Oxidized LDL and Cardiovascular Disease. Autoimmun. Rev. 2002, 1, 233–237. [Google Scholar] [CrossRef]
- Sethwala, A.M.; Goh, I.; Amerena, J.V. Combating inflammation in cardiovascular disease. Heart Lung Circ. 2021, 30, 197–206. [Google Scholar] [CrossRef]
- Khan, H.A.; Khan, I.; Lee, Y.K. Role of Immune Factors in Bioavailability and Toxicity of Carbon Nanomaterials. In Fullerenes, Graphenes and Nanotubes; William Andrew Publishing: Norwich, NY, USA, 2018; pp. 601–630. [Google Scholar]
- Popko, K.; Gorska, E.; Stelmaszczyk-Emmel, A.; Plywaczewski, R.; Stoklosa, A.; Gorecka, D.; Pyrzak, B.; Demkow, U. Proinflammatory Cytokines Il-6 and TNF-α and the Development of Inflammation in Obese Subjects. Eur. J. Med. Res. 2010, 15 (Suppl. S2), 120. [Google Scholar] [CrossRef]
- Kubota, Y.; Higashiyama, A.; Imano, H.; Sugiyama, D.; Kawamura, K.; Kadota, A.; Nishimura, K.; Okamura, T. Serum Polyunsaturated Fatty Acid Composition and Serum High-Sensitivity C-Reactive Protein Levels in Healthy Japanese Residents: The Kobe Study. J. Nutr. Health Aging 2015, 19, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Seidu, S.; Lawson, C.A.; Kunutsor, S.K.; Khunti, K.; Rosano, G.M. Blood Pressure Levels and Adverse Cardiovascular Outcomes in Heart Failure: A Systematic Review and Meta-Analysis. Eur. J. Heart Fail. 2024, 26, 1111–1124. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Wang, X.; Yang, H.; Zhang, P.; Wu, F.; Li, Y.; Zhou, Y.; Zhang, X.; Ma, H.; Zhang, W.; et al. α-Linolenic Acid but Not Linolenic Acid Protects Against Hypertension: Critical Role of SIRT3 and Autophagic Flux. Cell Death Dis. 2020, 11, 83. [Google Scholar] [CrossRef]
- Ogawa, A.; Suzuki, Y.; Aoyama, T.; Takeuchi, H. Dietary α-Linolenic Acid Inhibits Angiotensin-Converting Enzyme Activity and mRNA Expression Levels in the Aorta of Spontaneously Hypertensive Rats. J. Oleo Sci. 2009, 58, 355–360. [Google Scholar] [CrossRef]
- Sekine, S.; Sasanuki, S.; Aoyama, T.; Takeuchi, H. Lowering Systolic Blood Pressure and Increases in Vasodilator Levels in SHR with Oral α-Linolenic Acid Administration. J. Oleo Sci. 2007, 56, 341–345. [Google Scholar] [CrossRef]
- Su, H.; Liu, R.; Chang, M.; Huang, J.; Jin, Q.; Wang, X. Effect of Dietary Alpha-Linolenic Acid on Blood Inflammatory Markers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eur. J. Nutr. 2018, 57, 877–891. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Leyva, D.; Weighell, W.; Edel, A.L.; LaVallee, R.; Dibrov, E.; Pinneker, R.; Maddaford, T.G.; Ramijawan, B.; Aliani, M.; Guzman, R.; et al. Potent Antihypertensive Action of Dietary Flaxseed in Hypertensive Patients. Hypertension 2013, 62, 1081–1089. [Google Scholar] [CrossRef]
- Caligiuri, S.P.B.; Edel, A.L.; Aliani, M.; Pierce, G.N. Flaxseed for Hypertension: Implications for Blood Pressure Regulation. Curr. Hypertens. Rep. 2014, 16, 499. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45 (Suppl. S1), S17–S38. [Google Scholar] [CrossRef]
- Singh, S.; Verma, J.; Gupta, N.; Kathak, P.A.; Tiwari, V.; Rajput, M.S.; Kulshrestha, M.R. Interplay of Toxic Metal Levels and Endoplasmic Reticulum Stress Gene Profile in Type 2 Diabetes Mellitus. Gene Rep. 2024, 37, 102019. [Google Scholar] [CrossRef]
- Asghari, K.M.; Saleh, P.; Salekzamani, Y.; Dolatkhah, N.; Aghamohammadzadeh, N.; Hashemian, M. The Effect of Curcumin and High-Content Eicosapentaenoic Acid Supplementations in Type 2 Diabetes Mellitus Patients: A Double-Blinded Randomized Clinical Trial. Nutr. Diabetes 2024, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.A.; Yang, Y.; Zhang, L.; Sun, Z.; Jia, G.; Parrish, A.R.; Sowers, J.R. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism 2021, 119, 154766. [Google Scholar] [CrossRef] [PubMed]
- Madan, R.; Varghese, R.T. Assessing Insulin Sensitivity and Resistance in Humans. Endotext; 2024. Available online: https://www.ncbi.nlm.nih.gov/sites/books/NBK278954/ (accessed on 20 December 2024).
- Yu, X.; Huang, H.S.; Deng, Q.; Tang, Y.; Yao, P.; Tang, H.; Dong, X. Linseed Oil Improves Hepatic Insulin Resistance in Obese Mice through Modulating Mitochondrial Quality Control. J. Funct. Foods 2019, 53, 166–175. [Google Scholar] [CrossRef]
- Chicco, A.G.; D’Alessandro, M.E.; Hein, G.J.; Oliva, M.E.; Lombardo, Y.B. Dietary Chia Seed (Salvia hispanica L.) Rich in α-Linolenic Acid Improves Adiposity and Normalises Hypertriacylglycerolaemia and Insulin Resistance in Dyslipaemic Rats. Br. J. Nutr. 2008, 101, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.S.; Ghosh, M. Antioxidant and Anti-Inflammatory Effect of Conjugated Linolenic Acid Isomers Against Streptozotocin-Induced Diabetes. Br. J. Nutr. 2012, 108, 974–983. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.I. Can Dietary Intervention Produce Long-Term Reduction in Insulin Resistance? Br. J. Nutr. 2000, 83 (Suppl. S1), S169–S172. [Google Scholar] [CrossRef]
- Kristensen, M.; Jensen, M.G.; Aarestrup, J.; Petersen, K.E.; Søndergaard, L.; Mikkelsen, M.S.; Astrup, A. Flaxseed Dietary Fibers Lower Cholesterol and Increase Fecal Fat Excretion, but Magnitude of Effect Depend on Food Type. Nutr. Metab. 2012, 9, 8. [Google Scholar] [CrossRef]
- Kajla, P.; Sharma, A.; Sood, D.R. Flaxseed—A Potential Functional Food Source. J. Food Sci. Technol. 2015, 52, 1857–1871. [Google Scholar] [CrossRef]
- Tse, T.J.; Guo, Y.; Shim, Y.Y.; Purdy, S.K.; Kim, J.H.; Cho, J.Y.; Alcorn, J.; Reaney, M.J. Availability of Bioactive Flax Lignan from Foods and Supplements. Crit. Rev. Food Sci. 2023, 63, 9843–9858. [Google Scholar] [CrossRef]
- Romeo, S. ACAT2 as a Novel Therapeutic Target to Treat Fatty Liver Disease. J. Intern. Med. 2022, 292, 175–176. [Google Scholar] [CrossRef]
- Pan, A.; Yu, D.; Demark-Wahnefried, W.; Franco, O.H.; Lin, X. Meta-Analysis of the Effects of Flaxseed Interventions on Blood Lipids. Am. J. Clin. Nutr. 2009, 90, 288–297. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Jeidell, S.J.; Magni, P.; Santos, R.D.; Arsenaul, B.; Cuevas, A.; Hu, F.B.; et al. Waist Circumference as a Vital Sign in Clinical Practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Yoo, E.G. Waist-to-Height Ratio as a Screening Tool for Obesity and Cardiometabolic Risk. Korean J. Pediatr. 2016, 59, 425. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi-Sartang, M.; Mazloom, Z.; Raeisi-Dehkordi, H.; Barati-Boldaji, R.; Bellissimo, N.; Totosy de Zepetnek, J.O. The Effect of Flaxseed Supplementation on Body Weight and Body Composition: A Systematic Review and Meta-Analysis of 45 Randomized Placebo-Controlled Trials. Obes. Rev. 2017, 18, 1096–1107. [Google Scholar] [CrossRef]
- Zhao, M.; Wang, B.; Li, L.; Zhao, W. Anti-Obesity Effects of Dietary Fibers Extracted from Flaxseed Cake in Diet-Induced Obese Mice. Nutrients 2023, 15, 1718. [Google Scholar] [CrossRef] [PubMed]
- Waddell, I.S.; Orfila, C. Dietary fiber in the prevention of obesity and obesity-related chronic diseases: From epidemiological evidence to potential molecular mechanisms. Crit. Rev. Food Sci. Nutr. 2023, 63, 8752–8767. [Google Scholar] [CrossRef]
- Bellicha, A.; van Baak, M.A.; Battista, F.; Beaulieu, K.; Blundell, J.E.; Busetto, L.; Carraça, E.V.; Dicker, D.; Encantado, J.; Ermolao, A.; et al. Effect of exercise training on weight loss, body composition changes, and weight maintenance in adults with overweight or obesity: An overview of 12 systematic reviews and 149 studies. Obes. Rev. 2021, 22, e13256. [Google Scholar] [CrossRef] [PubMed]
- Burns-Whitmore, B.; Froyen, E.; Heskey, C.; Parker, T.; San Pablo, G. Alpha-Linolenic and Linoleic Fatty Acids in the Vegan Diet: Do They Require Dietary Reference Intake/Adequate Intake Special Consideration? Nutrients 2019, 11, 2365. [Google Scholar] [CrossRef]
- Williams, J.A.; Batten, S.E.; Harris, M.; Rockett, B.D.; Shaikh, S.R.; Stillwell, W.; Wassall, S.R. Docosahexaenoic and Eicosapentaenoic Acids Segregate Differently Between Raft and Nonraft Domains. Biophys. J. 2012, 103, 228–237. [Google Scholar] [CrossRef]
- Crawford, M.A.; Broadhurst, C.L.; Guest, M.; Nagar, A.; Wang, Y.; Ghebremeskel, K.; Schmidt, W.F. A Quantum Theory for the Irreplaceable Role of Docosahexaenoic Acid in Neural Cell Signalling Throughout Evolution. Prostaglandins Leukot. Essent. Fat. Acids 2013, 88, 5–13. [Google Scholar] [CrossRef]
- Burdge, G.C.; Calder, P.C. Dietary α-Linolenic Acid and Health-Related Outcomes: A Metabolic Perspective. Nutr. Res. Rev. 2006, 19, 26–52. [Google Scholar] [CrossRef] [PubMed]
- DeMar, J.C., Jr.; Lee, H.J.; Ma, K.; Chang, L.; Bell, J.M.; Rapoport, S.I.; Bazinet, R.P. Brain Elongation of Linoleic Acid Is a Negligible Source of the Arachidonate in Brain Phospholipids of Adult Rats. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2006, 1761, 1050–1059. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi Fard, S.; Wang, F.; Sinclair, A.J.; Elliott, G.; Turchini, G.M. How Does High DHA Fish Oil Affect Health? A Systematic Review of Evidence. Crit. Rev. Food Sci. Nutr. 2019, 59, 1684–1727. [Google Scholar] [CrossRef] [PubMed]
- Lagarde, M.; Hachem, M.; Picq, M.; Guichardant, M.; Bernoud-Hubac, N. AceDoPC, a Structured Phospholipid to Target the Brain with Docosahexaenoic Acid. OCL 2016, 23, D102. [Google Scholar] [CrossRef]
| Disease | Comprehensive Grade | Level of Evidence | Consistency | Health Impact | Study Population | Applicability | |
|---|---|---|---|---|---|---|---|
| Inflammation | B | Grade | Good | Good | Good | Good | Good |
| Remarks | Two systematic reviews and one retrospective study (average score 12.8) | More than 70% of the studies are consistent | Flaxseed oil has a significant effect on improving inflammation. | Including Europe, America, Asia, and other countries | Suitable for most people | ||
| Hypertension | B | Grade | Good | Good | Excellent | Good | Good |
| Remarks | Two systematic reviews and one RCT (average score 12.6) | More than 70% of the studies are consistent | All study results show that intake of flaxseed oil can reduce blood pressure. | Including Europe, America, Asia, and other countries | Suitable for most people | ||
| Type 2 diabetes mellitus | B | Grade | Good | Good | Good | Good | Good |
| Remarks | One systematic review and three RCTs (average score 12.5) | More than 70% of the studies are consistent | More than 70% of the study results show that the intake of flaxseed oil increases insulin sensitivity. | Including Europe, America, Asia countries | Suitable for most people | ||
| Hyperlipidemia | B | Grade | Good | Good | Poor | Good | Good |
| Remarks | 2 systematic reviews and 1 RCT (average score 9.3) | More than 70% of the studies are consistent | All results showed that flaxseed oil has no significant effect on reducing blood lipid. | Including Europe, America, Asia countries | Suitable for Chinese, but with some exceptions |
| Yang et al. [13] | Askarpour et al. [14] | Jiang et al. [15] | |
|---|---|---|---|
| Study Type | In a systematic review, nine related RCTs are included in the subgroup. | In a systematic review, twenty-one related RCTs are included in the subgroup. | A retrospective study. |
| Investigation Method | 4–13 week intervention experiments. | 3–18 week intervention experiments. | A 15-week intervention experiment. |
| Number of Cases | 630 | 560 | 120 |
| Participants’ Characteristics | Dyslipidemia populations from China, Germany, Canada, Iran, Greece, and Brazil, male and female, 45–66 years old. | Populations from Australia, Iran, Brazil, America, Germany, Canada, Greece, and Finland, male and female, 24–68 years old. | Populations diagnosed with both T2DM and CHD from Hubei, China, male and female, 40–100 years old. |
| Intake Amount/Frequency | Intake of flaxseed oil at a dosage of 0.4 g–24 g/day, with the control group consuming soybean oil, corn oil, and sunflower oil for 4 to 13 weeks. | Intake of flaxseed oil containing 1.0–13.7 g/d of ALA, with the control group consuming sunflower oil, soybean oil, medium-chain fatty acids, olive oil, etc., over 3–18 weeks. | Intake of flaxseed oil at a dosage of 1.0 g/day, with the control group taking 1.0 g/day of paraffin oil, for 15 weeks. |
| Results | Reduction in IL-6 (−0.35 pg/mL, p = 0.033) and hs-CRP (−1.54 mg/L, p = 0.004). | For unhealthy or overweight populations, the intake of flaxseed oil for less than 12 weeks can reduce IL-6 by −0.268 (−0.393, −0.143), but does not affect reducing CRP and TNF-α. | There was a significant difference in hs-CRP (p = 0.02) in the flaxseed oil group, compared with the control group. |
| Impact on Risk | Protective | Protective | Protective |
| Li et al. [16] | Mahmudiono et al. [17] | Paschos et al. [18] | |
|---|---|---|---|
| Study Type | In a systematic review, eleven related RCTs are included in the subgroup. | In a systematic review, five related RCTs are included in the subgroup | RCT |
| Investigation Method | 4–24 week intervention experiments. | 6–12 week intervention experiments | A 12-week intervention experiment |
| Number of Cases | 734 | 117 | 87 |
| Participants’ Characteristics | Both healthy and unhealthy people from Finland, Canada, Australia, America, and Iran, male and female, 32–63 years old. | People with metabolic syndrome, hypercholesterolemia, and hypertension from Iran, the United States, Australia, China, and Greece, male and female, 49–56 years old | Dyslipidemia populations from Greece, male, 52–55 years old |
| Intake Amount/Frequency | Intake of flaxseed oil at a dosage of 1–30 g/day, with the control group consuming soybean oil, corn oil, sunflower oil, and hempseed oil for a period of 4 to 24 weeks. | Flaxseed oil was consumed at a dosage of 2.2–23 g/day, with the control group taking soybean oil, corn oil, sunflower oil, and safflower oil for a duration of 6 to 12 weeks | Consumption of 15 mL of flaxseed oil containing 8 g/day of ALA, with the control group consuming 15 mL of safflower oil containing 11 g/day of LA, over 12 weeks |
| Results | Subgroup analysis showed that flaxseed oil could reduce systolic blood pressure by a WMD of −1.04 (95% CI: −1.73, −0.72) and diastolic blood pressure by a WMD of −0.54 (95% CI: −0.71, −0.38). | Flaxseed oil could significantly reduce systolic blood pressure by −3.86 mmHg (−7.59, −0.13), but had no significant effect on the reduction in diastolic blood pressure compared to the control group | Flaxseed oil significantly reduced systolic blood pressure (p = 0.016) and diastolic blood pressure (p = 0.011) |
| Impact on Risk | Protective | Protective | Protective |
| Kavyani et al. [19] | Soleimani et al. [20] | Hajiahmadi et al. [21] | Jamilian et al. [22] | |
|---|---|---|---|---|
| Study Type | In a systematic review, seven related RCTs are included in the subgroup. | RCT | RCT | RCT |
| Investigation Method | 6–12 week intervention experiments. | 12-week intervention experiment | 14-week intervention experiment | 12-week intervention experiment |
| Number of Cases | 417 | 60 | 36 | 40 |
| Participants’ Characteristics | People with T2 DM, metabolic disorders, and non-alcoholic fatty liver from the USA, Canada, and Iran, including both men and women, 30–65 years old. | An Iranian population with diabetic foot ulcers, including both men and women, is around 40–85 years old | An Iranian population with overweight and prediabetes, including both men and women, around 40 years old | An Iranian population with endometrial hyperplasia but with normal blood sugar levels, women 44–47 years old |
| Intake Amount/Frequency | Intake of flaxseed oil at a dosage of 2.0–30.0 g/day, with the control group consuming paraffin oil and sunflower oil for 6 to 12 weeks. | Intake of 2.0 g/day flaxseed oil, with the control group consuming paraffin oil over 12 weeks | Intake of 2.0 g/day flaxseed oil, with the control group consuming paraffin oil over 14 weeks | Intake of 2.0 g/day flaxseed oil, with the control group consuming paraffin oil over 12 weeks |
| Results | Compared with the control group, QUICKI was significantly increased by WMD 1.76 (95% CI: 0.82, −2.71), (p < 0.001). | Compared with the control group, QUICKI was significantly increased (p < 0.02) | Compared with the control group, QUICKI was significantly increased (p < 0.001) | Compared with the control group, no significant differences in QUICKI between groups. However, fasting blood glucose was significantly decreased (p = 0.003) |
| Impact on Risk | Protective | Protective | Protective | Unprotective |
| Yang et al. [13] | Hadi et al. [23] | Rezaei et al. [24] | |
|---|---|---|---|
| Study Type | A systematic review, nine related RCTs are included in the subgroup. | A systematic review, thirty-two related RCTs are included in the subgroup. | RCT |
| Investigation Method | 4–13 week intervention experiments. | 3–27 week intervention experiments. | 12-week intervention experiment |
| Number of Cases | 554 | 950 | 68 |
| Participants’ Characteristics | Participants with T2DM, metabolic disorders, non-alcohol fatty liver, and hypertriglyceridemia from China, Canada, Germany, Greece, and Iran, including both men and women, 47–64 years old. | Participants with T2DM, CVD, hypercholesterolemia, and healthy people from Canada, Brazil, Germany, USA, Japan, Australia, Greece, Finland, the UK, and China, including men and women between 25 and 68 years old. | Iranian obesity patients with non-alcoholic fatty liver disease, including both men and women, 40–45 years old |
| Intake Amount/Frequency | Intake of flaxseed oil at a dosage of 2.0–25.0 g/day, with the control group consuming paraffin oil, sunflower oil, corn oil, safflower oil, and high-oleic canola oil for a period of 4 to 13 weeks. | Intake of flaxseed oil containing 1.0–21.0 g/day ALA, with the control group consuming paraffin oil, sunflower oil, corn oil, safflower oil, olive oil, and hempseed oil over a period of 3–27 weeks. | Intake of 20 mL/day of flaxseed oil, with the control group consuming sunflower oil over a period of 12 weeks |
| Results | Flaxseed oil intervention had no significant effect on total cholesterol, triglyceride, LDL-C, or HDL-C. | Flaxseed oil intervention had no significant effect on total cholesterol, triglyceride, LDL-C, or HDL-C. | There was no significant change in total cholesterol, HDL-C, or LDL-C compared with the control group (p > 0.01) |
| Impact on Risk | Unprotective | Unprotective | Unprotective |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nie, Y.; Wang, Y.; Hui, J.; Shao, D.; Chen, R.; Deng, Q.; Chen, Y.; Wang, X.; Zhu, D. The Impact of Flaxseed (Linum usitatissimum L.) Oil Supplementation on Human Health: A Human-Centric Evidence-Graded Approach. Nutrients 2025, 17, 1791. https://doi.org/10.3390/nu17111791
Nie Y, Wang Y, Hui J, Shao D, Chen R, Deng Q, Chen Y, Wang X, Zhu D. The Impact of Flaxseed (Linum usitatissimum L.) Oil Supplementation on Human Health: A Human-Centric Evidence-Graded Approach. Nutrients. 2025; 17(11):1791. https://doi.org/10.3390/nu17111791
Chicago/Turabian StyleNie, Ying, Yuchen Wang, Ju Hui, Danqing Shao, Ran Chen, Qianchun Deng, Yashu Chen, Xiangyu Wang, and Dazhou Zhu. 2025. "The Impact of Flaxseed (Linum usitatissimum L.) Oil Supplementation on Human Health: A Human-Centric Evidence-Graded Approach" Nutrients 17, no. 11: 1791. https://doi.org/10.3390/nu17111791
APA StyleNie, Y., Wang, Y., Hui, J., Shao, D., Chen, R., Deng, Q., Chen, Y., Wang, X., & Zhu, D. (2025). The Impact of Flaxseed (Linum usitatissimum L.) Oil Supplementation on Human Health: A Human-Centric Evidence-Graded Approach. Nutrients, 17(11), 1791. https://doi.org/10.3390/nu17111791






