The Impact of Dietary Habits and Nutrition Knowledge on Harmful Alcohol Use and Nicotine Dependence Among Medical Students: A Single-Center, Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
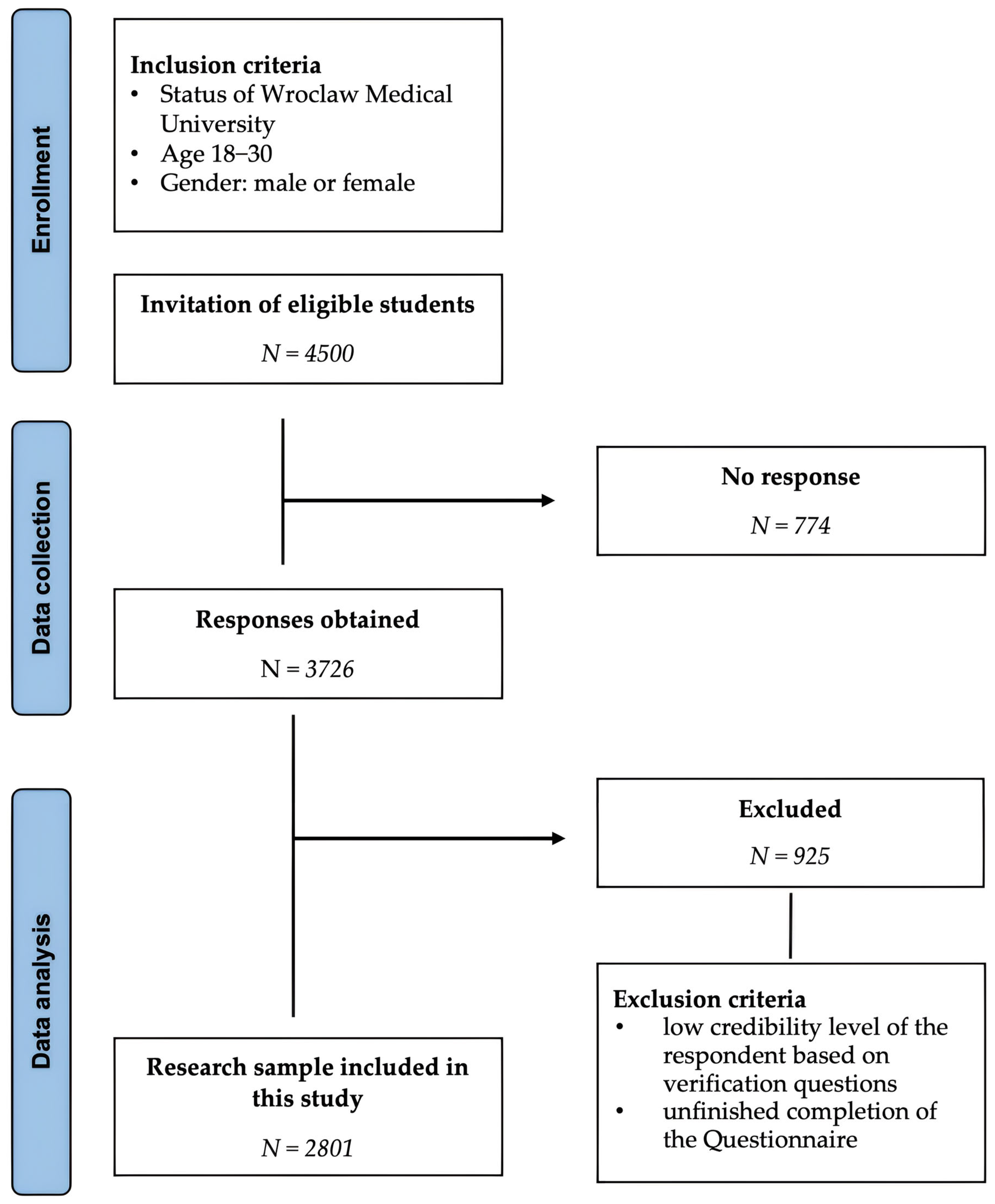
2.1. Study Design and Participants
2.2. KomPAN
2.3. The AUDIT
2.4. The Fagerström Test
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
3.2. Differences Between Drinking Alcohol and Smoking Status on Study Variables
3.3. Differences Between Study Variable Levels and AUDIT Domain Scores
3.4. Differences Between Study Variable Levels and Fagerstrom Test for Nicotine Dependence Total Scores
3.5. Cluster Analysis—AUDIT Total Score
3.6. Linear Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AUDIT | Alcohol Use Disorders Identification Test |
| BMI | Body Mass Index |
| DepSymp | Dependence Symptoms |
| DK | Dietary Knowledge |
| DQI | Diet Quality Index |
| FTND | Fagerström Test for Nicotine Dependence |
| HazAU | Hazardous Alcohol Use |
| IQR | Interquartile Ranges |
| NHD | non-Healthy Diet |
| PHD | pro-Healthy Diet |
| WHO | World Health Organization |
References
- Baqutayan, S.M.S. Stress and Coping Mechanisms: A Historical Overview. Mediterr. J. Soc. Sci. 2015, 6, 479. [Google Scholar] [CrossRef]
- Jin, S.Y.; Luo, X.Q.; Zhang, J.M. Current status of occupational stress among medical staff in Shenzhen, China and related influencing factors. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2019, 37, 596–601. [Google Scholar] [CrossRef]
- Oreskovich, M.R.; Shanafelt, T.; Dyrbye, L.N.; Tan, L.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Boone, S. The Prevalence of Substance Use Disorders in American Physicians. Am. J. Addict. 2015, 24, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Arora, A.; Kannan, S.; Gowri, S.; Choudhary, S.; Sudarasanan, S.; Khosla, P.P. Substance Abuse amongst the Medical Graduate Students in a Developing Country. Indian J. Med. Res. 2016, 143, 101–103. [Google Scholar] [CrossRef]
- Fares, J.; Al Tabosh, H.; Saadeddin, Z.; El Mouhayyar, C.; Aridi, H. Stress, Burnout and Coping Strategies in Preclinical Medical Students. N. Am. J. Med. Sci. 2016, 8, 75–81. [Google Scholar] [CrossRef]
- Jackson, E.R.; Shanafelt, T.D.; Hasan, O.; Satele, D.V.; Dyrbye, L.N. Burnout and Alcohol Abuse/Dependence Among U.S. Medical Students. Acad. Med. 2016, 91, 1251–1256. [Google Scholar] [CrossRef]
- Pazdro-Zastawny, K.; Dorobisz, K.; Bobak-Sarnowska, E.; Zatoński, T. Prevalence and Associated Factors of Cigarette Smoking Among Medical Students in Wroclaw, Poland. Risk Manag. Healthc. Policy 2022, 15, 509–519. [Google Scholar] [CrossRef]
- Janik-Koncewicz, K.; Zatoński, W.; Zatońska, K.; Stępnicka, Z.; Basiak-Rasała, A.; Zatoński, M.; Połtyn-Zaradna, K. Cigarette Smoking in Poland in 2019: The Continuing Decline in Smoking Prevalence. J. Health Inequal. 2020, 6, 87–94. [Google Scholar] [CrossRef]
- Newbury-Birch, D.; Walshaw, D.; Kamali, F. Drink and Drugs: From Medical Students to Doctors. Drug Alcohol Depend. 2001, 64, 265–270. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, J.; Jang, M. Factors Affecting Clinical Practicum Stress of Nursing Students: Using the Lazarus and Folkman’s Stress-Coping Model. J. Korean Acad. Nurs. 2019, 49, 437–448. [Google Scholar] [CrossRef]
- Nowakowska, I.; Lewczuk, K.; Gola, M. Changes in the Addiction Prevalence in Polish Population between 1990–2019: Review of Available Data. J. Addict. Sci. 2020, 6, 17–31. [Google Scholar] [CrossRef]
- Díaz, L.A.; Fuentes-López, E.; Idalsoaga, F.; Ayares, G.; Corsi, O.; Arnold, J.; Cannistra, M.; Vio, D.; Márquez-Lomas, A.; Ramirez-Cadiz, C.; et al. Association between Public Health Policies on Alcohol and Worldwide Cancer, Liver Disease and Cardiovascular Disease Outcomes. J. Hepatol. 2024, 80, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Sontate, K.V.; Rahim Kamaluddin, M.; Naina Mohamed, I.; Mohamed, R.M.P.; Shaikh, M.F.; Kamal, H.; Kumar, J. Alcohol, Aggression, and Violence: From Public Health to Neuroscience. Front. Psychol. 2021, 12, 699726. [Google Scholar] [CrossRef]
- Alvis, K.; Gunasena, P.; Hapuarachchi, T.; Ekanayake, U.; Rajapaksha, S.; Gunawardana, K.; Gunathilake, S. Unraveling the Complex Relationship Between Alcohol and Cancer Risk: Effects of Alcohol on Health. Res. Sq. 2024. [Google Scholar] [CrossRef]
- Dai, X.; Gil, G.; Reitsma, M.; Ahmad, N.; Anderson, J.; Bisignano, C.; Carr, S.; Feldman, R.; Hay, S.; He, J.; et al. Health Effects Associated with Smoking: A Burden of Proof Study. Nat. Med. 2022, 28, 2045–2055. [Google Scholar] [CrossRef]
- Hill, D.; Conner, M.; Clancy, F.; Moss, R.; Wilding, S.; Bristow, M.; O’Connor, D.B. Stress and Eating Behaviours in Healthy Adults: A Systematic Review and Meta-Analysis. Health Psychol. Rev. 2022, 16, 280–304. [Google Scholar] [CrossRef]
- Keaver, L.; Ruan, M.; Chen, F.; Du, M.; Ding, C.; Wang, J.; Shan, Z.; Liu, J.; Zhang, F.F. Plant- and Animal-Based Diet Quality and Mortality among US Adults: A Cohort Study. Br. J. Nutr. 2021, 125, 1405–1415. [Google Scholar] [CrossRef]
- Doak, S.; Kearney, J.M.; McCormack, J.M.; Keaver, L. The Relationship between Diet and Lifestyle Behaviours in a Sample of Higher Education Students; a Cross-Sectional Study. Clin. Nutr. ESPEN 2023, 54, 293–299. [Google Scholar] [CrossRef]
- Solomou, S.; Logue, J.; Reilly, S.; Perez-Algorta, G. A Systematic Review of the Association of Diet Quality with the Mental Health of University Students: Implications in Health Education Practice. Health Educ. Res. 2023, 38, 28–68. [Google Scholar] [CrossRef]
- Ramón-Arbués, E.; Granada-López, J.-M.; Martínez-Abadía, B.; Echániz-Serrano, E.; Antón-Solanas, I.; Jerue, B.A. Factors Related to Diet Quality: A Cross-Sectional Study of 1055 University Students. Nutrients 2021, 13, 3512. [Google Scholar] [CrossRef] [PubMed]
- Spronk, I.; Kullen, C.; Burdon, C.; O’Connor, H. Relationship between Nutrition Knowledge and Dietary Intake. Br. J. Nutr. 2014, 111, 1713–1726. [Google Scholar] [CrossRef] [PubMed]
- Belogianni, K.; Ooms, A.; Lykou, A.; Moir, H.J. Nutrition Knowledge among University Students in the UK: A Cross-Sectional Study. Public Health Nutr. 2021, 25, 2834–2841. [Google Scholar] [CrossRef] [PubMed]
- Leman, M.A.; Claramita, M.; Rahayu, G.R. Defining a “Healthy Role-Model” for Medical Schools: Learning Components That Count. J. Multidiscip. Healthc. 2020, 13, 1325–1335. [Google Scholar] [CrossRef]
- Ndung’u, J.; Kobia, J.; Waudo, J. Balancing Act: Exploring the Interplay Between Lifestyle Habits and Nutritional Status Among University Students. A Cross-Sectional Study. Res. Sq. 2024. [Google Scholar] [CrossRef]
- Jezewska-Zychowicz, M.; Gawecki, J.; Wadolowska, L.; Czarnocinska, J.; Galinski, G.; Kollajtis Dolowy, A.; Roszkowski, W.; Wawrzyniak, A.; Przybylowicz, K.; Stasiewicz, B.; et al. KomPAN® Dietary Habits and Nutrition Beliefs Questionnaire for People 15–65 Years Old, Version 1.1.—Interviewer Administered Questionnaire. In KomPAN® Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data; Committee of Human Nutrition, Polish Academy of Sciences: Warsaw, Poland, 2020; pp. 4–21. [Google Scholar]
- Kowalkowska, J.; Wadolowska, L.; Czarnocinska, J.; Czlapka-Matyasik, M.; Galinski, G.; Jezewska-Zychowicz, M.; Bronkowska, M.; Dlugosz, A.; Loboda, D.; Wyka, J. Reproducibility of a Questionnaire for Dietary Habits, Lifestyle and Nutrition Knowledge Assessment (KomPAN) in Polish Adolescents and Adults. Nutrients 2018, 10, 1845. [Google Scholar] [CrossRef]
- Kosendiak, A.A.; Adamczak, B.; Kontek, S.; Kuźnik, Z.; Roman, M.; Gostkowski, M.; Niedziółka, A. Level of Physical Activity, Sleep Quality and Use of Personal Protective Equipment of Students at Wroclaw Medical University during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 2406. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De La Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Daeppen, J.B.; Yersin, B.; Landry, U.; Pécoud, A.; Decrey, H. Reliability and Validity of the Alcohol Use Disorders Identification Test (AUDIT) Imbedded within a General Health Risk Screening Questionnaire: Results of a Survey in 332 Primary Care Patients. Alcohol Clin. Exp. Res. 2000, 24, 659–665. [Google Scholar] [CrossRef]
- Fagerström, K.O. Measuring Degree of Physical Dependence to Tobacco Smoking with Reference to Individualization of Treatment. Addict. Behav. 1978, 3, 235–241. [Google Scholar] [CrossRef]
- Fagerstrom, K.O.; Schneider, N.G. Measuring Nicotine Dependence: A Review of the Fagerstrom Tolerance Questionnaire. J. Behav. Med. 1989, 12, 159–182. [Google Scholar] [CrossRef]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerström, K.O. The Fagerström Test for Nicotine Dependence: A Revision of the Fagerström Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Pomerleau, C.S.; Carton, S.M.; Lutzke, M.L.; Flessland, K.A.; Pomerleau, O.F. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addict. Behav. 1994, 19, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.H.; The, C.H.; Lim, H.L.; Khoo, Y.Y.; Lau, K.J.; Yy, C.; Mohd Ghazalig, S.; Kee CC, C.C.; Lim, K.K.; Ibrahim, N.; et al. Reliability and Validity of the Fagerstrom Test for Cigarettes Dependence among Malaysian Adolescents. Iran. J. Public Health 2016, 45, 104–105. [Google Scholar]
- Moberly, T. Number of Women Entering Medical School Rises after Decade of Decline. BMJ 2018, 360, k254. [Google Scholar] [CrossRef]
- Alcohol Consumption Statistics. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Alcohol_consumption_statistics (accessed on 19 May 2025).
- Mandziuk, M.; Wasilewska, M.; Lukács, A. Alcohol consumption among students in the Lublin region of Poland. Health Probl. Civiliz. 2020, 14, 18–23. [Google Scholar] [CrossRef]
- Bryl, N.; Czarnecka-Iwańczuk, M.; Romanowska, M.; Stanisić, M.G.; Michalak, M.; Posadzy-Małaczyńska, A. Drinking Alcohol as a Way of Coping with Stress in Students of Medical Faculties. Psychiatr. Pol. 2020, 54, 265–277. [Google Scholar] [CrossRef]
- Tobacco Consumption Statistics. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Tobacco_consumption_statistics (accessed on 19 May 2025).
- Rodakowska, E.; Mazur, M.; Baginska, J.; Sierpinska, T.; La Torre, G.; Ottolenghi, L.; D’Egidio, V.; Guerra, F. Smoking Prevalence, Attitudes and Behavior among Dental Students in Poland and Italy. Int. J. Environ. Res. Public Health 2020, 17, 7451. [Google Scholar] [CrossRef]
- Fiore, M.; Ledda, C.; Rapisarda, V.; Sentina, E.; Mauceri, C.; D’Agati, P.; Oliveri Conti, G.; Serra-Majem, L.; Ferrante, M. Medical School Fails to Improve Mediterranean Diet Adherence among Medical Students. Eur. J. Public Health 2015, 25, 1019–1023. [Google Scholar] [CrossRef]
- Jassem, J.; Przewoźniak, K.; Zatoński, W. Tobacco Control in Poland—Successes and Challenges. Transl. Lung Cancer Res. 2014, 3, 280–285. [Google Scholar] [CrossRef]
- Grudziąż-Sękowska, J.; Sękowski, K.B.; Grześczyk-Nojszewska, Z.; Sierpiński, R.; Ostrowski, J.; Pinkas, J.; Jankowski, M. Public Support for New Tobacco Control Measures in Poland: A Cross-Sectional Survey 2024. Tobbaco Prev. Cessat. 2024, 10, 66. [Google Scholar] [CrossRef]
- Alkerwi, A.; Baydarlioglu, B.; Sauvageot, N.; Stranges, S.; Lemmens, P.; Shivappa, N.; Hébert, J.R. Smoking Status Is Inversely Associated with Overall Diet Quality: Findings from the ORISCAV-LUX Study. Clin. Nutr. 2017, 36, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Alfheeaid, H.A.; Alasqah, I.; Alqarawi, N.; Alotaibi, S.A.; Alribdi, F.F.; Almutairi, S.; Lima, M.J.; Teixeira-Lemos, E.; Raposo, A. Dietary Patterns among Smokers and Non-Smokers: Findings from the National Health and Nutritional Examination Survey (NHANES) 2017–2018. Nutrients 2024, 16, 2035. [Google Scholar] [CrossRef] [PubMed]
- Alruwaili, A.; King, J.A.; Deighton, K.; Kelly, B.M.; Liao, Z.; Innes, A.; Henson, J.; Yates, T.; Johnson, W.; Thivel, D.; et al. The Association of Smoking with Different Eating and Dietary Behaviours: A Cross-Sectional Analysis of 80 296 United Kingdom Adults. Addiction 2024, 119, 1737–1750. [Google Scholar] [CrossRef]
- Tackling NCDs: “Best Buys” and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases; World Health Organization: Geneva, Switzerland, 2017.
- Radišauskas, R.; Štelemėkas, M.; Petkevičienė, J.; Trišauskė, J.; Telksnys, T.; Miščikienė, L.; Gobina, I.; Stoppel, R.; Reile, R.; Janik-Koncewicz, K.; et al. Alcohol-Attributable Mortality and Alcohol Control Policy in the Baltic Countries and Poland in 2001–2020: An Interrupted Time-Series Analysis. Subst. Abuse Treat. Prev. Policy 2023, 18, 65. [Google Scholar] [CrossRef]
- Zatońska, K.; Psikus, P.; Basiak-Rasała, A.; Stępnicka, Z.; Wołyniec, M.; Wojtyła, A.; Szuba, A.; Połtyn-Zaradna, K. Patterns of Alcohol Consumption in the PURE Poland Cohort Study and Their Relationship with Health Problems. Int. J. Environ. Res. Public Health 2021, 18, 4185. [Google Scholar] [CrossRef]
- Caliendo, M.; Hennecke, J. Drinking Is Different! Examining the Role of Locus of Control for Alcohol Consumption. Empir. Econ. 2022, 63, 2785–2815. [Google Scholar] [CrossRef]
- Cobb-Clark, D.A.; Schurer, S. Two Economists’ Musings on the Stability of Locus of Control. Econ. J. 2013, 123, 358–400. [Google Scholar] [CrossRef]
- Cobb-Clark, D.A.; Kassenboehmer, S.C.; Schurer, S. Healthy Habits: The Connection between Diet, Exercise, and Locus of Control. J. Econ. Behav. Organ. 2014, 98, 1–28. [Google Scholar] [CrossRef]
- Navder, K.; Lieber, C. Nutrition and Alcoholism. In Nutritional Aspects and Clinical Management of Chronic Disorders and Diseases; CRC Press: Boca Raton, FL, USA, 2009; pp. 307–320. ISBN 978-0-8493-0945-8. [Google Scholar]
- Diet Quality Worsens as Alcohol Intake Increases. Available online: https://www.nih.gov/news-events/news-releases/diet-quality-worsens-alcohol-intake-increases (accessed on 19 May 2025).
- Lieber, C.S. Relationships between Nutrition, Alcohol Use, and Liver Disease. Alcohol Res. Health 2003, 27, 220–231. [Google Scholar]
- Joseph, P.V.; Zhou, Y.; Brooks, B.; McDuffie, C.; Agarwal, K.; Chao, A.M. Relationships among Alcohol Drinking Patterns, Macronutrient Composition, and Caloric Intake: National Health and Nutrition Examination Survey 2017–2018. Alcohol Alcohol. 2022, 57, 559–565. [Google Scholar] [CrossRef]
- Olson, J.S.; Hummer, R.A.; Harris, K.M. Gender and Health Behavior Clustering among U.S. Young Adults. Biodemogr. Soc. Biol. 2017, 63, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Monaci, M. Peer Pressure and Alcohol Consumption among University Students: The Moderating Effect of Emotional Intelligence. BPA Appl. Psychol. Bull. 2013, 60, 17. [Google Scholar]
- Chen, J.; Li, Y.; Zhang, Y.; Feng, J.; Jia, L. Descriptive Peer Drinking Norms and Binge Drinking: Enhancement Motives as a Mediator and Alcohol Resistance Self-Efficacy as a Moderator. Front. Psychol. 2022, 13, 876274. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, J.; Hublet, A.; De Clercq, B.; Kuntsche, E.; Maes, L.; Clays, E. Who Does Not Cut down? Comparing Characteristics and Drinking Motives of Drinkers and Abstainers during the Exam Periods. J. Am. Coll. Health 2017, 65, 558–566. [Google Scholar] [CrossRef]
- Alkazemi, D. Gender Differences in Weight Status, Dietary Habits, and Health Attitudes among College Students in Kuwait: A Cross-Sectional Study. Nutr. Health 2019, 25, 75–84. [Google Scholar] [CrossRef]
- White, A.M. Gender Differences in the Epidemiology of Alcohol Use and Related Harms in the United States. Alcohol Res. 2020, 40, 1. [Google Scholar] [CrossRef]
- Dieleman, L.A.; van Peet, P.G.; Vos, H.M.M. Gender Differences within the Barriers to Smoking Cessation and the Preferences for Interventions in Primary Care a Qualitative Study Using Focus Groups in The Hague, The Netherlands. BMJ Open 2021, 11, e042623. [Google Scholar] [CrossRef]
| Variables | Total N = 2801 [IQR] (%) |
|---|---|
| Age mean | 19.8 [19.0–20.0] |
| Gender | |
| Male | 643 (23.0) |
| Female | 2158 (77.0) |
| Place of Residence | |
| Rural area | 690 (24.6) |
| City < 20,000 * | 296 (10.6) |
| City 20,000–100,000 * | 593 (21.2) |
| City 100,000+ * | 1222 (43.6) |
| BMI | |
| Underweight | 113 (4.0) |
| Normal weight | 2352 (84.0) |
| Overweight and Obese | 336 (12.0) |
| Drinking Status | |
| Drinker | 2374 (84.8) |
| Non-drinker | 427 (15.2) |
| Smoking Status | |
| Smoker | 379 (13.5) |
| Non-smoker | 2422 (86.5) |
| Pro-Healthy Diet | |
| Low | 2299 (82.1) |
| Medium | 492 (17.6) |
| High | 10 (0.4) |
| Non-Healthy Diet | |
| Low | 2721 (97.1) |
| Medium | 75 (2.7) |
| High | 5 (0.2) |
| Diet Quality Index | |
| Low | 5 (0.2) |
| Medium | 2454 (87.6) |
| High | 342 (12.2) |
| Dietary Knowledge | |
| Insufficient | 380 (13.6) |
| Sufficient | 1631 (58.2) |
| Good | 790 (28.2) |
| Mean | Median | IQR | Mean | Median | IQR | p-Value | Z | |
|---|---|---|---|---|---|---|---|---|
| Drinkers, N = 2374 | Non-Drinkers, N = 427 | D vs. N-D | ||||||
| Pro-Healthy Diet | 22.95 | 21.7 | 14.7–29.5 | 23.76 | 21.8 | 14.1–31 | 0.65 | 0.45 |
| Non-Healthy Diet | 13.81 | 12.2 | 8.3–17.2 | 13.34 | 11.9 | 7.5–17.5 | 0.24 | 1.18 |
| Diet Quality Index | 9.15 | 7.6 | 0.2–17.0 | 10.41 | 7.9 | −0.1–19.9 | 0.27 | 1.10 |
| Dietary Knowledge | 13.73 | 14.0 | 11.0–17.0 | 12.41 | 14.0 | 9.0–17.0 | 0.002 | 3.18 |
| Smokers, N = 379 | Non-Smokers, N = 2422 | S vs. N-S | ||||||
| Pro-Healthy Diet | 21.94 | 19.6 | 12.9–28.1 | 23.25 | 22.0 | 14.8–30.0 | 0.002 | 3.08 |
| Non-Healthy Diet | 15.55 | 13.3 | 9.0–19.8 | 13.45 | 12.0 | 8.1–16.9 | 0.0009 | 3.33 |
| Diet Quality Index | 6.39 | 5.0 | −1.7–13.5 | 9.80 | 8.2 | 0.3–18.2 | <0.0001 | 4.99 |
| Dietary Knowledge | 12.72 | 13.0 | 10.0–16.0 | 13.65 | 14.0 | 11.0–17.0 | 0.0004 | 3.52 |
| Mean | Median | IQR | Mean | Median | IQR | Mean | Median | IQR | p-Value | Z/H* | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pro-Healthy Diet | |||||||||||
| Low, N = 1967 | Medium, N = 399 | High, N = 8 | L vs. M | ||||||||
| HazAU | 3.73 | 4.0 | 2.0–5.0 | 3.55 | 3.0 | 2.0–5.0 | 5.75 | 4.5 | 3.5–8.0 | 0.22 | 1.22 |
| DepSymp | 1.19 | 0.0 | 0.0–2.0 | 1.00 | 0.0 | 0.0–1.0 | 3.75 | 2.5 | 0.5–6.0 | 0.04 | 2.10 |
| HarmAU | 1.45 | 0.0 | 0.0–2.0 | 1.22 | 0.0 | 0.0–2.0 | 3.63 | 2.5 | 0.0–6.0 | 0.01 | 2.54 |
| AUDIT Total | 6.36 | 5.0 | 2.0–9.0 | 5.77 | 4.0 | 2.0–7.0 | 13.13 | 9.0 | 6.5–18.0 | 0.02 | 2.27 |
| Non-Healthy Diet | |||||||||||
| Low, N = 2303 | Medium, N = 67 | High, N = 4 | L vs. M | ||||||||
| HazAU | 3.66 | 3.0 | 2.0–5.0 | 4.93 | 4.0 | 3.0–6.0 | 7.75 | 8.0 | 5.5–10.0 | 0.0001 | 3.88 |
| DepSymp | 1.12 | 0.0 | 0.0–1.0 | 2.25 | 1.0 | 0.0–4.0 | 6.00 | 6.0 | 1.5–10.5 | 0.0001 | 3.88 |
| HarmAU | 1.37 | 0.0 | 0.0–2.0 | 2.64 | 1.0 | 0.0–4.0 | 6.00 | 6.0 | 2.0–10.0 | 0.0008 | 3.36 |
| AUDIT Total | 6.16 | 5.0 | 2.0–8.0 | 9.82 | 8.0 | 4.0–15.0 | 19.75 | 17.5 | 9.0–30.5 | <0.0001 | 4.10 |
| Diet Quality Index | |||||||||||
| Low, N = 5 | Medium, N = 2097 | High, N = 272 | M vs. H | ||||||||
| HazAU | 3.20 | 3.0 | 3.0–4.0 | 3.74 | 4.0 | 2.0–5.0 | 3.41 | 3.0 | 2.0–4.0 | 0.03 | 2.24 |
| DepSymp | 1.20 | 0.0 | 0.0–2.0 | 1.22 | 0.0 | 0.0–2.0 | 0.70 | 0.0 | 0.0–1.0 | <0.0001 | 4.45 |
| HarmAU | 2.60 | 4.0 | 0.0–4.0 | 1.47 | 0.0 | 0.0–2.0 | 0.99 | 0.0 | 0.0–1.0 | 0.001 | 3.19 |
| AUDIT Total | 7.00 | 9.0 | 3.0–10.0 | 6.44 | 5.0 | 2.0–9.0 | 5.10 | 4.0 | 2.0–6.5 | 0.0006 | 3.45 |
| Dietary Knowledge | |||||||||||
| Insufficient, N = 281 | Sufficient, N = 1421 | Good, N = 672 | In vs. S vs. G | ||||||||
| HazAU | 4.14 | 4.0 | 2.0–6.0 | 3.70 | 3.0 | 2.0–5.0 | 3.54 | 3.0 | 2.0–5.0 | 0.008 | 9.75 |
| DepSymp | 2.24 | 1.0 | 0.0–4.0 | 1.09 | 0.0 | 0.0–1.0 | 0.87 | 0.0 | 0.0–1.0 | <0.0001 | 65.46 |
| HarmAU | 2.49 | 1.0 | 0.0–5.0 | 1.33 | 0.0 | 0.0–2.0 | 1.15 | 0.0 | 0.0–2.0 | <0.0001 | 41.48 |
| AUDIT Total | 8.87 | 7.0 | 3.0–14.0 | 6.12 | 5.0 | 2.0–8.0 | 5.55 | 4.0 | 2.0–7.0 | <0.0001 | 36.91 |
| Mean | Median | IQR | Mean | Median | IQR | Mean | Median | IQR | p-Value | Z | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pro-Healthy Diet | |||||||||||
| Low, N = 324 | Medium, N = 52 | High, N = 3 | L vs. M | ||||||||
| FTND Score | 2.67 | 2.0 | 0.0–4.5 | 3.00 | 3.5 | 0.0–5.0 | 7.33 | 8.0 | 6.0–8.0 | 0.14 | 1.49 |
| Non-Healthy Diet | |||||||||||
| Low, N = 356 | Medium, N = 20 | High, N = 3 | L vs. M | ||||||||
| FTND Score | 2.68 | 2.0 | 0.0–5.0 | 3.35 | 4.0 | 1.0–6.0 | 7.33 | 8.0 | 6.0–8.0 | <0.0001 | 4.02 |
| Diet Quality Index | |||||||||||
| Low, N = 1 | Medium, N = 342 | High, N = 36 | M vs. H | ||||||||
| FTND Score | 2.00 | 2.0 | 2.0–2.0 | 2.75 | 2.0 | 0.0–5.0 | 2.81 | 3.0 | 0.0–5.0 | 0.11 | 1.59 |
| Dietary Knowledge | |||||||||||
| Insufficient, N = 67 | Sufficient, N = 229 | Good, N = 83 | In vs. S vs. G | ||||||||
| FTND Score | 3.42 | 4.0 | 1.0–5.0 | 2.69 | 2.0 | 0.0–5.0 | 2.39 | 2.0 | 0.0–4.0 | 0.002 | 3.15 |
| Cluster Number | Diet Quality Index | Dietary Knowledge | AUDIT Total | N (%) |
|---|---|---|---|---|
| 1 | 8.46 | 8.33 | 4.05 | 492 (20.7) |
| 2 | 22.75 | 18.35 | 4.14 | 582 (24.5) |
| 3 | 2.78 | 14.74 | 4.25 | 852 (35.9) |
| 4 | 6.02 | 14.91 | 14.67 | 302 (12.7) |
| 5 | 0.87 | 5.10 | 16.90 | 146 (6.2) |
| Cluster Number | B Coefficient ± SE | β Coefficient ± SE | p-Value |
|---|---|---|---|
| AUDIT Total Score | |||
| Intercept | 6.513 ± 0.402 | - | <0.0001 |
| Pro-Healthy Diet | −0.008 ± 0.010 | −0.017 ± 0.021 | 0.41 |
| Non-Healthy Diet | 0.146 ± 0.013 | 0.223 ± 0.020 | <0.0001 |
| Diet Quality Index | 0.0 | - | - |
| Dietary Knowledge | −0.150 ± 0.023 | −0.14 ± 0.021 | <0.0001 |
| FTND Score | |||
| Intercept | 0.382 ± 0.088 | - | <0.0001 |
| Pro-Healthy Diet | 0.0003 ± 0.002 | 0.105 ± 0.020 | 0.88 |
| Non-Healthy Diet | 0.016 ± 0.003 | 0.003 ± 0.020 | <0.0001 |
| Diet Quality Index | 0.0 | - | - |
| Dietary Knowledge | −0.018 ± 0.005 | −0.069 ± 0.020 | 0.0004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosendiak, A.A.; Adamczak, B.B.; Kuźnik, Z.; Makles, S.; Hariasz, W. The Impact of Dietary Habits and Nutrition Knowledge on Harmful Alcohol Use and Nicotine Dependence Among Medical Students: A Single-Center, Cross-Sectional Study. Nutrients 2025, 17, 1788. https://doi.org/10.3390/nu17111788
Kosendiak AA, Adamczak BB, Kuźnik Z, Makles S, Hariasz W. The Impact of Dietary Habits and Nutrition Knowledge on Harmful Alcohol Use and Nicotine Dependence Among Medical Students: A Single-Center, Cross-Sectional Study. Nutrients. 2025; 17(11):1788. https://doi.org/10.3390/nu17111788
Chicago/Turabian StyleKosendiak, Aureliusz Andrzej, Bartosz Bogusz Adamczak, Zofia Kuźnik, Szymon Makles, and Weronika Hariasz. 2025. "The Impact of Dietary Habits and Nutrition Knowledge on Harmful Alcohol Use and Nicotine Dependence Among Medical Students: A Single-Center, Cross-Sectional Study" Nutrients 17, no. 11: 1788. https://doi.org/10.3390/nu17111788
APA StyleKosendiak, A. A., Adamczak, B. B., Kuźnik, Z., Makles, S., & Hariasz, W. (2025). The Impact of Dietary Habits and Nutrition Knowledge on Harmful Alcohol Use and Nicotine Dependence Among Medical Students: A Single-Center, Cross-Sectional Study. Nutrients, 17(11), 1788. https://doi.org/10.3390/nu17111788







