Effects of Nutritional Education and Diet on Obesity and Asthma Progression in Children and Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics Issue
2.2. Minimum Sample Size Calculation
2.3. Study Population
2.4. Data Collection Timeline
| Stage | Time Point | Participants | Activity/Assessment | Purpose |
|---|---|---|---|---|
| 1 | Baseline (Visit 1) | All groups (AO, O, C) | Anthropometrics, fasting labs, food diary, YHEI, KIDMED 2.0, VAS | Initial health and dietary status assessment |
| 2 | Week 0 | AO and O | Individualized nutrition consultation (1) | Interview, goal setting, and motivation |
| 3 | Every 6–8 weeks (10 sessions total) | AO and O | Structured educational sessions (see Table 2 in manuscript) + follow-up, adaptation of recommendations | Gradual implementation of Mediterranean and anti-inflammatory dietary patterns |
| 4 | Throughout 12 months | AO and O | Motivational support, food diary analysis, and behavior reinforcement | Improve adherence, self-efficacy, and parental support |
| 5 | Month 12 (Final Visit) | All groups (AO, O, C) | Re-assessment: anthropometrics, labs, food diary, YHEI, KIDMED, VAS | Evaluation of intervention effectiveness |
| Consultation Number | Main Aim |
|---|---|
| 1 consultation | Interview, introduction, setting individual nutrition and health goals. Motivation. |
| 2 consultation | The basics of healthy eating are a plate of healthy food. Portion control, food awareness. |
| 3 consultation | Anti-inflammatory diet—what to eat, what to avoid. Products with anti-inflammatory effects reduce inflammation. Glycemic index and glycemic load. |
| 4 consultation | Role of fiber, fats, protein, and carbohydrates. |
| 5–6 consultation | Meal planning, shopping, and reading food labels. The role of snacks, sugar, and sweeteners. |
| 7–8 consultation | Practical tips for parents. The role of hydration, physical activity, and sleep. |
| 9–10 consultation | Summary and consolidation of habits. |
2.5. Outcome Measures
2.6. Intervention Description
2.7. Statistical Analysis
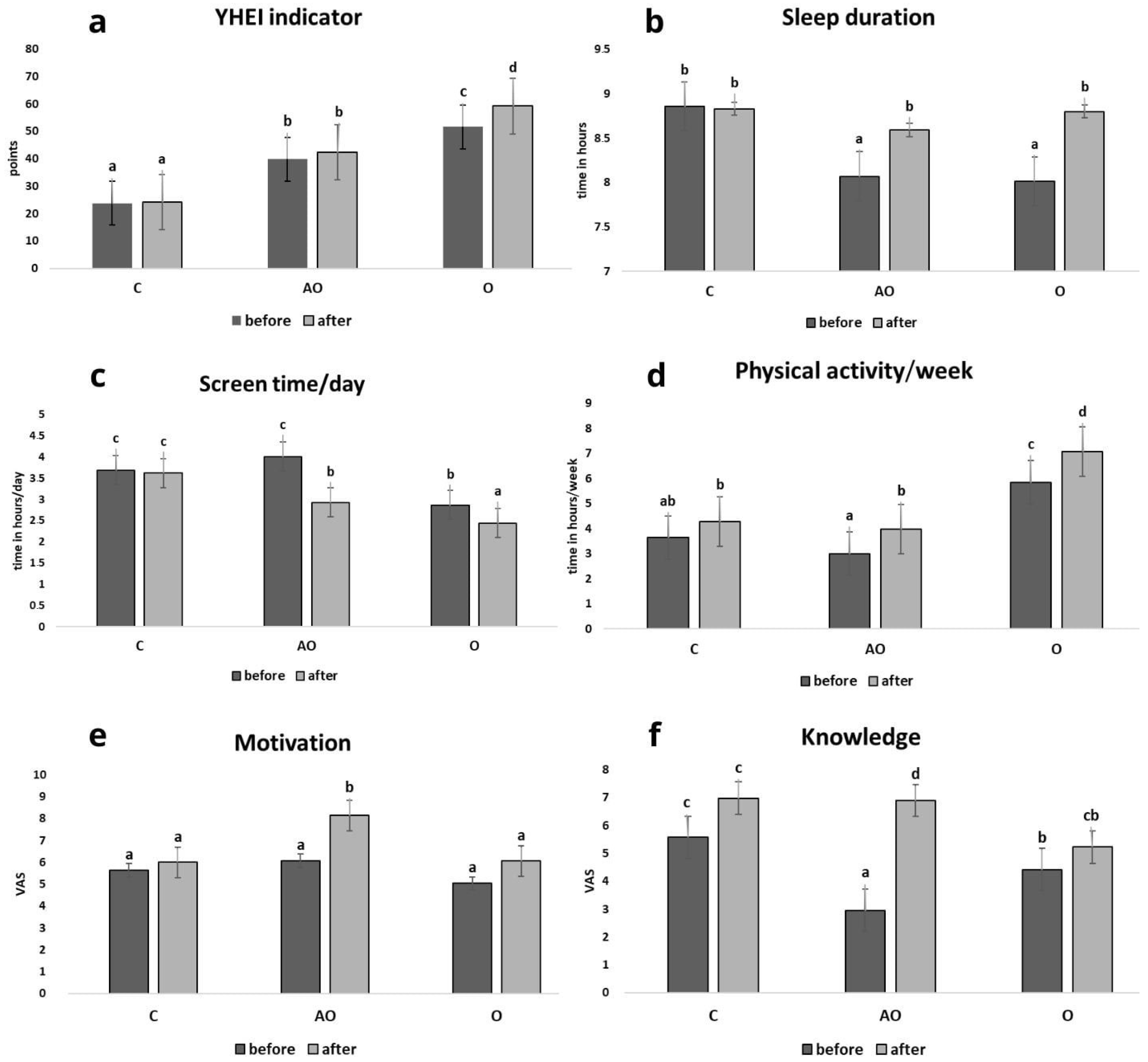
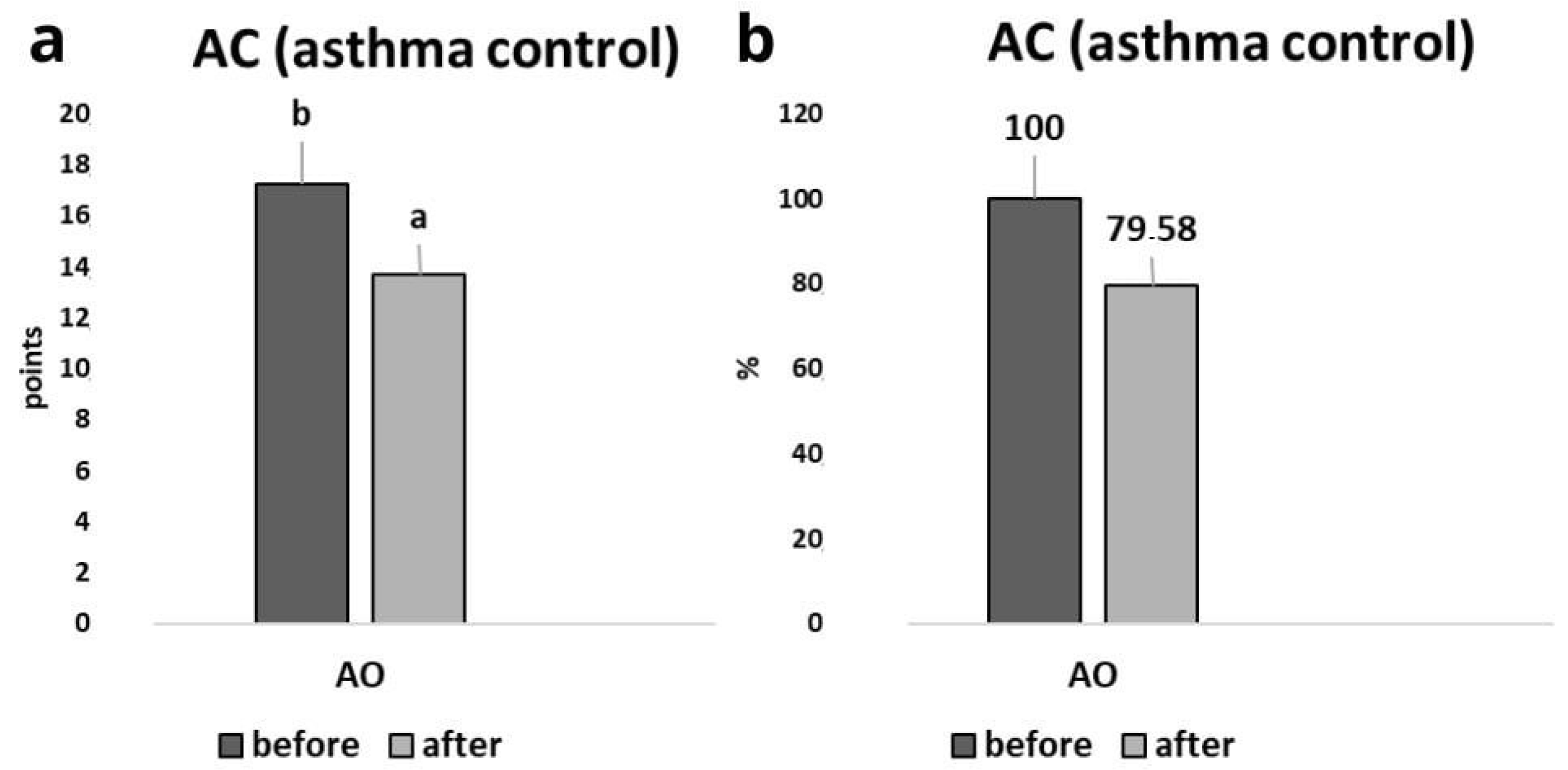
3. Results
4. Discussion
5. Conclusions
6. Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MD | Mediterranean diet |
| BMI | Body Mass Index |
| O | Obesity |
| C | Control |
| AO | Asthma and Obesity |
| AC | Asthma Control |
| YHEI | Young Healthy Eating Index |
| KIDMED | Nutrition Education’s Impact on the Mediterranean Diet Quality Index |
| VAS | Visual analogue scale |
| TC | Total cholesterol |
| HDL | High-density lipoprotein |
| LDL | Low-density lipoprotein |
| TG | Triglyceride |
| HOMA-IR | Homeostasis Model Assessment of Insulin Resistance |
| HbA1c | Glycated hemoglobin |
| NADS | The average number of days of asthma symptoms per month |
| CRP | C-Reactive Protein |
Appendix A
- How often during the last month did asthma symptoms occur?
- How often did asthma symptoms cause nighttime awakenings during the last month?
- How often did asthma limit your ability to engage in physical activity (e.g., play, sports, PE)?
- How often was it necessary to use a rescue inhaler?
- How would you rate your well-being in the last month?
- How would you rate your overall health and quality of life?
References
- Sikorska-Szaflik, H.; Połomska, J.; Sozańska, B. The impact of dietary intervention in obese children on asthma prevention and control. Nutrients 2022, 14, 4322. [Google Scholar] [CrossRef] [PubMed]
- Alwarith, J.; Kahleova, H.; Crosby, L.; Brooks, A.; Brandon, L.; Levin, S.M.; Barnard, N.D. The role of nutrition in asthma prevention and treatment. Nutr. Rev. 2020, 78, 928–938. [Google Scholar] [CrossRef] [PubMed]
- Soczewka, M.; Waśniowska, J.; Krawczyk, K.; Kędzia, A.; Skowrońska, B.; Niechciał, E. Assessment of parents’ awareness of the anti-inflammatory diet and its impact on their child’s health: Survey study. Pediatr. Endocrinol. Diabetes Metab. 2024, 30, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Soczewka, M.; Kędzia, A.; Skowrońska, B.; Niechciał, E. Importance of diet in children and adolescents with obesity and asthma. Pediatr. Endocrinol. Diabetes Metab. 2024, 30, 91–96. [Google Scholar] [CrossRef]
- Velázquez-López, L.; Santiago-Díaz, G.; Nava-Hernández, J.; Muñoz-Torres, A.V.; Medina-Bravo, P.; Torres-Tamayo, M. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatr. 2014, 14, 175. [Google Scholar] [CrossRef]
- Barragán-Vázquez, S.; Ariza, A.C.; Ramírez Silva, I.; Pedraza, L.S.; Rivera Dommarco, J.A.; Ortiz-Panozo, E.; Zambrano, E.; Castro, L.A.R.; Shivappa, N.; Hébert, J.R.; et al. A pro-inflammatory diet is associated with adiposity during childhood and with adipokines and inflammatory markers at 11 years in Mexican children. Nutrients 2020, 12, 3658. [Google Scholar] [CrossRef]
- Manuel, S.-S.; Luis, G.-M. Nutrition, obesity, and asthma inception in children. The role of lung function. Nutrients 2021, 13, 3837. [Google Scholar] [CrossRef]
- Sunnetci Silistre, E.; Yesil, A.; Kozanoglu, T.; Balci, M.C.; Karaca, M.; Gokcay, G.F. Challenging childhood obesity: The influence of education and close monitoring on obesity-related behaviors. Healthcare 2024, 12, 2048. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Sawicka-Gutaj, N.; Gruszczyński, D.; Guzik, P.; Mostowska, A.; Walkowiak, J. Publication Ethics of Human Studies in the Light of the Declaration of Helsinki-A Mini-Review. J. Med. Sci. 2022, 91, e700. [Google Scholar] [CrossRef]
- Wadolowska, L. Validation of food frequency questionnaire (FFQ): Reproducibility assessment. Bromat. Chem. Toksykol. 2005, 38, 27–33. [Google Scholar]
- Kułaga, Z.; Różdżyńska, A.; Palczewska, I.; Grajda, A.; Gurzkowska, B.; Napieralska, E.; Litwin, M.; Grupa Badaczy OLAF. Siatki centylowe wysokości, masy ciała i wskaźnika masy ciała dzieci i młodzieży w Polsce—Wyniki badania OLAF. Stand. Med. 2010, 7, 690–700. [Google Scholar]
- Artur, M.; Agnieszka, Z.; Joanna, B.; Katarzyna, D.; Edyta, Ł.; Aneta, W.; Justyna, W.; Justyna, D.; Ewa, S.; Dorota, D.; et al. Otyłość dziecięca: Stanowisko Polskiego Towarzystwa Pediatrycznego, Polskiego Towarzystwa Otyłości Dziecięcej, Polskiego Towarzystwa Endokrynologii i Diabetologii Dziecięcej, Kolegium Lekarzy Rodzinnych w Polsce oraz Polskiego Towarzystwa Badań nad Otyłością. Med. Prakt.-Pediatr. 2023, 1, 1–43. [Google Scholar]
- Feskanich, D.; Rockett, H.R.H.; Colditz, G.A. Modifying the healthy eating index to assess diet quality in children and adolescents. J. Am. Diet. Assoc. 2004, 104, 1375–1383. [Google Scholar] [CrossRef]
- López-Gajardo, M.A.; Leo, F.M.; Sánchez-Miguel, P.A.; López-Gajardo, D.; Soulas, C.; Tapia-Serrano, M.A. KIDMED 2.0, An update of the KIDMED questionnaire: Evaluation of the psychometric properties in youth. Front. Nutr. 2022, 9, 945721. [Google Scholar] [CrossRef]
- Tang, Q.; Li, X.; Song, P.; Xu, L. Optimal cut-off values for the homeostasis model assessment of insulin resistance (HOMA-IR) and pre-diabetes screening: Developments in research and prospects for the future. Drug Discov. Ther. 2015, 9, 380–385. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Verde, L.; Sulu, C.; Katsiki, N.; Hassapidou, M.; Frias-Toral, E.; Cucalón, G.; Pazderska, A.; Yumuk, V.D.; Colao, A.; et al. Mediterranean Diet and Obesity-related Disorders: What is the Evidence? Curr. Obes. Rep. 2022, 11, 287–304. [Google Scholar] [CrossRef]
- Chiva-Blanch, G.; Badimon, L.; Estruch, R. Latest evidence of the effects of the Mediterranean diet in prevention of cardiovascular disease. Curr. Atheroscler. Rep. 2014, 16, 446. [Google Scholar] [CrossRef]
- Esposito, K.; Maiorino, M.I.; Bellastella, G.; Chiodini, P.; Panagiotakos, D.; Giugliano, D. A journey into a Mediterranean diet and type 2 diabetes: A systematic review with meta-analyses. BMJ Open 2015, 5, e008222. [Google Scholar] [CrossRef]
- Dehghan, P.; Nejati, M.; Vahid, F.; Almasi-Hashiani, A.; Saleh-Ghadimi, S.; Parsi, R.; Jafari-Vayghan, H.; Shivappa, N.; Hébert, J.R. The association between dietary inflammatory index, dietary antioxidant index, and mental health in adolescent girls: An analytical study. BMC Public Health 2022, 22, 1513. [Google Scholar] [CrossRef]
- Costa-Urrutia, P.; Colistro, V.; Franco-Trecu, V.; Granados, J.; Álvarez Fariña, R.; Rodríguez-Arellano, M.E. Dyslipidemia, obesity, and ethnicity in Mexican children. Int. J. Environ. Res. Public Health 2021, 18, 12659. [Google Scholar] [CrossRef]
- Gobato, A.O.; Vasques, A.C.J.; Zambon, M.P.; Barros Filho Ade, A.; Hessel, G. Metabolic syndrome and insulin resistance in obese adolescents. Rev. Paul. Pediatr. 2014, 32, 55–59. [Google Scholar] [CrossRef]
- Guglani, L.; Joseph, C.L. Asthma and diet: Could food be thy medicine? Indian Pediatr. 2015, 52, 21–22. [Google Scholar]
- Lv, N.; Xiao, L.; Ma, J. Dietary pattern and asthma: A systematic review and meta-analysis. J. Asthma Allergy 2014, 7, 105–121. [Google Scholar]
- Garcia-Marcos, L.; Castro-Rodriguez, J.A.; Weinmayr, G.; Panagiotakos, D.B.; Priftis, K.N.; Nagel, G. Influence of Mediterranean diet on asthma in children: A systematic review and meta-analysis. Pediatr. Allergy Immunol. 2013, 24, 330–338. [Google Scholar] [CrossRef]
- Mccormack, M.C.; Appel, L.; White, K. Healthy eating better breathing: A dietary intervention study in asthma. Am. J. Respir. Crit. Care Med. 2015, 191, A1744. [Google Scholar]
- Romieu, I.; Barraza-Villarreal, A.; Escamilla-Núñez, C.; Texcalac-Sangrador, J.L.; Hernandez-Cadena, L.; Díaz-Sánchez, D.; De Batlle, J.; E Del Rio-Navarro, B. Dietary intake, lung function, and airway inflammation in Mexico City school children exposed to air pollutants. Respir. Res. 2009, 10, 122. [Google Scholar] [CrossRef]
- Calatayud-Sáez, F.M.; Calatayud, B.; Calatayud, A. Effects of the Mediterranean diet on morbidity from inflammatory and recurrent diseases with special reference to childhood asthma. Nutrients 2022, 14, 936. [Google Scholar] [CrossRef]
- Jensen, M.E.; Gibson, P.G.; Collins, C.E.; Hilton, J.M.; Wood, L.G. Diet-induced weight loss in obese children with asthma: A randomized controlled trial. Clin. Exp. Allergy 2013, 43, 775–784. [Google Scholar] [CrossRef]
- Korkmaz, G.Ö.; Kabaran, S. Protective effects of a Mediterranean-like dietary pattern on obesity, abdominal obesity, and large neck circumference in a cohort of Turkish children aged 6–9 years. Asia Pac. J. Clin. Nutr. 2020, 29, 363–371. [Google Scholar]
- Archero, F.; Ricotti, R.; Solito, A.; Carrera, D.; Civello, F.; Di Bella, R.; Bellone, S.; Prodam, F. Adherence to the Mediterranean diet among school children and adolescents living in northern Italy and unhealthy food behaviors associated with overweight. Nutrients 2018, 10, 1322. [Google Scholar] [CrossRef] [PubMed]
- Bawaked, R.A.; Gomez, S.F.; Homs, C.; Casas Esteve, R.; Cardenas, G.; Fíto, M.; Schröder, H. Association of eating behaviors, lifestyle, and maternal education with adherence to the Mediterranean diet in Spanish children. Appetite 2018, 130, 279–285. [Google Scholar] [CrossRef] [PubMed]
- He, Z.H.; Zhao, G.G.; Xing, R.; Quan, M.H.; Rong, X.; Quan, M.H. Effects of RCT interventions on sedentary behavior and Screentime in children and adolescents aged 2 to 18 based on smartphone technology: Meta-analysis. Chin. Sport Sci. Technol. 2022, 58, 98–107. [Google Scholar]
- Fang, K.; Mu, M.; Liu, K.; He, Y. Screen time and childhood overweight/obesity: A systematic review and meta-analysis. Child. Care Health Dev. 2019, 45, 744–753. [Google Scholar] [CrossRef]
- Li, M.Y.; Cui, Y.F.; Wang, S.Q.; Tian, Z.T.; Peng, Y.G. Correlations among screen time, outdoor activity time, and physical health of preschoolers. J. Bio-Educ. 2021, 9, 96–101. [Google Scholar]
- Haghjoo, P.; Siri, G.; Soleimani, E.; Farhangi, M.A.; Alesaeidi, S. Screen time increases overweight and obesity risk among adolescents: A systematic review and dose-response meta-analysis. BMC Prim. Care 2022, 23, 161. [Google Scholar] [CrossRef]

| Group Name | N | Gender | Mean Age at Baseline [Years] | Mean BMI ± SD at Baseline [kg/m2] | Mean BMI BMI ± SD at the End of the Study [kg/m2] |
|---|---|---|---|---|---|
| Asthma and overweight/obesity | 50 | 34 F | 12.54 ± 3.58 | 25.86 ± 4.16 | 22.08 ± 3.30 |
| 16 M | |||||
| Overweight/obesity | 50 | 23 F | 11.02 ± 3.23 | 26.42 ± 4.86 | 22.29 ± 4.45 |
| 27 M | |||||
| Control | 42 | 24 F | 12.24 ± 3.47 | 18.07 ± 1.66 | 18.66 ± 1.89 |
| 18 M |
| C-Before | C-After | AO-Before | AO-After | O-Before | O-After | |
|---|---|---|---|---|---|---|
| Selected laboratory parameter | n = 42 | n = 42 | n = 50 | n = 50 | n = 50 | n = 50 |
| TC [mg/dL] | 155.58 a ± 3.02 | 155.22 a ± 3.28 | 183.57 c ± 3.68 | 163.93 b ± 3.84 | 195.54 d ± 2.08 | 175.87 c ± 1.67 |
| HDL [mg/dL] | 45.51 abc ± 0.95 | 45.59 abc ± 1.18 | 42.50 a ± 1.29 | 49.49 c ± 1.16 | 43.43 ab ± 1.13 | 48.08 bc ± 1.09 |
| LDL [mg/dL] | 88.72 a ± 2.49 | 81.47 a ± 1.97 | 88.04 c ± 2.52 | 79.30 bc ± 2.39 | 99.00 c ± 2.08 | 87.35 b ± 2.01 |
| TG [mg/dL] | 85.69 a ± 4.02 | 82.60 a ± 3.50 | 119.58 d ± 3.74 | 99.03 c ± 2.85 | 99.89 bc ± 3.53 | 85.79 b ± 2.41 |
| glucose [mg/dL] | 87.84 b ± 1.38 | 87.39 b ± 1.46 | 95.02 c ± 1.74 | 89.95 b ± 1.84 | 86.84 b ± 1.65 | 81.92 a ± 1.62 |
| insulin [μU/mL] | 8.82 a ± 0.55 | 8.85 a ± 0.51 | 9.76 ab ± 0.82 | 8.81 a ± 0.80 | 12.87 c ± 0.97 | 11.57 bc ± 0.89 |
| HbA1c [%] | 5.35 ab ± 0.06 | 5.36 ab ± 0.06 | 5.50 b ± 0.07 | 5.26 a ± 0.07 | 5.73 c ± 0.07 | 5.41 ab ± 0.08 |
| HOMA-IR | 1.90 a ± 0.12 | 1.96 a ± 0.12 | 3.35 c ± 0.17 | 2.87 b ± 0.18 | 3.32 bc ± 0.16 | 2.93 bc ± 0.14 |
| AO-Before | AO-After | |
|---|---|---|
| n = 50 | n = 50 | |
| NDAS (days/month) | 15.26 b ± 1.23 | 7.40 a ± 0.97 |
| CRP level (mg/dL) | 1.46 b ± 0.07 | 1.01 a ± 0.09 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soczewka, M.; Waśniowska, J.; Skowrońska, B.; Szczepankiewicz, A.; Wojsyk-Banaszak, I.; Kędzia, A.; Niechciał, E. Effects of Nutritional Education and Diet on Obesity and Asthma Progression in Children and Adolescents. Nutrients 2025, 17, 1759. https://doi.org/10.3390/nu17111759
Soczewka M, Waśniowska J, Skowrońska B, Szczepankiewicz A, Wojsyk-Banaszak I, Kędzia A, Niechciał E. Effects of Nutritional Education and Diet on Obesity and Asthma Progression in Children and Adolescents. Nutrients. 2025; 17(11):1759. https://doi.org/10.3390/nu17111759
Chicago/Turabian StyleSoczewka, Monika, Justyna Waśniowska, Bogda Skowrońska, Aleksandra Szczepankiewicz, Irena Wojsyk-Banaszak, Andrzej Kędzia, and Elżbieta Niechciał. 2025. "Effects of Nutritional Education and Diet on Obesity and Asthma Progression in Children and Adolescents" Nutrients 17, no. 11: 1759. https://doi.org/10.3390/nu17111759
APA StyleSoczewka, M., Waśniowska, J., Skowrońska, B., Szczepankiewicz, A., Wojsyk-Banaszak, I., Kędzia, A., & Niechciał, E. (2025). Effects of Nutritional Education and Diet on Obesity and Asthma Progression in Children and Adolescents. Nutrients, 17(11), 1759. https://doi.org/10.3390/nu17111759







