Abstract
The detrimental impacts of postprandial hyperglycemia on health are a critical concern, and exercise is recognized a pivotal tool in enhancing glycemic control after a meal. However, current exercise recommendations for managing postprandial glucose levels remain fairly broad and require deeper clarification. This review examines the existing literature aiming to offer a comprehensive guide for exercise prescription to optimize postprandial glycemic management. Specifically, it considers various exercise parameters (i.e., exercise timing, type, intensity, volume, pattern) for crafting exercise prescriptions. Findings predominantly indicate that moderate-intensity exercise initiated shortly after meals may substantially improve glucose response to a meal in healthy individuals and those with type 2 diabetes. Moreover, incorporating short activity breaks throughout the exercise session may provide additional benefits for reducing glucose response.
1. Introduction
The adverse impacts of glucose variability and postprandial glucose spikes have undergone extensive scrutiny in recent years [1,2,3]. A significant portion of the day is spent in the postprandial state by most individuals [4,5], which amplifies the risks linked to prolonged high blood glucose levels. Notably, markedly excessive post-meal glucose spikes have been linked to increased oxidative stress, inflammatory markers, and endothelial dysfunction in both healthy individuals and those with diabetes. These conditions have been associated with an elevated susceptibility to developing cardiometabolic disorders and complications related to diabetes [1,3,6,7,8,9]. Nutrition and exercise are crucial as primary interventions to mitigate excessive glycemic responses in both healthy people and people with diabetes [10,11,12,13,14]. Nevertheless, despite the well documented benefits of exercise, sedentary behaviors are alarmingly on the rise across populations, contributing to an increased incidence of cardiometabolic disorders [15,16,17,18,19]. Therefore, incorporating regular physical activity and post-meal exercise is crucial for reducing the adverse effects of sedentary behaviors and managing blood glucose fluctuations.
Numerous studies have previously highlighted the advantages of exercise in regulating post-prandial blood glucose levels [10,11,12,13,14]. The American College of Sports Medicine (ACSM) has recently reiterated the significance of postprandial exercise for individuals with type 2 diabetes (T2D), recommending at least 45 min of any exercise type, at any intensity, after meals to improve postprandial glucose response [20]. This represents a significant step toward identifying specific exercise prescriptions for optimal post-meal glucose responses. However, fine-tuning modulation of exercise for maximum benefit remains a complex challenge.
Hence, this review aims to refine exercise prescriptions by examining the influence of various exercise parameters on post-meal glucose responses in both healthy individuals and those with T2D. By exploring the effects of exercise timing, volume (including duration and intensity), type, and pattern on post-meal glucose response, we could provide practical indications for tailoring exercise to enhance glucose management after meals for people with T2D and without.
2. Is There an Optimal Time for Exercise Relative to Meals? The Effects of Exercise Timing on Postprandial Glucose Response
The relationship between the timing of physical exercise and meals has garnered increasing attention for its potential to improve blood glucose levels after eating [10,12,13,14,21]. Given the crucial role of timing in exercise prescriptions, it has been suggested to introduce a third “T” into the FITT principles (frequency, intensity, time, and type) to emphasize this [22]. Furthermore, the latest physical activity guidelines for individuals with T2D recommend post-meal exercise for optimizing control over postprandial glucose excursions [20], echoing evidence that post-meal exercise significantly influences glucose management in healthy and diabetic individuals [10,11,12,14,21,23,24]. Although pre-meal exercise has been shown to attenuate postprandial lipid responses, particularly when performed several hours before eating [11,12], its impact on acute blood glucose management is less significant, especially if performed 12–16 h before eating [25,26]. Conversely, moderate-intensity aerobic or resistance exercises conducted 20–45 min prior to a meal have been shown to markedly lower post-meal glucose levels [27,28]. Similarly, Francois et al. (2014) reported improvements in the glucose response to each daily meal among individuals with impaired glucose tolerance and/or T2D who engaged in intense “exercise snacks” 30 min before meals [29]. These findings suggest benefits in timing exercise closely with meals. However, post-meal exercise seems to elicit a greater management of blood glucose compared with pre-meal exercise in healthy individuals and those with T2D [23,30,31,32,33,34], offering a significant reduction in the post-meal glucose excursion and the overall glycemic response [24,35,36]. The different effects between pre-prandial and post-prandial exercise may be influenced by several factors, such as the individual’s nutritional status, exercise intensity, and volume. These elements play critical roles in determining the efficacy of exercise in modulating glucose responses at a specific time.
Exercise prescriptions, therefore, consider not only the sequence of meals and exercise but also the time interval between them in relation to the expected blood glucose response. In healthy individuals, the glucose peak occurs 30 to 60 min after eating [9]. Research findings vary, with some studies reporting significant attenuation of the glucose peak when exercising 30 or 45 min after the start of the meal [37], while others have demonstrated that commencing exercise shortly after a meal more effectively blunts post-meal glucose excursion [23,28,34]. In particular, beginning exercise around 10–15 min after eating may attenuate the post-meal glucose peak more effectively compared to starting around 30 min later [23,38]. This is particularly relevant to prevent cardiometabolic disorders, as glucose levels in healthy individuals typically remains below 140 mg/dl, a threshold often surpassed in people with T2D [12,21,39].
Conversely, in people with diabetes, peak glucose levels reach considerably higher values, often occurring between 60 and 120 min after a meal [12,21,39]. This necessitates different considerations for optimal exercise timing prescriptions. Consistent with findings in healthy individuals, a broad consensus among studies suggests substantial benefits of exercising soon after a meal in people with T2D [12]. These studies demonstrate that exercising before the peak glucose levels occur yields greater benefits than waiting for longer periods post-meal [24,40]. For instance, 15 to 30 min of aerobic or resistance exercises initiated 30 min after a meal significantly reduced post-meal glucose peaks [24]. Similarly, a notable reduction in glucose excursions has been observed when exercise begins 45 min after breakfast or dinner [27,41], with some studies noting improvements even when activity commences 15 to 20 min after the start of a meal [35]. Despite these insights, further research is required to determine the optimal exercise timing for people with diabetes.
Considering all this evidence, initiating postprandial exercise before the peak glucose levels occur, approximately 15 min in healthy individuals and 30 min in people with T2D, is recommended. This approach may mitigate the post-meal glucose peak and overall glucose response.
In determining the optimal timing for exercise in relation to meal consumptions, it may be worth considering the specific metabolic effects induced by various options. Exercise enhances microvascular recruitment and blood flow in active muscles, thereby increasing glucose delivery, uptake, and disappearance from the bloodstream [42]. However, the nutritional state at the time of exercising may assume an important role in the dynamics of glucose appearance and disappearance.
Pre-meal exercise, especially in a fasted state, stimulates insulin sensitivity and fat oxidation, primarily sourcing glucose from hepatic sources, and in particular from glycogenolysis [42]. This mechanism aids in maintaining blood glucose stability, preventing hypoglycemia and countering the potential rise in glucose uptake induced by exercise via insulin-independent mechanisms [42]. Additionally, exercising in a fasted state may help in lowering fasting hyperglycemia and might be preferable to postprandial exercise, as it is characterized by lower gastrointestinal discomfort and may be more feasible for adopting higher intensities.
In the post-prandial state, glucose mainly derives from exogenous sources while hepatic glucose production is markedly reduced by food ingestion [42]. Glucose uptake during postprandial exercise is supported by both contraction and insulin-independent mechanisms, while the insulin response from meal ingestion is reduced [42]. With regards to the time window for postprandial exercise, it has been suggested that exercising too early after the meal may initially lower glucose levels, but could lead to a rebound increase later, diminishing the beneficial effects [12]. Therefore, it has been proposed that exercising in the so-called mid-postprandial period may represent the optimal choice for improving both the immediate post-meal glucose peak and overall daily glucose management in individuals with T2D or insulin resistance [43].
Incretin hormone (i.e., GLP-1 and GIP) secretion may be stimulated by exercise and play a role in slowing gastric emptying, thus facilitating the lowering of post-meal blood glucose concentrations [44].
One aspect to consider is that the glycemic response to the same meal can vary significantly between individuals [45], influenced by factors such as pre-exercise glucose levels, glucose tolerance, and glucose loads [46]. This variability suggests the importance of personalizing the starting time of exercise based on individual responses. In this regard, it has been suggested that initiating exercise 20 min before an individual postprandial glycemic peak can be effective [38]. This could be easily achieved by using continuous glucose monitoring (CGM), which could serve an educational purpose, helping individuals understand the impact of exercise on their glucose levels and potentially improving long-term adherence to exercise routines by providing real-time feedback on the effects of different activities and timings [47].
When discussing the optimal timing of exercise, another crucial factor to delve into is the specific time of day when physical activity occurs and its alignment with meals, which introduces significant complexity beyond the simple pre- or post-meal dichotomy. For instance, the dynamics of exercising before breakfast, in a state of fasting, vary distinctly from activity performed later in the day when the body is not in a fasted state. Research has shed light on the potential benefits of repeated exercise in a fasted state, often referred to as fasted training, which is noted for favorable adaptations in metabolic control, as highlighted in a comprehensive review by Edinburgh et al. (2022) [48].
Expanding this discussion further, it is crucial to acknowledge the influence of various factors beyond meal timing. Notably, the body’s insulin sensitivity is not static throughout the day; it diminishes as the day advances, with a significant reduction in the evening. This fluctuation could significantly impact the body’s response to exercise at different times of the day. Moreover, the post-meal glycemic response is influenced by more than just the immediately preceding meal. The “second-meal effect,” where the glycemic response to a meal is affected by earlier dietary intake and activity, underscores the interconnectedness of daily eating and exercise patterns. This effect suggests that the timing of exercise around lunch may have distinct outcomes compared to morning or evening sessions, areas that require further exploration given the concentration of research on morning and evening activities; far fewer studies have investigated the interaction between meals and exercise at lunchtime [49,50]. In addition, post-exercise nutrition, particularly carbohydrate intake, plays a critical role in enhancing insulin sensitivity, yet this does not always correlate directly with immediate postprandial glucose levels [51]. This phenomenon emphasizes the intricate interplay between the timing of meals and subsequent physical activity in shaping the metabolic responses.
Considering these multifaceted aspects provides a more comprehensive understanding of how the timing of exercise, in relation to meal schedules and the body’s circadian rhythms, can impact our metabolic responses and overall health outcomes.
In the context of diabetes, the interaction between exercise and pharmacological treatment is another relevant aspect to consider, as it may synergistically potentiate the reduction in post-meal glucose levels. However, findings on this aspect are restricted and discordant. In particular, it has been shown that diabetic individuals under metformin treatment have a significant reduction in the glucose peak after an exercise session started 30 min from the beginning of the meal [40,52]. Erikson et al. (2017) have reported that combining exercise and metformin elicited a greater reduction in the post-meal glucose response than either interventions alone [52]. Likewise, a recent study showed that engaging in 50 min of high-intensity interval exercise, initiated 90 min prior to an oral glucose tolerance test in conjunction with metformin, significantly improved insulin sensitivity compared to either intervention independently [42]. However, other research presents mixed outcomes, with some studies not observing additional benefits from combining exercise with metformin treatment, either acutely [53,54] or over the long term [55]. These findings highlight the potential for exercise to complement pharmacological treatment in diabetes management, though evidence remains varied. Further research is needed to clarify the optimal strategies for integrating physical activity with medication to maximize therapeutic benefits. Table 1 summarizes the key findings from the studies comparing different exercise timings.

Table 1.
Summary of representative studies comparing different exercise timings.
3. Which Type of Exercise Is the Most Effective?
Identifying the most effective exercise type for managing glucose plays an important role in prescribing exercise for post-meal glucose responses. It is firmly established that both aerobic and resistance exercises, especially when combined, significantly improve long-term glucose control in individuals with diabetes [56,57]. This is supported by research demonstrating their effectiveness in reducing 24 h and postprandial blood glucose levels, underscoring their important implications for diabetes management [10,11,14,41,58]. The latest physical activity guidelines for individuals with T2D recommend engaging in any form of exercise to enhance the glucose response after a meal [20].
Over recent years, numerous studies have explored the specific impacts of aerobic and resistance exercises in isolation on post-meal glucose responses. Specifically, research has demonstrated the efficacy of various aerobic exercises in reducing the glucose response to meals in both healthy individuals and those with T2D [23,59]. For example, studies have reported that cycling at different intensities significantly diminishes post-meal glucose excursions and overall responses in both healthy and diabetic populations [23,37,60,61,62]. Likewise, walking and running have shown significant improvements in the glucose response after a meal [23,30]. Studies conducted in our laboratory have indicated that engaging in 30 min of moderate-intensity walking, jogging, or cycling similarly reduced the post-meal glucose peak and 3 h postprandial glucose concentration in healthy individuals [23]. Additionally, elliptical exercise has been effective in lowering post-meal glucose spikes in healthy individuals [23].
While walking might be the simplest exercise to undertake due to its minimal equipment requirements, many individuals may find it challenging to step away from their workplace or home. Hence, alternative exercises that require minimal space availability or specific equipment, like stair climbing and descending and step exercises, fit these requirements. Several studies have demonstrated that brief intervals of 1 to 10 min of stair climbing and descending significantly enhance the post-meal glucose response in individuals with diabetes [63,64,65,66]. Recently, our findings have supported this, showing comparable benefits between 30 min of step exercises, structured as alternating 30 s of moderate-intensity work with 60 s of rest, and a 30 min continuous walk [32]. Taken together, this evidence indicates that although walking emerges as a primary option for improving the postprandial glucose response in both healthy individuals and those with diabetes, other aerobic exercise alternatives are available to accommodate the diversity in personal preferences and requirements.
Resistance exercise, like aerobic exercise, has shown positive impacts on post-meal glucose responses in both healthy and T2D individuals. Previous studies have highlighted the beneficial impact of engaging in resistance training either before or after consuming high-carbohydrate meals, with both approaches leading to significant improvements in glucose management [67,68,69]. Both traditional and circuit resistance training have demonstrated notable reductions in postprandial blood glucose levels. For example, performing 15 to 30 min of circuit resistance training after a standardized breakfast significantly lowered blood glucose levels in individuals with T2D and healthy counterparts, respectively [23,24]. Similarly, in the same populations, three sets of 16–30 repetitions at light-to-moderate intensity resulted in a clear reduction in the post-meal glucose peak and overall glycemic response to a meal [69].
Exploration into alternative methods of training muscle conditioning, such as neuromuscular electrical stimulation (NMES), has shown promising results. NMES has been reported to decrease glycemic levels after 30–60 min of passive application applied to leg muscles in both healthy and T2D individuals [70,71]. However, the combination of NMES with voluntary muscle contractions appears necessary to harness its full benefits, as passive NMES alone might not significantly alter postprandial glucose responses [32,72]. Recently, we have observed that 30 min of passive NMES, performed alternating 30 s of work with 60 s of rest, did not elicit any change on the postprandial glucose response in healthy individuals [32]. In contrast, performing voluntary muscle contractions in the lower limbs markedly decreased the glucose peak [32]. Furthermore, the advantageous outcomes of combining resistance exercise with NMES have also been observed in people with T2D. Indeed, 20 min of NMES combined with whole-body resistance exercises led to a notable attenuation of the post-meal glucose response [72]. This suggests that incorporating NMES into a resistance training regimen could offer a beneficial alternative for improving postprandial glucose control, especially for those unable to engage in traditional exercise routines. However, to ensure a practical and comfortable approach, careful consideration of frequency and duration of the stimulation must be given.
Aerobic and resistance exercises exhibit similar efficacy on the post-meal glucose response, offering valuable insights for both healthy individuals and those managing diabetes. For instance, engaging in 30 min of moderate-intensity aerobic exercise has been found to reduce overall glycemic responses as effectively as a matched-duration resistance exercise in healthy subjects [34]. This extends to those with T2D, where 45 min of pre-meal cycling and resistance exercise yielded comparable effects [73]. Furthermore, our research supports these findings, indicating that for people with T2D, 30 min of walking can lower post-meal glucose levels similarly to 15 min of resistance exercise. However, it was observed that aerobic exercise might offer a greater stimulus for mitigating the post-meal glucose peak [24], whereas resistance contributes to more stable glycemic levels over time [24].
The integration of aerobic and resistance exercises into a single regimen has been also investigated. Research has demonstrated that a combination of both exercise types offers superior benefits to the two types alone for improving 24 h glucose control [12,74]. However, when focusing solely on the post-meal glucose response, the benefits of the combination appear similar to aerobic or resistance exercise performed separately [23,24].
The sequence in which aerobic and resistance exercise are performed, when combined, may influence their effectiveness in glucose control in individuals with diabetes. Previous reports have indicated that, in individuals with type 1 diabetes, performing aerobic exercise before the resistance bout resulted in a more pronounced hypoglycemic effect compared to the reverse order [75]. These effects were attributed to the increased secretion of growth hormone during resistance exercise, which moderated the decline in glucose levels during the subsequent bout [76]. Recently, we have reported comparable outcomes in individuals with T2D, indicating a more significant decrease in the post-meal glucose peak following 30 min of combined aerobic–resistance exercise compared to the reverse sequence, highlighting the potential for strategically ordered exercise routines to enhance glycemic control in this population [24].
Hence, exercise prescriptions should consider various factors, including individuals’ time and space availability, cognitive and physical conditions, and personal preferences to promote adherence to the exercise program. While the overall reductions in post-meal glucose responses following aerobic exercise, resistance exercise, or a combination of both exercise types are comparable, individuals with T2D might benefit more from either engaging in aerobic exercise alone or starting with aerobic exercise before moving on to resistance training sessions to achieve a more pronounced mitigation of postprandial glucose excursions. In addition, for situations where traditional exercise may not be feasible, practical, or desired, incorporating simple movements or activities can be adopted to mitigate the glycemic response to a meal, even while seated. It has indeed been demonstrated that even simple “leg fidgeting” performed at regular intervals during the postprandial period can be effective in attenuating the postprandial glycemic and insulinemic response in obese individuals [77]. Furthermore, this strategy may counteract endothelial dysfunction induced by prolonged periods of sitting [78]. Similarly, the repeated contraction of a small amount of muscle mass for several hours post-meal, through so-called “soleus pushups”, appears to lead to a significant reduction in postprandial insulin and glucose concentrations in healthy individuals [79]. These minimal yet effective strategies can offer practical alternatives for improving glucose control, even in sedentary settings, underscoring the flexibility and adaptability required in managing diabetes effectively. Table 2 summarizes the key findings from the studies comparing different exercise types.

Table 2.
Summary of representative studies comparing different exercise types.
4. What Should Be the Exercise Duration and Intensity?
Exercise volume plays a crucial role in session planning, necessitating customized adjustments in duration and intensity to suit individual capabilities, yet guidelines on how to prescribe exercise volume for enhancing post-meal glucose control are still vague. The latest physical activity guidelines for individuals with T2D recommend engaging in 45 min of exercise at any intensity for improving post-meal glucose management [20]. However, time constraints pose a significant challenge to maintain high adherence to exercise. Similarly, high-intensity exercise might be challenging for some individuals, particularly when conducted shortly after a meal, which may lead to increased gastrointestinal disturbances, in addition to the increase in hepatic glucose production [81,82]. Hence, more detailed guidelines are required for ensuring a correct exercise volume prescription to provide an effective stimulus for enhancing postprandial glucose responses.
Duration and intensity should be tailored to enable individuals to complete the exercise session. Research covering a broad spectrum of exercise durations has shown that activities ranging from 10 to 120 min can positively affect post-meal glucose responses in both healthy individuals and those with T2D [34,38,83,84,85,86,87]. Notably, sessions lasting between 30 and 60 min has been consistently associated with significant improvements in postprandial blood glucose levels [60,62,70,86,87,88]. Such exercise durations have led to notable enhancements in overall glucose management, including reductions in post-meal glucose peaks and improvements in glycemic variability. This occurred for both light-to-moderate intensity exercises conducted after meals with varied compositions [23,24,31,32,34,38,60,62,88]. Our findings align with this, showing that engaging in 30 min of moderate-intensity aerobic exercise improved postprandial glucose responses similarly to a 45 min session [23]. Additionally, shorter durations of exercise, such as 10–15 min at light intensity, have demonstrated beneficial effects on glucose peaks and blood glucose levels comparable to longer durations of 30–40 min in healthy individuals [89,90].
Similar results were also observed in T2D patients. In fact, it has been shown that engaging in 15 min of light-to-moderate walking after each meal effectively reduces the postprandial response to the meal [41,91]. Likewise, 10 min of exercise yielded significant improvements in the post-meal glucose response, showing comparable effects to those observed with a 30 min session [83]. Additionally, engaging in 20 min of self-paced walking after a meal was equally effective as longer durations of 40 or 60 min in reducing postprandial blood glucose levels in individuals with T2D [92].
Collectively, these studies suggest that even brief exercise sessions at moderate intensities can serve as a viable stimulus for improving the glucose response to meals in both healthy individuals and those with T2D. Therefore, once the minimum dose is reached, the exercise duration has a smaller impact on postprandial glucose responses compared to other crucial parameters, such as timing. Table 3 summarizes the key findings from the studies comparing different exercise durations.

Table 3.
Summary of representative studies comparing different exercise durations.
Exercise intensity should be tailored not only in terms of exercise duration, but also to personal capabilities, health conditions, and preferences in order to promote adherence to postprandial exercise sessions. Some people may prefer short bouts of high-intensity exercise for higher enjoyment and as a time-saving strategy [93]. Indeed, previous studies have widely shown that high-intensity interval exercise is effective in improving post-meal glucose responses, daily glycemic variability, and overall 24 h glucose control [80,94]. These effects are comparable to those seen with continuous light- and moderate-intensity exercise in both healthy populations and populations with diabetes [28,95,96]. For example, Shambrook et al. (2018) found no difference in the post-meal glucose response among healthy individuals when they engaged in 30 min of postprandial continuous cycling starting 30 min after breakfast at either light (35 ± 7% VO2 reserve), moderate (48 ± 8% VO2 reserve), or vigorous intensity intervals (10 × 1 min bouts at 80% VO2 reserve with 2 min intervals at 31 ± 12% VO2 reserve) [62]. Conversely, Achten et al. (2003) reported that lower intensities (20 min of post-meal cycling at 20% or 40% of peak power output) were more effective in reducing post-meal glucose responses compared to higher intensities (cycling at 80% of peak power output) [97]. Light-to-moderate-intensity exercise after a meal may also offer a lower likelihood of gastrointestinal discomfort. Additionally, high-intensity exercise, due to the adrenergic response, may increase the rate of glucose appearance, resulting in the undesirable effect of blood glucose levels rising [12,42]. However, it has been previously shown that high-intensity interval exercise may increase glucose tolerance and insulin sensitivity, resulting in an enhanced glucose disposal to skeletal muscles, especially when performed after meals [43].
Therefore, the picture emerging from the current knowledge emphasizes the need to tailor exercise prescriptions to individual preferences and requirements. Notably, even a 15 to 30 min continuous exercise session can be effective in improving postprandial glycemia in both healthy individuals and those with T2D. Considering the duration, it is advisable to regulate intensity, favoring a light-to-moderate level when exercise is performed soon after meals. This approach not only supports more effective glucose management, but also encourages long-term exercise adherence by enhancing comfort, particularly due to potential gastrointestinal conditions at higher exercise intensities. Table 4 summarizes the key findings from the studies comparing different exercise intensities.

Table 4.
Summary of representative studies comparing different exercise intensities.
5. Activity Breaks: An Effective Exercise Modality
The rise in sedentary behaviors over recent years has posed significant challenges to maintaining optimal glucose control, especially post-meals. While continuous exercise effectively manages post-meal glycemia, its sustained execution can be challenging or undesirable for many. Dividing exercise into shorter bouts could provide an effective alternative for eliciting a positive impact on cardiometabolic variables and specifically for improving the post-meal glucose response. Studies have indicated that breaking up exercise into shorter segments, such as 15 min intervals around meals, may elicit similar or greater effects on meal-induced glucose responses in individuals with prediabetes or T2D compared to a singular longer session (45 min) performed in the morning or afternoon [98]. Similarly, these results were observed in healthy individuals, indicating improved postprandial glucose control with just 10 min of exercise before a meal [99]. Some evidence suggests that even shorter activity breaks might yield comparable or greater effects on post-meal glucose responses than prolonged exercise [23]. An interesting finding is that a combination of short activity breaks with a continuous exercise routine may be more effective than either modality alone. For example, combining 3 min activity breaks every 30 min of sitting with a 20–30 min continuous exercise routine significantly reduced the glucose responses to breakfast and lunch in obese individuals compared to continuous exercise without breaks [100].
Prescribing activity breaks requires consideration of several parameters, much like with continuous exercise, such as the type, intensity, duration, and frequency of the bouts. Studies have highlighted the effectiveness of various types of activity breaks in improving postprandial glucose responses. Individuals with cardiometabolic disorders, for instance, benefited from performing two sets of 15 repetitions of different resistance exercises every hour over a 4 h period post-meal [101]. Similarly, people with T2D also saw improvements from engaging in 6 min resistance exercises every 60 min of sitting for 7.5 h following their first meal of the day [102]. However, contrasting findings exist regarding the effects of resistance activity breaks in healthy individuals, with some noting significant benefits [103,104] and others observing no change in glucose responses [105,106]. Importantly, activity breaks can also consist of simple bodyweight exercises [104], which offer a versatile option in various everyday life contexts such as, for example, for avoiding prolonged sitting during the evening hours [107]. Activities like walking [23], leg cycling [108], and seated upper body movements have been proven effective for attenuating postprandial glycemic and insulinemic responses, particularly in obese individuals [109]. Stair climbing for short periods has also been shown to be an effective and practical exercise for breaking sedentary time [110,111], making it a viable option for workplace wellness programs [112]. Conversely, standing as an activity break type has yielded mixed results in postprandial glucose control and in any case exerts a lower effect compared to walking [113].
Studies examining the intensity of activity breaks have revealed that both light and moderate intensities can effectively mitigate post-meal glucose responses in individuals with metabolic disorders. For example, two minutes of light- or moderate-intensity walking breaks every 20 min of sitting significantly attenuated postprandial glucose responses in different population groups [114,115]. This effect extends to vigorous-intensity exercise, where two minutes of walking every 20 min of sitting, performed at moderate or vigorous intensities, significantly improved post-meal glucose responses in overweight and obese individuals [116]. Furthermore, there is evidence that vigorous-intensity activity breaks provided a better glycemic control when overweight/obese young men underwent activity breaks at higher compared to lower intensities [117].
Shorter bouts of activity may similarly impact postprandial glycemia compared with longer matched-intensity bouts. As a matter of fact, recent findings suggest brief walking breaks, lasting either 2.5 or 5 min, every 15 min of sitting, can similarly mitigate post-meal glucose excursions and improve glycemic responses over a 3 h period in healthy individuals [23].
While adjusting exercise bout duration and intensity is crucial to ensure tolerability for individuals based on their abilities and preferences, another essential factor to consider is the frequency of breaks, which appears to influence the post-meal glucose response. Several studies have shown a positive correlation between higher frequencies of activity breaks and greater improvements in postprandial glycemia in both healthy and diabetic populations [118,119,120]. While there is some variability in findings, with some studies indicating comparable effects regardless of break frequency, recent evidence suggests that more frequent breaks, such as exercising for 3 min every 15 min of sitting [120], or for 5 min every 30 min [121], might represent the optimal strategy for improving the post-meal glucose response.
In conclusion, activity breaks present a significant opportunity for both preventive and therapeutic intervention in managing postprandial glucose levels, particularly for those at risk of or with T2D. The mechanism underlying their effectiveness likely involves the substantial stimulation exerted by muscle during repeated short bouts of exercise, which may enhance glucose uptake and facilitate a steady reduction in blood sugar levels. Notably, the avoidance of a glucose rebound after the cessation of exercise sessions underscores the benefits of frequent muscle activation throughout the postprandial period [23]. However, further studies are required to elucidate this aspect, evaluating how activity breaks influence the post-meal glucose levels. Interestingly, the potential role of gut hormones in modulating the postprandial response, enhanced by intermittent exercise like walking, introduces an additional layer of complexity [122]. Incorporating the activity breaks-based approach may serve as a complement to traditional continuous exercise routines or as a standalone strategy to provide a flexible, accessible means of glucose control for individuals who may find prolonged exercise sessions challenging, offering similar if not even greater benefits. Table 5 summarizes the key findings from the studies comparing different activity break protocols.

Table 5.
Summary of representative studies comparing different activity breaks.
6. Conclusions
While it is established that physical exercise plays an essential role in promoting postprandial glycemic control, to date, recommendations are quite general, lacking the specificity needed for tailoring exercise prescriptions. Evidence suggests the efficacy of moderate-intensity exercise conducted in the postprandial period for acutely lowering post-meal glucose levels, with added benefits observed when exercise starts soon after the meal (around 10–20 min before the expected glucose peak for healthy individuals, and within 15–30 min from the onset of the meal for people with diabetes). A session duration of 30 min of moderate-intensity exercise may be adequate to enhance postprandial glucose control (Figure 1). High-intensity exercise may also provide benefits, although it is more suitable when performed before a meal.
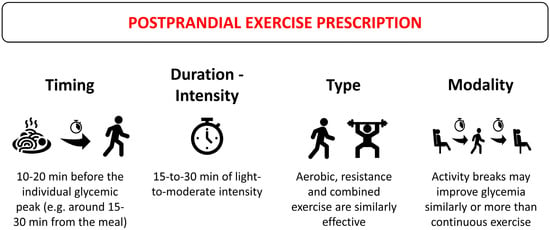
Figure 1.
General recommendations for postprandial exercise prescription for post-meal glucose management.
The reduction in the glucose response to a meal suggests that the type of exercise—whether aerobic, resistance, or a combination of those—should be guided by personal preference, accessibility, and feasibility for the individual. The sequence combining aerobic and resistance exercises could further optimize glycemic control in people with diabetes. Additionally, breaking down the exercise session into shorter activity bouts throughout the postprandial period might be more effective in improving post-meal glucose control in both healthy individuals and individuals with T2D.
Future studies should delve into the mechanisms that underpin the relationship between exercise and postprandial glucose control to better understand how exercise variables—such as timing, type, intensity and duration—specifically influence blood glucose dynamics after a meal. Additionally, exploring further the effects of exercising at different times of the day would further shed light on optimal windows for exercise to maximize glycemic benefits. Further studies are also required for a better understanding of the interplay between exercise and pharmacological treatments for diabetes, in order to elucidate whether a synergistic relationship exists between these interventions, potentially reducing reliance on medication through tailored exercise programs. In addition, further exploration is required to better understand the chronic effects of specific exercise regimens on metabolic health.
In any case, given the diverse ways through which exercise can exert its beneficial effects, an emphasis on personalized exercise prescriptions becomes paramount. A tailored approach that considers an individual’s specific needs, alongside their preferences and desires, ensures that the exercise regimen is not only practical but also enjoyable. This personalization is fundamental for promoting adherence over time and consequently enhancing its therapeutic effectiveness.
Author Contributions
Conceptualization, A.B. and M.S.; writing—original draft preparation, A.B.; writing—review and editing, A.B., A.S.d.P., A.N., I.B. and M.S.; supervision, M.S.; funding acquisition, I.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by University of Rome “Foro Italico”, grant number CDR2.BANDO2022NA.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ceriello, A.; Ihnat, M.A. ‘Glycaemic Variability’: A New Therapeutic Challenge in Diabetes and the Critical Care Setting. Diabet. Med. 2010, 27, 862–867. [Google Scholar] [CrossRef] [PubMed]
- Færch, K.; Alssema, M.; Mela, D.J.; Borg, R.; Vistisen, D. Relative Contributions of Preprandial and Postprandial Glucose Exposures, Glycemic Variability, and Non-Glycemic Factors to HbA 1c in Individuals with and without Diabetes. Nutr. Diabetes 2018, 8, 38. [Google Scholar] [CrossRef] [PubMed]
- Standl, E.; Schnell, O.; Ceriello, A. Postprandial Hyperglycemia and Glycemic Variability. Diabetes Care 2011, 34, S120–S127. [Google Scholar] [CrossRef] [PubMed]
- Monnier, L.; Colette, C. Contributions of Fasting and Postprandial Glucose to Hemoglobin A1c. Endocr. Pract. 2006, 12, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Monnier, L.; Colette, C.; Owens, D.R. Glycemic Variability: The Third Component of the Dysglycemia in Diabetes. Is It Important? How to Measure It? J. Diabetes Sci. Technol. 2008, 2, 1094–1100. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, M.; Gerstein, H.C.; Wang, Y.; Yusuf, S. The Relationship between Glucose and Incident Cardiovascular Events. A Metaregression Analysis of Published Data from 20 Studies of 95,783 Individuals Followed for 12.4 Years. Diabetes Care 1999, 22, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Giugliano, D.; Ceriello, A.; Esposito, K. Glucose Metabolism and Hyperglycemia. Am. J. Clin. Nutr. 2008, 87, 217S–222S. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, J.H.; Bell, D.S.H. Postprandial Hyperglycemia/Hyperlipidemia (Postprandial Dysmetabolism) Is a Cardiovascular Risk Factor. Am. J. Cardiol. 2007, 100, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Rendell, M.S.; Jovanovic, L. Targeting Postprandial Hyperglycemia. Metabolism 2006, 55, 1263–1281. [Google Scholar] [CrossRef]
- Teo, S.Y.M.; Kanaley, J.A.; Guelfi, K.J.; Cook, S.B.; Hebert, J.J.; Forrest, M.R.L.; Fairchild, T.J. Exercise Timing in Type 2 Diabetes Mellitus: A Systematic Review. Med. Sci. Sports Exerc. 2018, 50, 2387–2397. [Google Scholar] [CrossRef]
- Haxhi, J.; Scotto di Palumbo, A.; Sacchetti, M. Exercising for Metabolic Control: Is Timing Important? Ann. Nutr. Metab. 2013, 62, 14–25. [Google Scholar] [CrossRef]
- Chacko, E. Exercising Tactically for Taming Postmeal Glucose Surges. Scientifica 2016, 2016, 4045717. [Google Scholar] [CrossRef] [PubMed]
- Engeroff, T.; Groneberg, D.A.; Wilke, J. After Dinner Rest a While, After Supper Walk a Mile? A Systematic Review with Meta-Analysis on the Acute Postprandial Glycemic Response to Exercise Before and After Meal Ingestion in Healthy Subjects and Patients with Impaired Glucose Tolerance. Sports Med. 2023, 53, 849–869. [Google Scholar] [CrossRef]
- Aqeel, M.; Forster, A.; Richards, E.; Hennessy, E.; McGowan, B.; Bhadra, A.; Guo, J.; Gelfand, S.; Delp, E.; Eicher-Miller, H. The Effect of Timing of Exercise and Eating on Postprandial Response in Adults: A Systematic Review. Nutrients 2020, 12, 221. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.T.; Healy, G.N.; Dunstan, D.W.; Zderic, T.W.; Owen, N. Too Little Exercise and Too Much Sitting: Inactivity Physiology and the Need for New Recommendations on Sedentary Behavior. Curr. Cardiovasc. Risk Rep. 2008, 2, 292–298. [Google Scholar] [CrossRef]
- Kohl, H.W.; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The Pandemic of Physical Inactivity: Global Action for Public Health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Colley, R.C.; Saunders, T.J.; Healy, G.N.; Owen, N. Physiological and Health Implications of a Sedentary Lifestyle. Appl. Physiol. Nutr. Metab. 2010, 35, 725–740. [Google Scholar] [CrossRef]
- Healy, G.N.; Wijndaele, K.; Dunstan, D.W.; Shaw, J.E.; Salmon, J.; Zimmet, P.Z.; Owen, N. Objectively Measured Sedentary Time, Physical Activity, and Metabolic Risk. Diabetes Care 2008, 31, 369–371. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Owen, N.; Yates, T.E.; Kingwell, B.A.; Dunstan, D.W. Sitting Less and Moving More: Improved Glycaemic Control for Type 2 Diabetes Prevention and Management. Curr. Diabetes Rep. 2016, 16, 114. [Google Scholar] [CrossRef]
- Kanaley, J.A.; Colberg, S.R.; Corcoran, M.H.; Malin, S.K.; Rodriguez, N.R.; Crespo, C.J.; Kirwan, J.P.; Zierath, J.R. Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement from the American College of Sports Medicine. Med. Sci. Sports Exerc. 2022, 54, 353–368. [Google Scholar] [CrossRef]
- Erickson, M.L.; Jenkins, N.T.; McCully, K.K. Exercise after You Eat: Hitting the Postprandial Glucose Target. Front. Endocrinol. 2017, 8, 228. [Google Scholar] [CrossRef] [PubMed]
- Reid, R.E.R.; Thivel, D.; Mathieu, M.-E. Understanding the Potential Contribution of a Third “T” to FITT Exercise Prescription: The Case of Timing in Exercise for Obesity and Cardiometabolic Management in Children. Appl. Physiol. Nutr. Metab. 2019, 44, 911–914. [Google Scholar] [CrossRef]
- Bellini, A.; Nicolò, A.; Bazzucchi, I.; Sacchetti, M. Effects of Different Exercise Strategies to Improve Postprandial Glycemia in Healthy Individuals. Med. Sci. Sports Exerc. 2021, 53, 1334–1344. [Google Scholar] [CrossRef] [PubMed]
- Bellini, A.; Nicolò, A.; Bulzomì, R.; Bazzucchi, I.; Sacchetti, M. The Effect of Different Postprandial Exercise Types on Glucose Response to Breakfast in Individuals with Type 2 Diabetes. Nutrients 2021, 13, 1440. [Google Scholar] [CrossRef] [PubMed]
- Heden, T.D.; Liu, Y.; Kearney, M.L.; Park, Y.; Dellsperger, K.C.; Thomas, T.R.; Kanaley, J.A. Prior Exercise and Postprandial Incretin Responses in Lean and Obese Individuals. Med. Sci. Sports Exerc. 2013, 45, 1897–1905. [Google Scholar] [CrossRef] [PubMed]
- Rees, J.L.; Chang, C.R.; François, M.E.; Marcotte-Chénard, A.; Fontvieille, A.; Klaprat, N.D.; Dyck, R.A.; Funk, D.R.; Snydmiller, G.; Bastell, K.; et al. Minimal Effect of Walking before Dinner on Glycemic Responses in Type 2 Diabetes: Outcomes from the Multi-Site E-PAraDiGM Study. Acta Diabetol. 2019, 56, 755–765. [Google Scholar] [CrossRef]
- Heden, T.D.; Winn, N.C.; Mari, A.; Booth, F.W.; Rector, R.S.; Thyfault, J.P.; Kanaley, J.A. Postdinner Resistance Exercise Improves Postprandial Risk Factors More Effectively than Predinner Resistance Exercise in Patients with Type 2 Diabetes. J. Appl. Physiol. 2015, 118, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Karstoft, K.; Christensen, C.S.; Pedersen, B.K.; Solomon, T.P.J. The Acute Effects of Interval- Vs Continuous-Walking Exercise on Glycemic Control in Subjects with Type 2 Diabetes: A Crossover, Controlled Study. J. Clin. Endocrinol. Metab. 2014, 99, 3334–3342. [Google Scholar] [CrossRef] [PubMed]
- Francois, M.E.; Baldi, J.C.; Manning, P.J.; Lucas, S.J.E.; Hawley, J.A.; Williams, M.J.A.; Cotter, J.D. ‘Exercise Snacks’ before Meals: A Novel Strategy to Improve Glycaemic Control in Individuals with Insulin Resistance. Diabetologia 2014, 57, 1437–1445. [Google Scholar] [CrossRef]
- Hatamoto, Y.; Goya, R.; Yamada, Y.; Yoshimura, E.; Nishimura, S.; Higaki, Y.; Tanaka, H. Effect of Exercise Timing on Elevated Postprandial Glucose Levels. J. Appl. Physiol. 2017, 123, 278–284. [Google Scholar] [CrossRef]
- Bellini, A.; Nicolò, A.; Bazzucchi, I.; Sacchetti, M. The Effects of Postprandial Walking on the Glucose Response after Meals with Different Characteristics. Nutrients 2022, 14, 1080. [Google Scholar] [CrossRef] [PubMed]
- Bellini, A.; Nicolò, A.; Rocchi, J.E.; Bazzucchi, I.; Sacchetti, M. Walking Attenuates Postprandial Glycemic Response: What Else Can We Do without Leaving Home or the Office? IJERPH 2022, 20, 253. [Google Scholar] [CrossRef] [PubMed]
- Nygaard, H.; Rønnestad, B.R.; Hammarström, D.; Holmboe-Ottesen, G.; Høstmark, A.T. Effects of Exercise in the Fasted and Postprandial State on Interstitial Glucose in Hyperglycemic Individuals. J. Sports Sci. Med. 2017, 16, 254–263. [Google Scholar] [PubMed]
- Solomon, T.P.J.; Tarry, E.; Hudson, C.O.; Fitt, A.I.; Laye, M.J. Immediate Post-Breakfast Physical Activity Improves Interstitial Postprandial Glycemia: A Comparison of Different Activity-Meal Timings. Pflug. Arch. Eur. J. Physiol. 2020, 472, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Colberg, S.R.; Zarrabi, L.; Bennington, L.; Nakave, A.; Thomas Somma, C.; Swain, D.P.; Sechrist, S.R. Postprandial Walking Is Better for Lowering the Glycemic Effect of Dinner than Pre-Dinner Exercise in Type 2 Diabetic Individuals. J. Am. Med. Dir. Assoc. 2009, 10, 394–397. [Google Scholar] [CrossRef] [PubMed]
- Yoko, N.; Hiroshi, Y.; Ying, J. Type and Timing of Exercise during Lunch Breaks for Suppressing Postprandial Increases in Blood Glucose Levels in Workers. J. Occup. Health 2021, 63, e12199. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, A.; Venn, B. The Timing of Activity after Eating Affects the Glycaemic Response of Healthy Adults: A Randomised Controlled Trial. Nutrients 2018, 10, 1743. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wongpipit, W.; Sun, F.; Sheridan, S.; Huang, W.Y.; Sit, C.H.; Wong, S.H. Walking Initiated 20 Minutes before the Time of Individual Postprandial Glucose Peak Reduces the Glucose Response in Young Men with Overweight or Obesity: A Randomized Crossover Study. J. Nutr. 2021, 151, 866–875. [Google Scholar] [CrossRef]
- Slama, G.; Elgrably, F.; Sola, A.; Mbemba, J.; Larger, E. Postprandial Glycaemia: A Plea for the Frequent Use of Delta Postprandial Glycaemia in the Treatment of Diabetic Patients. Diabetes Metab. 2006, 32, 187–192. [Google Scholar] [CrossRef]
- Huang, T.; Lu, C.; Schumann, M.; Le, S.; Yang, Y.; Zhuang, H.; Lu, Q.; Liu, J.; Wiklund, P.; Cheng, S. Timing of Exercise Affects Glycemic Control in Type 2 Diabetes Patients Treated with Metformin. J. Diabetes Res. 2018, 2018, 2483273. [Google Scholar] [CrossRef]
- Van Dijk, J.-W.; Venema, M.; Van Mechelen, W.; Stehouwer, C.D.A.; Hartgens, F.; Van Loon, L.J.C. Effect of Moderate-Intensity Exercise Versus Activities of Daily Living on 24-Hour Blood Glucose Homeostasis in Male Patients with Type 2 Diabetes. Diabetes Care 2013, 36, 3448–3453. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Cabañas, A.; Gonzalez, J.T. Role of Prior Feeding Status in Mediating the Effects of Exercise on Blood Glucose Kinetics. Am. J. Physiol. Cell Physiol. 2023, 325, C823–C832. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Fardman, B.M.; Ratamess, N.A.; Faigenbaum, A.D.; Bush, J.A. Efficacy of Postprandial Exercise in Mitigating Glycemic Responses in Overweight Individuals and Individuals with Obesity and Type 2 Diabetes—A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 4489. [Google Scholar] [CrossRef]
- Holst, J.J.; Albrechtsen, N.J.W.; Rosenkilde, M.M.; Deacon, C.F. Physiology of the Incretin Hormones, GIP and GLP-1—Regulation of Release and Posttranslational Modifications. Compr. Physiol. 2019, 9, 1339–1381. [Google Scholar] [CrossRef] [PubMed]
- Zeevi, D.; Korem, T.; Zmora, N.; Israeli, D.; Rothschild, D.; Weinberger, A.; Ben-Yacov, O.; Lador, D.; Avnit-Sagi, T.; Lotan-Pompan, M.; et al. Personalized Nutrition by Prediction of Glycemic Responses. Cell 2015, 163, 1079–1094. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.; Solomon, T.P.J. Exercise-Induced Improvements in Postprandial Glucose Response Are Blunted by Pre-Exercise Hyperglycemia: A Randomized Crossover Trial in Healthy Individuals. Front. Endocrinol. 2020, 11, 566548. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.R.; Russell, B.M.; Cyriac, T.; Francois, M.E. Using Continuous Glucose Monitoring to Prescribe a Time to Exercise for Individuals with Type 2 Diabetes. JCM 2023, 12, 3237. [Google Scholar] [CrossRef] [PubMed]
- Edinburgh, R.M.; Koumanov, F.; Gonzalez, J.T. Impact of Pre-exercise Feeding Status on Metabolic Adaptations to Endurance-type Exercise Training. J. Physiol. 2022, 600, 1327–1338. [Google Scholar] [CrossRef] [PubMed]
- Haxhi, J.; Leto, G.; Di Palumbo, A.S.; Sbriccoli, P.; Guidetti, L.; Fantini, C.; Buzzetti, R.; Caporossi, D.; Di Luigi, L.; Sacchetti, M. Exercise at Lunchtime: Effect on Glycemic Control and Oxidative Stress in Middle-Aged Men with Type 2 Diabetes. Eur. J. Appl. Physiol. 2016, 116, 573–582. [Google Scholar] [CrossRef]
- Sacchetti, M.; Haxhi, J.; Sgrò, P.; Scotto Di Palumbo, A.; Nicolò, A.; Bellini, A.; Bazzucchi, I.; Di Luigi, L. Effects of Exercise before and/or after a Mixed Lunch on Postprandial Metabolic Responses in Healthy Male Individuals. Eur. J. Nutr. 2021, 60, 3437–3447. [Google Scholar] [CrossRef]
- Johnson-Bonson, D.A.; Narang, B.J.; Davies, R.G.; Hengist, A.; Smith, H.A.; Watkins, J.D.; Taylor, H.; Walhin, J.-P.; Gonzalez, J.T.; Betts, J.A. Interactive Effects of Acute Exercise and Carbohydrate-Energy Replacement on Insulin Sensitivity in Healthy Adults. Appl. Physiol. Nutr. Metab. 2021, 46, 1207–1215. [Google Scholar] [CrossRef] [PubMed]
- Erickson, M.L.; Little, J.P.; Gay, J.L.; McCully, K.K.; Jenkins, N.T. Postmeal Exercise Blunts Postprandial Glucose Excursions in People on Metformin Monotherapy. J. Appl. Physiol. 2017, 123, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Boulé, N.G.; Robert, C.; Bell, G.J.; Johnson, S.T.; Bell, R.C.; Lewanczuk, R.Z.; Gabr, R.Q.; Brocks, D.R. Metformin and Exercise in Type 2 Diabetes. Diabetes Care 2011, 34, 1469–1474. [Google Scholar] [CrossRef] [PubMed]
- Myette-Côté, É.; Terada, T.; Boulé, N.G. The Effect of Exercise with or Without Metformin on Glucose Profiles in Type 2 Diabetes: A Pilot Study. Can. J. Diabetes 2016, 40, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Pilmark, N.S.; Lyngbæk, M.; Oberholzer, L.; Elkjær, I.; Petersen-Bønding, C.; Kofoed, K.; Siebenmann, C.; Kellenberger, K.; Van Hall, G.; Abildgaard, J.; et al. The Interaction between Metformin and Physical Activity on Postprandial Glucose and Glucose Kinetics: A Randomised, Clinical Trial. Diabetologia 2021, 64, 397–409. [Google Scholar] [CrossRef] [PubMed]
- on behalf of the Diabetes Aerobic and Resistance Exercise (DARE) trial investigators; Larose, J.; Sigal, R.J.; Khandwala, F.; Prud’homme, D.; Boulé, N.G.; Kenny, G.P. Associations between Physical Fitness and HbA1c in Type 2 Diabetes Mellitus. Diabetologia 2011, 54, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Sigal, R.J.; Kenny, G.P.; Boulé, N.G.; Wells, G.A.; Prud’homme, D.; Fortier, M.; Reid, R.D.; Tulloch, H.; Coyle, D.; Phillips, P.; et al. Effects of Aerobic Training, Resistance Training, or Both on Glycemic Control in Type 2 Diabetes: A Randomized Trial. Ann. Intern. Med. 2007, 147, 357. [Google Scholar] [CrossRef] [PubMed]
- Munan, M.; Oliveira, C.L.P.; Marcotte-Chénard, A.; Rees, J.L.; Prado, C.M.; Riesco, E.; Boulé, N.G. Acute and Chronic Effects of Exercise on Continuous Glucose Monitoring Outcomes in Type 2 Diabetes: A Meta-Analysis. Front. Endocrinol. 2020, 11, 495. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, J.-W.; Tummers, K.; Stehouwer, C.D.A.; Hartgens, F.; Van Loon, L.J.C. Exercise Therapy in Type 2 Diabetes. Diabetes Care 2012, 35, 948–954. [Google Scholar] [CrossRef]
- Aadland, E.; Hostmark, A.T. Very Light Physical Activity after a Meal Blunts the Rise in Blood Glucose and Insulin. Open Nutr. J. 2008, 2, 94–99. [Google Scholar] [CrossRef]
- Karstoft, K.; Mortensen, S.P.; Knudsen, S.H.; Solomon, T.P.J. Direct Effect of Incretin Hormones on Glucose and Glycerol Metabolism and Hemodynamics. Am. J. Physiol. Endocrinol. Metab. 2015, 308, E426–E433. [Google Scholar] [CrossRef] [PubMed]
- Shambrook, P.; Kingsley, M.I.; Wundersitz, D.W.; Xanthos, P.D.; Wyckelsma, V.L.; Gordon, B.A. Glucose Response to Exercise in the Post-prandial Period Is Independent of Exercise Intensity. Scand. Med. Sci. Sports 2018, 28, 939–946. [Google Scholar] [CrossRef] [PubMed]
- Bartholomae, E.M.; Moore, J.; Ward, K.; Kressler, J. Sex Differences in Postprandial Glucose Response to Short Bouts of Exercise: A Randomized Controlled Trial. J. Sci. Med. Sport 2019, 22, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Honda, H.; Igaki, M.; Hatanaka, Y.; Komatsu, M.; Tanaka, S.; Miki, T.; Suzuki, T.; Takaishi, T.; Hayashi, T. Stair Climbing/Descending Exercise for a Short Time Decreases Blood Glucose Levels after a Meal in Participants with Type 2 Diabetes. BMJ Open Diabetes Res. Care 2016, 4, e000232. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.; Salmons, H.; Vinoskey, C.; Kressler, J. A Single One-Minute, Comfortable Paced, Stair-Climbing Bout Reduces Postprandial Glucose Following a Mixed Meal. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1967–1972. [Google Scholar] [CrossRef] [PubMed]
- Takaishi, T.; Hayashi, T. Stair Ascending–Descending Exercise Accelerates the Decrease in Postprandial Hyperglycemia More Efficiently than Bicycle Exercise. BMJ Open Diabetes Res. Care 2017, 5, e000428. [Google Scholar] [CrossRef] [PubMed]
- Andersen, E.; Høstmark, A.T. Effect of a Single Bout of Resistance Exercise on Postprandial Glucose and Insulin Response the Next Day in Healthy, Strength-Trained Men. J. Strength Cond. Res. 2007, 21, 487. [Google Scholar] [CrossRef] [PubMed]
- Bittel, A.J.; Bittel, D.C.; Mittendorfer, B.; Patterson, B.W.; Okunade, A.L.; Abumrad, N.A.; Reeds, D.N.; Cade, W.T. A Single Bout of Premeal Resistance Exercise Improves Postprandial Glucose Metabolism in Obese Men with Prediabetes. Med. Sci. Sports Exerc. 2021, 53, 694–703. [Google Scholar] [CrossRef]
- Moreira, S.R.; Simões, G.C.; Moraes, J.V.N.; Motta, D.F.; Campbell, C.S.G.; Simões, H.G. Blood Glucose Control for Individuals with Type-2 Diabetes: Acute Effects of Resistance Exercise of Lower Cardiovascular-Metabolic Stress. J. Strength Cond. Res. 2012, 26, 2806–2811. [Google Scholar] [CrossRef]
- Miyamoto, T.; Fukuda, K.; Kimura, T.; Matsubara, Y.; Tsuda, K.; Moritani, T. Effect of Percutaneous Electrical Muscle Stimulation on Postprandial Hyperglycemia in Type 2 Diabetes. Diabetes Res. Clin. Pract. 2012, 96, 306–312. [Google Scholar] [CrossRef]
- Jabbour, G.; Belliveau, L.; Probizanski, D.; Newhouse, I.; McAuliffe, J.; Jakobi, J.; Johnson, M. Effect of Low Frequency Neuromuscular Electrical Stimulation on Glucose Profile of Persons with Type 2 Diabetes: A Pilot Study. Diabetes Metab. J. 2015, 39, 264. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Holzer, R.; Schulte-Körne, B.; Seidler, J.; Predel, H.-G.; Brinkmann, C. Effects of Acute Resistance Exercise with and without Whole-Body Electromyostimulation and Endurance Exercise on the Postprandial Glucose Regulation in Patients with Type 2 Diabetes Mellitus: A Randomized Crossover Study. Nutrients 2021, 13, 4322. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, J.-W.; Manders, R.J.F.; Tummers, K.; Bonomi, A.G.; Stehouwer, C.D.A.; Hartgens, F.; Van Loon, L.J.C. Both Resistance- and Endurance-Type Exercise Reduce the Prevalence of Hyperglycaemia in Individuals with Impaired Glucose Tolerance and in Insulin-Treated and Non-Insulin-Treated Type 2 Diabetic Patients. Diabetologia 2012, 55, 1273–1282. [Google Scholar] [CrossRef] [PubMed]
- Borror, A.; Zieff, G.; Battaglini, C.; Stoner, L. The Effects of Postprandial Exercise on Glucose Control in Individuals with Type 2 Diabetes: A Systematic Review. Sports Med. 2018, 48, 1479–1491. [Google Scholar] [CrossRef] [PubMed]
- Yardley, J.E.; Kenny, G.P.; Perkins, B.A.; Riddell, M.C.; Malcolm, J.; Boulay, P.; Khandwala, F.; Sigal, R.J. Effects of Performing Resistance Exercise Before Versus After Aerobic Exercise on Glycemia in Type 1 Diabetes. Diabetes Care 2012, 35, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Yardley, J.E.; Sigal, R.J.; Riddell, M.C.; Perkins, B.A.; Kenny, G.P. Performing Resistance Exercise before versus after Aerobic Exercise Influences Growth Hormone Secretion in Type 1 Diabetes. Appl. Physiol. Nutr. Metab. 2014, 39, 262–265. [Google Scholar] [CrossRef]
- Pettit-Mee, R.J.; Ready, S.T.; Padilla, J.; Kanaley, J.A. Leg Fidgeting During Prolonged Sitting Improves Postprandial Glycemic Control in People with Obesity. Obesity 2021, 29, 1146–1154. [Google Scholar] [CrossRef]
- Morishima, T.; Restaino, R.M.; Walsh, L.K.; Kanaley, J.A.; Fadel, P.J.; Padilla, J. Prolonged Sitting-Induced Leg Endothelial Dysfunction Is Prevented by Fidgeting. Am. J. Physiol. Heart Circ. Physiol. 2016, 311, H177–H182. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.T.; Hamilton, D.G.; Zderic, T.W. A Potent Physiological Method to Magnify and Sustain Soleus Oxidative Metabolism Improves Glucose and Lipid Regulation. iScience 2022, 25, 104869. [Google Scholar] [CrossRef]
- Nakayama, Y.; Ono, K.; Okagawa, J.; Urabe, J.; Yamau, R.; Ishikawa, A. Home-Based High-Intensity Interval Exercise Improves the Postprandial Glucose Response in Young Adults with Postprandial Hyperglycemia. Int. J. Environ. Res. Public Health 2022, 19, 4227. [Google Scholar] [CrossRef]
- Holst, J.J.; Gribble, F.; Horowitz, M.; Rayner, C.K. Roles of the Gut in Glucose Homeostasis. Diabetes Care 2016, 39, 884–892. [Google Scholar] [CrossRef] [PubMed]
- Schiavon, M.; Hinshaw, L.; Mallad, A.; Man, C.D.; Sparacino, G.; Johnson, M.; Carter, R.; Basu, R.; Kudva, Y.; Cobelli, C.; et al. Postprandial Glucose Fluxes and Insulin Sensitivity during Exercise: A Study in Healthy Individuals. Am. J. Physiol. Endocrinol. Metab. 2013, 305, E557–E566. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, A.N.; Mann, J.I.; Williams, S.; Venn, B.J. Advice to Walk after Meals Is More Effective for Lowering Postprandial Glycaemia in Type 2 Diabetes Mellitus than Advice That Does Not Specify Timing: A Randomised Crossover Study. Diabetologia 2016, 59, 2572–2578. [Google Scholar] [CrossRef] [PubMed]
- Iida, Y.; Takeishi, S.; Fushimi, N.; Tanaka, K.; Mori, A.; Sato, Y. Effect of Postprandial Moderate-Intensity Walking for 15-Min on Glucose Homeostasis in Type 2 Diabetes Mellitus Patients. Diabetol. Int. 2020, 11, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Oberlin, D.J.; Mikus, C.R.; Kearney, M.L.; Hinton, P.S.; Manrique, C.; Leidy, H.J.; Kanaley, J.A.; Rector, R.S.; Thyfault, J.P. One Bout of Exercise Alters Free-Living Postprandial Glycemia in Type 2 Diabetes. Med. Sci. Sports Exerc. 2014, 46, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Colberg, S.R.; Grieco, C.R.; Somma, C.T. Exercise Effects on Postprandial Glycemia, Mood, and Sympathovagal Balance in Type 2 Diabetes. J. Am. Med. Dir. Assoc. 2014, 15, 261–266. [Google Scholar] [CrossRef]
- Erickson, M.L.; Little, J.P.; Gay, J.L.; McCully, K.K.; Jenkins, N.T. Effects of Postmeal Exercise on Postprandial Glucose Excursions in People with Type 2 Diabetes Treated with Add-on Hypoglycemic Agents. Diabetes Res. Clin. Pract. 2017, 126, 240–247. [Google Scholar] [CrossRef]
- Høstmark, A.T.; Ekeland, G.S.; Beckstrøm, A.C.; Meen, H.D. Postprandial Light Physical Activity Blunts the Blood Glucose Increase. Prev. Med. 2006, 42, 369–371. [Google Scholar] [CrossRef] [PubMed]
- Lunde, M.S.H.; Hjellset, V.T.; Høstmark, A.T. Slow Post Meal Walking Reduces the Blood Glucose Response: An Exploratory Study in Female Pakistani Immigrants. J. Immigr. Minor. Health 2012, 14, 816–822. [Google Scholar] [CrossRef]
- Nygaard, H.; Tomten, S.E.; Høstmark, A.T. Slow Postmeal Walking Reduces Postprandial Glycemia in Middle-Aged Women. Appl. Physiol. Nutr. Metab. 2009, 34, 1087–1092. [Google Scholar] [CrossRef]
- Francois, M.E.; Little, J.P. The Impact of Acute High-Intensity Interval Exercise on Biomarkers of Cardiovascular Health in Type 2 Diabetes. Eur. J. Appl. Physiol. 2017, 117, 1607–1616. [Google Scholar] [CrossRef] [PubMed]
- Blankenship, J.M.; Chipkin, S.R.; Freedson, P.S.; Staudenmayer, J.; Lyden, K.; Braun, B. Managing Free-Living Hyperglycemia with Exercise or Interrupted Sitting in Type 2 Diabetes. J. Appl. Physiol. 2019, 126, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.E.; Bourne, J.E.; Little, J.P. Where Does HIT Fit? An Examination of the Affective Response to High-Intensity Intervals in Comparison to Continuous Moderate- and Continuous Vigorous-Intensity Exercise in the Exercise Intensity-Affect Continuum. PLoS ONE 2014, 9, e114541. [Google Scholar] [CrossRef] [PubMed]
- Gillen, J.B.; Little, J.P.; Punthakee, Z.; Tarnopolsky, M.A.; Riddell, M.C.; Gibala, M.J. Acute High-intensity Interval Exercise Reduces the Postprandial Glucose Response and Prevalence of Hyperglycaemia in Patients with Type 2 Diabetes. Diabetes Obes. Metab. 2012, 14, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Little, J.P.; Jung, M.E.; Wright, A.E.; Wright, W.; Manders, R.J.F. Effects of High-Intensity Interval Exercise versus Continuous Moderate-Intensity Exercise on Postprandial Glycemic Control Assessed by Continuous Glucose Monitoring in Obese Adults. Appl. Physiol. Nutr. Metab. 2014, 39, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Parker, L.; Shaw, C.S.; Banting, L.; Levinger, I.; Hill, K.M.; McAinch, A.J.; Stepto, N.K. Acute Low-Volume High-Intensity Interval Exercise and Continuous Moderate-Intensity Exercise Elicit a Similar Improvement in 24-h Glycemic Control in Overweight and Obese Adults. Front. Physiol. 2017, 7, 661. [Google Scholar] [CrossRef] [PubMed]
- Achten, J.; Jeukendrup, A.E. Effects of Pre-Exercise Ingestion of Carbohydrate on Glycaemic and Insulinaemic Responses during Subsequent Exercise at Differing Intensities. Eur. J. Appl. Physiol. 2003, 88, 466–471. [Google Scholar] [CrossRef] [PubMed]
- DiPietro, L.; Gribok, A.; Stevens, M.S.; Hamm, L.F.; Rumpler, W. Three 15-Min Bouts of Moderate Postmeal Walking Significantly Improves 24-h Glycemic Control in Older People at Risk for Impaired Glucose Tolerance. Diabetes Care 2013, 36, 3262–3268. [Google Scholar] [CrossRef] [PubMed]
- Shambrook, P.; Kingsley, M.I.; Taylor, N.F.; Wundersitz, D.W.; Wundersitz, C.E.; Paton, C.D.; Gordon, B.A. A Comparison of Acute Glycaemic Responses to Accumulated or Single Bout Walking Exercise in Apparently Healthy, Insufficiently Active Adults. J. Sci. Med. Sport 2020, 23, 902–907. [Google Scholar] [CrossRef]
- Wheeler, M.J.; Green, D.J.; Cerin, E.; Ellis, K.A.; Heinonen, I.; Lewis, J.; Naylor, L.H.; Cohen, N.; Larsen, R.; Dempsey, P.C.; et al. Combined Effects of Continuous Exercise and Intermittent Active Interruptions to Prolonged Sitting on Postprandial Glucose, Insulin, and Triglycerides in Adults with Obesity: A Randomized Crossover Trial. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 152. [Google Scholar] [CrossRef]
- Kowalsky, R.J.; Jakicic, J.M.; Hergenroeder, A.; Rogers, R.J.; Gibbs, B.B. Acute Cardiometabolic Effects of Interrupting Sitting with Resistance Exercise Breaks. Appl. Physiol. Nutr. Metab. 2019, 44, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Homer, A.R.; Taylor, F.C.; Dempsey, P.C.; Wheeler, M.J.; Sethi, P.; Townsend, M.K.; Grace, M.S.; Green, D.J.; Cohen, N.D.; Larsen, R.N.; et al. Frequency of Interruptions to Sitting Time: Benefits for Postprandial Metabolism in Type 2 Diabetes. Diabetes Care 2021, 44, 1254–1263. [Google Scholar] [CrossRef]
- Climie, R.E.; Grace, M.S.; Larsen, R.L.; Dempsey, P.C.; Oberoi, J.; Cohen, N.D.; Owen, N.; Kingwell, B.A.; Dunstan, D.W. Regular Brief Interruptions to Sitting after a High-Energy Evening Meal Attenuate Glycemic Excursions in Overweight/Obese Adults. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Larsen, R.N.; Sethi, P.; Sacre, J.W.; Straznicky, N.E.; Cohen, N.D.; Cerin, E.; Lambert, G.W.; Owen, N.; Kingwell, B.A.; et al. Benefits for Type 2 Diabetes of Interrupting Prolonged Sitting with Brief Bouts of Light Walking or Simple Resistance Activities. Diabetes Care 2016, 39, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Gillen, J.B.; Estafanos, S.; Williamson, E.; Hodson, N.; Malowany, J.M.; Kumbhare, D.; Moore, D.R. Interrupting Prolonged Sitting with Repeated Chair Stands or Short Walks Reduces Postprandial Insulinemia in Healthy Adults. J. Appl. Physiol. 2021, 130, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Charlett, O.P.; Morari, V.; Bailey, D.P. Impaired Postprandial Glucose and No Improvement in Other Cardiometabolic Responses or Cognitive Function by Breaking up Sitting with Bodyweight Resistance Exercises: A Randomised Crossover Trial. J. Sports Sci. 2021, 39, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Gale, J.T.; Wei, D.L.; Haszard, J.J.; Brown, R.C.; Taylor, R.W.; Peddie, M.C. Breaking Up Evening Sitting with Resistance Activity Improves Postprandial Glycemic Response: A Randomized Crossover Study. Med. Sci. Sports Exerc. 2023, 55, 1471–1480. [Google Scholar] [CrossRef] [PubMed]
- Engeroff, T.; Füzeki, E.; Vogt, L.; Banzer, W. The Acute Effects of Single or Repeated Bouts of Vigorous-Intensity Exercise on Insulin and Glucose Metabolism during Postprandial Sedentary Behavior. Int. J. Environ. Res. Public Health 2022, 19, 4422. [Google Scholar] [CrossRef]
- McCarthy, M.; Edwardson, C.L.; Davies, M.J.; Henson, J.; Rowlands, A.; King, J.A.; Bodicoat, D.H.; Khunti, K.; Yates, T. Breaking up Sedentary Time with Seated Upper Body Activity Can Regulate Metabolic Health in Obese High-risk Adults: A Randomized Crossover Trial. Diabetes Obes. Metab. 2017, 19, 1732–1739. [Google Scholar] [CrossRef]
- Rafiei, H.; Omidian, K.; Myette-Côté, É.; Little, J.P. Metabolic Effect of Breaking Up Prolonged Sitting with Stair Climbing Exercise Snacks. Med. Sci. Sports Exerc. 2021, 53, 150–158. [Google Scholar] [CrossRef]
- Cho, M.J.; Bunsawat, K.; Kim, H.J.; Yoon, E.S.; Jae, S.Y. The Acute Effects of Interrupting Prolonged Sitting with Stair Climbing on Vascular and Metabolic Function after a High-Fat Meal. Eur. J. Appl. Physiol. 2020, 120, 829–839. [Google Scholar] [CrossRef]
- Stork, M.J.; Marcotte-Chénard, A.; Jung, M.E.; Little, J.P. Exercise in the Workplace: Examining the Receptivity of Practical and Time-Efficient Stair-Climbing “Exercise Snacks”. Appl. Physiol. Nutr. Metab. 2024, 49, 30–40. [Google Scholar] [CrossRef]
- Buffey, A.J.; Herring, M.P.; Langley, C.K.; Donnelly, A.E.; Carson, B.P. The Acute Effects of Interrupting Prolonged Sitting Time in Adults with Standing and Light-Intensity Walking on Biomarkers of Cardiometabolic Health in Adults: A Systematic Review and Meta-Analysis. Sports Med. 2022, 52, 1765–1787. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.P.; Broom, D.R.; Chrismas, B.C.R.; Taylor, L.; Flynn, E.; Hough, J. Breaking up Prolonged Sitting Time with Walking Does Not Affect Appetite or Gut Hormone Concentrations but Does Induce an Energy Deficit and Suppresses Postprandial Glycaemia in Sedentary Adults. Appl. Physiol. Nutr. Metab. 2016, 41, 324–331. [Google Scholar] [CrossRef]
- Dunstan, D.W.; Kingwell, B.A.; Larsen, R.; Healy, G.N.; Cerin, E.; Hamilton, M.T.; Shaw, J.E.; Bertovic, D.A.; Zimmet, P.Z.; Salmon, J.; et al. Breaking Up Prolonged Sitting Reduces Postprandial Glucose and Insulin Responses. Diabetes Care 2012, 35, 976–983. [Google Scholar] [CrossRef]
- Bhammar, D.M.; Sawyer, B.J.; Tucker, W.J.; Gaesser, G.A. Breaks in Sitting Time: Effects on Continuously Monitored Glucose and Blood Pressure. Med. Sci. Sports Exerc. 2017, 49, 2119–2130. [Google Scholar] [CrossRef]
- Hatamoto, Y.; Yoshimura, E.; Takae, R.; Komiyama, T.; Matsumoto, M.; Higaki, Y.; Tanaka, H. The Effects of Breaking Sedentary Time with Different Intensity Exercise Bouts on Energy Metabolism: A Randomized Cross-over Controlled Trial. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1879–1889. [Google Scholar] [CrossRef] [PubMed]
- Maylor, B.D.; Zakrzewski-Fruer, J.K.; Stensel, D.J.; Orton, C.J.; Bailey, D.P. Effects of Frequency and Duration of Interrupting Sitting on Cardiometabolic Risk Markers. Int. J. Sports Med. 2019, 40, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Mackie, P.; Crowfoot, G.; Gyawali, P.; Janssen, H.; Holliday, E.; Dunstan, D.; English, C. Acute Effects of Frequent Light-Intensity Standing-Based Exercises That Interrupt 8 Hours of Prolonged Sitting on Postprandial Glucose in Stroke Survivors: A Dose-Escalation Trial. J. Phys. Act. Health 2021, 18, 644–652. [Google Scholar] [CrossRef]
- Paing, A.C.; McMillan, K.A.; Kirk, A.F.; Collier, A.; Hewitt, A.; Chastin, S.F.M. Dose-Response between Frequency of Breaks in Sedentary Time and Glucose Control in Type 2 Diabetes: A Proof of Concept Study. J. Sci. Med. Sport 2019, 22, 808–813. [Google Scholar] [CrossRef]
- Duran, A.T.; Friel, C.P.; Serafini, M.A.; Ensari, I.; Cheung, Y.K.; Diaz, K.M. Breaking Up Prolonged Sitting to Improve Cardiometabolic Risk: Dose–Response Analysis of a Randomized Crossover Trial. Med. Sci. Sports Exerc. 2023, 55, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-C.; Walhin, J.-P.; Hengist, A.; Gonzalez, J.T.; Betts, J.A.; Thompson, D. Interrupting Prolonged Sitting with Intermittent Walking Increases Postprandial Gut Hormone Responses. Med. Sci. Sports Exerc. 2022, 54, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).