Abstract
Background and aims: Home parenteral nutrition (HPN) is a life-saving treatment for patients affected by chronic intestinal failure (CIF). Both this clinical condition and its therapy require radical lifestyle modifications, affecting life quality and psychological balance in patients as well as family members. Patient psychological burden has rarely been taken into consideration, not to mention that of caregivers. This study aims to evaluate the levels of anxiety in CIF patients on HPN, and their caregivers, consequently determining their impact on the psychological and physical aspects. Methods: After a brief introductory interview, adult patients on HPN for CIF and their caregivers were asked to fill in the HAMA-A questionnaire. Results: Fifty patients and their respective caregivers were enrolled. Mean HAMA-A scores were similar in patients and caregivers and testified the presence of a mild to severe impact of CIF and HPN in both groups, with a significantly higher impact on female patients and caregivers. After adjusting age, education level, duration of CIF and HPN dependence, and degree of kinship, no differences were revealed in the scores. Conclusions: The study confirms that CIF patients on HPN and their caregivers have a significant anxiety burden independently from the duration of the disease, therefore needing appropriate support.
1. Introduction
Chronic intestinal failure (CIF) is a severe malabsorptive condition in which patients become dependent on home parenteral nutrition (HPN) to assure their nutritional and fluid requirements [1,2].
In general, this condition occurs almost unexpectedly due to intestinal ischemia, Crohn’s disease, and other pathologies, significantly affecting the lives of patients and family members. Indeed, patients immediately find themselves in a new anatomical and clinical condition attributable to the loss of their bowel function. Patients initially feel disbelief, anxiety, hopelessness, and grief ascribable to the loss of freely eating and drinking, together with problems in body image, work, and family relationships [3,4].
Patients with CIF must struggle against a life-threatening disease and may be worried about repeated surgeries and hospital admissions, experiencing fatigue which interferes with their daily life activities [5]. Fatigue is a complex concept that may include physical, social, and psychological dimensions [6], and may also be associated with anxiety and depression [5]. Finally, patients may have a reduced working capacity since they have to manage HPN therapy, eating and drinking medical prescriptions, intestinal functions, and eventually a stoma [5,6].
HPN dependence influences patient autonomy, work ability, and capacity to travel and socialize [7]; moreover, sleep quality is significantly compromised due to the administration of therapy during night hours [8,9,10]. Most forms of CIF are often lifelong conditions with HPN dependency for many years. On the other hand, HPN infusions can last up to 12 h and longer in some instances, therefore affecting everyday life.
In addition, although life sustaining for CIF patients, HPN may be hampered by serious complications, often requiring hospitalization [9], including catheter-related bloodstream infections, thrombosis, embolism [9,10,11], and long-term hepatic failure and osteoporosis [12].
Affected by such a severe disease, patients almost always need the help of their family members [5]. For this reason, it is important to consider the psychological, economic, and social strains on caregivers who have to re-organize their life and work according to the new family condition. Initially, they may feel a certain amount of responsibility, stress, and anxiety in learning how to manage HPN and eventual consequential complications [13].
However, because of the low CIF prevalence, the burden that caregivers face has not been adequately characterized.
The objective of this study was to investigate the burden experienced by adult caregivers of adult patients with CIF. Caregivers may experience fatigue, sleep disturbance, and some strain and stress, with markedly reduced productivity; furthermore, caregiving responsibilities may limit time with family, friends, and recreational activities.
The levels of anxiety and stress in patients and their caregivers may influence the approach to the disease and to HPN, negatively affecting life quality [11,12,14,15].
To the best of our knowledge, very little emphasis has been placed on the psychological issues of CIF patients on HPN and even less on their caregivers.
2. Aims of the Study
The present study aims to measure the anxiety burden in CIF patients on HPN and in their caregivers. A secondary aim is to search for possible correlations between anxiety levels and disease duration, education, employment, and degree of kinship between patients and caregivers.
3. Patients and Methods
3.1. Study Population
All consecutive CIF patients on HPN and their caregivers, meeting the following inclusion and exclusion criteria, were asked to participate in this study.
3.2. Inclusion Criteria
- -
- CIF patients and caregivers aged between 18 and 70;
- -
- CIF patients on HPN from at least 1 month;
- -
- Signed informed consent.
3.3. Exclusion Criteria
- -
- Drug addiction or abuse;
- -
- Psychosis or personality disorders classified according to the DSM-V criteria;
- -
- Acute medical complications requiring hospitalization.
After having signed the informed consent, during a brief interview, data on age, employment, education, and degree of kinship were collected both for patients and their caregivers to evaluate a possible correlation with anxiety levels.
As far as education, patients and caregivers were classified as having completed primary school, secondary school, high school, or a university degree. As far as kinship, people were categorized as follows: husband, wife, son/daughter, mother/father, and brother/sister. Employment was identified as remunerated or non-remunerated, and the latter comprised housewives and unemployed people; in addition, the category of retirement was also identified.
Information on disease type and duration and HPN dependence was obtained from the patients’ medical records.
Patients and caregivers took part in an introductory meeting held with a dedicated psychologist to receive instructions on the modality to fill out the Hamilton Anxiety Rating Scale (HAM-A) questionnaire.
All subjects signed an informed consent for inclusion before participating in the study. The study was conducted in accordance with the declaration of Helsinki and approved by the Ethics Committee of A.O.U. Federico II—AORN Cardarelli (ethical approval date: 24 October 2018; prot. n: 317/18).
3.4. The Hamilton Anxiety Rating Scale (HAM-A)
The Hamilton Anxiety Rating Scale (HAM-A) [16], created by Hamilton in 1959, is still today one of the most widely used rating scales to measure the severity of perceived anxiety symptoms [17,18,19]. It is a clinician-rated evaluation, consisting of 14 symptom-defined elements, for both psychological and somatic symptoms.
Each item, based on a five-point ratio scale, is scored independently according to the intensity of symptoms perceived by the patients: 0 indicates an absence of feeling; 1 is equivalent to mild, 2 to moderate, 3 to severe, and 4 to very severe symptoms.
Once the evaluation is completed, the clinician sums up the scores based on the 14 individually rated items, yielding a result ranging from 0 to 56.
HAM-A cut offs are: ≥18—mild anxiety; ≥19–25—moderate anxiety; ≥19–25—moderate anxiety.
The 14 single items are as follows:
- Anxious mood (worries, fear of the worst, irritability);
- Tension (startle response, fatigability, restlessness, easy tearing, trembling, inability to relax);
- Fear (of the dark/traffic/crowds, of being left alone);
- Insomnia (difficulty in falling asleep, broken sleep, unsatisfying sleep and fatigue on waking, dreams, nightmares, night terrors);
- Cognitive functions (poor memory and difficulty in concentration);
- Depressed mood (loss of interest, lack of pleasure in hobbies, depression, shifting moods);
- Somatic muscular symptoms (aches and pains, stiffness, bruxism, twitching, myoclonic jerks, teeth grinding, unsteady voice, increased muscular tone);
- Sensory (tinnitus, blurred vision, hot and cold flushes, feelings of weakness, pricking sensation);
- Cardiovascular (tachycardia, extrasystoles, palpitations, chest pain, vessel throbbing, faint feeling);
- Respiratory (chest tightness, choking pressure, sighing, dyspnoea);
- Gastrointestinal (irritable bowel syndrome-type symptoms, abdominal colicky pain, burning sensations, abdominal fullness, swallowing difficulty, nausea, vomiting, borborygmi, looseness of bowels/constipation, weight loss);
- Genitourinary (urinary frequency or urgency, amenorrhea, menorrhagia, frigidity, premature ejaculation, loss of libido, impotence);
- Autonomic (dry mouth, tension headache, flushing, sweating, giddiness, goose bumps);
- Observed behaviour at interview (fidgeting, restlessness or pacing, tremor of hands, furrowed brow, strained face, sighing or rapid respiration, pallor, swallowing, etc.).
3.5. Statistical Analysis
Data were included in a database, expressed as mean ± SD, when appropriate, and analysed with SPSS ver. 28. The t-test was used for the comparison of continuous variables, while the Mann–Whitney test was used for the comparison of parametric variables. The significance level was reached with p values of p < 0.05.
4. Results
In total, 50 patients (28 F; 22 M) and 50 respective caregivers (34 F; 16 M), both aged between 18 and 70, were enrolled. Personal (age, sex) and social (work, education) information of both are reported in Table 1.

Table 1.
Personal and social information of patients and caregivers.
As far as residual small bowel length, 7 patients did not undergo resections, while 43 patients had a median remnant small bowel of 108 cm (range of 15–300). In 38 patients, the small bowel was in continuity with the colon and, consequently, regularly canalized (no stoma). The percentage of colon in continuity was calculated according to the Cummings percentage [20]. Seven patients had an ileocecal valve, and twelve patients had a stoma.
The total HAM-A score revealed the presence of anxiety both in patients and caregivers, with a similar distribution among the mild, moderate, and severe levels in the two groups. None of the differences between groups were significant (Figure 1).
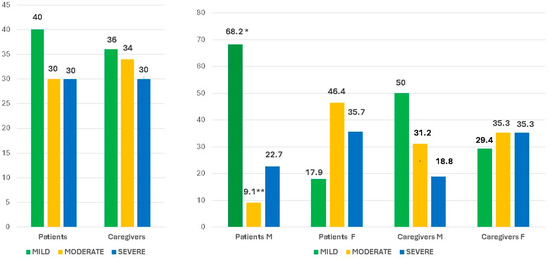
Figure 1.
Total HAM-A score in patients and caregivers both in the whole group and according to gender. * p= 0.001 M vs F; ** p = 0.004 M vs F.
Moreover, when dividing the groups according to gender, it can be seen that female patients had a significantly lower prevalence of mild (p = 0.001, Mann–Whitney test) and a higher prevalence of moderate (p = 0.004) anxiety levels than males (Figure 1).
In a similar way, although not significantly, in female caregivers, there was a trend for a higher prevalence of moderate and severe anxiety levels than males (Figure 1).
Education level and employment type did not influence the degree of anxiety.
The analysis of the single items of the HAM-A scale in patients and caregivers revealed the following (Figure 2):
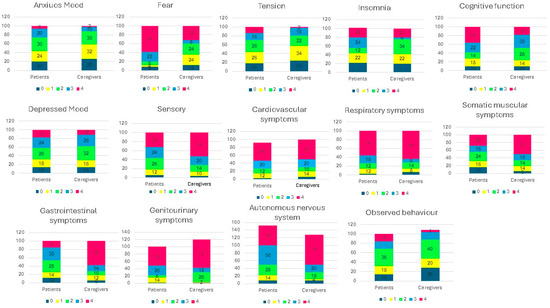
Figure 2.
Clinician-rated evaluation of the 14 items: anxious mood, tension, fear, insomnia, cognitive functions, depressed mood, somatic muscular symptoms, sensory, cardiovascular, respiratory, gastrointestinal, genitourinary, autonomic, observed behaviour at interview. Each item is based on a five-point ratio scale and is scored independently according to the intensity of what the patients felt: 0 = total absence of symptoms; 1 = mild symptoms; 2 = moderate symptoms; 3 = severe symptoms; 4 = very severe symptoms. Tension p: 0.027; fear: 0.009; Mann–Whitney test; somatic muscular symptoms: p = 0.024; sensory: p = 0.042; gastrointestinal p = 0.001; genitourinary p = 0.021.
Anxious mood: even if not statistically significant, there was a trend for higher rates of absent and mild anxiety in patients than caregivers.
The distribution of the tension levels was significantly different in the two groups; indeed, tension was absent in 14% of patients, while severe and very severe levels were mainly represented in the caregiver group.
Fear is almost absent (58 vs. 32%) or mild (22% vs. 8%) in patients, and moderate (24 vs. 8%) or severe (24 vs. 4%) in caregivers, with a significant different distribution among groups (p = 0.009).
As far as insomnia, there was no significant difference between the distribution levels in patients and caregivers, except for a higher trend of mild forms (22 vs. 4%) in patients and moderate forms in caregivers (34 vs. 12%).
Similarly, both intellectual functions and depressed mood are equally distributed in patients and caregivers, without significant differences.
Regarding somatic symptoms (muscular tension), 50% of caregivers (vs. 28% of patients) had no symptoms, and 16% of patients (vs. 6% of caregivers) had very severe symptoms, with a significantly different distribution (p = 0.026) among the two groups.
Also, sensory alterations were differently distributed between the two groups (p = 0.042) with 52% of caregivers (vs. 32% of patients) having no symptoms.
Cardiovascular and respiratory symptoms were almost absent or mild in both patients and caregivers, with a similar distribution in the two groups.
Gastrointestinal symptoms were absent in 58% of caregivers (vs. 16% patients), while they were present in most patients, with a different intensity. The calculated differences were significant (p = 0.003).
Similarly, genitourinary symptoms were absent in 78% of caregivers (vs. 52% of patients), while patients had diverse manifestation intensity with a meaningful different distribution between the two groups (p = 0.021).
Autonomic symptoms have analogous distribution in patients and controls; in 50% of both groups, an absence of symptoms was observed, whilst severe and very severe symptoms were found in a minority of patients (8%) and caregivers (12%).
Regarding the last item, observed behaviour at interview was absent in 14% of patients and 4% of caregivers, while for the other categories, the distribution was not significantly different in both groups.
5. Discussion
From the questionnaires completed, a mean moderate anxiety for disease and therapy was found in most patients and caregivers, with an approximate homogeneous distribution on the three levels. CIF patients are a group with heterogeneous clinical conditions, for many factors, including intestinal length, the presence of a stoma, the average volume of the parenteral nutritional support administered, and the frequency per week. The psychological state of patients was mostly derived from the awareness of their disease, the new anatomical and clinical conditions, HPN dependence, and worries regarding their future [1,8,13]. On the other hand, the new patient needs influenced the daily and working lives of caregivers [1,8,13]. Caregivers do not choose to care, but this happens because they have an emotional connection with the person requesting assistance.
Anxiety occurred independently from the type and duration of the disease, relation of kinship, education, and employment, confirming that both CIF and HPN represent an unexpected destabilization that chronically impacts daily life and lifestyle, and to which both patients and caregivers adapt with difficulty. Indeed, by dividing patients according to disease duration (< or >5 y), no significant differences emerged between groups, testifying that no adaptation to this condition occurred over time.
As far as gender, women showed higher emotional involvement than men in facing difficulties, both as caregivers and patients.
In the Italian culture, women have a primary role in caring for the family, and they are even further loaded in their care giving function when a member is affected by an illness. Often there is a tendency to lose the original relational function with the family member, i.e., a wife caregiver tends to change from a wife to a mother/child kinship, causing her discomfort and anxiety. Differently, a male caregiver generally tends to preserve his role [21,22,23].
Compared with males, female patients give a higher value and significance to their body image and function, which deeply influences their psychological sphere [24].
Our data are in contrast with the survey by Castinel J et al. [25] conducted in a French nutrition referral centre on patients with CIF, treated with HPN, and their caregivers; the authors found that male caregivers experienced a heavier burden than women. We are not able to explain the reasons for these differences in the two studies, but they are probably due to the different importance of the woman’s role in the family, as a consequence of cultural traditions.
Nonetheless, our findings agree with studies in the literature and highlight the importance of identifying and addressing the needs of patients and caregivers.
A retrospective multicentre cohort study by Silva R et al. [26] assessed the burden of CIF in Portuguese patients on parenteral nutrition (PN). Twenty of the thirty-one evaluated patients were paediatric. The author found that patient management was characterized by a substantial therapeutic burden and healthcare resource use, translating into high direct costs and a substantial impairment of the adult physical functions and the child school functions.
The article by Smith CE et al. [27] collected opinions from teens and young adults with CIF requiring long-term HPN on the following issues: illness-related stressors, daily management of HPN, and its effects on their everyday lives. These young patients struggled to live with gastrointestinal symptoms and multiple disease exacerbations requiring hospitalizations. When compared to those with similar medical conditions but without HPN, teen and young adult patients report psychological and social problems. Rather than accepting this lifelong procedure, young patients, desiring alternative restoring solutions, search for answers to their questions on various levels.
Finally, this type of study should be extended to other groups of patients with chronic diseases needing the help of a family caregiver. For example, Kurita GP et al. [28] evaluated three Danish populations of caregivers of patients with different life-threatening pathologies (renal failure, cystic fibrosis, and CIF). All three caregiver groups had a self-perception of poor energy and health, investing many hours into the care role.
The evaluation performed in the present study is part of a future aim consisting of the organization of focused therapeutical support carried out by a psychologist providing the necessary instruments for anxiety management for both patients and caregivers.
In the following ongoing phase, the systemic-relational method will be used, focusing on the preservation of the relational function between patient and family member caregiver, which generally is modified due to the disease [29].
Systemic-relational psychotherapy considers the subject within the family. The family is a unit where each member has a specific role. According to this theory, critical events like a separation, a severe disease, or grief do not represent an individual issue, but one that influences the whole family system. In the presence of a disease, deep psychological and structural transformations happen and may generate not only a crisis to the individual, but a complete unbalance of the whole family.
In addition to the global result, each of the 14 items was evaluated, revealing that caregivers appeared, for some aspects, more psychologically involved. The data obtained from the first three items (anxiety, tension, and fear) led us to hypothesize that patients were inclined to transfer these burdens onto their caregivers. The next three items—insomnia, altered intellectual functions, and depressed mood—were consistently present and equally distributed in both groups. Insomnia might partially derive from the nocturnal infusion of the nutritional mixture; moreover, sleeplessness significantly influences daily attention, concentration, and performance.
Furthermore, the somatic symptom items were more emphasized in patients, going from muscular tension to sensory alterations, more specifically gastrointestinal and genitourinary symptoms. Gastrointestinal disturbances were most probably influenced by intestinal insufficiency, responsible for urgent evacuations, intestinal rumours, and abdominal pain. Genitourinary complaints were influenced by nocturnal HPN, responsible for increased diuresis.
The items regarding cardiovascular and respiratory symptoms showed no differences between patients and caregivers.
6. Study Limitations
This is a monocentric study, with a relatively small number of participants due to the rarity of the disease. For this reason, findings often were not statistically significant and might not be generalizable to other settings, also because the management of this rare disease is non-homogeneous in the different Italian and European centres.
Moreover, we did not use a specific test for CIF patients on HPN [8]. Indeed, HAM-A is a non-selective/specific test, extendible to different study populations, and it was used in the present work as part of a broader investigation that included different types of patients.
As already stated, the comparison of gastrointestinal symptoms between patients and caregivers may be a limitation of the HAM-A questionnaire because patients with CIF frequently have diarrhoea, abdominal pain, etc.; nevertheless, this is one of the fourteen points in the questionnaire.
Finally, a control group (patients with chronic gastrointestinal disease but not on HPN) would have been interesting, but unfortunately, our outpatient unit is specifically for adult patients with CIF on HPN.
In the literature, only a few studies are available on the quality of life of CIF patients on HPN and their family members; additionally, the tools used were multiple and differentiated according to the aims (emotional, social, or economic burden, etc.). Furthermore, most studies are focused on oncological or paediatric patients [30,31,32,33,34].
7. Conclusions
Despite these limitations, this is one of the few studies evaluating the impact of CIF and HPN not only on patients, but particularly on family members providing care, evidencing a significant influence on the quality of life of both and the importance of psychological counselling and care.
We believe that these results may be of inspiration for a multicentre study extendible to other European CIF Centres.
As already mentioned, it would be of extreme help and interest to evaluate the anxiety burden of caregivers, extending this new future evaluation to other fields of chronic and life-threatening illnesses, particularly those involving lengthy procedures.
Author Contributions
R.O.: practical performance; L.A.: practical performance; M.M.: data analysis and interpretation; F.C.: study design and critical review; F.P.: study design and critical review; L.S.: original draft writing, review, and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of A.O.U. Federico II—AORN Cardarelli. (ethical approval date 24 October 2018; prot. n: 317/18).
Informed Consent Statement
Written informed consent was obtained from all the subjects involved in the study to publish this paper.
Data Availability Statement
Data available on request due to privacy and legal/ethical reasons.
Conflicts of Interest
All the authors declare no conflicts of interest.
References
- Sowerbutts, A.M.; Panter, C.; Dickie, G.; Bennett, B.; Ablett, J.; Burden, S.; Lal, S. Short bowel syndrome and the impact on patients and their families: A qualitative study. J. Hum. Nutr. Diet. 2020, 33, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Carroll, R.E.; Benedetti, E.; Schowalter, J.P.; Buchman, A.L. Management and Complications of Short Bowel Syndrome: An Updated Review. Curr. Gastroenterol. Rep. 2016, 18, 40. [Google Scholar] [CrossRef] [PubMed]
- Burden, S.T.; Jones, D.J.; Gittins, M.; Ablett, J.; Taylor, M.; Mountford, C.; Tyrrell-Price, J.; Donnellan, C.; Leslie, F.; Bowling, T.; et al. Needs-based quality of life in adults dependent on home parenteral nutrition. Clin. Nutr. 2019, 38, 1433–1438. [Google Scholar] [CrossRef] [PubMed]
- Wilburn, J.; McKenna, S.P.; Heaney, A.; Rouse, M.; Taylor, M.; Culkin, A.; Gabe, S.; Burden, S.; Lal, S. Development and validation of the Parenteral Nutrition Impact Questionnaire (PNIQ), a patient-centric outcome measure for Home Parenteral Nutrition. Clin. Nutr. 2018, 37, 978–983. [Google Scholar] [CrossRef] [PubMed]
- Jeppesen, P.B.; Shahraz, S.; Hopkins, T.; Worsfold, A.; Genestin, E. Impact of intestinal failure and parenteral support on adult patients with short-bowel syndrome: A multinational, noninterventional, cross-sectional survey. JEPN J. Parenter. Enteral Nutr. 2022, 46, 1650–1659. [Google Scholar] [CrossRef] [PubMed]
- Heaney, A.; McKenna, S.P.; Wilburn, J.; Rouse, M.; Taylor, M.; Burden, S.; Lal, S. The impact of home parenteral nutrition on the lives of adults with type 3 intestinal failure. Clin. Nutr. ESPEN 2018, 24, 35–40. [Google Scholar] [CrossRef]
- Gulledge, A.D.; Gipson, W.T.; Steiger, E.; Hooley, R.; Srp, F. Home parenteral nutrition for the short bowel syndrome. Psychological issues. Gen. Hosp. Psychiatry 1980, 2, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Sowerbutts, A.M.; Jones, D.; Lal, S.; Burden, S. Quality of life in patients and in family members of those receiving home parenteral support with intestinal failure: A systematic review. Clin. Nutr. 2021, 40, 3210–3220. [Google Scholar] [CrossRef]
- Winkler, M.F.; Smith, C.E. Clinical, social, and economic impacts of home parenteral nutrition dependence in short bowel syndrome. J. Parenter. Enter. Nutr. 2014, 38 (Suppl. S1), 32Se7S. [Google Scholar] [CrossRef]
- Kumpf, V.J. Challenges and obstacles of long-term home parenteral nutrition. Nutr. Clin. Pract. 2019, 34, 196–203. [Google Scholar] [CrossRef]
- Messing, B.; Crenn, P.; Beau, P.; Boutron-Ruault, M.C.; Rambaud, J.-C.; Matuchansky, C. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 1999, 117, 1043.e50. [Google Scholar] [CrossRef] [PubMed]
- Baxter, J.P.; Fayers, P.M.; McKinlay, A.W. A review of the quality of life of adult patients treated with long-term parenteral nutrition. Clin. Nutr. 2006, 25, 543–553. [Google Scholar] [CrossRef] [PubMed]
- French, C.; Lal, S.; Jones, D.; Sowerbutts, A.M.; Brundrett, D.; Burch, N.; Calvert, C.; Cooper, S.C.; Donnellan, C.; Forbes, A.; et al. Impact of home parenteral nutrition on family members: A national multi-centre cross-sectional study. Clin. Nutr. 2022, 41, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Jeppesen, P.B.; Chen, K.; Murphy, R.; Shahraz, S.; Goodwin, B. Impact on caregivers of adult patients receiving parenteral support for short-bowel syndrome with intestinal failure: A multinational, cross-sectional survey. J. Parenter. Enter. Nutr. 2022, 46, 905–914. [Google Scholar] [CrossRef] [PubMed]
- Dibb, M.; Soop, M.; Teubner, A.; Shaffer, J.; Abraham, A.; Carlson, G.; Lal, S. Survival and nutritional dependence on home parenteral nutrition: Three decades of experience from a single referral centre. Clin. Nutr. 2017, 36, 570.e6. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Thompson, E. Hamilton Rating Scale for Anxiety (HAM-A). Occup. Med. 2015, 65, 601. [Google Scholar] [CrossRef] [PubMed]
- Donzuso, G.; Cerasa, A.; Gioia, M.C.; Caracciolo, M.; Quattrone, A. The neuroanatomical correlates of anxiety in a healthy population: Differences between the State-Trait Anxiety Inventory and the Hamilton Anxiety Rating Scale. Brain Behav. 2014, 4, 504–514. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A. Relationship between the Beck Anxiety inventory and the Hamilton Anxiety Rating Scale with anxious outpatients. J. Anx. Disord. 1991, 5, 213–223. [Google Scholar] [CrossRef]
- Cummings, J.H.; James, W.P.; Wiggins, H.S. Role of the colon in ileal-resection diarrhoea. Lancet 1973, 1, 344–347. [Google Scholar] [CrossRef]
- Neumann, M.L.; Allen, J.Y.; Ladner, A.; Kakani, S.; Weaver, M.S.; Mercer, D.F. Exploring the impact of pediatric short bowel syndrome on parent well-being using a disease-specific pilot survey. Nutr. Clin. Pract. 2023, 39, 154–167. [Google Scholar] [CrossRef]
- Belza, C.; Avitzur, Y.; Ungar, W.J.; Stremler, R.; Fehlings, D.; Wales, P.W. Stress, anxiety, depression, and health-related quality of life in caregivers of children with intestinal failure receiving parenteral nutrition: A cross-sectional survey study. JEPN J. Parenter. Enteral Nutr. 2023, 47, 342–353. [Google Scholar] [CrossRef] [PubMed]
- van Oers, H.A.; Haverman, L.; Olieman, J.F.; Neelis, E.G.; Jonkers-Schuitema, C.F.; Grootenhuis, M.A.; Tabbers, M.M. Health-related quality of life, anxiety, depression and distress of mothers and fathers of children on Home parenteral nutrition. Clin. Nutr. 2019, 38, 1905–1912. [Google Scholar] [CrossRef] [PubMed]
- Selvi, K.; Parling, T.; Ljótsson, B.; Welch, E.; Ghaderi, A. Two randomized controlled trials of the efficacy of acceptance and commitment therapy-based educational course for body shape dissatisfaction. Scand. J. Psychol. 2021, 62, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Castinel, J.; Pellet, G.; Laharie, D.; Zerbib, F.; Silvain, C.; Wilsius, E.; Kerlogot, L.; Rivière, P.; Poullenot, F. Male gender is associated with informal caregiver burden in patients with chronic intestinal failure treated with home parenteral nutrition. JEPN J. Parenter. Enteral Nutr. 2022, 46, 1593–1601. [Google Scholar] [CrossRef]
- Silva, R.; Guerra, P.; Rocha, A.; Correia, M.; Ferreira, R.; Fonseca, J.; Lima, E.; Oliveira, A.; Gomes, M.V.; Ramos, D.; et al. Clinical, Economic, and Humanistic Impact of Short-Bowel Syndrome/Chronic Intestinal Failure in Portugal (PARENTERAL Study). GE Port. J. Gastroenterol. 2022, 30, 293–304. [Google Scholar] [CrossRef]
- Kurita, G.P.; Eidemak, I.; Larsen, S.; Jeppesen, P.B.; Antonsen, L.B.; Molsted, S.; Liem, Y.S.; Pressler, T.; Sjøgren, P. The impact of caring on caregivers of patients with life-threatening organ failure. Palliat. Support. Care 2023, 1–7. [Google Scholar] [CrossRef]
- Smith, C.E.; Yadrich, D.; Wright, S.; Ridder, L.; Werkowitch, M.; Bruce, A.; Bonar, J.R.M. Themes of Stressors, Emotional Fatigue, and Communication Challenges Found in Mobile Care Discussion Sessions With Patients Requiring Lifelong Home Parenteral Nutrition Infusions. JEPN J. Parenter. Enteral Nutr. 2021, 45, 499–506. [Google Scholar] [CrossRef]
- Marchese, F.; Bonanno, B.; Borinato, D.; Burgio, S.; Mangiapane, D.; Matranga, M.; Saputo, E.; La Barbera, D. Psychosis, symbol, affectivity 2: Another perspective on the treatment of psychotic disorder. J. Anal. Psychol. 2021, 66, 200–220. [Google Scholar] [CrossRef]
- Santarpia, L.; Bozzetti, F. Acute impact of home parenteral nutrition in patients with late-stage cancer on family caregivers: Preliminary data. Support. Care Cancer 2018, 26, 667.e71. [Google Scholar] [CrossRef]
- Osse, B.H.; Vernooij-Dassen, M.J.; Schade, E.; Grol, R.P. Problems experienced by the informal caregivers of cancer patients and their needs for support. Cancer Nurs. 2006, 29, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Beurskens-Meijerink, J.; Huisman-de Waal, G.; Wanten, G. Evaluation of quality of life and caregiver burden in home parenteral nutrition patients: A cross sectional study. Clin. Nutr. ESPEN 2020, 37, 50.e7. [Google Scholar] [CrossRef] [PubMed]
- Sowerbutts, A.M.; Lal, S.; Sremanakova, J.; Clamp, A.R.; Jayson, G.C.; Teubner, A.; Hardy, L.; Todd, C.; Raftery, A.-M.; Sutton, E.; et al. Palliative home parenteral nutrition in patients with ovarian cancer and malignant bowel obstruction: Experiences of women and family caregivers. BMC Palliat. Care 2019, 18, 120. [Google Scholar] [CrossRef] [PubMed]
- Riffin, C.; Wolff, J.L.; Estill, M.; Prabhu, S.; Pillemer, K.A. Caregiver needs assessment in primary care: Views of clinicians, staff, patients, and caregivers. J. Am. Geriatr. Soc. 2020, 68, 1262.e70. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).