The Impact of Stress and Social Determinants on Diet in Cardiovascular Prevention in Young Women
Abstract
1. Introduction
2. Gender Differences in CVD Prevention
2.1. The Long Journey of Atherosclerosis: Gender Differences
2.2. Estrogens Prevent the CVD before Menopause
2.3. Estrogen Is Not a Whole Story: The Impact of Lifestyle and (SDOH)
3. Strategies for CV Primary Prevention in Women
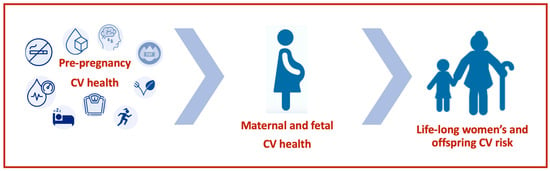
3.1. Pregnancy Stage Is a Good Time to Introduce Primary Prevention in Women
3.2. Peripartum Cardiomyopathy
4. SDOH and Stress in Women
4.1. How Stress Influences Diet and Dietary Behavior in Women
4.2. Stress during Pregnancy and Its Relationship with Food
4.3. Perinatal Depression and Its Relationship with Food
5. Proposed Intervention for Prevention in Young Women: The WEAR-Being Project
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Vogel, B.; Acevedo, M.; Appelman, Y.; Bairey Merz, C.N.; Chieffo, A.; Figtree, G.A.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.H.E.M.; et al. The Lancet women and cardiovascular disease Commission: Reducing the global burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Moscucci, F.; Sciomer, S.; Maffei, S.; Nasi, M.; Pinti, M.; Bucciarelli, V.; Dei Cas, A.; Parati, G.; Ciccone, M.M.; et al. Cardiovascular prevention in women: Un update By the Italian Society of Cardiology Working Group On “Prevention, Hypertension and peripheral disease”. J. Cardiovasc. Med. 2023, 24 (Suppl. S2), e147–e155. [Google Scholar] [CrossRef] [PubMed]
- Nathani, M.; Vogel, B.; Mehran, R. Closing the gap: Cardiovascular disease in women. Climacteric J. Int. Menopause Soc. 2024, 27, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed]
- D’Ascenzi, F.; Sciaccaluga, C.; Cameli, M.; Cecere, A.; Ciccone, M.M.; Di Francesco, S.; Ganau, A.; Imbalzano, E.; Liga, R.; Palermo, P.; et al. When should cardiovascular prevention begin? The importance of antenatal, perinatal and primordial prevention. Eur. J. Prev. Cardiol. 2021, 28, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.M. Atherosclerotic cardiovascular disease beginning in childhood. Korean Circ. J. 2010, 40, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zanini, G.; Selleri, V.; Roncati, L.; Coppi, F.; Nasi, M.; Farinetti, A.; Manenti, A.; Pinti, M.; Mattioli, A.V. Vascular “Long COVID”: A New Vessel Disease? Angiology 2024, 75, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Ross, R. Atherosclerosis—An inflammatory disease. N. Engl. J. Med. 1999, 340, 115–126. [Google Scholar] [CrossRef]
- Nair, A.R.; Pillai, A.J.; Nair, N. Cardiovascular Changes in Menopause. Curr. Cardiol. Rev. 2021, 17, e230421187681. [Google Scholar] [CrossRef]
- Foà, A.; Canton, L.; Bodega, F.; Bergamaschi, L.; Paolisso, P.; De Vita, A.; Villano, A.; Mattioli, A.V.; Tritto, I.; Morrone, D.; et al. Myocardial infarction with nonobstructive coronary arteries: From pathophysiology to therapeutic strategies. J. Cardiovasc. Med. 2023, 24 (Suppl. S2), e134–e146. [Google Scholar] [CrossRef]
- Mosca, L.; Hammond, G.; Mochari-Greenberger, H.; Towfighi, A.; Albert, M.A.; American Heart Association Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Cardiovascular Nursing; Council on High Bloo. Fifteen-year trends in awareness of heart disease in women: Results of a 2012 American Heart Association national survey. Circulation 2013, 127, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- Lerner, D.J.; Kannel, W.B. Patterns of coronary heart disease morbidity and mortality in the sexes: A 26-year follow-up of the Framingham population. Am. Heart J. 1986, 111, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Taddei, S.; Virdis, A.; Ghiadoni, L.; Mattei, P.; Sudano, I.; Bernini, G.; Pinto, S.; Salvetti, A. Menopause is associated with endothelial dysfunction in women. Hypertension 1996, 28, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, S.S.; Neri, S.; Sciacchitano, S.; Pino, L.D.; Costa, M.P.; Marchese, G.; Celotta, G.; Cassibba, N.; Pennisi, G.; Caschetto, S. Behaviour of some indicators of oxidative stress in postmenopausal and fertile women. Maturitas 2006, 53, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Maffei, S.; Meloni, A.; Deidda, M.; Sciomer, S.; Cugusi, L.; Cadeddu, C.; Gallina, S.; Franchini, M.; Scambia, G.; Surico, D.; et al. Cardiovascular Risk Perception and Knowledge among Italian Women: Lessons from IGENDA Protocol. J. Clin. Med. 2022, 11, 1695. [Google Scholar] [CrossRef] [PubMed]
- Vlassoff, C. Gender differences in determinants and consequences of health and illness. J. Health Popul. Nutr. 2007, 25, 47–61. [Google Scholar] [PubMed]
- Woodward, M. Cardiovascular disease and the female disadvantage. Int. J. Environ. Res. Public Health 2019, 16, 1165. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Coppi, F.; Bucciarelli, V.; Gallina, S. Cardiovascular risk stratification in young women: The pivotal role of pregnancy. J. Cardiovasc. Med. 2023, 24, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Humphries, K.H.; Izadnegahdar, M.; Sedlak, T.; Saw, J.; Johnston, N.; Schenck-Gustafsson, K.; Shah, R.U.; Regitz-Zagrosek, V.; Grewal, J.; Vaccarino, V.; et al. Sex differences in cardiovascular disease—Impact on care and outcomes. Front. Neuroendocrinol. 2017, 46, 46–70. [Google Scholar] [CrossRef]
- Khan, S.S.; Brewer, L.C.; Canobbio, M.M.; Cipolla, M.J.; Grobman, W.A.; Lewey, J.; Michos, E.D.; Miller, E.C.; Perak, A.M.; Wei, G.; et al. Optimizing Prepregnancy Cardiovascular Health to Improve Outcomes in Pregnant and Postpartum Individuals and Offspring: A Scientific Statement from the American Heart Association. Circulation 2023, 147, e76–e91. [Google Scholar] [CrossRef]
- Mehta, L.S.; Sharma, G.; Creanga, A.A.; Hameed, A.B.; Hollier, L.M.; Johnson, J.C.; Leffert, L.; McCullough, L.D.; Mujahid, M.S.; Watson, K.; et al. Call to action: Maternal health and saving mothers: A policy statement from the American Heart Association. Circulation 2021, 144, e251–e269. [Google Scholar] [CrossRef]
- Lunova, T.; Komorovsky, R.; Klishch, I. Gender differences in treatment delays, management and mortality among patients with acute coronary syndrome: A systematic review and meta-analysis. Curr. Cardiol. Rev. 2023, 19, e300622206530. [Google Scholar] [CrossRef]
- Agarwala, A.; Patel, J.; Stephens, J.; Roberson, S.; Scott, J.; Beckie, T.; Jackson, E.A.; American Heart Association Prevention Science Committee of the Council on Epidemiology and Prevention and Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Lifestyle and Cardiometabolic Health. Implementation of Prevention Science to Eliminate Health Care Inequities in Achieving Cardiovascular Health: A Scientific Statement from the American Heart Association. Circulation 2023, 148, 1183–1193. [Google Scholar] [CrossRef]
- Wilkins, E.; Wickramasinghe, K.; Pullar, J.; Demaio, A.R.; Roberts, N.; Perez-Blanco, K.M.; Noonan, K.; Townsend, N. Maternal nutrition and its intergenerational links to non-communicable disease metabolic risk factors: A systematic review and narrative synthesis. J. Health Popul. Nutr. 2021, 40, 20. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Coppi, F.; Nasi, M.; Gallina, S. Stress and cardiovascular risk burden after the pandemic: Current status and future prospects. Expert Rev. Cardiovasc. Ther. 2022, 20, 507–513. [Google Scholar] [CrossRef]
- Shibeshi, K.; Lemu, Y.; Gebretsadik, L.; Gebretsadik, A.; Morankar, S. Understanding Gender-Based Perception during Pregnancy: A Qualitative Study. Int. J. Women’s Health 2023, 15, 1523–1535. [Google Scholar] [CrossRef] [PubMed]
- Naaz, A.; Muneshwar, K.N. How Maternal Nutritional and Mental Health Affects Child Health During Pregnancy: A Narrative Review. Cureus 2023, 15, e48763. [Google Scholar] [CrossRef] [PubMed]
- Safira, A.; Tjahjadi, A.K.; Adytia, G.J.; Waitupu, A.; Sutanto, H. Peripartum cardiomyopathy unveiled: Etiology, diagnosis, and therapeutic insights. Curr. Probl. Cardiol. 2024, 49, 102474. [Google Scholar] [CrossRef]
- Arany, Z.; Elkayam, U. Peripartum cardiomyopathy. Circulation 2016, 133, 1397–1409. [Google Scholar] [CrossRef]
- Tak, B.T.; Cay, S.; Pamukcu, H.E.; Ekizler, F.A.; Kafes, H.; Cetin, E.H.O.; Ulvan, N.; Ozeke, O.; Ozcan, F.; Topaloglu, S.; et al. Prognostic nutritional index as a novel marker for prediction of prognosis in patients with peripartum cardiomyopathy. Medicine 2020, 99, e19524. [Google Scholar] [CrossRef]
- Sliwa, K.; Skudicky, D.; Bergemann, A.; Candy, G.; Puren, A.; Sareli, P. Peripartum cardiomyopathy: Analysis of clinical outcome, left ventricular function, plasma levels of cytokines and Fas/APO-1. J. Am. Coll. Cardiol. 2000, 35, 701–705. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Tarabini Castellani, E.; Vivoli, D.; Molinari, R.; Mattioli, G. Restoration of atrial function after atrial fibrillation of different etiological origins. Cardiology 1996, 87, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Adamson, D.L.; Nelson-Piercy, C. Managing palpitations and arrhythmias during pregnancy. Heart 2007, 93, 1630–1636. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed on 22 March 2024).
- Koenig, H.G. Physical health consequences of psychological conditions. Int. J. Psychiatry Med. 2024, 59, 135–138. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Wei, F.; Li, G. The evolution of the concept of stress and the framework of the stress system. Cell Stress 2021, 5, 76–85. [Google Scholar] [CrossRef]
- Cameli, M.; Lembo, M.; Sciaccaluga, C.; for the Working Groups of Echocardiography and Arterial Hypertension of Italian Society of Cardiology (SIC). Identification of cardiac organ damage in arterial hypertension: Insights by echocardiography for a comprehensive assessment. J. Hypertens. 2020, 38, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, N.; Bordbar, A.; Bavarsad, S.S.; Ghasemi, P.; Bakhshi, M.; Rezaeeyan, H. Molecular Insights into the Relationship Between Platelet Activation and Endothelial Dysfunction: Molecular Approaches and Clinical Practice. Mol. Biotechnol. 2024. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Koh, E.; Kang, Y. Susceptibility of Women to Cardiovascular Disease and the Prevention Potential of Mind-Body Intervention by Changes in Neural Circuits and Cardiovascular Physiology. Biomolecules 2021, 11, 708. [Google Scholar] [CrossRef]
- Gianaros, P.J.; Hariri, A.R.; Sheu, L.K.; Muldoon, M.F.; Sutton-Tyrrell, K.; Manuck, S.B. Preclinical atherosclerosis covaries with individual differences in reactivity and functional connectivity of the amygdala. Biol. Psychiatry 2009, 65, 943–950. [Google Scholar] [CrossRef]
- Coppi, F.; Farinetti, A.; Stefanelli, C.; Mattioli, A.V. Changes in food during the COVID-19 pandemic: The different roles of stress and depression in women and men. Nutrition 2023, 108, 111981. [Google Scholar] [CrossRef]
- Ha, O.R.; Lim, S.L. The role of emotion in eating behavior and decisions. Front. Psychol. 2023, 14, 1265074. [Google Scholar] [CrossRef] [PubMed]
- Legget, K.T.; Cornier, M.-A.; Sarabia, L.; Delao, E.M.; Mikulich-Gilbertson, S.K.; Natvig, C.; Erpelding, C.; Mitchell, T.; Hild, A.; Kronberg, E.; et al. Sex Differences in Effects of Mood, Eating-Related Behaviors, and BMI on Food Appeal and Desire to Eat: A Cross-Sectional Survey Study. Nutrients 2023, 15, 762. [Google Scholar] [CrossRef] [PubMed]
- Borer, K.T. Why We Eat Too Much, Have an Easier Time Gaining Than Losing Weight, and Expend Too Little Energy: Suggestions for Counteracting or Mitigating These Problems. Nutrients 2021, 13, 3812. [Google Scholar] [CrossRef] [PubMed]
- Li, D.L.; Hodge, A.M.; Cribb, L.; Southey, M.C.; Giles, G.G.; Milne, R.L.; Dugué, P.A. Body size, diet quality, and epigenetic ageing: Cross-sectional and longitudinal analyses. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2024, 24, glae026. [Google Scholar] [CrossRef]
- Gilmartin, T.; Dipnall, J.F.; Gurvich, C.; Sharp, G. Identifying overcontrol and undercontrol personality types among young people using the five factor model, and the relationship with disordered eating behaviour, anxiety and depression. J. Eat. Disord. 2024, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Martín, B.C.; Meule, A. Food craving: New contributions on its assessment, moderators, and consequences. Front. Psychol. 2015, 6, 21. [Google Scholar] [CrossRef]
- Langley, E.B.; O’Leary, D.J.; Gross, J.J.; Shiota, M.N. Breaking the Link between Negative Emotion and Unhealthy Eating: The Role of Emotion Regulation. Affect. Sci. 2023, 4, 702–710. [Google Scholar] [CrossRef]
- You, Z.; Shan, L.; Cheng, S.; Xia, Y.; Zhao, Y.; Zhang, H.; Zhao, Z. Dietary intake patterns during pregnancy and excessive gestational weight gain: A systematic review and meta-analysis. Food Funct. 2023, 14, 5910–5920. [Google Scholar] [CrossRef] [PubMed]
- Çelik, G.; Yılmaz, E.; Nazik, F.; Unver, H. Determination of distress, emotional eating and internalized weight bias levels of Turkish pregnant women. J. Obstet. Gynaecol. J. Inst. Obstet. Gynaecol. 2023, 43, 2153020. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Gallina, S. Early cardiovascular prevention: The crucial role of nurse-led intervention. BMC Nurs. 2023, 22, 347. [Google Scholar] [CrossRef]
- Jackson, H.; Stickler, E.; Biddle, S.; Trilk, J.L. Do Pregnant Women Perceive Being Counseled about Nutrition by Healthcare Providers? A Cross-Sectional Study of the Recall and Satisfaction of Nutrition Counseling of Patients throughout the Course of Their Pregnancy. Am. J. Lifestyle Med. 2023. [Google Scholar] [CrossRef]
- World Health Organization. Sustainable Healthy Diets: Guiding Principles. 2019. Available online: https://www.who.int/publications/i/item/9789241516648 (accessed on 23 July 2022).
- Truzzi, M.L.; Ballerini Puviani, M.; Tripodi, A.; Toni, S.; Farinetti, A.; Nasi, M.; Mattioli, A.V. Mediterranean Diet as a model of sustainable, resilient and healthy diet. Prog. Nutr. 2020, 22, 388–394. [Google Scholar]
- Mattioli, A.V.; Coppi, F.; Migaldi, M.; Farinetti, A. Fruit and vegetables in hypertensive women with asymptomatic peripheral arterial disease. Clin. Nutr. ESPEN 2018, 27, 110–112. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.; Kaur, M.; Rasane, P.; Kaur, S.; Kaur, J.; Sharma, K.; Gulati, A. Nutritional management and interventions in complications of pregnancy: A systematic review. Nutr. Health, 2023; published online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Migaldi, M.; Farinetti, A. Coffee in hypertensive women with asymptomatic peripheral arterial disease: A potential nutraceutical effect. J. Cardiovasc. Med. 2018, 19, 183–185. [Google Scholar] [CrossRef] [PubMed]
- Food Standards Australian and New Zealand. Available online: https://www.foodstandards.gov.au/consumer/generalissues/pages/caffeine.aspx#:~:text=It%20sets%20maximum%20permitted%20levels,is%20320%20mg%20per%20litre (accessed on 12 January 2024).
- Coppi, F.; Bucciarelli, V.; Sinigaglia, G.; Zanini, G.; Selleri, V.; Nasi, M.; Pinti, M.; Gallina, S.; Mattioli, A.V. Sex Related Differences in the Complex Relationship between Coffee, Caffeine and Atrial Fibrillation. Nutrients 2023, 15, 3299. [Google Scholar] [CrossRef]
- ESFA Journal “Scientific Opinion on the Safety of Caffeine”. 2015. Available online: https://www.efsa.europa.eu/en/efsajournal/pub/4102 (accessed on 12 January 2024).
- Klevebrant, L.; Frick, A. Effects of caffeine on anxiety and panic attacks in patients with panic disorder: A systematic review and meta-analysis. Gen. Hosp. Psychiatry 2022, 74, 22–31. [Google Scholar] [CrossRef]
- Emokpae, M.A.; Brown, S.I. Effects of lifestyle factors on fertility: Practical recommendations for modification. Reprod. Fertil. 2021, 2, R13–R26. [Google Scholar] [CrossRef]
- Caro, R.; Fast, J. Pregnancy Myths and Practical Tips. Am. Fam. Physician 2020, 102, 420–426. [Google Scholar]
- Wikoff, D.; Welsh, B.T.; Henderson, R.; Brorby, G.P.; Britt, J.; Myers, E.; Goldberger, J.; Lieberman, H.R.; O’Brien, C.; Peck, J.; et al. Systematic review of the potential adverse effects of caffeine consumption in healthy adults, pregnant women, adolescents, and children. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2017, 109 Pt 1, 585–648. [Google Scholar] [CrossRef]
- Grosso, G.; Godos, J.; Galvano, F.; Giovannucci, E.L. Coffee, Caffeine, and Health Outcomes: An Umbrella Review. Annu. Rev. Nutr. 2017, 37, 131–156. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Pluchinotta, F.R.; Marventano, S.; Buscemi, S.; Li Volti, G.; Galvano, F.; Grosso, G. Coffee components and cardiovascular risk: Beneficial and detrimental effects. Int. J. Food Sci. Nutr. 2014, 65, 925–936. [Google Scholar] [CrossRef] [PubMed]
- Pan, M.H.; Tung, Y.C.; Yang, G.; Li, S.; Ho, C.T. Molecular mechanisms of the anti-obesity effect of bioactive compounds in tea and coffee. Food Funct. 2016, 7, 4481–4491. [Google Scholar] [CrossRef] [PubMed]
- Hillier, S.E.; Olander, E.K. Women’s dietary changes before and during pregnancy: A systematic review. Midwifery 2017, 49, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.L.; Bernard, C.; Lipshultz, S.E.; Czachor, J.D.; Westphal, J.A.; Mestre, M.A. The Safety of Ingested Caffeine: A Comprehensive Review. Front. Psychiatry 2017, 8, 80. [Google Scholar] [CrossRef] [PubMed]
- Mattioli, A.V.; Sabatini, S. Changes in energy drink consumption during the COVID-19 quarantine. Clin. Nutr. ESPEN 2021, 45, 516–517. [Google Scholar] [CrossRef] [PubMed]
- Craig, W.J.; Mangels, A.R.; Fresán, U.; Marsh, K.; Miles, F.L.; Saunders, A.V.; Haddad, E.H.; Heskey, C.E.; Johnston, P.; Larson-Meyer, E.; et al. The Safe and Effective Use of Plant-Based Diets with Guidelines for Health Professionals. Nutrients 2021, 13, 4144. [Google Scholar] [CrossRef] [PubMed]
- Ratjen, I.; Morze, J.; Enderle, J.; Both, M.; Borggrefe, J.; Muller, H.P.; Kassubek, J.; Koch, M.; Lieb, W. Adherence to a plant-based diet in relation to adipose tissue volumes and liver fat content. Am. J. Clin. Nutr. 2020, 112, 354–363. [Google Scholar] [CrossRef] [PubMed]
- Mayra, S.; Ugarte, N.; Johnston, C.S. Health Biomarkers in Adults Are More Closely Linked to Diet Quality Attributes than to Plant-Based Diet Categorization. Nutrients 2019, 11, 1427. [Google Scholar] [CrossRef]
- Wang, T.; Kroeger, C.M.; Cassidy, S.; Mitra, S.; Ribeiro, R.V.; Jose, S.; Masedunskas, A.; Senior, A.M.; Fontana, L. Vegetarian Dietary Patterns and Cardiometabolic Risk in People With or at High Risk of Cardiovascular Disease: A Systematic Review and Meta-analysis. JAMA Netw. Open 2023, 6, e2325658. [Google Scholar] [CrossRef]
- Lakin, V.; Haggarty, P.; Abramovich, D.R.; Ashton, J.; Moffat, C.F.; McNeill, G.; Danielian, P.J.; Grubb, D. Dietary intake and tissue concentration of fatty acids in omnivore, vegetarian and diabetic pregnancy. Prostaglandins Leukot. Essent. Fat. Acids 1998, 59, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Leung, B.M.; Kaplan, B.J. Perinatal depression: Prevalence, risks, and the nutrition link–a review of the literature. J. Am. Diet Assoc. 2009, 109, 1566–1575. [Google Scholar] [CrossRef] [PubMed]
- Christian, C.; Zerwas, S.C.; Levinson, C.A. The Unique and Moderating Role of Social and Self-Evaluative Factors on Perinatal Eating Disorder and Depression Symptoms. Behav. Ther. 2024, 55, 122–135. [Google Scholar] [CrossRef] [PubMed]
- Albert, P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015, 40, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Cattane, N.; Räikkönen, K.; Anniverno, R.; Mencacci, C.; Riva, M.A.; Pariante, C.M.; Cattaneo, A. Depression, obesity and their comorbidity during pregnancy: Effects on the offspring’s mental and physical health. Mol. Psychiatry 2021, 26, 462–481. [Google Scholar] [CrossRef] [PubMed]
- US Preventive Services Task Force; Curry, S.J.; Krist, A.H.; Owens, D.K.; Barry, M.J.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Grossman, D.C.; et al. Interventions to Prevent Perinatal Depression: US Preventive Services Task Force Recommendation Statement. JAMA 2019, 321, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry 2017, 4, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Bear, T.L.K.; Dalziel, J.E.; Coad, J.; Roy, N.C.; Butts, C.A.; Gopal, P.K. The role of the gut microbiota in dietary interventions for depression and anxiety. Adv. Nutr. 2020, 11, 890–907. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, S.; Zhang, X.; Xu, Y.; Cheng, J.; Yang, X. The role of diet, eating behavior, and nutrition intervention in seasonal affective disorder: A systematic review. Front. Psychol. 2020, 11, 1451. [Google Scholar] [CrossRef]
- Ross, F.C.; Mayer, D.E.; Gupta, A.; Gill, C.I.R.; Del Rio, D.; Cryan, J.F.; Lavelle, A.; Ross, R.P.; Stanton, C.; Mayer, E.A. Existing and Future Strategies to Manipulate the Gut Microbiota with Diet as a Potential Adjuvant Treatment for Psychiatric Disorders. Biol. Psychiatry 2024, 95, 348–360. [Google Scholar] [CrossRef]
- Zidan, S.; Hilary, S.; Al Dhaheri, A.S.; Cheikh Ismail, L.; Ali, H.I.; Apostolopoulos, V.; Stojanovska, L. Could psychobiotics and fermented foods improve mood in middle-aged and older women? Maturitas 2024, 181, 107903. [Google Scholar] [CrossRef]
- Dinu, M.; Lotti, S.; Mattioli, A.V.; Gensini, G.F.; Ambrosio, G.; Sofi, F. Effects of Omega-3 Fatty Acid Supplementation on Revascularization and Major Cardiovascular Events: A Systematic Review and Meta-Analysis. Proceedings 2023, 91, 199. [Google Scholar] [CrossRef]
- Li, D.; Wang, K.; Yang, Z.; Li, H.; Wang, S. Vitamin d supplementation in mice with advanced maternal age and cognitive function of the offspring. Am. J. Trans. Res. 2021, 13, 7641–7653. [Google Scholar]
- Liang, Q.; Cai, C.; Duan, D.; Hu, X.; Hua, W.; Jiang, P.; Zhang, L.; Xu, J.; Gao, Z. Postnatal vitamin d intake modulates hippocampal learning and memory in adult mice. Front. Neurosci. 2018, 12, 322097. [Google Scholar] [CrossRef]
- de Abreu, D.F.; Eyles, D.; Feron, F. Vitamin D, a neuro-immunomodulator: Implications for neurodegenerative and autoimmune diseases. Psychoneuroendocrinology 2009, 34, S265–S277. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Zhou, B.; Kan, J.; Liu, G.; Zhang, S.; Si, L.; Zhang, X.; Yang, X.; Ma, J.; Cheng, J.; et al. Gut microbiota: Linking nutrition and perinatal depression. Front. Cell. Infect. Microbiol. 2022, 12, 932309. [Google Scholar] [CrossRef]
- Wang, J.; Liu, N.; Sun, W.; Chen, D.; Zhao, J.; Zhang, W. Association between vitamin d deficiency and antepartum and postpartum depression: A systematic review and meta-analysis of longitudinal studies. Arch. Gynecol Obstet. 2018, 298, 1045–1059. [Google Scholar] [CrossRef]
- Vaziri, F.; Nasiri, S.; Tavana, Z.; Dabbaghmanesh, M.H.; Sharif, F.; Jafari, P. A randomized controlled trial of vitamin D supplementation on perinatal depression: In Iranian pregnant mothers. BMC Pregnancy Childbirth 2016, 16, 239. [Google Scholar] [CrossRef] [PubMed]
- Kabuyanga, R.K.; Tugirimana, P.L.; Sifa, B.; Balezi, M.; Dikete, M.E.; Mitangala, P.N.; Elongi, J.P.M.; Kinenkinda, X.K.; Kakoma, J.S.Z. Effect of early vitamin D supplementation on the incidence of preeclampsia in primigravid women: A randomised clinical trial in Eastern Democratic Republic of the Congo. BMC Pregnancy Childbirth 2024, 24, 107. [Google Scholar] [CrossRef]
- Ferenc, K.; Sokal-Dembowska, A.; Helma, K.; Motyka, E.; Jarmakiewicz-Czaja, S.; Filip, R. Modulation of the Gut Microbiota by Nutrition and Its Relationship to Epigenetics. Int. J. Mol. Sci. 2024, 25, 1228. [Google Scholar] [CrossRef]
- Theofilis, P.; Vlachakis, P.K.; Oikonomou, E.; Tsioufis, K.; Tousoulis, D. Targeting the Gut Microbiome to Treat Cardiometabolic Disease. Curr. Atheroscler. Rep. 2024. [Google Scholar] [CrossRef] [PubMed]
- Aziz, T.; Hussain, N.; Hameed, Z.; Lin, L. Elucidating the role of diet in maintaining gut health to reduce the risk of obesity, cardiovascular and other age-related inflammatory diseases: Recent challenges and future recommendations. Gut Microbes 2024, 16, 2297864. [Google Scholar] [CrossRef] [PubMed]
- Bucciarelli, V.; Mattioli, A.V.; Sciomer, S.; Moscucci, F.; Renda, G.; Gallina, S. The Impact of Physical Activity and Inactivity on Cardiovascular Risk across Women’s Lifespan: An Updated Review. J. Clin. Med. 2023, 12, 4347. [Google Scholar] [CrossRef] [PubMed]
- Academy of Nutrition and Dietetics. Available online: https://www.eatright.org/health/pregnancy/prenatal-nutrition/healthy-weight-during-pregnancy (accessed on 29 January 2024).
- Mattioli, A.V.; Selleri, V.; Zanini, G.; Nasi, M.; Pinti, M.; Stefanelli, C.; Fedele, F.; Gallina, S. Physical Activity and Diet in Older Women: A Narrative Review. J. Clin. Med. 2022, 12, 81. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.A.J.M.; Hutchinson, J.; Cade, J.E.; Poston, L.; Barrett, G.; Crozier, S.R.; Barker, M.; et al. Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.F.; Li, R.N.; Deng, J.L.; Chen, X.L.; Zhou, Q.L.; Qi, Y.; Zhang, Y.P.; Fan, J.M. Effects of mindfulness-based interventions on cardiovascular risk factors: An umbrella review of systematic reviews and meta-analyses. J. Psychosom. Res. 2024, 177, 111586. [Google Scholar] [CrossRef]
- Tyler, J.; Won Choi, S.; Tewari, M. Real-time, personalized medicine through wearable sensors and dynamic predictive modeling: A new paradigm for clinical medicine. Curr. Opin. Syst. Biol. 2020, 20, 17–25. [Google Scholar] [CrossRef]
- Meghan Rimol, Gartner Forecasts Global Spending on Wearable Devices to Total $81.5 Billion in 2021, STAMFORD, Conn. 12 January 2021. Available online: https://www.gartner.com/en/newsroom/press-releases/2021-01-11-gartner-forecasts-global-spending-on-wearable-devices-to-total-81-5-billion-in-2021 (accessed on 15 November 2023).
- Latest Trends in Medical Monitoring Devices and Wearable Health Technology. Available online: https://www.businessinsider.in/latest-trends-in-medical-monitoring-devices-and-wearable-health-technology/articleshow/70907962.cms (accessed on 15 November 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coppi, F.; Bucciarelli, V.; Solodka, K.; Selleri, V.; Zanini, G.; Pinti, M.; Nasi, M.; Salvioli, B.; Nodari, S.; Gallina, S.; et al. The Impact of Stress and Social Determinants on Diet in Cardiovascular Prevention in Young Women. Nutrients 2024, 16, 1044. https://doi.org/10.3390/nu16071044
Coppi F, Bucciarelli V, Solodka K, Selleri V, Zanini G, Pinti M, Nasi M, Salvioli B, Nodari S, Gallina S, et al. The Impact of Stress and Social Determinants on Diet in Cardiovascular Prevention in Young Women. Nutrients. 2024; 16(7):1044. https://doi.org/10.3390/nu16071044
Chicago/Turabian StyleCoppi, Francesca, Valentina Bucciarelli, Kateryna Solodka, Valentina Selleri, Giada Zanini, Marcello Pinti, Milena Nasi, Beatrice Salvioli, Savina Nodari, Sabina Gallina, and et al. 2024. "The Impact of Stress and Social Determinants on Diet in Cardiovascular Prevention in Young Women" Nutrients 16, no. 7: 1044. https://doi.org/10.3390/nu16071044
APA StyleCoppi, F., Bucciarelli, V., Solodka, K., Selleri, V., Zanini, G., Pinti, M., Nasi, M., Salvioli, B., Nodari, S., Gallina, S., & Mattioli, A. V. (2024). The Impact of Stress and Social Determinants on Diet in Cardiovascular Prevention in Young Women. Nutrients, 16(7), 1044. https://doi.org/10.3390/nu16071044