Ginseng Berry Juice (GBJ) Regulates the Inflammation in Acute Ulcerative Mouse Models and the Major Bioactive Substances Are Ginsenosides Rb3, Rc, Rd, and Re
Abstract
1. Introduction
2. Materials and Methods
2.1. Plant Materials and Analytic Conditions
2.2. Analysis of Biomarkers
2.3. HCl/Ethanol-Induced Acute Gastric Injury Model
2.4. Macroscopic and Microscopic Analysis
2.5. Immunofluorescent and Immunohistochemical Analyses
2.6. Ethics Statement
2.7. Statistical Analysis
3. Results
3.1. GBJ Prevented the HCl/Ethanol-Induced Morphological Changes
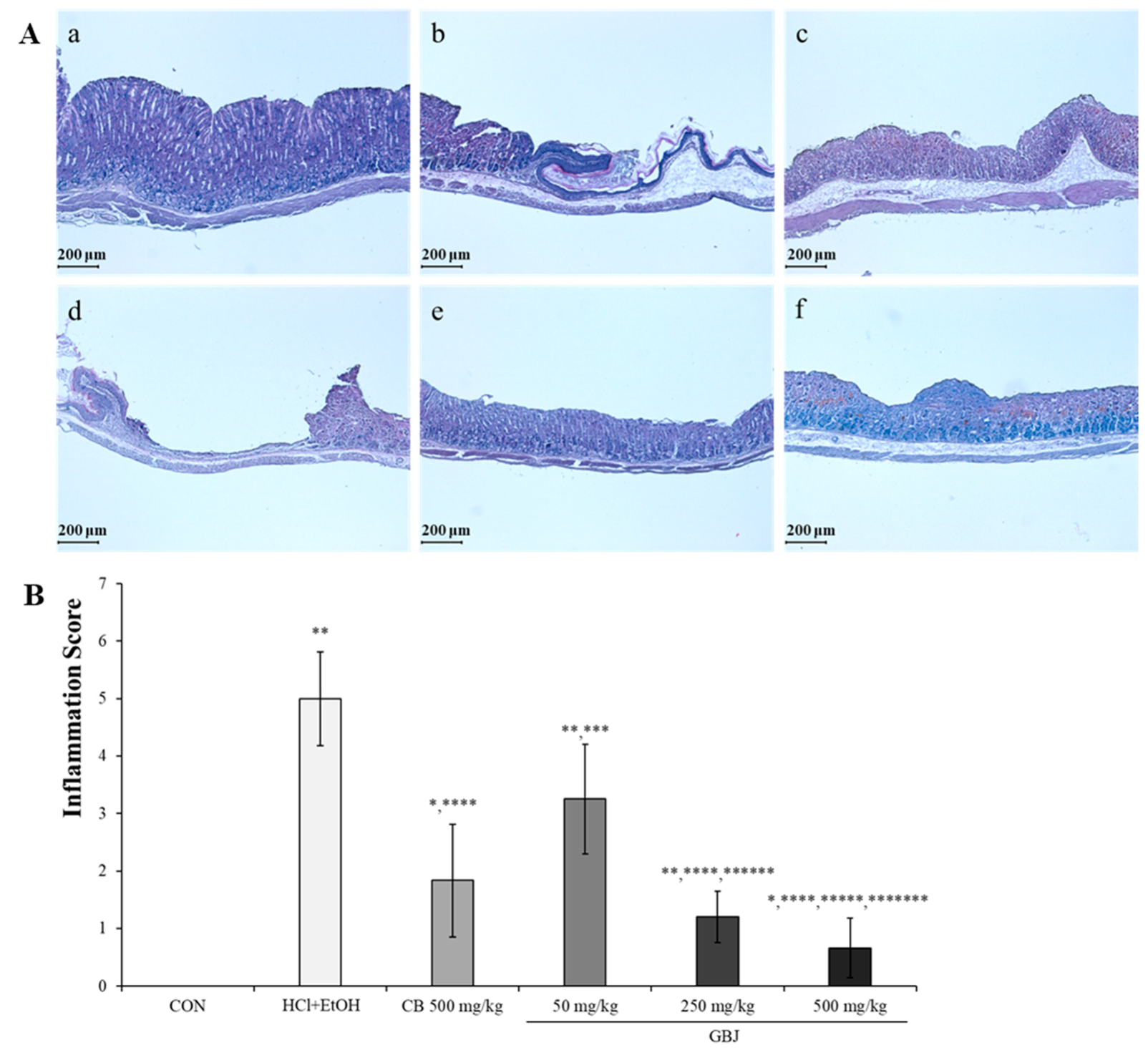
3.2. BGJ Prevented the HCl/Ethanol-Induced Histopathological Changes
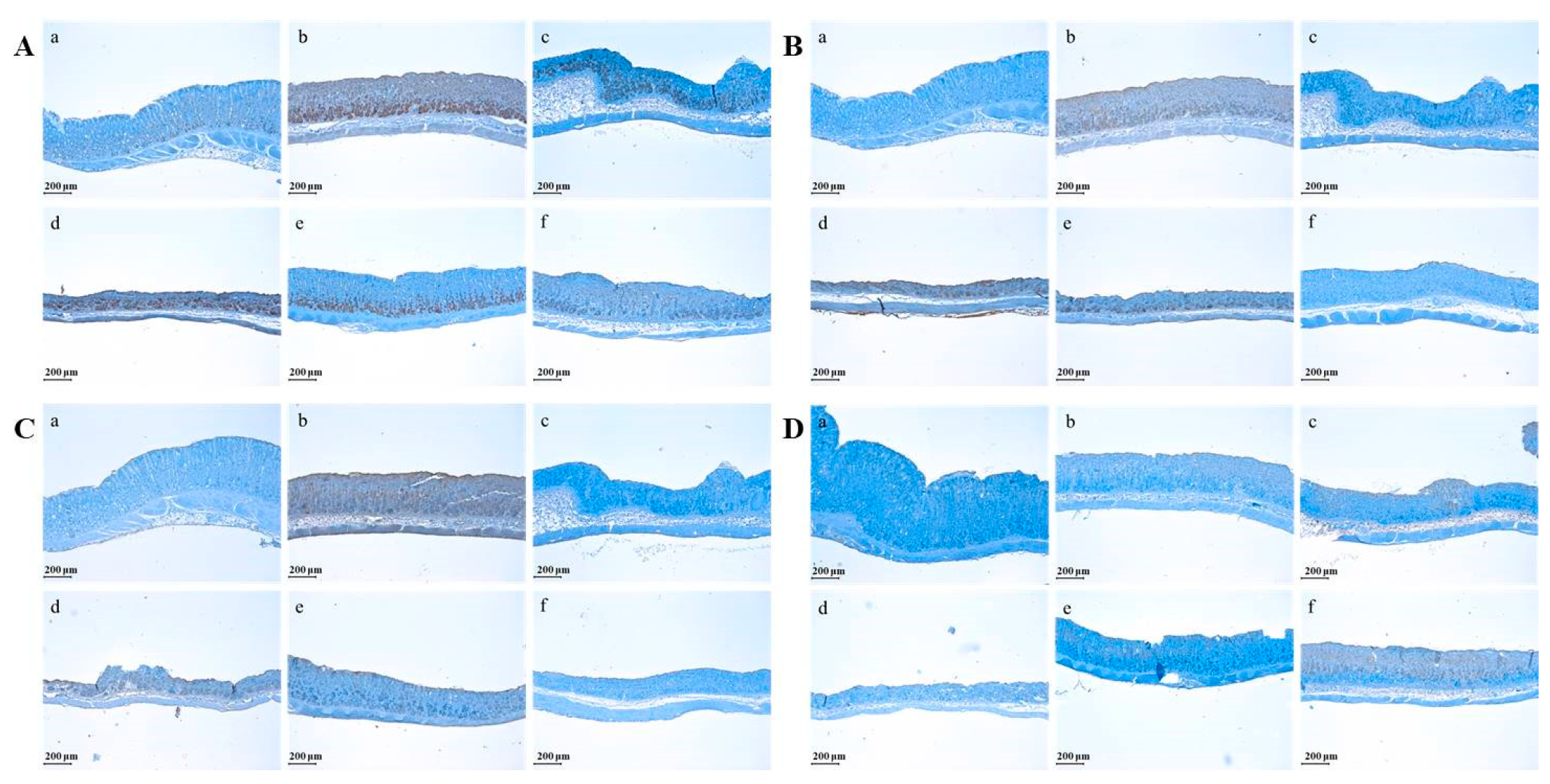
3.3. GBJ Suppressed the Expression of Pro-Inflammatory Cytokines Such as TNF-α, IL-6, and IL-13 but Increased the Expression of Anti-Inflammatory Cytokines Such as IL-10
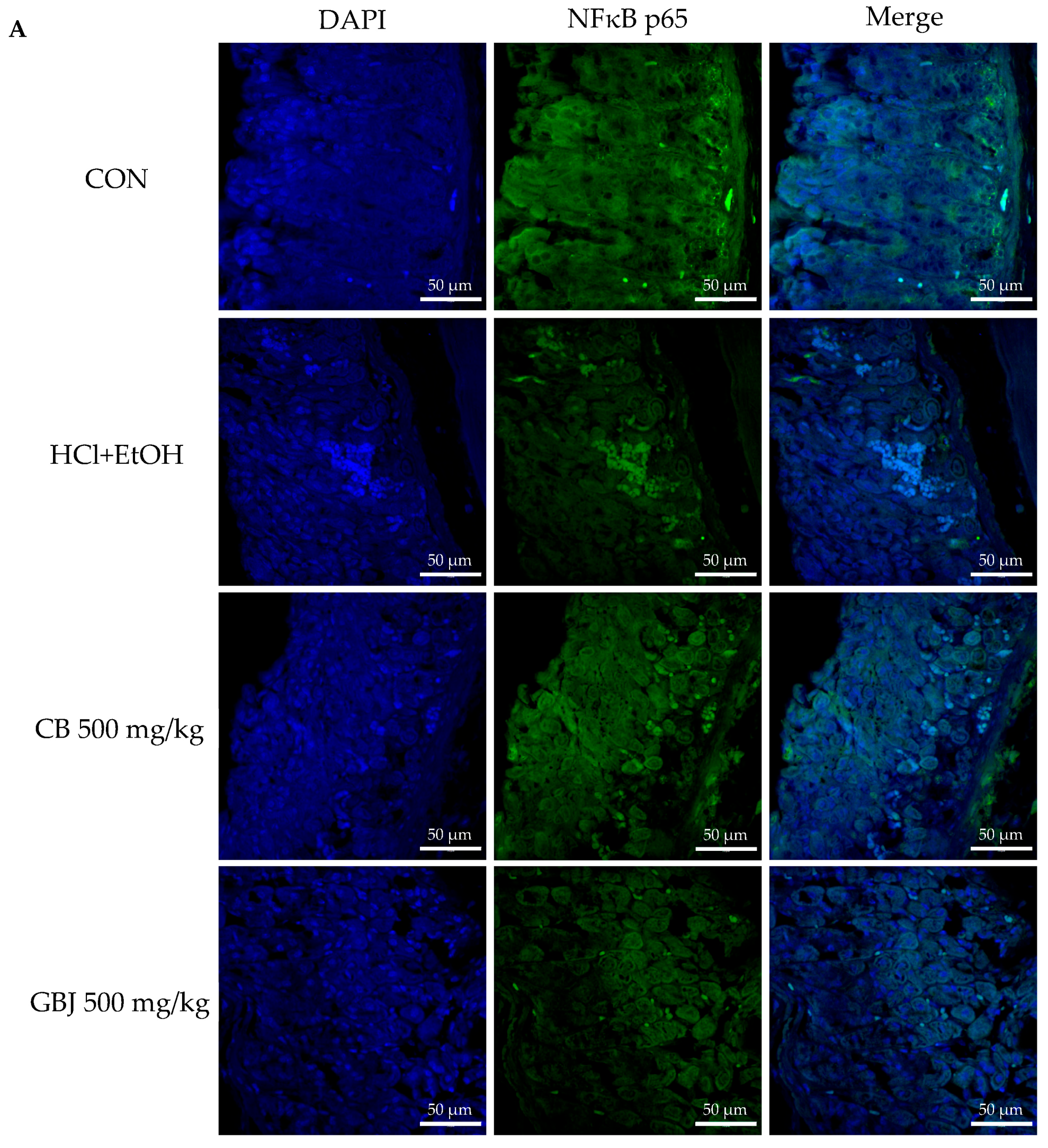
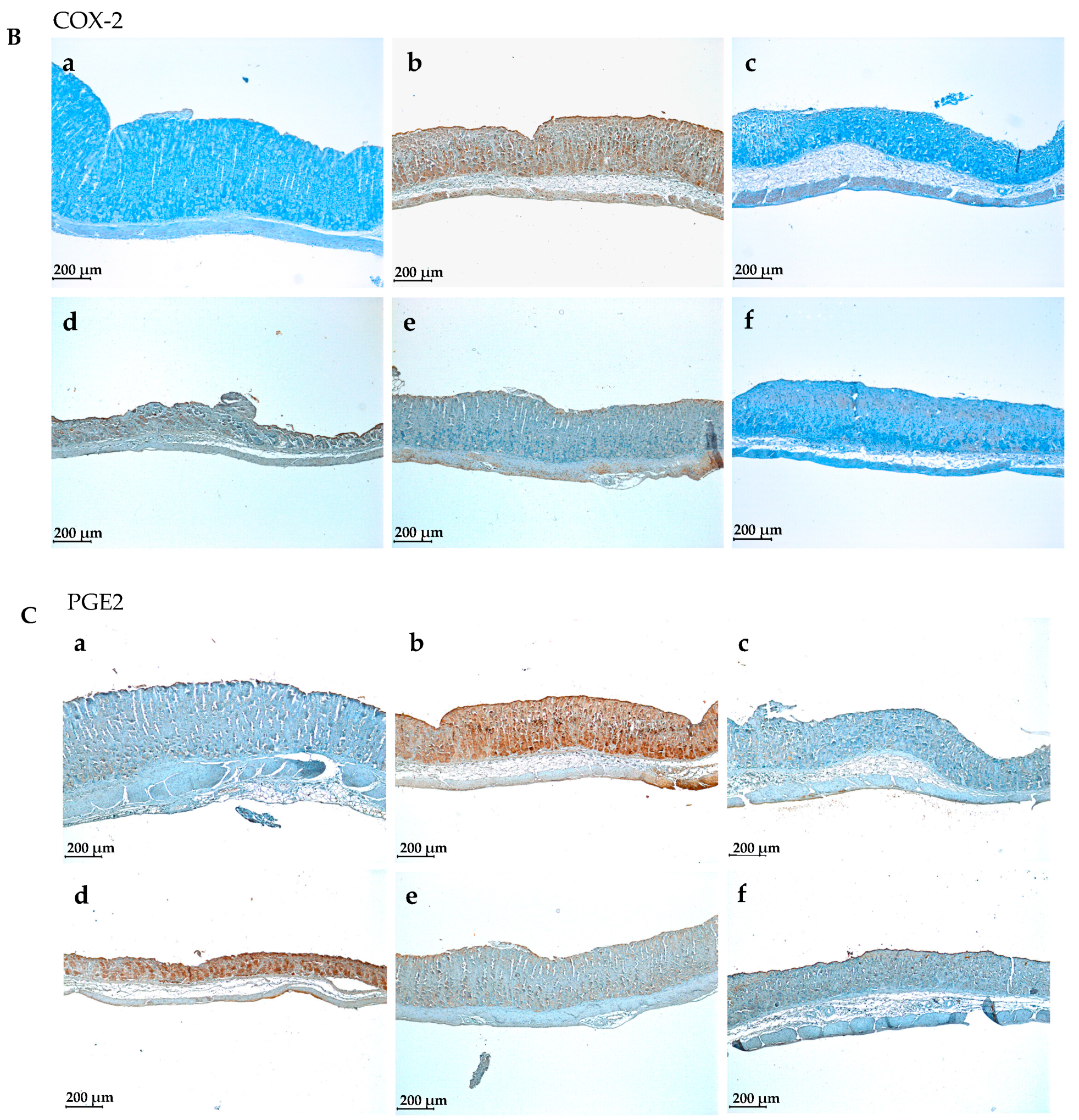
3.4. GBJ Controls the Translocation of NF-κBp65 from the Cytoplasm to the Nucleus to Prevent Inflammation and Then Suppresses the Production of Cyclooxygenase 2 (COX-2) and Prostaglandin E2
3.5. Preparation and Quantitative Analysis of Anti-Ulcerative Biomarkers in GBJ
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dey, L.; Zhang, L.; Yuan, C.S. Anti-diabetic and anti-obese effects of ginseng berry extract: Comparison between intraperitoneal and oral administrations. Am. J. Chin. Med. 2002, 30, 645–647. [Google Scholar] [CrossRef] [PubMed]
- Attele, A.S.; Zhou, Y.P.; Xie, J.T.; Wu, J.A.; Zhang, L.; Dey, L.; Pugh, W.; Rue, P.A.; Polonsky, K.S.; Yuan, C.S. Antidiabetic effects of Panax ginseng berry extract and the identification of an effective component. Diabetes 2002, 51, 1851–1858. [Google Scholar] [CrossRef] [PubMed]
- Byun, J.; Kim, S.K.; Ban, J.Y. Anti-Inflammatory and Anti-Oxidant Effects of Korean Ginseng Berry Extract in LPS-Activated RAW264.7 Macrophages. Am. J. Chin. Med. 2021, 49, 719–735. [Google Scholar] [CrossRef]
- Xu, H.; Liu, M.; Chen, G.; Wu, Y.; Xie, L.; Han, X.; Zhang, G.; Tan, Z.; Ding, W.; Fan, H.; et al. Anti-Inflammatory Effects of Ginsenoside Rb3 in LPS-Induced Macrophages Through Direct Inhibition of TLR4 Signaling Pathway. Front. Pharmacol. 2022, 13, 714554. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Jung, S.Y.; Choi, S.M.; Yang, E.J. Effects of ginsenoside Re on LPS-induced inflammatory mediators in BV2 microglial cells. BMC Complement. Altern. Med. 2012, 12, 196. [Google Scholar] [CrossRef] [PubMed]
- Nam, Y.; Ko, S.K.; Sohn, U.D. Hepatoprotective effect of ultrasonicated ginseng berry extract on a rat mild bile duct ligation model. J. Ginseng Res. 2019, 43, 606–617. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.Y.; Yi, E.S.; Kang, C.H.; Liu, Y.; Lee, Y.G.; Choi, H.S.; Jang, H.B.; Huo, Y.; Baek, N.I.; Yang, D.C.; et al. Whitening and inhibiting NF-κB-mediated inflammation properties of the biotransformed green ginseng berry of new cultivar K1, ginsenoside Rg2 enriched, on B16 and LPS-stimulated RAW 264.7 cells. J. Ginseng Res. 2021, 45, 631–641. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.T.; Wang, C.Z.; Ni, M.; Wu, J.A.; Mehendale, S.R.; Aung, H.H.; Foo, A.; Yuan, C.S. American ginseng berry juice intake reduces blood glucose and body weight in ob/ob mice. J. Food Sci. 2007, 72, S590–S594. [Google Scholar] [CrossRef]
- Hu, J.R.; Chun, Y.S.; Kim, J.K.; Cho, I.J.; Ku, S.K. Ginseng berry aqueous extract prevents scopolamine-induced memory impairment in mice. Exp. Ther. Med. 2019, 18, 4388–4396. [Google Scholar] [CrossRef]
- Kim, M.H.; Lee, J.; Jung, S.; Kim, J.W.; Shin, J.H.; Lee, H.J. The involvement of ginseng berry extract in blood flow via regulation of blood coagulation in rats fed a high-fat diet. J. Ginseng Res. 2017, 41, 120–126. [Google Scholar] [CrossRef]
- Shin, J.E.; Jeon, S.H.; Lee, S.J.; Choung, S.Y. The Administration of Panax ginseng Berry Extract Attenuates High-Fat-Diet-Induced Sarcopenic Obesity in C57BL/6 Mice. Nutrients 2022, 14, 1747. [Google Scholar] [CrossRef] [PubMed]
- Song, S.Y.; Park, D.H.; Seo, S.W.; Park, K.M.; Bae, C.S.; Son, H.S.; Kim, H.G.; Lee, J.H.; Yoon, G.; Shim, J.H.; et al. Effects of Harvest Time on Phytochemical Constituents and Biological Activities of Panax ginseng Berry Extracts. Molecules 2019, 24, 3343. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Cho, S.S.; Li, Y.; Bae, C.S.; Park, K.M.; Park, D.H. Anti-inflammatory Effect of Curcuma longa and Allium hookeri Co-treatment via NF-κB and COX-2 Pathways. Sci. Rep. 2020, 10, 5718. [Google Scholar] [CrossRef] [PubMed]
- Baeg, I.H.; So, S.H. The world ginseng market and the ginseng (Korea). J. Ginseng Res. 2013, 37, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Yi, Y.S.; Kim, J.; Han, S.Y.; Kim, S.H.; Seo, D.B.; Cho, J.Y.; Shin, S.S. Effect of polysaccharides from a Korean ginseng berry on the immunosenescence of aged mice. J. Ginseng Res. 2018, 42, 447–454. [Google Scholar] [CrossRef]
- Nam, Y.; Bae, J.; Jeong, J.H.; Ko, S.K.; Sohn, U.D. Protective effect of ultrasonication-processed ginseng berry extract on the D-galactosamine/lipopolysaccharide-induced liver injury model in rats. J. Ginseng Res. 2018, 42, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Seo, Y.W.; Choi, J.Y.; Kim, S.H. Vestibular function is associated with residual low-frequency hearing loss in patients with bi-allelic mutations in the SLC26A4 gene. Hear. Res. 2016, 335, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.; Jeong, J.-J.; Eun, S.-H.; Kim, D.-H. Anti-inflammatory effects of ginsenoside Rg1 and its metabolites ginsenoside Rh1 and 20(S)-protopanaxatriol in mice with TNBS-induced colitis. Eur. J. Pharmacol. 2015, 762, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.-J.; Han, I.-H.; Kim, Y.-J.; Yamabe, N.; Lee, D.; Hwang, G.S.; Oh, M.; Choi, K.-C.; Kim, S.-N.; Ham, J.; et al. Anticarcinogenic Effects of Products of Heat-Processed Ginsenoside Re, a Major Constituent of Ginseng Berry, on Human Gastric Cancer Cells. J. Agric. Food Chem. 2014, 62, 2830–2836. [Google Scholar] [CrossRef]
- Park, C.H.; Park, S.K.; Seung, T.W.; Jin, D.E.; Guo, T.; Heo, H.J. Effect of Ginseng (Panax ginseng) Berry EtOAc Fraction on Cognitive Impairment in C57BL/6 Mice under High-Fat Diet Inducement. Evid.-Based Complement. Altern. Med. eCAM 2015, 2015, 316527. [Google Scholar] [CrossRef]
- Kim, J.M.; Park, C.H.; Park, S.K.; Seung, T.W.; Kang, J.Y.; Ha, J.S.; Lee, D.S.; Lee, U.; Kim, D.O.; Heo, H.J. Ginsenoside Re Ameliorates Brain Insulin Resistance and Cognitive Dysfunction in High Fat Diet-Induced C57BL/6 Mice. J. Agric. Food Chem. 2017, 65, 2719–2729. [Google Scholar] [CrossRef] [PubMed]
- GutiErrez-Grijalva, E.P.; Ambriz-Pere, D.L.; Leyva-Lopez, N.; Castillo-Lopez, R.I.; Heiedia, J.B. Review: Dietary phenolic compounds, health benefits and bioaccessibility. Arch. Latinoam. Nutr. 2016, 66, 87–100. [Google Scholar] [PubMed]
- Bondia-Pons, I.; Aura, A.-M.; Vuorela, S.; Kolehmainen, M.; Mykkänen, H.; Poutanen, K. Rye phenolics in nutrition and health. J. Cereal Sci. 2009, 49, 323–336. [Google Scholar] [CrossRef]
- Garcia-Martinez, O.; Ruiz, C.; Gutierrez-Ibanez, A.; Illescas-Montes, R.; Melguizo-Rodriguez, L. Benefits of Olive Oil Phenolic Compounds in Disease Prevention. Endocr. Metab. Immune Disord. Drug Targets 2018, 18, 333–340. [Google Scholar] [CrossRef]
- Leung, K.W.; Wong, A.S. Pharmacology of ginsenosides: A literature review. Chin. Med. 2010, 5, 20. [Google Scholar] [CrossRef]
- Xie, H.T.; Wang, G.J.; Chen, M.; Jiang, X.L.; Li, H.; Lv, H.; Huang, C.R.; Wang, R.; Roberts, M. Uptake and metabolism of ginsenoside Rh2 and its aglycon protopanaxadiol by Caco-2 cells. Biol. Pharm. Bull. 2005, 28, 383–386. [Google Scholar] [CrossRef]
- Karikura, M.; Tanizawa, H.; Hirata, T.; Miyase, T.; Takino, Y. Studies on absorption, distribution, excretion and metabolism of ginseng saponins. VIII. Isotope labeling of ginsenoside Rb2. Chem. Pharm. Bull. (Tokyo) 1992, 40, 2458–2460. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.F.; Fang, X.L.; Chen, D.F. Pharmacokinetics and bioavailability of ginsenoside Rb1 and Rg1 from Panax notoginseng in rats. J. Ethnopharmacol. 2003, 84, 187–192. [Google Scholar] [CrossRef]
- Han, M.; Fang, X.L. Difference in oral absorption of ginsenoside Rg1 between in vitro and in vivo models. Acta Pharmacol. Sin. 2006, 27, 499–505. [Google Scholar] [CrossRef]
- Han, M.; Sha, X.; Wu, Y.; Fang, X. Oral absorption of ginsenoside Rb1 using in vitro and in vivo models. Planta Med. 2006, 72, 398–404. [Google Scholar] [CrossRef]
- Shimoyama, A.T.; Santin, J.R.; Machado, I.D.; De Oliveira e Silva, A.M.; De Melo, I.L.; Mancini-Filho, J.; Farsky, S.H. Antiulcerogenic activity of chlorogenic acid in different models of gastric ulcer. Naunyn-Schmiedebergs Arch. Pharmacol. 2013, 386, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Boeing, T.; Costa, P.; Venzon, L.; Meurer, M.; Mariano, L.N.B.; França, T.C.S.; Gouveia, L.; De Bassi, A.C.; Steimbach, V.; De Souza, P.; et al. Gastric healing effect of p-coumaric acid isolated from Baccharis dracunculifolia DC on animal model. Naunyn-Schmiedebergs Arch. Pharmacol. 2021, 394, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.A.; Hyam, S.R.; Jang, S.E.; Han, M.J.; Kim, D.H. Ginsenoside Re ameliorates inflammation by inhibiting the binding of lipopolysaccharide to TLR4 on macrophages. J. Agric. Food Chem. 2012, 60, 9595–9602. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Rhee, M.H.; Lee, J.; Kim, S.H.; Yang, Y.; Kim, H.G.; Kim, Y.; Kim, C.; Kwak, Y.S.; Kim, J.H.; et al. Ginsenoside Rc from Korean Red Ginseng (Panax ginseng C.A. Meyer) Attenuates Inflammatory Symptoms of Gastritis, Hepatitis and Arthritis. Am. J. Chin. Med. 2016, 44, 595–615. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.L.; Guo, T.K.; Wang, Y.H.; Huang, Y.H.; Liu, X.; Wang, X.X.; Li, W.; Zhao, X.; Wang, L.P.; Yan, S.; et al. Ginsenoside Rd attenuates the inflammatory response via modulating p38 and JNK signaling pathways in rats with TNBS-induced relapsing colitis. Int. Immunopharmacol. 2012, 12, 408–414. [Google Scholar] [CrossRef]
- Carvalho, C.A.; Fernandes, K.M.; Matta, S.L.; Silva, M.B.; Oliveira, L.L.; Fonseca, C.C. Evaluation of antiulcerogenic activity of aqueous extract of Brassica oleracea var. capitata (cabbage) on Wistar rat gastric ulceration. Arq. Gastroenterol. 2011, 48, 276–282. [Google Scholar] [CrossRef]


| Time | % A | % B | |
|---|---|---|---|
| Conditions | 0 | 10 | 90 |
| 3 | 12 | 88 | |
| 6 | 14 | 86 | |
| 9 | 16 | 84 | |
| 12 | 18 | 82 | |
| 32 | 26 | 74 | |
| 40 | 36 | 64 | |
| 50 | 50 | 50 | |
| 55 | 100 | 0 | |
| 57 | 10 | 90 | |
| 60 | 10 | 90 |
| Biomarker | Content (%) |
|---|---|
| Ginsenoside rb3 | 2.55 ± 0.04 |
| Ginsenoside re | 5.21 ± 0.21 |
| Ginsenoside rc | 2.12 ± 0.16 |
| Ginsenoside rd | 2.73 ± 0.02 |
| Chlorogenic acid | 0.16 ± 0.03 |
| Caffeic acid | 0.07 ± 0.001 |
| p-Coumaric acid | 0.03 ± 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-Y.; Song, S.-Y.; Lee, S.-H.; Kim, G.-Y.; Park, J.-W.; Bae, C.-S.; Park, D.-H.; Cho, S.-S. Ginseng Berry Juice (GBJ) Regulates the Inflammation in Acute Ulcerative Mouse Models and the Major Bioactive Substances Are Ginsenosides Rb3, Rc, Rd, and Re. Nutrients 2024, 16, 1031. https://doi.org/10.3390/nu16071031
Lee S-Y, Song S-Y, Lee S-H, Kim G-Y, Park J-W, Bae C-S, Park D-H, Cho S-S. Ginseng Berry Juice (GBJ) Regulates the Inflammation in Acute Ulcerative Mouse Models and the Major Bioactive Substances Are Ginsenosides Rb3, Rc, Rd, and Re. Nutrients. 2024; 16(7):1031. https://doi.org/10.3390/nu16071031
Chicago/Turabian StyleLee, Soon-Young, Seung-Yub Song, Sung-Ho Lee, Gye-Yeop Kim, Jin-Woo Park, Chun-Sik Bae, Dae-Hun Park, and Seung-Sik Cho. 2024. "Ginseng Berry Juice (GBJ) Regulates the Inflammation in Acute Ulcerative Mouse Models and the Major Bioactive Substances Are Ginsenosides Rb3, Rc, Rd, and Re" Nutrients 16, no. 7: 1031. https://doi.org/10.3390/nu16071031
APA StyleLee, S.-Y., Song, S.-Y., Lee, S.-H., Kim, G.-Y., Park, J.-W., Bae, C.-S., Park, D.-H., & Cho, S.-S. (2024). Ginseng Berry Juice (GBJ) Regulates the Inflammation in Acute Ulcerative Mouse Models and the Major Bioactive Substances Are Ginsenosides Rb3, Rc, Rd, and Re. Nutrients, 16(7), 1031. https://doi.org/10.3390/nu16071031








