Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses
Abstract
1. Introduction
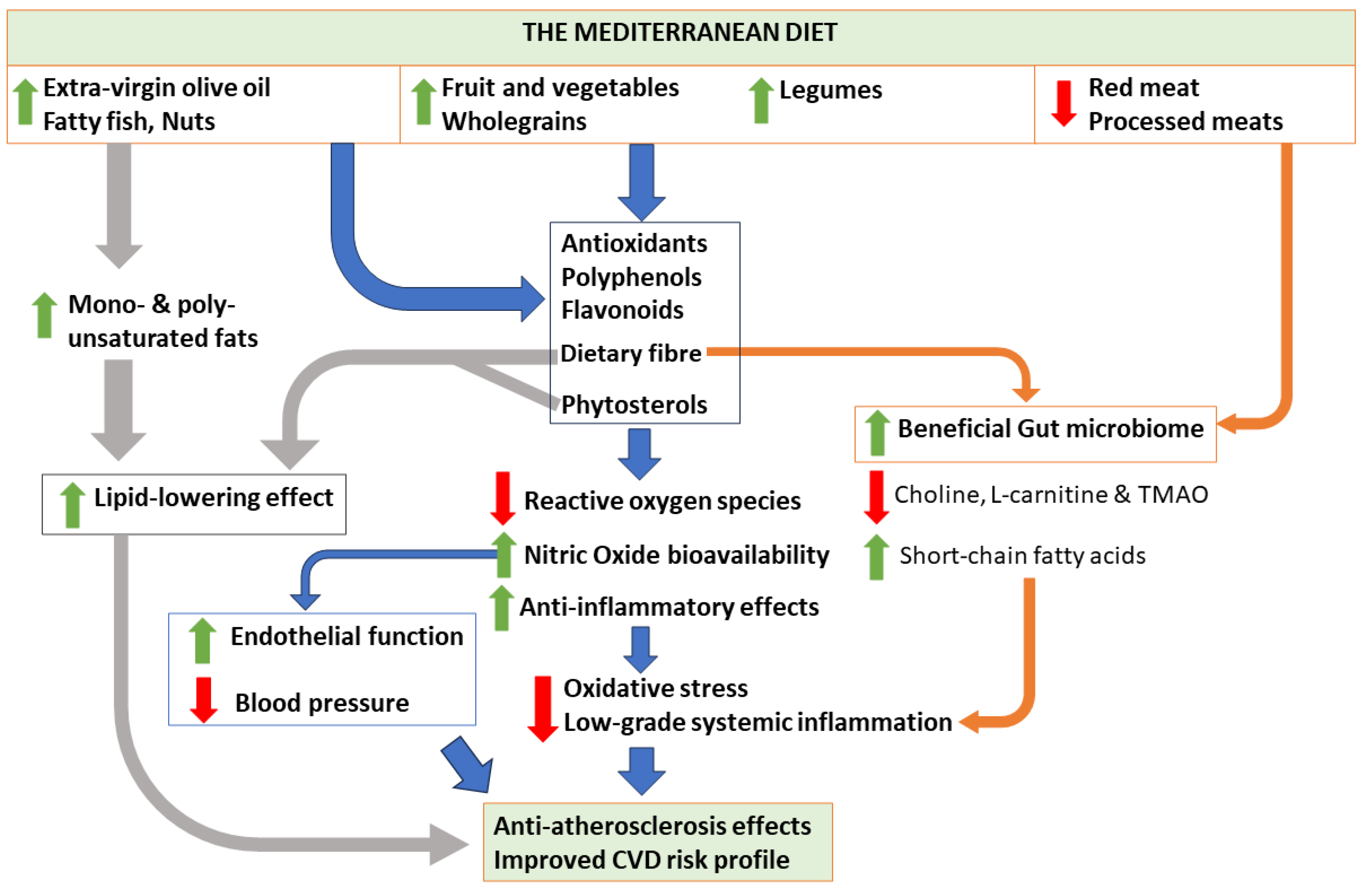
2. Cardio-Protective Benefits of the MD
3. Comparison with Other Diets
3.1. Western Diet
3.2. Low-Fat Diet
3.3. Dietary Approaches to Stop Hypertension (DASH)
3.4. Vegetarian/Vegan Diets
3.5. Region-Specific Dietary Patterns
4. Sex-Specific Mechanisms in Nutrition
5. Current Evidence on the MD and Cardiovascular Health
5.1. The MD and Cardiovascular Outcomes in Women Versus Men
5.2. Hypertension (or High BP)
5.3. T2DM
5.4. Anthropometric and Metabolic Parameters
6. The MD and Female-Specific Conditions
6.1. PCOS
6.2. Pregnancy-Related Complications
6.3. Female-Predominant Inflammatory Autoimmune Conditions
7. Future Directions
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| CVD | cardiovascular disease |
| MD | Mediterranean diet |
| EVOO | extra-virgin olive oil |
| GDM | gestational diabetes mellitus |
| PCOS | polycystic ovarian syndrome |
| RA | rheumatoid arthritis |
| SLE | systemic erythematous lupus |
| BP | blood pressure |
| ROS | reactive oxygen species |
| BMI | body mass index |
| DASH | dietary approaches to stop hypertension |
| LDL-C | low-density lipoprotein cholesterol |
| HDL-C | high-density lipoprotein cholesterol |
| Hs-CRP | high-sensitivity C-reactive protein |
| T2DM | type 2 diabetes mellitus |
| APOE | apolipoprotein E gene |
| ACE | angiotensin-converting enzyme |
| RCT | randomized–controlled trial |
| PREDIMED | Prevención con Dieta Mediterránea |
| CORDIOPREV | CORonary Diet Intervention with Olive oil and cardiovascular PREVention |
| US | United States of America |
| CHD | coronary heart disease |
| HDP | hypertensive disorders of pregnancy |
| LC-PUFA | long-chain polyunsaturated fatty acid |
References
- Vogel, B.; Acevedo, M.; Appelman, Y.; Merz, C.N.B.; Chieffo, A.; A Figtree, G.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.H.E.M.; et al. The Lancet women and cardiovascular disease Commission: Reducing the global burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef] [PubMed]
- Tyrovola, D.; Soulaidopoulos, S.; Tsioufis, C.; Lazaros, G. The Role of Nutrition in Cardiovascular Disease: Current Concepts and Trends. Nutrients 2023, 15, 1064. [Google Scholar] [CrossRef]
- Nestel, P.J.; Mori, T.A. Dietary patterns, dietary nutrients and cardiovascular disease. Rev. Cardiovasc. Med. 2022, 23, 17. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef] [PubMed]
- Keys, A. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease; Harvard University Press: Cambridge, MA, USA, 1980. [Google Scholar]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean Diet, its Components, and Cardiovascular Disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; A Martínez-González, M.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef]
- Papadaki, A.; Nolen-Doerr, E.; Mantzoros, C.S. The Effect of the Mediterranean Diet on Metabolic Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults. Nutrients 2020, 12, 3342. [Google Scholar] [CrossRef]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardiovascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2017, 58, 173–191. [Google Scholar] [CrossRef]
- Pant, A.; Gribbin, S.; McIntyre, D.; Trivedi, R.; Marschner, S.; Laranjo, L.; Mamas, M.A.; Flood, V.; Chow, C.K.; Zaman, S. Primary prevention of cardiovascular disease in women with a Mediterranean diet: Systematic review and meta-analysis. Heart 2023, 109, 1208–1215. [Google Scholar] [CrossRef] [PubMed]
- Feskens, E.J.M.; Bailey, R.; Bhutta, Z.; Biesalski, H.K.; Eicher-Miller, H.; Krämer, K.; Pan, W.H.; Griffiths, J.C. Women’s health: Optimal nutrition throughout the lifecycle. Eur. J. Nutr. 2022, 61 (Suppl S1), 1–23. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.; Mulvagh, S.L.; Merz, C.N.B.; Buring, J.E.; Manson, J.E. Cardiovascular Disease in Women. Circ. Res. 2016, 118, 1273–1293. [Google Scholar] [CrossRef]
- Guan, C.; Zahid, S.; Minhas, A.S.; Ouyang, P.; Vaught, A.; Baker, V.L.; Michos, E.D. Polycystic ovary syndrome: A “risk-enhancing” factor for cardiovascular disease. Fertil. Steril. 2022, 117, 924–935. [Google Scholar] [CrossRef] [PubMed]
- Australian Chronic Disease Prevention Alliance. AusCVDRisk. Department of Health and Aged Care. 2023. Available online: https://www.cvdcheck.org.au/ (accessed on 12 November 2023).
- Mehta, L.S.; Velarde, G.P.; Lewey, J.; Sharma, G.; Bond, R.M.; Navas-Acien, A.; Fretts, A.M.; Magwood, G.S.; Yang, E.; Blumenthal, R.S.; et al. Cardiovascular Disease Risk Factors in Women: The Impact of Race and Ethnicity: A Scientific Statement From the American Heart Association. Circulation 2023, 147, 1471–1487. [Google Scholar] [CrossRef]
- Jebari-Benslaiman, S.; Galicia-García, U.; Larrea-Sebal, A.; Olaetxea, J.R.; Alloza, I.; Vandenbroeck, K.; Benito-Vicente, A.; Martín, C. Pathophysiology of Atherosclerosis. Int. J. Mol. Sci. 2022, 23, 3346. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Simonetta, I.; Daidone, M.; Mogavero, A.; Ortello, A.; Pinto, A. Metabolic and Vascular Effect of the Mediterranean Diet. Int. J. Mol. Sci. 2019, 20, 4716. [Google Scholar] [CrossRef]
- Richardson, L.A.; Izuora, K.; Basu, A. Mediterranean Diet and Its Association with Cardiovascular Disease Risk Factors: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 12762. [Google Scholar] [CrossRef]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. Ser. A 2018, 73, 318–326. [Google Scholar] [CrossRef]
- Shah, R.; Makarem, N.; Emin, M.; Liao, M.; Jelic, S.; Aggarwal, B. Mediterranean diet components are linked to greater endothelial function and lower inflammation in a pilot study of ethnically diverse women. Nutr. Res. 2020, 75, 77–84. [Google Scholar] [CrossRef]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef]
- Tang, W.H.W.; Wang, Z.; Levison, B.S.; Koeth, R.A.; Britt, E.B.; Fu, X.; Wu, Y.; Hazen, S.L. Intestinal Microbial Metabolism of Phosphatidylcholine and Cardiovascular Risk. N. Engl. J. Med. 2013, 368, 1575–1584. [Google Scholar] [CrossRef]
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jönsson, L.S.; Kolb, H.; Lansink, M.; et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br. J. Nutr. 2011, 106, S5–S78. [Google Scholar] [CrossRef]
- García-Montero, C.; Fraile-Martínez, O.; Gómez-Lahoz, A.M.; Pekarek, L.; Castellanos, A.J.; Noguerales-Fraguas, F.; Coca, S.; Guijarro, L.G.; García-Honduvilla, N.; Asúnsolo, A.; et al. Nutritional Components in Western Diet Versus Mediterranean Diet at the Gut Microbiota–Immune System Interplay. Implications for Health and Disease. Nutrients 2021, 13, 699. [Google Scholar] [CrossRef]
- Kopp, W. How Western Diet and Lifestyle Drive the Pandemic of Obesity and Civilization Diseases. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2221–2236. [Google Scholar] [CrossRef] [PubMed]
- Christ, A.; Lauterbach, M.; Latz, E. Western Diet and the Immune System: An Inflammatory Connection. Immunity 2019, 51, 794–811. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, R.; Shively, C.A.; Register, T.C.; Craft, S.; Yadav, H. Gut microbiome-Mediterranean diet interactions in improving host health. F1000Research 2019, 8, 699. [Google Scholar] [CrossRef]
- Klonizakis, M.; Bugg, A.; Hunt, B.; Theodoridis, X.; Bogdanos, D.P.; Grammatikopoulou, M.G. Assessing the Physiological Effects of Traditional Regional Diets Targeting the Prevention of Cardiovascular Disease: A Systematic Review of Randomized Controlled Trials Implementing Mediterranean, New Nordic, Japanese, Atlantic, Persian and Mexican Dietary Interventions. Nutrients 2021, 13, 3034. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.B.; Fedacko, J.; Fatima, G.; Magomedova, A.; Watanabe, S.; Elkilany, G. Why and How the Indo-Mediterranean Diet May Be Superior to Other Diets: The Role of Antioxidants in the Diet. Nutrients 2022, 14, 898. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Delgado-Lista, J.; Alcala-Diaz, J.F.; Torres-Peña, J.D.; Quintana-Navarro, G.M.; Fuentes, F.; Garcia-Rios, A.; Ortiz-Morales, A.M.; I Gonzalez-Requero, A.; I Perez-Caballero, A.; Yubero-Serrano, E.M.; et al. Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): A randomised controlled trial. Lancet 2022, 399, 1876–1885. [Google Scholar] [CrossRef]
- Nordmann, A.J.; Suter-Zimmermann, K.; Bucher, H.C.; Shai, I.; Tuttle, K.R.; Estruch, R.; Briel, M. Meta-Analysis Comparing Mediterranean to Low-Fat Diets for Modification of Cardiovascular Risk Factors. Am. J. Med. 2011, 124, 841–851.e2. [Google Scholar] [CrossRef]
- Critselis, E.; Kontogianni, M.D.; Georgousopoulou, E.; Chrysohoou, C.; Tousoulis, D.; Pitsavos, C.; Panagiotakos, D.B. Comparison of the Mediterranean diet and the Dietary Approach Stop Hypertension in reducing the risk of 10-year fatal and non-fatal CVD events in healthy adults: The ATTICA Study (2002–2012). PhotoniX 2020, 24, 2746–2757. [Google Scholar] [CrossRef]
- Bertoia, M.L.; Triche, E.W.; Michaud, D.S.; Baylin, A.; Hogan, J.W.; Neuhouser, M.L.; Tinker, L.F.; Van Horn, L.; E Waring, M.; Li, W.; et al. Mediterranean and Dietary Approaches to Stop Hypertension dietary patterns and risk of sudden cardiac death in postmenopausal women. Am. J. Clin. Nutr. 2014, 99, 344–351. [Google Scholar] [CrossRef]
- Panbehkar-Jouybari, M.; Mollahosseini, M.; Salehi-Abargouei, A.; Fallahzadeh, H.; Mirzaei, M.; Hosseinzadeh, M. The Mediterranean diet and dietary approach to stop hypertension (DASH)-style diet are differently associated with lipid profile in a large sample of Iranian adults: A cross-sectional study of Shahedieh cohort. BMC Endocr. Disord. 2021, 21, 192. [Google Scholar] [CrossRef]
- Jalilpiran, Y.; Mofrad, M.D.; Mozaffari, H.; Bellissimo, N.; Azadbakht, L. Adherence to dietary approaches to stop hypertension (DASH) and Mediterranean dietary patterns in relation to cardiovascular risk factors in older adults. Clin. Nutr. ESPEN 2020, 39, 87–95. [Google Scholar] [CrossRef]
- Sofi, F.; Dinu, M.; Pagliai, G.; Cesari, F.; Gori, A.M.; Sereni, A.; Becatti, M.; Fiorillo, C.; Marcucci, R.; Casini, A. Low-Calorie Vegetarian Versus Mediterranean Diets for Reducing Body Weight and Improving Cardiovascular Risk Profile: CARDIVEG Study (Cardiovascular Prevention with Vegetarian Diet). Circulation 2018, 137, 1103–1113. [Google Scholar] [CrossRef]
- Rogerson, D.; Maçãs, D.; Milner, M.; Liu, Y.; Klonizakis, M. Contrasting Effects of Short-Term Mediterranean and Vegan Diets on Microvascular Function and Cholesterol in Younger Adults: A Comparative Pilot Study. Nutrients 2018, 10, 1897. [Google Scholar] [CrossRef]
- Barnard, N.D.; Alwarith, J.; Rembert, E.; Brandon, L.; Nguyen, M.; Goergen, A.; Horne, T.; Nascimento, G.F.D.; Lakkadi, K.; Tura, A.; et al. A Mediterranean Diet and Low-Fat Vegan Diet to Improve Body Weight and Cardiometabolic Risk Factors: A Randomized, Cross-over Trial. J. Am. Nutr. Assoc. 2021, 41, 127–139. [Google Scholar] [CrossRef]
- Bonaccio, M.; the Moli-sani Study Investigators; Di Castelnuovo, A.; Costanzo, S.; De Curtis, A.; Persichillo, M.; Cerletti, C.; Donati, M.B.; de Gaetano, G.; Iacoviello, L. Association of a traditional Mediterranean diet and non-Mediterranean dietary scores with all-cause and cause-specific mortality: Prospective findings from the Moli-sani Study. Eur. J. Nutr. 2020, 60, 729–746. [Google Scholar] [CrossRef]
- Galbete, C.; Kröger, J.; Jannasch, F.; Iqbal, K.; Schwingshackl, L.; Schwedhelm, C.; Weikert, C.; Boeing, H.; Schulze, M.B. Nordic diet, Mediterranean diet, and the risk of chronic diseases: The EPIC-Potsdam study. BMC Med. 2018, 16, 99. [Google Scholar] [CrossRef]
- Li, Y.; Roswall, N.; Ström, P.; Sandin, S.; Adami, H.O.; Weiderpass, E. Mediterranean and Nordic diet scores and long-term changes in body weight and waist circumference: Results from a large cohort study. Br. J. Nutr. 2015, 114, 2093–2102. [Google Scholar] [CrossRef]
- Hooper, L.; Abdelhamid, A.; Moore, H.J.; Douthwaite, W.; Skeaff, C.M.; Summerbell, C.D. Effect of reducing total fat intake on body weight: Systematic review and meta-analysis of randomised controlled trials and cohort studies. BMJ 2012, 345, e7666. [Google Scholar] [CrossRef]
- Temporelli, P.L. Cardiovascular prevention: Mediterranean or low-fat diet? Eur. Heart J. Suppl. 2023, 25, B166–B170. [Google Scholar] [CrossRef]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef]
- Olukorode, J.; A Omokore, O.; Odunaike, O.S.; Omiko, R.; Osaghae, O.W.; Sange, W.; A Orimoloye, D.; O Kristilere, H.; Addeh, E.; Onwuzo, S.; et al. DASH Diet: A Review of Its Scientifically Proven Hypertension Reduction and Health Benefits. Cureus 2023, 15, e44692. [Google Scholar] [CrossRef]
- Zampelas, A.; Magriplis, E. Dietary patterns and risk of cardiovascular diseases: A review of the evidence. Proc. Nutr. Soc. 2019, 79, 68–75. [Google Scholar] [CrossRef]
- Kahleova, H.; Salas-Salvadó, J.; Rahelić, D.; Kendall, C.W.; Rembert, E.; Sievenpiper, J.L. Dietary Patterns and Cardiometabolic Outcomes in Diabetes: A Summary of Systematic Reviews and Meta-Analyses. Nutrients 2019, 11, 2209. [Google Scholar] [CrossRef]
- Jalilpiran, Y.; Jayedi, A.; Djafarian, K.; Shab-Bidar, S. The Nordic diet and the risk of non-communicable chronic disease and mortality: A systematic review and dose-response meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 2020, 62, 3124–3136. [Google Scholar] [CrossRef]
- Krznarić, Ž.; Karas, I.; Kelečić, D.L.; Bender, D.V. The Mediterranean and Nordic Diet: A Review of Differences and Similarities of Two Sustainable, Health-Promoting Dietary Patterns. Front. Nutr. 2021, 8, 683678. [Google Scholar] [CrossRef]
- Shirota, M.; Watanabe, N.; Suzuki, M.; Kobori, M. Japanese-Style Diet and Cardiovascular Disease Mortality: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients 2022, 14, 2008. [Google Scholar] [CrossRef]
- Marino, M.; Masella, R.; Bulzomi, P.; Campesi, I.; Malorni, W.; Franconi, F. Nutrition and human health from a sex–gender perspective. Mol. Asp. Med. 2011, 32, 1–70. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Frank, G.; De Santis, G.L.; Cianci, R.; Bigioni, G.; De Lorenzo, A. Sex Differences in the Efficacy of Mediterranean Diet Treatment: A Nutrigenomics Pilot Study. Genes 2023, 14, 1980. [Google Scholar] [CrossRef]
- de Toda, I.M.; González-Sánchez, M.; Cerro, E.D.-D.; Valera, G.; Carracedo, J.; Guerra-Pérez, N. Sex differences in markers of oxidation and inflammation. Implications for ageing. Mech. Ageing Dev. 2023, 211, 111797. [Google Scholar] [CrossRef]
- Kander, M.C.; Cui, Y.; Liu, Z. Gender difference in oxidative stress: A new look at the mechanisms for cardiovascular diseases. J. Cell. Mol. Med. 2017, 21, 1024–1032. [Google Scholar] [CrossRef]
- Bédard, A.; Lamarche, B.; Corneau, L.; Dodin, S.; Lemieux, S. Sex differences in the impact of the Mediterranean diet on systemic inflammation. Nutr. J. 2015, 14, 46. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Kim, M.; Paye, S.; Benayoun, B.A. Sex as a Biological Variable in Nutrition Research: From Human Studies to Animal Models. Annu. Rev. Nutr. 2022, 42, 227–250. [Google Scholar] [CrossRef]
- Peng, C.; Xu, X.; Li, Y.; Li, X.; Yang, X.; Chen, H.; Zhu, Y.; Lu, N.; He, C. Sex-specific association between the gut microbiome and high-fat diet-induced metabolic disorders in mice. Biol. Sex Differ. 2020, 11, 5. [Google Scholar] [CrossRef]
- Pettersson, U.S.; Waldén, T.B.; Carlsson, P.-O.; Jansson, L.; Phillipson, M. Female Mice are Protected against High-Fat Diet Induced Metabolic Syndrome and Increase the Regulatory T Cell Population in Adipose Tissue. PLoS ONE 2012, 7, e46057. [Google Scholar] [CrossRef]
- Grzymisławska, M.; Puch, E.; Zawada, A.; Grzymisławski, M. Do nutritional behaviors depend on biological sex and cultural gender? Adv. Clin. Exp. Med. 2020, 29, 165–172. [Google Scholar] [CrossRef]
- Valeri, F.; Endres, K. How biological sex of the host shapes its gut microbiota. Front. Neuroendocr. 2021, 61, 100912. [Google Scholar] [CrossRef]
- Wardle, J.; Haase, A.M.; Steptoe, A.; Nillapun, M.; Jonwutiwes, K.; Bellisie, F. Gender differences in food choice: The contribution of health beliefs and dieting. Ann. Behav. Med. 2004, 27, 107–116. [Google Scholar] [CrossRef]
- Razavi, A.C.; Potts, K.S.; Kelly, T.N.; Bazzano, L.A. Sex, gut microbiome, and cardiovascular disease risk. Biol. Sex Differ. 2019, 10, 29. [Google Scholar] [CrossRef]
- Nissensohn, M.; Román-Viñas, B.; Sánchez-Villegas, A.; Piscopo, S.; Serra-Majem, L. The Effect of the Mediterranean Diet on Hypertension: A Systematic Review and Meta-Analysis. J. Nutr. Educ. Behav. 2016, 48, 42–53.e1. [Google Scholar] [CrossRef] [PubMed]
- Katherine, E.; Maria Ida, M.; Giuseppe, B.; Paolo, C.; Demosthenes, P.; Dario, G. A journey into a Mediterranean diet and type 2 diabetes: A systematic review with meta-analyses. BMJ Open 2015, 5, e008222. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Veronese, N.; Di Bella, G.; Cusumano, C.; Parisi, A.; Tagliaferri, F.; Ciriminna, S.; Barbagallo, M. Mediterranean diet in the management and prevention of obesity. Exp. Gerontol. 2023, 174, 112121. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 2019, CD009825. [Google Scholar] [CrossRef]
- de Lorgeril, M.; Salen, P.; Martin, J.-L.; Monjaud, I.; Delaye, J.; Mamelle, N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: Final report of the Lyon Diet Heart Study. Circulation 1999, 99, 779–785. [Google Scholar] [CrossRef]
- Fung, T.T.; Rexrode, K.M.; Mantzoros, C.S.; Manson, J.E.; Willett, W.C.; Hu, F.B. Mediterranean Diet and Incidence of and Mortality From Coronary Heart Disease and Stroke in Women. Circulation 2009, 119, 1093–1100. [Google Scholar] [CrossRef]
- Esposito, K.; Pontillo, A.; Di Palo, C.; Giugliano, G.; Masella, M.; Marfella, R.; Giugliano, D. Effect of Weight Loss and Lifestyle Changes on Vascular Inflammatory Markers in Obese Women. JAMA 2003, 289, 1799–1804. [Google Scholar] [CrossRef]
- Toobert, D.J.; Glasgow, R.E.; Strycker, L.A.; Barrera, M.; Radcliffe, J.L.; Wander, R.C.; Bagdade, J.D. Biologic and Quality-of-Life Outcomes From the Mediterranean Lifestyle Program. Diabetes Care 2003, 26, 2288–2293. [Google Scholar] [CrossRef]
- Storniolo, C.E.; Casillas, R.; Bulló, M.; Castañer, O.; Ros, E.; Sáez, G.T.; Toledo, E.; Estruch, R.; Ruiz-Gutiérrez, V.; Fitó, M.; et al. A Mediterranean diet supplemented with extra virgin olive oil or nuts improves endothelial markers involved in blood pressure control in hypertensive women. Eur. J. Nutr. 2015, 56, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Dunn, S.L.; Boutcher, S.H.; Freund, J.; Siu, W. The effect of a lifestyle intervention on metabolic health in young women. Diabetes Metab. Syndr. Obes. Targets Ther. 2014, 7, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Buscemi, S.; Verga, S.; Tranchina, M.R.; Cottone, S.; Cerasola, G. Effects of hypocaloric very-low-carbohydrate diet vs. Mediterranean diet on endothelial function in obese women. Eur. J. Clin. Investig. 2009, 39, 339–347. [Google Scholar] [CrossRef]
- Bajerska, J.; Chmurzynska, A.; Muzsik, A.; Krzyżanowska-Jankowska, P.; Mądry, E.; Malinowska, A.M.; Walkowiak, J. Weight loss and metabolic health effects from energy-restricted Mediterranean and Central-European diets in postmenopausal women: A randomized controlled trial. Sci. Rep. 2018, 8, 11170. [Google Scholar] [CrossRef]
- Jennings, A.; Berendsen, A.M.; De Groot, L.C.P.G.M.; Feskens, E.J.M.; Brzozowska, A.; Sicińska, E.; Pietruszka, B.; Meunier, N.; Caumon, E.; Malpuech-Brugère, C.; et al. Mediterranean-Style Diet Improves Systolic Blood Pressure and Arterial Stiffness in Older Adults. Hypertension 2019, 73, 578–586. [Google Scholar] [CrossRef]
- Ahmad, S.; Demler, O.V.; Sun, Q.; Moorthy, M.V.; Li, C.; Lee, I.-M.; Ridker, P.M.; Manson, J.E.; Hu, F.B.; Fall, T.; et al. Association of the Mediterranean Diet With Onset of Diabetes in the Women’s Health Study. JAMA Netw. Open 2020, 3, e2025466. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Bulló, M.; Babio, N.; Martínez-González, M.; Ibarrola-Jurado, N.; Basora, J.; Estruch, R.; Covas, M.I.; Corella, D.; Arós, F.; et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: Results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2011, 34, 14–19. [Google Scholar] [CrossRef]
- Mei, S.; Ding, J.; Wang, K.; Ni, Z.; Yu, J. Mediterranean Diet Combined with a Low-Carbohydrate Dietary Pattern in the Treatment of Overweight Polycystic Ovary Syndrome Patients. Front. Nutr. 2022, 9, 876620. [Google Scholar] [CrossRef]
- Cincione, I.R.; Graziadio, C.; Marino, F.; Vetrani, C.; Losavio, F.; Savastano, S.; Colao, A.; Laudisio, D. Short-time effects of ketogenic diet or modestly hypocaloric Mediterranean diet on overweight and obese women with polycystic ovary syndrome. J. Endocrinol. Investig. 2022, 46, 769–777. [Google Scholar] [CrossRef]
- Pérez-Ferre, N.; Del Valle, L.; Torrejón, M.J.; Barca, I.; Calvo, M.I.; Matía, P.; Rubio, M.A.; Calle-Pascual, A.L. Diabetes mellitus and abnormal glucose tolerance development after gestational diabetes: A three-year, prospective, randomized, clinical-based, Mediterranean lifestyle interventional study with parallel groups. Clin. Nutr. 2014, 34, 579–585. [Google Scholar] [CrossRef]
- Riemer, M.; Schulze, S.; Wagner, L.; Richter, M.; Ayerle, G.; Simm, A.; Seeger, S.; Schwesig, R.; Tchirikov, M.; Seliger, G. Cardiovascular Risk Reduction in Women Following Hypertensive Disorders of Pregnancy—A Prospective, Randomised, Controlled Interventional Study. Geburtshilfe Frauenheilkd. 2021, 81, 966–978. [Google Scholar] [CrossRef]
- Crovetto, F.; Crispi, F.; Casas, R.; Martín-Asuero, A.; Borràs, R.; Vieta, E.; Estruch, R.; Gratacós, E. Effects of Mediterranean Diet or Mindfulness-Based Stress Reduction on Prevention of Small-for-Gestational Age Birth Weights in Newborns Born to At-Risk Pregnant Individuals: The IMPACT BCN Randomized Clinical Trial. JAMA 2021, 326, 2150–2160. [Google Scholar] [CrossRef]
- Casas, I.; Nakaki, A.; Pascal, R.; Castro-Barquero, S.; Youssef, L.; Genero, M.; Benitez, L.; Larroya, M.; Boutet, M.L.; Casu, G.; et al. Effects of a Mediterranean Diet Intervention on Maternal Stress, Well-Being, and Sleep Quality throughout Gestation-The IMPACT-BCN Trial. Nutrients 2023, 15, 2362. [Google Scholar] [CrossRef]
- Mahjoub, F.; Ben Jemaa, H.; Ben Sabeh, F.; Ben Amor, N.; Gamoudi, A.; Jamoussi, H. Impact of nutrients and Mediterranean diet on the occurrence of gestational diabetes. Libyan J. Med. 2021, 16, 1930346. [Google Scholar] [CrossRef]
- Papandreou, P.; Gioxari, A.; Daskalou, E.; Grammatikopoulou, M.G.; Skouroliakou, M.; Bogdanos, D.P. Mediterranean Diet and Physical Activity Nudges versus Usual Care in Women with Rheumatoid Arthritis: Results from the MADEIRA Randomized Controlled Trial. Nutrients 2023, 15, 676. [Google Scholar] [CrossRef]
- Pocovi-Gerardino, G.; Correa-Rodríguez, M.; Callejas-Rubio, J.-L.; Ríos-Fernández, R.; Martín-Amada, M.; Cruz-Caparros, M.-G.; Rueda-Medina, B.; Ortego-Centeno, N. Beneficial effect of Mediterranean diet on disease activity and cardiovascular risk in systemic lupus erythematosus patients: A cross-sectional study. Rheumatology 2020, 60, 160–169. [Google Scholar] [CrossRef]
- Neelakantan, N.; Koh, W.-P.; Yuan, J.-M.; van Dam, R.M. Diet-Quality Indexes Are Associated with a Lower Risk of Cardiovascular, Respiratory, and All-Cause Mortality among Chinese Adults. J. Nutr. 2018, 148, 1323–1332. [Google Scholar] [CrossRef]
- Reedy, J.; Krebs-Smith, S.M.; Miller, P.E.; Liese, A.D.; Kahle, L.L.; Park, Y.; Subar, A.F. Higher Diet Quality Is Associated with Decreased Risk of All-Cause, Cardiovascular Disease, and Cancer Mortality among Older Adults. J. Nutr. 2014, 144, 881–889. [Google Scholar] [CrossRef]
- George, S.M.; Ballard-Barbash, R.; Manson, J.E.; Reedy, J.; Shikany, J.M.; Subar, A.F.; Tinker, L.F.; Vitolins, M.; Neuhouser, M.L. Comparing Indices of Diet Quality With Chronic Disease Mortality Risk in Postmenopausal Women in the Women’s Health Initiative Observational Study: Evidence to Inform National Dietary Guidance. Am. J. Epidemiol. 2014, 180, 616–625. [Google Scholar] [CrossRef]
- Buckland, G.; González, C.A.; Agudo, A.; Vilardell, M.; Berenguer, A.; Amiano, P.; Ardanaz, E.; Arriola, L.; Barricarte, A.; Basterretxea, M.; et al. Adherence to the Mediterranean Diet and Risk of Coronary Heart Disease in the Spanish EPIC Cohort Study. Am. J. Epidemiol. 2009, 170, 1518–1529. [Google Scholar] [CrossRef]
- Strengers, J.G.; Ruijter, H.M.D.; Boer, J.M.; Asselbergs, F.W.; Verschuren, W.M.; van der Schouw, Y.T.; Sluijs, I. The association of the Mediterranean diet with heart failure risk in a Dutch population. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Moorthy, M.V.; Demler, O.V.; Hu, F.B.; Ridker, P.M.; Chasman, D.I.; Mora, S. Assessment of Risk Factors and Biomarkers Associated With Risk of Cardiovascular Disease Among Women Consuming a Mediterranean Diet. JAMA Netw. Open 2018, 1, e185708. [Google Scholar] [CrossRef]
- Chan, R.; Chan, D.; Woo, J. The association of a priori and a posterior dietary patterns with the risk of incident stroke in Chinese older people in Hong Kong. J. Nutr. Health Aging 2013, 17, 866–874. [Google Scholar] [CrossRef]
- Dilis, V.; Katsoulis, M.; Lagiou, P.; Trichopoulos, D.; Naska, A.; Trichopoulou, A. Mediterranean diet and CHD: The Greek European Prospective Investigation into Cancer and Nutrition cohort. Br. J. Nutr. 2012, 108, 699–709. [Google Scholar] [CrossRef]
- Van Den Brandt, P.A. The impact of a Mediterranean diet and healthy lifestyle on premature mortality in men and women. Am. J. Clin. Nutr. 2011, 94, 913–920. [Google Scholar] [CrossRef]
- Tang, C.; Wang, X.; Qin, L.-Q.; Dong, J.-Y. Mediterranean Diet and Mortality in People with Cardiovascular Disease: A Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 2623. [Google Scholar] [CrossRef]
- Ndanuko, R.N.; Tapsell, L.C.; E Charlton, K.; Neale, E.P.; Batterham, M.J. Dietary Patterns and Blood Pressure in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. Int. Rev. J. 2016, 7, 76–89. [Google Scholar] [CrossRef]
- Filippou, C.D.; Thomopoulos, C.G.; Kouremeti, M.M.; Sotiropoulou, L.I.; Nihoyannopoulos, P.I.; Tousoulis, D.M.; Tsioufis, C.P. Mediterranean diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. 2021, 40, 3191–3200. [Google Scholar] [CrossRef]
- Esposito, K.; Marfella, R.; Ciotola, M.; Di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a Mediterranean-Style Diet on Endothelial Dysfunction and Markers of Vascular Inflammation in the Metabolic Syndrome: A Randomized Trial. J. Am. Med. Assoc. 2004, 292, 1440–1446. [Google Scholar] [CrossRef]
- Bédard, A.; Riverin, M.; Dodin, S.; Corneau, L.; Lemieux, S. Sex differences in the impact of the Mediterranean diet on cardiovascular risk profile. Br. J. Nutr. 2012, 108, 1428–1434. [Google Scholar] [CrossRef]
- Esposito, K.; Giugliano, D. Mediterranean diet and type 2 diabetes. Diabetes/Metab. Res. Rev. 2014, 30, 34–40. [Google Scholar] [CrossRef]
- Martín-Peláez, S.; Fito, M.; Castaner, O. Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients 2020, 12, 2236. [Google Scholar] [CrossRef] [PubMed]
- Huo, R.; Du, T.; Xu, Y.; Xu, W.; Chen, X.; Sun, K.; Yu, X. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: A meta-analysis. Eur. J. Clin. Nutr. 2015, 69, 1200–1208. [Google Scholar] [CrossRef]
- Kaaks, R.; Bellati, C.; Venturelli, E.; Rinaldi, S.; Secreto, G.; Biessy, C.; Pala, V.; Sieri, S.; Berrino, F. Effects of dietary intervention on IGF-I and IGF-binding proteins, and related alterations in sex steroid metabolism: The Diet and Androgens (DIANA) Randomised Trial. Eur. J. Clin. Nutr. 2003, 57, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Ruiz-Gutiérrez, V.; Covas, M.I.; Fiol, M.; Gómez-Gracia, E.; López-Sabater, M.C.; Vinyoles, E.; et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: A randomized trial. Ann. Intern. Med. 2006, 145, 1–11. [Google Scholar] [CrossRef]
- Mancini, J.G.; Filion, K.B.; Atallah, R.; Eisenberg, M.J. Systematic Review of the Mediterranean Diet for Long-Term Weight Loss. Am. J. Med. 2016, 129, 407–415.e4. [Google Scholar] [CrossRef]
- Esposito, K.; Kastorini, C.-M.; Panagiotakos, D.B.; Giugliano, D. Mediterranean Diet and Weight Loss: Meta-Analysis of Randomized Controlled Trials. Metab. Syndr. Relat. Disord. 2011, 9, 1–12. [Google Scholar] [CrossRef]
- Teede, H.J.; Tay, C.T.; E Laven, J.J.; Dokras, A.; Moran, L.J.; Piltonen, T.T.; Costello, M.F.; Boivin, J.; Redman, L.M.; A Boyle, J.; et al. Recommendations From the 2023 International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. J. Clin. Endocrinol. Metab. 2023, 108, 2447–2469. [Google Scholar] [CrossRef]
- Osibogun, O.; Ogunmoroti, O.; Michos, E.D. Polycystic ovary syndrome and cardiometabolic risk: Opportunities for cardiovascular disease prevention. Trends Cardiovasc. Med. 2019, 30, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Cutillas-Tolín, A.; Arense-Gonzalo, J.J.; Mendiola, J.; Adoamnei, E.; Navarro-Lafuente, F.; Sánchez-Ferrer, M.L.; Prieto-Sánchez, M.T.; Carmona-Barnosi, A.; Vioque, J.; Torres-Cantero, A.M. Are Dietary Indices Associated with Polycystic Ovary Syndrome and Its Phenotypes? A Preliminary Study. Nutrients 2021, 13, 313. [Google Scholar] [CrossRef]
- Wang, Q.; Sun, Y.; Xu, Q.; Liu, W.; Wang, P.; Yao, J.; Zhao, A.; Chen, Y.; Wang, W. Higher dietary inflammation potential and certain dietary patterns are associated with polycystic ovary syndrome risk in China: A case-control study. Nutr. Res. 2022, 100, 1–18. [Google Scholar] [CrossRef]
- Barrea, L.; Arnone, A.; Annunziata, G.; Muscogiuri, G.; Laudisio, D.; Salzano, C.; Pugliese, G.; Colao, A.; Savastano, S. Adherence to the Mediterranean Diet, Dietary Patterns and Body Composition in Women with Polycystic Ovary Syndrome (PCOS). Nutrients 2019, 11, 2278. [Google Scholar] [CrossRef]
- Moran, L.J.; Grieger, J.A.; Mishra, G.D.; Teede, H.J. The Association of a Mediterranean-Style Diet Pattern with Polycystic Ovary Syndrome Status in a Community Cohort Study. Nutrients 2015, 7, 8553–8564. [Google Scholar] [CrossRef]
- Marschner, S.; Pant, A.; Henry, A.; Maple-Brown, L.J.; Moran, L.; Cheung, N.W.; Chow, C.K.; Zaman, S. Cardiovascular risk management following gestational diabetes and hypertensive disorders of pregnancy: A narrative review. Med. J. Aust. 2023, 218, 484–491. [Google Scholar] [CrossRef]
- Wu, P.; Park, K.; Gulati, M. The fourth trimester: Pregnancy as a predictor of cardiovascular disease. Eur. Cardiol. Rev. 2021, 16, e31. [Google Scholar] [CrossRef]
- Marshall, N.E.; Abrams, B.; Barbour, L.A.; Catalano, P.; Christian, P.; Friedman, J.E.; Hay, W.W.; Hernandez, T.L.; Krebs, N.F.; Oken, E.; et al. The importance of nutrition in pregnancy and lactation: Lifelong consequences. Am. J. Obstet. Gynecol. 2021, 226, 607–632. [Google Scholar] [CrossRef]
- Panaitescu, A.M.; Popescu, M.R.; Ciobanu, A.M.; Gica, N.; Cimpoca-Raptis, B.A. Pregnancy Complications Can Foreshadow Future Disease—Long-Term Outcomes of a Complicated Pregnancy. Medicina 2021, 57, 1320. [Google Scholar] [CrossRef]
- McNestry, C.; Killeen, S.L.; Crowley, R.K.; McAuliffe, F.M. Pregnancy complications and later life women’s health. Acta Obstet. Gynecol. Scand. 2023, 102, 523–531. [Google Scholar] [CrossRef]
- Middleton, P.; Gomersall, J.C.; Gould, J.F.; Shepherd, E.; Olsen, S.F.; Makrides, M. Omega-3 fatty acid addition during pregnancy. Cochrane Database Syst. Rev. 2018, 11, CD003402. [Google Scholar] [CrossRef]
- Irwinda, R.; Hiksas, R.; Siregar, A.A.; Saroyo, Y.B.; Wibowo, N. Long-chain polyunsaturated fatty acid (LC-PUFA) status in severe preeclampsia and preterm birth: A cross sectional study. Sci. Rep. 2021, 11, 14701. [Google Scholar] [CrossRef]
- Godhamgaonkar, A.A.; Wadhwani, N.S.; Joshi, S.R. Exploring the role of LC-PUFA metabolism in pregnancy complications. Prostaglandins Leukot. Essent. Fat. Acids 2020, 163, 102203. [Google Scholar] [CrossRef]
- Traylor, C.S.; Johnson, J.D.; Kimmel, M.C.; Manuck, T.A. Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: An expert review. Am. J. Obstet. Gynecol. MFM 2020, 2, 100229. [Google Scholar] [CrossRef]
- Coussons-Read, M.E. Effects of prenatal stress on pregnancy and human development: Mechanisms and pathways. Obstet. Med. 2013, 6, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Marschner, S.; Mukherjee, S.; Watts, M.; Min, H.; Beale, A.L.; O’Brien, J.; Juneja, A.; Tremmel, J.A.; Zaman, S. Prevention of Cardiovascular Disease in Women With Pregnancy-Related Risk Factors: A Prospective Women’s Heart Clinic Study. J. Am. Heart Assoc. 2023, 12, e030015. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xia, M.; Weng, S.; Wang, C.; Yuan, P.; Tang, S. Effect of Mediterranean diet for pregnant women: A meta-analysis of randomized controlled trials. J. Matern. Neonatal Med. 2021, 35, 4824–4829. [Google Scholar] [CrossRef]
- Al Wattar, B.H.; Dodds, J.; Placzek, A.; Beresford, L.; Spyreli, E.; Moore, A.; Carreras, F.J.G.; Austin, F.; Murugesu, N.; Roseboom, T.J.; et al. Mediterranean-style diet in pregnant women with metabolic risk factors (ESTEEM): A pragmatic multicentre randomised trial. PLoS Med. 2019, 16, e1002857. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Chen, J.-L.; Whittemore, R.; Whitaker, E. Postpartum Lifestyle Interventions to Prevent Type 2 Diabetes Among Women with History of Gestational Diabetes: A Systematic Review of Randomized Clinical Trials. J. Women’s Health 2016, 25, 38–49. [Google Scholar] [CrossRef]
- Macphail, M.G.; Juul, S.; Wollny, K.; Negre, J.Y.; Metcalfe, A.; Chaput, K.H.; Butalia, S.; Nerenberg, K.A. Nutrition Interventions for Lowering Cardiovascular Risk After Hypertensive Disorders of Pregnancy: A Systematic Review. CJC Open 2023. [Google Scholar] [CrossRef]
- Angum, F.; Khan, T.; Kaler, J.; Siddiqui, L.; Hussain, A. The Prevalence of Autoimmune Disorders in Women: A Narrative Review. Cureus 2020, 12, e8094. [Google Scholar] [CrossRef] [PubMed]
- Schurz, H.; Salie, M.; Tromp, G.; Hoal, E.G.; Kinnear, C.J.; Möller, M. The X chromosome and sex-specific effects in infectious disease susceptibility. Hum. Genom. 2019, 13, 2. [Google Scholar] [CrossRef]
- Forsyth, C.; Kouvari, M.; D’cunha, N.M.; Georgousopoulou, E.N.; Panagiotakos, D.B.; Mellor, D.D.; Kellett, J.; Naumovski, N. The effects of the Mediterranean diet on rheumatoid arthritis prevention and treatment: A systematic review of human prospective studies. Rheumatol. Int. 2017, 38, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Smedslund, G.; Byfuglien, M.G.; Olsen, S.U.; Hagen, K.B. Effectiveness and Safety of Dietary Interventions for Rheumatoid Arthritis: A Systematic Review of Randomized Controlled Trials. J. Am. Diet. Assoc. 2010, 110, 727–735. [Google Scholar] [CrossRef]
- McKellar, G.; Morrison, E.; McEntegart, A.; Hampson, R.; Tierney, A.; Mackle, G.; Scoular, J.; A Scott, J.; A Capell, H. A pilot study of a Mediterranean-type diet intervention in female patients with rheumatoid arthritis living in areas of social deprivation in Glasgow. Ann. Rheum. Dis. 2007, 66, 1239–1243. [Google Scholar] [CrossRef] [PubMed]
- Gavilán-Carrera, B.; Ruiz-Cobo, A.; Amaro-Gahete, F.J.; Soriano-Maldonado, A.; Vargas-Hitos, J.A. No Changes in Body Composition and Adherence to the Mediterranean Diet after a 12-Week Aerobic Training Intervention in Women with Systemic Lupus Erythematosus: The EJERCITA-LES Study. Nutrients 2023, 15, 4424. [Google Scholar] [CrossRef] [PubMed]
| Diet | Foods | Cardio-Protective Properties | Cardiovascular Benefits | Comparative Studies with MD | Results: MD vs. Comparator Diet |
|---|---|---|---|---|---|
| LF | Vegetables, fruits, whole grains, legumes, lean meats, seafood/fish, low-fat dairy <30% fat intake of total energy | Lipid-lowering effects on total and LDL cholesterol levels | Weight loss Better lipid profile Lower risk of CVD | Estruch et al., 2018 [31], Spain (RCT) Delgado-Lista et al., 2022 [32], Spain (RCT) Nordmann et al., 2011 [33], (SR) | Adherence to MD vs. LF led to: Lower incidence of MACE Greater changes in body weight and BMI Greater reductions in DBP and SBP Greater reductions in inflammatory marker hs-CRP |
| DASH | Vegetables, fruits, whole grains, legumes, low-fat dairy, and nuts Limit intake of cholesterol, total/saturated fat, and red/processed meats Limited added sugars Sodium intake restricted to 1500 mg/d | High in dietary fibre and protein Increased intake of minerals associated with reducing BP, like potassium and magnesium | Reduced SBP and DBP Better lipid profile Lower risk of CVD and T2DM | Critselis et al., 2021 [34], Greece (Prospective cohort) Bertoia et al., 2014 [35], US (Prospective cohort) Panbehkar-Jouybari et al., 2021 [36], Iran (Cross-sectional) Jalilipiran et al., 2020 [37], Iran (Cross-sectional) | Only the MD was associated with reduced CVD risk and sudden cardiac death The DASH diet led to lower levels of total cholesterol, triglycerides, LDL-C, HDL-C, and LDL/HDL ratio; the MD only improved LDL/HDL ratio The DASH diet improved insulin, hs-CRP, fibrinogen levels, and DBP, while the MD only improved DBP and fibrinogen levels |
| Plant-based (Vegetarian/Vegan) | Excludes meat and meat products, poultry, and fish/seafood Variety of plant foods, such as fruits, vegetables, legumes, and whole grains | High in dietary fibre; phytochemicals; antioxidants; and minerals such as magnesium, folic acid, and vitamin C Low in cholesterol and total fat | Lipid-lowering effect Lower BP Reduced BMI levels Lower incidence of CVD | Sofi et al., 2018 [38], Italy (RCT) Rogerson et al., 2018 [39], UK (RCT) Barnard et al., 2020 [40], US (Cross-sectional RCT) | Both the MD and the vegetarian diet led to significant reductions in BMI, fat mass, and body weight, and there were no significant group differences between the two diets The MD was more beneficial to vasodilatory ability and NO levels than the vegan diet The vegan diet led to greater improvements in body weight, insulin sensitivity, and lipid concentrations than the MD The MD led to greater improvements in BP |
| Nordic | Vegetables and fruits (mainly root vegetables, apples/pears, and berries), whole grains (e.g., rye, barley), seafood/fish, and use of rapeseed oil | Higher in dietary fibre, phytochemicals, antioxidants, and monounsaturated fats | Decrease in body weight and DBP Improved lipid profile Lower incidence of CVD and stroke | Bonaccio et al., 2021 [41], Italy (prospective cohort) Galbete et al., 2018 [42], Germany (prospective cohort) Li et al, 2015 [43], Sweden, (prospective cohort) | The MD lowered the risk of all-cause mortality and T2DM, but the Nordic diet showed no significance for either outcome |
| Japanese-style diets | Fruit, vegetables, legumes (mainly soybean/soy products), rice bran oil as the primary source of fat, fermented foods such as miso soup and pickles, seafood, seaweed, and rice Lower in animal protein, particularly red meat | Lower in total fat Increased flavonoids and dietary fibre | Decrease in BP, body weight, and BMI Improved LDL and HDL cholesterol levels Lower incidence of CVD and stroke mortality | N/R | N/R |
| Author, Year, Country | Study Design | Population | Sample Size | Study Duration/ Follow-Up | Intervention/ Exposure | Comparator | Outcome | Result: MD vs. Comparator | |
|---|---|---|---|---|---|---|---|---|---|
| N | % Female | ||||||||
| CVD | |||||||||
| Fung et al., 2009 [70] (NHS I), US | Prospective cohort | Healthy female nurses without history of CVD (aged 38–63 years) | 74,886 | 100% | 20 years (maximum) | Higher MD adherence, assessed by an Alternate MDS | Lower MD adherence | CHD Stroke | Higher MD adherence led to: Lower CHD incidence, RR = 0.71 (95% CI 0.62–0.82) Lower stroke incidence, RR = 0.87 (95% CI 0.73–1.02) |
| Estruch et al., 2018 [31] (PREDIMED), Spain | RCT | Participants without CVD (aged 55–80 years) | 7447 | 57% | Median follow-up of 4.3 years | MD with EVOO or nuts | Low-fat | MACE (defined as myocardial infarction, stroke, or death from cardiovascular causes) | Exposure to the two MD groups combined led to: Lower risk of MACE in men only (HR = 0.69 (95% CI 0.51–0.94)), but not in women (HR = 0.73 (95% CI 0.50–1.07)) No sex interaction = p = 0.62 |
| Delgado-Lista et al., 2020 [32] (CORDIOPREV), Spain | RCT | Patients with CHD (aged 20–75 years) | 1002 | 17.5% | 7 years follow-up | MD rich in olive oil | Low-fat | MACE | Higher MD adherence led to: Lower MACE risk for men (HR = 0.68 (95% CI 0.50–0.94)) but not for women (HR = 1.27 (95% CI 0.64–2.49)). Sex interaction: p = 0.03 |
| Rosato et al., 2019 [10] | SR of 29 observational studies | Participants without CVD (aged ≥18 years) | N/A | N/A | N/A | Higher MD adherence, assessed using MDS | Lower MD adherence | Overall CVD | Higher MD adherence led to: Lower CVD risk for women (RR = 0.85 (95% CI 0.72–0.98)) and men (RR = 0.85 (95% CI 0.72–0.98)) |
| Pant et al., 2023 [11] | SR of 16 prospective cohort studies | Participants without CVD (aged ≥18 years) | 722,495 | 100% | Median follow-up of 12.5 years | Higher MD adherence, assessed using MDS | Lower MD adherence | Incident CVD Total mortality | Higher MD adherence led to: Lower CVD incidence in women: HR = 0.76 (95% CI 0.72 to 0.81) Total mortality HR = 0.77 (95% CI 0.74 to 0.80) Lower CVD incidence in men HR = 0.78 (95% CI 0.72 to 0.83) Total mortality HR = 0.77 (95% CI 0.75 to 0.79) |
| Tang et al., 2021 [23] | SR of 7 cohort studies | Participants with history of CVD | 37,879 | N/A | Between 3.8 to 10.0 years | Higher MD adherence, assessed using MDS | Lower MD adherence | Total mortality | Women: no significant effect (HR = 0.97 (95% CI 0.92–1.02)) Men: inverse association with total mortality (HR = 0.94 (95% CI 0.90–0.98)) |
| Traditional cardiovascular risk factors | |||||||||
| Esposito et al., 2003 [71], Italy | RCT | Premenopausal women with obesity (aged 20–46 years) | 120 | 100% | 2 years | MD intervention: education on dietary calories, personal goal setting, and self-monitoring | Usual care | Anthropometric parameters, BP Insulin sensitivity Lipid profile Inflammatory markers | In the MD group, significant reductions in body weight, BMI, SBP/DBP, glucose, insulin and HOMA, triglycerides, and FFA. HDL-C was increased more significantly in the intervention. Serum concentrations of interleukins 6 and 18 and hs-CRP were significantly reduced. |
| Toobert et al., 2003 [72], US | RCT | Postmenopausal women with T2DM (aged >30 years) | 279 | 100% | 6 months | Mediterranean lifestyle program: MD, stress management, exercise, and smoking cessation | Usual care | HbA1c Lipid profile BMI BP Plasma fatty acids | In the MLP group, significant improvements were observed for HbA1c, BMI, plasma fatty acids, and quality of life at the 6-month follow-up |
| Storniolo et al., 2017 [73], Spain (PREDIMED) | RCT | Women with moderate hypertension (aged 60–80 years) | 90 | 100% | 1 year | MD with EVOO or nuts | Low-fat | Endothelial markers: nitric oxide and endothelial-1 | Improvements in endothelial markers for both the MD interventions, but not the low-fat diet |
| Dunn et al., 2014 [74], Australia | RCT | Premenopausal women who were overweight (mean age 22 ± 0.8 years) | 30 | 100% | 12 weeks | Combined lifestyle intervention: high-intensity intermittent exercise, MD, and fish oil | Usual care | Anthropometric parameters Insulin resistance Inflammatory markers Blood pressure | In the MD-integrated lifestyle intervention, significant reductions in BMI, abdominal adiposity, waist circumference, SBP, fasting insulin, triglycerides and interleukin-6. |
| Buscemi et al., 2009 [75], Italy | RCT | Healthy women who were overweight/obese (aged 30–55 years) | 20 | 100% | 2 months | Mediterranean hypocaloric diet (group M) | Atkins low-carbohydrate diet (group A) | Endothelial function assessed by flow-mediated dilation Metabolic parameters Lipid profile | At follow-up, Group M had significantly greater reductions in SBP. More significant weight loss in Group A than Group M No group significance for endothelial function |
| Bajerska et al., 2018 [76], Finland | RCT | Postmenopausal women with central obesity | 144 | 100% | 16 weeks | MD | Central European diet | Body weight Visceral fat loss | Similar improvements in both groups, with group significance only for visceral fat in women consuming the Central European diet. |
| Bedard et al., 2012 [57], Canada | RCT | Men and premenopausal women (aged 25–50 years) | 70 | 45.7% | 4 weeks | Isoenergetic MD | N/A | Cardiometabolic parameters | Total cholesterol, LDL-C, and diastolic BP significantly decreased in both. Only men had significantly improved insulin homeostasis and SBP. More significant effects on body weight, BMI, and 2 h postload insulin were found in men |
| Jennings et al., 2009 [77], 5 recruitment centres in Europe: Italy, Netherlands, Poland, France, United Kingdom | RCT | Men and women aged 65–79 years | 1294 | 48.3% | 1 year | MD group received tailored standardised dietary advice administered 9 times (via telephone/in person) | Usual care | BP measurements Arterial stiffness assessed by pulse wave velocity | Significant reduction in SBP in males, but not females. Significant improvements in atrial stiffness in females, but not males. Significant interaction with sex and SBP. |
| Ahmad et al., 2020 [78], US | Prospective cohort study | Healthy women without baseline diabetes (mean age: 52.9 ± 9.9 years) | 25,317 | 100% | Mean 19.8 years | Higher MD adherence, assessed by the Alternate MD | Lower MD adherence | T2DM | Lower risk of T2DM in the higher MD adherence group: HR = 0.85 (95% CI, 0.76–0.96) |
| Salas-Salvado et al., 2011 (corrected in 2018) [79], Spain (PREDIMED) | RCT | Non-diabetic men and women (aged 55–80) years | 418 | 58.4% | Median 4.0 years | MD with EVOO or nuts | Low-fat | T2DM | Lower risk of T2DM only for female participants consuming the MD: MD with nuts vs. control Male: HR = 0.65 (95% CI, 0.21–2.00) Female: HR = 0.32 (95% CI 0.11–0.93) Both MD groups vs. control: Male: HR = 0.55 (95% CI 0.21–1.43) Female: HR = 0.40 (95% CI 0.18–0.90) |
| PCOS | |||||||||
| Mei et al., 2022 [80], China | RCT | Patients with PCOS who were overweight (aged 16–45 years) | 72 | 100% | 12 weeks | Low-carbohydrate MD | Low-fat | Anthropometric parameters, insulin resistance, and lipids | In the MD group, significant reductions in weight, BMI, body fat percentage, and HOMA-IR were found. Significant differences in total cholesterol, triglycerides, and LDL-C were observed in the low-fat group. |
| Cincione et al. [81], 2022, US | RCT | Women with PCOS who were overweight/ obese (aged 18–45 years) | 144 | 100% | 45 days | MD | Ketogenic diet | Anthropometric parameters | Significant reductions in all parameters in the ketogenic group compared to the MD group. |
| Pregnancy-related complications | |||||||||
| Perez-Ferre et al., 2014 [82], Spain | RCT | Women with past GDM 6 to 12 weeks postpartum | 260 | 100% | 3 weeks | Mediterranean lifestyle intervention on nutrition and physical activity | Control | Glucose disorders of impaired fasting glucose, impaired glucose tolerance, or DM2 | The MD-integrated lifestyle program led to a reduction in all glucose disorders. |
| Reimer et al., 2021 [83], Germany | Prospective RCT | Women with past HDP 6-weeks postpartum | 38 | 100% | 6 months | MD and cardiovascular exercise program | Control | Arterial stiffness measured by pulse wave velocity | Significant reduction in arterial stiffness in the intervention group compared to control |
| Crovetto et al, 2020 [84], Spain Casas et al, 2023 [85], Spain | Parallel-group RCT | Pregnant individuals at 19–23 weeks’ gestation | 1221 | 100% | 34–36 weeks | MD group OR 8-week stress reduction program adapted for pregnancy | Usual care | Incidence of SGA maternal stress, well-being, and sleep quality | Significantly lower rates of SGA babies after delivery in both the MD and the stress reduction group Significantly lower maternal stress, anxiety, and sleep quality in the MD group than usual care |
| Inflammatory autoimmune diseases | |||||||||
| McKellar et al., 2007 [86], Scotland | Pilot RCT | Patients with RA (aged 30–70 years) | 130 | 100% | 6 weeks | Nutritional information on the Mediterranean-style diet provided in weekly 2 h sessions | Dietary written information only | Pain score Early morning stiffness SBP | Improvements in pain scores at 3 months and 6 months, early-morning stiffness at 6 months, and significant improvements in SBP in the intervention group only. |
| Papandreou et al., 2023 [87], Greece | RCT | Women with RA in remission (mean age 34.03 ± 5.45 years) | 40 | 100% | 12-week | Isocaloric MD plan with lifestyle consultations on physical activity | Control | Disease activity Anthropometric parameters Blood lipids | Greater improvements in the MD group than the control for body weight, body composition, blood glucose, and lower disease activity. |
| Pocovi-Gerardino et al., 2021 [88], Spain | Cross-sectional study | Patients with SLE (mean age: 46.9 ± 12.85 years) | 280 | 90.4% | N/A | Higher MD adherence | Lower MD adherence | Anthropometric parameters, disease activity, inflammatory markers, cardiovascular risk factors | Patients consuming higher versus lower MD intake had significantly lower fat mass percentage, BMI, and triglycerides. Higher MD adherence was associated with less damage and disease activity. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pant, A.; Chew, D.P.; Mamas, M.A.; Zaman, S. Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses. Nutrients 2024, 16, 570. https://doi.org/10.3390/nu16040570
Pant A, Chew DP, Mamas MA, Zaman S. Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses. Nutrients. 2024; 16(4):570. https://doi.org/10.3390/nu16040570
Chicago/Turabian StylePant, Anushriya, Derek P. Chew, Mamas A. Mamas, and Sarah Zaman. 2024. "Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses" Nutrients 16, no. 4: 570. https://doi.org/10.3390/nu16040570
APA StylePant, A., Chew, D. P., Mamas, M. A., & Zaman, S. (2024). Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses. Nutrients, 16(4), 570. https://doi.org/10.3390/nu16040570





