Malnutrition–Inflammation Score of Patients with Chronic Kidney Disease from Early Stage to Initiation of Dialysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Data Collection
2.3. Cardiometabolic Syndrome
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Patients with CKD Stages 1–5
3.2. Malnutrition–Inflammation Across CKD Stages
3.3. Factors Associated with Baseline MIS
3.4. Longitudinal Study of Patients Developing ESRD
3.5. Factors Associated with Pre-Dialysis MIS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76 (Suppl. S1), S1–S107. [Google Scholar] [CrossRef] [PubMed]
- Obi, Y.; Qader, H.; Kovesdy, C.P.; Kalantar-Zadeh, K. Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Tinti, F.; Lai, S.; Noce, A.; Rotondi, S.; Marrone, G.; Mazzaferro, S.; Di Daniele, N.; Mitterhofer, A.P. Chronic Kidney Disease as a Systemic Inflammatory Syndrome: Update on Mechanisms Involved and Potential Treatment. Life 2021, 11, 419. [Google Scholar] [CrossRef]
- Ikizler, T.A.; Cano, N.J.; Franch, H.; Fouque, D.; Himmelfarb, J.; Kalantar-Zadeh, K.; Kuhlmann, M.K.; Stenvinkel, P.; TerWee, P.; Teta, D.; et al. Prevention and treatment of protein energy wasting in chronic kidney disease patients: A consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013, 84, 1096–1107. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Jafar, T.H.; Nitsch, D.; Neuen, B.L.; Perkovic, V. Chronic kidney disease. Lancet 2021, 398, 786–802. [Google Scholar] [CrossRef]
- Amparo, F.C.; Kamimura, M.A.; Molnar, M.Z.; Cuppari, L.; Lindholm, B.; Amodeo, C.; Carrero, J.J.; Cordeiro, A.C. Diagnostic validation and prognostic significance of the Malnutrition-Inflammation Score in nondialyzed chronic kidney disease patients. Nephrol. Dial. Transpl. 2015, 30, 821–828. [Google Scholar] [CrossRef]
- Dai, L.; Mukai, H.; Lindholm, B.; Heimburger, O.; Barany, P.; Stenvinkel, P.; Qureshi, A.R. Clinical global assessment of nutritional status as predictor of mortality in chronic kidney disease patients. PLoS ONE 2017, 12, e0186659. [Google Scholar] [CrossRef]
- Perez-Torres, A.; Gonzalez Garcia, M.E.; San Jose-Valiente, B.; Bajo Rubio, M.A.; Celadilla Diez, O.; Lopez-Sobaler, A.M.; Selgas, R. Protein-energy wasting syndrome in advanced chronic kidney disease: Prevalence and specific clinical characteristics. Nefrol. Engl. Ed. 2018, 38, 141–151. [Google Scholar] [CrossRef]
- Carrero, J.J.; Thomas, F.; Nagy, K.; Arogundade, F.; Avesani, C.M.; Chan, M.; Chmielewski, M.; Cordeiro, A.C.; Espinosa-Cuevas, A.; Fiaccadori, E.; et al. Global Prevalence of Protein-Energy Wasting in Kidney Disease: A Meta-analysis of Contemporary Observational Studies From the International Society of Renal Nutrition and Metabolism. J. Ren. Nutr. 2018, 28, 380–392. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Liao, C.-T.; Lin, M.-Y.; Lin, M.-H.; Chen, Y.-W.; Zheng, C.-M.; Lin, Y.-C.; Wu, M.-Y.; Chiu, Y.-W.; Hwang, S.-J.; et al. Summary of the 2021 Annual Report on Kidney Disease in Taiwan. Acta Nephrol. 2022, 36, 169–179. [Google Scholar] [CrossRef]
- Kovesdy, C.P.; Kopple, J.D.; Kalantar-Zadeh, K. Management of protein-energy wasting in non-dialysis-dependent chronic kidney disease: Reconciling low protein intake with nutritional therapy. Am. J. Clin. Nutr. 2013, 97, 1163–1177. [Google Scholar] [CrossRef] [PubMed]
- Carrero, J.J.; Stenvinkel, P.; Cuppari, L.; Ikizler, T.A.; Kalantar-Zadeh, K.; Kaysen, G.; Mitch, W.E.; Price, S.R.; Wanner, C.; Wang, A.Y.; et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: A consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J. Ren. Nutr. 2013, 23, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Amparo, F.C.; Cordeiro, A.C.; Carrero, J.J.; Cuppari, L.; Lindholm, B.; Amodeo, C.; Kamimura, M.A. Malnutrition-inflammation score is associated with handgrip strength in nondialysis-dependent chronic kidney disease patients. J. Ren. Nutr. 2013, 23, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Jagadeswaran, D.; Indhumathi, E.; Hemamalini, A.J.; Sivakumar, V.; Soundararajan, P.; Jayakumar, M. Inflammation and nutritional status assessment by malnutrition inflammation score and its outcome in pre-dialysis chronic kidney disease patients. Clin. Nutr. 2019, 38, 341–347. [Google Scholar] [CrossRef]
- Reber, E.; Gomes, F.; Vasiloglou, M.F.; Schuetz, P.; Stanga, Z. Nutritional Risk Screening and Assessment. J. Clin. Med. 2019, 8, 1065. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Kopple, J.D.; Block, G.; Humphreys, M.H. A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am. J. Kidney Dis. 2001, 38, 1251–1263. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Moore, L.W. Renal Telenutrition for Kidney Health: Leveraging Telehealth and Telemedicine for Nutritional Assessment and Dietary Management of Patients With Kidney Disorders. J. Ren. Nutr. 2020, 30, 471–474. [Google Scholar] [CrossRef]
- Sa Martins, V.; Adragao, T.; Aguiar, L.; Pinto, I.; Dias, C.; Figueiredo, R.; Lourenco, P.; Pascoal, T.; Pereira, J.; Pinheiro, T.; et al. Prognostic Value of the Malnutrition-inflammation Score in Hospitalization and Mortality on Long-term Hemodialysis. J. Ren. Nutr. 2022, 32, 569–577. [Google Scholar] [CrossRef]
- Rambod, M.; Bross, R.; Zitterkoph, J.; Benner, D.; Pithia, J.; Colman, S.; Kovesdy, C.P.; Kopple, J.D.; Kalantar-Zadeh, K. Association of Malnutrition-Inflammation Score with quality of life and mortality in hemodialysis patients: A 5-year prospective cohort study. Am. J. Kidney Dis. 2009, 53, 298–309. [Google Scholar] [CrossRef]
- Kopple, J.D.; Greene, T.; Chumlea, W.C.; Hollinger, D.; Maroni, B.J.; Merrill, D.; Scherch, L.K.; Schulman, G.; Wang, S.R.; Zimmer, G.S. Relationship between nutritional status and the glomerular filtration rate: Results from the MDRD study. Kidney Int. 2000, 57, 1688–1703. [Google Scholar] [CrossRef]
- Kovesdy, C.P.; George, S.M.; Anderson, J.E.; Kalantar-Zadeh, K. Outcome predictability of biomarkers of protein-energy wasting and inflammation in moderate and advanced chronic kidney disease. Am. J. Clin. Nutr. 2009, 90, 407–414. [Google Scholar] [CrossRef] [PubMed]
- National Kidney, F. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 39 (Suppl. S1), S1–S266. [Google Scholar]
- Frere, J.J.; tenOever, B.R. Cardiometabolic syndrome—An emergent feature of Long COVID? Nat. Rev. Immunol. 2022, 22, 399–400. [Google Scholar] [CrossRef] [PubMed]
- Castro, J.P.; El-Atat, F.A.; McFarlane, S.I.; Aneja, A.; Sowers, J.R. Cardiometabolic syndrome: Pathophysiology and treatment. Curr. Hypertens. Rep. 2003, 5, 393–401. [Google Scholar] [CrossRef]
- Harris, D.C.; Chen, Y.M.; Saito, A.; Yu, A.W. Timely initiation of dialysis for chronic kidney disease: Perspective from four Asian countries. Nephrology 2010, 15 (Suppl. S2), 61–65. [Google Scholar] [CrossRef]
- de Mutsert, R.; Grootendorst, D.C.; Axelsson, J.; Boeschoten, E.W.; Krediet, R.T.; Dekker, F.W.; Group, N.S. Excess mortality due to interaction between protein-energy wasting, inflammation and cardiovascular disease in chronic dialysis patients. Nephrol. Dial. Transpl. 2008, 23, 2957–2964. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Ikizler, T.A.; Block, G.; Avram, M.M.; Kopple, J.D. Malnutrition-inflammation complex syndrome in dialysis patients: Causes and consequences. Am. J. Kidney Dis. 2003, 42, 864–881. [Google Scholar] [CrossRef]
- Campbell, K.L.; Ash, S.; Bauer, J.D.; Davies, P.S. Evaluation of nutrition assessment tools compared with body cell mass for the assessment of malnutrition in chronic kidney disease. J. Ren. Nutr. 2007, 17, 189–195. [Google Scholar] [CrossRef]
- Liyanage, T.; Toyama, T.; Hockham, C.; Ninomiya, T.; Perkovic, V.; Woodward, M.; Fukagawa, M.; Matsushita, K.; Praditpornsilpa, K.; Hooi, L.S.; et al. Prevalence of chronic kidney disease in Asia: A systematic review and analysis. BMJ Glob. Health 2022, 7, e007525. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Joshi, S.; Schlueter, R.; Cooke, J.; Brown-Tortorici, A.; Donnelly, M.; Schulman, S.; Lau, W.L.; Rhee, C.M.; Streja, E.; et al. Plant-Dominant Low-Protein Diet for Conservative Management of Chronic Kidney Disease. Nutrients 2020, 12, 1931. [Google Scholar] [CrossRef]
- Marini, H.R. Mediterranean Diet and Soy Isoflavones for Integrated Management of the Menopausal Metabolic Syndrome. Nutrients 2022, 14, 1550. [Google Scholar] [CrossRef] [PubMed]
- de Roij van Zuijdewijn, C.L.; ter Wee, P.M.; Chapdelaine, I.; Bots, M.L.; Blankestijn, P.J.; van den Dorpel, M.A.; Nube, M.J.; Grooteman, M.P. A Comparison of 8 Nutrition-Related Tests to Predict Mortality in Hemodialysis Patients. J. Ren. Nutr. 2015, 25, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Perez Vogt, B.; Costa Teixeira Caramori, J. Are Nutritional Composed Scoring Systems and Protein-Energy Wasting Score Associated With Mortality in Maintenance Hemodialysis Patients? J. Ren. Nutr. 2016, 26, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Chiang, H.P.; Chiu, Y.W.; Lee, J.J.; Hung, C.C.; Hwang, S.J.; Chen, H.C. Blood pressure modifies outcomes in patients with stage 3 to 5 chronic kidney disease. Kidney Int. 2020, 97, 402–413. [Google Scholar] [CrossRef]
- Borges, M.C.; Vogt, B.P.; Martin, L.C.; Caramori, J.C. Malnutrition Inflammation Score cut-off predicting mortality in maintenance hemodialysis patients. Clin. Nutr. ESPEN 2017, 17, 63–67. [Google Scholar] [CrossRef]
- National Institutes of Health. USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health: Bethesda, MD, USA, 2022.
- Otten, L.; Stobaus, N.; Franz, K.; Genton, L.; Muller-Werdan, U.; Wirth, R.; Norman, K. Impact of sarcopenia on 1-year mortality in older patients with cancer. Age Ageing 2019, 48, 413–418. [Google Scholar] [CrossRef]
- Cunha, A.I.L.; Veronese, N.; de Melo Borges, S.; Ricci, N.A. Frailty as a predictor of adverse outcomes in hospitalized older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2019, 56, 100960. [Google Scholar] [CrossRef]
- De Nicola, L.; Donfrancesco, C.; Minutolo, R.; Lo Noce, C.; Palmieri, L.; De Curtis, A.; Iacoviello, L.; Zoccali, C.; Gesualdo, L.; Conte, G.; et al. Prevalence and cardiovascular risk profile of chronic kidney disease in Italy: Results of the 2008-12 National Health Examination Survey. Nephrol. Dial. Transpl. 2015, 30, 806–814. [Google Scholar] [CrossRef]
- Sze, S.; Pellicori, P.; Kazmi, S.; Rigby, A.; Cleland, J.G.F.; Wong, K.; Clark, A.L. Prevalence and Prognostic Significance of Malnutrition Using 3 Scoring Systems Among Outpatients With Heart Failure: A Comparison With Body Mass Index. JACC Heart Fail 2018, 6, 476–486. [Google Scholar] [CrossRef]
- Raposeiras Roubin, S.; Abu Assi, E.; Cespon Fernandez, M.; Barreiro Pardal, C.; Lizancos Castro, A.; Parada, J.A.; Perez, D.D.; Blanco Prieto, S.; Rossello, X.; Ibanez, B.; et al. Prevalence and Prognostic Significance of Malnutrition in Patients With Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2020, 76, 828–840. [Google Scholar] [CrossRef]
- Rodin, R.; Chan, C.T. Determinants and Prevention of Coronary Disease in Patients With Chronic Kidney Disease. Can. J. Cardiol. 2019, 35, 1181–1187. [Google Scholar] [CrossRef]

| Variable | CKD Stage | p Value | |||
|---|---|---|---|---|---|
| 1 + 2 | 3 | 4 | 5 | ||
| No. of patients | 356 (9.7%) | 1183 (32.3%) | 961 (26.3%) | 1159 (31.7%) | <0.001 |
| Age (year) | 51.8 (15.8) | 63.5 (13.3) | 65.0 (13.8) | 62.1 (13.4) | <0.001 |
| Sex (female) | 143 (40.2%) | 309 (26.1%) | 447 (46.5%) | 638 (55.0%) | <0.001 |
| Comorbidity | |||||
| Cardiovascular disease | 29 (8.1%) | 256 (21.6%) | 268 (27.9%) | 337 (29.1%) | <0.001 |
| Diabetes mellitus | 148 (41.6%) | 558 (47.2%) | 524 (54.5%) | 578 (49.9%) | <0.001 |
| Hypertension | 179 (50.3%) | 695 (58.7%) | 639 (66.5%) | 850 (73.3%) | <0.001 |
| Severe liver disease | 16 (4.5%) | 55 (4.6%) | 51 (5.3%) | 56 (4.8%) | 0.888 |
| Cancer | 20 (5.6%) | 79 (6.7%) | 91 (9.5%) | 123 (10.6%) | <0.001 |
| Charlson score | 2.4 (1.7) | 3.3 (2.0) | 3.7 (2.1) | 3.6 (2.1) | <0.001 |
| Mean BP (mmHg) | 99.0 (13.1) | 99.3 (13.2) | 99.6 (13.9) | 100.9 (14.2) | 0.017 |
| Laboratory data | |||||
| eGFR (mL/min/1.73 m2) | 77.8 (68.0–95.8) | 41.1 (35.2–47.8) | 22.2 (18.4–26.0) | 8.9 (6.5–11.7) | <0.001 |
| UPCR (mg/g) | 660(147–2547) | 397(69–1071) | 1218(540–2731) | 1903(1088–4035) | <0.001 |
| Hba1c (%) | 6.5 (1.6) | 6.8 (2.0) | 6.6 (1.6) | 6.7 (1.8) | <0.001 |
| WBC (×1000/uL) | 7.2 (2.3) | 7.1 (2.4) | 7.1 (2.2) | 7.4 (2.3) | 0.008 |
| Hemoglobin (g/dL) | 13.8 (2.0) | 12.8 (2.0) | 10.8 (1.8) | 9.1 (1.4) | <0.001 |
| Total cholesterol (mg/d) | 205 (173–239) | 192 (165–221) | 192 (165–225) | 188 (156–217) | <0.001 |
| Triglyceride (mg/dL) | 127 (82–189) | 124 (89–186) | 132 (98–194) | 123 (87–176) | <0.001 |
| Phosphorus (mg/dL) | 3.7 (0.8) | 3.7 (0.7) | 4.2 (0.9) | 5.4 (1.4) | <0.001 |
| Calcium (mg/dL) | 9.3 (0.6) | 9.3 (0.6) | 9.1 (0.7) | 8.8 (0.9) | <0.001 |
| Malnutrition–inflammation | |||||
| Albumin (g/dL) | 3.9 (0.7) | 4.0 (0.5) | 3.8 (0.5) | 3.7 (0.5) | <0.001 |
| Body mass index (kg/m2) | 24.8 (4.0) | 25.4 (4.5) | 25.1 (3.7) | 25.0 (4.2) | <0.001 |
| Muscle mass index(kg/m2) | 3.3 (0.5) | 3.4 (0.6) | 3.4 (0.4) | 3.3 (0.5) | 0.005 |
| C-reactive protein (mg/L) | 0.8 (0.2–4.9) | 0.9 (0.3–3.6) | 1.3 (0.5–5.5) | 1.5 (0.5–7.0) | <0.001 |
| MIS | 3.7 (2.8) | 3.3 (2.6) | 4.5 (3.1) | 5.7 (3.4) | <0.001 |
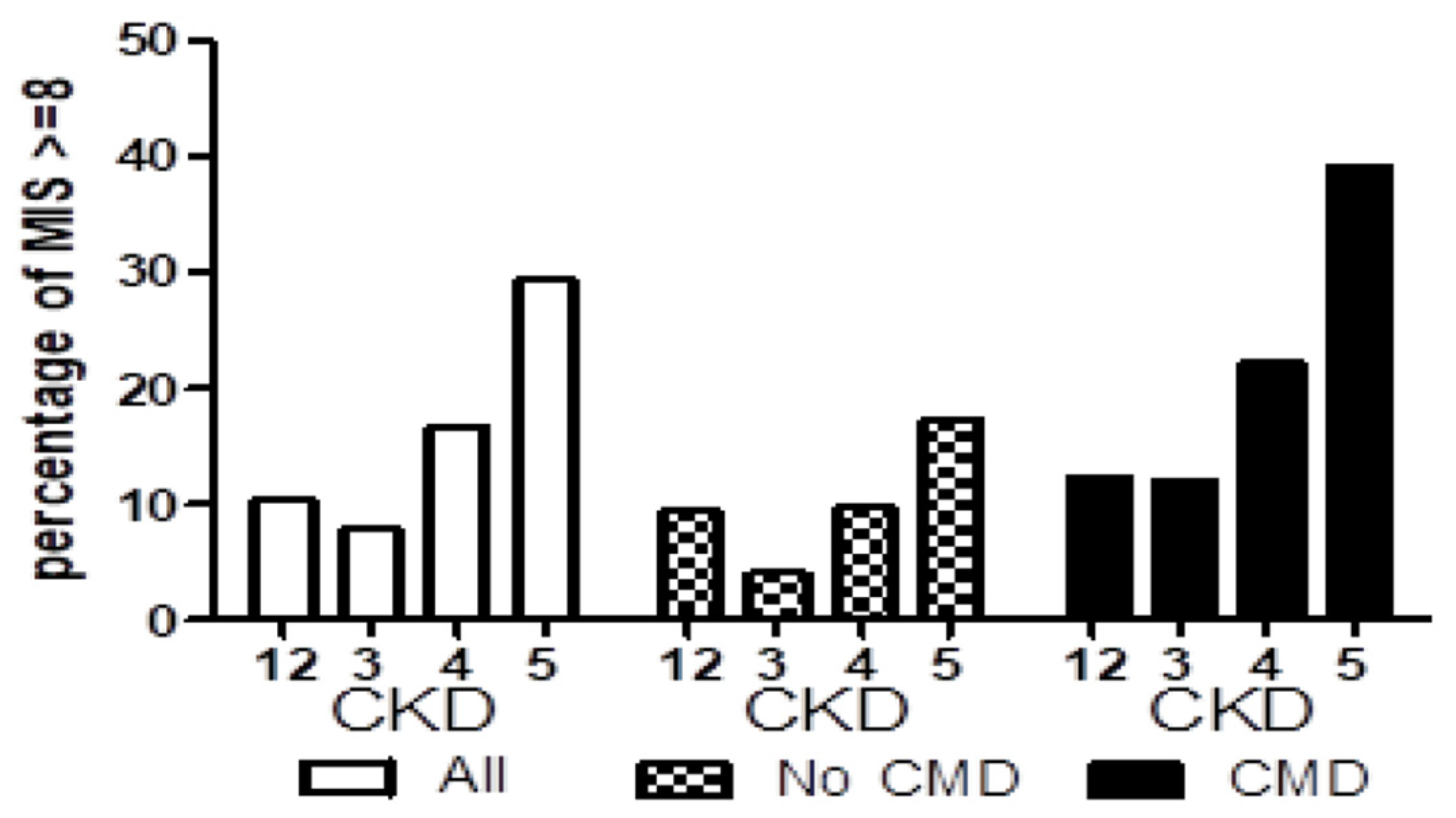
| MIS ≥ 8 | 37 (10.4%) | 94 (7.9%) | 160 (16.6%) | 341 (29.4%) | <0.001 |
| SGA C | 16 (4.5%) | 44 (3.7%) | 59 (6.1%) | 134 (11.6%) | <0.001 |
| Outcomes | |||||
| ESRD | 19 (5.3%) | 137 (11.6%) | 391 (40.7%) | 893 (77.0%) | <0.001 |
| All-cause mortality | 20 (5.6%) | 199 (16.8%) | 305 (31.7%) | 403 (34.8%) | <0.001 |
| MIS | ||
|---|---|---|
| Variables | Beta Coefficient (95% CI) | p |
| Age (years) | −0.010 (−0.016 to −0.004) | <0.001 |
| Gender (male) | 0.114 (−0.061 to 0.290) | 0.202 |
| eGFR (ml/min/1.73 m2) | 0.006 (0.002 to 0.010) | 0.001 |
| UPCR log | 0.064 (−0.092 to 0.221) | 0.421 |
| Diabetes | 0.283 (0.113 to 0.454) | <0.001 |
| Cardiovascular disease | 1.132 (0.920 to 1.345) | <0.001 |
| Cancers | 0.644 (0.349 to 0.939) | <0.001 |
| Smokers | −0.062 (−0.290 to 0.167) | 0.596 |
| Hypertension | −0.266 (−0.429 to −0.102) | 0.001 |
| Hemoglobin (g/dL) | −0.110 (−0.156 to −0.064) | <0.001 |
| Cholesterol log | −1.350 (−2.069 to −0.632) | <0.001 |
| Mean BP (mmHg) | −0.007 (−0.013 to 0.002) | 0.011 |
| Body mass index (kg/m2) | −0.102 (−0.121 to −0.082) | <0.001 |
| Muscle mass index (kg/m2) | −0.240 (−0.778 to −0.023) | 0.025 |
| Albumin(g/dL) | −2.810 (−2.980 to −2.640) | <0.001 |
| CRP log | 0.924 (0.840 to 1.009) | <0.001 |
| Phosphorus (mg/dL) | −0.155 (−0.256 to −0.054) | 0.003 |
| Variable | Baseline | Pre-Dialysis | p Value |
|---|---|---|---|
| Age (year) | 60.8 (13.6) | 66.5 (13.6) | - |
| Sex (female) | 559 (49.4%) | 559 (49.4%) | - |
| Charlson score | 3.4 (2.1) | 3.6 (2.2) | 0.125 |
| eGFR (ml/min/1.73 m2) | 30.6 (24.3) | 4.9 (2.8) | <0.001 |
| Malnutrition–inflammation | |||
| MIS | 5.7 (3.2) | 7.8 (3.2) | <0.001 |
| MIS ≥ 8 | 320 (28.5%) | 554 (49.3%) | <0.001 |
| SGA C | 118 (10.5%) | 688 (61.2%) | <0.001 |
| MIS1 (change in body weight) | 108 (9.5%) | 513 (45.6%) | <0.001 |
| MIS2 (dietary intake) | 264 (23.3%) | 649 (57.8%) | <0.001 |
| MIS3 (GI symptoms) | 250 (22.1%) | 935 (82.6%) | <0.001 |
| MIS4 (functional capacity) | 234 (20.7%) | 648 (57.7%) | <0.001 |
| MIS5 (comorbidities) | 482 (42.6%) | 601 (53.5%) | 0.015 |
| MIS6 (decreased fat stores) | 165 (14.6%) | 239 (21.3%) | 0.016 |
| MIS7 (muscle wasting) | 238 (21.0%) | 367 (32.7%) | <0.001 |
| MIS8 (body mass index) | 126 (11.1%) | 182 (16.2%) | 0.135 |
| MIS9 (serum albumin) | 814 (71.9%) | 955 (85.0%) | <0.001 |
| MIS10 (serum TIBC) | 540 (48.0%) | 540 (48.0%) | - |
| Pre-Dialysis MIS | ||
|---|---|---|
| Variables | 95% CI Beta Coefficient | p |
| Baseline MIS | 0.751 (0.692 to 0.810) | <0.001 |
| Follow up years | −0.000 (0.000 to 0.000) | 0.872 |
| Age (years) | 0.014 (0.004 to 0.024) | 0.007 |
| Gender (female) | 0.240 (−0.040 to 0.521) | 0.093 |
| eGFR (ml/min/1.73 m2) | 0.019 (0.001 to 0.036) | 0.038 |
| UPCR log | 0.134 (−0.248 to 0.515) | 0.492 |
| Diabetes | −0.158 (−0.478 to 0.162) | 0.332 |
| Cardiovascular disease | 0.672 (0.334 to 1.010) | <0.001 |
| Cancer | 0.594 (0.142 to 1.047) | 0.010 |
| Smoker | −0.003 (−0.453 to 0.446) | 0.988 |
| Hypertension | 0.072 (−0.230 to 0.375) | 0.640 |
| Hemoglobin (g/dL) | 0.038 (−0.054 to 0.130) | 0.416 |
| Cholesterol log | −0.285 (−1.456 to 0.885) | 0.632 |
| Mean BP (mmHg) | −0.007 (−0.017 to 0.003) | 0.160 |
| Body mass index (kg/m2) | −0.029 (−0.063 to 0.006) | 0.105 |
| Muscle mass index(kg/m2) | −0.041 (−0.174 to 0.092) | 0.552 |
| Albumin (g/dL) | 0.207 (−0.133 to 0.547) | 0.232 |
| CRP log | −0.177 (−0.338 to −0.016) | 0.031 |
| Phosphorus (mg/dL) | −0.113 (−0.218 to −0.008) | 0.034 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, L.-M.; Kuo, H.-T.; Chao, Y.-L.; Shen, F.-C.; Chen, Y.-K.; Chiu, Y.-W.; Hwang, S.-J.; Hung, C.-C. Malnutrition–Inflammation Score of Patients with Chronic Kidney Disease from Early Stage to Initiation of Dialysis. Nutrients 2024, 16, 4014. https://doi.org/10.3390/nu16234014
Lim L-M, Kuo H-T, Chao Y-L, Shen F-C, Chen Y-K, Chiu Y-W, Hwang S-J, Hung C-C. Malnutrition–Inflammation Score of Patients with Chronic Kidney Disease from Early Stage to Initiation of Dialysis. Nutrients. 2024; 16(23):4014. https://doi.org/10.3390/nu16234014
Chicago/Turabian StyleLim, Lee-Moay, Hung-Tien Kuo, Yu-Lin Chao, Feng-Ching Shen, Yi-Kong Chen, Yi-Wen Chiu, Shang-Jyh Hwang, and Chi-Chih Hung. 2024. "Malnutrition–Inflammation Score of Patients with Chronic Kidney Disease from Early Stage to Initiation of Dialysis" Nutrients 16, no. 23: 4014. https://doi.org/10.3390/nu16234014
APA StyleLim, L.-M., Kuo, H.-T., Chao, Y.-L., Shen, F.-C., Chen, Y.-K., Chiu, Y.-W., Hwang, S.-J., & Hung, C.-C. (2024). Malnutrition–Inflammation Score of Patients with Chronic Kidney Disease from Early Stage to Initiation of Dialysis. Nutrients, 16(23), 4014. https://doi.org/10.3390/nu16234014





