Lipidomic Signature of Healthy Diet Adherence and Its Association with Cardiometabolic Risk in American Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Dietary Assessment
2.3. MIDUS Healthy Eating Index (MIDUS-HEI)
2.4. Sociodemographic and Health Information
2.5. Metabolic Syndrome (MetS)
2.6. Lipid Profiling
2.7. Lipid Signature of MIDUS-HEI
2.8. Cardiovascular Risk
2.9. Statistical Analyses
3. Results
3.1. Sociodemographic Characterization of the Sample and Its Diet Quality
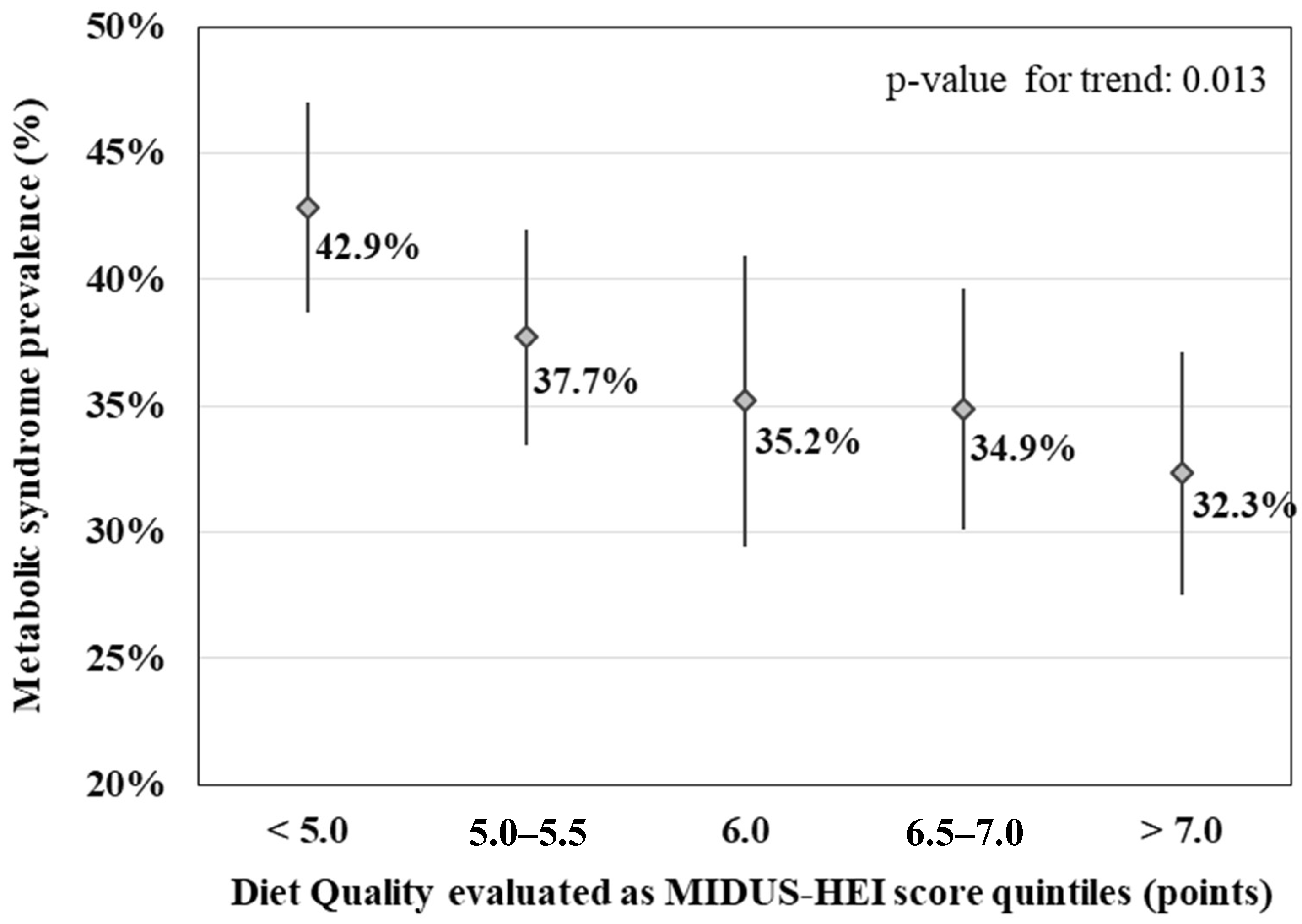
3.2. Association of MIDUS-HEI Score with MetS
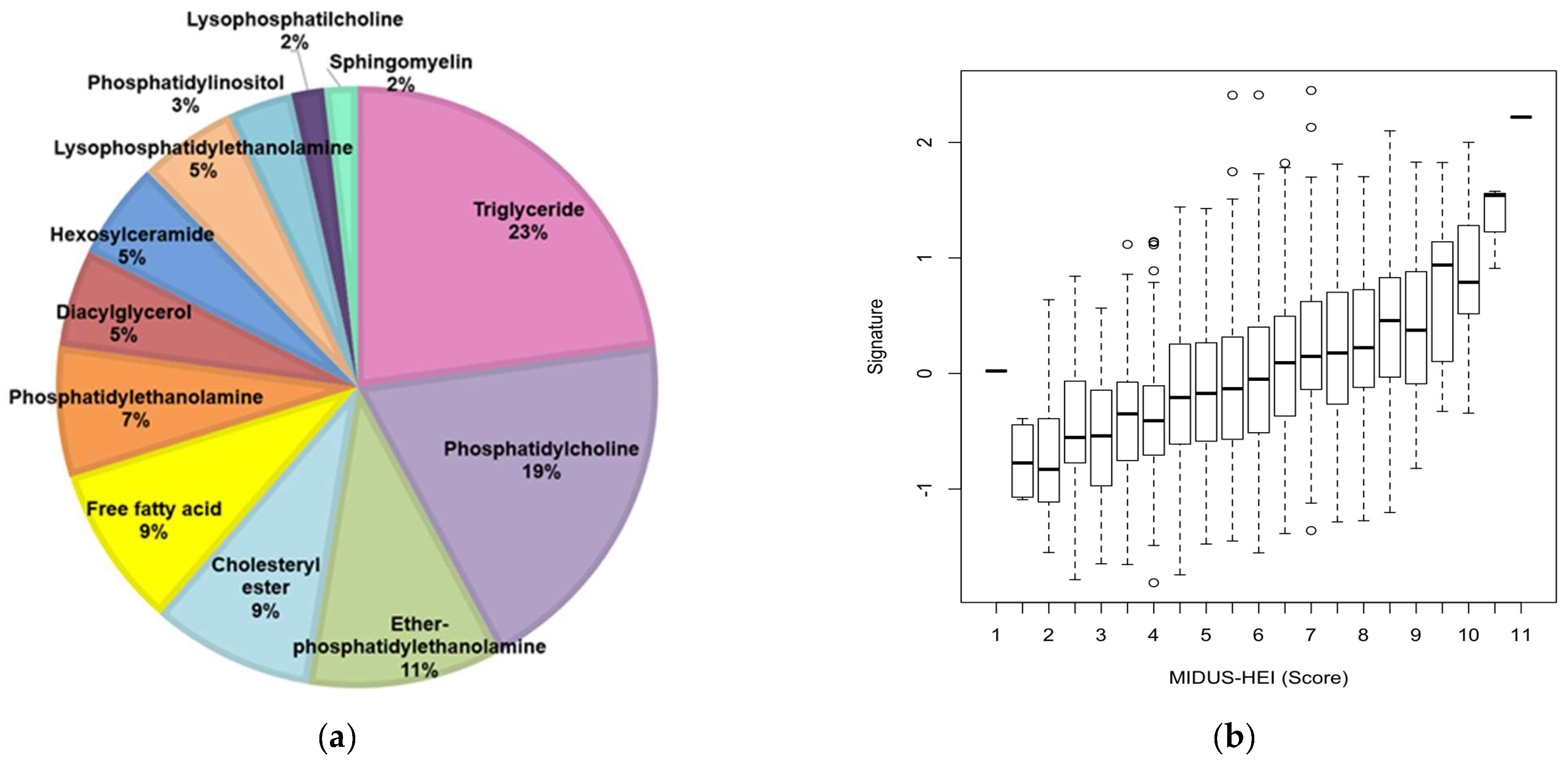
3.3. Lipidomic Signature of MIDUS-HEI
3.4. Association Between Lipidomic Signature of MIDUS-HEI and Cardiometabolic Biomarkers
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization Noncommunicable diseases. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 15 November 2023).
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Bhupathiraju, S.N.; Tucker, K.L. Coronary heart disease prevention: Nutrients, foods, and dietary patterns. Clin. Chim. Acta 2011, 412, 1493–1514. [Google Scholar] [CrossRef] [PubMed]
- Lassale, C.; Fezeu, L.; Andreeva, V.A.; Hercberg, S.; Kengne, A.P.; Czernichow, S.; Kesse-Guyot, E. Association between dietary scores and 13-year weight change and obesity risk in a French prospective cohort. Int. J. Obes. 2012, 36, 1455–1462. [Google Scholar] [CrossRef] [PubMed]
- Nestel, P.J.; Mori, T.A. Dietary patterns, dietary nutrients and cardiovascular disease. Rev. Cardiovasc. Med. 2022, 23, 17. [Google Scholar] [CrossRef]
- Chiuve, S.E.; Fung, T.T.; Rimm, E.B.; Hu, F.B.; McCullough, M.L.; Wang, M.; Stampfer, M.J.; Willett, W.C. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 2012, 142, 1009–1018. [Google Scholar] [CrossRef]
- Varraso, R.; Chiuve, S.E.; Fung, T.T.; Barr, R.G.; Hu, F.B.; Willett, W.C.; Camargo, C.A. Alternate Healthy Eating Index 2010 and risk of chronic obstructive pulmonary disease among US women and men: Prospective study. BMJ 2015, 350, h286. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Henríquez-Sánchez, P.; Ruiz-Canela, M.; Lahortiga, F.; Molero, P.; Toledo, E.; Martínez-González, M.A. A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN Project. BMC Med. 2015, 13, 197. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Whitton, C.; Collins, C.E.; Mullan, B.A.; Rollo, M.E.; Dhaliwal, S.S.; Norman, R.; Boushey, C.J.; Delp, E.J.; Zhu, F.; McCaffrey, T.A.; et al. Accuracy of energy and nutrient intake estimation versus observed intake using 4 technology-assisted dietary assessment methods: A randomized crossover feeding study. Am. J. Clin. Nutr. 2024, 120, 196–210. [Google Scholar] [CrossRef]
- Brennan, L.; Hu, F.B.; Sun, Q. Metabolomics Meets Nutritional Epidemiology: Harnessing the Potential in Metabolomics Data. Metabolites 2021, 11, 709. [Google Scholar] [CrossRef]
- Li, J.; Guasch-Ferré, M.; Chung, W.; Ruiz-Canela, M.; Toledo, E.; Corella, D.; Bhupathiraju, S.N.; Tobias, D.K.; Tabung, F.K.; Hu, J.; et al. The Mediterranean diet, plasma metabolome, and cardiovascular disease risk. Eur. Heart J. 2020, 41, 2645–2656. [Google Scholar] [CrossRef] [PubMed]
- Thomasset, B.; Sarazin, C. Biodiversity of lipid species—Benefit for nutrition and effects on health. Biochimie 2020, 178, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Zupo, R.; Castellana, F.; Piscitelli, P.; Crupi, P.; Desantis, A.; Greco, E.; Severino, F.P.; Pulimeno, M.; Guazzini, A.; Kyriakides, T.C.; et al. Scientific evidence supporting the newly developed one-health labeling tool “Med-Index”: An umbrella systematic review on health benefits of mediterranean diet principles and adherence in a planeterranean perspective. J. Transl. Med. 2023, 21, 75. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.A.; García-Arellano, A.; Toledo, E.; Salas-Salvadó, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schröder, H.; Arós, F.; Gómez-Gracia, E.; et al. A 14-item mediterranean diet assessment tool and obesity indexes among high-risk subjects: The PREDIMED trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef]
- McCullough, M.L.; Feskanich, D.; Stampfer, M.J.; Giovannucci, E.L.; Rimm, E.B.; Hu, F.B.; Spiegelman, D.; Hunter, D.J.; Colditz, G.A.; Willett, W.C. Diet quality and major chronic disease risk in men and women: Moving toward improved dietary guidance. Am. J. Clin. Nutr. 2002, 76, 1261–1271. [Google Scholar] [CrossRef]
- Love, G.D.; Seeman, T.E.; Weinstein, M.; Ryff, C.D. Bioindicators in the MIDUS national study: Protocol, measures, sample, and comparative context. J. Aging Health 2010, 22, 1059–1080. [Google Scholar] [CrossRef]
- Grundy, S.M.; Brewer, H.B., Jr.; Cleeman, J.I.; Smith, S.C., Jr.; Lenfant, C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004, 109, 433–438. [Google Scholar] [CrossRef]
- Berkowitz, L.; Salazar, C.; Ryff, C.D.; Coe, C.L.; Rigotti, A. Serum sphingolipid profiling as a novel biomarker for metabolic syndrome characterization. Front. Cardiovasc. Med. 2022, 9, 1092331. [Google Scholar] [CrossRef]
- Blom, G. Statistical Estimates and Transformed Beta-Variables; Almqvist & Wiksell: Stockholm, Sweden, 1958. [Google Scholar]
- Tibshirani, R. Regression Shrinkage and Selection Via the Lasso. J. R. Stat. Soc. Ser. B 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Regularization Paths for Generalized Linear Models via Coordinate Descent. J. Stat. Softw. 2010, 33, 1–22. [Google Scholar] [CrossRef]
- Goff, D.C.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2935–2959. [Google Scholar] [CrossRef] [PubMed]
- EBMcalc. 2024. Available online: https://www.uptodate.com/contents/calculator-cardiovascular-risk-assessment-in-adults-10-year-acc-aha-2013-patient-education (accessed on 4 June 2024).
- Roberson, P.N.; Shorter, R.L.; Woods, S.; Priest, J. How health behaviors link romantic relationship dysfunction and physical health across 20 years for middle-aged and older adults. Soc. Sci. Med. 2018, 201, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Boylan, J.M.; Robert, S.A. Neighborhood SES is particularly important to the cardiovascular health of low SES individuals. Soc. Sci. Med. 2017, 188, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Boehm, J.K.; Williams, D.R.; Rimm, E.B.S.; Ryff, C.; Kubzansky, L.D. Association between optimism and serum antioxidants in the midlife in the united states study. Psychosom. Med. 2013, 75, 2–10. [Google Scholar] [CrossRef]
- Yoo, J.; Miyamoto, Y.; Rigotti, A.; Ryff, C.D. Linking Positive Affect to Blood Lipids: A Cultural Perspective. Psychol. Sci. 2017, 28, 1468–1477. [Google Scholar] [CrossRef]
- Boehm, J.K.; Chen, Y.; Williams, D.R.; Ryff, C.D.; Kubzansky, L.D. Subjective well-being and cardiometabolic health: An 8–11 year study of midlife adults. J. Psychosom. Res. 2016, 85, 1–8. [Google Scholar] [CrossRef]
- Ambroselli, D.; Masciulli, F.; Romano, E.; Catanzaro, G.; Besharat, Z.M.; Massari, M.C.; Ferretti, E.; Migliaccio, S.; Izzo, L.; Ritieni, A.; et al. New Advances in Metabolic Syndrome, from Prevention to Treatment: The Role of Diet and Food. Nutrients 2023, 15, 640. [Google Scholar] [CrossRef]
- Medina-Remón, A.; Kirwan, R.; Lamuela-Raventós, R.M.; Estruch, R. Dietary patterns and the risk of obesity, type 2 diabetes mellitus, cardiovascular diseases, asthma, and neurodegenerative diseases. Crit. Rev. Food Sci. Nutr. 2017, 58, 262–296. [Google Scholar] [CrossRef]
- Ponnampalam, E.N.; Sinclair, A.J.; Holman, B.W.B. The Sources, Synthesis and Biological Actions of Omega-3 and Omega-6 Fatty Acids in Red Meat: An Overview. Foods 2021, 10, 1358. [Google Scholar] [CrossRef]
- Nababan, S.H.H.; Nishiumi, S.; Kawano, Y.; Kobayashi, T.; Yoshida, M.; Azuma, T. Adrenic acid as an inflammation enhancer in non-alcoholic fatty liver disease. Arch. Biochem. Biophys. 2017, 623–624, 64–75. [Google Scholar] [CrossRef]
- Zhao, J.; Nishiumi, S.; Tagawa, R.; Yano, Y.; Inoue, J.; Hoshi, N.; Yoshida, M.; Kodama, Y. Adrenic acid induces oxidative stress in hepatocytes. Biochem. Biophys. Res. Commun. 2020, 532, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Mazidi, M.; Shekoohi, N.; Katsiki, N.; Banach, M. Omega-6 fatty acids and the risk of cardiovascular disease: Insights from a systematic review and meta-analysis of randomized controlled trials and a Mendelian randomization study. Arch. Med. Sci. 2021, 18, 466–479. [Google Scholar] [CrossRef] [PubMed]
- Lauritzen, L.; Brambilla, P.; Mazzocchi, A.; Harsløf, L.B.S.; Ciappolino, V.; Agostoni, C. DHA Effects in Brain Development and Function. Nutrients 2016, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Mallick, R.; Basak, S.; Duttaroy, A.K. Docosahexaenoic acid, 22:6n-3: Its roles in the structure and function of the brain. Int. J. Dev. Neurosci. 2019, 79, 21–31. [Google Scholar] [CrossRef]
- Martínez-González, M.; Hernández, A.H. Effect of the Mediterranean diet in cardiovascular prevention. Rev. Espanola Cardiol. 2024, 77, 574–582. [Google Scholar] [CrossRef]


| MIDUS-HEI Component | Minimal Score (0) | Intermediate Score (0.5 Point) | Maximal Score (1 Point) | Maximal Double Score (2 Points) * |
|---|---|---|---|---|
| Direct relation between score and food intake | ||||
| Vegetables and fruits (servings/day) | None | 1–2 | 3–4 | ≥5 |
| Whole grains (servings/day) | None | 1–2 | ≥3 | |
| Oily fish (servings/week) | None | <1 | ≥1 | |
| Lean meat (servings/week) | None | 0–2 | ≥3 | |
| Non-meat protein food (servings/week) | <1 | 1–2 | ≥3 | |
| Inverse relation between score and food intake | ||||
| Sugared beverages (servings/day) | ≥4 | 1–3 | None | |
| High-fat meat (servings/week) | ≥3 | 1–2 | <1 | |
| Fast food (times/week) | ≥1 | <1 | None | |
| Non-linear relation between score and food intake | ||||
| Fermented dairy (servings/day) | <1 or ≥5 | (1 to <2) or (4 to <5) | ≥2 and <4 | |
| Alcohol (Frequency and quantity) | Nondrinker or (Quantity: Men: >2 drinks/day and Women: >1 drinks/day) | (Frequency: <3 days/week) and (Quantity: Men: 1–2 drinks/day and Women: 1 drinks/day) | (Frequency: ≥3 days/week) and (Quantity: Men: 1–2 drinks/day and Women: 1 drinks/day) | |
| Total MIDUS-HEI score | 0 | 11 | ||
| Characteristics | MIDUS Core 59.3% (n = 1255) | MIDUS Refresher 40.7% (n = 862) |
|---|---|---|
| Sex | ||
| Men | 43.2 (542) | 47.9 (413) |
| Women | 56.8 (713) | 52.1 (450) |
| Age group | ||
| <50 years | 29.1 (365) | 45.3 (391) |
| 50–65 years | 44.8 (562) | 38.9 (336) |
| >65 years | 26.1 (328) | 15.8 (136) |
| Race | ||
| White | 78.7 (985) | 70.2 (606) |
| Non-white | 21.3 (266) | 29.8 (257) |
| Educational level | ||
| Higher education or less | 28.0 (350) | 17.3 (149) |
| College education | 50.2 (629) | 55.0 (474) |
| Postgraduate studies | 21.8 (273) | 27.7 (239) |
| Nutritional status | ||
| Under or normal weight | 23.8 (298) | 24.8 (214) |
| Overweight | 35.1 (440) | 30.0 (259) |
| Obesity | 41.1 (516) | 45.2 (390) |
| Metabolic syndrome | ||
| No | 60.8 (750) | 65.3 (554) |
| Yes | 39.2 (484) | 34.7 (295) |
| MIDUS-HEI~ | Coef (95% CI) | p-Value |
|---|---|---|
| Sample | ||
| MIDUS Core vs. MIDUS Refresher | −0.467 (−0.612 to −0.323) | 0.000 |
| Sex | ||
| Men vs. women | −0.420 (−0.557 to −0.284) | 0.000 |
| Race | ||
| White vs. non-white | 0.369 (0.207 to 0.531) | 0.000 |
| Age | ||
| Age (years old) | 0.020 (0.014 to 0.025) | <0.001 |
| Educational level | ||
| Higher education or less vs. postgraduate studies | −0.693 (−0.899 to −0.486) | 0.000 |
| College education vs. postgraduate studies | −0.313 (−0.483 to −0.144) | 0.000 |
| Nutritional status | ||
| BMI (kg/m2) | −0.369 (−0.207 to −0.531) | 0.000 |
| Smoking status | ||
| Never vs. current smoker | 0.520 (0.310 to 0.731) | <0.001 |
| Former vs. current smoker | 0.541 (0.322 to 0.760) | <0.001 |
| Variables | Model I 1 | Model II 2 | Model III 3 | |||
|---|---|---|---|---|---|---|
| Coef | p-Value | Coef | p-Value | Coef | p-Value | |
| BMI (kg/m2) | −0.213 | <0.0001 | ||||
| LDL-c (mg/dL) | −0.033 | 0.167· | −0.021 | 0.376 | −0.013 | 0.614 |
| HDL-c (mg/dL) | 0.291 | <0.0001 | 0.227 | <0.0001 | 0.213 | <0.0001 |
| HOMA-IR | −0.242 | <0.0001 | −0.132 | <0.0001 | −0.119 | <0.0001 |
| Insulin (mg/dL) | −0.245 | <0.0001 | −0.134 | <0.0001 | −0.120 | <0.0001 |
| Glucose (mg/dL) | −0.098 | <0.0001 | −0.051 | 0.028 | −0.051 | 0.038 |
| HbA1c (%) | −0.077 | <0.001 | −0.031 | 0.169 | −0.031 | 0.186 |
| IL-6 (pg/mL) | −0.263 | <0.0001 | −0.191 | <0.0001 | −0.179 | <0.0001 |
| CRP (mg/L) | −0.237 | <0.0001 | −0.142 | <0.0001 | −0.125 | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berkowitz, L.; Echeverría, G.; Salazar, C.; Faúndez, C.; Coe, C.L.; Ryff, C.; Rigotti, A. Lipidomic Signature of Healthy Diet Adherence and Its Association with Cardiometabolic Risk in American Adults. Nutrients 2024, 16, 3995. https://doi.org/10.3390/nu16233995
Berkowitz L, Echeverría G, Salazar C, Faúndez C, Coe CL, Ryff C, Rigotti A. Lipidomic Signature of Healthy Diet Adherence and Its Association with Cardiometabolic Risk in American Adults. Nutrients. 2024; 16(23):3995. https://doi.org/10.3390/nu16233995
Chicago/Turabian StyleBerkowitz, Loni, Guadalupe Echeverría, Cristian Salazar, Cristian Faúndez, Christopher L. Coe, Carol Ryff, and Attilio Rigotti. 2024. "Lipidomic Signature of Healthy Diet Adherence and Its Association with Cardiometabolic Risk in American Adults" Nutrients 16, no. 23: 3995. https://doi.org/10.3390/nu16233995
APA StyleBerkowitz, L., Echeverría, G., Salazar, C., Faúndez, C., Coe, C. L., Ryff, C., & Rigotti, A. (2024). Lipidomic Signature of Healthy Diet Adherence and Its Association with Cardiometabolic Risk in American Adults. Nutrients, 16(23), 3995. https://doi.org/10.3390/nu16233995







