The Effects of Time-Restricted Eating on Fat Loss in Adults with Overweight and Obese Depend upon the Eating Window and Intervention Strategies: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Literature Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Quality Assessment
2.6. Statistical Analysis
3. Results
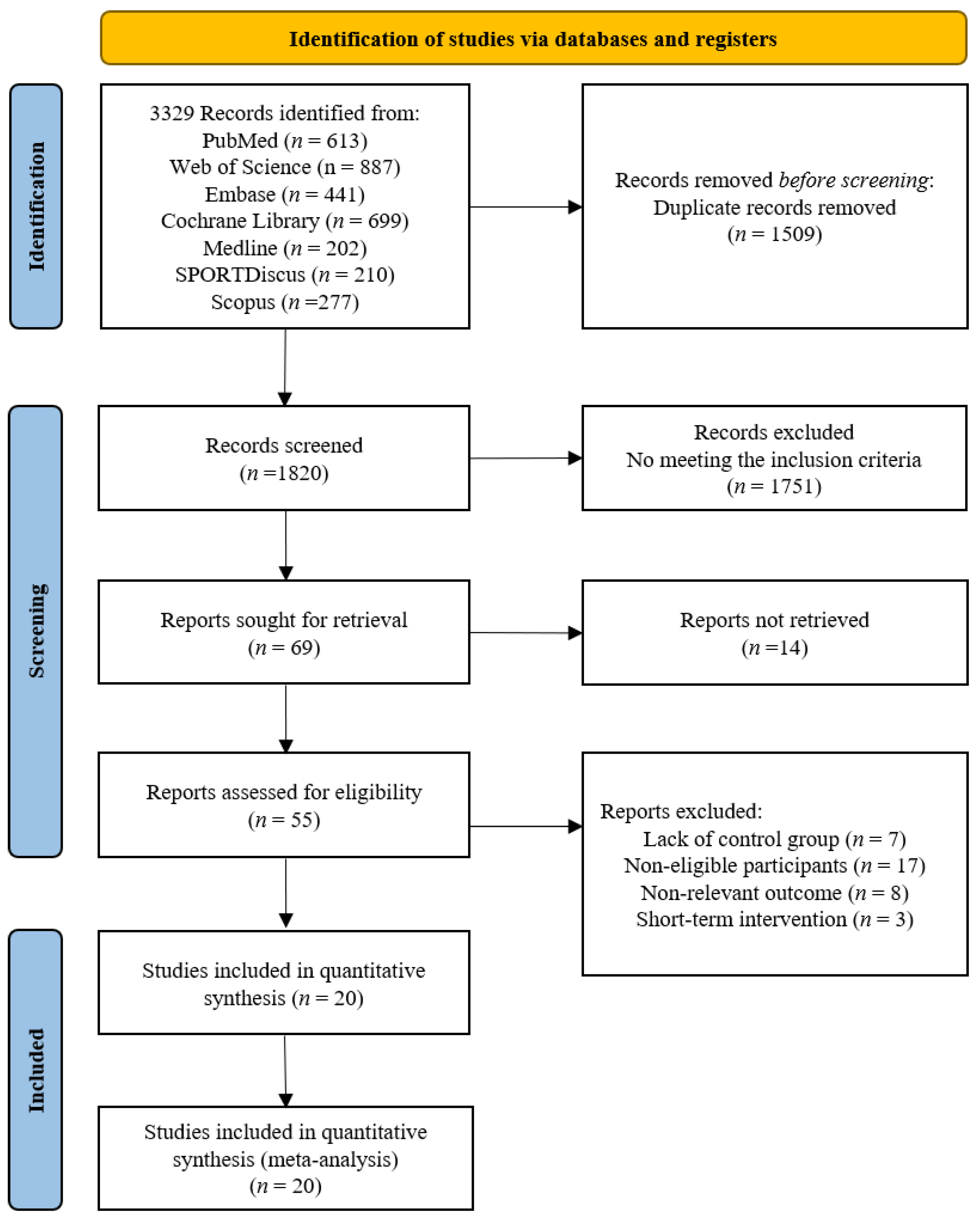
3.1. Study Selection
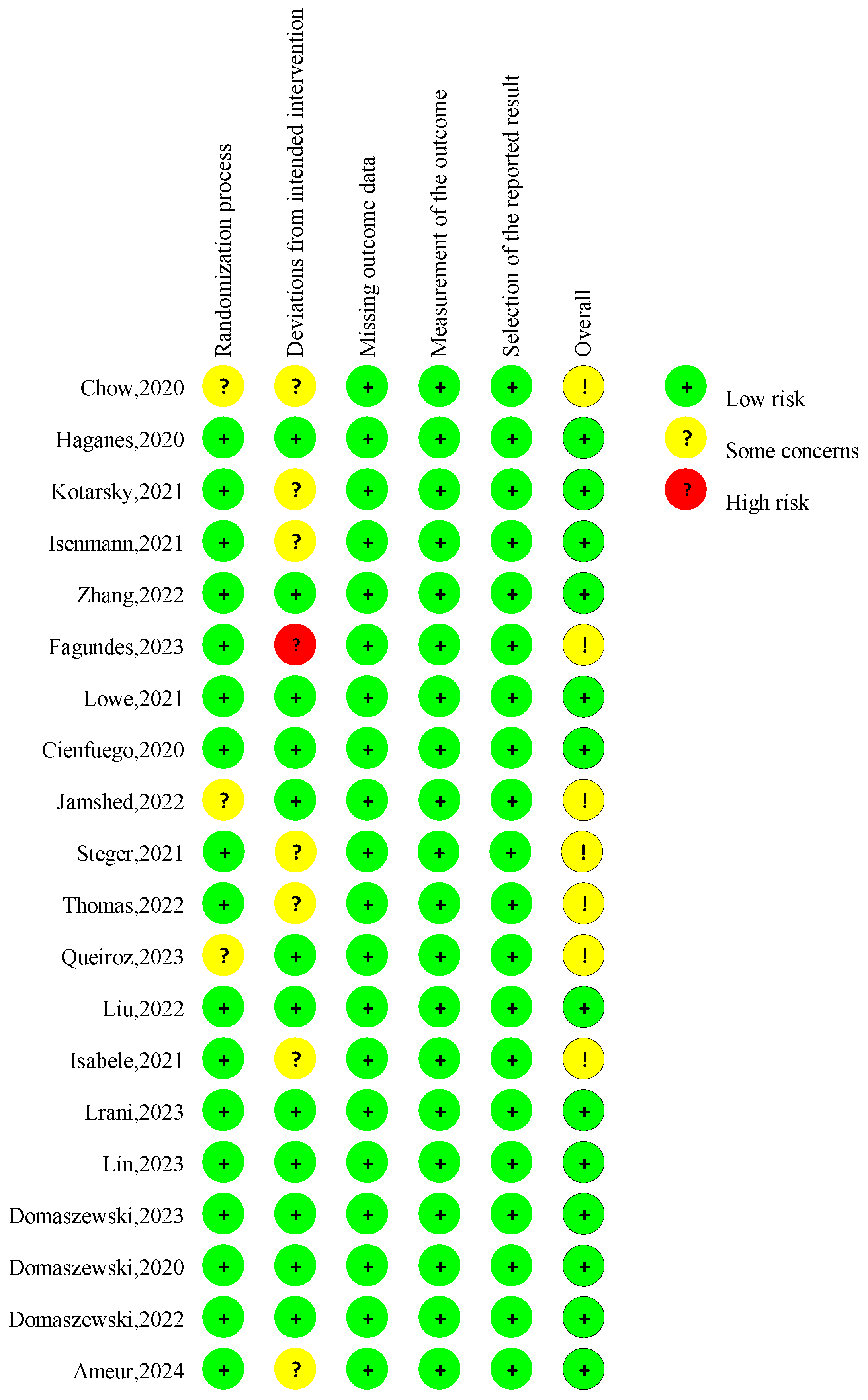
3.2. Quality Assessment
3.3. Assessment of Evidence Certainty
3.4. Characteristics of the Included Studies
3.4.1. Participants
3.4.2. Study Design
3.5. Intervention Characteristics
3.5.1. Diet and Exercise Interventions
3.5.2. TRE Protocol
3.5.3. Outcome Measurement
3.6. Adverse Events and Side Effects
4. Meta-Analysis
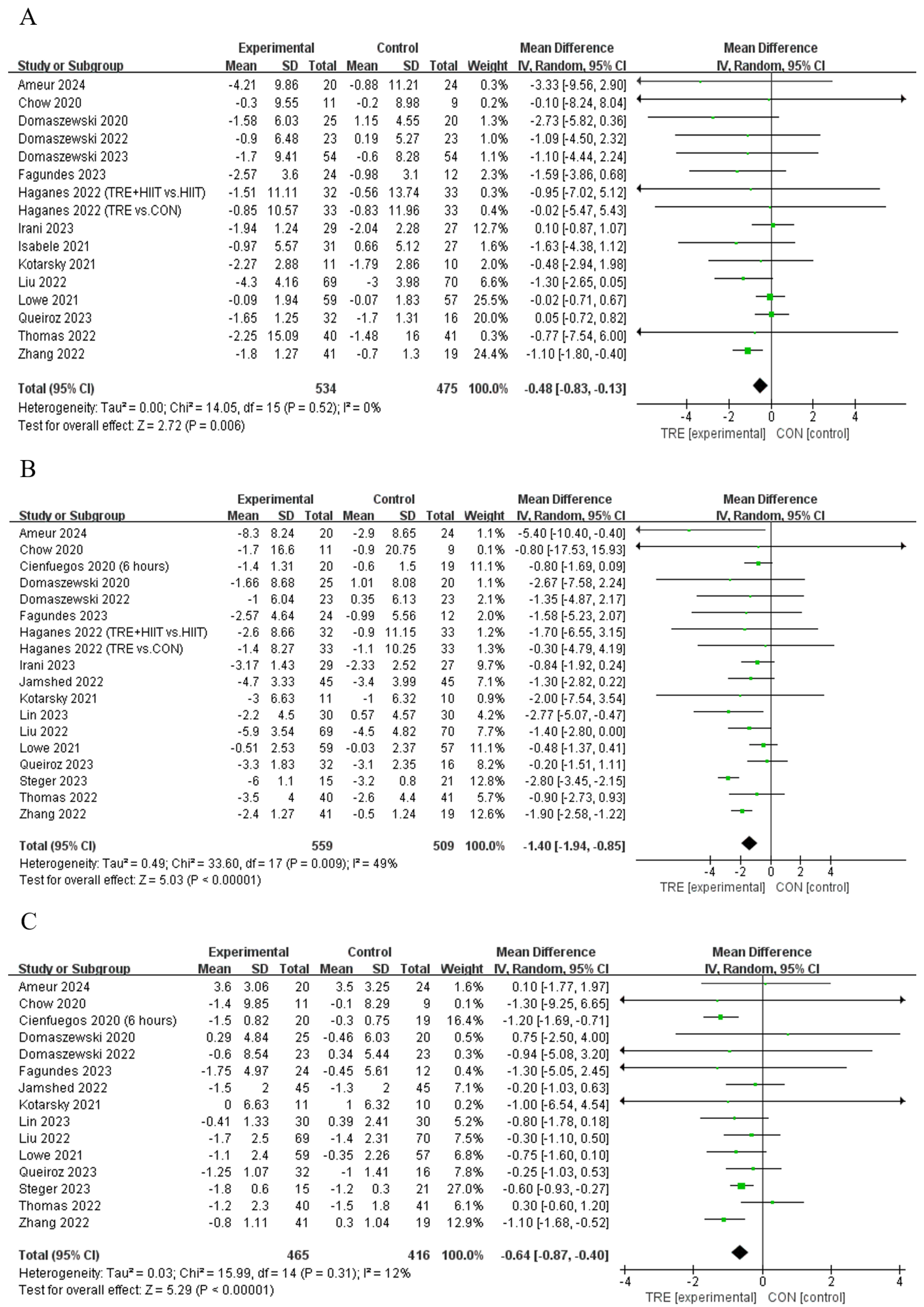
4.1. Effects of TRE on Body Composition
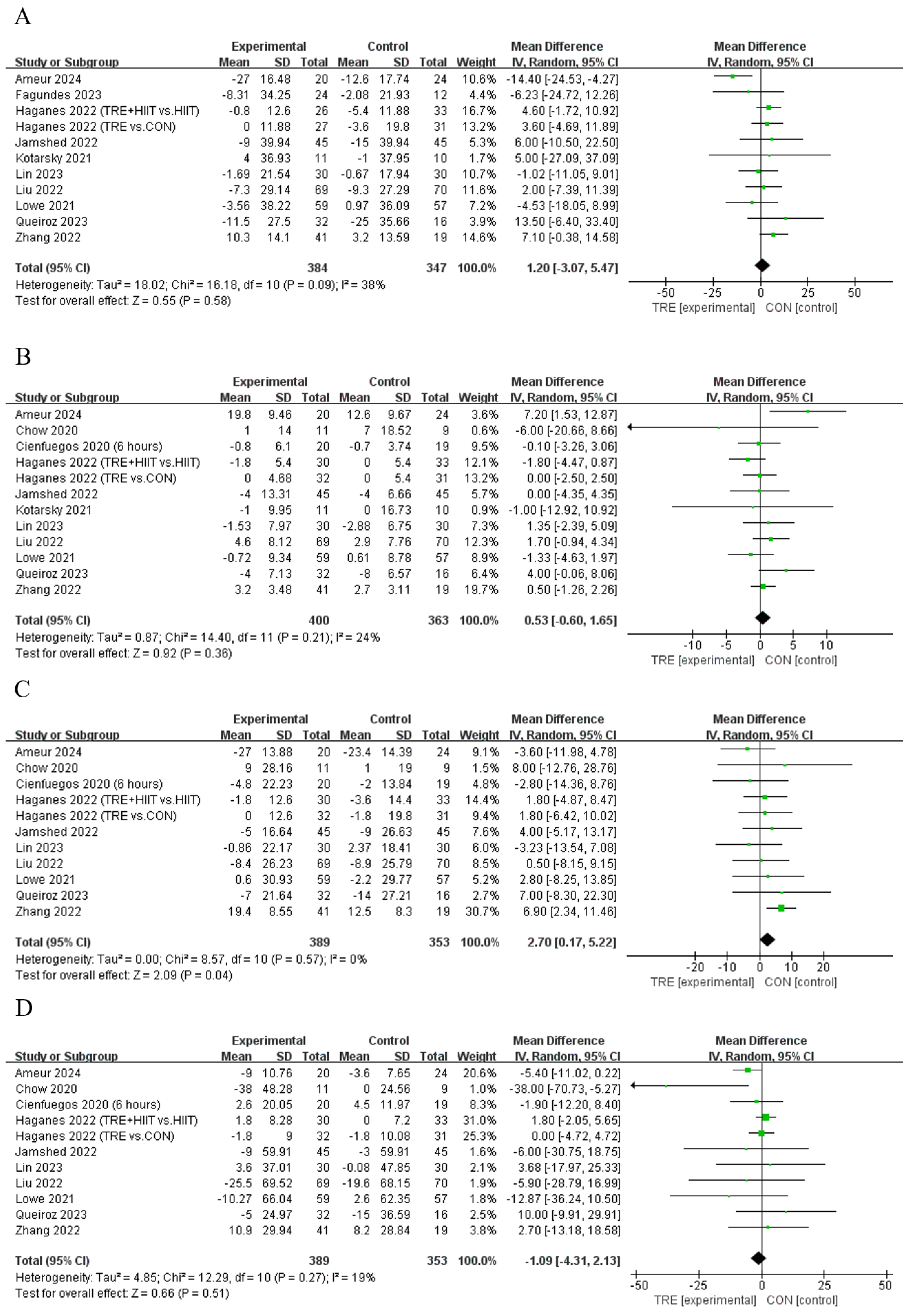
4.1.1. Body Fat Percentage
4.1.2. Fat Mass
4.1.3. Lean Mass
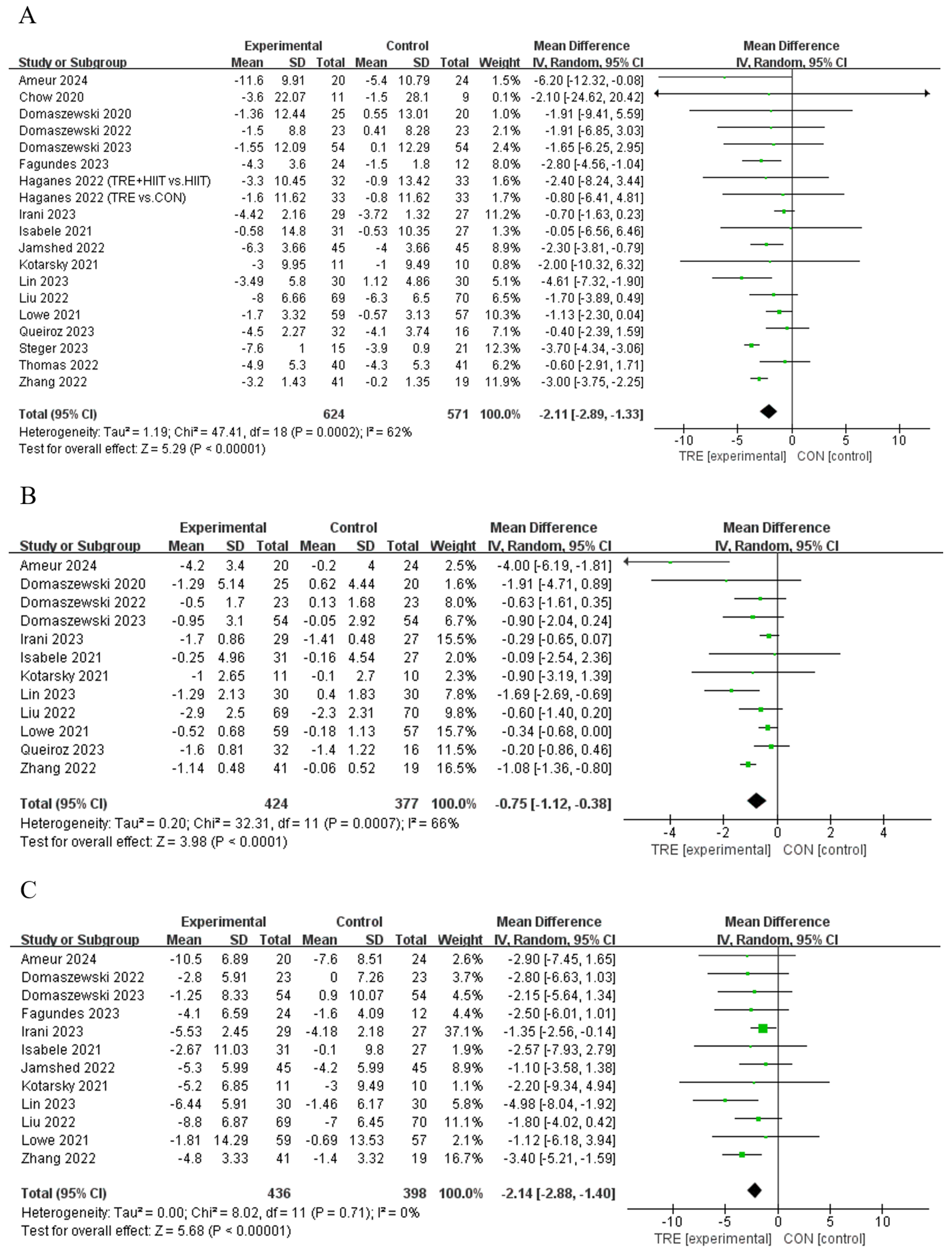
4.2. Effects of TRE on Anthropometric Measures
4.2.1. Body Mass
4.2.2. Body Mass Index
4.2.3. Waist Circumference
4.3. Effects of TRE on Blood Lipid
5. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blüher, M. Obesity: Global Epidemiology and Pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- Kolotkin, R.L.; Meter, K.; Williams, G.R. Quality of Life and Obesity. Obes. Rev. 2001, 2, 219–229. [Google Scholar] [CrossRef]
- World Health Organization. World Health Statistics 2022: Monitoring Health for the SDGs, Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2022.
- McDowell, A.; Caughman, R.; Bischo, L. Total Energy Intake of the US Population: The Third National Health and Nutrition Examination Survey, 1988–1991. Am. J. Clin. Nutr. 1995, 62, 1072S–1080S. [Google Scholar]
- Gallant, A.R.; Lundgren, J.; Drapeau, V. The Night-Eating Syndrome and Obesity: NES and Obesity. Obes. Rev. 2012, 13, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O. Understanding and Addressing the Epidemic of Obesity: An Energy Balance Perspective. Endocr. Rev. 2006, 27, 750–761. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.C.; Gallop, M.R.; Flores Ramos, S.; Zarrinpar, A.; Broussard, J.L.; Chondronikola, M.; Chaix, A.; Klein, S. Complex Physiology and Clinical Implications of Time-Restricted Eating. Physiol. Rev. 2022, 102, 1991–2034. [Google Scholar] [CrossRef] [PubMed]
- Chaix, A.; Manoogian, E.N.C.; Melkani, G.C.; Panda, S. Time-Restricted Eating to Prevent and Manage Chronic Metabolic Diseases. Annu. Rev. Nutr. 2019, 39, 291–315. [Google Scholar] [CrossRef]
- Queiroz, J.D.N.; Macedo, R.C.O.; Tinsley, G.M.; Reischak-Oliveira, A. Time-Restricted Eating and Circadian Rhythms: The Biological Clock Is Ticking. Crit. Rev. Food Sci. Nutr. 2021, 61, 2863–2875. [Google Scholar] [CrossRef]
- Cienfuegos, S.; Gabel, K.; Kalam, F.; Ezpeleta, M.; Wiseman, E.; Pavlou, V.; Lin, S.; Oliveira, M.L.; Varady, K.A. Effects of 4- and 6-h Time-Restricted Feeding on Weight and Cardiometabolic Health: A Randomized Controlled Trial in Adults with Obesity. Cell Metab. 2020, 32, 366–378.e3. [Google Scholar] [CrossRef]
- Jamshed, H.; Steger, F.L.; Bryan, D.R.; Richman, J.S.; Warriner, A.H.; Hanick, C.J.; Martin, C.K.; Salvy, S.J.; Peterson, C.M. Effectiveness of Early Time-Restricted Eating for Weight Loss, Fat Loss, and Cardiometabolic Health in Adults with Obesity: A Randomized Clinical Trial. JAMA Intern. Med. 2022, 182, 953–962. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, Z.; Wang, J.; Li, R.; Ren, J.; Gao, X.; Lv, S.; Liang, L.; Zhang, F.; Yin, B.; et al. Randomized Controlled Trial for Time-Restricted Eating in Overweight and Obese Young Adults. Iscience 2022, 25, 104870. [Google Scholar] [CrossRef] [PubMed]
- Lowe, D.A.; Wu, N.; Rohdin-Bibby, L.; Moore, A.H.; Kelly, N.; Liu, Y.E.; Philip, E.; Vittinghoff, E.; Heymsfield, S.B.; Olgin, J.E.; et al. Effects of Time-Restricted Eating on Weight Loss and Other Metabolic Parameters in Women and Men With Overweight and Obesity: The TREAT Randomized Clinical Trial. JAMA Intern. Med. 2020, 180, 1491–1499. [Google Scholar] [CrossRef]
- Chen, J.-H.; Lu, L.W.; Ge, Q.; Feng, D.; Yu, J.; Liu, B.; Zhang, R.; Zhang, X.; Ouyang, C.; Chen, F. Missing Puzzle Pieces of Time-Restricted-Eating (TRE) as a Long-Term Weight-Loss Strategy in Overweight and Obese People? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit. Rev. Food Sci. Nutr. 2023, 63, 2331–2347. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Chen, W.; Wu, D.; Hu, F. Metabolic Efficacy of Time-Restricted Eating in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Endocrinol. Metab. 2022, 107, 3428–3441. [Google Scholar] [CrossRef]
- Huang, L.; Chen, Y.; Wen, S.; Lu, D.; Shen, X.; Deng, H.; Xu, L. Is Time-Restricted Eating (8/16) Beneficial for Body Weight and Metabolism of Obese and Overweight Adults? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Food Sci. Nutr. 2023, 11, 1187–1200. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Introduction to Meta-Analysis, 1st ed.; Wiley: Hoboken, NJ, USA, 2009. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Collaboration, C. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Cochrane Book Series; Wiley-Blackwell: Hoboken, NJ, USA, 2019. [Google Scholar]
- Xue, Y.; Yang, Y.; Huang, T. Effects of Chronic Exercise Interventions on Executive Function among Children and Adolescents: A Systematic Review with Meta-Analysis. Br. J. Sports Med. 2019, 53, 1397–1404. [Google Scholar] [CrossRef] [PubMed]
- Fagundes, G.B.P.; Tibães, J.R.B.; Silva, M.L.; Braga, M.M.; Silveira, A.L.M.; Teixeira, A.L.; Ferreira, A.V.M. Metabolic and Behavioral Effects of Time-Restricted Eating in Women with Overweight or Obesity: Preliminary Findings from a Randomized Study. Nutrition 2023, 107, 111909. [Google Scholar] [CrossRef]
- Petzold, A.; Steeb, T.; Wessely, A.; Koch, E.A.T.; Vera, J.; Berking, C.; Heppt, M.V. Is Tebentafusp Superior to Combined Immune Checkpoint Blockade and Other Systemic Treatments in Metastatic Uveal Melanoma? A Comparative Efficacy Analysis with Population Adjustment. Cancer Treat. Rev. 2023, 115, 102543. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://training.cochrane.org/handbook (accessed on 1 October 2024).
- Higgins, J.P.T. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S. GRADE Guidelines: 3. Rating the Quality of Evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Meader, N.; King, K.; Llewellyn, A.; Norman, G.; Brown, J.; Rodgers, M.; Moe-Byrne, T.; Higgins, J.P.; Sowden, A.; Stewart, G. A Checklist Designed to Aid Consistency and Reproducibility of GRADE Assessments: Development and Pilot Validation. Syst. Rev. 2014, 3, 82. [Google Scholar] [CrossRef]
- Haganes, K.L.; Silva, C.P.; Eyjólfsdóttir, S.K.; Steen, S.; Grindberg, M.; Lydersen, S.; Hawley, J.A.; Moholdt, T. Time-Restricted Eating and Exercise Training Improve HbA1c and Body Composition in Women with Overweight/Obesity: A Randomized Controlled Trial. Cell Metab. 2022, 34, 1457–1471.e4. [Google Scholar] [CrossRef] [PubMed]
- Chow, L.S.; Manoogian, E.N.C.; Alvear, A.; Fleischer, J.G.; Thor, H.; Dietsche, K.; Wang, Q.; Hodges, J.S.; Esch, N.; Malaeb, S.; et al. Time-Restricted Eating Effects on Body Composition and Metabolic Measures in Humans Who Are Overweight: A Feasibility Study. Obesity 2020, 28, 860–869. [Google Scholar] [CrossRef]
- Domaszewski, P.; Konieczny, M.; Pakosz, P.; Bączkowicz, D.; Sadowska-Krępa, E. Effect of a Six-Week Intermittent Fasting Intervention Program on the Composition of the Human Body in Women over 60 Years of Age. Int. J. Environ. Res. Public Health 2020, 17, 4138. [Google Scholar] [CrossRef]
- Kotarsky, C.J.; Johnson, N.R.; Mahoney, S.J.; Mitchell, S.L.; Schimek, R.L.; Stastny, S.N.; Hackney, K.J. Time-Restricted Eating and Concurrent Exercise Training Reduces Fat Mass and Increases Lean Mass in Overweight and Obese Adults. Physiol. Rep. 2021, 9, e14868. [Google Scholar] [CrossRef]
- Isenmann, E.; Dissemond, J.; Geisler, S. The Effects of a Macronutrient-Based Diet and Time-Restricted Feeding (16:8) on Body Composition in Physically Active Individuals—A 14-Week Randomised Controlled Trial. Nutrients 2021, 13, 3122. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Maranhão Pureza, I.R.; da Silva, A.E., Jr.; Silva Praxedes, D.R.; Lessa Vasconcelos, L.G.; de Lima Macena, M.; Vieira de Melo, I.S.; de Menezes Toledo Florêncio, T.M.; Bueno, N.B. Effects of Time-Restricted Feeding on Body Weight, Body Composition and Vital Signs in Low-Income Women with Obesity: A 12-Month Randomized Clinical Trial. Clin. Nutr. 2021, 40, 759–766. [Google Scholar] [CrossRef]
- Domaszewski, P.; Konieczny, M.; Pakosz, P.; Łukaniszyn-Domaszewska, K.; Mikuláková, W.; Sadowska-Krępa, E.; Anton, S. Effect of a Six-Week Times Restricted Eating Intervention on the Body Composition in Early Elderly Men with Overweight. Sci. Rep. 2022, 12, 9816. [Google Scholar] [CrossRef]
- Liu, D.; Huang, Y.; Huang, C.; Yang, S.; Wei, X.; Zhang, P.; Guo, D.; Lin, J.; Xu, B.; Li, C.; et al. Calorie Restriction with or without Time-Restricted Eating in Weight Loss. N. Engl. J. Med. 2022, 386, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.A.; Zaman, A.; Sloggett, K.J.; Steinke, S.; Grau, L.; Catenacci, V.A.; Cornier, M.; Rynders, C.A. Early Time-restricted Eating Compared with Daily Caloric Restriction: A Randomized Trial in Adults with Obesity. Obesity 2022, 30, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, J.d.N.; Macedo, R.C.O.; dos Santos, G.C.; Munhoz, S.V.; Machado, C.L.F.; de Menezes, R.L.; Menzem, E.N.; Moritz, C.E.J.; Pinto, R.S.; Tinsley, G.M.; et al. Cardiometabolic Effects of Early v. Delayed Time-Restricted Eating plus Energetic Restriction in Adults with Overweight and Obesity: An Exploratory Randomised Clinical Trial. Br. J. Nutr. 2023, 129, 637–649. [Google Scholar] [CrossRef]
- Domaszewski, P.; Konieczny, M.; Dybek, T.; Łukaniszyn-Domaszewska, K.; Anton, S.; Sadowska-Krępa, E.; Skorupska, E. Comparison of the Effects of Six-Week Time-Restricted Eating on Weight Loss, Body Composition, and Visceral Fat in Overweight Older Men and Women. Exp. Gerontol. 2023, 174, 112116. [Google Scholar] [CrossRef]
- Irani, H.; Abiri, B.; Khodami, B.; Yari, Z.; Lafzi Ghazi, M.; Hosseinzadeh, N.; Saidpour, A. Effect of Time Restricted Feeding on Anthropometric Measures, Eating Behavior, Stress, Serum Levels of BDNF and LBP in Overweight/Obese Women with Food Addiction: A Randomized Clinical Trial. Nutr. Neurosci. 2024, 27, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Cienfuegos, S.; Ezpeleta, M.; Gabel, K.; Pavlou, V.; Mulas, A.; Chakos, K.; McStay, M.; Wu, J.; Tussing-Humphreys, L.; et al. Time-Restricted Eating Without Calorie Counting for Weight Loss in a Racially Diverse Population: A Randomized Controlled Trial. Ann. Intern. Med. 2023, 176, 885–895. [Google Scholar] [CrossRef]
- Steger, F.L.; Jamshed, H.; Bryan, D.R.; Richman, J.S.; Warriner, A.H.; Hanick, C.J.; Martin, C.K.; Salvy, S.-J.; Peterson, C.M. Early Time-Restricted Eating Affects Weight, Metabolic Health, Mood, and Sleep in Adherent Completers: A Secondary Analysis. Obesity 2023, 31 (Suppl. S1), 96–107. [Google Scholar] [CrossRef]
- Ameur, R.; Maaloul, R.; Tagougui, S.; Neffati, F.; Hadj Kacem, F.; Najjar, M.F.; Ammar, A.; Hammouda, O. Unlocking the Power of Synergy: High-Intensity Functional Training and Early Time-Restricted Eating for Transformative Changes in Body Composition and Cardiometabolic Health in Inactive Women with Obesity. PLoS ONE 2024, 19, e0301369. [Google Scholar] [CrossRef]
- Cienfuegos, S.; Gabel, K.; Kalam, F.; Ezpeleta, M.; Pavlou, V.; Lin, S.; Wiseman, E.; Varady, K.A. The Effect of 4-h versus 6-h Time Restricted Feeding on Sleep Quality, Duration, Insomnia Severity and Obstructive Sleep Apnea in Adults with Obesity. Nutr. Health Berkhamsted Herts. 2022, 28, 5–11. [Google Scholar] [CrossRef]
- Adafer, R.; Messaadi, W.; Meddahi, M.; Patey, A.; Haderbache, A.; Bayen, S.; Messaadi, N. Food Timing, Circadian Rhythm and Chrononutrition: A Systematic Review of Time-Restricted Eating’s Effects on Human Health. Nutrients 2020, 12, 3770. [Google Scholar] [CrossRef]
- Longo, V.D.; Panda, S. Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan. Cell Metab. 2016, 23, 1048–1059. [Google Scholar] [CrossRef] [PubMed]
- Arble, D.M.; Bass, J.; Laposky, A.D.; Vitaterna, M.H.; Turek, F.W. Circadian Timing of Food Intake Contributes to Weight Gain. Obesity 2009, 17, 2100–2102. [Google Scholar] [CrossRef] [PubMed]
- Manoogian, E.N.C.; Chow, L.S.; Taub, P.R.; Laferrère, B.; Panda, S. Time-Restricted Eating for the Prevention and Management of Metabolic Diseases. Endocr. Rev. 2022, 43, 405–436. [Google Scholar] [CrossRef]
- Chantranupong, L.; Wolfson, R.L.; Sabatini, D.M. Nutrient-Sensing Mechanisms across Evolution. Cell 2015, 161, 67–83. [Google Scholar] [CrossRef] [PubMed]
- Garrow, J.S.; Summerbell, C.D. Meta-Analysis: Effect of Exercise, with or without Dieting, on the Body Composition of Overweight Subjects. Eur. J. Clin. Nutr. 1995, 49, 1–10. [Google Scholar]
- Batsis, J.A.; Villareal, D.T. Sarcopenic Obesity in Older Adults: Aetiology, Epidemiology and Treatment Strategies. Nat. Rev. Endocrinol. 2018, 14, 513–537. [Google Scholar] [CrossRef]
- Westerterp-Plantenga, M.S.; Nieuwenhuizen, A.; Tomé, D.; Soenen, S.; Westerterp, K.R. Dietary Protein, Weight Loss, and Weight Maintenance. Annu. Rev. Nutr. 2009, 29, 21–41. [Google Scholar] [CrossRef]
- Cava, E.; Yeat, N.C.; Mittendorfer, B. Preserving Healthy Muscle during Weight Loss. Adv. Nutr. 2017, 8, 511–519. [Google Scholar] [CrossRef]
- Rennie, M.J.; Wackerhage, H.; Spangenburg, E.E.; Booth, F.W. Control of the Size of the Human Muscle Mass. Annu. Rev. Physiol. 2004, 66, 799–828. [Google Scholar] [CrossRef]
- Krieger, J.W.; Sitren, H.S.; Daniels, M.J.; Langkamp-Henken, B. Effects of Variation in Protein and Carbohydrate Intake on Body Mass and Composition during Energy Restriction: A Meta-Regression. Am. J. Clin. Nutr. 2006, 83, 260–274. [Google Scholar] [CrossRef]
- Varady, K.A.; Lin, S.; Oddo, V.M.; Cienfuegos, S. Debunking the Myths of Intermittent Fasting. Nat. Rev. Endocrinol. 2024, 20, 503–504. [Google Scholar] [CrossRef] [PubMed]
- Laurens, C.; Grundler, F.; Damiot, A.; Chery, I.; Le Maho, A.; Zahariev, A.; Le Maho, Y.; Bergouignan, A.; Gauquelin-Koch, G.; Simon, C.; et al. Is Muscle and Protein Loss Relevant in Long-Term Fasting in Healthy Men? A Prospective Trial on Physiological Adaptations. J. Cachexia Sarcopenia Muscle 2021, 12, 1690–1703. [Google Scholar] [CrossRef]
- Peterson, M.D.; Sen, A.; Gordon, P.M. Influence of Resistance Exercise on Lean Body Mass in Aging Adults: A Meta-Analysis. Med. Sci. Sports Exerc. 2011, 43, 249–258. [Google Scholar] [CrossRef]
- Pasiakos, S.M.; Cao, J.J.; Margolis, L.M.; Sauter, E.R.; Whigham, L.D.; McClung, J.P.; Rood, J.C.; Carbone, J.W.; Combs, G.F.; Young, A.J. Effects of High-Protein Diets on Fat-Free Mass and Muscle Protein Synthesis Following Weight Loss: A Randomized Controlled Trial. FASEB J. 2013, 27, 3837–3847. [Google Scholar] [CrossRef]
- Dai, Z.; Wan, K.; Miyashita, M.; Ho, R.S.; Zheng, C.; Poon, E.T.; Wong, S.H. The Effect of Time-Restricted Eating Combined with Exercise on Body Composition and Metabolic Health: A Systematic Review and Meta-Analysis. Adv. Nutr. 2024, 15, 100262. [Google Scholar] [CrossRef]
- Ravussin, E.; Beyl, R.A.; Poggiogalle, E.; Hsia, D.S.; Peterson, C.M. Early Time-Restricted Feeding Reduces Appetite and Increases Fat Oxidation But Does Not Affect Energy Expenditure in Humans. Obesity 2019, 27, 1244–1254. [Google Scholar] [CrossRef]
- Moon, S.; Kang, J.; Kim, S.H.; Chung, H.S.; Kim, Y.J.; Yu, J.M.; Cho, S.T.; Oh, C.-M.; Kim, T. Beneficial Effects of Time-Restricted Eating on Metabolic Diseases: A Systemic Review and Meta-Analysis. Nutrients 2020, 12, 1267. [Google Scholar] [CrossRef] [PubMed]
- Sutton, E.F.; Beyl, R.; Early, K.S.; Cefalu, W.T.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metab. 2018, 27, 1212–1221.e3. [Google Scholar] [CrossRef] [PubMed]
- Chaix, A.; Zarrinpar, A.; Miu, P.; Panda, S. Time-Restricted Feeding Is a Preventative and Therapeutic Intervention against Diverse Nutritional Challenges. Cell Metab. 2014, 20, 991–1005. [Google Scholar] [CrossRef]
- Ryan, D.H.; Yockey, S.R. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr. Obes. Rep. 2017, 6, 187–194. [Google Scholar] [CrossRef]
- Gooley, J.J. Circadian Regulation of Lipid Metabolism. Proc. Nutr. Soc. 2016, 75, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Stiegler, P.; Cunliffe, A. The Role of Diet and Exercise for the Maintenance of Fat-Free Mass and Resting Metabolic Rate during Weight Loss. Sports Med. 2006, 36, 239–262. [Google Scholar] [CrossRef] [PubMed]
| Study | Participants | BMI (kg/m2) | Group (n) | TRE Protocol (Fasting: Eating) | TRE Eating Time | Diet and Exercise Interventions | Duration (Weeks) |
|---|---|---|---|---|---|---|---|
| Chow et al., 2020 [29] | 3 M, 17 F; 46 ± 12 y; overweight and obese adults | 34 ± 8 | TRE (11) CON (9) | 16:08 | Self-selecting | 12 | |
| Cienfuegos et al., 2020 [10] | 5 M, 53 F; 46 ± 3 y; obese adults | 37 ± 1 | 4-h TRE (19) 6-h TRE (20) CON (19) | 20:04; 18:06 | 15:00–19:00; 13:00–19:00 | 8 | |
| Domaszewski et al., 2020 [30] | 45 F; 65 ± 5 y; overweight adults | 28 ± 5 | TRE (25) CON (20) | 16:08 | 12:00–20:00 | 6 | |
| Lowe et al., 2020 [13] | 70 M, 46 F; 47 ± 11 y; overweight and obese adults | 31 ± 4 | TRE (59) CON (57) | 16:08 | 12:00–20:00 | 12 | |
| Kotarsky et al., 2021 [31] | 3 M, 18 F; 44 ± 7 y; overweight and obese adults | 30 ± 3 | TRE (11) CON (10) | 16:08 | 12:00–20:00 | Concurrent training: aerobic and supervised resistance training | 8 |
| Isenmann et al., 2021 [32] | 14 M, 21 F; 28 ± 5 y; overweight adults | 26 | TRE (18) MBD (17) | 16:08 | 12:00–20:00 | At least two training sessions per week at the local gym; diets contain 45–65% carbohydrate, 20–35% fat, and 20–35% protein | 14 |
| Isabele et al., 2021 [33] | 58 F; 31.4 ± 7 y; overweight and obese females | 33 ± 4 | HD + TRE (31) HD (27) | 12:12 | Self-selecting | Subtract 500–1000 kcal from total energy consumption | 52 |
| Haganes et al., 2022 [28] | 131 F; 36 ± 6 y; overweight and obese females | 32 ± 4 | TRE + HIIT (33) CON (32) TRE (33) HIIT (33) | 14:10 | No later than 20:00 | High-intensity interval training supervised treadmill training three times per week | 7 |
| Domaszewski et al., 2022 [34] | 46 M; 70 ± 3 y; overweight adults | 28 ± 2 | TRE (23) CON (23) | 16:08 | 12:00–20:00 | 6 | |
| Liu et al., 2022 [35] | 71 M, 68 F; 32 ± 9 y; overweight and obese adults | 32 ± 3 | TRE (69) CON (70) | 16:08 | 8:00–16:00 | Diets contain 40–55% carbohydrate, 5–20% protein, and 20–30% fat; the regimen accounts for approximately 75% of the subject’s baseline daily caloric intake (F:1200–1500 kcal/d) (M:1500–1800 kcal/d) | 52 |
| Zhang et al., 2022 [12] | 33 M, 27 F; 23 ± 1 y; overweight and obese adults | 28 ± 1 | eTRE (41) CON (19) | 18:06 | 7:00–13:00; 12:00–18:00 | 8 | |
| Jamshed et al., 2022 [11] | 18 M, 72 F; 43 ± 11 y; obese adults | 40 ± 7 | eTRE + ER (45) CON + ER (45) | 16:08 | 7:00–15:00 | Low-calorie diet (500 kcal/d lower than resting energy expenditure) and 75–150 min/week of exercise is recommended | 14 |
| Thomas et al., 2022 [36] | 12 M, 69 F; 38 ± 8 y; overweight and obese adults | 34 ± 6 | eTRE + DCR (41) DCR (40) | 14:10 | Within 3 h of waking | Diets contain 35% caloric restriction (10% reduction in personal resting energy expenditure); 150 min/week of moderate-intensity physical activity is recommended | 39 |
| Queiroz et al., 2023 [37] | 6 M, 42 F; 30 ± 6 y; overweight and obese adults | 31 ± 3 | eTRE (16) dTRE (16) CON (16) | 16:08 | 8:00–16:00; 12:00–20:00 | Energy restriction (resting energy*1.4 PAL-25% of daily energy requirement), a diet consisting of 50% carbohydrate, 20% protein, and 30% fat | 8 |
| Fagundes et al., 2023 [21] | 36 F; 35 ± 9 y; overweight and obese females | 30 ± 3 | TRE (24) CON (12) | 16:08 | 8:00–16:00 or 12:00–20:00 | Diets contain 40–45% carbohydrate, 30–35% fat, and 20–25% protein; energy limitation range 513–770 kcal/d | 8 |
| Domaszewski et al., 2023 [38] | 51 M, 57 F; 69 ± 4 y; overweight adults | 28 ± 3 | TRE (54) CON (54) | 16:08 | 12:00–20:00 | 6 | |
| Irani et al., 2023 [39] | 56 F; 42 ± 9 y; overweight and obese females | 31 ± 4 | TRE (29) CON (27) | 14:10 | 10:00–20:00 | Low-calorie diet (total calories calculated by multiplying the Mifflin-St. Joer formula by the coefficient of physical activity and the thermic effect of the food, from which 300–500 kcal are subtracted), with 52% carbohydrates, 18% proteins, and 30% fats | 8 |
| Lin et al., 2023 [40] | 10 M, 50 F; 40 ± 11 y; obese adults | 38 ± 6 | TRE (30) CON (30) | 16:08, 14:10 | BM loss phase (12:00–20:00); BM maintenance phase (10:00–20:00) | 52 | |
| Steger et al., 2023 [41] | 10 M, 26 F; 44 ± 12 y; obese adults | 38 ± 6 | eTRE + ER (15) CON + ER (21) | 16:08 | 7:00–15:00 | Low-calorie diet (500 kcal/d lower than resting energy expenditure) and 75–150 min/week of exercise is recommended | 14 |
| Ameur et al., 2024 [42] | 44 F; 32 ± 10 y; obese females | 35 ± 4 | TRE (20) CON (24) | 16:08 | 8:00–16:00 | HIFT was performed 3 days per week on Monday, Wednesday, and Friday in the evening at the fasting window (i.e., 5:00 pm) | 12 |
| Study | Outcomes (TRE vs. Control) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BF% | FM | LM | BM | BMI | WC | TC | HDL | LDL | TG | |
| Chow et al., 2020 [29] | ↔ | ↔ | ↓ | ↓ | ↔ | ↔ | ↔ | |||
| Cienfuegos et al., 2020 (6 h) [10] | ↓ | ↓ | ↔ | ↔ | ↔ | |||||
| Domaszewski et al., 2020 [30] | ↓ | ↓ | ↔ | ↔ | ↓ | ↓ | ||||
| Lowe et al., 2020 [13] | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ |
| Kotarsky et al., 2021 [31] | ↓ | ↔ | ↓ | ↓ | ↔ | ↔ | ↔ | |||
| Isabele et al., 2021 [33] | ↓ | ↔ | ↔ | ↔ | ||||||
| Haganes et al., 2022 (TRE vs. CON) [28] | ↓ | ↓ | ↔ | ↔ | ↔ | ↔ | ||||
| Haganes et al., 2022 (TRE + HIIT vs. HIIT) [28] | ↓ | ↓ | ↔ | ↔ | ↔ | ↔ | ||||
| Domaszewski et al., 2022 [34] | ↓ | ↓ | ↔ | ↓ | ↓ | ↓ | ||||
| Zhang et al., 2022 [12] | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↔ | ↔ | ↑ | ↔ |
| Liu et al., 2022 [35] | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ |
| Jamshed et al., 2022 [11] | ↔ | ↔ | ↓ | ↔ | ↔ | ↔ | ↔ | ↔ | ||
| Thomas et al., 2022 [36] | ↔ | ↔ | ↔ | |||||||
| Queiroz et al., 2023 [37] | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | |
| Fagundes et al., 2023 [21] | ↓ | ↓ | ↓ | ↓ | ↓ | ↔ | ||||
| Domaszewski et al., 2023 [38] | ↔ | ↔ | ↔ | |||||||
| Irani et al., 2023 [39] | ↔ | ↓ | ↓ | ↓ | ↓ | |||||
| Lin et al., 2023 [40] | ↓ | ↔ | ↓ | ↓ | ↓ | ↔ | ↔ | ↔ | ↔ | |
| Steger et al., 2023 [41] | ↓ | ↔ | ↓ | |||||||
| Ameur et al., 2024 [42] | ↓ | ↔ | ↓ | ↓ | ↓ | ↓ | ↔ | ↔ | ↓ | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, Y.; Zhou, K.; Shang, Z.; Bao, D.; Zhou, J. The Effects of Time-Restricted Eating on Fat Loss in Adults with Overweight and Obese Depend upon the Eating Window and Intervention Strategies: A Systematic Review and Meta-Analysis. Nutrients 2024, 16, 3390. https://doi.org/10.3390/nu16193390
Xie Y, Zhou K, Shang Z, Bao D, Zhou J. The Effects of Time-Restricted Eating on Fat Loss in Adults with Overweight and Obese Depend upon the Eating Window and Intervention Strategies: A Systematic Review and Meta-Analysis. Nutrients. 2024; 16(19):3390. https://doi.org/10.3390/nu16193390
Chicago/Turabian StyleXie, Yixun, Kaixiang Zhou, Zhangyuting Shang, Dapeng Bao, and Junhong Zhou. 2024. "The Effects of Time-Restricted Eating on Fat Loss in Adults with Overweight and Obese Depend upon the Eating Window and Intervention Strategies: A Systematic Review and Meta-Analysis" Nutrients 16, no. 19: 3390. https://doi.org/10.3390/nu16193390
APA StyleXie, Y., Zhou, K., Shang, Z., Bao, D., & Zhou, J. (2024). The Effects of Time-Restricted Eating on Fat Loss in Adults with Overweight and Obese Depend upon the Eating Window and Intervention Strategies: A Systematic Review and Meta-Analysis. Nutrients, 16(19), 3390. https://doi.org/10.3390/nu16193390






