The Beneficial Effects of Regular Intake of Lactobacillus paragasseri OLL2716 on Gastric Discomfort in Healthy Adults: A Randomized, Double-Blind, Placebo-Controlled Study
Abstract
1. Introduction
2. Materials and Methods
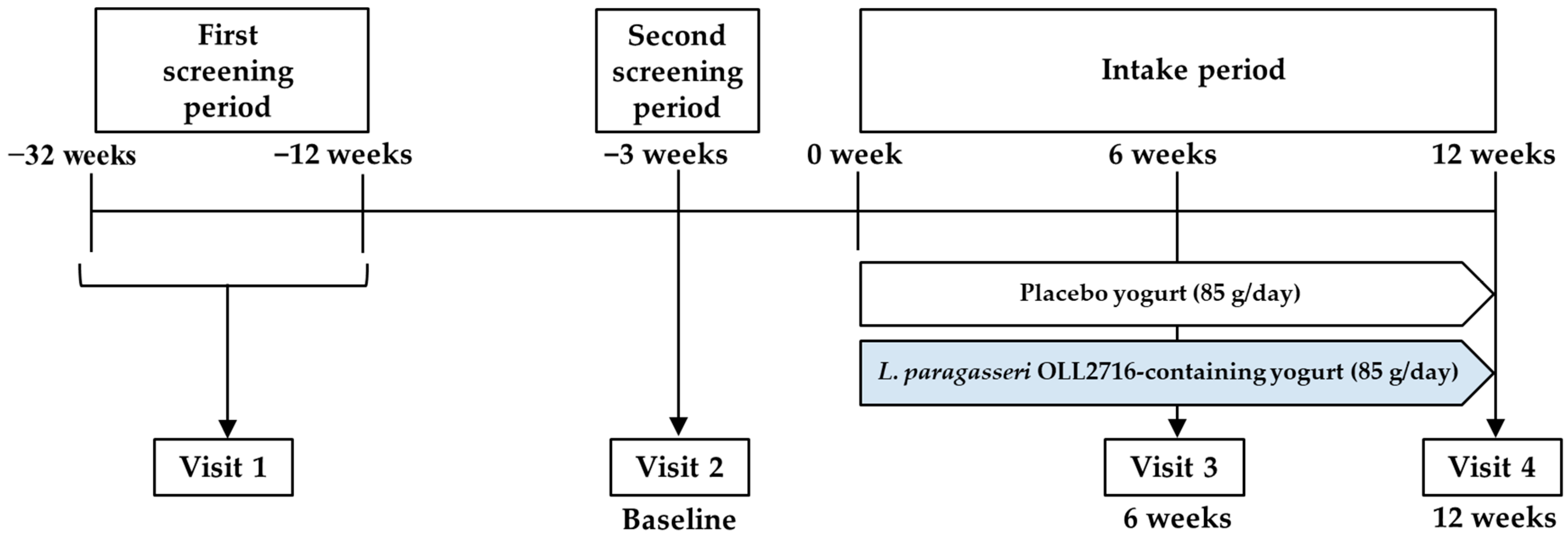
2.1. Study Design
2.2. Participants
2.3. Study Protocol
2.4. Helicobacter Pylori Screening Test
2.5. FD Rome IV Diagnostic Criteria
2.6. Individual Gastric Symptom Scores (Questionnaire for Gastric Symptoms of the Participants)
2.7. Short-Form Nepean Dyspepsia Index (SF-NDI)
2.8. Gastrointestinal Symptom Rating Scale (GSRS)
2.9. Council on Nutrition Appetite Questionnaire-Japanese (CNAQ-J)
2.10. Statistical Analyses
3. Results
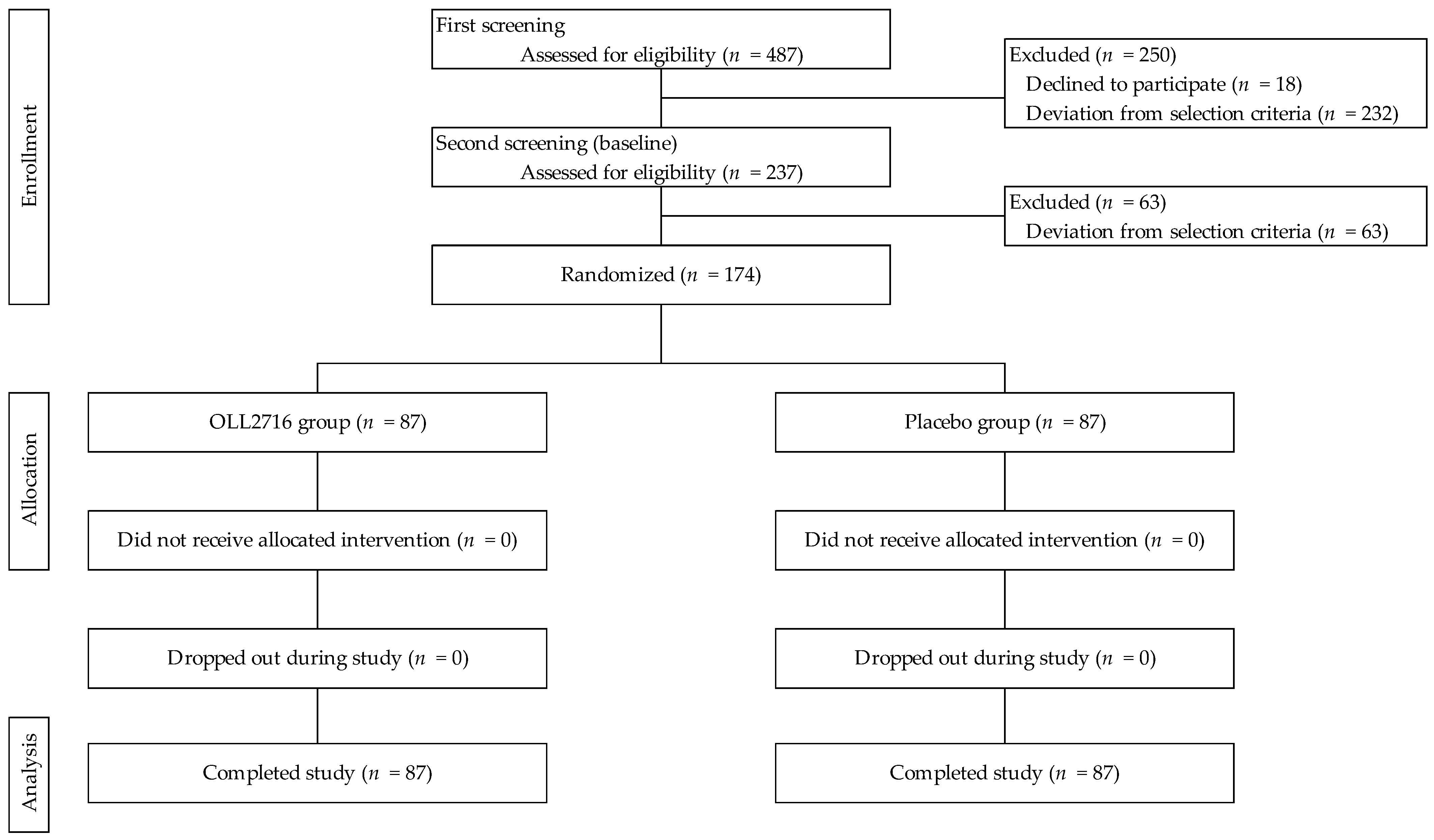
3.1. Participant Selection and Baseline Characteristics
3.2. Primary Endpoint
3.3. Secondary Endpoints
3.3.1. SF-NDI
3.3.2. GSRS
3.3.3. CNAQ-J
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parkman, H.P.; Hasler, W.L.; Fisher, R.S. American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Gastroenterology 2004, 127, 1592–1622. [Google Scholar] [CrossRef] [PubMed]
- Browning, K.N. Stress-induced modulation of vagal afferents. Neurogastroenterol. Motil. 2019, 31, e13758. [Google Scholar] [CrossRef] [PubMed]
- Ohtsu, T.; Haruma, K.; Ide, Y.; Takagi, A. The effect of continuous intake of Lactobacillus gasseri OLL2716 on mild to moderate delayed gastric emptying: A randomized controlled study. Nutrients 2021, 13, 1852. [Google Scholar] [CrossRef] [PubMed]
- Vijayvargiya, P.; Jameie-Oskooei, S.; Camilleri, M.; Chedid, V.; Erwin, P.J.; Murad, M.H. Association between delayed gastric emptying and upper gastrointestinal symptoms: A systematic review and meta-analysis. Gut 2019, 68, 804–813. [Google Scholar] [CrossRef]
- Travagli, R.A.; Anselmi, L. Vagal neurocircuitry and its influence on gastric motility. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 389–401. [Google Scholar] [CrossRef]
- Holtmann, G.; Talley, N.J. The stomach–brain axis. Best Pract. Res. Clin. Gastroenterol. 2014, 28, 967–979. [Google Scholar] [CrossRef]
- Rebollo, I.; Devauchelle, A.D.; Béranger, B.; Tallon-Baudry, C. Stomach-brain synchrony reveals a novel, delayed-connectivity resting-state network in humans. eLife 2018, 7, e33321. [Google Scholar] [CrossRef]
- Konturek, P.C.; Brzozowski, T.; Konturek, S.J. Stress and the gut: Pathophysiology, clinical consequences, diagnostic approach, and treatment options. J. Physiol. Pharmacol. 2011, 62, 591–599. [Google Scholar]
- Aro, P.; Talley, N.J.; Agréus, L.; Johansson, S.E.; Bolling-Sternevald, E.; Storskrubb, T.; Ronkainen, J. Functional dyspepsia impairs quality of life in the adult population. Aliment. Pharmacol. Ther. 2011, 33, 1215–1224. [Google Scholar] [CrossRef]
- Talley, N.J.; Locke, G.R., 3rd; Lahr, B.D.; Zinsmeister, A.R.; Tougas, G.; Ligozio, G.; Rojavin, M.A.; Tack, J. Functional dyspepsia, delayed gastric emptying, and impaired quality of life. Gut 2006, 55, 933–939. [Google Scholar] [CrossRef]
- Jones, M.P.; Tack, J.; Van Oudenhove, L.; Walker, M.M.; Holtmann, G.; Koloski, N.A.; Talley, N.J. Mood and anxiety disorders precede development of functional gastrointestinal disorders in patients but not in the population. Clin. Gastroenterol. Hepatol. 2017, 15, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Koloski, N.A.; Jones, M.; Kalantar, J.; Weltman, M.; Zaguirre, J.; Talley, N.J. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: A 12-year prospective population-based study. Gut 2012, 61, 1284–1290. [Google Scholar] [CrossRef] [PubMed]
- Koloski, N.A.; Jones, M.; Talley, N.J. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: A 1-year, population-based prospective study. Aliment. Pharmacol. Ther. 2016, 44, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Black, C.J.; Drossman, D.A.; Talley, N.J.; Ruddy, J.; Ford, A.C. Functional gastrointestinal disorders: Advances in understanding and management. Lancet 2020, 396, 1664–1674. [Google Scholar] [CrossRef]
- Otomi, K.; Ymaguchi, T.; Watanabe, S.; Kobayashi, A.; Kobayashi, H.; Hashiguchi, N. Effects of yogurt containing Lactobacillus gasseri OLL2716 on autonomic nerve activities and physiological functions. Health 2015, 7, 397–405. [Google Scholar] [CrossRef]
- Gomi, A.; Yamaji, K.; Watanabe, O.; Yoshioka, M.; Miyazaki, K.; Iwama, Y.; Urita, Y. Bifidobacterium bifidum YIT 10347 fermented milk exerts beneficial effects on gastrointestinal discomfort and symptoms in healthy adults: A double-blind, randomized, placebo-controlled study. J. Dairy Sci. 2018, 101, 4830–4841. [Google Scholar] [CrossRef]
- Sakamoto, I.; Igarashi, M.; Kimura, K.; Takagi, A.; Miwa, T.; Koga, Y. Suppressive effect of Lactobacillus gasseri OLL 2716 (LG21) on Helicobacter pylori infection in humans. J. Antimicrob. Chemother. 2001, 47, 709–710. [Google Scholar] [CrossRef]
- Ohtsu, T.; Takagi, A.; Uemura, N.; Inoue, K.; Sekino, H.; Kawashima, A.; Uchida, M.; Koga, Y. The ameliorating effect of Lactobacillus gasseri OLL2716 on functional dyspepsia in Helicobacter pylori-uninfected individuals: A randomized, controlled study. Digestion 2017, 96, 92–102. [Google Scholar] [CrossRef]
- Stanghellini, V.; Chan, F.K.; Hasler, W.L.; Malagelada, J.R.; Suzuki, H.; Tack, J.; Talley, N.J. Gastroduodenal disorders. Gastroenterology 2016, 150, 1380–1392. [Google Scholar] [CrossRef]
- Tack, J.; Talley, N.J.; Camilleri, M.; Holtmann, G.; Hu, P.; Malagelada, J.R.; Stanghellini, V. Functional gastroduodenal disorders. Gastroenterology 2006, 130, 1466–1479. [Google Scholar] [CrossRef]
- Veldhuyzen van Zanten, S.J.; Chiba, N.; Armstrong, D.; Barkun, A.N.; Thomson, A.B.; Mann, V.; Escobedo, S.; Chakraborty, B.; Nevin, K. Validation of a 7-point Global Overall Symptom scale to measure the severity of dyspepsia symptoms in clinical trials. Aliment. Pharmacol. Ther. 2006, 23, 521–529. [Google Scholar] [CrossRef]
- Iwakiri, R.; Tominaga, K.; Furuta, K.; Inamori, M.; Furuta, T.; Masuyama, H.; Kanke, K.; Nagahara, A.; Haruma, K.; Kinoshita, Y.; et al. Randomised clinical trial: Rabeprazole improves symptoms in patients with functional dyspepsia in Japan. Aliment. Pharmacol. Ther. 2013, 38, 729–740. [Google Scholar] [CrossRef] [PubMed]
- Talley, N.J.; Verlinden, M.; Jones, M. Quality of life in functional dyspepsia: Responsiveness of the Nepean Dyspepsia Index and development of a new 10-item short form. Aliment. Pharmacol. Ther. 2001, 15, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Arslan, G.; Lind, R.; Olafsson, S.; Florvaag, E.; Berstad, A. Quality of life in patients with subjective food hypersensitivity: Applicability of the 10-item short form of the Nepean Dyspepsia Index. Dig. Dis. Sci. 2004, 49, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Kulich, K.R.; Madisch, A.; Pacini, F.; Piqué, J.M.; Regula, J.; Van Rensburg, C.J.; Ujszászy, L.; Carlsson, J.; Halling, K.; Wiklund, I.K. Reliability and validity of the Gastrointestinal Symptom Rating Scale (GSRS) and Quality of Life in Reflux and Dyspepsia (QOLRAD) questionnaire in dyspepsia: A six-country study. Health Qual. Life Outcomes 2008, 6, 12. [Google Scholar] [CrossRef] [PubMed]
- Revicki, D.A.; Wood, M.; Wiklund, I.; Crawley, J. Reliability and validity of the Gastrointestinal Symptom Rating Scale in patients with gastroesophageal reflux disease. Qual. Life Res. 1998, 7, 75–83. [Google Scholar] [CrossRef]
- Tokudome, Y.; Okumura, K.; Kumagai, Y.; Hirano, H.; Kim, H.; Morishita, S.; Watanabe, Y. Development of the Japanese version of the Council on Nutrition Appetite Questionnaire and its simplified versions, and evaluation of their reliability, validity, and reproducibility. J. Epidemiol. 2017, 27, 524–530. [Google Scholar] [CrossRef]
- Wilson, M.M.G.; Thomas, D.R.; Rubenstein, L.Z.; Chibnall, J.T.; Anderson, S.; Baxi, A.; Diebold, M.R.; Morley, J.E. Appetite assessment: Simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am. J. Clin. Nutr. 2005, 82, 1074–1081. [Google Scholar] [CrossRef]
- Tack, J.; Verbeure, W.; Mori, H.; Schol, J.; van den Houte, K.; Huang, I.H.; Balsiger, L.; Broeders, B.; Colomier, E.; Scarpellini, E.; et al. The gastrointestinal tract in hunger and satiety signalling. United Eur. Gastroenterol. J. 2021, 9, 727–734. [Google Scholar] [CrossRef]
- Nakamura, C.; Ishii, A.; Matsuo, T.; Ishida, R.; Yamaguchi, T.; Takada, K.; Uji, M.; Yoshikawa, T. Neural effects of acute stress on appetite: A magnetoencephalography study. PLoS ONE 2020, 15, e0228039. [Google Scholar] [CrossRef]
- Petrowski, K.; Wintermann, G.B.; Joraschky, P.; Päßler, S. Chewing after stress: Psychosocial stress influences chewing frequency, chewing efficacy, and appetite. Psychoneuroendocrinology 2014, 48, 64–76. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K. Health benefits of probiotics: Probiotics for Helicobacter pylori infection. Food Sci. Technol. Res. 2004, 10, 1–5. [Google Scholar] [CrossRef][Green Version]
- Takagi, A.; Yanagi, H.; Ozawa, H.; Uemura, N.; Nakajima, S.; Inoue, K.; Kawai, T.; Ohtsu, T.; Koga, Y. Effects of Lactobacillus gasseri OLL2716 on Helicobacter pylori-associated dyspepsia: A multicenter, randomized, double-blind, controlled trial. Gastroenterol. Res. Pract. 2016, 2016, 7490452. [Google Scholar] [CrossRef] [PubMed]
- Koga, Y.; Ohtsu, T.; Kimura, K.; Asami, Y. Probiotic L. gasseri strain (LG21) for the upper gastrointestinal tract acting through improvement of indigenous microbiota. BMJ Open Gastroenterol. 2019, 6, e000314. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Yoshida, K.; Uchida, M. Novel functions of bovine milk-derived α-lactalbumin: Anti-nociceptive and anti-inflammatory activity caused by inhibiting cyclooxygenase-2 and phospholipase A2. Biol. Pharm. Bull. 2009, 32, 366–371. [Google Scholar] [CrossRef]
- Carrillo, W.; Monteiro, K.M.; Spindola, H.; Ramos, M.; de Carvalho, J.E. Antiulcerative and antinociceptive activities of casein and whey proteins. J. Med. Food 2018, 21, 605–611. [Google Scholar] [CrossRef]
- Lukic, S.; Mijac, D.; Filipovic, B.; Sokic-Milutinovic, A.; Tomasevic, R.; Krstic, M.; Milosavljevic, T. Chronic abdominal pain: Gastroenterologist approach. Dig. Dis. 2022, 40, 181–186. [Google Scholar] [CrossRef]
- Bailey, J.M. Gastrointestinal conditions: Peptic ulcer disease. FP Essent. 2024, 540, 16–23. [Google Scholar]
- Scida, S.; Russo, M.; Miraglia, C.; Leandro, G.; Franzoni, L.; Meschi, T.; De’Angelis, G.L.; Di Mario, F. Relationship between Helicobacter pylori infection and GERD. Acta Biomed. 2018, 89, 40–43. [Google Scholar] [CrossRef]
- Leung, W.K.; Graham, D.Y. Ulcer and gastritis. Endoscopy 2001, 33, 8–15. [Google Scholar] [CrossRef]
- Mayer, E.A. The neurobiology of stress and gastrointestinal disease. Gut 2000, 47, 861–869. [Google Scholar] [CrossRef]
| Characteristics | OLL2716 (n = 87) | Placebo (n = 87) | p-Value |
|---|---|---|---|
| Female | 55 | 56 | 0.875 1 |
| Male | 32 | 31 | |
| Age (year) | 37.4 ± 11.9 | 37.0 ± 11.1 | 0.792 2 |
| Postprandial fullness score | 2.5 ± 0.7 | 2.5 ± 0.8 | 0.839 2 |
| Early satiety score | 2.1 ± 0.9 | 2.1 ± 1.0 | 0.814 2 |
| BMI [kg(m2)−1] | 22.2 ± 3.7 | 22.4 ± 3.5 | 0.777 2 |
| Items | Score Change before Ingestion (⊿) | Number of Participants with Improved Scores (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | 0 Week | 6 Weeks | 12 Weeks | 6 Weeks–0 Week | p Value 1 | 12 Weeks–0 Week | p Value 1 | 6 Weeks | p Value 2 | 12 Weeks | p Value 2 | |||
| 1. Postprandial fullness | OLL2716 | 2.5 ± 0.7 | 2.0 ± 0.8 | 1.7 ± 0.9 | −0.5 ± 0.8 | 0.564 | −0.8 ± 1.0 | 0.745 | 37 | (42.5%) | 0.879 | 50 | (57.5%) | 1.000 |
| Placebo | 2.5 ± 0.8 | 1.9 ± 0.9 | 1.6 ± 1.0 | −0.6 ± 1.1 | −0.9 ± 1.2 | 39 | (44.8%) | 49 | (56.3%) | |||||
| 2. Early satiety | OLL2716 | 2.1 ± 0.9 | 1.9 ± 1.0 | 1.6 ± 1.1 | −0.2 ± 1.0 | 0.483 | −0.5 ± 1.0 | 0.841 | 29 | (33.3%) | 0.528 | 37 | (42.5%) | 0.760 |
| Placebo | 2.1 ± 1.0 | 1.8 ± 1.0 | 1.6 ± 1.1 | −0.3 ± 1.0 | −0.5 ± 1.1 | 34 | (39.1%) | 40 | (46.0%) | |||||
| 3. Epigastric bloating | OLL2716 | 2.3 ± 1.1 | 1.9 ± 1.0 | 1.6 ± 1.1 | −0.5 ± 1.1 | 0.362 | −0.7 ± 1.1 | 0.861 | 46 | (52.9%) | 0.544 | 48 | (55.2%) | 1.000 |
| Placebo | 2.2 ± 1.2 | 1.9 ± 1.3 | 1.5 ± 1.1 | −0.4 ± 1.2 | −0.7 ± 1.4 | 41 | (47.1%) | 48 | (55.2%) | |||||
| 4. Epigastric pain | OLL2716 | 1.6 ± 1.1 | 1.1 ± 1.1 | 1.0 ± 1.0 | −0.5 ± 1.3 | 0.020 | −0.7 ± 1.2 | 0.028 | 45 | (51.7%) | 0.032 | 47 | (54.0%) | 0.095 |
| Placebo | 1.3 ± 1.2 | 1.2 ± 1.1 | 1.1 ± 1.0 | −0.1 ± 1.3 | −0.2 ± 1.4 | 30 | (34.5%) | 35 | (40.2%) | |||||
| 5. Epigastric burning | OLL2716 | 1.3 ± 1.2 | 0.9 ± 1.0 | 1.0 ± 1.0 | −0.4 ± 1.0 | 0.256 | −0.4 ± 1.0 | 0.289 | 33 | (37.9%) | 0.753 | 34 | (39.1%) | 0.754 |
| Placebo | 1.1 ± 1.2 | 0.9 ± 0.9 | 0.9 ± 1.0 | −0.3 ± 1.3 | −0.2 ± 1.4 | 30 | (34.5%) | 31 | (35.6%) | |||||
| 6. Heartburn | OLL2716 | 1.5 ± 1.2 | 1.1 ± 1.0 | 1.0 ± 1.0 | −0.5 ± 1.1 | 0.550 | −0.6 ± 1.1 | 0.322 | 37 | (42.5%) | 1.000 | 50 | (57.5%) | 0.225 |
| Placebo | 1.4 ± 1.2 | 1.1 ± 1.1 | 1.0 ± 0.9 | −0.3 ± 1.2 | −0.4 ± 1.3 | 36 | (41.4%) | 41 | (47.1%) | |||||
| 7. Reflex feeling of gastric acid | OLL2716 | 1.5 ± 1.1 | 1.0 ± 1.0 | 1.0 ± 1.0 | −0.5 ± 1.0 | 0.258 | −0.5 ± 1.1 | 0.094 | 41 | (47.1%) | 0.166 | 39 | (44.8%) | 0.442 |
| Placebo | 1.2 ± 1.2 | 0.9 ± 1.0 | 1.0 ± 1.0 | −0.3 ± 1.2 | −0.2 ± 1.3 | 31 | (35.6%) | 33 | (37.9%) | |||||
| 8. Nausea | OLL2716 | 1.0 ± 1.1 | 0.7 ± 1.0 | 0.7 ± 1.0 | −0.3 ± 1.0 | 0.583 | −0.3 ± 0.9 | 0.413 | 29 | (33.3%) | 0.873 | 30 | (34.5%) | 1.000 |
| Placebo | 1.0 ± 1.0 | 0.8 ± 1.0 | 0.8 ± 0.9 | −0.2 ± 1.0 | −0.2 ± 1.2 | 31 | (35.6%) | 30 | (34.5%) | |||||
| 9. Belching | OLL2716 | 1.6 ± 1.2 | 1.4 ± 1.1 | 1.2 ± 1.1 | −0.3 ± 1.1 | 0.653 | −0.4 ± 1.0 | 0.818 | 33 | (37.9%) | 0.877 | 40 | (46.0%) | 1.000 |
| Placebo | 1.7 ± 1.3 | 1.3 ± 1.1 | 1.3 ± 1.0 | −0.3 ± 1.1 | −0.4 ± 1.2 | 35 | (40.2%) | 40 | (46.0%) | |||||
| 10. Abdominal bloating | OLL2716 | 2.1 ± 1.2 | 1.7 ± 1.0 | 1.6 ± 1.2 | −0.4 ± 1.2 | 0.108 | −0.5 ± 1.3 | 0.638 | 43 | (49.4%) | 0.091 | 41 | (47.1%) | 0.649 |
| Placebo | 2.0 ± 1.4 | 1.7 ± 1.3 | 1.4 ± 1.1 | −0.2 ± 1.3 | −0.6 ± 1.4 | 31 | (35.6%) | 45 | (51.7%) | |||||
| PDS-like (1 and 2) | OLL2716 | 4.5 ± 1.3 | 3.8 ± 1.6 | 3.3 ± 1.8 | −0.7 ± 1.5 | 0.455 | −1.2 ± 1.7 | 0.689 | 43 | (49.4%) | 0.880 | 51 | (58.6%) | 0.757 |
| Placebo | 4.6 ± 1.4 | 3.7 ± 1.8 | 3.2 ± 1.9 | −0.9 ± 1.7 | −1.4 ± 2.0 | 45 | (51.7%) | 54 | (62.1%) | |||||
| EPS-like (4 and 5) | OLL2716 | 3.0 ± 2.1 | 2.0 ± 1.9 | 1.9 ± 1.9 | −0.9 ± 2.1 | 0.028 | −1.0 ± 1.9 | 0.073 | 52 | (59.8%) | 0.010 | 49 | (56.3%) | 0.068 |
| Placebo | 2.4 ± 2.0 | 2.1 ± 1.8 | 1.9 ± 1.8 | −0.3 ± 2.3 | −0.5 ± 2.5 | 34 | (39.1%) | 36 | (41.4%) | |||||
| FD-like (PDS-like and EPS-like) | OLL2716 | 7.5 ± 2.9 | 5.9 ± 3.0 | 5.2 ± 3.3 | −1.6 ± 3.0 | 0.207 | −2.3 ± 3.0 | 0.377 | 50 | (57.5%) | 0.129 | 52 | (59.8%) | 0.540 |
| Placebo | 7.0 ± 2.8 | 5.7 ± 3.1 | 5.1 ± 3.4 | −1.3 ± 3.3 | −1.9 ± 4.0 | 39 | (44.8%) | 47 | (54.0%) | |||||
| Items | Score Change before Ingestion (⊿) | Number of Participants with Improved Scores (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | 0 Week | 6 Weeks | 12 Weeks | 6 Weeks–0 Week | p Value 1 | 12 Weeks–0 Week | p Value1 | 6 Weeks | p Value 2 | 12 Weeks | p Value 2 | |
| 1. General emotional well-being | OLL2716 | 2.0 ± 0.6 | 1.7 ± 0.6 | 1.6 ± 0.6 | −0.3 ± 0.7 | 0.084 | −0.4 ± 0.7 | 0.822 | 28 (32.2%) | 0.121 | 39 (44.8%) | 0.760 |
| Placebo | 2.0 ± 0.6 | 1.9 ± 0.6 | 1.6 ± 0.5 | −0.1 ± 0.7 | −0.4 ± 0.7 | 18 (20.7%) | 36 (41.4%) | |||||
| 2. Irritable, tense, or frustrated | OLL2716 | 2.2 ± 0.5 | 1.7 ± 0.6 | 1.6 ± 0.6 | −0.5 ± 0.6 | 0.042 | −0.6 ± 0.7 | 0.666 | 40 (46.0%) | 0.061 | 47 (54.0%) | 0.544 |
| Placebo | 2.2 ± 0.5 | 1.9 ± 0.6 | 1.6 ± 0.6 | −0.3 ± 0.7 | −0.6 ± 0.7 | 27 (31.0%) | 42 (48.3%) | |||||
| 3. Fun (ability) | OLL2716 | 1.7 ± 0.7 | 1.3 ± 0.5 | 1.3 ± 0.5 | −0.3 ± 0.8 | 0.353 | −0.4 ± 0.8 | 0.457 | 34 (39.1%) | 0.429 | 39 (44.8%) | 0.279 |
| Placebo | 1.6 ± 0.8 | 1.4 ± 0.6 | 1.3 ± 0.5 | −0.2 ± 0.7 | −0.3 ± 0.7 | 28 (32.2%) | 31 (35.6%) | |||||
| 4. Fun (enjoyment) | OLL2716 | 1.7 ± 0.7 | 1.3 ± 0.5 | 1.3 ± 0.5 | −0.4 ± 0.8 | 0.284 | −0.4 ± 0.8 | 0.909 | 38 (44.2%) | 0.279 | 39 (45.3%) | 0.760 |
| Placebo | 1.7 ± 0.8 | 1.4 ± 0.7 | 1.3 ± 0.5 | −0.3 ± 0.8 | −0.4 ± 0.7 | 31 (35.6%) | 37 (42.5%) | |||||
| 5. Eat or drink (ability) | OLL2716 | 1.9 ± 0.7 | 1.6 ± 0.6 | 1.4 ± 0.6 | −0.2 ± 0.7 | 0.215 | −0.5 ± 0.7 | 0.226 | 29 (33.3%) | 0.177 | 44 (50.6%) | 0.287 |
| Placebo | 1.8 ± 0.7 | 1.6 ± 0.6 | 1.4 ± 0.6 | −0.1 ± 0.6 | −0.4 ± 0.7 | 20 (23.0%) | 36 (41.4%) | |||||
| 6. Eating or drinking (enjoyment) | OLL2716 | 2.0 ± 0.7 | 1.5 ± 0.6 | 1.4 ± 0.6 | −0.5 ± 0.9 | 0.031 | −0.6 ± 0.8 | 0.150 | 42 (48.3%) | 0.044 | 52 (59.8%) | 0.171 |
| Placebo | 1.9 ± 0.8 | 1.6 ± 0.6 | 1.4 ± 0.6 | −0.2 ± 0.7 | −0.5 ± 0.8 | 28 (32.2%) | 42 (48.3%) | |||||
| 7. Wondered (always) | OLL2716 | 1.7 ± 0.7 | 1.3 ± 0.5 | 1.2 ± 0.5 | −0.4 ± 0.7 | 0.421 | −0.4 ± 0.8 | 0.454 | 31 (35.6%) | 0.63 | 38 (43.7%) | 0.537 |
| Placebo | 1.6 ± 0.8 | 1.4 ± 0.6 | 1.2 ± 0.5 | −0.3 ± 0.8 | −0.4 ± 0.9 | 27 (31.0%) | 33 (37.9%) | |||||
| 8. Thought (very serious illness) | OLL2716 | 1.3 ± 0.5 | 1.1 ± 0.4 | 1.1 ± 0.4 | −0.1 ± 0.5 | 0.182 | −0.2 ± 0.5 | 0.097 | 16 (18.4%) | 0.403 | 19 (21.8%) | 0.328 |
| Placebo | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.1 ± 0.3 | 0.0 ± 0.5 | −0.1 ± 0.5 | 11 (12.6%) | 13 (14.9%) | |||||
| 9. Work or study (ability) | OLL2716 | 1.6 ± 0.6 | 1.5 ± 0.6 | 1.3 ± 0.5 | −0.1 ± 0.7 | 0.620 | −0.3 ± 0.7 | 0.677 | 24 (27.6%) | 1.000 | 30 (34.5%) | 1.000 |
| Placebo | 1.6 ± 0.6 | 1.4 ± 0.7 | 1.3 ± 0.5 | −0.1 ± 0.7 | −0.3 ± 0.6 | 24 (27.6%) | 29 (33.3%) | |||||
| 10. Work or study (enjoyment) | OLL2716 | 1.6 ± 0.7 | 1.4 ± 0.6 | 1.3 ± 0.6 | −0.2 ± 0.8 | 0.681 | −0.3 ± 0.8 | 0.890 | 30 (34.5%) | 0.747 | 31 (35.6%) | 0.749 |
| Placebo | 1.6 ± 0.7 | 1.4 ± 0.6 | 1.3 ± 0.5 | −0.2 ± 0.8 | −0.3 ± 0.7 | 27 (31.0%) | 28 (32.2%) | |||||
| Tension (1 and 2) | OLL2716 | 4.1 ± 0.9 | 3.4 ± 1.1 | 3.1 ± 1.2 | −0.7 ± 1.1 | 0.026 | −1.0 ± 1.2 | 0.675 | 45 (51.7%) | 0.032 | 54 (62.1%) | 0.357 |
| Placebo | 4.2 ± 1.0 | 3.8 ± 1.1 | 3.2 ± 1.1 | −0.4 ± 1.3 | −1.0 ± 1.2 | 30 (34.5%) | 47 (54.0%) | |||||
| Interference with daily activities (3 and 4) | OLL2716 | 3.4 ± 1.2 | 2.7 ± 1.0 | 2.6 ± 1.0 | −0.7 ± 1.4 | 0.262 | −0.8 ± 1.4 | 0.575 | 42 (48.8%) | 0.361 | 46 (53.5%) | 0.288 |
| Placebo | 3.3 ± 1.5 | 2.8 ± 1.3 | 2.5 ± 1.0 | −0.5 ± 1.4 | −0.8 ± 1.3 | 36 (41.4%) | 39 (44.8%) | |||||
| Eating/drinking (5 and 6) | OLL2716 | 3.9 ± 1.3 | 3.2 ± 1.0 | 2.8 ± 1.1 | −0.7 ± 1.4 | 0.057 | −1.1 ± 1.5 | 0.095 | 45 (51.7%) | 0.224 | 56 (64.4%) | 0.217 |
| Placebo | 3.6 ± 1.3 | 3.2 ± 1.1 | 2.8 ± 1.1 | −0.4 ± 1.1 | −0.9 ± 1.3 | 36 (41.4%) | 47 (54.0%) | |||||
| Knowledge/control (7 and 8) | OLL2716 | 3.0 ± 1.0 | 2.5 ± 0.8 | 2.4 ± 0.8 | −0.5 ± 1.0 | 0.240 | −0.6 ± 1.1 | 0.223 | 37 (42.5%) | 0.210 | 41 (47.1%) | 0.358 |
| Placebo | 2.9 ± 1.2 | 2.5 ± 0.9 | 2.4 ± 0.8 | −0.3 ± 1.1 | −0.5 ± 1.3 | 28 (32.2%) | 34 (39.1%) | |||||
| Work/study (9 and 10) | OLL2716 | 3.2 ± 1.3 | 2.8 ± 1.1 | 2.6 ± 1.0 | −0.3 ± 1.5 | 0.977 | −0.6 ± 1.4 | 0.942 | 33 (37.9%) | 0.875 | 36 (41.4%) | 1.000 |
| Placebo | 3.2 ± 1.3 | 2.9 ± 1.3 | 2.6 ± 0.9 | −0.3 ± 1.4 | −0.7 ± 1.2 | 31 (35.6%) | 35 (40.2%) | |||||
| Items | Score Change before Ingestion (⊿) | Number of Participants with Improved Scores (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | 0 Week | 6 Weeks | 12 Weeks | 6 Weeks–0 Week | p Value 1 | 12 Weeks–0 Week | p Value 1 | 6 Weeks | p Value 2 | 12 Weeks | p Value 2 | |
| 1. Abdominal pain | OLL2716 | 2.5 ± 1.1 | 2.0 ± 0.8 | 1.9 ± 0.8 | −0.4 ± 1.2 | 0.369 | −0.6 ± 1.1 | 0.143 | 37 (42.5%) | 0.643 | 48 (55.2%) | 0.288 |
| Placebo | 2.2 ± 1.0 | 2.0 ± 1.0 | 1.8 ± 1.0 | −0.2 ± 1.1 | −0.4 ± 1.1 | 33 (37.9%) | 40 (46.0%) | |||||
| 2. Heartburn | OLL2716 | 2.1 ± 0.8 | 1.9 ± 0.8 | 1.7 ± 0.8 | −0.2 ± 1.0 | 0.439 | −0.4 ± 0.8 | 0.641 | 27 (31.0%) | 0.522 | 38 (43.7%) | 0.879 |
| Placebo | 2.1 ± 1.0 | 1.8 ± 0.9 | 1.6 ± 0.8 | −0.3 ± 1.0 | −0.5 ± 0.9 | 32 (36.8%) | 40 (46.0%) | |||||
| 3. Acid regurgitation | OLL2716 | 2 ± 0.9 | 1.8 ± 0.8 | 1.6 ± 0.7 | −0.2 ± 0.9 | 0.843 | −0.4 ± 0.8 | 0.220 | 26 (29.9%) | 0.736 | 42 (48.3%) | 0.221 |
| Placebo | 1.9 ± 0.9 | 1.7 ± 0.8 | 1.6 ± 0.8 | −0.2 ± 0.9 | −0.3 ± 1.0 | 23 (26.4%) | 33 (37.9%) | |||||
| 4. Sucking sensations in the epigastrium | OLL2716 | 2.1 ± 0.9 | 1.9 ± 0.9 | 1.7 ± 0.8 | −0.2 ± 1.0 | 0.534 | −0.4 ± 1.0 | 0.228 | 34 (39.1%) | 0.340 | 38 (43.7%) | 0.440 |
| Placebo | 2.0 ± 0.8 | 1.8 ± 0.9 | 1.7 ± 0.9 | −0.2 ± 0.9 | −0.2 ± 0.9 | 27 (31.0%) | 32 (36.8%) | |||||
| 5. Nausea and vomiting | OLL2716 | 1.9 ± 1.0 | 1.6 ± 0.9 | 1.6 ± 0.7 | −0.3 ± 1.2 | 0.498 | −0.3 ± 0.8 | 0.701 | 33 (37.9%) | 0.144 | 33 (37.9%) | 0.635 |
| Placebo | 1.9 ± 0.9 | 1.8 ± 0.8 | 1.7 ± 0.9 | −0.1 ± 0.9 | −0.3 ± 0.9 | 23 (26.4%) | 29 (33.3%) | |||||
| 6. Borborygmus | OLL2716 | 2.3 ± 1.1 | 2.4 ± 1.0 | 2.1 ± 1.0 | 0.0 ± 1.0 | 0.089 | −0.3 ± 1.0 | 0.931 | 24 (27.6%) | 0.147 | 34 (39.1%) | 0.754 |
| Placebo | 2.6 ± 1.2 | 2.3 ± 1.1 | 2.2 ± 1.1 | −0.3 ± 1.1 | −0.3 ± 1.2 | 34 (39.1%) | 31 (35.6%) | |||||
| 7. Abdominal distension | OLL2716 | 2.4 ± 1.0 | 2.1 ± 0.8 | 2.0 ± 0.8 | −0.3 ± 1.1 | 0.507 | −0.4 ± 1.0 | 0.654 | 35 (40.2%) | 1.000 | 38 (43.7%) | 0.761 |
| Placebo | 2.4 ± 1.0 | 2.1 ± 0.9 | 1.9 ± 0.9 | −0.4 ± 1.0 | −0.5 ± 1.1 | 34 (39.1%) | 41 (47.1%) | |||||
| 8. Eructation | OLL2716 | 2.0 ± 0.9 | 1.8 ± 0.8 | 1.8 ± 0.9 | −0.2 ± 0.9 | 0.671 | −0.2 ± 0.9 | 0.830 | 27 (31.0%) | 0.522 | 29 (33.3%) | 0.528 |
| Placebo | 2.1 ± 1.1 | 1.9 ± 0.8 | 1.8 ± 0.8 | −0.3 ± 1.1 | −0.3 ± 1.0 | 32 (36.8%) | 34 (39.1%) | |||||
| 9. Increased flatus | OLL2716 | 2.4 ± 1.0 | 2.2 ± 0.9 | 2.0 ± 0.8 | −0.2 ± 1.0 | 0.821 | −0.4 ± 1.0 | 0.605 | 32 (36.8%) | 0.751 | 39 (44.8%) | 0.646 |
| Placebo | 2.5 ± 1.2 | 2.3 ± 1.1 | 2.1 ± 0.9 | −0.2 ± 1.1 | −0.4 ± 1.0 | 29 (33.3%) | 35 (40.2%) | |||||
| 10. Decreased passage of stools | OLL2716 | 2.4 ± 1.1 | 2.1 ± 1.0 | 1.8 ± 0.9 | −0.3 ± 1.0 | 0.479 | −0.6 ± 1.1 | 0.526 | 33 (37.9%) | 0.877 | 42 (48.3%) | 0.543 |
| Placebo | 2.4 ± 1.4 | 2.0 ± 1.2 | 1.9 ± 1.0 | −0.4 ± 1.1 | −0.5 ± 1.2 | 35 (40.2%) | 37 (42.5%) | |||||
| 11. Increased passage of stools | OLL2716 | 2.1 ± 1.1 | 1.9 ± 1.0 | 1.6 ± 0.7 | −0.1 ± 1.0 | 0.532 | −0.4 ± 0.9 | 0.147 | 27 (31.0%) | 0.747 | 34 (39.1%) | 0.264 |
| Placebo | 1.9 ± 1.1 | 1.7 ± 1.1 | 1.7 ± 1.0 | −0.2 ± 1.0 | −0.2 ± 1.1 | 30 (34.5%) | 26 (29.9%) | |||||
| 12. Loose stools | OLL2716 | 2.0 ± 1.0 | 1.9 ± 0.9 | 1.7 ± 0.7 | −0.1 ± 0.9 | 0.813 | −0.3 ± 0.8 | 0.617 | 26 (29.9%) | 1.000 | 29 (33.3%) | 1.000 |
| Placebo | 1.9 ± 1.1 | 1.7 ± 0.8 | 1.6 ± 0.8 | −0.2 ± 1.1 | −0.3 ± 1.1 | 25 (28.7%) | 28 (32.2%) | |||||
| 13. Hard stools | OLL2716 | 2.2 ± 1.1 | 2.1 ± 1.0 | 1.8 ± 0.8 | −0.1 ± 0.9 | 0.273 | −0.4 ± 1.0 | 0.827 | 29 (33.3%) | 0.347 | 33 (37.9%) | 0.757 |
| Placebo | 2.3 ± 1.2 | 1.9 ± 1.0 | 1.9 ± 1.0 | −0.3 ± 1.1 | −0.4 ± 1.2 | 36 (41.4%) | 36 (41.4%) | |||||
| 14. Urgent need for defecation | OLL2716 | 2.2 ± 1.0 | 2.2 ± 1.0 | 1.8 ± 0.8 | 0.0 ± 1.1 | 0.598 | −0.4 ± 1.0 | 0.151 | 25 (28.7%) | 1.000 | 34 (39.1%) | 0.637 |
| Placebo | 2.2 ± 1.2 | 2.2 ± 1.1 | 2.1 ± 1.1 | 0.0 ± 1.1 | −0.1 ± 1.2 | 26 (29.9%) | 30 (34.5%) | |||||
| 15. Feeling of incomplete evacuation | OLL2716 | 2.4 ± 1.1 | 2.2 ± 0.9 | 1.9 ± 0.9 | −0.2 ± 1.1 | 0.510 | −0.5 ± 1.0 | 0.225 | 31 (35.6%) | 0.630 | 41 (47.1%) | 0.358 |
| Placebo | 2.3 ± 1.0 | 2.2 ± 1.0 | 2.0 ± 0.9 | −0.1 ± 0.9 | −0.3 ± 1.0 | 27 (31.0%) | 34 (39.1%) | |||||
| RS (2 and 3) | OLL2716 | 2.1 ± 0.8 | 1.9 ± 0.7 | 1.7 ± 0.7 | −0.2 ± 0.8 | 0.780 | −0.4 ± 0.7 | 0.762 | 31 (35.6%) | 0.639 | 50 (57.5%) | 0.648 |
| Placebo | 2.0 ± 0.8 | 1.8 ± 0.7 | 1.6 ± 0.7 | −0.3 ± 0.9 | −0.4 ± 0.9 | 35 (40.2%) | 46 (52.9%) | |||||
| AP (1, 4, and 5) | OLL2716 | 2.1 ± 0.8 | 1.8 ± 0.8 | 1.7 ± 0.7 | −0.3 ± 0.9 | 0.251 | −0.5 ± 0.8 | 0.126 | 44 (50.6%) | 0.362 | 54 (62.1%) | 0.169 |
| Placebo | 2.0 ± 0.8 | 1.9 ± 0.8 | 1.7 ± 0.8 | −0.2 ± 0.7 | −0.3 ± 0.8 | 37 (42.5%) | 44 (50.6%) | |||||
| IS (6, 7, 8, and 9) | OLL2716 | 2.3 ± 0.8 | 2.1 ± 0.7 | 2.0 ± 0.7 | −0.2 ± 0.8 | 0.370 | −0.3 ± 0.8 | 0.859 | 32 (36.8%) | 0.219 | 48 (55.2%) | 0.363 |
| Placebo | 2.4 ± 0.9 | 2.1 ± 0.8 | 2.0 ± 0.8 | −0.3 ± 0.8 | −0.4 ± 0.9 | 41 (47.1%) | 41 (47.1%) | |||||
| CS (10, 13, and 15) | OLL2716 | 2.4 ± 0.9 | 2.1 ± 0.8 | 1.8 ± 0.8 | −0.2 ± 0.8 | 0.775 | −0.5 ± 0.8 | 0.227 | 41 (47.1%) | 0.879 | 54 (62.1%) | 0.221 |
| Placebo | 2.3 ± 1.0 | 2.1 ± 1.0 | 1.9 ± 0.9 | −0.3 ± 0.8 | −0.4 ± 0.9 | 43 (49.4%) | 45 (51.7%) | |||||
| DS (11, 12, and 14) | OLL2716 | 2.1 ± 0.9 | 2.0 ± 0.8 | 1.7 ± 0.7 | −0.1 ± 0.8 | 0.638 | −0.4 ± 0.7 | 0.127 | 32 (36.8%) | 1.000 | 45 (51.7%) | 0.288 |
| Placebo | 2.0 ± 1.0 | 1.9 ± 0.8 | 1.8 ± 0.8 | −0.1 ± 0.7 | −0.2 ± 0.9 | 31 (35.6%) | 37 (42.5%) | |||||
| Upper GI (RS, AP, and IS) | OLL2716 | 2.2 ± 0.7 | 2.0 ± 0.6 | 1.8 ± 0.6 | −0.2 ± 0.7 | 0.970 | −0.4 ± 0.7 | 0.424 | 28 (32.2%) | 0.271 | 47 (54.0%) | 0.225 |
| Placebo | 2.2 ± 0.8 | 2.0 ± 0.7 | 1.8 ± 0.7 | −0.2 ± 0.7 | −0.4 ± 0.7 | 36 (41.4%) | 38 (43.7%) | |||||
| Lower GI (CS and DS) | OLL2716 | 2.2 ± 0.8 | 2.1 ± 0.7 | 1.8 ± 0.6 | −0.1 ± 0.7 | 0.730 | −0.4 ± 0.7 | 0.078 | 36 (41.4%) | 0.533 | 52 (59.8%) | 0.048 |
| Placebo | 2.2 ± 0.9 | 2.0 ± 0.7 | 1.9 ± 0.7 | −0.2 ± 0.6 | −0.3 ± 0.8 | 31 (35.6%) | 38 (43.7%) | |||||
| Over-all | OLL2716 | 2.2 ± 0.6 | 2.0 ± 0.6 | 1.8 ± 0.6 | −0.2 ± 0.7 | 0.855 | −0.4 ± 0.6 | 0.160 | 19 (21.8%) | 0.229 | 39 (44.8%) | 0.041 |
| Placebo | 2.2 ± 0.7 | 2.0 ± 0.6 | 1.8 ± 0.7 | −0.2 ± 0.6 | −0.3 ± 0.7 | 27 (31.0%) | 25 (28.7%) | |||||
| Items | Score Change before Ingestion (⊿) | Number of Participants with Improved Scores (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | 0 Week | 6 Weeks | 12 Weeks | 6 Weeks–0 Week | p Value 1 | 12 Weeks–0 Week | p Value 1 | 6 Weeks | p Value 2 | 12 Weeks | p Value 2 | |||
| 1. Appetite | OLL2716 | 3.3 ± 0.5 | 3.4 ± 0.5 | 3.4 ± 0.6 | 0.1 ± 0.5 | 0.393 | 0.1 ± 0.6 | 0.207 | 6 | (6.9%) | 0.307 | 7 | (8.0%) | 0.331 |
| Placebo | 3.3 ± 0.6 | 3.4 ± 0.6 | 3.4 ± 0.6 | 0.0 ± 0.6 | 0.1 ± 0.6 | 11 | (12.6%) | 12 | (13.8%) | |||||
| 2. Feeling full | OLL2716 | 3.7 ± 0.5 | 3.7 ± 0.4 | 3.8 ± 0.4 | 0.1 ± 0.4 | 0.502 | 0.1 ± 0.5 | 0.781 | 5 | (5.7%) | 0.188 | 4 | (4.6%) | 0.535 |
| Placebo | 3.7 ± 0.5 | 3.7 ± 0.4 | 3.8 ± 0.4 | 0.0 ± 0.5 | 0.1 ± 0.5 | 11 | (12.6%) | 7 | (8.0%) | |||||
| 3. Feeling hungry | OLL2716 | 3.0 ± 0.7 | 3.0 ± 0.8 | 3.1 ± 0.8 | 0.1 ± 0.7 | 0.570 | 0.1 ± 0.8 | 0.020 | 13 | (14.9%) | 0.685 | 13 | (14.9%) | 0.063 |
| Placebo | 3.1 ± 0.8 | 3.2 ± 0.7 | 3.0 ± 0.7 | 0.0 ± 0.7 | –0.1 ± 0.8 | 16 | (18.4%) | 24 | (27.6%) | |||||
| 4. Food tastes | OLL2716 | 3.6 ± 0.6 | 3.7 ± 0.6 | 3.7 ± 0.7 | 0.1 ± 0.6 | 0.271 | 0.1 ± 0.6 | 0.330 | 6 | (6.9%) | 0.432 | 9 | (10.3%) | 0.194 |
| Placebo | 3.7 ± 0.6 | 3.7 ± 0.6 | 3.8 ± 0.7 | 0.1 ± 0.6 | 0.1 ± 0.7 | 10 | (11.5%) | 16 | (18.4%) | |||||
| 5. Food tastes compared to when younger | OLL2716 | 3.2 ± 0.6 | 3.3 ± 0.6 | 3.2 ± 0.6 | 0.0 ± 0.6 | 0.538 | 0.0 ± 0.7 | 0.873 | 9 | (10.3%) | 1.000 | 13 | (14.9%) | 1.000 |
| Placebo | 3.3 ± 0.6 | 3.4 ± 0.7 | 3.3 ± 0.6 | 0.1 ± 0.6 | 0.0 ± 0.6 | 9 | (10.3%) | 12 | (13.8%) | |||||
| 6. Meal frequency a day | OLL2716 | 3.8 ± 0.4 | 3.8 ± 0.4 | 3.9 ± 0.4 | 0.0 ± 0.3 | 0.314 | 0.0 ± 0.4 | 0.162 | 3 | (3.4%) | 0.720 | 2 | (2.3%) | 1.000 |
| Placebo | 3.9 ± 0.3 | 3.9 ± 0.4 | 3.9 ± 0.3 | 0.0 ± 0.4 | 0.0 ± 0.2 | 5 | (5.7%) | 2 | (2.3%) | |||||
| 7. Feeling sick or nauseated when eating | OLL2716 | 4.1 ± 0.7 | 4.3 ± 0.7 | 4.4 ± 0.7 | 0.2 ± 0.7 | 0.367 | 0.3 ± 0.7 | 0.210 | 11 | (12.6%) | 0.524 | 9 | (10.3%) | 0.194 |
| Placebo | 4.2 ± 0.7 | 4.3 ± 0.7 | 4.3 ± 0.7 | 0.1 ± 0.9 | 0.1 ± 0.9 | 15 | (17.2%) | 16 | (18,4%) | |||||
| 8. Usual mood | OLL2716 | 3.4 ± 0.6 | 3.4 ± 0.6 | 3.4 ± 0.6 | 0.0 ± 0.5 | 0.087 | 0.0 ± 0.5 | 0.070 | 9 | (10.3%) | 0.794 | 7 | (10.3%) | 0.794 |
| Placebo | 3.3 ± 0.5 | 3.4 ± 0.6 | 3.4 ± 0.5 | 0.1 ± 0.5 | 0.1 ± 0.5 | 7 | (8.0%) | 7 | (8.0%) | |||||
| 2 and 3 | OLL2716 | 6.7 ± 0.9 | 6.8 ± 0.9 | 6.9 ± 1.0 | 0.1 ± 0.8 | 0.603 | 0.3 ± 1.0 | 0.045 | – | – | – | – | ||
| Placebo | 6.9 ± 0.9 | 6.9 ± 0.8 | 6.9 ± 0.8 | 0.0 ± 0.9 | 0.0 ± 1.0 | – | – | – | – | |||||
| 1, 2, and 3 | OLL2716 | 9.9 ± 1.2 | 10.1 ± 1.2 | 10.3 ± 1.3 | 0.2 ± 1.0 | 0.531 | 0.4 ± 1.3 | 0.022 | – | – | – | – | ||
| Placebo | 10.2 ± 1.3 | 10.3 ± 1.1 | 10.3 ± 1.1 | 0.1 ± 1.2 | 0.0 ± 1.3 | – | – | – | – | |||||
| Over-all | OLL2716 | 28.1 ± 2.5 | 28.7 ± 2.3 | 29.0 ± 2.5 | 0.6 ± 2.0 | 0.711 | 0.9 ± 2.4 | 0.144 | – | – | – | – | ||
| Placebo | 28.6 ± 2.4 | 29.0 ± 2.5 | 29.0 ± 2.3 | 0.4 ± 2.2 | 0.4 ± 2.3 | – | – | – | – | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, N.; Kobayashi, K.; Nagira, A.; Toshimitsu, T.; Sato, A.; Kano, H.; Hojo, K. The Beneficial Effects of Regular Intake of Lactobacillus paragasseri OLL2716 on Gastric Discomfort in Healthy Adults: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients 2024, 16, 3188. https://doi.org/10.3390/nu16183188
Yamada N, Kobayashi K, Nagira A, Toshimitsu T, Sato A, Kano H, Hojo K. The Beneficial Effects of Regular Intake of Lactobacillus paragasseri OLL2716 on Gastric Discomfort in Healthy Adults: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients. 2024; 16(18):3188. https://doi.org/10.3390/nu16183188
Chicago/Turabian StyleYamada, Naruomi, Kyosuke Kobayashi, Akika Nagira, Takayuki Toshimitsu, Asako Sato, Hiroshi Kano, and Kenichi Hojo. 2024. "The Beneficial Effects of Regular Intake of Lactobacillus paragasseri OLL2716 on Gastric Discomfort in Healthy Adults: A Randomized, Double-Blind, Placebo-Controlled Study" Nutrients 16, no. 18: 3188. https://doi.org/10.3390/nu16183188
APA StyleYamada, N., Kobayashi, K., Nagira, A., Toshimitsu, T., Sato, A., Kano, H., & Hojo, K. (2024). The Beneficial Effects of Regular Intake of Lactobacillus paragasseri OLL2716 on Gastric Discomfort in Healthy Adults: A Randomized, Double-Blind, Placebo-Controlled Study. Nutrients, 16(18), 3188. https://doi.org/10.3390/nu16183188






